Introduction
Obstructive sleep apnea (OSA) is a common sleep
disorder characterized by repetitive partial or complete
obstruction of the upper airway during sleep, leading to the
disruption of breathing and sleeping. Body mass index (BMI) and the
apnea-hypopnea index (AHI) are frequent measures used to evaluate
the severity of OSA (1). The
Epworth sleepiness scale (ESS) is a commonly used questionnaire to
assess subjective daytime sleepiness in patients with sleep
disorders. This questionnaire asks individuals to rate their
likelihood of falling asleep during eight different daily
situations on a scale of 0 to 3 for each question. The scoring
range of the ESS is from 0 to 24, and a higher score implies a more
pronounced tendency for daytime sleepiness (2). BMI is a measure of body mass based on
height and weight, while AHI measures the number of apneas and
hypopneas per hour of sleep (3).
As defined, apnea is when the flow of air is ceased for a minimum
of 10 sec, while hypopnea denotes a decrease in airflow below the
threshold outlined in the definition of apnea (4). Obesity is a chronic disease that is
complex and multifactorial in nature, and it is the most prevalent
condition of fat metabolism among humans. This condition arises due
to a combination of genetic and environmental factors (5). Insufficient sleep, poor sleep quality
and delayed bedtime are linked with the overconsumption of food,
inferior dietary habits and the development of obesity (6).
The aim of the present epidemiological study on
sleep was to determine the possible correlation between BMI and the
AHI index, and the ESS in an Iraqi population.
Subjects and methods
Study design
The present study was a cross-sectional study
conducted between February, 2019 and March, 2021. The study was
written in line with the STROCSS 2019 Guideline (7).
Study setting
The data for the present study were obtained by
evaluating the records of 150 consecutive participants who
underwent sleep assessments at a community-based healthcare
facility (Faruq Medical City, Sulaimani, Iraq) from 2019 to
2021.
The collected data included various parameters, such
as the age, BMI and ESS scores of the participants, as well as the
presence or absence of excessive daytime sleepiness and AHI. BMI
was computed by dividing the body weight in kilograms by the height
in meters squared. The ESS scores ranged from 0 to 24, with scores
>10 indicating abnormal levels of daytime sleepiness. A BMI
>25 kg/m2 was regarded as overweight for both males
and females. AHI was assessed through the utilization of an
ambulatory sleep study known as ApneaLink Plus (ALP) Polygraphy
(ResMed UK Ltd.). Sleep apnea refers to the temporary and often
recurring cessation of breath or significant reduction in airflow
for ≥10 sec during sleep. This type of apnea occurs when the upper
airway is partially or completely blocked, which is known as OSA.
Hypopnea represents a partial loss or reduction in airflow of
breath for ≥10 sec during sleep, typically associated with slow
breathing, which is common in sleep apnea, particularly in OSA
(with a noticeable reduction of at least 50%). To calculate AHI,
the total count of apneas and hypopneas was measured and then
divided this sum by the total duration of sleep (in hours).
Eligibility criteria
The inclusion criteria included individuals who
experienced sleep-related breathing issues (snoring with or without
apneic attacks) and/or excessive daytime sleepiness
(hypersomnolence). The ESS score was used as an objective measure
of daytime sleepiness, and participants with a score >10 or
<10 who still reported sleep-related breathing problems and
excessive daytime sleepiness were also included.
Statistical analysis
Statistical analysis was performed using SPSS
software version 26 (IBM Corp.), and the outcomes are presented as
the mean ± standard deviation. Continuous variables were analyzed
using one-way ANOVA and numerical data were analyzed using the
Chi-squared test. Pearson's and Spearman's correlation analyses
were utilized to measure the degree of correlation between the
variables (presenting as R or Rho values, respectively). A value of
P<0.05 was considered to indicate a statistically significant
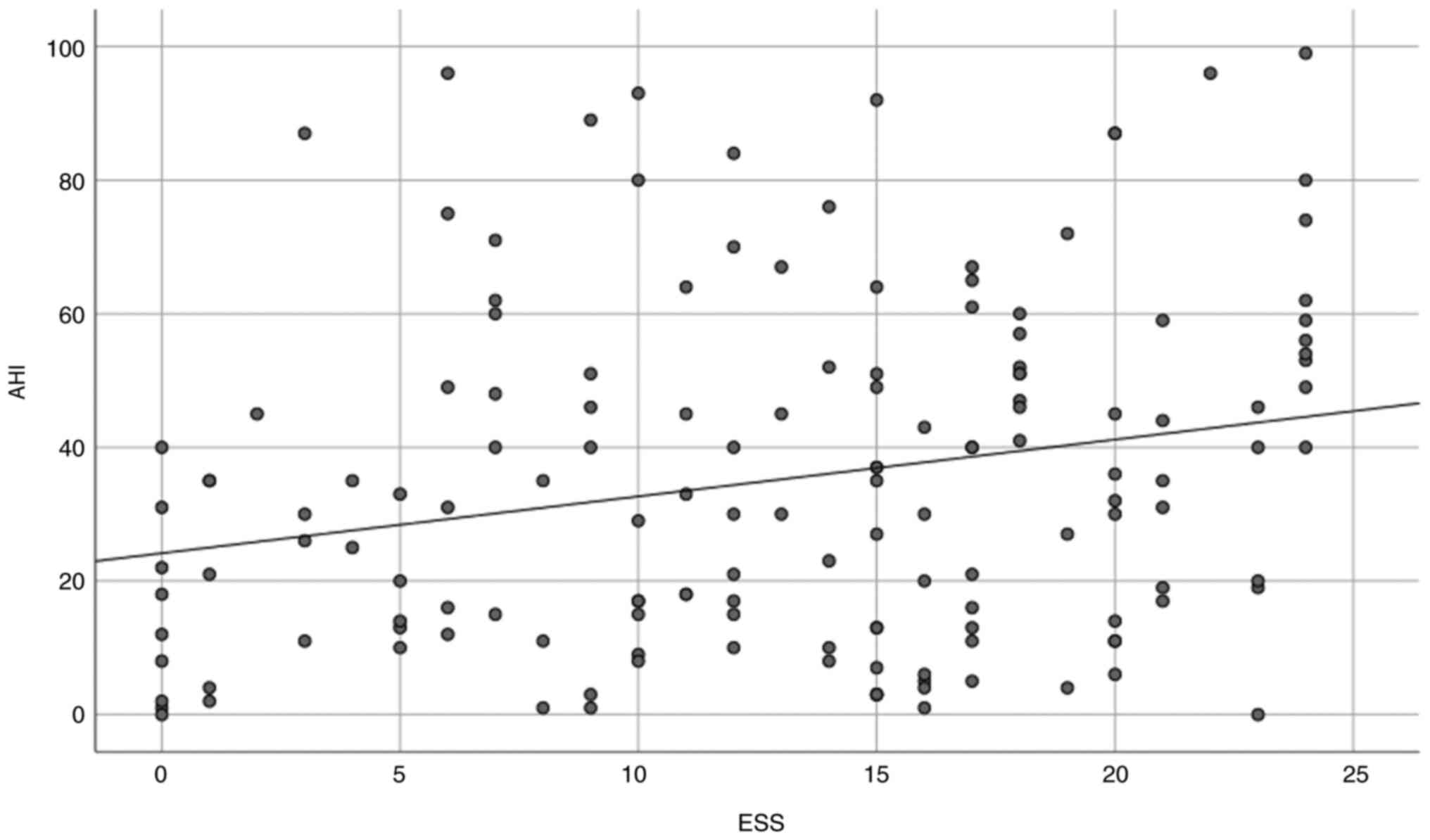
difference. A regression estimation graph was utilized to
illustrate the association between ESS and AHI.
Results
The present study included a total of 150 cases with
an equal sex distribution. The age of the participants ranged from
18 to 79 years in males, and it was between 31 and 82 years in
females. A statistical variation was observed between the age
(P=0.001) and BMI (P=0.001) of the males and females, whereas the
ESS was found to be comparable in both groups. Furthermore, no
statistically significant difference was observed between sex and
AHI (P=0.180; Table I). No
correlation was found between ESS and AHI in females (Rho=0.025,
P=0.834); however, a correlation was found in males (Rho=0.468,
P=0.001) and when the information of both sexes was assessed
collectively (Rho=0.244, P=0.003; Table II and Fig. 1).
 | Table IDistribution of the demographic data
of the study subjects. |
Table I
Distribution of the demographic data
of the study subjects.
| Characteristic | Males (n=75) | Females (n=75) | Total (n=150) | P-value |
|---|
| Mean age (years) | 49.04±13.743 | 60.9±11.581 | 54.97±13.995 | 0.001a |
| Mean BMI
(kg/m2) | 34.99±8.216 | 43.32±10.166 | 39.15±10.116 |
<0.001a |
| Mean ESS | 12.07±7.136 | 13.85±6.772 | 12.96±6.991 | P=0.424b |
| Mean AHI | 37.99±17.011 | 32.37±12.288 | 35.18±15.058 | P=0.180a |
 | Table IIResults of the correlation analyses
between BMI, ESS and AHI. |
Table II
Results of the correlation analyses
between BMI, ESS and AHI.
| Correlations
examined | Males (n=75) | Females (n=75) | Total (n=150) |
|---|
| ESS and AHI | Rho=0.468 | Rho=0.025 | Rho=0.244 |
| | P=0.001a | P=0.834 | P=0.003a |
| BMI and AHI | R=0.294 | R=0.254 | R=0.197 |
| | P=0.011a | P=0.028a | P=0.016a |
| ESS and BMI | Rho=0.077 | Rho=0.132 | Rho=0.170 |
| | P=0.510 | P=0.260 | P=0.037 |
A significant correlation was discovered between BMI
and AHI in both sexes (males: R=0.294, P=0.011; females: R=0.254,
P=0.028), as well as in the combined data of both sexes (R=0.197,
P=0.016) (Table II).
Of note, no correlation was found between ESS and
BMI in males (Rho=0.077, P=0.510), females (Rho=0.132, P=0.260).
However, a significant correlation was found when the data of both
sexes was assessed collectively (Rho=0.170, P=0.037) (Table II).
Discussion
The correlation between BMI, AHI and ESS is a key
topic in the field of sleep medicine. The ESS is a self-report
questionnaire that is widely used to assess daytime sleepiness,
while BMI is a measure of body weight relative to height and AHI is
a measure of the severity of sleep-disordered breathing (3,8).
Individuals who are overweight or obese have a higher prevalence of
obstructive sleep apnea, which occurs when the upper airway of an
individual becomes narrowed or blocked during sleep due to the
accumulation of fat in the neck region, known as pharyngeal fat.
This can cause snoring as air has to squeeze through the restricted
airway, and dietary habits play a crucial role in OSA; some authors
have demonstrated a negative association between fiber-rich
nutrients and OSA severity, while a positive association with
high-fat food consumption has been demonstrated (3,9).
The present study found a significant positive
correlation between ESS and AHI, indicating that a higher AHI
severity is associated with higher ESS scores. This association was
noted in males when data from both sexes were analyzed separately.
It was previously observed that in females, correlations between
ESS and AHI were only observed in severe sleep-disordered
breathing; however, this correlation was notably weaker compared to
males (10). However, as one of
the limitations of the present study, sleep-disordered breathing
was not concluded in the participants examined herein. The finding
of the present study is in accordance with that of a
cross-sectional study conducted by Lipford et al (10). Sleep deprivation has been linked to
increases in the levels of ghrelin, a hormone that stimulates
appetite. As a result, individuals may experience an increase in
cravings for high-calorie foods (7,11).
Further evidence indicates that not getting a sufficient amount of
sleep can result in excessive eating and obesity and a decrease in
the amount of fat that is lost during calorie restriction (12).
The present study did not find any association
between ESS and BMI, which is in line with the findings of the
study by Roure et al (8).
However, when the data for both sexes were collectively analyzed, a
statistically significant correlation was found between ESS and
BMI. This finding aligns with the hypothesis presented in the study
by Basta and Vgontzas (11), which
indicated that metabolic factors may not have a significant
influence on ESS. Furthermore, excess body fat around the abdomen
can lead to the compression of the chest wall, resulting in a
decrease in lung volume. This reduction in airflow can cause the
upper airway to collapse during sleep, increasing the likelihood of
OSA. The risk of developing this condition increases as BMI
increases. Even a 10% increase in weight can elevate the risk of
OSA by up to 6-fold. Ciavarella et al (3) found no correlation between BMI and
AHI, and Basta and Vgontzas (11)
claimed that obesity-related objective daytime sleepiness was less
associated with OSA and these findings are in contrast with those
of the present study; herein, a correlation was found between these
two factors. However, this finding is consistent with the findings
of the study by Soylu et al (13); their study demonstrated that an
increase in BMI, waist circumference and neck circumference was
associated with a greater severity of OSA (13). It is important to note that the
present study study was limited first by its sample size, which may
limit the generalizability of the findings to larger populations.
Second, the present study did not include data regarding the
comorbidities of the participants in the questionnaire.
In conclusion, the present study found a clear
correlation between being overweight or obese and AHI; the majority
of the study subjects with AHI had a BMI >25 kg/m2.
The correlation analysis revealed a significant correlation between
BMI and AHI, indicating that the severity of sleep apnea worsens
with higher BMI values. This correlation was observed in both males
and females.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HMWA and HMA were major contributors to the
conception of the study, as well as in the literature search for
related studies. HOA, SMA and FHK were involved in the literature
review, in the writing of the manuscript and in the design of the
study. SFA, FHF, BAA and KAOK were involved in the literature
review, in the design of the study, in the critical revision of the
manuscript and in the processing of the figure. FHK and HMWA
confirm the authenticity of all the raw data. SJH, SOK and SHM were
involved in data collection and analysis. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from all the
study subjects for their participation in the present study.
Ethical approval was obtained from the Ethics Committee of the
University of Sulaimani (Sulaimani, Iraq; reference no. 88).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ip MS, Lam BI, Ng MMT, Lam WK, Tsang KWT
and Lam KSL: Obstructive sleep apnea is independently associated
with insulin resistance. Am J Respir Crit Care Med. 165:670–676.
2002.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Johns MW: A new method for measuring
daytime sleepiness: The Epworth sleepiness scale. Sleep.
14:540–545. 1991.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ciavarella D, Tepedino M, Chimenti C,
Troiano G, Mazzotta M, Foschino Barbaro MP, Lo Muzio L and Cassano
M: Correlation between body mass index and obstructive sleep apnea
severity indexes-a retrospective study. Am J Otolaryngol.
39:388–391. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gulotta G, Iannella G, Vicini C, Polimeni
A, Greco A, de Vincentiis M, Visconti IC, Meccariello G, Cammaroto
G, De Vito A, et al: Risk factors for obstructive sleep apnea
syndrome in children: State of the art. Int J Environ Res Public
Health. 16(3235)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gullvåg M, Gjeilo KH, Fålun N, Norekvål
TM, Mo R and Broström A: Sleepless nights and sleepy days: A
qualitative study exploring the experiences of patients with
chronic heart failure and newly verified sleep-disordered
breathing. Scand J Caring Sci. 33:750–759. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Papaconstantinou E, Quick V, Vogel E,
Coffey S, Miller A and Zitzelsberger H: Exploring relationships of
sleep duration with eating and physical activity behaviors among
Canadian university students. Clocks Sleep. 2:194–207.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Agha R, Abdall-Razak A, Crossley E, Dowlut
N, Iosifidis C and Mathew G: STROCSS Group. STROCSS 2019 guideline:
Strengthening the reporting of cohort studies in surgery. Int J
Surg. 72:156–165. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Roure N, Gomez S, Mediano O, Duran J, de
la Peña M, Capote F, Capote F, Teran J, Masa JF, Alonso ML, et al:
Daytime sleepiness and polysomnography in obstructive sleep apnea
patients. Sleep Med. 9:727–731. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lin YC: The predictive relationship of
health related quality of life on objectively-measured sleep in
children: A comparison across BMI ranges. Front Neurosci.
13(1003)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lipford MC, Wahner-Roedler DL, Welsh GA,
Mandrekar J, Thapa P and Olson EJ: Correlation of the Epworth
sleepiness scale and sleep-disordered breathing in men and women. J
Clin Sleep Med. 15:33–38. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Basta M and Vgontzas AN: Metabolic
abnormalities in obesity and sleep apnea are in a continuum. Sleep
Med. 1:5–7. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sun Y, Ning Y, Huang L, Lei F, Li Z, Zhou
G and Tang X: Polysomnographic characteristics of daytime
sleepiness in obstructive sleep apnea syndrome. Sleep Breath.
16:375–381. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Soylu AC, Levent E, Sarıman N, Yurtlu Ş,
Alparslan S and Saygı A: Obstructive sleep apnea syndrome and
anthropometric obesity indexes. Sleep Breath. 16:1151–1158.
2012.PubMed/NCBI View Article : Google Scholar
|