Introduction
Granulomatous mastitis (GM) is a rare breast
inflammation, affecting ~2.4 out of every 100,000 females in the
USA (1). Typically, GM is defined
by non-caseating granulomatous inflammation occurring near the
ducts and lobules of the breast. These granulomas are often
unilateral and commonly present as a solid mass in the upper outer
quadrant of the breast (2).
GM can be etiologically classified into two main
categories: Idiopathic GM and secondary GM. An unknown underlying
cause characterizes idiopathic GM, although an autoimmune origin is
widely supported due to its responsiveness to steroid therapy and
its association with autoimmune disorders (3). By contrast, secondary GM results from
identifiable causes, including infectious agents such as
Mycobacterium tuberculosis, fungal or parasitic infections
and bacterial pathogens, as well as systemic diseases such as
sarcoidosis and granulomatosis with polyangiitis (2,3).
Based on clinical, pathological and radiological
findings, GM can easily be mistaken for breast cancer and other
conditions such as tuberculosis, fungal infections and syphilis
(2). Moreover, the presence of GM
alongside other breast pathologies, such as lobular carcinoma in
situ and ductal carcinoma in situ (DCIS), underscores
the complexities of diagnosing this condition (4). The present study describes a rare
case of GM, high-grade DCIS and invasive ductal carcinoma (IDC)
occurring simultaneously in the same breast. The report was
prepared following the CaReL guidelines (5). All references cited were assessed for
eligibility (6).
Case report
Patient information
A 36-year-old woman presented to Smart Health Tower,
Sulaymaniyah, Iraq, with a 2-week history of pain in her left
breast. She was a mother of 3 children, having breastfed her
children for 4 years, and was currently nursing her youngest. She
had a history of passive smoking, no notable previous medical or
surgical history, and no family history of breast cancer.
Clinical findings
Upon an examination, a large, firm and immovable
lump was detected in the upper outer quadrant of the left breast.
Additionally, palpable lymph nodes (LNs) were noted in the left
axilla.
Diagnostic assessment
A breast ultrasonography (US) revealed a
heterogeneous area with fluid echogenicity and moderate surrounding
edema in the left breast. This resulted in localized skin
thickening and contour distortion at the 2 o'clock position,
measuring 64x27 mm. Several reactive LNs were noted in the left
axilla. The right breast and axilla appeared normal. A follow-up US
revealed similar size and morphological characteristics. A core
needle biopsy (CNB) of the lesion confirmed a diagnosis of
high-grade DCIS with both solid and comedo patterns, along with
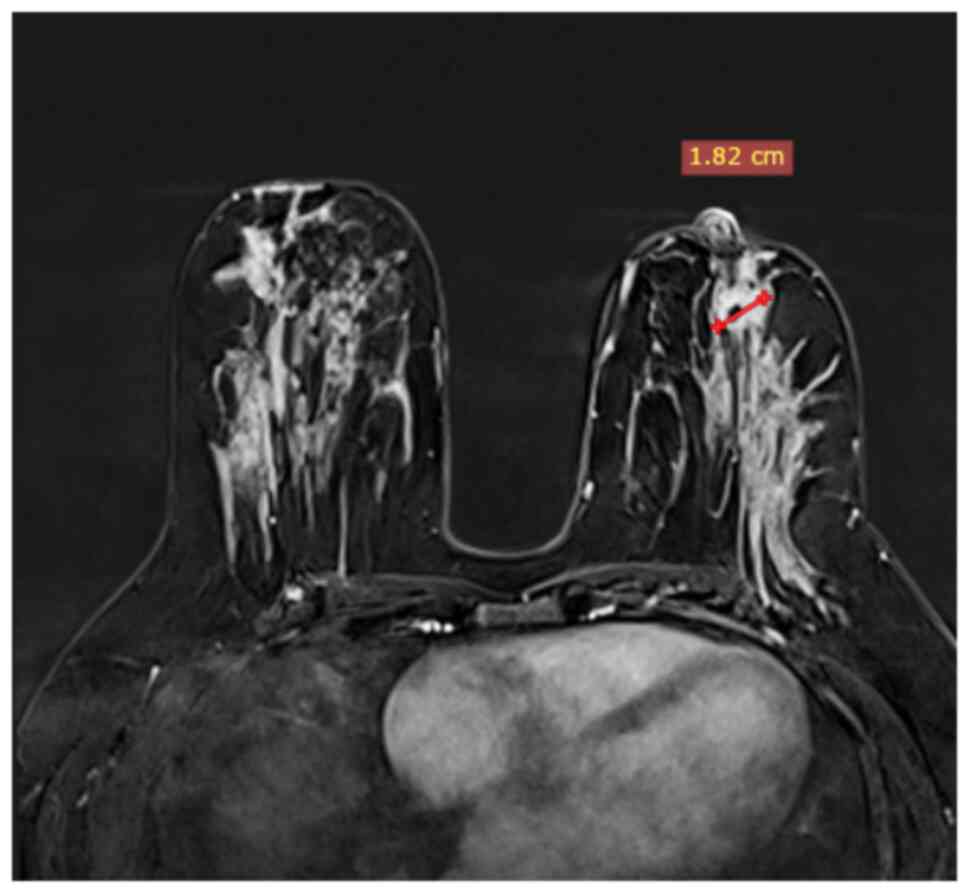
suppurative GM. Subsequent breast magnetic resonance imaging (MRI)
revealed heterogeneous non-mass-like enhancement, a small central
mass measuring 18 mm, and bilateral enlarged axillary LNs (Fig. 1). Fine-needle aspiration of the
bilateral axillary LNs revealed no evidence of malignancy.
Therapeutic intervention
At the initial visit, the patient was prescribed
ibuprofen tablets (200 mg, one tablet twice daily) for 7 days and
amoxicillin/clavulanic acid tablets (875/125 mg, one tablet twice
daily) for 20 days. Following the presentation of the case of the
patient at the multidisciplinary team meeting and additional
investigations, the initial treatment plan included
breast-conserving therapy and sentinel LN biopsy. A comprehensive
pre-operative assessment was conducted, and the patient
subsequently underwent surgery involving a wide local excision of
the breast mass and excision of sentinel-sampled axillary LNs. Both
tissue samples were submitted for histopathological examination
(HPE). The 5-µm-thick sections were fixed in 10% neutral-buffered
formalin at room temperature for 24 h and embedded in paraffin.
They were subsequently stained with hematoxylin and eosin (Bio
Optica Co.) for 1-2 min at room temperature, and then examined
using a light microscope (Leica Microsystems GmbH).
Following discharge, the patient was closely
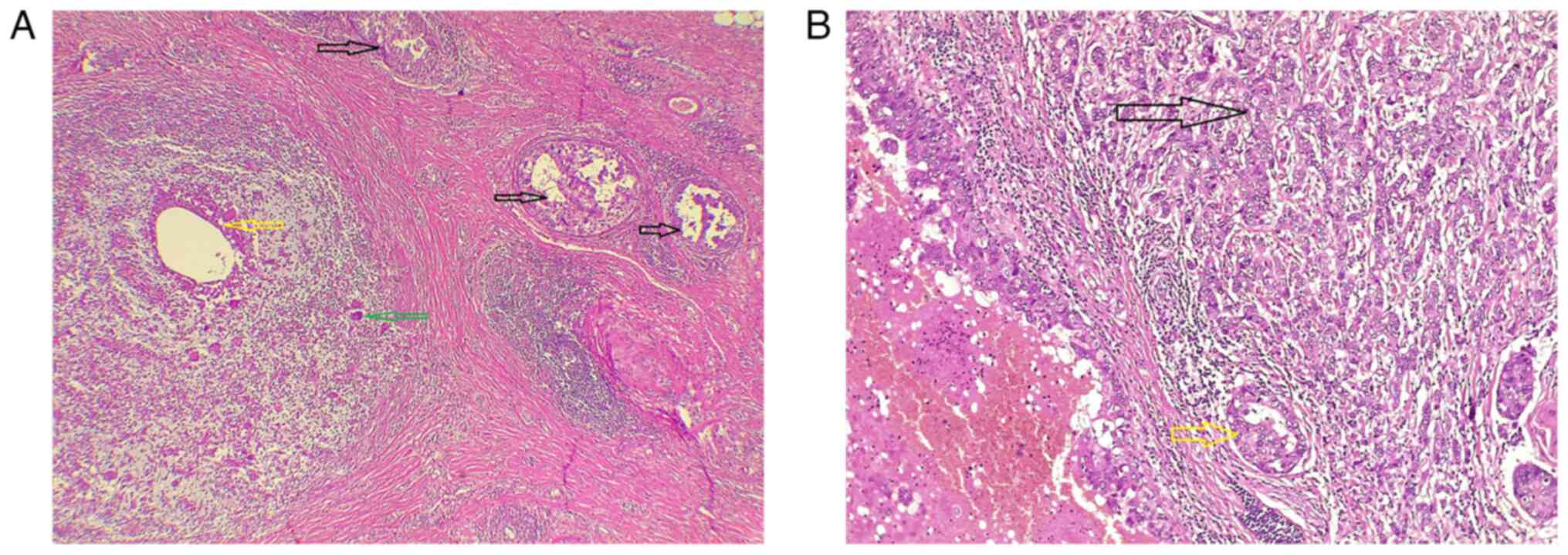
monitored with no post-operative complications. The HPE from the
first surgery revealed IDC of no specific type, poorly
differentiated, with extensive DCIS and suppurative GM (Fig. 2). The tumor was multifocal, and
DCIS involved the inferior margin. Additionally, one of the nine
LNs sampled exhibited macro-metastasis with extra-nodal extension,
resulting in a pathological staging of pT1cN1a (7). A chest, abdomen and pelvis computed
tomography scan confirmed the absence of distant metastasis.
The oncology team recommended a revision of breast
surgery with axillary LN dissection since the patient declined a
mastectomy. Consent was obtained for another surgery in the case
that margin involvement was identified in the HPE. The HPE from the
second operation again indicated the involvement of the inferior
margin by DCIS, leading to the decision for a left completion
mastectomy with immediate reconstruction using a transverse rectus
abdominis myocutaneous (TRAM) flap.
The final HPE revealed high-grade DCIS without
invasive components and clear resection margins. Subsequently, the
patient was referred to an oncologist. The treatment regimen
consisted of six cycles of chemotherapy with Docetaxel (Taxotere)
150 mg IV and carboplatin (Paraplatin) 886.9 mg IV, followed by a
one-year course of trastuzumab (Herceptin) 546 mg IV. Additionally,
endocrine therapy was initiated with oral exemestane (Aromasin) and
subcutaneous Goserelin (Zoladex) injections. Following
chemotherapy, the patient will be referred to a radiation
oncologist to evaluate the need for radiotherapy.
Follow-up
Upon the last follow-up, the patient was monitored
and remained stable with no post-operative complications.
Discussion
In 1972, Kessler and Wolloch (8) reported the first case of GM and noted
that it may be mistaken for breast cancer due to similarities in
clinical signs and presentations. These include lumps, pain,
swelling, skin changes, abscesses, ulcerations, sinus tracts,
fistulas in severe or chronic cases, and occasional association
with axillary lymphadenopathy (8,9).
Typically, GM occurs in women of childbearing age
within 5 years following their last childbirth and is extremely
rare in nulliparous women. The condition often involves abscess
formation, predominantly affecting the lobules, and is
characterized by the absence of caseating granulomas, acid-fast
bacteria, or fungi (10). The
patient in the present case report was a mother of 3 children who
had breastfed for 4 years and was currently nursing her youngest
child.
The development of GM is considered to begin with
damage to the breast ductal epithelium. This damage allows luminal
secretions to spread into the lobular connective tissue, triggering
local inflammation. Subsequently, lymphocytes and macrophages
migrate to the affected area, resulting in a granulomatous
inflammatory response (2).
The diagnosis of GM can often be challenging, as
ultrasound, mammography and MRI findings are typically non-specific
and mainly confirm the presence of a mass, parenchymal
irregularities, or multifocal lesions. Since histology remains the
gold standard for diagnosis, all suspicious areas should be
biopsied. For GM, chronic granulomatous inflammation is identified
by giant cells, leukocytes, epithelioid cells and macrophages
(11).
In some cases, patients initially diagnosed with
breast cancer and treated with mastectomy and LN removal later
find, through pathological analysis, that they had GM (8). Additionally, there are rare instances
where individuals diagnosed with GM and managed non-invasively were
later found to have breast cancer after surgery due to no
significant improvement in their condition (12). The first documented association
between chronic mastitis and malignancy involved five sisters with
chronic mastitis, three of whom subsequently developed breast
cancer (13). Whether the
coexistence of GM and breast cancer is incidental or indicative of
an underlying biological relationship remains uncertain. Some
hypotheses suggest that chronic inflammation, as observed in GM,
may contribute to carcinogenesis through sustained immune
activation, cytokine release, and oxidative stress. However,
current evidence does not support a direct causal link. The
majority of experts consider the two conditions to be coexisting
rather than causally related, with inflammation potentially
unmasking or mimicking an adjacent neoplastic process (9).
The simultaneous presence of GM and breast cancer
has rarely been reported in the literature (4). In a review of the literature
utilizing the PubMed and Google Scholar databases, only 13 cases of
simultaneous GM and breast cancer were identified (9-11,14-21).
The average age of these patients was 43.07±12.10 years, with ages
ranging from 34 to 77 years. Among the patients, 7 (53.85%)
patients had both GM and breast cancer in the left breast, while
only 2 cases (15.38%) involved the conditions in contralateral
breasts. A total of 8 cases (61.54%) had a concurrent diagnosis of
GM and DCIS (Table I). The case
described in the present study was a 36-year-old breastfeeding
woman with suppurative GM, high-grade DCIS and IDC, all localized
in the left breast. This combination of findings is rare and
clinically significant, as it represents only the second reported
case, in which GM, DCIS and IDC were simultaneously identified in
the same breast. The first such case was described by Çalış and
Kilitçi (19), involving a
77-year-old woman who presented with right breast pain, edema and
skin thickening near the areola. A biopsy revealed IDC and DCIS,
and the final mastectomy specimen confirmed the presence of GM as
well. Similar to that report, the case described herein also
presented with breast pain and was ultimately diagnosed with all
three pathologies following wide local excision. However, the case
in the present study is further distinguished by the multifocal
nature of the lesion and persistent positive margins after two
surgeries, which necessitated a completion mastectomy. The
breastfeeding status of the patient, commonly associated with
idiopathic GM, may have contributed to initial diagnostic
uncertainty, as the condition was first managed conservatively.
Taken together, these features underscore the diagnostic and
therapeutic complexity of managing such rare presentations.
 | Table IOverview of literature on the
concurrent presence of granulomatous mastitis and breast
carcinoma. |
Table I
Overview of literature on the
concurrent presence of granulomatous mastitis and breast
carcinoma.
| | IHC | |
|---|
| First author, year of
publication | No. of cases | Age, years/(sex) | Presentation | US findings | MRI findings | MMG | Treatment | Diagnosis | Location | Positive | Negative | Follow-up | (Refs.) |
|---|
| Salih, 2023 | 1 | 34/F | Left breast pain for
7 days. | A full-length ectatic
duct from the nipple root to the 5-7 o'clock position, with
heterogeneous internal echoes, mild edema, and reactive axillary
lymph nodes, suggesting GM recurrence. | A clumped
non-mass-like enhancement of 20x6 mm was found in a focally ectatic
duct in the left breast, with smaller foci of 4-5 mm. The total
area measured 60x50 mm, with a BI-RADS score of MR-4. Additionally,
a focal, heterogeneous, non-mass-like enhancement of 19x13 mm was
noted in the surgical bed, 12 mm from the pectoralis major. (after
a WLE). | In the central part
of the left breast, below the scar line and at mid-depth, there
were two rounded, scattered, faint micro-calcifications. The
BI-RADS score was M2 bilaterally. (after a WLE). | A total mastectomy of
the left breast and WLE of the right breast. | GM and DCIS | Left breast | ER | N/A | Disease-free after 6
months | (9) |
| Yoshida, 2023 | 1 | 34/F | A mass and redness in
the left breast. | An irregular
hypoechoic area measuring over 4 cm was found in the left mammary
gland. | Persistent small
nodular and irregular enhancement effects were observed. | N/A | A total mastectomy of
the left breast. | GLM and DCIS | Left breast | ER, PR,
E-cadherin | N/A | Recurrence-free
status for 18 months. | (10) |
| Evans, 2021 | 1 | 35/F | A left breast
mass. | A 60-mm irregularity
with no underlying collection at the 10 o'clock position, 2 cm from
the nipple. | A resectable 60-mm
area in the right outer quadrant | Asymmetric density
with hyperemia was found in the medial left breast. The right
breast had two clusters of irregular pleomorphic
microcalcifications, measuring 16x11x11 mm and 9x10x7 mm. | Oncoplastic right WLE
with SLNB, subsequently requiring an axillary dissection due to
Macro metastatic axillary disease. | GM and high-grade
DCIS | Right breast IDC and
Left breast GM | PR | HER2 | N/A | (11) |
| Zhu, 2023 | 3 | 51/F | A hard mass in the
left breast for one day. | Left breast edema
with dilated ducts led to the consideration of an inflammatory
lesion. | Edema in the
glandular layer of the left breast with dilation of the ducts. | N/A | Surgical dissection
of the lesion. | GLM with solid-type
high-grade DCIS. | Left breast | p63, | ER, PR, HER2 | N/A | (14) |
| | | 50/F | A mass in the left
breast for over six months. | Localized glandular
hypertrophy in the lateral portion of the left breast, with
multiple internal hypoechoic nodules, which were classified as
BI-RADS grade 4a. | A suspicious mass
with shadowing and enlarged ducts was observed in the left breast,
suggesting the potential presence of breast cancer. | Enlarged ducts with
dense calcifications that resemble gravel within the ducts. | Surgical resection of
the lesion. | GLM with solid-type
high-grade DCIS. | Left breast | p63, CK5/6 | ER, PR, HER2 | N/A | (14) |
| | | 45/F | A left breast lump
for two months. | Several dark,
fluid-filled areas were identified, leading to a suspicion of an
inflammatory lesion. | N/A | N/A | Mass resection | GLM with solid-type
high-grade DCIS. | Left breast | p63, CK5/6 | ER, PR, HER2 | N/A | (14) |
| Tavakol, 2022 | 1 | 35/F | Pain and a small mass
in the right breast for one month; a small mass in the left breast
for 6 years. | A diffuse, irregular
area with microcalcifications and skin thickening (BIRADS 4b) was
noted in the right UOQ. A well-defined hypoechoic mass (BIRADS 3)
was seen in the left breast at 12 o'clock. | Fibroglandular, dense
breast (type C). In the right UOQ, there was asymmetrical
parenchymal thick ening with multiple rim-enhanced masses (14-35
mm) and extensive asymmetrical non-mass enhancement (140x80x60 mm)
extending to the retroareolar region, with a type 3 dynamic
curve. | A large hypoechoic to
heteroechoic mass (150 mm) in the lateral right breast, without
microcalcifications or distortion. | Conservative
treatment | IGM and LCIS | Right breast | P63, CK5/6, P120
catenin, e-cadherin | N/A | N/A | (15) |
| Zangouri, 2022 | 1 | 38/F | A left breast.
mass | An irregular
hypoechoic mass with tubular extensions. | N/A | A well-defined
high-density mass | N/A | GM and grade III
IDC | Left breast | N/A | N/A | N/A | (16) |
| Oddó, 2019 | 1 | 44/F | Swelling and pain
in the left breast. | Inflammatory
changes with skin thickening, increased echogenicity, superficial
fluid collections, and loss of fatty planes. | N/A | Suggestive of DCIS
involvement. | A total mastectomy
of the left breast | GLM and DCIS | Left breast | ER, PR | N/A | N/A | (17) |
| Özşen, 2018 | 1 | 35/F | Swelling in right
breast. | A heterogeneous,
irregular hypoechoic area extending 3 cm from the subareolar zone
in the right breast, with a 34x9 mm fluid collection near the
nipple at 12 o'clock. | N/A | N/A | N/A | GLM and DCIS | Right breast | CD10, CK 5/6,
p63 | N/A | N/A | (18) |
| Çalış, 2018 | 1 | 77/F | Right breast
pain. | Increased fibro
glandular tissue with indistinct borders and an inflammatory
appearance, along with a 2x2 cm non-reactive lymphadenopathy in the
right axilla. | N/A | An amorphous mass
with axillary lymphadenopathy and focal asymmetric opacity with
calcifications in the retroareolar and outer quadrant of the right
breast. | Modified radical
mastectomy | IDC, DCIS, and
GM | Right breast | ER, PR | E-cadherin,
C-erb | N/A | (19) |
| Kaviani, 2017 | 1 | 48/F | Large palpable
masses in both breasts and nipple retraction in her right
breast. | Large irregular
hypoechoic mass with echogenic foci and inflammation, indicating
mastitis. | A single mass in
the left breast measured 20x12 mm with no satellite lesions at the
end of chemotherapy. | Mass-like lesions
and distortion in both breasts due to highly dense breast
tissue. | BCS with
oncoplastic repair (round block technique) and sentinel lymph node
biopsy were performed. | IDC and IGM | Left breast IDC and
right breast GM | N/A | N/A | N/A | (20) |
| Mazlan, 2011 | 1 | 34/F | A right breast
abscess for 8 years, and progressive loss of vision of the left
eye. | N/A | Extensive scarring
in the right breast appeared suspicious for malignancy. | N/A | The patient
declined treatment | CGM and IDC | Right breast | ER, PR | C-erb | Passed away after 6
months | (21) |
Typically, DCIS is characterized by an abnormal
growth of epithelial cells within the mammary ducts without
invasion into other areas of the breast tissue. It is rarely
symptomatic or clinically palpable. The lesion is enclosed by an
intact basement membrane and bordered by a layer of partially
continuous myoepithelial cells (9). Oddó et al (17) reported the case of a 44-year-old
woman who presented with painful swelling in her left breast. The
patient was diagnosed with GM but did not respond to any antibiotic
treatments. A subsequent biopsy confirmed the presence of GM along
with DCIS. Özşen et al (18) described a similar case of a
35-year-old woman with swelling in her right breast. Initially
diagnosed with GM through a core needle biopsy, the patient
underwent excisional surgery due to a poor response to treatment.
The final diagnosis revealed granulomatous lobular mastitis and
DCIS.
Differentiating between breast cancer and GM can be
challenging; however, it is crucial due to the significant
differences in treatment strategies. Currently, histopathological
diagnosis remains the most reliable method (10). Although there are no established
treatment guidelines for GM, steroid therapy is commonly used as
the initial approach. For patients who resist corticosteroid
treatment or suffer from side effects like impaired glucose
tolerance and Cushing's syndrome, adding methotrexate (10-15
mg/week) has been found effective. Incorporating methotrexate helps
reduce the corticosteroid dosage and lowers the likelihood of side
effects (22). However, for
patients diagnosed with DCIS, treatment typically involves a
combination of surgery, radiation, and endocrine therapy (9). The patient in the present study was
initially treated with analgesics and antibiotics for 20 days. An
HPE following a CNB of the lesion confirmed the coexistence of GM
and breast cancer in the same breast. After undergoing two breast
surgeries, the patient had a left complete mastectomy with
immediate reconstruction using a TRAM flap.
For clinicians, this case underscores the necessity
of histopathologic confirmation in all patients with suspected GM,
particularly in cases when the clinical course deviates from the
expected response to therapy. Breast imaging alone is often
insufficient, as both GM and malignancy can present as
heterogeneous, ill-defined, or mass-like lesions on ultrasound and
MRI.
In conclusion, distinguishing between breast cancer
and GM is challenging. Although the simultaneous presence of GM and
breast cancer is rare, it remains essential to consider this
possibility. However, further research is required to clarify the
relationship between GM and breast cancer.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FHK and AMS were major contributors to the
conception of the study, as well as to the literature search for
related studies. HAN, BOH and SHH contributed to the clinical
management of the patient, assisted in data acquisition and
interpretation, and participated in the literature review and
manuscript preparation. SL, HOA and KMS contributed to the
conception and design of the study, the literature review, the
critical revision of the manuscript, and the processing of the
table. LRAP was the radiologist who performed the assessment of the
case. AMS and SL assisted in diagnosing the patient, contributed to
the management of the patient, and participated in manuscript
review. AMA was the pathologist who performed the diagnosis of the
case. RMA was the oncologist involved in the management of the
patient. FHK and HAN confirm the authenticity of all the raw data.
All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for her participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case and any
accompanying images
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Goldman M, Selke HM, Pardo I, Clare SE,
Emerson RE, Howell JF, Shieh WJ, Zaki S, Sanchez C,
Sinkowitz-Cochran RL, et al: Idiopathic granulomatous mastitis in
hispanic Women-Indiana, 2006-2008. MMWR: Morbidity & Mortality
Weekly Report. 58:1317–1321. 2009.PubMed/NCBI
|
|
2
|
Esmaeil NK, Salih AM, Hammood ZD, Pshtiwan
LR, Abdullah AM, Kakamad FH, Abdullah HO, Ahmed GS, Abdalla BA and
Salih RQ: Clinical, microbiological, immunological and hormonal
profiles of patients with granulomatous mastitis. Biomed Rep.
18(41)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wang X, He X, Liu J, Zhang H, Wan H, Luo J
and Yang J: Immune pathogenesis of idiopathic granulomatous
mastitis: From etiology toward therapeutic approaches. Front
Immunol. 15(1295759)2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Esmaeil NK and Salih AM: Investigation of
multi-infections and breast disease comorbidities in granulomatous
mastitis. Ann Med Surg (Lond). 86:1881–1886. 2024.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Prasad S, Nassar M, Azzam AY,
García-Muro-San José F, Jamee M, Sliman RK, Evola G, Mustafa AM,
Abdullah HO, Abdalla BA, et al: CaReL guidelines: A consensus-based
guideline on case reports and literature review (CaReL). Barw Med
J. 2:13–19. 2024.
|
|
6
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
7
|
Amin MB, Edge SB, Greene FL, Byrd DR,
Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR,
Sullivan DC (eds), et al: AJCC Cancer Staging Manual, 8th edition.
Springer, Cham, 2017.
|
|
8
|
Kessler E and Wolloch Y: Granulomatous
mastitis: A lesion clinically simulating carcinoma. Am J Clin
Pathol. 58:642–646. 1972.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Salih AM, Pshtiwan LR, Abdullah AM, Dhahir
HM, Ali HO, Muhialdeen AS, Hussein BO, Hassan SH and Kakamad FH:
Granulomatous mastitis masking ductal carcinoma in situ: A
case report with literature review. Biomed Rep.
20(17)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Yoshida N, Nakatsubo M, Yoshino R, Ito A,
Ujiie N, Yuzawa S and Kitada M: Concurrent granulomatous mastitis
and ductal carcinoma in situ. Cureus. 15(e38377)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Evans J, Sisk L, Chi K, Brown S and To H:
Concurrent granulomatous mastitis and invasive ductal cancer in
contralateral breasts-a case report and review. J Surg Case Rep.
7(rjab519)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sakurai T, Oura S, Tanino H, Yoshimasu T,
Kokawa Y, Kinoshita T and Okamura Y: A case of granulomatous
mastitis mimicking breast carcinoma. Breast Cancer. 9:265–268.
2002.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Handley WS: Chronic mastitis and breast
cancer. Br Med J. 2(113)1938.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhu J, Miao X, Li X, Zhang Y, Lou Y, Chen
H and Liu X: Granulomatous lobular mastitis co-existing with ductal
carcinoma in situ: Report of three cases and review of the
literature. Ann Diagn Pathol. 68(152241)2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tavakol M, Alvand S, Ardalan FA and
Assarian A: Idiopathic granulomatous mastitis with incidental
lobular carcinoma in situ: A case report: IGM with LCIS. Archives
of Breast Cancer. 9 (3-SI):315–319. 2022.
|
|
16
|
Zangouri V, Niazkar HR, Nasrollahi H,
Homapour F, Ranjbar A and Seyyedi MS: Benign or premalignant?
Idiopathic granulomatous mastitis later diagnosed as ductal
carcinoma breast cancer: Case report and review of literature. Clin
Case Rep. 10(e6323)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Oddó D, Domínguez F, Gómez N, Méndez GP
and Navarro ME: Granulomatous lobular mastitis associated with
ductal carcinoma in situ of the breast. SAGE Open Med Case Rep.
7(2050313X19836583)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Özşen M, Tolunay Ş and Gökgöz MŞ: Case
report: Ductal carcinoma in situ within a granulomatous mastitis.
Eur J Breast Health. 14(186)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Çalış H and Kilitçi A: Granulomatous
mastitis concurrence with breast cancer. Eur J Breast Health.
14:58–60. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kaviani A, Zand S, Karbaksh M and Ardalan
FA: Synchronous idiopathic granulomatosis mastitis and breast
cancer: A case report and review of literature. Arch Breast Cancer.
4:32–36. 2017.
|
|
21
|
Mazlan L, Suhaimi SN, Jasmin SJ, Latar NH,
Adzman S and Muhammad R: Breast carcinoma occurring from chronic
granulomatous mastitis. Malays J Med Sci. 19:82–85. 2012.PubMed/NCBI
|
|
22
|
Kim J, Tymms KE and Buckingham JM:
Methotrexate in the management of granulomatous mastitis. ANZ J
Surg. 73:247–249. 2003.PubMed/NCBI View Article : Google Scholar
|