Introduction
Enchondromas are benign tumors composed of mature
hyaline cartilage found within the medullary cavity of bones. They
originate from cartilage cell nests that separate from the central
growth plate during the development process. This leads to the
abnormal accumulation of mature hypertrophic hyaline cartilage that
fails to undergo normal resorption or ossification (1-3).
Enchondromas vary in prevalence depending on their
location within the human body. They constitute ~90% of all bone
tumors in the hand. By contrast, foot enchondromas are much less
frequent and primarily affect the phalanges and metatarsal bones.
While these tumors can occur at any age, they typically manifest
between the first and fourth decades of life, affecting both sexes
equally (1,4,5).
Enchondromas in the small bones of the feet are
typically asymptomatic and are often discovered incidentally during
routine X-ray examinations. When they become symptomatic, patients
may present with pain primarily due to increased pressure from the
growth of the lesion, which can deform the cortex of the affected
bone or from fractures within the lesion, including pathological or
stress fractures. Patients may also report a gradual enlargement of
the affected digit (1,2,6).
Enchondromas in different locations of the foot have
been documented in the literature (1-5,7-12).
The presented study reports a case of symptomatic enchondroma in
the proximal phalanx of the left second toe. The case report has
been prepared in accordance with the CaReL guidelines, and
referenced studies were reviewed to ensure the exclusion of
non-peer-reviewed data (13,14).
Case report
Patient information
A 20-year-old male patient presented to Smart Health
Tower (Sulaymaniyah, Iraq) with a painless, slow-growing lump on
his left second toe, which had gradually caused deformity over the
past 6 months. Over the past 2 weeks, he began experiencing pain
while wearing shoes, hindering his daily activities. He reported no
history of foot trauma, chronic medical conditions, or prior
surgical interventions.
Clinical findings
Upon a physical examination, a hard mass on the
medial border of the proximal phalanx of the left second toe was
found, causing a lateral deviation of the toe (Fig. 1). The mass was firmly fixed to the
underlying bone, with no tenderness upon palpation or signs of
local inflammation. The metatarsophalangeal and interphalangeal
joints exhibited a good range of motion and no sensory deficits in
the toe.
Diagnostic approach
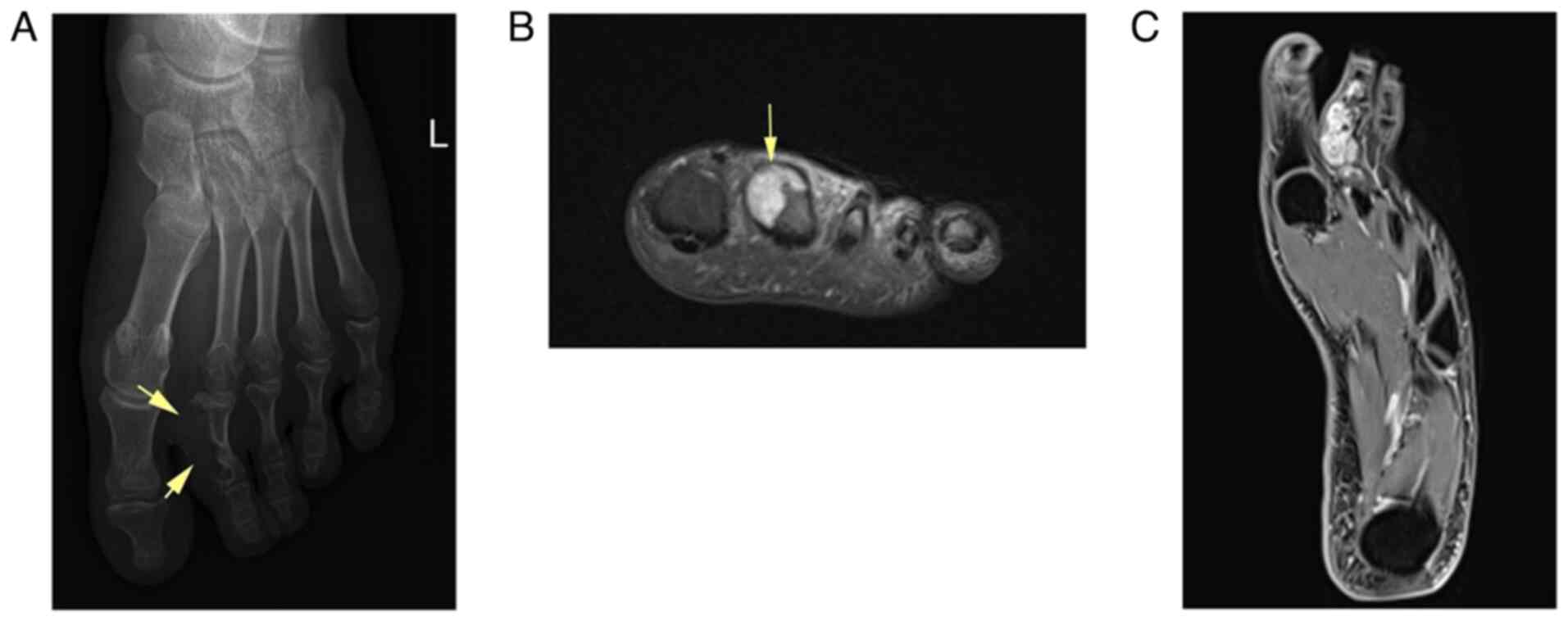
An X-ray revealed a radiolucent, eccentric lesion
within the proximal phalanx of the left second toe, with the loss
of the medial bone cortex. Magnetic resonance imaging (MRI)
revealed an expansile osteolytic lesion breaching three cortices of
the proximal phalanx of the left second toe, with no involvement of
soft tissue, consistent with enchondroma (Fig. 2).
Therapeutic intervention
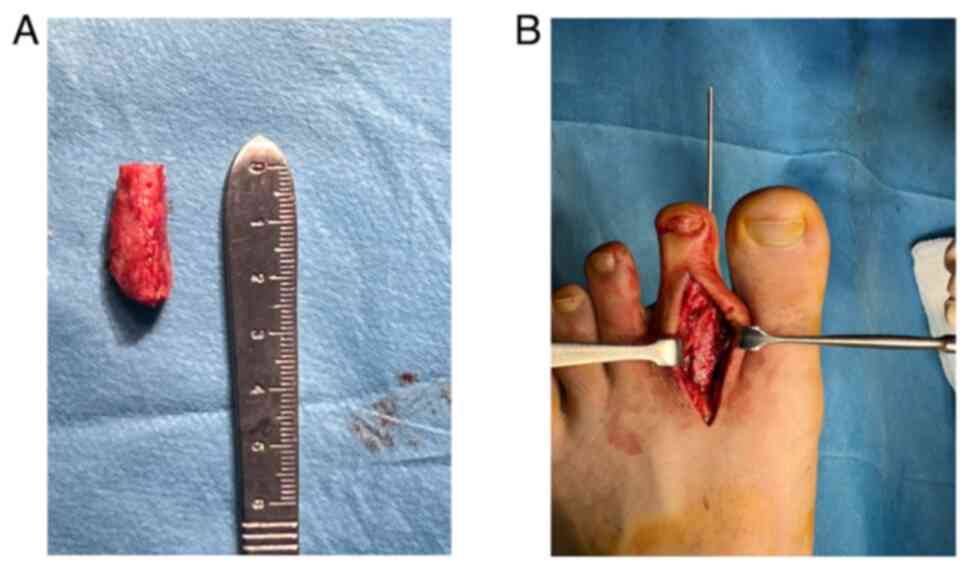
Surgery was decided under spinal anesthesia. The
left limb was prepped and draped, and the ipsilateral iliac crest
was prepared for harvesting a bone graft. Using a thigh tourniquet
following the exsanguination of the leg, a longitudinal dorsal
approach incision was made over the center of the toe, extending
from the metatarsophalangeal joint to the proximal interphalangeal
joint. The extensor digitorum longus tendon was exposed and
retracted laterally, revealing the proximal phalanx with its
lesion. After separating and protecting the neurovascular
structures, the lesion was resected using a no. 15 surgical blade.
The tumor bed was subsequently cleaned using Rongeur forceps and a
bone curette, followed by shaving the tumor bed with a small,
high-speed burr (Fig. 3).
Subsequently, after measuring the osseous defect, a tricortical
iliac bone autograft was harvested from the ipsilateral site and
placed into the defect. A 1.6-mm Kirschner wire was inserted
antegrade through the harvested graft into the middle and distal
phalanges and then retrograded back into the metatarsal head
(Fig. 4). Layered closure was
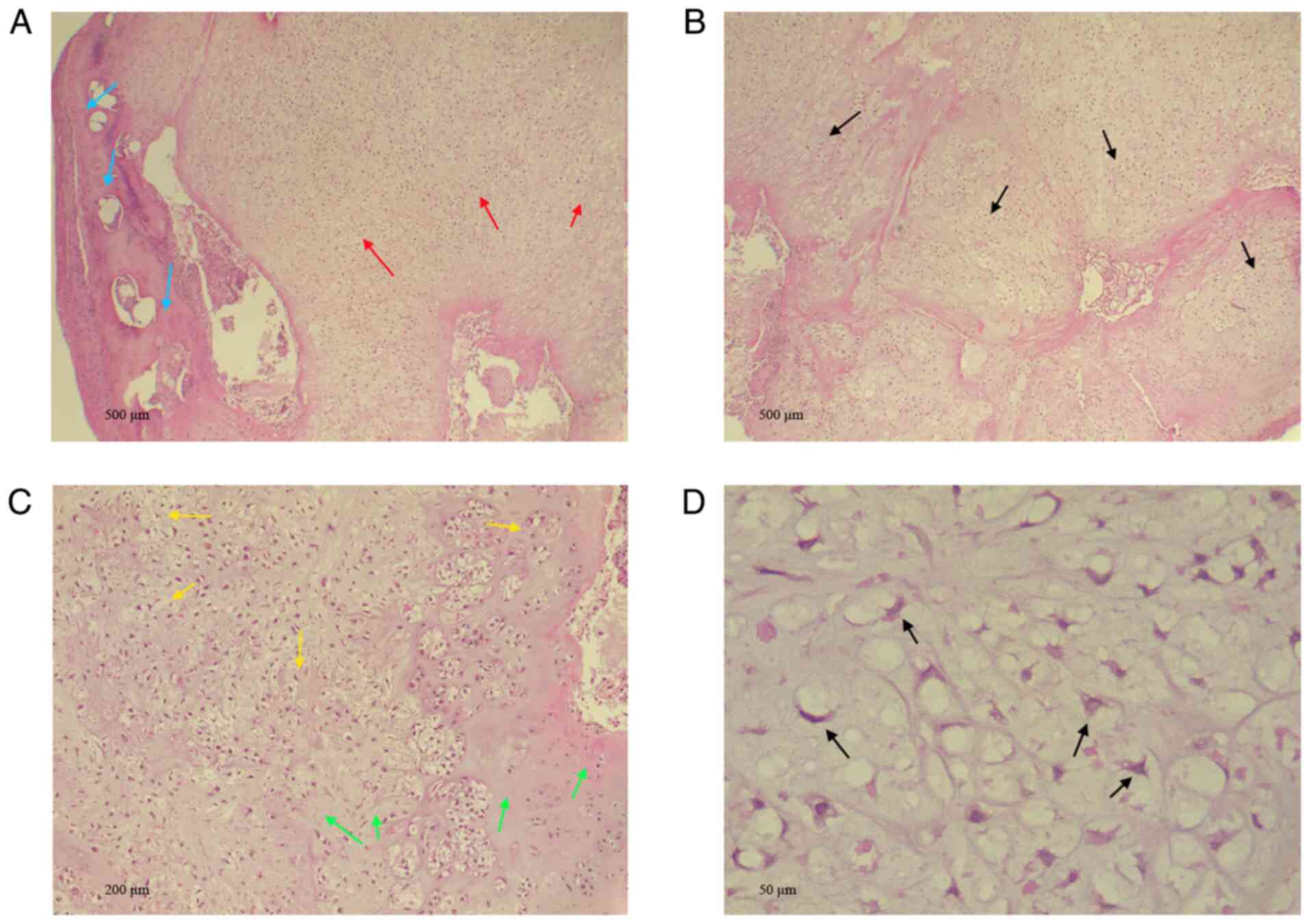
performed for both wounds. A histopathological examination was
performed by the laboratory at Smart Health Tower, as follows: The
analysis was performed on 5-µm-thick, paraffin-embedded sections.
The sections were fixed in 10% neutral-buffered formalin at room
temperature for 24 h, and the sections were then stained with
hematoxylin and eosin (H&E; Bio Optica Co.) for 1-2 min at room
temperature. The sections were then examined under a light
microscope (Leica Microsystems GmbH). The histopathological
analysis of the tumor revealed hypercellular sheets of chondrocytes
encased by mature bone trabeculae without cortical destruction,
pre-existing lamellar bone entrapment, or soft tissue invasion. The
tumor had a partly lobular configuration with varying cellularity.
Chondrocytes within lacunae in a myxoid and hyaline matrix had
elongated and stellate nuclei with fine chromatin. There was no
multinucleation, significant pleomorphism, mitotic activity, or
necrosis (Fig. 5).
Follow-up
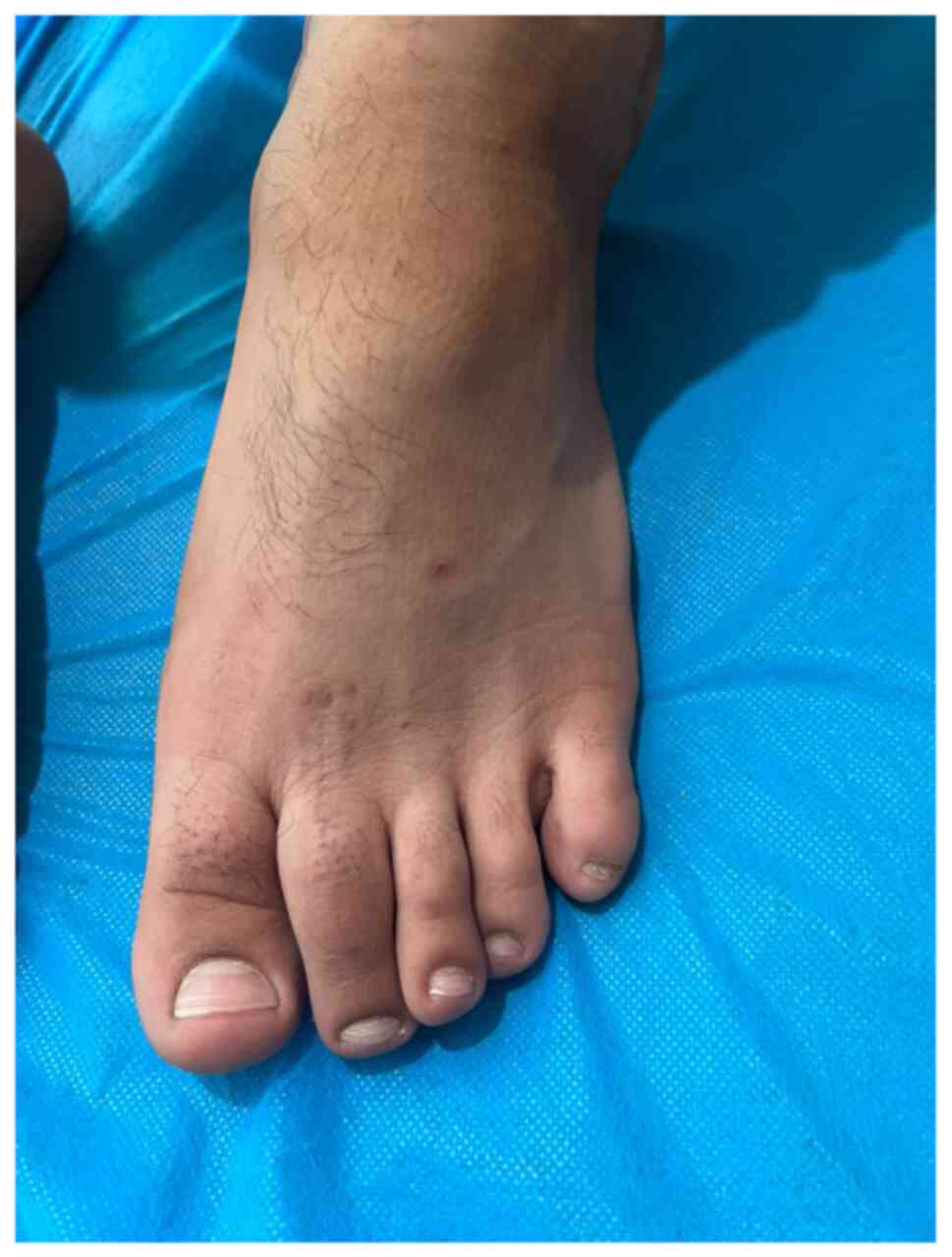
Post-operatively, the patient was placed in
heel-touch weight bearing. The Kirschner wire was removed after 6
weeks, and the bone showed good signs of healing. At 6 months
postoperatively, the patient demonstrated excellent toe range of
motion, was pain-free and maintained proper alignment (Fig. 6). An X-ray revealed a complete
union of the bone with the graft.
Discussion
Enchondromas grow gradually without infiltrating
nearby tissues or spreading to distant body parts (3,15).
In reviewing 19 cases of foot enchondroma (Table I), only two instances were found
where an enchondroma transformed into chondrosarcoma, leading to
amputation (11,12).
 | Table IReview of 19 cases of enchondroma of
the foot . |
Table I
Review of 19 cases of enchondroma of
the foot .
| First author, year of
publication | No. of cases | Age (years) | Sex | Site of the
lesion | Tumor size (cm) | Presenting
symptom | Medical history | Physical
examination | U/S | X-ray | CT | MRI | Management | Histopathology | Follow-up
(months) | Recurrence | (Refs.) |
|---|
| Komurcu, 2015 | 1 | 53 | M | Calcaneus | 2.1 | Pain | Negative | Tenderness and
swelling | NA | A lesion with
calcification and peripheral sclerosis | Cortical thinning
adjacent to the lesion | A lesion with
hyperintense signaling on T2-weighted sequences and peripheral
heterogeneous enhancement pattern on contrast-enhanced T1-weighted
sequences | Curettage of the
lesion and grafting | Lobules of different
sizes of hyaline cartilage tissue and chondrocytes without atypia
inside hyaline cartilage | NA | No | (1) |
| Lui, 2014 | 1 | 51 | F | 1st toe PP | NA | Pain | Negative | Swelling | NA | Fracture with an
enchondroma | NA | NA | Endoscopic curettage
and bone grafting | NA | 31 | No | (2) |
| Edwards, 2020 | 1 | 27 | M | 4th toe PP | 1 | Pain | Controlled type I
diabetes mellitus and depression | Moderate edema and
tenderness | Mild soft tissue
edema | Lucent lesion | NA | Expansile lesion
breaching the inferior and lateral cortical bone | Resection and tibial
bone graft | A well circumscribed
tumor composed of lobules of hyaline cartilage encased in bone and
covered by fibrous tissue. | 12 | No | (3) |
| De Yoe, 1999 | 2 | 43 | F | 3rd toe MT | 0.7 | Pain | Controlled
hypertension | Tenderness | NA | A lytic ovoid lesion
with disrupted lateral cortex of the metatarsal | NA | NA | Surgical excision
with autogenous bone grafting | Confirmed enchondroma
(no detail available) | 10 | No | (4) |
| | | 45 | M | Cuneiform | 0.4 | Pain | Negative | Tenderness | NA | Lytic lesion | NA | NA | Curettage with
autogenous bone graft | Confirmed enchondroma
(no detail available) | 12 | No | (4) |
| Goto, 2004 | 8 | 48 | F | 3rd toe PP | 0.8 | Pain | Negative | NA | NA | Eccentrically
located radiolucent area, and pathological fracture | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 13 | No | (5) |
| | | 25 | F | 1st toe DP | 2.1 | Incidental
finding | Negative | NA | NA | NA | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 30 | No | (5) |
| | | 32 | F | 3rd toe PP | 0.6 | Pain | Negative | NA | NA | Pathological
fracture | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 6 | No | (5) |
| | | 39 | M | 1st toe DP | 0.54 | Pain | Negative | NA | NA | Pathological
fracture | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 41 | No | (5) |
| | | 23 | F | 2nd toe PP | 0.33 | Pain | Negative | NA | NA | Pathological
fracture | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 34 | No | (5) |
| | | 50 | M | 3rd toe PP | 0.24 | Incidental
finding | Negative | NA | NA | NA | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 13 | No | (5) |
| | | 31 | M | 2nd toe MP | 2.1 | Pain | Negative | NA | NA | Radiolucent area
with some calcifications and ballooning of the cortex | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 18 | No | (5) |
| | | 31 | M | 1st toe DP | 0.2 | Pain | Negative | NA | NA | NA | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 12 | No | (5) |
| | | | | 1st toe PP | 4.7 | Incidental
finding | Negative | NA | NA | NA | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 12 | No | (5) |
| | | | | 1st toe MT | 4.6 | Incidental
finding | Negative | NA | NA | NA | NA | NA | Simple curettage
without bone grafting | Confirmed
enchondroma (no detail available) | 12 | No | (5) |
| Stess, 1995 | 1 | 36 | M | 2nd toe PP | 2.2 | Pain | NA | Swelling and
tenderness | NA | An osseous
metaphyseal lesion with diminished density | NA | NA | Total phalangectomy
of the proximal phalanx with syndactylization of the second and
third toes. | NA | 12 | No | (7) |
| Remba, 2021 | 1 | 30 | M | 1st toe MT | NA | Inversion of the
foot | Negative | Edema and pain
during mobility and walking | NA | Tumor and soft
tissue edema | NA | Heterogeneous
intramedullary lesion, hypo-intense in T1 and hyper-intense in
T2 | Curettage of the
lesion with bone grafting | Confirmed
enchondroma (no detail available) | 6 | No | (8) |
| Patel, 2022 | 1 | 17 | M | 1st toe PP | 2.8 | Pain | Negative | Swelling | NA | Lytic lesions,
scalloping of the cortex, and whorls of calcification | NA | Hyperintense mass
on FS-PD, and soft tissue edema and swelling on T1-weighted
sequences | Surgical excision
with bone grafting | Confirmed
enchondroma (no detail available) | 24 | No | (9) |
| Alhosain, 2020 | 1 | 16 | F | 2nd toe PP | 1.3 | Pain | Negative | Hard, round mass
fixed to the bone | NA | Well circumscribed,
lucent, a central medullary lesion with cortical expansion and
thinning | NA | NA | Curettage and
subsequent bone grafting | Lobules of hyaline
cartilage encased by normal bone and fibrous tissue | 3 | No | (10) |
| Mahajan, 2009 | 1 | 86 | F | 3rd toe PP | NA | Pain | Negative | Movement
restriction of the metatarso-phalangeal joint, swelling | NA | Expansile swelling
contained within the cortex without malignant change | NA | Cystic change,
consistent with benign lesion. Six months later, it turned into
malignancy | Ray amputation due
to malignant change into chondrosarcoma | chondrosarcoma
grade II, mainly and III focally | NA | NA | (11) |
| Koak, 2000 | 1 | 33 | F | 3rd toe DP | NA | Pain and
swelling | Foot trauma | The toe had a
drumstick appearance with enlargement | NA | Expanding lytic
lesion with a fracture | NA | NA | Partial amputation
of the toe | The features
indicated low-grade (Grade 1) chondrosarcoma | NA | NA | (12) |
Enchondroma primarily manifests in the phalanges of
the hand, although it can also occur in the phalanges and
metatarsal bones of the foot (1).
Among the reviewed cases, the most commonly affected toe was the
first toe (38%), followed by the third toe (28.6%), the second toe
(19%), the fourth toe (4.8%), the calcaneus (4.8%) and the
cuneiform bone (4.8%). Among the 17 cases with 19 lesions located
on the toes, the most common sites were the proximal phalanx
(57.9%), followed by the distal phalanx (21%), metatarsal (15.8%)
and middle phalanx (5.3%). In the present case, the lesion was
located on the proximal phalanx of the second toe.
The tumor is typically found as a solitary lesion,
known as a solitary enchondroma (8). However, they can also appear as
multiple lesions, as seen in conditions such as multiple
enchondromatosis (Ollier disease) and multiple enchondromatosis
associated with hemangiomas (Maffucci syndrome) (3). Enchondromatosis is linked to somatic
mutations in the isocitrate dehydrogenase (IDH)1 and IDH2 genes.
These mutations produce defective IDH, an enzyme in the
tricarboxylic acid cycle that converts isocitrate to
α-ketoglutarate. The mutated enzyme facilitates the reduction of
α-ketoglutarate to the oncometabolite D-2-hydroxyglutarate
(D-2-HG), and by competitively inhibiting α-ketoglutarate-dependent
enzymes, D-2-HG results in hypermethylation of DNA and modification
of histones. These processes encourage the development of
cartilaginous tumors and disrupt the normal osteogenic
differentiation of mesenchymal stem cells (6). All reviewed cases in the present
study involved solitary enchondromas, apart from 1 patient with
multiple lesions in the distal phalanx, proximal phalanx, and
metatarsal bones of the first toe of the same foot (5).
Foot enchondromas can occur at any age, although
they are most commonly observed in patients between the first and
fourth decades of life (9). The
youngest case reported among the cases reviewed herein involved a
16-year-old female, while the oldest was an 86-year-old female
(1,11). In accordance with the study by De
Yoe and Rockett (4), in the
present study, a review of the literature revealed no sex
predilection in the prevalence of foot enchondromas, with 10 males
and 9 females. The case in the present study was a 20-year-old
male.
Generally, enchondromas remain asymptomatic for
extended periods of time. When symptoms do manifest, they may
include pain, swelling, or deformity of the affected bone (6). The primary source of pain often stems
from elevated pressure caused by the cortical expansion of the
lesion, pathological fracture, or malignant conversion of the
lesion (1,3,4). The
lesion in the majority of the reviewed cases caused pain (76.2%)
and food inversion in 1 case (4.8%), while the remaining lesions
were diagnosed incidentally on foot radiographs (19%).
Additionally, 6 out of the 19 cases had pathological fractures.
Various modalities and methods are available to
healthcare professionals for detecting and diagnosing enchondromas.
The primary and most crucial method remains a comprehensive
clinical history (8). After
assessing the clinical presentation, plain radiographs are the
preferred initial diagnostic imaging modality (9). Radiographically, enchondromas appear
as lytic lesions with clearly defined borders and variable degrees
of stippled or punctate calcifications, typically without the
involvement of the surrounding soft tissues (3). In general, computed tomography scans
and MRIs can provide additional detail about the lesion,
particularly when there is rapid growth or suspicion of soft tissue
involvement (4). In the identified
literature, plain radiography was the most commonly employed
diagnostic modality, showing lytic lesions. In the case presented
herein, the radiograph revealed a radiolucent, eccentric lesion
with loss of the medial bone cortex, and the MRI revealed an
expansile osteolytic lesion breaching three cortices of the
affected phalanx.
Radiological findings suggesting a lesion are not
always conclusive for diagnosing an enchondroma; therefore, a
histopathological analysis is mandatory (9). Distinguishing between benign and
malignant lesions presents a significant challenge. All available
tissues need to be thoroughly examined. Enchondromas can be
visually identified as bluish, semi-translucent masses of hyaline
cartilage arranged in lobular patterns. Microscopically,
enchondromas display small chondrocytes within lacunar spaces
characterized by round, uniform nuclei resembling those found in
hyaline cartilage. Some enchondromas may also exhibit areas of
ossification within the cartilage matrix (4,6). The
nuclei of these cells are generally regular, showing a few mitotic
activities. Enchondromas located near the bone cortex, including
those in the hands, may exhibit increased cellularity and atypia
while remaining benign (6).
Histologically, enchondroma and low-grade (well-differentiated)
chondrosarcoma can appear deceptively similar, although they can be
distinguished by their tissue architecture and patterns of
invasion: enchondromas typically display multiple discrete nodules
of hyaline cartilage separated by normal marrow elements and are
often surrounded by lamellar host bone conforming to the shape of
the cartilage lobules; by contrast, low-grade chondrosarcomas tend
to form a single confluent mass of cartilage that permeates the
marrow, ‘trapping’ host lamellar bone, infiltrating the Haversian
systems or marrow fat, and often exhibiting fibrous bands between
peripheral cartilage lobules. These features reflect its malignant
nature. Additional supportive indicators include the presence of
lobulation patterns and fibrous tissue formation around the lesion,
which have been shown to correlate with malignant recurrence in
follow-up studies, whereas enchondromas generally remain benign
(16,17). The histopathological analysis of
the specimen in the case in the present study revealed
hypercellular sheets of chondrocytes encased by mature bone
trabeculae at the periphery without cortical destruction,
entrapment of pre-existing lamellar bone, or soft tissue invasion.
There was no multinucleation, significant pleomorphism, mitotic
activity, or necrosis.
The treatment of enchondroma can range from close
monitoring and regular follow-up, particularly for small,
asymptomatic lesions, to complete surgical removal with bone
grafting for larger, symptomatic lesions (2). Surgery is recommended for patients
experiencing ongoing symptoms and lesions >2 cm, as they pose a
significant risk of pathological fractures. It includes complete
tumor removal with or without bone grafting, as well as curettage
followed by bone grafting. Goto et al (5) reported that the radiographic and
functional outcomes of simple curettage without bone grafting are
comparable to those of curettage with autologous bone grafting.
They also highlighted several advantages of performing curettage
without bone grafting for foot enchondromas: i) It eliminates the
pain and discomfort associated with the bone donor site; ii) the
procedure can be performed on an outpatient basis; and iii) the
shorter operation time provides economic benefits and decreases the
risk of infection (5). However,
Edwards and Kingsford (3) reported
that curettage alone is not recommended due to a high rate of
non-union (67%). They found that the surgical option involving bone
grafting is more suitable, as it offers a recovery period similar
to that of curettage alone, despite the additional wound that
requires healing (3). Patel et
al (9) also reported that the
latest management option for foot enchondroma involves using an
autologous bone graft from the iliac crest, which can be either
cortical or cancellous. Chun et al (18) reported a series of 20 cases in
which all patients underwent tumor curettage followed by bone
grafting. No recurrences or post-operative complications were
observed during the 24-month follow-up period (18). In addition, Futani et al
(19) conducted a retrospective
cohort study comparing osteoscopic and conventional open surgery
for foot enchondromas. A total of 17 patients underwent osteoscopic
surgery, and 8 patients underwent open surgery. They reported that
functional recovery was significantly improved in the osteoscopic
group at 1 and 2 weeks post-operatively, though no differences were
noted after 1 month. Additionally, osteoscopic surgery was
associated with fewer complications (12% vs. 50%) and no
recurrences in either group (19).
Among the reviewed cases, 8 (42.1%) cases were managed with
excision or curettage combined with bone grafting, another 8
(42.1%) cases were managed with simple curettage without bone
grafting, 1 (5.3%) case was managed with total phalangectomy, and 2
cases underwent partial and ray amputation (10.5%). All reported
cases had favorable surgical outcomes without any recurrence. In
the case in the present study, the tumor was surgically removed,
and a tricortical iliac bone autograft from the ipsilateral site
was placed into the defect. The surgical outcome was favorable,
with no signs of recurrence or complications. The unretrievable
last follow-up X-ray image, which revealed the complete union of
the bone with the graft, may be a limitation of the present case
report.
In conclusion, enchondroma is a benign tumor rarely
found in the foot. For symptomatic cases, the surgical removal of
the lesion combined with autologous iliac bone grafting may result
in favorable outcomes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
FHK and AKG were major contributors to the
conception of the study, as well as to the literature search for
related studies. HOA, MGH and SOK were involved in the literature
review, in the conception and design of the study and in the
writing of the manuscript. RJR, AMA and HAS were involved in the
literature review, in the design and conception of the study, the
critical revision of the manuscript, and the processing of the
figures and table. AAM was the radiologist who performed the
assessment of the case. RMA and AMA were the pathologists who
performed the diagnosis of the case. FHK and AKG confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient for his participation in the present study.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Komurcu E, Kaymaz B, Golge UH, Goksel F,
Resorlu M and Kılınç N: Atypical localization of enchondroma in the
calcaneus. J Am Podiatr Med Assoc. 105:260–263. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lui TH: Endoscopic curettage and bone
grafting of the enchondroma of the proximal phalanx of the great
toe. Foot Ankle Surg. 21:137–141. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Edwards SR and Kingsford AC: Surgical
management of an enchondroma of the proximal phalanx of the foot:
An illustrative case report. SAGE Open Med Case Rep.
8(2050313X20945894)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
De Yoe BE and Rockett MS: Enchondroma as a
cause of midfoot pain. J Foot Ankle Surg. 38:139–142.
1999.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Goto T, Kawano H, Yamamoto A, Yokokura S,
Iijima T, Motoi T and Nakamura K: Simple curettage without bone
grafting for enchondromas of the foot. Arch Orthop Trauma Surg.
124:301–305. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Biondi NL, Tiwari V and Varacallo M:
Enchondroma. In: StatPearls (Internet). StatPearls Publishing,
Treasure Island, FL, 2025. Accessed on August 13, 2024. https://www.ncbi.nlm.nih.gov/books/NBK536938/.
|
|
7
|
Stess RM and Tang RE: Enchondroma of the
proximal phalanx. J Foot Ankle Surg. 34:79–81. 1995.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Remba SJ, San Martín RÁ, Amiga IB and
Santos DP: Solitary enchondroma in a metatarsal bone, an incidental
discovery. Int J Surg Case Rep. 78:254–258. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Patel S, Yadav S, Gurnani S, Yadav P and
Selvin B: A solitary enchondroma of the great toe in an adolescent
male: A case report. Cureus. 14(e21772)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Alhosain D, Kouba L, Dandashy A and Jejan
W: A painful lump on a teenager's toe is a benign enchondroma.
Lancet. 396(1663)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mahajan RH, Dalal RB, Sahu A, Dalal N,
Banzal R and Anand S: Secondary chondrosarcoma in an enchondroma in
a proximal phalanx of toe. A diagnostic problem. A case report.
Foot (Edinb). 19:62–64. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Koak Y, Patil P and Mackenny R:
Chondrosarcoma of the distal phalanx of a toe: A case report. Acta
Orthop Belg. 66:286–288. 2000.PubMed/NCBI
|
|
13
|
Abdullah HO, Abdalla BA, Kakamad FH, Ahmed
JO, Baba HO, Hassan MN, Bapir R, Rahim HM, Omar DA, Kakamad SH, et
al: Predatory publishing lists: A review on the ongoing battle
against fraudulent actions. Barw Med J. 2:26–30. 2024.
|
|
14
|
Prasad S, Nassar M, Azzam AY, José FGM,
Jamee M, Sliman RK, Evola G, Mustafa AM, Abdullah HO, Abdalla BA,
et al: CaReL guidelines: A consensus-based guideline on case
reports and literature review (CaReL). Barw Med J. 2:13–19.
2024.
|
|
15
|
Abdullah AS, Ahmed AG, Mohammed SN, Qadir
AA, Bapir NM and Fatah GM: Benign tumor publication in one year
(2022): A cross-sectional study. Barw Med J. 1:20–25. 2023.
|
|
16
|
Torbaghan SS, Ashouri M, Naderi NJ and
Baherini N: Histopathologic differentiation between enchondroma and
well-differentiated chondrosarcoma: Evaluating the efficacy of
diagnostic histologic structures. J Dent Res Dent Clin Dent
Prospects. 5:98–101. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ferrer-Santacreu EM, Ortiz-Cruz EJ,
Díaz-Almirón M and Kreilinger JJ: Enchondroma versus chondrosarcoma
in long bones of appendicular skeleton: Clinical and radiological
criteria-a follow-up. J Oncol. 2016(8262079)2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chun KA, Stephanie S, Choi JY, Nam JH and
Suh JS: Enchondroma of the Foot. J Foot Ankle Surg. 54:836–839.
2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Futani H, Kawaguchi T, Sawai T and
Tachibana T: Osteoscopic versus open surgery for the treatment of
enchondroma in the foot. Arch Orthop Trauma Surg. 143:4899–4905.
2023.PubMed/NCBI View Article : Google Scholar
|