1. Introduction
Periodontology and implantology represent dynamic
and evolving disciplines within clinical dentistry, marked by
continuous innovations in diagnostic methodologies, biomaterials
and surgical techniques (1). The
advent of minimally invasive procedures, regenerative therapies and
computer-guided implantology has revolutionized patient care,
enabling clinicians to achieve functional and aesthetic
rehabilitation with increasing predictability and precision
(2,3).
However, these advances have led to a parallel
increase in clinical complexity and the potential for procedural
errors and biological complications. Treatment-related mishaps may
arise at any stage, from initial diagnosis and treatment planning
to intraoperative execution and long-term maintenance. Factors
contributing to such complications include inadequate case
selection, an incomplete understanding of anatomical intricacies,
surgical inexperience and patient-specific considerations, such as
systemic health, compliance and oral hygiene practices (4,5).
While some complications are minor and
self-limiting, others can be severe, resulting in delayed healing,
graft or implant failure, aesthetic dissatisfaction, or
irreversible damage to surrounding tissues. Notably, a number of
these adverse outcomes are preventable through comprehensive
treatment planning, adherence to evidence-based protocols and
continuous clinical vigilance (6,7).
The literature on periodontal and implant
complications is expanding; however, a large amount of this
research remains fragmented, anecdotal or lacking in standardized
classification (1,3). There remains a pressing need to
consolidate current knowledge and identify recurring patterns of
clinical error to foster improved protocols and training.
The present review aimed to provide a structured and
in-depth exploration of the errors and complications encountered in
both periodontal and implant therapy. By dissecting the
multifactorial causes, highlighting diagnostic pitfalls and
outlining contemporary management strategies, the present review
aimed to equip clinicians with the insights necessary to mitigate
risks and refine their practice. A proactive, prevention-driven
approach is paramount, not only to preserve hard-won clinical
outcomes, but also to uphold the highest standards of patient care
in an increasingly demanding therapeutic landscape (8).
Successful outcomes in periodontal and implant
therapy are highly dependent on appropriate patient and site
selection. Several systemic, local, anatomical and patient-related
factors need to be evaluated before deciding on the treatment plan.
A balanced consideration of these determinants allows clinicians to
distinguish between favorable and unfavorable cases. A summary of
the essential aspects of good vs. poor case selection is provided
in Table I.
 | Table ICase selection criteria. |
Table I
Case selection criteria.
| Aspect | Good case
selection | Bad case
selection |
|---|
| Systemic
health | Medically fit
patients or those with well-controlled conditions (e.g., diabetes,
hypertension). | Uncontrolled
systemic diseases (e.g., diabetes, bleeding disorders, recent
cardiac events, patients on chemotherapy, radiotherapy, or IV
bisphosphonates). |
| Oral hygiene and
motivation | Consistently low
plaque levels, compliance with oral hygiene instructions, and
willingness to attend maintenance visits. | Poor oral hygiene,
persistent plaque/calculus, and lack of cooperation with
maintenance therapy. |
| Periodontal
defects | Well-contained
infrabony pockets, class I furcations, and moderate gingival
recessions that are surgically manageable. | Non-contained
vertical bone loss, class III furcations, or teeth with hopeless
prognosis and advanced mobility. |
| Gingival/tissue
factors | Thick gingival
biotype, sufficient keratinized gingiva, stable soft tissue
conditions. | Thin biotype,
minimal keratinized tissue, high risk of gingival recession and
poor flap stability. |
| Anatomical
considerations | Manageable anatomy;
no severe fenestrations, minimal mandibular tori or tuberosities,
adequate vestibular depth for flap reflection. | Unfavourable
features: prominent external oblique ridge, high genial tubercle,
thin mucosa over mandibular tori, or pronounced undercuts risking
perforation/bleeding. |
| Bone factors
(implants) | Adequate ridge
dimensions (≥6-7 mm width and ≥8 mm height), favourable bone
density (type II-III). | Severe ridge
atrophy, knife-edge ridges, poor bone density, extreme sinus
pneumatization with <4 mm residual bone. |
| Anatomical
safety | Safe distances from
vital structures; inferior alveolar nerve, mental foramen, incisive
canal, sublingual/submental arteries; sinus anatomy favourable or
correctable. | Unclear nerve
location, large anterior loop/incisive canal, high-risk sinus
anatomy, or proximity to critical structures. |
| Radiographic
planning | CBCT or OPG used to
map out implant site and confirm safety margins. | Inadequate imaging
or proceeding without precise radiographic assessment. |
| Patient
factors | Motivated
individuals with realistic aesthetic and functional expectations,
willing to invest in long-term care. | Heavy smokers,
parafunctional habits (e.g., bruxism) without protective therapy,
non-compliant with maintenance, or unrealistic expectations. |
2. Treatment errors and complications in
non-surgical periodontal therapy
Non-surgical periodontal therapy (NSPT),
particularly scaling and root planing (SRP), is the foundation of
periodontal disease management. Although considered conservative
and minimally invasive, these procedures are not free of
complications, particularly when performed without proper
technique, careful instrument selection or sufficient clinical
awareness (9,10). One of the most frequent
complications is trauma to the soft tissues, which may occur due to
excessive lateral pressure, incorrect instrument angulation, or use
of dull curettes. Similarly, improper handling of ultrasonic
scalers without adequate irrigation can generate excess heat,
jeopardizing pulpal health and adjacent periodontal tissues
(11). Hard tissue complications
also arise from aggressive root planing, which may strip away vital
cementum or dentin, thereby reducing the regenerative potential of
the root surface and even damaging restorative margins. Misuse of
air-polishing devices can additionally cause epithelial abrasions
and, in rare cases, subcutaneous emphysema (10). Common sequelae include dentinal
hypersensitivity due to exposed tubules, temporary increases in
tooth mobility in patients with advanced bone loss, and instrument
fractures within periodontal pockets, which occasionally require
surgical retrieval (1,10).
Another well-recognized limitation of NSPT is the
incomplete removal of calculus and biofilm, particularly in deep
periodontal pockets (>6 mm), furcations and root concavities.
Despite modern powered instrumentation, residual deposits
frequently persist. This challenge can be reduced by combining hand
and ultrasonic instruments, using slim ultrasonic tips in narrow or
deep sites, prescribing adjunctive antimicrobials such as
amoxicillin with metronidazole in advanced or aggressive cases, and
re-evaluating sites with unresolved inflammation to determine the
need for surgical access. Over-instrumentation should also be
avoided, since endotoxins are weakly bound to root surfaces and
minimal debridement is usually sufficient. Post-treatment
hypersensitivity can be managed with topical desensitizing agents
and patient reassurance (10.11).
Discomfort during SRP may compromise compliance;
therefore, the judicious use of local anaesthesia, quadrant-wise or
full-mouth protocols and personalized oral hygiene instruction can
improve patient cooperation. Adjunctive treatments, such as lasers,
photodynamic therapy, or antiseptic irrigants have exhibited only
limited or short-term benefits and should be considered secondary
to thorough debridement, with patients clearly informed of their
restricted role. Likewise, systemic antimicrobials, though
beneficial in selected advanced cases, carry risks of resistance,
drug interactions and adverse events, and should be prescribed only
with strict clinical justification (8,9,11).
Clinical decision-making must also respect the principle of
‘critical probing depth’: SRP is most effective at sites with
probing depths >2.9 mm, whereas flap surgery provides superior
results in pockets >5.4 mm (11).
Evidence from long-term studies emphasizes that NSPT
in advanced disease may present further risks (12). For instance, almost one-third of
patients treated with SRP experience disease recurrence within 3
years, compared with approximately half that proportion following
surgical access therapy. Residual deep pockets >6 mm function as
high-risk sites for biofilm persistence, facilitating recurrent
breakdown and eventual tooth loss. Both surgical and non-surgical
approaches have also been shown to cause attachment loss in shallow
sites (≤3 mm), underscoring the iatrogenic risks of unnecessary
instrumentation. A further error involves undervaluing supportive
periodontal therapy; although the average annual attachment loss in
well-maintained SRP and surgical patients is only 0.07-0.1 mm,
individuals with poor recall compliance or untreated residual deep
sites are much more likely to experience recurrent disease.
Therefore, inadequate maintenance, incomplete instrumentation in
deep lesions and failure to detect residual ‘loser sites’ represent
key clinical errors (6,12). To prevent these outcomes,
clinicians should recognize that surgical access often yields more
stable long-term results in advanced cases, enforce rigorous
supportive care, and customize treatment strategies according to
probing depth, anatomical complexity and patient susceptibility,
thereby optimizing safety and the predictability of outcomes
(12).
3. Treatment errors and complications in
flap surgeries
Poor case selection, surgical technique flaws and
anatomical difficulties are frequently the causes of errors and
complications in periodontal and implant therapy. An example of how
intraoperative mistakes, such as a poorly designed incision or
overharvesting >7 mm from the greater palatine foramen, can
result in major complications, such as arterial damage, excessive
bleeding, or tissue necrosis, is the palatal donor site, which is
frequently used for harvesting connective tissue and free gingival
grafts. Inadequate flap tension or graft immobilization during
periodontal operations can result in delayed healing or graft
failure. Similarly, flap necrosis, soft tissue abnormalities, or
reduced function and appearance may arise from inadequate flap
reflection, severe tissue damage, or incorrect implant angulation
in implant therapy (13).
In such situations, the risk of infection, graft
shrinkage, or colour mismatch is further increased by subpar
post-operative care. Thorough anatomical evaluation, accurate
surgical planning, cautious execution and attentive post-operative
monitoring are necessary for prevention. To minimize problems and
guarantee positive results, clinician experience and adherence to
best procedures are essential (13).
4. Treatment errors and complications in
regenerative periodontal surgery
Regenerative periodontal procedures involving the
use of membranes and bone grafts are among the most complex and
biologically demanding interventions in periodontology. These
procedures aim to restore lost periodontal structures through the
regeneration of bone and soft tissue. However, the technical and
biological complexity of these surgeries increases the potential
for complications. One of the most frequent errors is poor flap
design, which can result in excessive tension on the surgical site
and prevent optimal passive closure. This failure to achieve proper
closure can lead to premature exposure of the membrane, allowing
bacteria to colonize and compromise the regenerative process
(14).
Membrane exposure is a critical complication in
regenerative surgery, as it greatly hampers the healing process and
reduces the regenerative potential of the surgical site. This
exposure can lead to infection, graft displacement, fibrous
encapsulation and delayed healing, all of which diminish the
effectiveness of the regenerative procedure. Inadequate space
maintenance is another common error, often resulting in graft
collapse or resorption, further complicating healing (3,15).
The selection of biomaterials is crucial to the
success of regenerative procedures. Using materials that are not
biocompatible or clinically proven can result in material allergy,
graft failure and poor clinical outcomes. Additionally, patient
factors, such as smoking, diabetes and poor compliance with
post-operative care can markedly increase the risk of developing
complications. Smokers are at an increased risk of delayed healing
due to a reduced blood supply and compromised immune function.
Diabetic patients may experience impaired wound healing and an
increased risk of infection due to poor metabolic control (3).
To minimize complications and improve success rates,
clinicians need to adhere to strict case selection criteria and be
sure that the materials used are supported by robust clinical
evidence of efficacy and biocompatibility. Moreover, comprehensive
patient education regarding post-operative care, including smoking
cessation and the management of comorbid conditions, is essential
for optimizing surgical outcomes. Regular follow-up visits are also
critical for monitoring healing and addressing any potential issues
promptly (16-19).
5. Treatment errors and complications in
root coverage therapy
Root coverage procedures, such as coronally advanced
flaps and connective tissue grafts, are frequently employed to
manage gingival recession defects for both functional and aesthetic
purposes. While these techniques have high success rates, they
remain inherently technique sensitive and prone to various clinical
errors that may compromise outcomes (5,20-22).
Diagnostic inaccuracies are among the earliest
pitfalls in root coverage therapy. Mistaking altered passive
eruption or gingival overgrowth for true recession can lead to
misguided treatment decisions. Moreover, neglecting to assess key
risk factors, such as tobacco use, traumatic tooth brushing habits,
or an insufficient zone of keratinized mucosa, can markedly reduce
the predictability of root coverage procedures (23).
Intraoperative complications often stem from poor
flap design or execution. Inadvertent flap perforation, inadequate
thickness, or improperly released incisions may jeopardize the
vascular supply to the grafted area. Donor site morbidity,
particularly when harvesting from the palatal region, may present
as immediate or delayed haemorrhage, hematoma, discomfort, or
tissue necrosis if anatomical landmarks are not used (23,24).
Post-operative healing may be complicated by graft
sloughing, partial or complete flap necrosis, infection, or
excessive scarring, particularly in cases of excessive tissue
tension or compromised patient compliance. Inadequate haemostasis,
flawed suturing, or premature mechanical trauma (e.g., from
brushing or mastication) may further disrupt the healing process
and aesthetic integration (25).
Optimal outcomes depend on a combination of factors:
Precise anatomical assessment, atraumatic surgical technique,
stable graft immobilization and meticulous post-operative care.
Patient education, particularly in maintaining hygiene without
disrupting the surgical site, plays an equally critical role in
ensuring long-term success. A delicate balance between surgical
finesse and biological principles underpins the successful
execution of root coverage procedures (26).
6. Treatment errors and complications in
ridge augmentation
Ridge augmentation procedures, such as guided bone
regeneration, are vital for creating sufficient bone volume for
implant placement. These procedures often involve the use of
autogenous or xenograft materials, which are typically covered by
barrier membranes to prevent soft tissue invasion. However, one of
the most common complications associated with ridge augmentations
is membrane exposure, which can occur due to insufficient soft
tissue thickness, improper flap design or premature trauma to the
area (27).
Other complications include wound dehiscence,
infection, graft resorption and failure of the graft to integrate
properly with the host bone. Procedural errors, such as overfilling
the defect with insufficient stabilization of the graft or
inadequate space maintenance, contribute to compromised outcomes
and a greater risk of treatment failure (17).
In order to reduce the risk of such complications,
meticulous planning is paramount. Pre-operative imaging, such as
cone-beam computed tomography (CBCT), allows for precise defect
evaluation and optimal graft material selection. Tension-free flap
advancement and patient-specific graft selection tailored to
individual anatomical needs can enhance the success of the
procedure. Post-operative care, including clear instructions on
diet and hygiene and avoiding trauma, is equally crucial in
promoting healing and ensuring favourable outcomes (17).
7. Wound healing dynamics, morbidity and
complications of palatal soft tissue harvesting
Owing to the abundant keratinized tissue and
advantageous regeneration qualities, the palatal donor site is
frequently employed for harvesting connective tissue grafts and
free gingival grafts in mucogingival procedures. However, there are
a number of vascular and anatomical issues at this location that
could cause issues. As the palatal mucosa is extremely sensitive,
post-operative pain and discomfort are typical, particularly when
large or thick grafts are harvested. This can affect patient
comfort and recovery (23,28). Significant bleeding or hematoma
formation can be caused by intraoperative issues, such as
unintentional injury to the larger palatine artery, which calls for
prompt medical attention. Additionally, if the surgical site is not
sufficiently protected during the early healing phase, delayed
bleeding or the formation of a liver clot may occur within 48 h
(23,29).
A thick layer of epithelial tissue at the donor site
may further impede healing, causing prolonged discomfort; improper
incision design can compromise the blood supply, resulting in
tissue necrosis or sloughing, complicating healing and increasing
morbidity; delayed healing, colour mismatch, graft shrinkage and
unsatisfactory aesthetic outcomes; in certain cases, this can also
result in inadequate vascularization or poor graft immobilization,
which can lead to graft failure. To reduce these risks, clinicians
need to carefully plan the dimensions of the graft, avoid
harvesting >7 mm from the greater palatine foramen and ensuring
tension-free suturing; effective post-operative care, including the
use of palatal stents, analgesics, cold packs and close monitoring,
is essential for promoting healing and minimizing discomfort
(3,22,29,30).
8. Treatment errors and complications in
implant positioning in the aesthetic zone and posterior region
Aesthetic zone
Successful implant placement in the anterior maxilla
requires precise three-dimensional alignment within the prosthetic
envelope. Even minor deviations in depth or angulation can
compromise the harmony of the gingival margin and papillary
architecture, leading to aesthetic disharmony that patients readily
perceive (31). Errors usually
arise from the inadequate use of prosthetically driven planning
tools or failure to respect the underlying bone anatomy and
soft-tissue biotype. Restorative challenges, such as compromised
emergence profiles may necessitate additional grafting or
prosthetic modifications. Incorporating CBCT-based planning,
surgical templates and coordinated treatment with restorative
specialists helps safeguard against these aesthetic failures
(32-34).
Posterior region
Implant placement in posterior sites is complicated
by reduced visibility and the proximity of vital anatomical
structures. In the maxilla, the insufficient evaluation of residual
bone height or sinus morphology may result in intraoperative
mishaps and long-term sinus complications. In the mandible, the
underestimation of lingual concavity depth or bone thickness can
increase the risk of perforation and vascular injury. Beyond
surgical risks, limited interarch space and dense bone quality can
complicate prosthetic alignment and osseointegration. Reliance on
advanced imaging, meticulous assessment of anatomic landmarks, and
staged augmentation procedures are critical strategies to reduce
errors in these challenging regions (6,35,36).
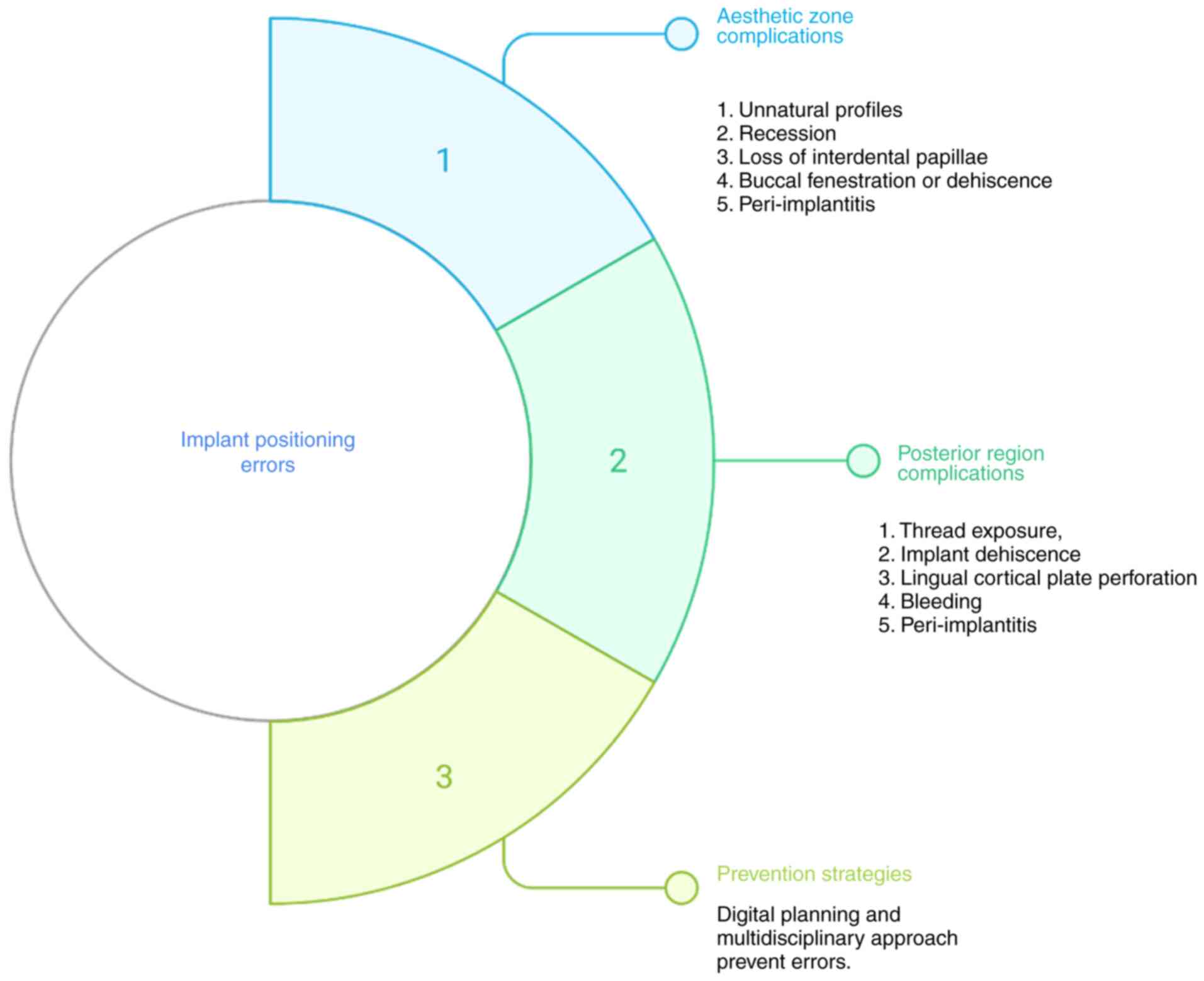
A schematic diagram of the treatment errors and
complications in implant positioning in the anterior and posterior
zone is presented in Fig. 1.
9. Treatment errors and complications in
peri-implant soft tissue management
In healthy conditions, the peri-implant site is
characterized by the absence of erythema, and the absence of
bleeding on probing, swelling and suppuration. Peri-implantitis is
a plaque-associated pathological condition that occurs in tissues
around dental implants and is characterized by inflammation in the
peri-implant mucosa and subsequent progressive loss of supporting
bone. Histologically, peri-implantitis manifests as apically
extending lesions beyond the junctional epithelium, with dense
infiltrates rich in neutrophils, macrophages and plasma cells,
reflecting a more advanced and destructive state than peri-implant
mucositis does. Clinically, peri-implantitis is characterized by
mucosal recession, increased probing depths, bleeding on probing
and/or suppuration and progressive radiographic bone loss, which is
frequently associated with plaque accumulation and inadequate
maintenance (19,37). The health and stability of
peri-implant soft tissues are critical to the long-term success of
dental implants. Complications, such as mucosal recession,
insufficient attached gingiva and inadequate vestibular depth can
arise from poor flap management, improper soft tissue handling, or
failure to perform soft tissue augmentation procedures when
indicated. Thin biotypes are particularly prone to gingival
fenestrations, whereas inadequate stabilization or improper
suturing during soft tissue grafting can lead to graft exposure,
infection, or loss of the graft (38).
In order to mitigate these risks, the early and
thorough assessment of mucosal thickness and biotype should guide
treatment planning. The use of autogenous grafts or xenogenic
collagen matrices, alongside the careful timing of soft tissue
augmentation, either at the time of implant placement or as a
separate procedure, can significantly reduce the likelihood of
complications. Ensuring proper graft stabilization and a
well-designed flap that accommodates the needs of the graft are
essential for the success of soft tissue management around implants
(20,38).
10 Treatment errors and complications in
peri-implant hard tissue management
Peri-implantitis represents one of the most
formidable challenges in ensuring the long-term success of dental
implants. Characterized by progressive bone loss, chronic
inflammation and pocket formation, peri-implantitis compromises the
structural integrity of the implant and its surrounding tissues. A
multifactorial aetiology underlies this condition, with poor plaque
control, cement remnants, excessive occlusal loading and a history
of periodontitis contributing significantly to its onset and
progression (6,19).
Early diagnosis and intervention are paramount.
Failure to recognize mucositis, often the precursor to
peri-implantitis, can lead to irreversible bone destruction and
implant failure. Once diagnosed, effective management involves a
comprehensive approach, including implant surface decontamination
techniques such as air abrasion, laser therapy, or the use of
chemical decontaminants. In advanced cases, surgical or
regenerative treatments are required to arrest disease progression
and promote tissue healing.
Prevention remains the cornerstone of successful
implant therapy. Ensuring accurate implant placement, avoiding
excessive occlusal stress and educating patients on optimal oral
hygiene practices are essential for reducing the risk of
peri-implant complications. Additionally, regular maintenance
visits and early intervention in the event of tissue changes are
critical for prolonging the lifespan of implants (33,34).
11. Avoiding intra- and post-operative
complications in maxillary sinus elevation
Maxillary sinus elevation procedures are critical
components of implantology when insufficient bone volume in the
posterior maxilla is addressed. The procedure, however, is not
without its complications, particularly intraoperative challenges
(35). One of the most common and
concerning intraoperative complications is perforation of the
Schneiderian membrane. This delicate membrane plays a pivotal role
in maintaining sinus integrity, and its perforation can lead to
severe complications, including infection, graft migration and
oroantral communication (24).
Other intraoperative challenges include the risk of
developing sinusitis, haemorrhage and excessive post-operative
congestion. These issues can be mitigated by adopting minimally
invasive techniques, such as piezosurgery, which enables atraumatic
bone cutting and preserves accurate localization of the sinus
anatomy, reducing the likelihood of membrane perforation and other
complications (39).
Post-operative management is equally critical.
Antibiotics to prevent infection, nasal decongestants to reduce
swelling and patient positioning recommendations to avoid undue
pressure on the graft site are essential components of
post-surgical care. In cases of significant membrane perforation,
adjunctive therapies, such as collagen membranes or platelet-rich
fibrin can promote membrane healing and further safeguard the
success of the procedure.
12. Lack of evidence regarding errors and
complications in periodontal and implant therapy
Despite the well-established nature of complications
in periodontal and implant therapies, there remains a notable
paucity of high-quality evidence documenting their true incidence
classification and long-term outcomes. An ample amount of the
available evidence is derived from small cohort studies, case
series, or anecdotal reports, which limits the ability to
generalize findings or identify consistent patterns across diverse
patient populations and clinical settings (5,36).
The absence of standardized definitions for
complications exacerbates the difficulty in comparing outcomes
across studies and clinical practices. A comprehensive and unified
classification system would allow for more reliable reporting and a
clearer understanding of complication rates. In order to fill these
gaps, there is an urgent need for longitudinal, randomized
controlled trials, as well as the establishment of national and
international registries to track implant-related failures and
complications over extended periods of time.
Furthermore, the development of evidence-based
clinical guidelines would greatly benefit clinicians by providing
clear frameworks for the prevention, early detection and management
of complications. Such evidence will not only improve patient
outcomes, but will also enhance training programs for future
clinicians, equipping them with the tools necessary to mitigate
risk and optimize treatment strategies (5).
13. Treatment errors and complications in
periodontal therapy in medically compromised patients
Periodontal therapy in medically compromised
patients presents unique challenges, as systemic conditions such as
uncontrolled diabetes mellitus, bleeding disorders, cardiovascular
diseases and immunosuppression exacerbate the risk of
complications. For example, poor glycaemic control in diabetic
patients markedly impairs wound healing, elevates infection rates
and increases the risk of periodontal breakdown. Similarly.
Patients receiving anticoagulant therapy are at an increased risk
of perioperative bleeding, which can complicate surgical
procedures.
Failure to adequately modify treatment protocols for
these patients can lead to severe outcomes, such as delayed wound
healing, wound dehiscence, osteonecrosis, or even systemic
infections. A thorough pre-operative evaluation, including a
comprehensive medical history, interprofessional communications
with the healthcare team of the patient, and relevant laboratory
investigations (such as international normalized ratio, HbA1c
levels and platelet count), is essential for mitigating these
risks.
Treatment strategies to reduce complications include
the use of local haemostatic agents, the use of therapeutic
interventions to limit stress on the patient, antibiotic
prophylaxis to prevent infection, and patient-specific oral hygiene
instructions. Clinicians need to balance the therapeutic benefits
of periodontal intervention with the potential systemic risks,
proceed with caution and adjust the treatment approach as necessary
to safeguard patient health (40).
A summary of preventive and corrective measures is
outlined in Table II. This table
provides practical strategies to minimize errors and manage
complications across different phases of periodontal and implant
therapy.
 | Table IIStrategies for the prevention and
management of errors and complications in periodontal and implant
therapy. |
Table II
Strategies for the prevention and
management of errors and complications in periodontal and implant
therapy.
|
Section/procedure | Common errors and
complications | Preventive and
management strategies |
|---|
| 1. Non-surgical
periodontal therapy (SRP/NSPT) | Soft tissue trauma,
root surface over-instrumentation, dentinal hypersensitivity,
incomplete calculus removal in deep pockets, instrument fracture,
subcutaneous emphysema, discomfort, poor compliance. | Use proper
instrument angulation and sharp curettes; ensure adequate
irrigation with ultrasonics; combine hand and powered instruments
in deep/narrow pockets; avoid aggressive root planing; prescribe
adjunctive antimicrobials (e.g., amoxicillin + metronidazole) only
in advanced cases; use local anaesthesia for comfort; re-evaluate
unresolved pockets for surgical access; manage hypersensitivity
with desensitizing agents; emphasize supportive periodontal therapy
(SPT) with strict recall. |
| 2. Flap
surgeries | Poor incision
design, overharvesting palatal tissue, flap necrosis, excessive
bleeding, graft mobility, tissue shrinkage, infection, compromised
aesthetics. | Careful case
selection; respect anatomical landmarks (avoid >7 mm from
greater palatine foramen); achieve tension-free flap closure;
ensure graft immobilization; atraumatic reflection; meticulous
suturing; good post-operative instructions; clinician training and
surgical experience. |
| 3. Regenerative
periodontal surgery | Flap tension,
membrane exposure, infection, graft collapse/resorption, allergic
reactions, poor healing in smokers/diabetics. | Design tension-free
flaps with primary closure; ensure space maintenance; use
biocompatible, evidence-based biomaterials; control systemic
conditions (diabetes); enforce smoking cessation; provide rigorous
post-operative care and frequent monitoring. |
| 4. Root coverage
procedures | Misdiagnosis of
recession, poor flap thickness/design, flap perforation, donor site
morbidity, graft necrosis, scarring, colour mismatch. | Correct diagnosis
(differentiate from altered passive eruption); evaluate risk
factors (smoking, trauma, thin biotype); use atraumatic harvesting
with respect to palatal landmarks; ensure adequate flap thickness
and vascularity; stabilize grafts; maintain haemostasis; instruct
patients on careful hygiene; ensure tension-free sutures. |
| 5. Ridge
augmentation (GBR) | Membrane exposure,
wound dehiscence, infection, graft resorption, graft
instability. | Perform CBCT-based
pre-operative planning; select graft materials appropriately; avoid
overfilling; achieve set al fixation and space maintenance;
tension-free flap advancement; prescribe proper post-operative
instructions to avoid trauma. |
| 6. Palatal soft
tissue harvesting | Post-operative
pain, bleeding, hematoma, tissue necrosis, delayed healing, graft
shrinkage, poor aesthetics. | Limit graft size
and thickness; avoid harvesting too close to greater palatine
foramen; design incisions preserving blood supply; use palatal
stents and cold packs post-operatively; ensure meticulous
haemostasis; prescribe analgesics; close monitoring for delayed
bleeding or necrosis. |
| 7. Implant
placement-aesthetic zone | Incorrect 3D
positioning, poor emergence profile, gingival recession, papilla
loss, aesthetic failure. | Prosthetically
driven planning; CBCT-based site analysis; use surgical
guides/templates; coordinate with restorative specialists; assess
gingival biotype and bone morphology pre-operatively. |
| 8. Implant
placement-posterior region | Limited visibility,
sinus perforation, vascular injury, poor interarch space, dense
bone complications. | Detailed CBCT
assessment; identify sinus anatomy and mandibular landmarks; staged
augmentation if inadequate bone; use careful drilling protocols;
manage occlusion precisely. |
| 9. Peri-implant
soft tissue management | Mucosal recession,
thin biotype complications, graft exposure, inadequate vestibular
depth. | Assess soft tissue
biotype early; plan augmentation when indicated; use autografts or
collagen matrices; design tension-free flaps; ensure graft
stabilization; educate patients on post-operative hygiene. |
| 10. Peri-implant
hard tissue management (peri-implantitis) | Bone loss,
pocketing, implant failure, progression from mucositis to
peri-implantitis. | Early detection and
treatment of mucositis; regular maintenance visits; avoid excess
cement/occlusal overload; decontaminate implant surfaces (air
abrasion, laser, chemicals); use regenerative surgery in advanced
cases; reinforce patient hygiene. |
| 11. Maxillary sinus
elevation | Schneiderian
membrane perforation, sinusitis, graft migration, bleeding,
oroantral communication. | Use minimally
invasive techniques (e.g., piezosurgery); precise anatomical
localization via CBCT; manage membrane perforation with
collagen/PRF; prescribe antibiotics and decongestants; patient
positioning instructions post-op. |
| 12.
Periodontal/implant therapy in medically compromised patients | Delayed healing,
excessive bleeding, infection, osteonecrosis, systemic
complications. | Pre-operative
medical consultation and investigations (HbA1c, INR, platelet
count); modify treatment protocols; use local haemostatic agents;
prescribe antibiotics when indicated; minimize surgical trauma;
schedule close follow-up; customize oral hygiene instructions. |
14. Conclusion and future perspectives
Limitations of current evidence
Current knowledge on errors and complications in
periodontal and implant therapy is constrained by weak evidence.
The majority of studies are observational, with small cohorts and
inconsistent outcome measures, limiting comparability and clinical
translation (13,15). In implant research, variations in
operator skill, surgical protocols, and patient selection further
complicate interpretation. Data on long-term outcomes and rare
complications remain limited. These shortcomings highlight the need
for standardized definitions, uniform reporting, and well-designed
prospective multi-centre trials to provide stronger guidance for
prevention and management strategies.
In conclusion, although not uncommon, complications
in periodontal and implant therapy can significantly affect
treatment success and long-term patient outcomes. These
complications often arise from a combination of anatomical
limitations, operator error and systemic health factors,
underscoring the need for a comprehensive and proactive approach to
prevention and management. As summarized in the present review, a
thorough understanding of the potential challenges, combined with
careful planning and adherence to evidence protocols, is critical
for minimizing complications. Emphasizing patient-specific care,
precise surgical techniques and continuous professional development
will allow clinicians to anticipate risks and optimize treatment
strategies. Furthermore, embracing a multidisciplinary,
patient-centred approach will not only enhance clinical outcomes,
but will also ensure the delivery of safe, effective and
personalized care. By refining these practices, clinicians can
markedly improve the success rate of periodontal and implant
therapies, ultimately advancing the standard of care and improving
the quality of life of patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
VR was involved in the conception and design of the
study, the compilation of data from the literature, the analysis
and interpretation of data from the literature and manuscript
preparation. AU was involved in the design of the study, and in the
reviewing and editing of the manuscript. AS was involved in
manuscript preparation, and in the reviewing and editing of the
manuscript. SUN was involved in the conception and design of the
study, the compilation of data from the literature, the analysis
and interpretation of data from the literature, and in manuscript
preparation. All authors have read and approved the final
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zucchelli G, Wang HL and Chambrone L:
Complications and treatment errors in periodontal and implant
therapy. Periodontol 2000. 92:9–12. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cairo F, Pagliaro U and Nieri M: Treatment
of gingival recession with coronally advanced flap procedures: A
systematic review. J Clin Periodontol. 35 (8 Suppl):S136–S162.
2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sculean A, Stavropoulos A, Windisch P,
Keglevich T, Karring T and Gera I: Healing of human intrabony
defects following regenerative periodontal therapy with a
bovine-derived xenograft and guided tissue regeneration. Clin Oral
Investig. 8:70–74. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Marzadori M, Stefanini M, Mazzotti C, Ganz
S, Sharma P and Zucchelli G: Soft-tissue augmentation procedures in
edentulous esthetic areas. Periodontol 2000. 77:111–122.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Stefanini M, Marzadori M, Aroca S, Felice
P, Sangiorgi M and Zucchelli G: Decision making in root-coverage
procedures for the esthetic outcome. Periodontol 2000. 77:54–64.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Seyssens L, Eghbali A and Cosyn J: A
10-year prospective study on single immediate implants. J Clin
Periodontol. 47:1248–1258. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Buser D, Sennerby L and De Bruyn H: Modern
implant dentistry based on osseointegration: 50 years of progress,
current trends and open questions. Periodontol 2000. 73:7–21.
2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Coluzzi DJ, Mizutani K, Yukna R, Al-Falaki
R, Lin T and Aoki A: Surgical laser therapy for periodontal and
Peri-implant disease. Clin Dentistry Rev. 6(7)2022.
|
|
9
|
Mizutani K, Aoki A, Coluzzi D, Yukna R,
Wang CY, Pavlic V and Izumi Y: Lasers in minimally invasive
periodontal and Peri-implant therapy. Periodontol 2000. 71:185–212.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Graziani F, Tinto M, Orsolini C, Izzetti R
and Tomasi C: Complications and treatment errors in nonsurgical
periodontal therapy. Periodontol 2000. 92:21–61. 2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Thennukonda RA and Natarajan BR: Adverse
events associated with ultrasonic scalers: A manufacturer and user
facility device experience database analysis. Indian J Dent Res.
26:598–602. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Heitz-Mayfield LJA and Lang NP: Surgical
and nonsurgical periodontal therapy. Learned and unlearned
concepts. Periodontol 2000. 62:218–231. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rinieshah Nair R, Baskran and
Ganesh BS: Analysis of localized periodontal flap surgical
techniques: An institutional based retrospective study. Ann Med
Health Sci Res. 11:319–324. 2021.
|
|
14
|
Kripal K, Chandrashekar BM, Anuroopa P,
Rajan S, Sirajuddin S, Prabhu S, Kumuda MN and Apine A: Practical
periodontal surgery: An overview. J Evol Med Dent Sci.
3:14398–14409. 2014.
|
|
15
|
Tietmann C, Jepsen S, Heibrok H, Wenzel S
and Jepsen K: Long-term stability of regenerative periodontal
surgery and orthodontic tooth movement in stage IV periodontitis:
10-year data of a retrospective study. J Periodontol. 94:1176–1186.
2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cortellini P and Tonetti MS: Focus on
intrabony defects: Guided tissue regeneration. Periodontol 2000.
22:104–132. 2000.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jepsen S, Schwarz F, Cordaro L, Derks J,
Hämmerle CHF, Heitz-Mayfield LJ, Hernández-Alfaro F, Meijer HJA,
Naenni N, Ortiz-Vigón A, et al: Regeneration of alveolar ridge
defects. Consensus report of group 4 of the 15th European Workshop
on Periodontology on Bone Regeneration. J Clin Periodontol.
46:277–286. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Cortellini P and Tonetti MS: Clinical
concepts for regenerative therapy in intrabony defects. Periodontol
2000. 68:282–307. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chiapasco M and Casentini P: Horizontal
bone-augmentation procedures in implant dentistry: Prosthetically
guided regeneration. Periodontology 2000. 77:213–240.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mounssif I, Stefanini M, Mazzotti C,
Marzadori M, Sangiorgi M and Zucchelli G: Esthetic evaluation and
Patient-centered outcomes in Root-coverage procedures.
Periodontology 2000. 77:19–53. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Huang L, Neiva REF and Wang H: Factors
affecting the outcomes of coronally advanced flap root coverage
procedure. J Periodontol. 76:1729–1734. 2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rebele SF, Zuhr O, Schneider D, Jung RE
and Hürzeler MB: Tunnel technique with connective tissue graft
versus coronally advanced flap with enamel matrix derivative for
root coverage: A RCT using 3D digital measuring methods. Part II.
Volumetric studies on healing dynamics and gingival dimensions. J
Clin Periodontol. 41:593–603. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Blyleven GM, Johnson TM, Inouye KA,
Stancoven BW and Lincicum AR: Factors influencing intraoperative
and postoperative complication occurrence: A series of 1135
periodontal and implant-related surgeries. Clin Exp Dent Res.
10(e849)2024.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Testori T, Tavelli L, Scaini R, Saibene
AM, Felisati G, Barootchi S, Decker AM, Deflorian MA, Rosano G,
Wallace SS, et al: How to avoid intraoperative and postoperative
complications in maxillary sinus elevation. Periodontology 2000.
92:299–328. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Griffin TJ, Cheung WS, Zavras AI and
Damoulis PD: Postoperative complications following gingival
augmentation procedures. J Periodontol. 77:2070–2079.
2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Morzycki AD, Hudson AS, Samargandi OA,
Bezuhly M and Williams JG: Reporting adverse events in plastic
surgery: A systematic review of randomized controlled trials. Plast
Reconstr Surg. 143:199e–208e. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Jung RE, Ioannidis A, Hämmerle CHF and
Thoma DS: Alveolar ridge preservation in the esthetic zone.
Periodontology 2000. 77:165–175. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tavelli L, Barootchi S, Stefanini M,
Zucchelli G, Giannobile WV and Wang HL: Wound healing dynamics,
morbidity, and complications of palatal soft-tissue harvesting.
Periodontology 2000. 92:90–119. 2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kumar Sharma V, Kirmani M, Trivedi H, Bey
A and Sharma VK: Post-operative complications of periodontal
surgery. Int J Contemporary Med Res, 2016. www.ijcmr.com.
|
|
30
|
Ripoll S, de Velasco-Tarilonte AF, Bullón
B, Ríos-Carrasco B and Fernández-Palacín A: Complications in the
use of deepithelialized free gingival graft vs. Connective tissue
graft: A one-year randomized clinical trial. Int J Environ Res
Public Health. 18(4504)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Testori T, Weinstein T, Scutellà F, Wang
HL and Zucchelli G: Implant placement in the esthetic area:
Criteria for positioning single and multiple implants. Periodontol
2000. 77:176–196. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sachin PG, Uppoor AS and Nayak SU:
Nanoscale surface modification of dental implants-An emerging boon
for osseointegration and biofilm control. Acta Marisiensis Seria
Med Sci. 68:154–158. 2022.
|
|
33
|
Zucchelli G, Sharma P and Mounssif I:
Esthetics in periodontics and implantology. Periodontology 2000.
77:7–18. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kamakshi L, Uppoor A, Nayak D and Pralhad
S: Evaluation of papilla levels following three different
techniques for the second stage of implants-A clinical and
radiographic study. J Indian Soc Periodontol. 25:120–127.
2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Jensen OT: Article in the International
journal of oral & maxillofacial implants [Internet], 1996.
Available from: https://www.researchgate.net/publication/13568970.
|
|
36
|
Chambrone L and Zucchelli G: Why is there
a lack of evidence regarding errors and complications in
periodontal and implant therapy? Periodontology 2000. 92:13–20.
2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pjetursson BE, Tan WC, Zwahlen M and Lang
NP: A systematic review of the success of sinus floor elevation and
survival of implants inserted in combination with sinus floor
elevation. J Clin Periodontol. 35 (8 Suppl):S216–S240.
2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Mazzotti C, Stefanini M, Felice P,
Bentivogli V, Mounssif I and Zucchelli G: Soft-tissue dehiscence
coverage at peri-implant sites. Periodontology 2000. 77:256–272.
2018.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Hegde R, Prasad K and Shroff KK: Maxillary
sinus augmentation using sinus membrane elevation without grafts-A
systematic review. J Indian Prosthodont Soc. 16:317–322.
2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Samara W, Moztarzadeh O, Hauer L and
Babuska V: Dental implant placement in medically compromised
patients: A literature review. Cureus. 16(e54199)2024.PubMed/NCBI View Article : Google Scholar
|