Introduction
Anterior cruciate ligament (ACL) injuries are among
the most common and economically significant musculoskeletal
injuries, particularly in athletes and physically active
individuals, with an estimated annual incidence of 1 in 3,500
individuals and ~400,000 ACL reconstruction (ACLR) procedures
performed annually in the USA (1).
These injuries frequently result in knee instability, reduced
functional capacity and long-term degenerative changes (2). ACLR is the standard surgical
intervention used to restore knee stability and enable a return to
pre-injury activity levels, with studies demonstrating that 80% of
individuals return to some form of sport and 55% return to
competitive levels following reconstruction (3). While ACLR is widely accepted as
effective, the optimal timing of the surgery remains a critical yet
unresolved clinical question. Early reconstruction is often
advocated to prevent secondary injuries, while delayed approaches
aim to reduce post-operative complications, such as arthrofibrosis
(2,4). This dichotomy underscores the need to
balance immediate surgical intervention with pre-operative
rehabilitation to optimize outcomes.
The debate surrounding early vs. delayed ACLR
centers on competing biomechanical, biological and clinical
considerations. Proponents of early surgery argue that prompt
stabilization reduces the risk of meniscal and chondral damage
caused by persistent knee instability (4,5).
Conversely, delayed reconstruction allows for the resolution of
acute inflammation and the restoration of pre-operative range of
motion, potentially minimizing post-operative stiffness (2,4).
Clinical guidelines lack consensus, with variations in recommended
waiting periods ranging from weeks to several months depending on
institutional protocols (2,6).
This variability reflects gaps in evidence regarding how surgical
timing interacts with patient-specific factors, such as age,
activity level and pre-operative rehabilitation compliance.
Muscle atrophy and neuromuscular dysfunction
represent significant consequences of ACL injury that influence
both surgical timing and rehabilitation outcomes. Quadriceus
weakness of up to 30% compared to the contralateral limb is nearly
ubiquitous following ACL injury, resulting from a combination of
disuse atrophy and central activation failure. Research indicates
that the optimal window for ACLR regarding muscle preservation may
lie between 21-100 days post-injury, as longer delays increase the
risk of progressive quadriceps atrophy and impaired early
rehabilitation (7).
The existing literature on the timing of ACLR has
been limited by heterogeneous study designs, inconsistent
definitions of ‘early’ vs. ‘delayed’ surgery, and short follow-up
durations (2,5). While recent investigations have
explored objective outcomes, such as muscle strength recovery and
return-to-sport rates, only a limited number of studies have
comprehensively evaluated patient-reported outcomes across diverse
demographic groups (6).
Furthermore, previous research often focuses on isolated ACL
injuries, neglecting the impact of concomitant meniscal repairs or
degenerative changes that frequently accompany delayed
presentations (4,5). These limitations hinder the
development of standardized, evidence-based protocols tailored to
individual patient needs and activity demands.
The present retrospective study aimed to address
these gaps in available evidence by analyzing the association
between the timing of ACLR and multidimensional patient outcomes in
a large, heterogeneous cohort. Despite numerous investigations, the
lack of an available consensus on optimal surgical timing persists,
particularly regarding its interaction with patient age,
preoperative activity level and concomitant knee pathology
(3,4,6). By
evaluating functional recovery, complication rates, and
patient-reported outcomes across different surgical intervals, the
present study aimed to provide clinicians with data-driven insights
to guide shared decision-making. The primary objective of the
present study was to determine whether early ACLR demonstrates
superior outcomes compared to delayed reconstruction when
controlling for demographic variables and injury characteristics,
thereby informing personalized treatment strategies for
ACL-deficient patients.
Patients and methods
Study design and setting
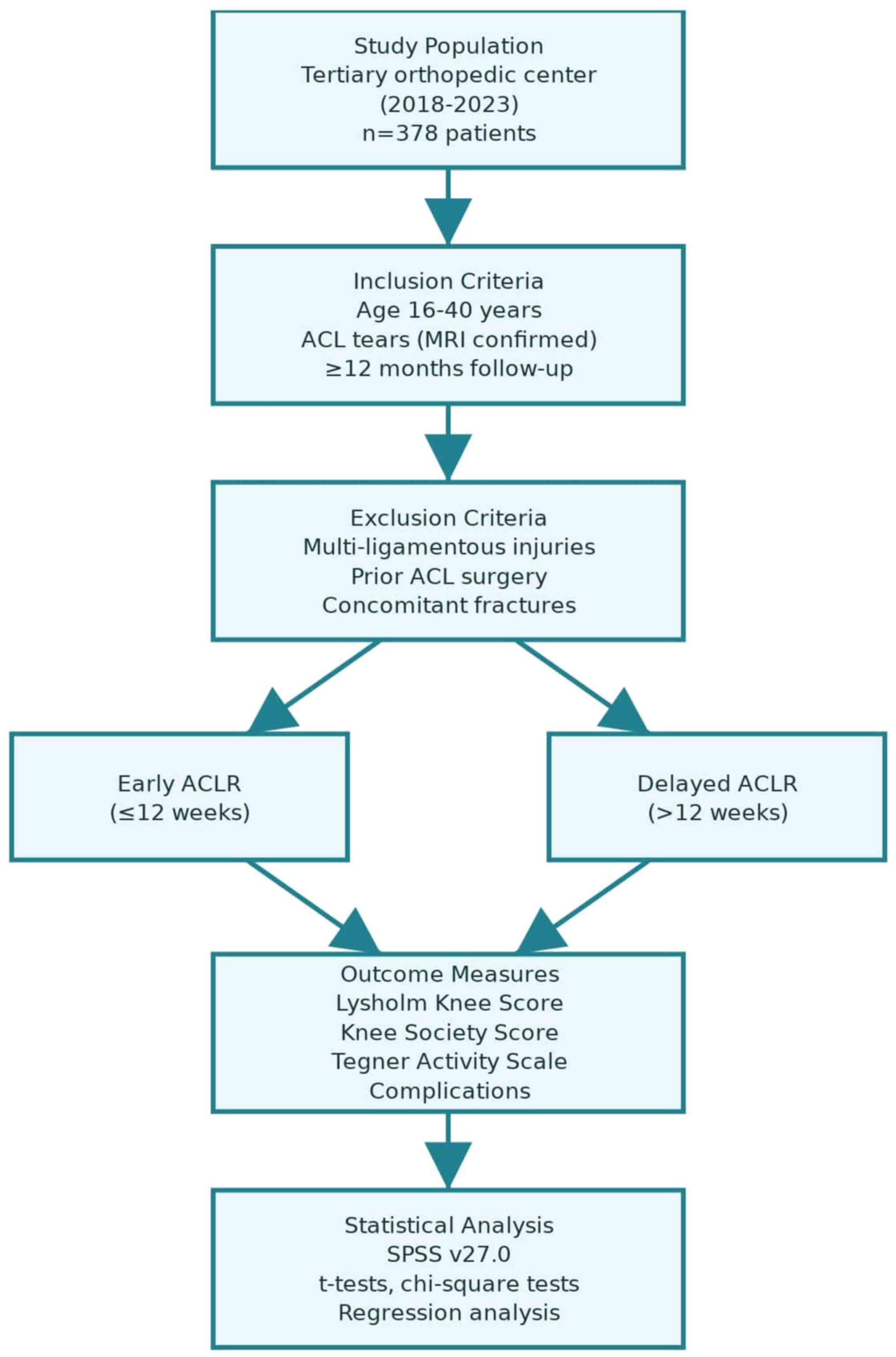
A retrospective cohort study was conducted at a
tertiary orthopedic center to evaluate the effects of early vs.
delayed ACLR on patient outcomes. The study protocol received
ethical approval from the Institutional Review Board of Raparin
University (Sulaymaniyah, Iraq; Reference no. 2866/28-5-2023). The
dataset comprised electronic medical records covering the period
between January, 2018 to December 20, 2024. The authors retrieved
these records and conducted follow-up assessments using structured
questionnaires between December 20, 2024 and April 10, 2025,
through in-person visits and telephone interviews. This combined
approach, retrospective clinical data supplemented with
contemporaneous patient-reported outcomes, is consistent with
current methodological standards aimed at enhancing data
completeness and validity. A detailed overview of participant
inclusion and analysis is illustrated in Fig. 1.
Participants and sampling
A non-probability purposive sampling strategy was
employed to select participants aged 16-40 years diagnosed with
partial or complete ACL tears via magnetic resonance imaging (MRI)
and a clinical examination. The sample size was calculated using
G*Power software (version 3.1), based on an effect size of 0.35
derived from a comparable study, with α=0.05 and 80% power,
yielding a minimum required sample of 68 participants. To account
for potential attrition, the target sample was increased, resulting
in 378 patients. The inclusion criteria required documented ACL
injury management at the study site and the completion of
post-operative follow-up for a period ≥12 months. The exclusion
criteria excluded individuals with multi-ligamentous injuries,
prior ipsilateral ACL reconstruction, cognitive impairments
affecting self-reporting, or concomitant fractures/dislocations
that could confound the recovery outcomes.
The present study reviewed the outcomes of ACL
injury regarding surgical timing, comparing early (within 12 weeks
post-injury) and delayed (>12 weeks post-injury) interventions
in a heterogeneous patient population. The objective was to
identify differences in the outcome measures related to surgical
timing, thereby providing insight applicable to a broad spectrum of
patients.
Data collection instruments and
variables
The data were extracted from electronic medical
records and structured questionnaires adapted from validated tools,
including the Lysholm Knee Score (LKS) (8), Knee Society Score (KSS) (9) and Tegner Activity Scale (TAS)
(8). The retrieval of medical
record data and the administration of questionnaires were carried
out by the authors between December 20, 2024 and April 10, 2025,
after obtaining ethical approval. The questionnaire was comprised
of three domains: i) Socio-demographics: Age, sex, occupation,
education level, residence and pre-injury activity level. ii)
Clinical and surgical details: Injury mechanism, surgical timing
stratified as early (≤12 weeks) or delayed (>12 weeks). iii)
Rehabilitation: The duration of pre-operative and post-operative
rehabilitation and participation.
The outcome measures were the following: Functional
recovery (LKS and KSS), activity level (measured using the TAS),
complications (infection, re-tear, stiffness, pain, instability,
nerve injury) and patient satisfaction. To ensure reliability, the
questionnaire underwent pilot testing with 5 patients, which was
conducted by the authors between December 1, 2024, and December 15,
2024, demonstrating excellent internal consistency (Cronbach s
α=0.89) and content validity, as assessed by three orthopedic
surgeons independently. Final data collection was subsequently
carried out by the authors via telephone or electronic
communication to maximize follow-up completeness.
Ethical considerations
All data were anonymized and stored on secure,
password-protected servers. Ethical approval for the full study,
including pilot testing and patient follow-up, was obtained prior
to data collection. The study adhered to STROBE guidelines for
observational research to ensure methodological rigor and
transparency.
Statistical analysis
Statistical analyses were performed using SPSS
Statistics (v27.0). Descriptive statistics summarized the baseline
characteristics. Continuous variables were compared between early
and delayed groups using independent t-tests or Mann-Whitney U
tests, depending on normality (assessed using Shapiro-Wilk tests).
The categorical variables (e.g., complication rates) were analyzed
using Chi-squared or Fisher s exact tests. Multivariable
linear and logistic regression models adjusted for confounders,
including age, body mass index, pre-operative activity level and
meniscal/chondral injuries.
Results
The study included a total of 378 patients, with 108
(28.6%) patients in the early ACL group and 270 (71.4%) patients in
the delayed ACLR group. Among these, 95 (88.0%) patients in the
early ACLR group were male compared to 264 (97.8%) in the delayed
ACLR group, and the difference between the groups was statistically
significant (P<0.001). The median age of all the patients was 29
years [quartile range (QR), 24-35], with the early ACLR group
having a younger median age of 27 years (QR, 22.5-33), compared to
30 years (QR, 25-37) in the delayed ACLR group (P=0.003). As
regards occupation, heavy manual labor was the most common type of
work, reported by 37 (34.3%) patients in the early group and 90
(33.3%) patients in the delayed ACLR group (P=0.096). The majority
of the patients had attained a higher education, with 46 (42.6%)
patients in the early ACLR group and 143 (53.0%) patients in the
delayed ACLR group (P=0.138). Urban residency was reported by 58
(53.7%) of the patients in the early ACLR group and 128 (47.4%) of
the patients in the delayed ACLR group (P=0.425). Sports-related
injury was the leading cause of ACL rupture, accounting for 73
(67.6%) of early cases and 210 (77.8%) of delayed cases (P=0.217)
(Table I).
 | Table IComparison of demographic,
socioeconomic and clinical characteristics between the early and
delayed ACLR groups. |
Table I
Comparison of demographic,
socioeconomic and clinical characteristics between the early and
delayed ACLR groups.
| Variables | Total (n=378) | Early ACLR
(n=108) | Delayed ACLR
(n=270) | P-value |
|---|
| Sex, n (%) | | | | <0.001 |
|
Male | 359 | 95 (88.0) | 264 (97.8) | |
|
Female | 19 | 13 (12.0) | 6 (2.2) | |
| Age, median (QR) | 29 (24-35) | 27 (22.5-33) | 30 (25-37) | 0.003 |
| BMI, median (QR) | 26.2 (23.8-28.7) | 25.9 (23.1-27.9) | 26.2 (24.2-29.1) | 0.547 |
| Occupation, n
(%) | | | | 0.096 |
|
Heavy manual
labor | 127 | 37 (34.3) | 90 (33.3) | |
|
Light manual
labor | 21 | 5 (4.6) | 16 (5.9) | |
|
Nonmanual
(walking/standing) | 71 | 14 (13.0) | 57 (21.1) | |
|
Non-manual
(non-office) | 59 | 24 (22.2) | 35 (13.0) | |
|
Office | 92 | 24 (22.2) | 68 (25.2) | |
|
Domestic | 8 | 4 (3.7) | 4 (1.5) | |
| Educational level, n
(%) | | | | 0.138 |
|
Illiterate | 12 | 4 (3.7) | 8 (3.0) | |
|
Primary | 43 | 10 (9.3) | 33 (12.2) | |
|
Secondary | 65 | 26 (24.1) | 39 (14.4) | |
|
High
school | 69 | 22 (20.4) | 47 (17.4) | |
|
Higher
education | 189 | 46 (42.6) | 143 (53.0) | |
| Time from injury to
surgery, weeks, median (QR) | 48.0
(12.0-144.0) | 4.0 (2.0-8.0) | 80.0
(36.0-208.0) | <0.001 |
| Residence, n (%) | | | | 0.425 |
|
Urban | 186 | 58 (53.7) | 128 (47.4) | |
|
Sub-urban | 180 | 46 (42.6) | 134 (49.6) | |
|
Rural | 12 | 4 (3.7) | 8 (3.0) | |
| History of other knee
injury, n (%) | | | | 0.315 |
|
Yes | 72 | 24 (22.2) | 48 (17.8) | |
|
No | 306 | 84 (77.8) | 222 (82.2) | |
| Monthly income, n
(%) | | | | 0.366 |
|
Sufficient | 114 | 33 (30.6) | 81 (30.0) | |
|
Barely
sufficient | 243 | 72 (66.7) | 171 (63.3) | |
|
Insufficient | 21 | 3 (2.8) | 18 (6.7) | |
| Causes of ACL
injury, n (%) | | | | 0.217 |
|
Sport | 283 | 73 (67.6) | 210 (77.8) | |
|
Road traffic
accident | 15 | 7 (6.5) | 8 (3.0) | |
|
Bullet | 2 | 0 (0.0) | 2 (0.7) | |
|
Fall from
height | 39 | 15 (13.9) | 24 (8.9) | |
|
Disease | 3 | 1 (0.9) | 2 (0.7) | |
|
Others | 36 | 12 (11.1) | 24 (8.9) | |
| Return to daily
activity, weeks, median (QR) | 6 (4-9) | 7 (2-9) | 6 (2-9) | 0.987 |
Among the 378 patients included in the present
study, 114 (30.2%) patients underwent rehabilitation prior to
surgery, with a significantly higher proportion in the delayed ACLR
group (n=90, 33.3%) compared to the early ACLR group (n=24, 22.2%)
(P=0.035). The median duration of pre-operative rehabilitation was
4.0 weeks (QR, 2.5-8.5), with patients in the delayed ACLR group
receiving longer periods of rehabilitation (median, 5.0 weeks; QR,
4.0-10.0) than those in the early ACLR group (median, 3.0 weeks;
QR, 2.0-4.0) (P=0.011). Post-operative rehabilitation was almost
universal, with 366 (96.8%) patients participating and no
significant difference observed between the early (n=106, 98.1%)
and delayed ACLR groups (n=260, 96.3%) (P=0.285). The median
duration of post-operative rehabilitation was 9.0 weeks (QR,
5.0-17.0), with comparable durations between the groups (P=0.734).
A history of knee popping sounds was reported in 230 (60.8%)
patients, with similar rates between the early (n=63, 58.3%) and
delayed (n=167, 61.9%) ACLR groups (P=0.275). The median frequency
of knee popping was 30 episodes per month (QR, 15.0-75.0),
consistent across both groups (P=0.606) (Table II).
 | Table IIPre-operative and post-operative
rehabilitation profiles and symptomatology in early vs. delayed
ACLR. |
Table II
Pre-operative and post-operative
rehabilitation profiles and symptomatology in early vs. delayed
ACLR.
| Variables | Total (n=378) | Early ACLR
(n=108) | Delayed ACLR
(n=270) | P-value |
|---|
| Rehabilitation
prior to surgery, n (%) | | | | 0.035 |
|
Yes | 114 | 24 (22.2) | 90 (33.3) | |
|
No | 264 | 84 (77.8) | 180 (66.7) | |
| Pre-operative
rehabilitation duration, weeks, median (QR) | 4.0 (2.5-8.5) | 3.0 (2.0-4.0) | 5.0 (4.0-10.0) | 0.011 |
| Post-operative
rehabilitation, n (%) | | | | 0.285 |
|
Yes | 366 | 106 (98.1) | 260 (96.3) | |
|
No | 12 | 2 (1.9) | 10 (3.7) | |
| Post-operative
rehabilitation, weeks, median (QR) | 9.0 (5.0-17.0) | 8.0 (4.0-16.0) | 9.0 (5.0-20.0) | 0.734 |
| History of knee
popping sound, n (%) | | | | 0.275 |
|
Yes | 230 | 63 (58.3) | 167 (61.9) | |
|
No | 148 | 45 (41.6) | 103 (38.1) | |
| Knee popping
sound/month, median (QR) | 30.0
(15.0-75.0) | 30.0
(15.0-50.0) | 30.0
(15.0-75.0) | 0.606 |
| History of knee
locking, n (%) | | | | 0.415 |
|
Yes | 85 | 21 (19.4) | 64 (23.7) | |
|
No | 293 | 87 (80.6) | 206 (76.3) | |
The functional outcomes assessed using the LKS
demonstrated that 200 (52.9%) patients achieved an excellent
outcome, with a significantly higher proportion in the early ACL
group (n=88, 81.5%) compared to the delayed ACLR group (n=112,
41.5%) (P<0.001). Good, fair and poor outcomes were reported in
26.5, 15.3 and 5.3% of the total cohort, respectively. The KSS for
range of motion indicated that the majority of the patients
attained excellent (n=286, 75.7%) or good (n=79, 20.9%) results,
with no significant difference between the early and delayed ACLR
groups (P=0.126). Similarly, the TAS revealed that 292 (77.2%)
patients achieved excellent activity levels, with a higher
percentage observed in the early ACLR group (n=93, 86.1%) compared
to the delayed ACLR group (n=199, 73.7%), reaching borderline
statistical significance (P=0.05) (Table III).
 | Table IIIComparison of functional outcomes,
range of motion, and activity levels in early vs. delayed ACLR
using LKS, KSS and TAS. |
Table III
Comparison of functional outcomes,
range of motion, and activity levels in early vs. delayed ACLR
using LKS, KSS and TAS.
| Variables | Total (n=378) | Early ACLR
(n=108) | Delayed ACLR
(n=270) | P-value |
|---|
| LKS for functional
outcome, n (%) | | | | <0.001 |
|
Excellent | 200 (52.9) | 88 (81.5) | 112 (41.5) | |
|
Good | 100 (26.5) | 8 (7.4) | 92 (34.1) | |
|
Fair | 58 (15.3) | 9 (8.3) | 49 (18.1) | |
|
Poor | 20 (5.3) | 3 (2.8) | 17 (6.3) | |
| KSS for range of
motion, n (%) | | | | 0.126 |
|
Excellent | 286 (75.7) | 89 (82.4) | 197 (73.0) | |
|
Good | 79 (20.9) | 15 (13.9) | 64 (23.7) | |
|
Fair | 11 (2.9) | 4 (3.7) | 7 (2.6) | |
|
Poor | 2 (0.5) | 0 (0.0) | 2 (0.7) | |
| TAS for activity
level, n (%) | | | | 0.05 |
|
Excellent | 292 (77.2) | 93 (86.1) | 199 (73.7) | |
|
Good | 73 (19.3) | 13 (12.0) | 60 (22.2) | |
|
Fair | 9 (2.4) | 2 (1.9) | 7 (2.6) | |
|
Poor | 4 (1.1) | 0 (0.0) | 4 (1.5) | |
Complications occurred in varying frequencies among
the patients. Infection was reported in 67 (17.7%) cases, with no
significant difference between the early (n=21, 19.4%) and delayed
ACLR groups (n=46, 17.0%) (P=0.655). Re-tear rates were low,
observed in 11 (2.9%) patients overall, and tended to be higher in
the delayed ACLR group (n=10, 3.7%) compared to the early ACLR
group (n=1, 0.9%), although this difference was not statistically
significant (P=0.190). Knee stiffness was significantly more
frequent in the delayed ACLR group 23, 8.5%) than in the early ACLR
group (n=2, 1.9%) (P=0.020). Nerve damage was rare, occurring in
only 1 (0.3%) patient in the delayed ACLR group, with no cases
reported in the early ACLR group. Persistent pain affected 55
(14.6%) patients, and was significantly more common in the delayed
ACLR group (n=49, 18.1%) than the early ACLR group (n=6, 5.6%)
(P=0.001). Similarly, knee instability was significantly higher in
the delayed ACLR group 22(8.1%) compared to the early ACLR group
(n=2, 1.9%) (P=0.020) (Table
IV).
 | Table IVComparison of postoperative
complications in early vs. delayed ACLR. |
Table IV
Comparison of postoperative
complications in early vs. delayed ACLR.
| Complications | Total (n=378) | Early ACLR
(n=108) | Delayed ACLR
(n=270) | P-value |
|---|
| Infection, n
(%) | 67 (17.7) | 21 (19.4) | 46 (17.0) | 0.655 |
|
Yes | 311 (82.3) | 87 (80.6) | 224 (83.0) | |
|
No | | | | |
| Re-tear, n (%) | | | | 0.190 |
|
Yes | 11 (2.9) | 1 (0.9) | 10 (3.7) | |
|
No | 367 (97.1) | 107 (99.1) | 260 (96.3) | |
| Knee-stiffness, n
(%) | | | | 0.020 |
|
Yes | 25 (6.6) | 2 (1.9) | 23 (8.5) | |
|
No | 353 (93.4) | 106 (98.1) | 247 (91.5) | |
| Nerve damage, n
(%) | | | | NS |
|
Yes | 1 (0.3) | 0 (0.0) | 1 (0.4) | |
|
No | 377 (99.7) | 108 (100.0) | 269 (99.6) | |
| Persistent pain, n
(%) | | | | 0.001 |
|
Yes | 55 (14.6) | 6 (5.6) | 49 (18.1) | |
|
No | 323 (85.4) | 102 (94.4) | 221 (81.9) | |
| Knee instability, n
(%) | | | | 0.020 |
|
Yes | 24 (6.3) | 2 (1.9) | 22 (8.1) | |
|
No | 354 (93.7) | 106 (98.1) | 248 (91.9) | |
Discussion
The optimal timing for ACL reconstruction remains a
topic of ongoing debate, with recent high-quality systematic
reviews and meta-analyses yielding conflicting results regarding
the impact of early vs. delayed intervention on comprehensive
patient outcomes. In the present study, a cohort of 378 patients
was analyzed, with 108 undergoing early ACLR and 270 receiving
delayed surgery. Notably, the delayed group demonstrated a
significantly higher proportion of male patients and an older
median age, which may reflect the demographic profile commonly
observed in large cohorts of ACL-deficient patients seeking care at
tertiary centers (2,10). Heavy manual labor was the most
common occupation in both groups, and the majority of patients had
attained higher education, suggesting that socioeconomic factors
did not significantly influence the timing of surgery in this
population. Urban vs. rural residency also did not differ between
groups, indicating that access to care may not have been a major
determinant of surgical timing (11).
Herein, sports-related injury mechanisms accounted
for the majority of ACL ruptures in both groups, consistent with
epidemiological data identifying sports participation as the
leading cause of ACL injury in young, active populations.
Specifically, non-contact mechanisms account for ~70% of ACL
injuries, typically occurring during pivoting, cutting, or landing
maneuvers that generate combined rotational and translational
forces. This injury pattern was reflected in the cohort in the
present study and aligns with broader epidemiological trends
demonstrating ACL injury rates of 6.5 per 100,000 athlete exposures
in high school sports, with competition carrying a 7-fold higher
risk than practice (12,13).
A significantly higher proportion of patients in the
delayed ACLR group underwent pre-operative rehabilitation, and the
duration of this rehabilitation was longer compared to the early
ACLR group. This practice reflects current evidence-based
recommendations to optimize knee function, reduce effusion and
restore range of motion prior to surgery, although recent evidence
suggests that the benefits of pre-operative rehabilitation may be
limited in certain populations (2,14). A
recent systematic review demonstrated that structured
prehabilitation programs, incorporating quadriceps strengthening,
range of motion exercises and neuromuscular training, provide
measurable benefits in post-operative recovery (15). However, the optimal duration and
intensity of prehabilitation remain subjects of ongoing
investigation, with programs ranging from 4-6 weeks demonstrating
the most consistent benefits (15). In the present study, post-operative
rehabilitation was almost universal in both groups with no
significant difference in participation or duration, reflecting the
widespread adoption of accelerated rehabilitation protocols in
modern ACLR (16).
Functional outcomes, as assessed using the LKS,
revealed a marked advantage for the early ACLR group, with 81.5%
achieving excellent results compared to 41.5% in the delayed ACLR
group. This finding appears to be in contrast to the most recent
and comprehensive meta-analysis by Shen et al (2), which analyzed 11 randomized
controlled trials involving 972 participants and found no
significant differences in the majority of functional outcomes
between early and delayed ACLR. However, their analysis did
identify small, yet statistically significant advantages for early
reconstruction in IKDC scores (mean difference, 2.77 points) and
2-year Lysholm scores (mean difference, 2.61 points) (2). The magnitude of difference observed
in the present study exceeds these meta-analytic findings,
potentially reflecting the influence of confounding variables
inherent in retrospective cohort designs or differences in patient
populations and rehabilitation protocols. Other studies have
reported that early reconstruction may be associated with improved
knee function and movement ability at short-term follow-up,
particularly in highly active patients (14).
Contemporary evidence regarding functional outcomes
demonstrates considerable variability across studies, largely
attributable to heterogeneous definitions of ‘early’ and ‘delayed’
timing, ranging from 2 days to 7 months for early reconstruction
and 3 weeks to several years for delayed procedures. This
definitional inconsistency complicates direct comparisons between
studies and contributes to ongoing clinical uncertainty. Recent
investigations have attempted to establish more precise timing
thresholds, with some evidence suggesting that reconstruction
performed within 3-5 months of injury may optimize outcomes while
minimizing complications (17,18).
In the present study, the KSS for range of motion
indicated that most patients achieved excellent or good results,
with no significant difference between the groups. This is
consistent with the findings of recent systematic reviews, which
found no significant difference in the objective measures of knee
motion or stability between early and delayed reconstruction
(2,14). The TAS revealed that a higher
percentage of patients in the early ACLR group achieved excellent
activity levels with a borderline significant difference. This
suggests that early intervention may facilitate a more rapid return
to pre-injury activity, although the evidence from randomized
trials remains equivocal (2,14).
Return-to-sport outcomes are critical indicators of
the success of ACLR, particularly among athletic populations.
Successful return to sport is influenced, not only by biomechanical
recovery, but also by psychological readiness, self-efficacy and
knee-related quality of life. Previous studies have demonstrated
that patients who achieve a return to their pre-injury activity
levels report significantly higher satisfaction rates and improved
quality of life measures (19,20).
In the present study, the median duration for return to daily
activities was 5 weeks (QR, 4-9 weeks), with no significant
difference observed between the early and delayed reconstruction
groups (7.0, 2.0-9.0 weeks for the early group vs. 6.0, 2.0-9.0
weeks for the delayed group).
Complication rates were generally low in both
groups, with no significant difference in infection or re-tear
rates. This finding is supported by recent meta-analyses, which
found no significant difference in the rates of these complications
between early and delayed ACL reconstruction (2,21).
However, knee stiffness and persistent pain were significantly more
common in the delayed ACLR group, echoing findings from
observational studies that have reported higher rates of
arthrofibrosis and persistent symptoms in patients with prolonged
preoperative intervals (11). In
the present study, there was no significant difference in infection
rates between the early and delayed ACL reconstruction groups. The
initially reported infection rate of 67 out of 378 cases included
all postoperative inflammatory events, such as superficial wound
erythema and minor serous discharge, which were conservatively
managed with oral antibiotics, rather than only confirmed deep
joint infections. Upon reclassification, only 3 cases (0.8%) met
the criteria for deep surgical-site infection, which is consistent
with the globally reported incidence range of 0.4-1.4%, as
documented in recent meta-analyses (22).
Recent studies have also highlighted the risk of
secondary intra-articular pathology with delayed ACLR. For example,
a previous prospective observational study found that the odds of
chondral injury increased significantly with a longer time since
the original injury, while meniscal injuries were less predictable
but still tended to increase over time (11). Another study reported that the risk
of concomitant intra-articular pathology, particularly chondral
injuries, increased linearly with a longer time to surgery
(23). This suggests that while
early reconstruction may not always result in improved functional
outcomes, it may help to reduce the risk of additional joint
damage.
The optimal window for ACLR with respect to muscle
atrophy has been suggested to lie between 21 and 100 days following
injury, as delaying surgery beyond this period may increase the
risk of quadriceps atrophy and impair early rehabilitation
(14). This is consistent with the
findings of the present study, where increased stiffness and
persistent pain was found in the delayed group, which may be
related to prolonged immobilization or reduced muscle strength.
Several limitations should be considered in the
interpretation of the present study. First, its retrospective and
non-randomized nature introduces the potential for confounding
variables, such as differences in surgical technique, graft
selection, or associated injuries, which could influence outcomes
and make it difficult to establish causality between the timing of
ACLR and the clinical results. Second, all ACLRs were performed by
a single surgeon, which, while ensuring procedural consistency, may
limit the generalizability of the findings. The influence of the
experience of the surgeon on outcomes is acknowledged as a
potential source of bias and further studies are required to
consider including multiple surgeons to better account for this
variable. Finally, the lack of long-term follow-ups and the
comprehensive assessment of secondary intra-articular pathology,
such as meniscal or chondral injuries, may have resulted in an
incomplete understanding of the true impact of surgical timing on
knee health and function.
In conclusion, the present study demonstrates that
early ACLR (performed within 12 weeks post-injury) is associated
with superior functional outcomes, higher activity levels and
reduced rates of knee stiffness, persistent pain, and instability
compared to delayed surgery. Although delayed reconstruction allows
for longer pre-operative rehabilitation, it may increase the risk
of developing post-operative complications that adversely affect
recovery. These findings support early surgical intervention as a
strategy to optimize patient outcomes, particularly in younger,
active individuals. Individualized treatment decisions should
consider patient-specific factors such as age, activity demands,
and concomitant knee pathology to tailor the timing of ACLR for
optimal recovery.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors contributions
Both authors (BMR and YKB) contributed equally to
the conception and design of the study, as well as in data
collection and analysis, and in the writing of the manuscript. BMR
and YKB confirm the authenticity of the raw data. Both authors have
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Ethical approval was obtained from the Scientific
Committee of University of Raparin (Sulaymaniyah, Iraq; Reference
no. 2866/28-5-2023). Written informed consent was obtained from the
patients or the patients parents (in the case of patients who
were underage) for participation in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kaeding CC, Léger-St-Jean B and Magnussen
RA: Epidemiology and diagnosis of anterior cruciate ligament
injuries. Clin Sports Med. 36:1–8. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shen X, Liu T, Xu S, Chen B, Tang X, Xiao
J and Qin Y: Optimal timing of anterior cruciate ligament
reconstruction in patients with anterior cruciate ligament tear: A
systematic review and meta-analysis. JAMA Netw Open.
5(e2242742)2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Waldron K, Brown M, Calderon A and Feldman
M: Anterior cruciate ligament rehabilitation and return to sport:
How fast is too fast? Arthrosc Sports Med Rehabil. 4:e175–e179.
2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Herbst E, Hoser C, Gföller P, Hepperger C,
Abermann E, Neumayer K, Musahl V and Fink C: Impact of surgical
timing on the outcome of anterior cruciate ligament reconstruction.
Knee Surg Sports Traumatol Arthrosc. 25:569–577. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Anstey DE, Heyworth BE, Price MD and Gill
TJ: Effect of timing of ACL reconstruction in surgery and
development of meniscal and chondral lesions. Phys Sportsmed.
40:36–40. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Högberg J, Fridh E, Piussi R, Senorski RH,
Cristiani R, Samuelsson K, Thomeé R and Senorski EH: Delayed
anterior cruciate ligament reconstruction is associated with lower
odds of returning to preinjury physical activity level at 12 months
Follow-Up. Arthroscopy. 41:3401–3412.e4. 2025.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Thomas AC, Wojtys EM, Brandon C and
Palmieri-Smith RM: Muscle atrophy contributes to quadriceps
weakness after anterior cruciate ligament reconstruction. J Sci Med
Sport. 19:7–11. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Briggs KK, Kocher MS, Rodkey WG and
Steadman JR: Reliability, validity, and responsiveness of the
Lysholm knee score and Tegner activity scale for patients with
meniscal injury of the knee. J Bone Joint Surg Am. 88:698–705.
2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Scuderi GR, Bourne RB, Noble PC, Benjamin
JB, Lonner JH and Scott W: The new knee society knee scoring
system. Clin Orthop Relat Res. 470:3–19. 2011.
|
|
10
|
Migliorini F, Lucenti L, Mok YR, Bardazzi
T, D Ambrosi R, De Carli A, Paolicelli D and Maffulli N:
Anterior cruciate ligament reconstruction using lateral
Extra-articular procedures: A systematic review. Medicina (Kaunas).
61(294)2025.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Patra SK, Unnava N, Patro BP and Mohanty
S: Timing of anterior cruciate ligament reconstruction and its
effect on associated chondral damage and meniscal injury: A
prospective observational study. Int J Res Orthop. 9:770–775.
2023.
|
|
12
|
Joseph AM, Collins CL, Henke NM, Yard EE,
Fields SK and Comstock RD: A multisport epidemiologic comparison of
anterior cruciate ligament injuries in high school athletics. J
Athl Train. 48:810–817. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Montalvo AM, Schneider DK, Webster KE, Yut
L, Galloway MT, Heidt RS Jr, Kaeding CC, Kremcheck TE, Magnussen
RA, Parikh SN and Stanfield DT: Anterior cruciate ligament injury
risk in sport: A systematic review and meta-analysis of injury
incidence by sex and sport classification. J Athl Train.
54:472–482. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Widhalm HK, Draschl A, Horns J, Rilk S,
Leitgeb J, Hajdu S and Sadoghi P: The optimal window for
reconstruction of the anterior cruciate ligament (ACL) with respect
to quadriceps atrophies lies within 21 to 100 days. PLoS One.
19(e0296943)2024.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zakharia A, Zhang K, Al-Katanani F, Rathod
P, Uddandam A, Kay J, Murphy B, Ogborn D and de SAD:
Prehabilitation prior to anterior cruciate ligament reconstruction
is a safe and effective intervention for short-to long-term
benefits: A systematic review. Knee Surg Sports Traumatol Arthrosc.
33:4148–4166. 2025.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ricupito R, Grassi A, Mourad F, Di Filippo
L, Gobbo M and Maselli F: Anterior Cruciate Ligament Return to
Play:‘A Framework for Decision Making’. J Clin Med.
14(2146)2025.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Liu AF, Guo TC, Feng HC, Yu WJ, Chen JX
and Zhai JB: Efficacy and safety of early versus delayed
reconstruction for anterior cruciate ligament injuries: A
systematic review and meta-analysis. Knee. 44:43–58.
2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zsidai B, Kaarre J, Narup E and Samuelsson
K: Timing of anterior cruciate ligament surgery. Clin Sports Med.
43:331–341. 2024.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Battaglia M, Arner JW, Midtgaard KS, Haber
DB, Peebles LA, Peebles AM, Ganokroj P, Whalen RJ, Provencher MT,
Torre G and Ciatti R: Early versus standard return to play
following ACL reconstruction: Impact on volume of play and career
longevity in 180 professional European soccer players: A
retrospective cohort study. J Orthop Traumatol.
26(29)2025.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Piussi R, Simonson R, Zsidai B, Grassi A,
Karlsson J, Della Villa F, Samuelsson K and Senorski EH: Better
safe than sorry? A systematic review with meta-analysis on time to
return to sport after ACL reconstruction as a risk factor for
second ACL injury. J Orthop Sports Phys Ther. 54:161–175.
2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lee YS, Lee OS, Lee SH and Hui TS: Effect
of the timing of anterior cruciate ligament reconstruction on
clinical and stability outcomes: A systematic review and
Meta-analysis. Arthroscopy. 34:592–602. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Cassano GD, Moretti L, Vicenti G, Buono C,
Albano F, Ladogana T, Rausa I, Notarnicola A and Solarino G:
Infection after anterior cruciate ligament reconstruction: A
narrative review of the literature. Healthcare (Basel).
12(894)2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Phillips T, Ronna B, Terner Z, Cushing T,
Goldenberg N and Shybut T: After 40 days intra-articular injury,
risk profile increases linearly with time to surgery in adolescent
patients undergoing primary anterior cruciate ligament
reconstruction. Knee Surg Sports Traumatol Arthrosc. 33:1192–1201.
2025.PubMed/NCBI View Article : Google Scholar
|