Introduction
Cholelithiasis remains a highly prevalent condition,
accounting for ~1 million hospitalizations and >700,000 surgical
procedures annually in the USA (1,2).
Choledocholithiasis, characterized by the presence of gallstones
within the common bile duct (CBD), is observed in 10 to 18% of
patients with cholelithiasis, with almost one-quarter of these
individuals experiencing disease-related complications including
acute cholangitis, biliary pancreatitis, obstructive jaundice
(2,3). The reported prevalence of
choledocholithiasis varies considerably depending on geographic
region and study methodology, ranging from 4% to ~12% in European
populations (4), 1 to 20.9% in
South American cohorts (5) and 1
to 15% among patients with gallstones in the USA (6). Although choledocholithiasis is not
inherently life-threatening, it significantly diminishes the
quality of life of patients, typically manifesting with pain and
biliary obstruction. Moreover, if left untreated, it may lead to
severe complications, such as acute cholangitis, resulting from
bacterial biofilm formation and potentially progressing to
life-threatening sepsis, as well as gallstone pancreatitis
secondary to distal CBD obstruction at the level of the
pancreaticobiliary junction (7).
The primary approach for the management of
choledocholithiasis involves the surgical or endoscopic extraction
of stones from the common bile duct. The conventional strategy
typically comprises two distinct procedures: Endoscopic retrograde
cholangiography (ERC) with sphincterotomy for stone removal from
the common bile duct (first stage), followed by laparoscopic
cholecystectomy (LC) for the treatment of cholecystolithiasis as a
second stage (8,9). It has been proposed that laparoscopic
cholecystectomy should be performed promptly after the first stage;
however, the optimal timing between these interventions remains a
subject of discussion (6,10,11).
Although this two-stage strategy consisting of
endoscopic stone extraction (ERC with sphincterotomy) followed by
laparoscopic cholecystectomy remains the most widely employed
approach for the management of cholecysto-choledocholithiasis, it
is associated with substantial complications, the majority of which
are related to the endoscopic intervention. The most common of
these is post-endoscopic retrograde cholangiopancreatography (ERCP)
pancreatitis (PEP) (12), which is
associated with prolonged hospitalization and increased healthcare
costs. Reported rates of PEP vary between 2 and 15%, with severe
pancreatitis occurring in 0.3 to 0.8% of cases and a mortality rate
of ~0.2% (12,13). Identified risk factors for PEP
include operator-, patient- and procedure-related elements, such as
the experience of the endoscopist, a history of recurrent or prior
ERCP-induced pancreatitis, difficult biliary cannulation,
inadvertent pancreatic duct cannulation or contrast injection and
pancreatic sphincterotomy (14).
The primary pathophysiological mechanisms implicated in PEP are
mechanical and hydrostatic injuries. Moreover, individual patient
characteristics, multiple cannulation attempts and
procedure-specific factors further increase the risk; thus,
comprehensive risk assessment is essential for minimizing the
occurrence of this complication (15). Following the endoscopic clearance
of CBD stones, LC should be performed following appropriate patient
recovery (16). However, as these
represent two separate procedures with distinct timelines, they
result in two hospitalizations with prolonged rehabilitation and
increased stress for the patient, as well as an increased financial
burden, typically borne by the patient (16).
The laparo-endoscopic rendezvous (LERV) technique is
a single-stage approach that combines LC with intraoperative
endoscopic stone extraction, providing the potential to reduce
complication rates, shorten periods of hospitalization and decrease
overall healthcare costs. First introduced toward the end of the
20th century (17), LERV has been
proposed as a favorable alternative to the conventional two-stage
strategy of preoperative endoscopic intervention followed by LC.
Several advantages have been attributed to LERV, including a
reduced overall morbidity and shorter periods of hospitalization
(18). Additional benefits include
diminished patient stress, decreased surgical expenses (11,19),
the convenience of a single hospital admission and a single
anesthesia exposure. Moreover, compared with the traditional
endoscopic-first approach, LERV may reduce the risk of inadvertent
contrast injection into the pancreatic duct, thereby lowering the
incidence of post-ERCP pancreatitis (20). Nevertheless, limitations of the
LERV technique include prolonged operative times and the
requirement for specialized expertise and close coordination
between the laparoscopic surgeon and the endoscopist (18,20).
The present study aimed to assess the safety and
efficacy of the single-stage LERV technique in the management of
cholecysto-choledocholithiasis. The findings are discussed in light
of outcomes reported in large-scale studies.
Patients and methods
Study design and patient
selection
A retrospective review of medical records was
conducted from patients who underwent the LERV procedure at Innova
Medical Center, Tbilisi, Georgia, between May, 2018 and February,
2025. This technique has been established as standard clinical
practice since 2018, and all patients diagnosed with
cholecysto-choledocholithiasis have been managed using the LERV
approach. Data extraction and collection from medical records were
conducted between March 10 and April 26, 2025. The study included
80 consecutive patients who underwent either elective or urgent
LERV based on clinical indications and individualized treatment
decisions. The study cohort comprised 28 male and 52 female
patients, with ages ranging from 12 to 87 years (median age, 51.5
years). Patient hospitalization, diagnosis and all procedures were
carried out at Innova Medical Center. The diagnosis of
cholecysto-choledocholithiasis was established based on clinical
presentation and imaging findings, including abdominal ultrasound,
computed tomography, magnetic resonance cholangiopancreatography
(MRCP), or intraoperative trans-cystic cholangiography (the latter
was used in 3 cases with moderate predictors of common bile duct
stones that were not visualized on preoperative ultrasound and
where MRCP could not be performed). All procedures were performed
by the surgical team, led by L.K., a surgeon with 16 years of
laparoscopic surgical experience and 14 years of endoscopic
practice, and O.K., with 43 years of surgical experience and 40
years of endoscopic practice. The study was approved by the Ethics
Committee of the Innova Medical Center (Approval no. 239, issued on
March 3, 2025).
Surgical technique
Standard laparoscopic techniques were used to
dissect and mobilize the cystic duct. A small incision was made in
the cystic duct to facilitate catheter insertion for intraoperative
cholangiography. A standard endoscopic guidewire was advanced
through the catheter into the duodenum, visualized endoscopically
and retrieved through the working channel of the duodenoscope.
Under guidewire assistance, direct biliary cannulation and
sphincterotomy were performed. The CBD stone(s) were extracted
using a Dormia basket and/or stone extraction balloon. Following
duct clearance, the endoscope was withdrawn and laparoscopic
cholecystectomy was completed.
Study endpoints
The primary endpoint of the present study was the
efficacy of the LERV procedure in achieving complete CBD stone
clearance. Secondary endpoints included morbidity, mortality,
operative time and the duration of hospitalization. Complications
were categorized as intraoperative, early post-operative (within 30
days), or late post-operative (beyond 30 days). The mean follow-up
duration was 32.8 months. The severity of complications was
classified according to the Dindo-Clavien classification system for
surgical complications (21).
Statistical analysis
Statistical analyses and graphical presentations
were performed using GraphPad Prism 5 (Dotmatics). Data
distribution was assessed using the Shapiro-Wilk normality test.
Continuous variables are presented as median and interquartile
range (IQR) apart from the event when only the range is available.
Differences between groups were analyzed using the non-parametric
Mann-Whitney U test. A value of P<0.05 was considered to
indicate a statistically significant difference.
Results
Patients and outcomes
A total of 80 patients diagnosed with
cholecysto-choledocholithiasis underwent treatment during the study
period. The demographic and clinical characteristics of the study
population are summarized in Table
I. The LERV procedure was successfully performed in 79 patients
(98.7%) with no conversions to open surgery (0%). The initial
success rate was achieved in 97.5% (77 patients out of 79
successful LERV). The mean follow-up was 32.8 months.
 | Table IPatient demographics and outcomes. |
Table I
Patient demographics and outcomes.
| Metric | Value |
|---|
| Male patients | 28 (35%) |
| Female patients | 52 (65%) |
| Age, years; median
(range) | 51.5 (12-87) |
| Elective surgery | 44 (55.0%) |
| Urgent surgery | 36 (45.0%) |
| Operation time, min;
median (range) | 115 (55-310) |
| Duration of
hospitalization, days; median (range) | 3 (1-24) |
| History of
pancreatitis (prior to LERV) | 10 (12.5%) |
| Complications
following LERV | 7 (8.8%) |
| Successful
cannulation | 79 (98.7%) |
| Successful clearance
of CBD stones | 77 (97.5%) |
| CBD
exploration/choledochotomy or conversion to open surgery | 0 |
Of the patients, 44 (55%) patients underwent
elective procedures, and 36 (45%) patients underwent urgent
interventions. Successful laparoscopic antegrade trans-cystic
cannulation of the CBD with a cholangiography catheter was achieved
in 79 patients (98.7%). In 1 case (1.3%), catheterization was not
feasible due to complete cystic duct obstruction caused by severe
inflammation. In this instance, a standard endoscopic intervention
was performed under the same anesthesia following laparoscopic
cholecystectomy, without any complications.
A total of 6 patients (7.5%) had a history of
bariatric surgery, and 5 patients (6.3%) were pediatric cases. In
total, 10 patients (12.5%) presented with a pre-existing history of
biliary pancreatitis, including 2 cases of mild biliary
pancreatitis at the time of hospitalization.
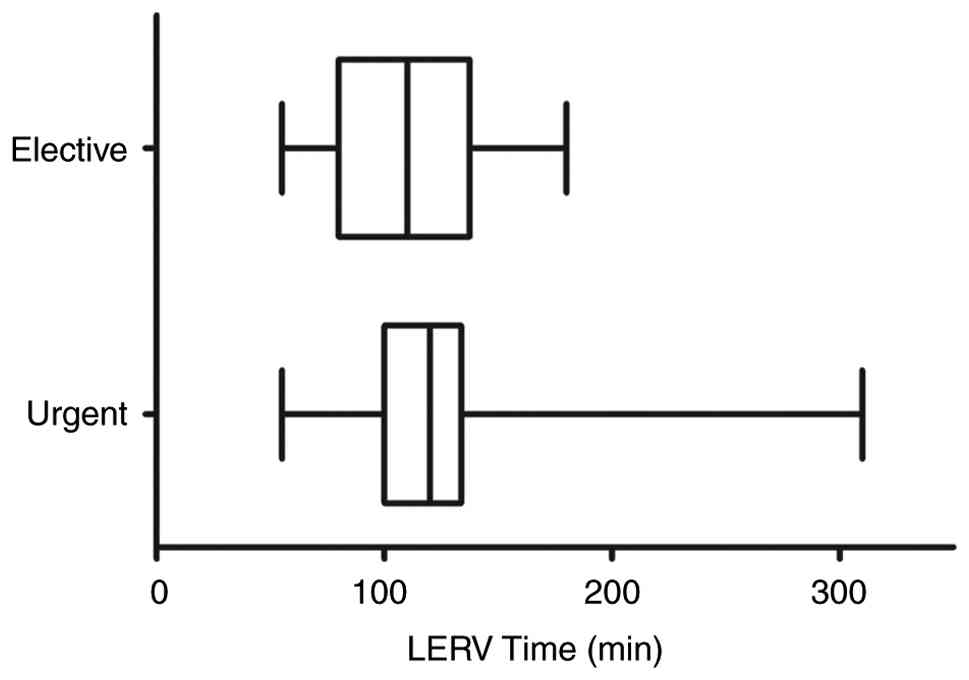
The median operative time across the cohort was 115
min (range, 55-310 min), with a mean of 118.9 min (± standard
deviation, 42.5 min), reflecting variability based on procedure
complexity. The association between urgent/elective intervention
and operative time is depicted in Fig.
1. Operation times in the urgent group (n=36) were
significantly more variable and exhibited a non-normal distribution
(P<0.001), whereas the elective group (n=44) did not deviate
from normality (P=0.068). The median operation time was 120 min
(IQR, 100-134 min) for the urgent cases and 110 min (IQR, 80-137
min) for the elective cases. Comparisons between the groups
revealed no statistically significant difference (P=0.139)
(Fig. 1). The median duration of
hospitalization was 3 days (range, 1-24 days) (Table I).
No mortality was observed. A total of 7 patients
(8.8%) developed post-operative complications, which were
classified according to the Dindo-Clavien system (21) and are presented in Table II. Among these, 5 patients
experienced acute pancreatitis. Notably, 2 of these 5 patients had
a prior history of pancreatitis. The remaining 2 patients had
complications related to residual CBD stones; the majority of
post-operative complications were mild, with 71.4% graded as
Dindo-Clavien Grade I or II.
 | Table IIComplications graded according to the
modified Dindo-Clavien classification (21). |
Table II
Complications graded according to the
modified Dindo-Clavien classification (21).
|
Complication/condition | No. (%) | Grade I-II | Grade III |
|---|
| Post-LERV
pancreatitis | 5 (6.3) | 5 | - |
| Residual CBD
stones | 2 (2.5) | - | 2 |
| Total | 7 (8.8) | | |
Post-LERV additional
interventions
Additional interventions were required in 2 cases
due to residual CBD stones. Of note, 1 patient underwent the
successful endoscopic extraction of residual stones, while another
patient required a repeat LERV due to biliary hyperpressure caused
by a residual CBD stone, clip dislodgement from the cystic duct,
and biliary leakage. Of note, both cases occurred during the early
learning curve of the surgical team (i.e., within the first 15
procedures) and involved particularly complex choledocholithiasis
(characterized by multiple common bile duct stones of varying sizes
and morphologies).
Discussion
The present retrospective study evaluated the
outcomes of the LERV technique in 80 patients with
cholecysto-choledocholithiasis, achieving a high initial success
rate (97.5%) with no conversions to open surgery. The findings
confirm that LERV is a highly effective and safe single-stage
approach for the simultaneous management of gallbladder and CBD
stones. The low morbidity rate (8.8%) and absence of mortality in
the present study cohort align with the results reported in other
large-scale studies (20,22), supporting the utility of the LERV
procedure as a viable alternative to the traditional two-stage
strategy. Additionally, the majority of post-operative
complications were mild (Dindo-Clavien Grade I-II), and the need
for additional interventions was limited to early cases, likely
reflecting the impact of the learning curve on initial
outcomes.
In the present study cohort, the initial success
rate of LERV was 97.5%, with no conversions to open surgery. This
aligns favorably with the results reported in the study by La Barba
et al (20), who described
a success rate of 95% and a 3% conversion rate in their large
series involving 200 patients. The overall post-procedural
complication rate in the present study was 8.8%, aligning with the
9% reported in the study by La Barba et al (20) and lower than the 14.5% observed in
the study by Qian et al (22). Notably, in the present case series,
post-procedural pancreatitis occurred in 6.3% of patients, slightly
higher than the 2.4-3% typically reported for LERV in large series,
yet still favorable compared to the higher rates associated with
the traditional two-stage approach (8-10%) (20,22).
In the present study, the median operative time (115 min) was more
or less similar to that of other studies [La Barba et al
(20), 120 min; Qian et al
(22), ~140 min], reflecting the
technical complexity and experience-gaining phase of LERV.
Additionally, the average period of hospitalization of 3 days
(range, 1-24 days) in the present case series was in line with the
previous research (4-5 days) (20), yet considerably shorter than the
prolonged stays associated with two-stage approaches, and
consistent with the trend toward faster recovery reported in prior
studies (22). These findings
further reinforce LERV as a safe, efficient, and
complication-sparing approach for managing
cholecysto-choledocholithiasis, particularly when considering the
long-term reduction of biliary complications noted in one-stage
strategies.
It should be mentioned that in the present study
cohort, the LERV technique was successfully applied in specific
challenging clinical scenarios, including patients with a history
of bariatric surgery, pediatric patients, and those with
periampullary diverticulum (PAD), providing insight into its
applicability and technical advantages in anatomically and
clinically complex situations. In patients with a history of
bariatric surgery, particularly Roux-en-Y gastric bypass,
conventional ERCP often poses substantial technical challenges.
Accessing the papilla typically requires a transgastric approach
assisted by laparoscopy, and the altered anatomy results in a
tangential view of the papilla with the patient in a supine
position, making cannulation highly complex. In such cases, LERV
can simplify biliary access by providing antegrade guidewire
passage, facilitating easier cannulation. This is consistent with
the findings of the study by Voermans et al (23), who demonstrated the feasibility,
but recognized the technical difficulties of laparoscopic-assisted
ERCP in post-bariatric patients. Similarly, anatomical variations,
such as PAD or atypical papillary morphology [e.g., type 2 or
3/small or protruding papillae, as described by Chen et al
(24)] can hinder successful
cannulation during conventional ERCP. In the present study cohort,
3 patients with PAD underwent successful biliary access using the
LERV technique without the need for advanced cannulation maneuvers.
The guidewire-assisted method thus provides a safer and more
predictable approach in the presence of anatomical abnormalities.
Furthermore, pediatric patients may particularly benefit from LERV.
The rarity of choledocholithiasis in the pediatric population
limits the experience of pediatric endoscopists with standard ERCP,
increasing the risk of failed cannulation or post-ERCP
complications (25). By allowing
controlled antegrade guidewire passage, LERV enhances procedural
safety and reduces the technical burden in this vulnerable group.
Taken together, these observations suggest that LERV is not only an
effective alternative, but may be the preferred first-line strategy
in selected high-risk populations, warranting further prospective
validation.
Despite its advantages, the LERV technique is
associated with several limitations that should be considered. One
of the primary challenges lies in the organizational and logistical
requirements: Successful LERV demands close coordination between an
experienced laparoscopic surgeon and a skilled endoscopist, both
available simultaneously during the procedure. In centers where
surgical and endoscopic expertise are compartmentalized or
scheduling resources are constrained, implementing LERV may prove
difficult. Furthermore, the learning curve for mastering LERV may
be significant, necessitating additional training and experience
for both teams to ensure procedural safety and efficiency. In
addition, several methodological constraints should be
acknowledged. The present study was a retrospective, single-center
study performed under the supervision of a single surgical
leadership, which may limit the generalizability of the findings to
other clinical settings or surgical teams with varying levels of
expertise. Moreover, although the sample size of 80 consecutive
patients is adequate for a focused institutional experience, it may
lack the statistical power to detect less frequent adverse events
in specific patient subgroups.
In conclusion, the findings of the present study
demonstrate that the LERV technique is a safe, effective and
efficient single-stage approach for the management of
cholecysto-choledocholithiasis, achieving high success rates with
low morbidity. LERV proved particularly beneficial in complex
scenarios, such as pediatric patients, post-bariatric surgery cases
and patients with anatomical abnormalities, such as PAD. While the
technique requires substantial coordination, expertise and
logistical support, its advantages over conventional two-stage
approaches are increasingly evident and support its broader
adoption in clinical practice.
Acknowledgements
The authors would like to thank Dr Thierry Berney
and Dr David Otiashvili, School of Medicine, Ilia State University,
Tbilisi, Georgia, for their valuable feedback and thorough review
of the manuscript.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study are not
publicly available due to patient confidentiality but can be
provided in an anonymized form by the corresponding author upon
reasonable request.
Authors' contributions
All authors (LK, OK, DA, LM, SG and IA) contributed
to the conception and design of the study. LK, OK, DA and SG
conducted patient management and performed all clinical
manipulations. Data collection and analysis were performed by LK,
IA and LM. The first draft of the manuscript was written by LK, and
all authors commented on previous versions and approved the final
manuscript. IA and LK confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Innova Medical Center, Tbilisi, Georgia (Approval no. 239,
issued on March 3, 2025). The requirement for informed consent was
waived due to the retrospective design of the study. However,
consent had been obtained from all patients and parents of the
under-age patients prior to performing the surgeries.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, AI tools were
used to improve the readability and language of the manuscript or
to generate images, and subsequently, the authors revised and
edited the content produced by the AI tools as necessary, taking
full responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Gallaher JR and Charles A: Acute
cholecystitis: A review. JAMA. 327:965–975. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ding YB, Deng B, Liu XN, Wu J, Xiao WM,
Wang YZ, Ma JM, Li Q and Ju ZS: Synchronous vs sequential
laparoscopic cholecystectomy for cholecystocholedocholithiasis.
World J Gastroenterol. 19:2080–2086. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Salman B, Yilmaz U, Kerem M, Bedirli A,
Sare M, Sakrak O and Tatlicioglu E: The timing of laparoscopic
cholecystectomy after endoscopic retrograde
cholangiopancreaticography in cholelithiasis coexisting with
choledocholithiasis. J Hepatobiliary Pancreat Surg. 16:832–836.
2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Manes G, Paspatis G, Aabakken L, Anderloni
A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM,
Gigot JF, et al: Endoscopic management of common bile duct stones:
European society of gastrointestinal endoscopy (ESGE) guideline.
Endoscopy. 51:472–491. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Csendes A, Burdiles P, Diaz JC, Maluenda
F, Korn O, Vallejo E and Csendes P: Prevalence of common bile duct
stones according to the increasing number of risk factors present.
A prospective study employing routinely intraoperative
cholangiography in 477 cases. Hepatogastroenterology. 45:1415–1421.
1998.PubMed/NCBI
|
|
6
|
McNicoll CF, Pastorino A, Farooq U,
Froehlich MJ and St Hill CR: Choledocholithiasis. In: StatPearls
[Internet]. StatPearls Publishing, Treasure Island, FL, 2025.
|
|
7
|
Wilkins T, Agabin E, Varghese J and
Talukder A: Gallbladder dysfunction: Cholecystitis,
choledocholithiasis, cholangitis, and biliary dyskinesia. Prim
Care. 44:575–597. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Schiphorst AH, Besselink MG, Boerma D,
Timmer R, Wiezer MJ, van Erpecum KJ, Broeders IA and van Ramshorst
B: Timing of cholecystectomy after endoscopic sphincterotomy for
common bile duct stones. Surg Endosc. 22:2046–2050. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li VKM, Yum JLK and Yeung YP: Optimal
timing of elective laparoscopic cholecystectomy after acute
cholangitis and subsequent clearance of choledocholithiasis. Am J
Surg. 200:483–488. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Reinders JS, Gouma DJ, Heisterkamp J,
Tromp E, van Ramshorst B and Boerma D: Laparoscopic cholecystectomy
is more difficult after a previous endoscopic retrograde
cholangiography. HPB (Oxford). 15:230–234. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kostro J, Marek I, Pęksa R, Łaski D,
Hellmann AR, Kobiela J, Hać S, Pieńkowska J, Adrych K and
Śledziński Z: Cholecystectomy after endoscopic retrograde
cholangiopancreatography-effect of time on treatment outcomes. Prz
Gastroenterol. 13:251–257. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pekgoz M: Post-endoscopic retrograde
cholangiopancreatography pancreatitis: A systematic review for
prevention and treatment. World J Gastroenterol. 25:4019–4042.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Akshintala VS, Kanthasamy K, Bhullar FA,
Sperna Weiland CJ, Kamal A, Kochar B, Gurakar M, Ngamruengphong S,
Kumbhari V, Brewer-Gutierrez OI, et al: Incidence, severity, and
mortality of post-ERCP pancreatitis: An updated systematic review
and meta-analysis of 145 randomized controlled trials. Gastrointest
Endosc. 98:1–6.e12. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Barkin JS, Casal GL, Reiner DK, Goldberg
RI, Phillips RS and Kaplan S: A comparative study of contrast
agents for endoscopic retrograde pancreatography. Am J
Gastroenterol. 86:1437–1441. 1991.PubMed/NCBI
|
|
15
|
Kochar B, Akshintala VS, Afghani E,
Elmunzer BJ, Kim KJ, Lennon AM, Khashab MA, Kalloo AN and Singh VK:
Incidence, severity, and mortality of post-ERCP pancreatitis: A
systematic review by using randomized, controlled trials.
Gastrointest Endosc. 81:143–149.e9. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Enochsson L, Swahn F, Arnelo U, Nilsson M,
Löhr M and Persson G: Nationwide, population-based data from 11,074
ERCP procedures from the Swedish registry for gallstone surgery and
ERCP. Gastrointest Endosc. 72:1175–1184.e1-e3. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Deslandres E, Gagner M, Pomp A, Rheault M,
Leduc R, Clermont R, Gratton J and Bernard EJ: Intraoperative
endoscopic sphincterotomy for common bile duct stones during
laparoscopic cholecystectomy. Gastrointest Endosc. 39:54–58.
1993.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lin Y, Su Y, Yan J and Li X:
Laparoendoscopic rendezvous versus ERCP followed by laparoscopic
cholecystectomy in the management of cholecystocholedocholithiasis:
A systemic review and meta-analysis. Surg Endosc. 34:4214–4224.
2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zang JF, Zhang C and Gao JY: Endoscopic
retrograde cholangiopancreatography and laparoscopic
cholecystectomy during the same session: Feasibility and safety.
World J Gastroenterol. 19:6093–6097. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
La Barba G, Gardini A, Cavargini E,
Casadei A, Morgagni P, Bazzocchi F, D'Acapito F, Cavaliere D, Curti
R, Tringali D, et al: Laparoendoscopic rendezvous in the treatment
of cholecysto-choledocholitiasis: A single series of 200 patients.
Surg Endosc. 32:3868–3873. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Qian Y, Xie J, Jiang P, Yin Y and Sun Q:
Laparoendoscopic rendezvous versus ERCP followed by laparoscopic
cholecystectomy for the management of
cholecysto-choledocholithiasis: A retrospectively cohort study.
Surg Endosc. 34:2483–2489. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Voermans RP, Eisendrath P, Bruno MJ, Le
Moine O, Devière J and Fockens P: ARCADE group. Initial evaluation
of a novel prototype forward-viewing US endoscope in transmural
drainage of pancreatic pseudocysts (with videos). Gastrointest
Endosc. 66:1013–1017. 2007.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Chen PH, Tung CF, Peng YC, Yeh HZ, Chang
CS and Chen CC: Duodenal major papilla morphology can affect
biliary cannulation and complications during ERCP, an observational
study. BMC Gastroenterol. 20(310)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Perera KDR, Nawarathne NMM, Samarawickrama
VT, Deraniyagala MP, Luxman WGE and Fernandopulle ANR: Endoscopic
retrograde cholangiopancreatography in children: Feasibility,
success, and safety with standard adult endoscopes and accessories.
Pediatr Gastroenterol Hepatol Nutr. 25:406–412. 2022.PubMed/NCBI View Article : Google Scholar
|