Introduction
Lung ischemic-reperfusion (I/R) injury typically
occurs as a result of lung transplantation, pulmonary
thromboembolism resection, pulmonary embolism following
thrombolysis treatment and numerous other types of extracorporeal
circulation cardiac surgery; I/R is an early post-operative
complication, and an important cause of mortality (1). Lung transplantation is the last-resort
treatment option for patients with end-stage lung disease, but
following lung transplantation, the patient 1-year survival rate is
only ~70%; patients tend to succumb to post-operative mortality
within 30 days of surgery (2). Graft
failure following transplantation can cause lung I/R injury,
including injury to the pulmonary vascular endothelium, resulting
in marked lung damage (3).
The complex etiology of pulmonary vascular
dysfunction has not been fully elucidated; previous studies have
associated this disease with oxidative damage caused by oxygen free
radicals, calcium overload and neutrophil recruitment caused by
excessive inflammation. These physiological effects may produce a
greater number of oxygen free radicals than are removed, causing an
exacerbation of lung I/R injury (4).
A previous study associated hypoxia inducible factor-1α (HIF-1α)
and inducible nitric oxide synthase (iNOS) with pulmonary
hypertension; furthermore, structural damage to the pulmonary
vascular endothelium was also considered to be an initial
contributor to pulmonary vascular dysfunction (5).
Silymarin is an active element extracted from
Silybum marianum, by 4 isomers of the original ketone group
dihydrogen color, including Silybum marianum, has the main
pharmacological effects (6).
Silymarin can eliminate reactive oxygen species, protect against
lipid peroxidation, maintain cell membrane fluidity, protect liver
cell membranes and promote liver cell repair and regeneration,
which all contribute to combat liver fibrosis (7). The present study aimed to investigate
the effects of silymarin on pulmonary vascular dysfunction in a
lung I/R injury rat model and assess its underlying molecular
mechanism of action.
Materials and methods
Animals
All experimental procedures conformed to the Guide
for the Care and Use of Laboratory Animals (Shandong University,
Shandong, China) and were approved by the Institutional Ethics
Committee of Shandong University. Male Sprague Dawley (SD) rats
(180–220 g) were obtained from the Laboratory Animal Center of
Shandong University, and were housed in units maintained at
appropriate environmental conditions, with access to food and water
ad libitum.
Lung I/R injury
SD rats were administered 0.1 mg/kg/min of
pentobarbital by intraperitoneal injection. Following endotracheal
intubation, mechanical ventilation with 100% oxygen was applied,
with a tidal volume of 10 ml/kg (70 breaths/min). A midline
thoracotomy was performed under sterile conditions, the pericardium
was opened, and then the left pulmonary artery was ligated using an
8-0 prolene suture and was secured with polyethylene tubing without
damaging the vessel. After 1 h of ischemia, the left pulmonary
artery occlusion was cleared and the artery was reperfused with
blood. The chest cavity was then closed, and SD rats were restored
to normal respiration. Following 24 h of reperfusion, the rats were
sacrificed by decollation following anesthetization.
Experimental design
SD rats were randomly divided into 3 groups, as
follows: i) Control group rats (n=10), administered saline
solution; ii) I/R group rats (n=10), receiving the aforementioned
lung I/R injury and administered saline solution; iii) silymarin
group rats (n=10), receiving lung I/R injury and administered 250
mg/kg/day of silymarin (Sigma-Aldrich, St. Louis, MO, USA) for 8
days (8).
Vascular reactivity
Vascular reactivity was recorded with a myograph, as
previously described (9). Briefly,
the pulmonary arteries were dissected from the rats and the
connective tissue was removed. The pulmonary arteries and
surrounding endothelium were maintained in Krebs solution and a
myograph was used to estimate the tension in relation to internal
circumference. The functional integrity of the pulmonary artery
tissue segments was confirmed using 60 mmol/l KCl after 60 min of
stabilization. The endothelium function was evaluated by measuring
the relaxant response of segments that had been contracted with 1
µmol/l phenylephrine (Wuhan Xinxin beauty Biotechnology, Co., Ltd.,
Wuhan, China) to 1 µmol/l acetylcholine (Wuhan Dong Kangyuan
Technology, Co., Ltd., Wuhan, China).
Mass calculations
Lung tissue samples were weighed to calculate wet
mass; they were then placed in a drying oven at 80°C for 12–36 h
and the corresponding dry weight was also recorded. Lung moisture
was calculated as the wet/dry weight ratio.
Western blotting
Following treatment with silymarin, lung tissue
samples were homogenized with radioimmunoprecipitation assay lysis
buffer (Beyotime Institute of Biotechnology, Jiangsu, China). The
homogenized samples were centrifuged at 1,200 × g for 10 min at
4°C. The total protein in each supernatant was quantified using a
bicinchoninic acid assay (Beyotime Institute of Biotechnology).
Equal protein was separated by 10% sodium dodecyl
sulfate-polyacrylamide gel electrophoresis and transferred to
nitrocellulose membranes at 100 V for 1–2 h. The membranes were
blocked with phosphate-buffered saline containing 5% skimmed milk
powder for 1–2 h at room temperature to prevent non-specific
binding. The membranes were incubated with primary antibodies
against HIF-1α (1:1,000; C-19; Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA), iNOS (1:1,000; sc-49058; Santa Cruz
Biotechnology, Inc.) and β-actin (1:500; D110007; Sangon Biotech
Co. Ltd., Shanghai, China) overnight at 4°C. The membranes were
incubated with secondary antibodies (1:5,000, BestBio Inc,
Shanghai, China) for 2–3 h, then developed using chemiluminescence
detection (BestBio Inc.). Relative band density was measured using
Multi-Analyst software (Bio-Rad Laboratories, Inc., Hercules, CA,
USA).
Inflammatory cytokine levels
The supernatant from centrifuged, homogenized lung
tissue samples was acquired and the serum levels of nuclear
factor-κB (NF-κB), tumor necrosis factor-α (TNF-α), interleukin
(IL)-1β and IL-6 were analyzed using ELISA kits (KF008, R019 and
H002, respectively; Nanjing Jiancheng Bioengineering Institute,
Nanjing, China), according to the manufacturer's protocols.
Oxidative stress
The supernatant from centrifuged, homogenized lung
tissue samples was acquired and the serum superoxide dismutase
(SOD) and malondialdehyde (MDA) levels were analyzed using ELISA
kits (A001-3 and A003-1, respectively; Nanjing Jiancheng
Bioengineering Institute), according to the manufacturer's
protocols.
Caspase-9 and caspase-3 levels
The supernatant from centrifuged, homogenized lung
tissue samples was acquired and the total protein was quantified
using the bicinchoninic acid assay. Equal protein (30 µg) across
samples was incubated with reaction buffer (Ac-DEVD-pNA to detect
caspase-3 or Ac-LEHD-pNA to detect caspase-9) at 37°C for 2 h in
the dark, and caspase-3 and −9 levels were measured at an
absorbance of 405 nm.
Statistical analysis
Data are presented as the mean ± standard error of
the mean. Statistical analyses, including a one-way analysis of
variance with Student's t-test post-hoc analysis, were conducted
using SPSS 15.0 statistical software (SPSS, Inc., Chicago, IL,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
Silymarin improves I/R-induced
pulmonary vascular dysfunction
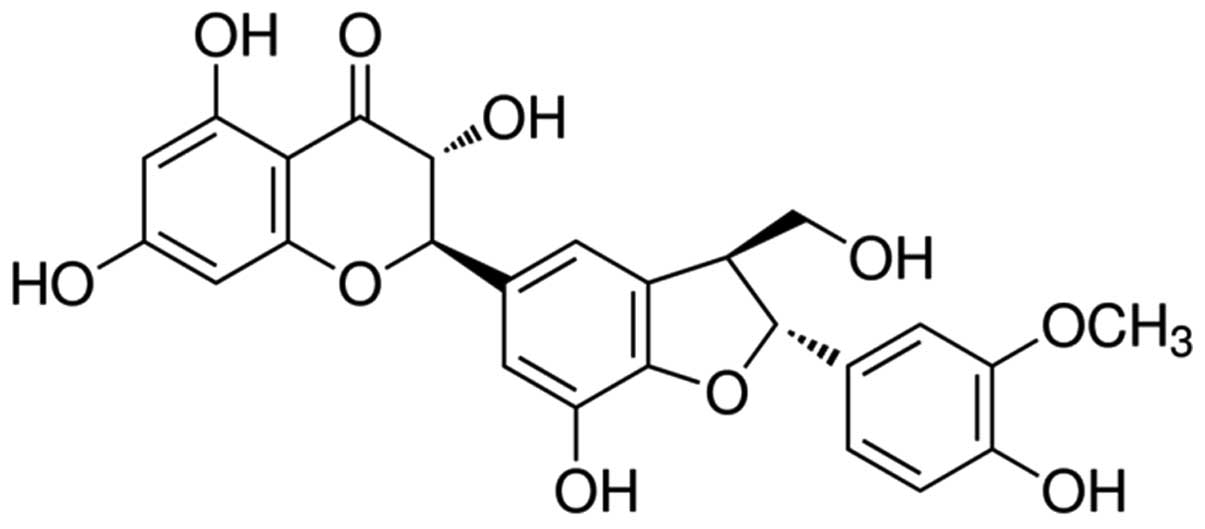
The chemical structure of silymarin is indicated in
Fig. 1 (Sigma-Aldrich Chemie Gmbh,
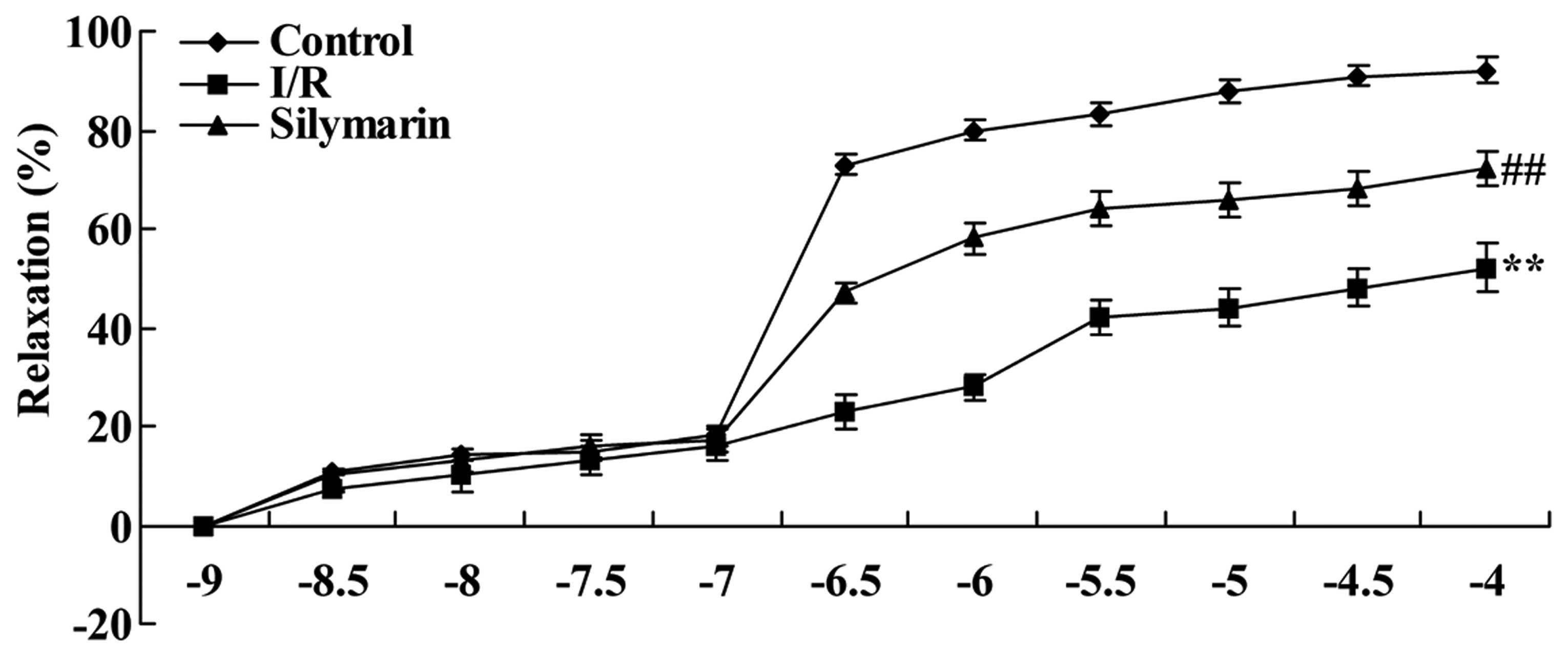
Munich, Germany). To determine whether silymarin affects lung
I/R-induced pulmonary vascular dysfunction in rats, vascular
reactivity was evaluated following reperfusion. Compared with the
control group, the relaxant response was effectively decreased in
lung I/R-injured rats (P<0.01; Fig.
2). However, treatment with silymarin improved the relaxant
response in lung I/R-injured rats, when compared with that of the
saline-treated lung I/R-injured group (P<0.01; Fig. 2).
Silymarin reduces I/R-induced lung
moisture
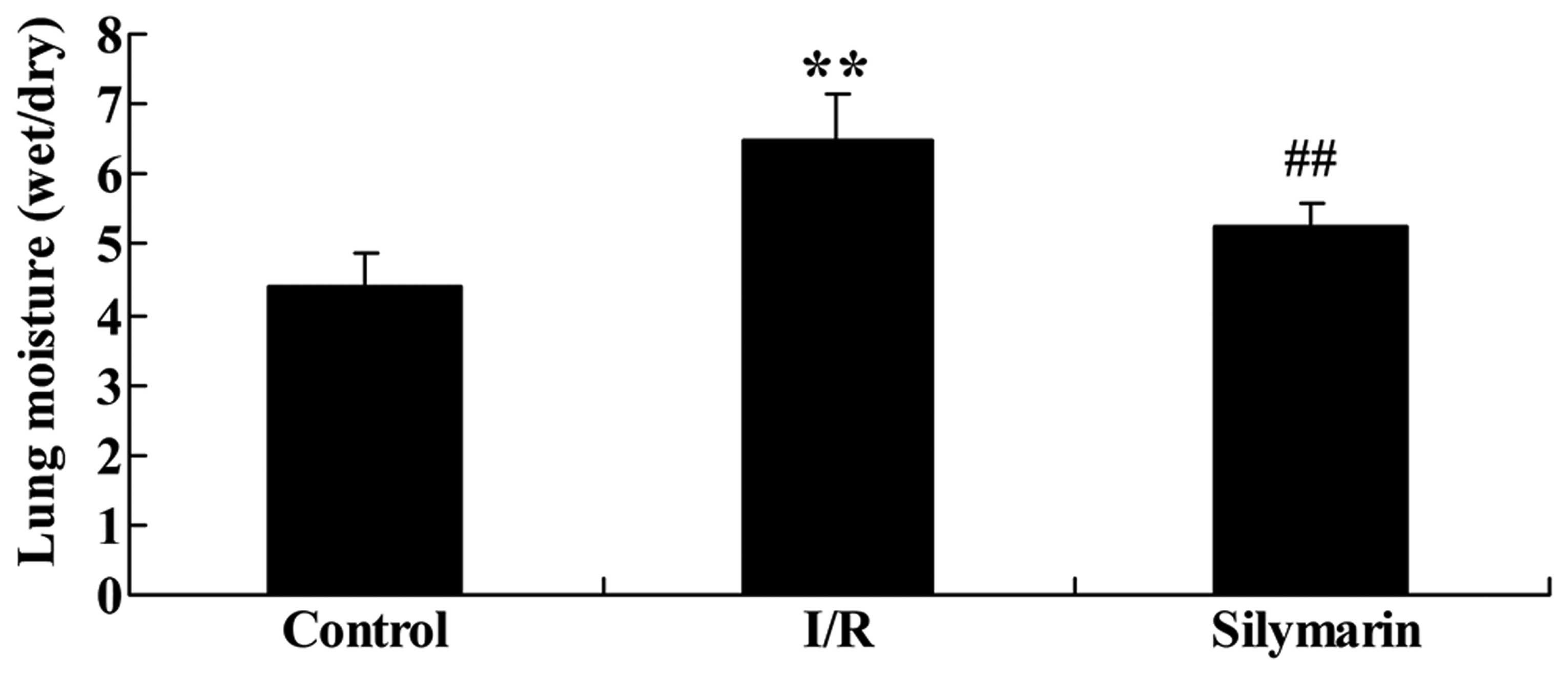
The effects of silymarin on lung moisture following
I/R injury were also evaluated. As indicated in Fig. 3, lung moisture was significantly
higher in the I/R-injured group than the control group (P<0.01),
but treatment with silymarin markedly reduced lung moisture
compared with the I/R-injured group (P<0.01).
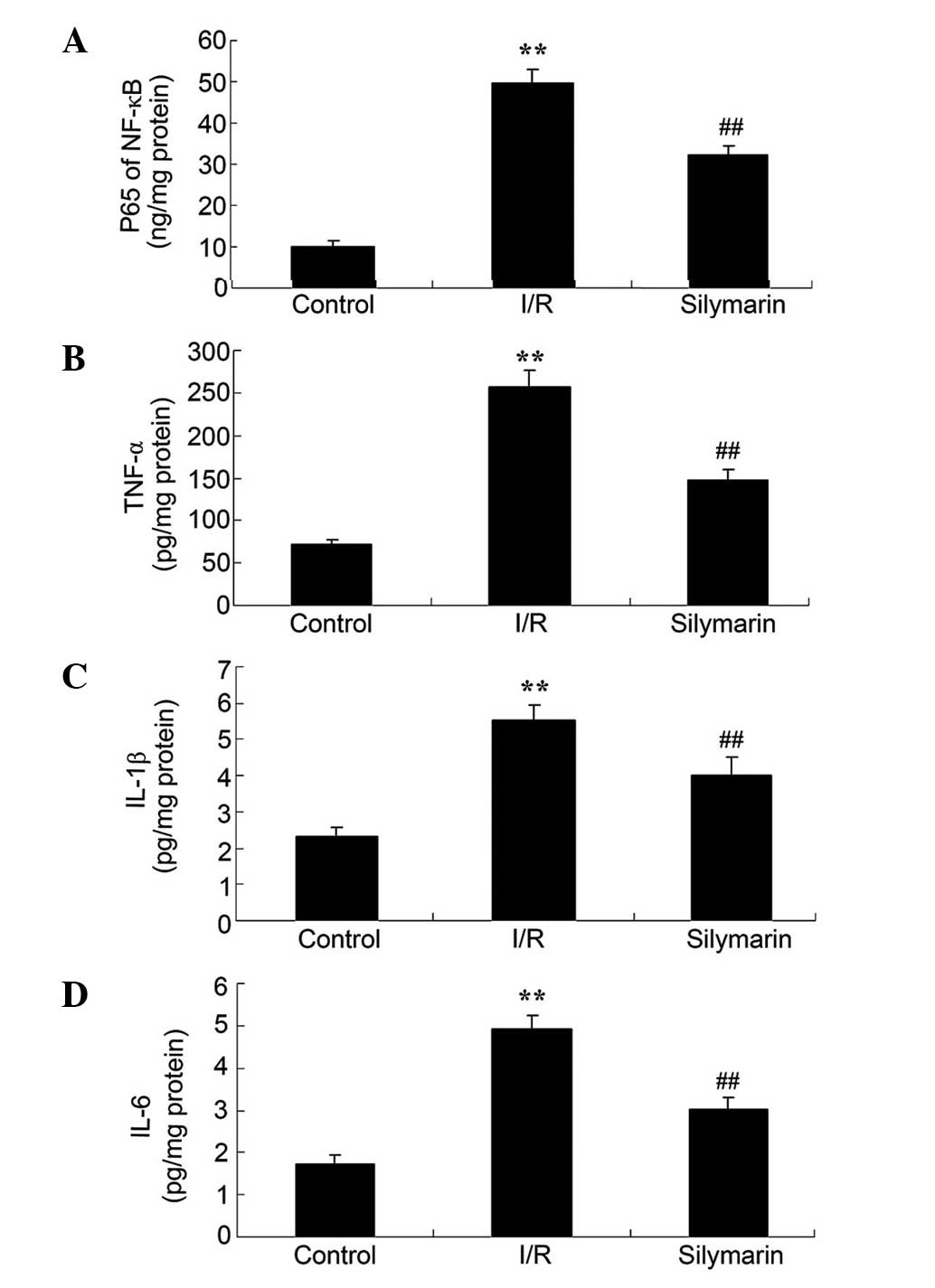
Silymarin reduces I/R-induced inflammation of the
lungs. In order to investigate the inflammatory effects of
silymarin, the serum NF-κB, TNF-α, IL-1β and IL-6 protein levels
were analyzed following reperfusion. These inflammatory factors
were significantly increased in I/R-injured rats compared with the
control group (P<0.01; Fig. 4).
However, protein levels of these inflammatory factors were
significantly reduced following silymarin treatment of I/R-injured
rats (P<0.01; Fig. 4).
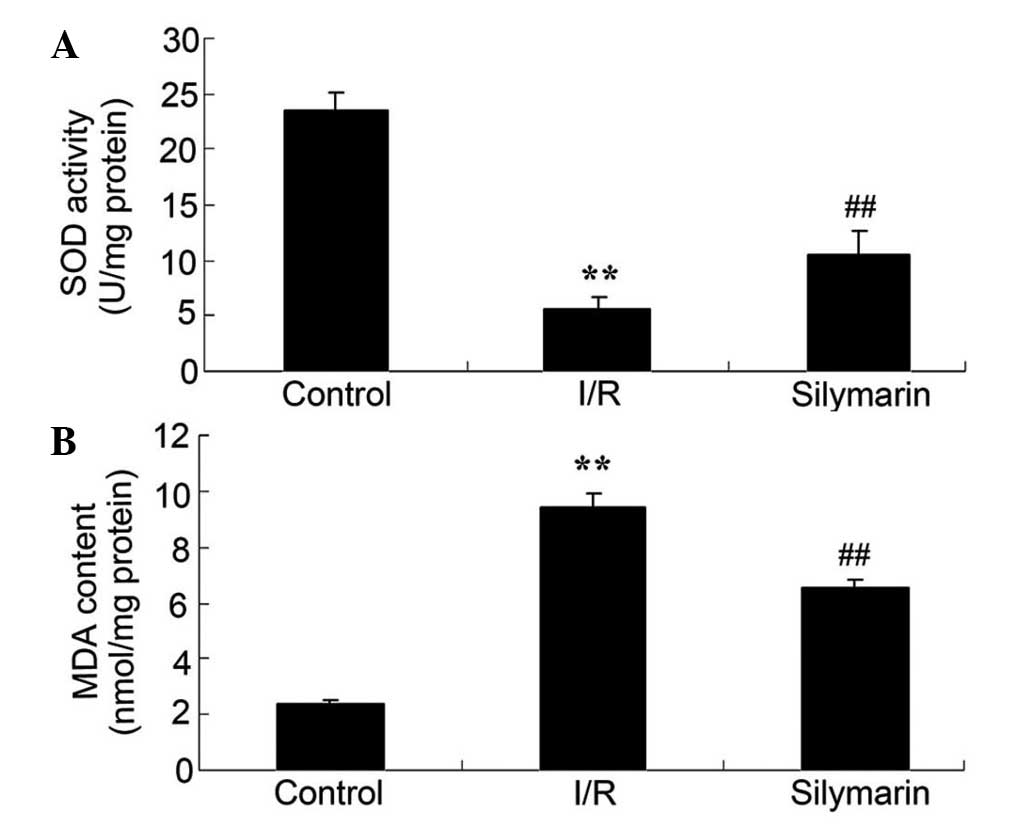
Silymarin increases SOD and reduces
MDA levels in rat lungs following I/R injury
The anti-oxidative effects of silymarin were also
examined, using the serum SOD and MDA levels. Serum SOD levels were
significantly decreased and serum MDA levels were significantly
increased in the lungs of rats following I/R injury, as compared
with the control group (P<0.01; Fig.
5). However, serum levels of SOD were significantly increased
and serum levels of MDA were significantly decreased in the lungs
of silymarin-treated rats, as compared with the I/R-injured group
(P<0.01; Fig. 5).
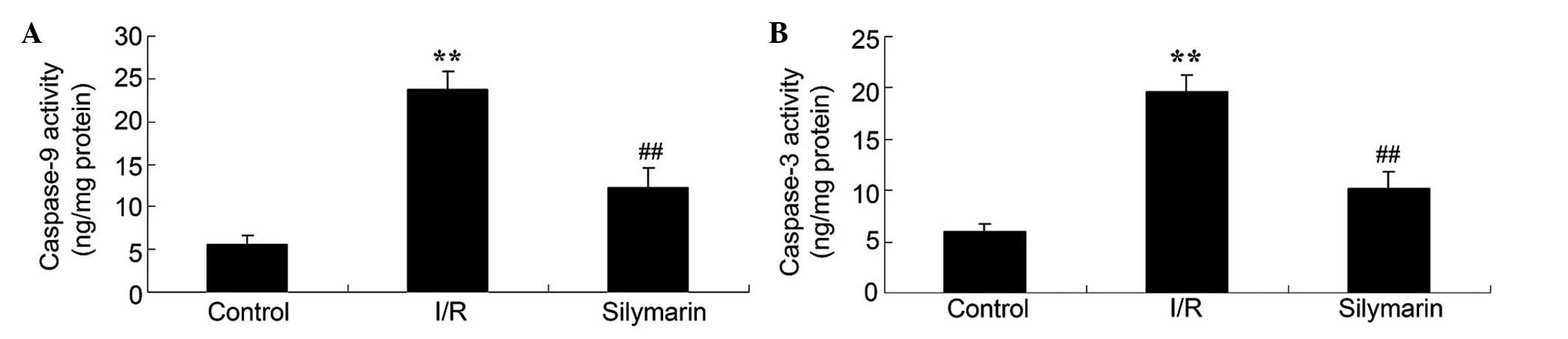
Silymarin ameliorates I/R-induced cell
apoptosis in the lungs
In order to elucidate the effect of silymarin on
cell apoptosis following lung I/R, the levels of caspase-3 and
caspase-9 were investigated following reperfusion. Lung I/R injury
markedly increased the caspase-3 and −9 levels compared with the
control group (P<0.01; Fig. 6).
However, treatment with silymarin markedly decreased caspase-3 and
−9 levels compared with the I/R-injured group (P<0.01; Fig. 6).
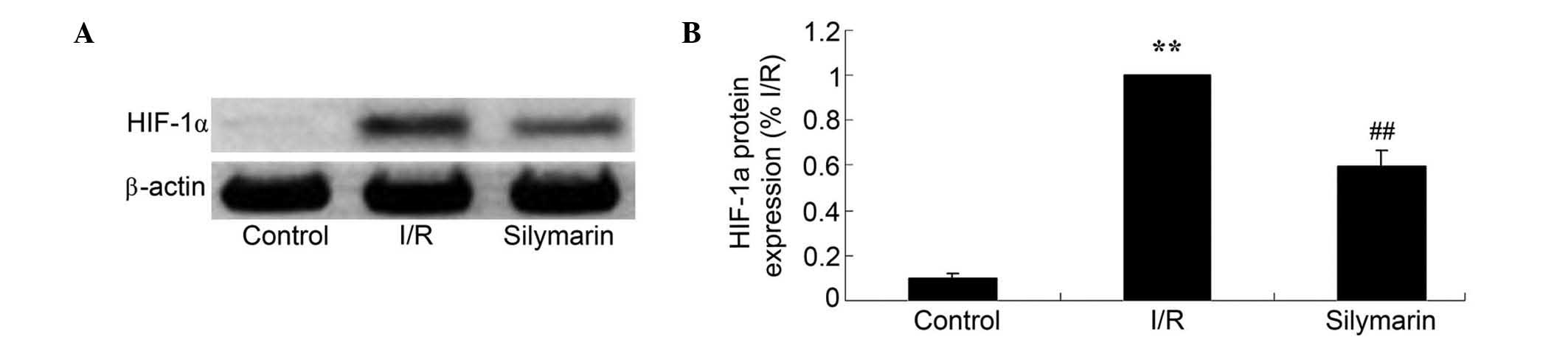
Silymarin attenuates I/R-induced
HIF-1α expression in the lungs
In order to reveal the effects of silymarin on
HIF-1α expression, HIF-1α protein expression was analyzed using
western blotting. HIF-1α protein levels were increased subsequent
to I/R injury compared with the control group (P<0.01; Fig. 7). As demonstrated in Fig. 7, HIF-1α protein levels were decreased
following silymarin treatment of lung I/R-injured rats (P<0.01;
Fig. 7).
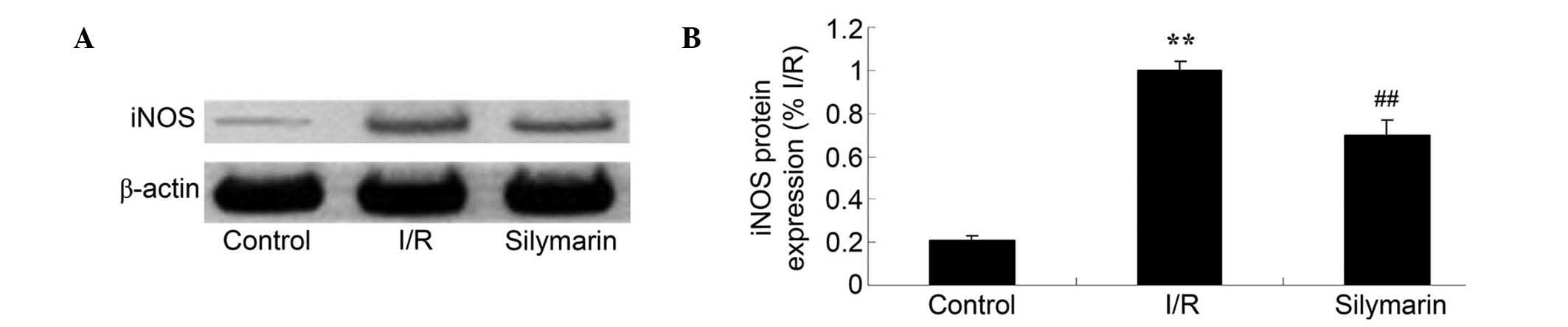
Silymarin reduces I/R-induced iNOS
expression in the lungs
The effects of silymarin treatment on iNOS
expression were examined using western blotting; this revealed that
the protein expression level of iNOS was increased following I/R
injury compared with the control group (P<0.01; Fig. 8). However, silymarin treatment
decreased iNOS expression compared with that in lung I/R-injured
rats (P<0.01; Fig. 8).
Discussion
Lung I/R injury refers to restore blood flow
perfusion, on the basis of ischemia of lung tissue damage is
aggravating pathological state. In numerous situations known to
cause lung I/R injury, including thrombolysis for pulmonary
embolism, interventional therapy and lung transplantation, the
clinical focus is the prevention of lung I/R injury (10). The major pathological changes
following I/R injury are as follows: i) Intimal hyperplasia of the
pulmonary artery, increased elastic fibers and collagen matrix,
hardening of blood vessels and increased resistance of the blood
vessels; ii) hyperplasia and hypertrophy of the smooth muscle cell
membrane, leading to intermembrane hypertrophy; and iii) loss of
the muscular layer of the pulmonary arteriole (11). The present study demonstrated that
silymarin significantly reduced lung I/R-induced pulmonary vascular
dysfunction and lung moisture. Concordantly, Demir et al
(12) revealed that silymarin
attenuates mesenteric I/R injury, and Turgut et al (13) reported that silymarin protects
against kidney I/R injury. The use of silymarin may therefore be
considered a novel therapeutic strategy for protection against lung
I/R injury.
Animal and clinical trials have confirmed that the
inflammatory response is focal to continuing tissue damage
following cerebral ischemia, and this is observed to a greater
degree following lung I/R injury (14,15).
Reduction in the inflammatory response is therefore an important
strategy to attenuate lung I/R injury. NF-κB is an important signal
transduction molecule in the inflammatory response, with a central
role in the inflammatory response to lung I/R injury (16,17).
Activation of the NF-κB pathway induces the expression of adhesion
molecules and chemokines, and the expression of pro-inflammatory
factors; this response leads to leukocyte adhesion, aggregation and
infiltration in the ischemic region, aggravating lung I/R injury
(18). In the present study,
silymarin significantly reduced the serum NF-κB, TNF-α, IL-1β and
IL-6 levels in the lungs of I/R-injured rats. A previous study
demonstrated that silymarin suppressed inflammation in
mycobacterial adjuvant-induced arthritis (19) and in the skin of SENCAR mice
(20). Silymarin may therefore
represent a potent agent for protection against the lung
I/R-induced inflammatory response.
Lung I/R injury is a significant cause of
post-operative acute lung injury and multiple organ failure.
Oxidative stress is central to I/R injury; a previous study
reported that the majority of lung tissue cells generate damaging
reactive oxygen species, and that the abundant capillaries and
fragile wall structure of the lungs makes them vulnerable to
oxidative stress (21). MDA is a
terminal product of lipid peroxidation, such that its expression
levels reflect the degree of lipid peroxidation damage (22). Furthermore, SOD and catalase are
important antioxidant enzymes of the cell; the levels of which
reflect the protective ability of lung tissue cells (23). Therefore, oxidative stress is may be
considered important in the process of lung I/R injury (22). The data from the present study
demonstrated that silymarin significantly increased the serum
levels of SOD in rats with lung I/R injuries. A previous study by
Clichici et al (24) reported
that silymarin inhibited the progression of fibrosis through
suppression of oxidative stress, and Moshtaghion et al
(25) revealed that silymarin
prevented varicocele-induced damage through an increase in MDA
expression. The beneficial effects of silymarin may therefore be
attributed to anti-oxidative effects.
HIF-1α is a transcription factor involved in
altering cellular oxygen concentration and regulation of gene
expression (26). The lung I/R
injury-induced HIF-1α expression observed in the present study
likely exacerbated the injury of lung tissue cells, which is
consistent with the results of a previous study (27). HIF-1α promotion of lung tissue cell
injury may be associated with hypoxia; the mitochondria of
I/R-conditioned cells produce large amounts of reactive oxygen
species, in addition to the hydroxide produced during I/R (28). A previous study in a rat model of
pulmonary hypertension reported increased HIF-1α expression in the
pulmonary artery intima, raising the level of downstream iNOS
expression; this resulted in the proliferation of vascular
endothelial cells within the pulmonary artery intima and
concomitant structural damage to the pulmonary vascular
endothelium, thereby promoting angiogenesis and pulmonary vascular
remodeling (29). This prior study
indicated that, at the protein and gene level, HIF-1α and iNOS may
contribute to hypoxia, causing lung I/R injury (4). In the present study, silymarin
significantly reduced caspase-3 and −9, HIF-1α and iNOS expression
levels in rats following lung I/R injury. Similarly, Li et
al (30) previously reported
that silymarin reduced the UV-irradiated caspase-3 and −9
activities in A375-S2 cells, and Atawia et al (31) demonstrated that silymarin reduced the
production of inflammatory mediators by downregulation of HIF-1α,
iNOS and NF-κB. Kim et al (32) demonstrated that silymarin inhibits NO
and iNOS production in pancreatic β cells. Therefore, the
regulatory effect of silymarin against lung I/R injury may be
associated with the caspase/HIF-1α/iNOS pathway.
In conclusion, the present study demonstrated that
silymarin treatment was able to improve pulmonary vascular
dysfunction following lung I/R injury via the HIF-1α-iNOS pathway.
Further studies are required in order to elucidate the protective
effects of silymarin against lung I/R injury.
Acknowledgements
The present study was supported by the Natural
Science Foundation of Shandong Province (grant no. ZR2012HL54 and
ZR2013HL022) and the Seed Fund of The Second Hospital of Shandong
University (grant no. S2015010018).
References
|
1
|
Mansour Z, Charles AL, Kindo M, Pottecher
J, Chamaraux-Tran TN, Lejay A, Zoll J, Mazzucotelli JP and Geny B:
Remote effects of lower limb ischemia-reperfusion: Impaired lung,
unchanged liver, and stimulated kidney oxidative capacities. BioMed
Res Int. 2014:3923902014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Diao TJ, Chen X, Deng LH, Chen HX, Liang
Y, Zhao XD, Wang QH, Yuan WS, Gao BC and Ye Y: Protective effect of
nitric oxide on hepatopulmonary syndrome from ischemia-reperfusion
injury. World J Gastroenterol. 18:3310–3316. 2012.PubMed/NCBI
|
|
3
|
Lv X, Tan J, Liu D, Wu P and Cui X:
Intratracheal administration of p38α short-hairpin RNA plasmid
ameliorates lung ischemia-reperfusion injury in rats. J Heart Lung
Transplant. 31:655–662. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhao X, Jin Y, Li H, Wang Z, Zhang W and
Feng C: Hypoxia-inducible factor 1alpha contributes to pulmonary
vascular dysfunction in lung ischemia-reperfusion injury. Int J
Clin Exp Pathol. 7:3081–3088. 2014.PubMed/NCBI
|
|
5
|
Natarajan R, Jones DG, Fisher BJ, Wallace
TJ, Ghosh S and Fowler AA III: Hypoxia inducible factor-1:
Regulation by nitric oxide in posthypoxic microvascular
endothelium. Biochem Cell Biol. 83:597–607. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Malekinejad H, Sheikhzadeh S and
Hobbenaghi R: Silymarin attenuates mycophenolate mofetil-induced
duodenal disorders in rats. Avicenna J Phytomed. 4:170–181.
2014.PubMed/NCBI
|
|
7
|
Bonifaz V, Shan Y, Lambrecht RW, Donohue
SE, Moschenross D and Bonkovsky HL: Effects of silymarin on
hepatitis C virus and haem oxygenase-1 gene expression in human
hepatoma cells. Liver Int. 29:366–373. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rao PR and Viswanath RK: Cardioprotective
activity of silymarin in ischemia-reperfusion-induced myocardial
infarction in albino rats. Exp Clin Cardiol. 12:179–187.
2007.PubMed/NCBI
|
|
9
|
Moral-Sanz J, Menendez C, Moreno L, Moreno
E, Cogolludo A and Perez-Vizcaino F: Pulmonary arterial dysfunction
in insulin resistant obese Zucker rats. Respir Res. 12:512011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Luo C, Yuan D, Zhao W, Chen H, Luo G, Su G
and Hei Z: Sevoflurane ameliorates intestinal
ischemia-reperfusion-induced lung injury by inhibiting the
synergistic action between mast cell activation and oxidative
stress. Mol Med Rep. 12:1082–1090. 2015.PubMed/NCBI
|
|
11
|
Shoji T, Omasa M, Nakamura T, Yoshimura T,
Yoshida H, Ikeyama K, Fukuse T and Wada H: Mild hypothermia
ameliorates lung ischemia reperfusion injury in an ex vivo rat lung
model. Eur Surg Res. 37:348–353. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Demir M, Amanvermez R, Polat Kamalı A,
Karabıçak I, Cınar H, Kesicioğlu T and Polat C: The effect of
silymarin on mesenteric ischemia-reperfusion injury. Med Princ
Pract. 23:140–144. 2014.PubMed/NCBI
|
|
13
|
Turgut F, Bayrak O, Catal F, Bayrak R,
Atmaca AF, Koc A, Akbas A, Akcay A and Unal D: Antioxidant and
protective effects of silymarin on ischemia and reperfusion injury
in the kidney tissues of rats. Int Urol Nephrol. 40:453–460. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yousefi H, Ahmadiasl N, Alihemmati A and
Habibi P: Effect of renal ischemia-reperfusion on lung injury and
inflammatory responses in male rat. Iran J Basic Med Sci.
17:802–807. 2014.PubMed/NCBI
|
|
15
|
Chen LF, Tian YF, Lin CH, Huang LY, Niu KC
and Lin MT: Repetitive hyperbaric oxygen therapy provides better
effects on brain inflammation and oxidative damage in rats with
focal cerebral ischemia. J Formos Med Assoc. 113:620–628. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang F, Lu M, Wang H and Ren T: Aspirin
attenuates angiotensin II-induced inflammation in bone marrow
mesenchymal stem cells via the inhibition of ERK1/2 and NF-κB
activation. Biomed Rep. 1:930–934. 2013.PubMed/NCBI
|
|
17
|
Jin LY, Li CF, Zhu GF, Wu CT, Wang J and
Yan SF: Effect of siRNA against NF-κB on sepsis-induced acute lung
injury in a mouse model. Mol Med Rep. 10:631–637. 2014.PubMed/NCBI
|
|
18
|
Amoruso A, Bardelli C, Cattaneo CI, Fresu
LG, Manzetti E and Brunelleschi S: Neurokinin (NK)-1 receptor
expression in monocytes from bipolar disorder patients: A pilot
study. J Affect Disord. 178:188–192. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gupta OP, Sing S, Bani S, Sharma N,
Malhotra S, Gupta BD, Banerjee SK and Handa SS: Anti-inflammatory
and anti-arthritic activities of silymarin acting through
inhibition of 5-lipoxygenase. Phytomedicine. 7:21–24. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhao J, Lahiri-Chatterjee M, Sharma Y and
Agarwal R: Inhibitory effect of a flavonoid antioxidant silymarin
on benzoyl peroxide-induced tumor promotion, oxidative stress and
inflammatory responses in SENCAR mouse skin. Carcinogenesis.
21:811–816. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yao R, Zhou Y, He Y, Jiang Y, Liu P, Ye L,
Zheng Z, Lau WB, Cao Y and Zeng Z: Adiponectin protects against
paraquat-induced lung injury by attenuating oxidative/nitrative
stress. Exp Ther Med. 9:131–136. 2015.PubMed/NCBI
|
|
22
|
Sulkowska M and Sulkowski S: The effect of
pentoxifylline on ultrastructural picture of type II alveolar
epithelial cells and generation of reactive oxygen species during
cyclophosphamide-induced lung injury. J Submicrosc Cytol Pathol.
29:487–496. 1997.PubMed/NCBI
|
|
23
|
Fu Z, Liu X, Geng B, Fang L and Tang C:
Hydrogen sulfide protects rat lung from ischemia-reperfusion
injury. Life Sci. 82:1196–1202. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Clichici S, Olteanu D, Nagy AL, Oros A,
Filip A and Mircea PA: Silymarin inhibits the progression of
fibrosis in the early stages of liver injury in
CCl4-treated rats. J Med Food. 18:290–298. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Moshtaghion SM, Malekinejad H, Razi M and
Shafie-Irannejad V: Silymarin protects from varicocele-induced
damages in testis and improves sperm quality: Evidence for E2f1
involvement. Syst Biol Reprod Med. 59:270–280. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Prangsaengtong O, Park JY, Inujima A,
Igarashi Y, Shibahara N and Koizumi K: Enhancement of
lymphangiogenesis in vitro via the regulations of HIF-1α expression
and nuclear translocation by deoxyshikonin. Evid Based Complement
Alternat Med. 2013:1482972013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kannan KB, Colorado I, Reino D, Palange D,
Lu Q, Qin X, Abungu B, Watkins A, Caputo FJ, Xu DZ, et al:
Hypoxia-inducible factor plays a gut-injurious role in intestinal
ischemia reperfusion injury. Am J Physiol Gastrointest Liver
Physiol. 300:G853–G861. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Haddad JJ: Science review: Redox and
oxygen-sensitive transcription factors in the regulation of
oxidant-mediated lung injury: Role for hypoxia-inducible factor-1
alpha. Crit Care. 7:47–54. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jiang H, Huang Y, Xu H, Hu R and Li QF:
Inhibition of hypoxia inducible factor-1α ameliorates lung injury
induced by trauma and hemorrhagic shock in rats. Acta Pharmacol
Sin. 33:635–643. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li LH, Wu LJ, Zhou B, Wu Z, Tashiro S,
Onodera S, Uchiumi F and Ikejima T: Silymarin prevents UV
irradiation-induced A375-S2 cell apoptosis. Biol Pharm Bull.
27:1031–1036. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Atawia RT, Mosli HH, Tadros MG, Khalifa
AE, Mosli HA and Abdel-Naim AB: Modulatory effect of silymarin on
inflammatory mediators in experimentally induced benign prostatic
hyperplasia: Emphasis on PTEN, HIF-1α, and NF-κB. Naunyn
Schmiedebergs Arch Pharmacol. 387:1131–1140. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kim EJ, Kim J, Lee MY, Sudhanva MS,
Devakumar S and Jeon YJ: Silymarin inhibits cytokine-stimulated
pancreatic beta cells by blocking the ERK1/2 pathway. Biomol Ther
(Seoul). 22:282–287. 2014. View Article : Google Scholar : PubMed/NCBI
|