Epigenetics is the study of genomic structural
modifications that affect gene expression without altering the
underlying nucleotide sequence (1–3).
Epigenetic mechanisms involved in the regulation of gene expression
include the regulation of non-coding RNA, chromatin remodeling, DNA
methylation and histone modifications (4,5). Of
these mechanisms, DNA methylation has been implicated in numerous
biological functions, such as the development of spermatozoa and
early embryos, and the repression of endogenous retrotransposons,
while it also has a wide range of effects in gene expression
(2,3,6). The
dysregulation of DNA methylation has previously been associated
with various human disorders, and has been shown to increase the
risk of fertilization failure, dysfunction in embryogenesis,
perinatal mortality, congenital abnormalities, preterm birth and
low birth weight (7–11). The present review assesses the
significance of DNA methylation in spermatogenesis in order to
elucidate the association between the dysregulation of DNA
methylation and male infertility. This may provide a basis for the
prevention and treatment of male infertility, as well as permit the
evaluation of the epigenetic quality of sperm in order to reduce
the risk of epigenetic diseases in cases where conception is
performed by assisted reproductive technology (ART).
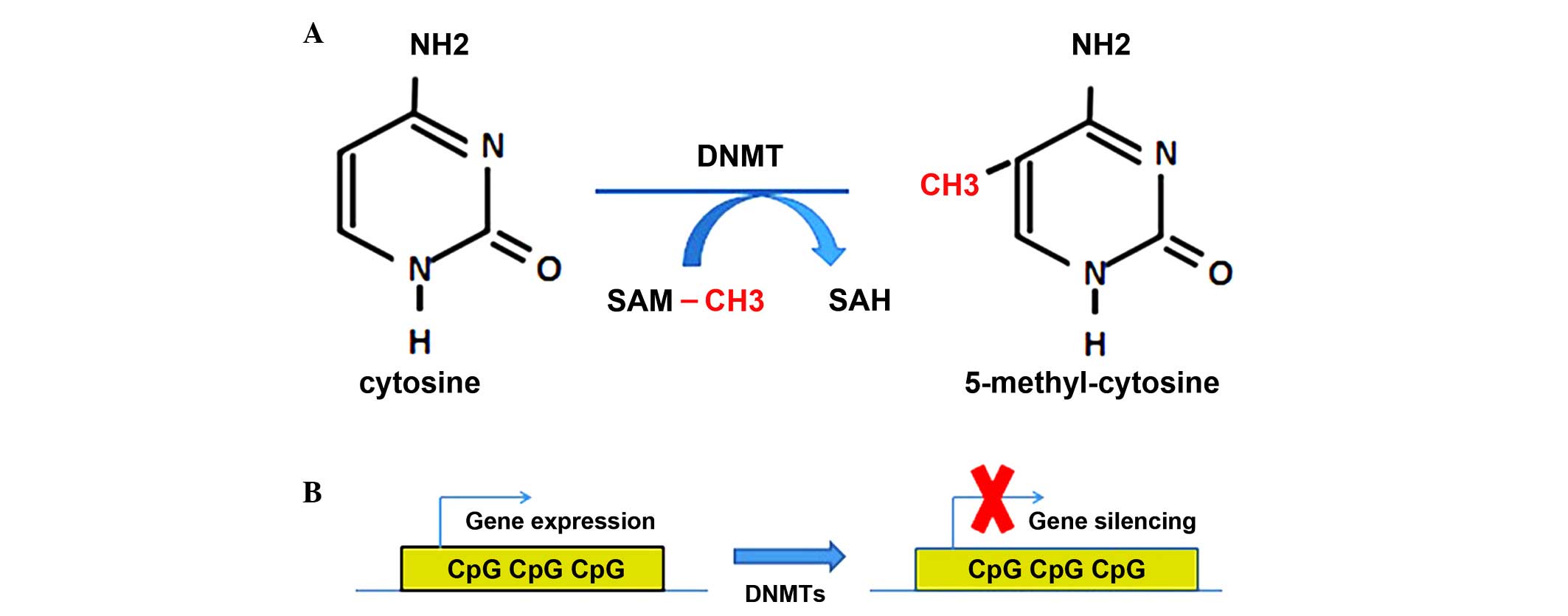
Epigenetic mechanisms are critical regulators of
gene expression during spermatogenesis that may influence male
fertility (12–14). Cytosine, a key DNA base, is
methylated at the position, typically in the context of CpG
dinucleotides. The methylation of constitutive heterochromatic and
promoter regions is generally associated with reduced gene
transcription (Fig. 1A) (15–18).
Therefore, DNA methylation is a type of epigenetic modification
that can effectively promote gene silencing (Fig. 1B). The methyl group for this chemical
modification of the DNA is donated by S-adenosyl-L-methionine (SAM)
(17–22), and the methylation reaction is
catalyzed by members of the DNA methyltransferases (DNMT) family,
which are classified into the following three types in mammals:
DNMT1, DNMT2 and DNMT3. It was demonstrated that DNMT1, DNMT3a and
DNMT3b are robustly expressed in the early embryonic stage;
however, the biological functions of DNMT2 remain elusive (23–25).
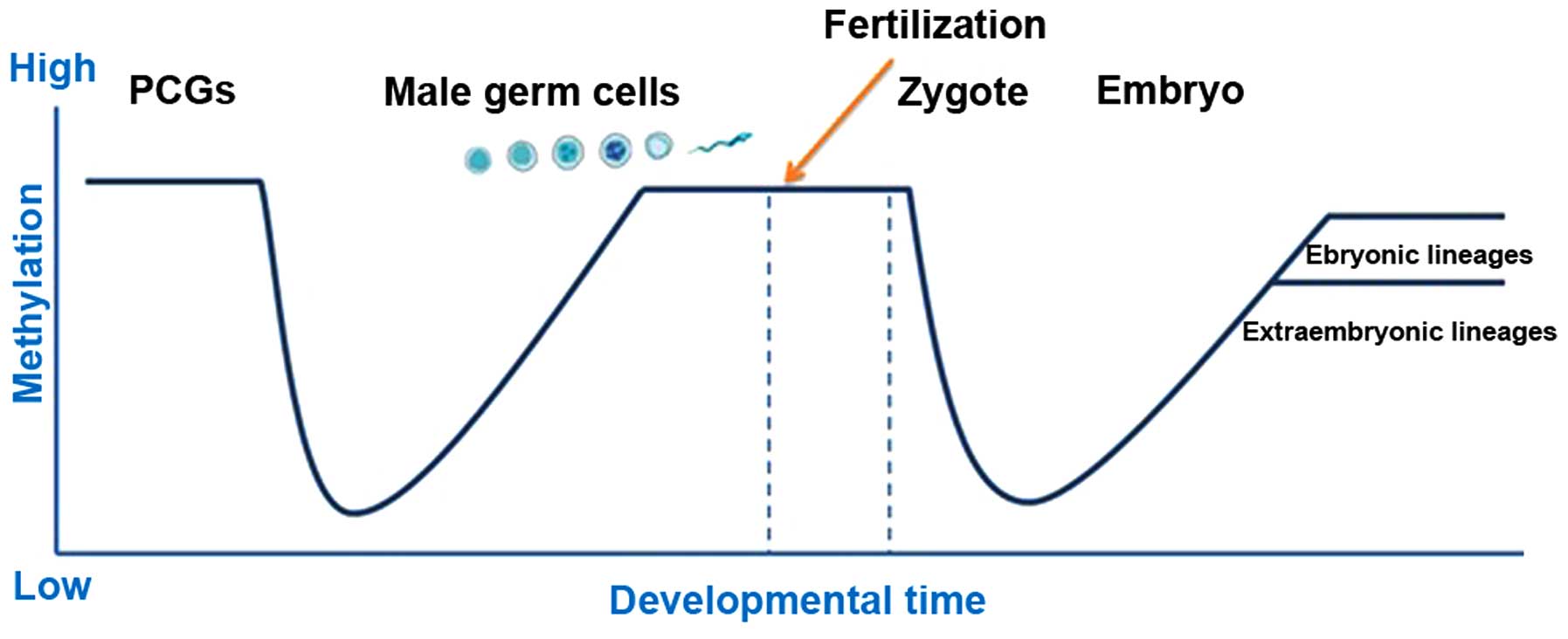
Germ cell development is a highly ordered process
initiated during the growth of a fetus and is completed in adults.
The epigenetic modifications occurring in germ cells are crucial
for the function of germ cells and for embryonic development after
fertilization (50,51). Previous studies have demonstrated
that male germ cells in adult mice have a highly distinct
epigenetic pattern, characterized by a unique genome-wide pattern
of DNA methylation (42,52–55). The
methylation status of testicular DNA is highly distinct, displaying
an eight times higher number of hypomethylated loci, as compared
with somatic tissues (51,56–58).
Alterations in DNA methylation serve a crucial role in establishing
an epigenetic state during the early stages in the development of
germ cells, allowing for transcription to occur at the later stages
(Fig. 2) (59–61).
Genome-wide methylation studies have demonstrated
that the epigenomes of sperm cells and of somatic cells are
significantly different; however, the sperm epigenome is very
similar to that of embryonic stem cells (61–65).
Using restriction landmark genomic scanning technology, DNA
methylation was detected for chromosomes 6, 20 and 22 in
spermatozoa, with numerous sites in sperm and somatic cells
exhibiting varying degrees of methylation (66–68). The
extent of methylation in sperm cells was significantly increased,
as compared with fibroblasts (>20%), liver cells (10%), and
CD4+ and CD8+ lymphocytes (5%) (68,69). DNA
hypermethylation is associated with gene silencing. By contrast,
hypomethylation is associated with gene expression. In sperm cells,
promoters of developmental genes are highly hypomethylated. A
previous gene ontology analysis demonstrated that hypomethylation
in mature sperm cells promoted developmental transcription and
signaling, which is bound by self-renewal mesh transcription factor
of human embryonic stem cells, including OCT4, SOX2, NANOG, KLF4
and FOXD3 protein. Furthermore, recurrent regions of the sperm
genome reportedly demonstrate high degrees of methylation, while
transposons manifest weaker methylation. Whether other mechanisms
exist requires further analysis (65,69,70).
The paternally expressed human gene, MEST/PEG1, is
demethylated in the fetus and remains unmethylated throughout all
stages of sperm development in the adult life (37,71). By
contrast, in male germ cells, the H19 gene is methylated prior to
meiosis at the spermatogonial stage of development (37,72).
Reinitiation of mitotic division of male germ cells during puberty
coincides with an upregulation of DNMT1 within the spermatocytes.
During the early stage of meiosis, DNMT1 levels in spermatocytes
are increased; however, the level of the DNMT1 enzyme is reduced in
pachytene stage spermatocytes (37,73). In
previous studies, the knockout of DNMT1 resulted in a lack of DNA
methylation in the fetus, which, due to a lack of genomic
imprinting, led to apoptosis of spermatagonial cells (65,67,70,74).
However, DNMT1 heterozygous mice had a normal reproductive ability,
thus suggesting that DNMT1 in the heterozygous state is sufficient
to maintain the required DNA methylation pattern (30,75,76).
DNMT3a expression in the testis is upregulated prior to birth and
during early postnatal life, whereas DNMT3b expression is
downregulated during embryonic development and upregulated
postnatally (15–20). Notably, mice lacking DNMT3L have
smaller testes, and a negligible number of spermatozoa by
adulthood, resulting in sterile animals. In a previous study,
DNMT3L was expressed only in germ cells, and the expression pattern
was observed in males and females (77). However, in males, DNMT3L was
initially detected at 12.5 days after fertilization of the egg, and
the levels peaked at 15.5 days and remained upregulated until birth
(77–79). However, the expression of DNMT3L was
significantly 79 following birth and was found to be low in mature
germ cells (36–38), suggesting an association between
DNMT3L and DNA methylation. In addition, the inactivation of DNMT3L
was shown to cause mitotic delays, chromosome synapsis errors and
the ceasing of spermatogenesis at the zygotene stage of mitosis,
thus inhibiting the maturation of germ cells (46–48).
In certain individuals with deletion mutations in
DNMT genes, a proportion of the paternal differentially methylated
regions (DMRs) were normal, which suggested that DNMTs have some
functional duplication (77–79). Notably, oocytes lacking DNMT3L were
able to undergo normal meiosis and exhibited methylation of repeat
sequences; however, a significant lack of methylation-mediated
imprinting existed only in the female imprinting positions
(48–52). This difference in the effects of gene
knockout between males and females raises the question of the
divergent regulatory mechanisms between genders (65,69).
Genomic imprinting is an epigenetic mechanism
resulting in parental expression of certain genes resulting in the
alteration of gene transcription, while the actual gene sequence
remains unchanged (56,80,81). DNA
methylation regulates genomic imprinting, thus resulting in only
one inherited copy of the relevant imprinted gene being expressed
in an embryo. The majority of imprinted genes contain DMRs, in
which methylation differs between the paternal and maternal
alleles. DNA methylation-mediated genomic imprinting is established
during gametogenesis, prior to fertilization (59,60).
By the time the primitive streak has formed during
embryonic development [embryonic day 7.5 (E7.5)], the primordial
germ cells (PGCs) carry the paternally and maternally inherited
imprinting patterns (82). This DNA
methylation pattern is maintained in PGCs, but is rapidly lost
around E8, when PGCs begin to migrate towards the developing gonad.
Upon their arrival at the genital ridge (between E10.5 and E11.5),
global demethylation of mouse PGCs begins in order to remove their
inherited imprinting pattern (61,62). At
this time, PGCs continue to proliferate and undergo differentiation
into distinct male and female germlines (at ~E12.5), while the DNA
methylation pattern of somatic cells is maintained. By E13-14,
demethylation of the DNA is completed and male gametes are arrested
at the prophase stage of mitosis (59,60). It
has previously been suggested that mitosis arrest may be required
following demethylation, since the replication of unmethylated DNA
has been associated with an increased risk of unrepressed
retrotransposon transposition, which may lead to mutations.
Therefore, in sperm cells, DNA methylation-mediated genomic
imprinting is initiated prenatally, prior to meiosis, and is
completed by the pachytene phase of postnatal spermatogenesis
(61,62,65,69,70,74).
Infertility is a major public health concern that
has a significant social, psychological and economic impact, with
an equal proportion of males and females affected (83–85).
Male infertility is associated with genetic, environmental and
numerous other factors (86,87). The underlying mechanisms are unknown
in 70% of male infertility cases, even in cases where the causes of
male infertility are clear. Therefore, further studies are required
in order to elucidate the mechanisms underlying male infertility.
In male factor infertility, epigenetic modifications may serve a
pivotal role by regulating male germ cell development and
maintenance (88–92). Thus, abnormal imprinting as a result
of DNA methylation dysregulation may be associated with male
infertility.
Previous studies have demonstrated that disturbed
spermatogenesis is associated with incorrect imprinting (74). An analysis of semen from infertile
men has shown that 14.4% of anomalous patriarchal methylation
occurred in H19 and gene trap locus 2 gene (93–95). In
spermatozoa from oligozoospermic men, the occurrence of
hypermethylation at several maternal DMRs or hypomethylation of H19
and intergenic-DMR was increased, particularly in patients with
ejaculation volumes of <10×106/ml (96–99). In
men with oligoasthenoteratozoospermia, methylation was markedly
reduced at all CpGs, reaching statistical significance in subgroups
with a sperm concentration of <10×106/ml. These
findings suggest that abnormal DNA methylation-mediated genomic
imprinting is associated with oligoasthenoteratozoospermia and
oligozoospermia (100–107).
In patients with male infertility, paternally and
maternally imprinted gene methylation abnormalities have previously
been reported. In oligospermic patients, a low methylation or
unmethylation pattern at the H19 imprinted gene has been associated
with hypermethylation at the MEST imprinted gene, as well as a
reduced sperm quality and decreased DNA methylation-mediated
imprinting, as compared with fertile men (108,109).
DNA methylation markers have been detected in the
spermatogonia stage; therefore, the abnormal DNA methylation
patterns observed in infertile men may be due to the failure of
re-methylation in spermatogonia or alterations to methylation
maintenance in spermatocytes, sperm cells or the mature sperm cell.
In addition, abnormal DNA methylation may be associated with the
abnormal activation of DNMTs (110–114).
Alterations in DNA methylation-mediated genomic
imprinting have been observed more frequently in men with
oligoasthenoteratozoospermia and oligozoospermia (115). However, whether methylation defects
in imprinted genes will affect the development and growth processes
of ART offspring remains to be elucidated. If epigenetic
modifications are a key factor in the maturation of sperm cells,
alterations in the epigenetic patterns of infertile men may provide
a reasonable explanation for complications associated with ART,
including low birth weight, premature births, congenital
abnormalities, an increased perinatal mortality rate and pregnancy
complications (116,117). Embryos obtained from patients with
hypospermatogenesis and almost complete hypomethylation at the H19
DMR following ART all exhibited developmental arrest (117,118).
However, patients with oligoasthenoteratozoospermia with a partial
hypomethylation of H19 presented a reduced fertilization rate
following intracytoplasmic sperm injection (ICSI). A previous
analysis of the methylation status of ICSI infants with a low birth
weight revealed hypermethylation at the MEST gene in one of the
infants included in the study (119,120).
In conclusion, DNA methylation has been closely
associated with male infertility (66,121).
Understanding the mechanisms underlying DNA methylation is
particularly important in order to develop therapeutic strategies
for male genital system diseases caused by abnormal sperm DNA
methylation. Studies on the mechanisms underlying the regulation of
DNA methylation during spermatogenesis are still in their initial
stages. Numerous issues remain, such as transgenerational
inheritance of human epigenetic genes and the association between
DNA methylation and other epigenetic factors, while it is unclear
whether the risk of abnormal methylation-induced embryonic diseases
has a threshold or is continuously increasing process.
|
1
|
Molaro A, Falciatori I, Hodges E, Aravin
AA, Marran K, Rafii S, McCombie WR, Smith AD and Hannon GJ: Two
waves of de novo methylation during mouse germ cell development.
Genes Dev. 28:1544–1549. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Verma A, Rajput S, De S, Kumar R,
Chakravarty AK and Datta TK: Genome-wide profiling of sperm DNA
methylation in relation to buffalo (Bubalus bubalis) bull
fertility. Theriogenology. 82:750–759, e751. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Xu C and Song N: Epigenetic regulation in
spermatogenesis. Zhong Hua Nan Ke Xue. 20:387–391. 2014.(In
Chinese).
|
|
4
|
Dogra S, Sona C, Kumar A and Yadav PN:
Epigenetic regulation of G protein coupled receptor signaling and
its implications in psychiatric disorders. Int J Biochem Cell Biol.
16:S1357–S2725. 2016.
|
|
5
|
Wang P, Zhang H, Hou H, Wang Q, Li Y,
Huang Y, Xie L, Gao F, He S and Li L: Cell cycle arrest induced by
inhibitors of epigenetic modifications in maize (Zea mays) seedling
leaves: Characterization of the process and possible mechanisms
involved. New Phytol. Apr 4–2016.(Epub ahead of print). View Article : Google Scholar
|
|
6
|
Cheng P, Chen H, Zhang RP, Liu SR and
Zhou-Cun A: Polymorphism in DNMT1 may modify the susceptibility to
oligospermia. Reprod Biomed Online. 28:644–649. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Albertini DF: Relevant and irrelevant
translational discovery and male infertility: The case of the Y
chromosome and more! J Assist Reprod Genet. 31:1113–1114. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen J, Xiao HJ, Qi T, Chen DL, Long HM
and Liu SH: Rare earths exposure and male infertility: The injury
mechanism study of rare earths on male mice and human sperm.
Environ Sci Pollut Res Int. 22:2076–2086. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Komiya A, Kato T, Kawauchi Y, Watanabe A
and Fuse H: Clinical factors associated with sperm DNA
fragmentation in male patients with infertility. Scientific World
Journal. 2014:8683032014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cheng BW, Guo H, Li ZF, Ma L, Wang YL,
Yang LJ, Ye JJ and Zheng S: Identification of null and duplicated
alleles for forensic DYS549, DYS527 and DYS459 in male infertility
population. Yi Chuan. 36:786–792. 2014.(In Chinese). PubMed/NCBI
|
|
11
|
Katib AA, AlHawsawi K, Motair W and Bawa
AM: Secondary infertility and the aging male, overview. Cent
European J Urol. 67:184–188. 2014.PubMed/NCBI
|
|
12
|
Griseri P, Garrone O, Lo Sardo A,
Monteverde M, Rusmini M, Tonissi F, Merlano M, Bruzzi P, Lo Nigro C
and Ceccherini I: Genetic and epigenetic factors affect RET gene
expression in breast cancer cell lines and influence survival in
patients. Oncotarget. Mar 28–2016.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
DeVries A and Vercelli D: Epigenetic
Mechanisms in Asthma. Ann Am Thorac Soc. 13(Suppl 1): S48–S50.
2016.PubMed/NCBI
|
|
14
|
Kim SY, Morales CR, Gillette TG and Hill
JA: Epigenetic regulation in heart failure. Curr Opin Cardiol.
31:255–265. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jena SC, Kumar S, Rajput S, Roy B, Verma
A, Kumaresan A, Mohanty TK, De S, Kumar R and Datta TK:
Differential methylation status of IGF2-H19 locus does not affect
the fertility of crossbred bulls but some of the CTCF binding sites
could be potentially important. Mol Reprod Dev. 81:350–362. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
KuramochiMiyagawa S, KitaKojima K,
Shiromoto Y, Ito D, Koshima H and Nakano T: DNA methylation in
mouse testes. Methods Mol Biol. 1093:97–109. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Schütte B, El Hajj N, Kuhtz J, Nanda I,
Gromoll J, Hahn T, Dittrich M, Schorsch M, Müller T and Haaf T:
Broad DNA methylation changes of spermatogenesis, inflammation and
immune response-related genes in a subgroup of sperm samples for
assisted reproduction. Andrology. 1:822–829. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kläver R, Tüttelmann F, Bleiziffer A, Haaf
T, Kliesch S and Gromoll J: DNA methylation in spermatozoa as a
prospective marker in andrology. Andrology. 1:731–740. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Calicchio R, Doridot L, Miralles F, Méhats
C and Vaiman D: DNA methylation, an epigenetic mode of gene
expression regulation in reproductive science. Curr Pharm Des.
20:1726–1750. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gan H, Wen L, Liao S, Lin X, Ma T, Liu J,
Song CX, Wang M, He C, Han C, et al: Dynamics of
5-hydroxymethylcytosine during mouse spermatogenesis. Nat Commun.
4:19952013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Boissonnas CC, Jouannet P and Jammes H:
Epigenetic disorders and male subfertility. Fertil Steril.
99:624–631. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mychasiuk R, Harker A, Ilnytskyy S and
Gibb R: Paternal stress prior to conception alters DNA methylation
and behaviour of developing rat offspring. Neuroscience.
241:100–105. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Paluch BE, Naqash AR, Brumberger Z, Nemeth
MJ and Griffiths EA: Epigenetics: A primer for clinicians. Blood
Rev. Feb 26–2016.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu X, Zhou P, Lu Y and Luo Y: Progresses
of DNA methylation in common ocular tumor. Zhonghua Yan Ke Za Zhi.
51:950–954. 2015.(In Chinese). PubMed/NCBI
|
|
25
|
Wijenayake S and Storey KB: The role of
DNA methylation during anoxia tolerance in a freshwater turtle
(Trachemys scripta elegans). J Comp Physiol B. 186:333–342. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ko YG, Yun J, Park HJ, Tanaka S, Shiota K
and Cho JH: Dynamic methylation pattern of the methyltransferase1o
(Dnmt1o) 5′-flanking region during mouse oogenesis and
spermatogenesis. Mol Reprod Dev. 80:212–222. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Okamura E, Matsuzaki H, Sakaguchi R,
Takahashi T, Fukamizu A and Tanimoto K: The H19 imprinting control
region mediates preimplantation imprinted methylation of nearby
sequences in yeast artificial chromosome transgenic mice. Mol Cell
Biol. 33:858–871. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Meikar O, Da Ros M and Kotaja N:
Epigenetic regulation of male germ cell differentiation. Subcell
Biochem. 61:119–138. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bose R, Adiga SK, D'Souza F, Salian SR,
Uppangala S, Kalthur G, Jain N, Radhakrishnan RA, Bhat N,
Krishnamurthy H, et al: Germ cell abnormalities in streptozotocin
induced diabetic mice do not correlate with blood glucose level. J
Assist Reprod Genet. 29:1405–1413. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Saferali A, Moussette S, Chan D, Trassler
J, Chen T, Rozen R and Nauvoma AK: DNA methyltransferase 1 (Dnmt1)
mutation affects Snrpn imprinting in the mouse male germ line.
Genome. 55:673–682. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kato Y and Nozaki M: Distinct DNA
methylation dynamics of spermatogenic cell-specific intronless
genes is associated with CpG content. PLoS One. 7:e436582012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang GL, Zhang XF, Feng YM, Li L, Huynh
E, Sun XF, Sun ZY and Shen W: Exposure to bisphenol A results in a
decline in mouse spermatogenesis. Reprod Fertil Dev. 25:847–859.
2013. View
Article : Google Scholar : PubMed/NCBI
|
|
33
|
Coral S, Covre A, Nicolay HJ, Parisi G,
Rizzo A, Colizzi F, Dalla Santa S, Fonsatti E, Fratta E, Sigalotti
L, et al: Epigenetic remodelling of gene expression profiles of
neoplastic and normal tissues: Immunotherapeutic implications. Br J
Cancer. 107:1116–1124. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jenkins TG and Carrell DT: The sperm
epigenome and potential implications for the developing embryo.
Reproduction. 143:727–734. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Carrell DT: Epigenetics of the male
gamete. Fertil Steril. 97:267–274. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
vanMontfoort AP, Hanssen LL, de Sutter P,
Viville S, Geraedts JP and de Boer P: Assisted reproduction
treatment and epigenetic inheritance. Hum Reprod Update.
18:171–197. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Marques CJ, Joao Pinho M, Carvalho F,
Bieche I, Barros A and Sousa M: DNA methylation imprinting marks
and DNA methyltransferase expression in human spermatogenic cell
stages. Epigenetics. 6:1354–1361. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Niles KM, Chan D, La Salle S, Oakes CC and
Trasler JM: Critical period of nonpromoter DNA methylation
acquisition during prenatal male germ cell development. PLoS One.
6:e241562011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Rajender S, Avery K and Agarwal A:
Epigenetics, spermatogenesis and male infertility. Mutat Res.
727:62–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
LeBouc Y, Rossignol S, Azzi S, Brioude F,
Cabrol S, Gicquel C and Netchine I: Epigenetics, genomic imprinting
and developmental disorders. Bull Acad Natl Med. 194:287–297.
2010.(In French). PubMed/NCBI
|
|
41
|
NavarroCosta P, Nogueira P, Carvalho M,
Leal F, Cordeiro I, CalhazJorge C, Gonçalves J and Plancha CE:
Incorrect DNA methylation of the DAZL promoter CpG island
associates with defective human sperm. Hum Reprod. 25:2647–2654.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Takashima S, Takehashi M, Lee J, Chuma S,
Okano M, Hata K, Suetake I, Nakatsuji N, Miyoshi H, Tajima S, et
al: Abnormal DNA methyltransferase expression in mouse germline
stem cells results in spermatogenic defects. Biol Reprod.
81:155–164. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yaman R and Grandjean V: Timing of entry
of meiosis depends on a mark generated by DNA methyltransferase 3a
in testis. Mol Reprod Dev. 73:390–397. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tucker KL, Beard C, Dausmann J,
JacksonGrusby L, Laird PW, Lei H, Li E and Jaenisch R: Germ-line
passage is required for establishment of methylation and expression
patterns of imprinted but not of nonimprinted genes. Genes Dev.
10:1008–1020. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gebert C, Kunkel D, Grinberg A and Pfeifer
K: H19 imprinting control region methylation requires an imprinted
environment only in the male germ line. Mol Cell Biol.
30:1108–1115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Colosimo A, Di Rocco G, Curini V, Russo V,
Capacchietti G, Berardinelli P, Mattioli M and Barboni B:
Characterization of the methylation status of five imprinted genes
in sheep gametes. Anim Genet. 40:900–908. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Boissonnas CC, Abdalaoui HE, Haelewyn V,
Fauque P, Dupont JM, Gut I, Vaiman D, Jouannet P, Tost J and Jammes
H: Specific epigenetic alterations of IGF2-H19 locus in spermatozoa
from infertile men. Eur J Hum Genet. 18:73–80. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Trasler JM: Epigenetics in
spermatogenesis. Mol Cell Endocrinol. 306:33–36. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Feil R: Epigenetic asymmetry in the zygote
and mammalian development. Int J Dev Biol. 53:191–201. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Schoenmakers S, Wassenaar E, Hoogerbrugge
JW, Laven JS, Grootegoed JA and Baarends WM: Female meiotic sex
chromosome inactivation in chicken. PLoS Genet. 5:e10004662009.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Marques CJ, Francisco T, Sousa S, Carvalho
F, Barros A and Sousa M: Methylation defects of imprinted genes in
human testicular spermatozoa. Fertil Steril. 94:585–594. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Godmann M, Lambrot R and Kimmins S: The
dynamic epigenetic program in male germ cells: Its role in
spermatogenesis, testis cancer, and its response to the
environment. Microsc Res Tech. 72:603–619. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Henckel A and Feil R: Differential
epigenetic marking on imprinted genes and consequences in human
diseases. Med Sci (Paris). 24:747–752. 2008.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Houshdaran S, Cortessis VK, Siegmund K,
Yang A, Laird PW and Sokol RZ: Widespread epigenetic abnormalities
suggest a broad DNA methylation erasure defect in abnormal human
sperm. PLoS One. 2:e12892007. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Tanaka H: Regulation of gene expression in
spermatogenesis. Tanpakushitsu Kakusan Koso. 52(Suppl 1):
2116–2123. 2007.(In Japanese). PubMed/NCBI
|
|
56
|
Rijlaarsdam MA, Tax DM, Gillis AJ,
Dorssers LC, Koestler DC, de Ridder J and Looijenga LH: Genome wide
DNA methylation profiles provide clues to the origin and
pathogenesis of germ cell tumors. PLoS One. 10:e01221462015.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Minor A, Chow V and Ma S: Aberrant DNA
methylation at imprinted genes in testicular sperm retrieved from
men with obstructive azoospermia and undergoing vasectomy reversal.
Reproduction. 141:749–757. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Peltomäki P: DNA methylation changes in
human testicular cancer. Biochim Biophys Acta. 1096:187–196. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kato Y, Kaneda M, Hata K, Kumaki K, Hisano
M, Kohara Y, Okano M, Li E, Nozaki M and Sasaki H: Role of the
Dnmt3 family in de novo methylation of imprinted and repetitive
sequences during male germ cell development in the mouse. Hum Mol
Genet. 16:2272–2280. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Oakes CC, La Salle S, Smiraglia DJ,
Robaire B and Trasler JM: Developmental acquisition of genome-wide
DNA methylation occurs prior to meiosis in male germ cells. Dev
Biol. 307:368–379. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Delaval K, Govin J, Cerqueira F, Rousseaux
S, Khochbin S and Feil R: Differential histone modifications mark
mouse imprinting control regions during spermatogenesis. EMBO J.
26:720–729. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
PaoloniGiacobino A, D'Aiuto L, Cirio MC,
Reinhart B and Chaillet JR: Conserved features of imprinted
differentially methylated domains. Gene. 399:33–45. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Chong S, Vickaryous N, Ashe A, Zamudio N,
Youngson N, Hemley S, Stopka T, Skoultchi A, Matthews J, Scott HS,
et al: Modifiers of epigenetic reprogramming show paternal effects
in the mouse. Nat Genet. 39:614–622. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
PaoloniGiacobino A: Epigenetics in
reproductive medicine. Pediatr Res. 61:51R–57R. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Omisanjo OA, Biermann K, Hartmann S,
Heukamp LC, Sonnack V, Hild A, Brehm R, Bergmann M, Weidner W and
Steger K: DNMT1 and HDAC1 gene expression in impaired
spermatogenesis and testicular cancer. Histochem Cell Biol.
127:175–181. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gunes S, Arslan MA, Hekim GN and Asci R:
The role of epigenetics in idiopathic male infertility. J Assist
Reprod Genet. Mar 3–2016.(Epub ahead of print). View Article : Google Scholar
|
|
67
|
Laurentino SS, Borgmann J and Gromoll J:
On the origin of sperm epigenetic heterogeneity. Reproduction
REP-15-0436. 2016.
|
|
68
|
Casas E and Vavouri T: Sperm epigenomics:
Challenges and opportunities. Front Genet. 5:3302014. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Rousseaux S, Faure AK, Thévenon J,
Escoffier E, Lestrat C, Govin J, Hennebicq S, Sèle B, Caron C and
Khochbin S: Epigenetics of the sperm cell. Gynecol Obstet Fertil.
34:831–835. 2006.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
70
|
La Salle S and Trasler JM: Dynamic
expression of DNMT3a and DNMT3b isoforms during male germ cell
development in the mouse. Dev Biol. 296:71–82. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Riesewijk AM, Hu L, Schulz U, Tariverdian
G, Höglund P, Kere J, Ropers HH and Kalscheuer VM: Monoallelic
expression of human PEG1/MEST is paralleled by parent-specific
methylation in fetuses. Genomics. 42:236–244. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Kerjean A, Dupont JM, Vasseur C, Le
Tessier D, Cuisset L, Pàldi A, Jouannet P and Jeanpierre M:
Establishment of the paternal methylation imprint of the human H19
and MEST/PEG1 genes during spermatogenesis. Hum Mol Genet.
9:2183–2187. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Li Z, Dai H, Martos SN, Xu B, Gao Y, Li T,
Zhu G, Schones DE and Wang Z: Distinct roles of DNMT1-dependent and
DNMT1-independent methylation patterns in the genome of mouse
embryonic stem cells. Genome Biol. 16:1152015. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Hartmann S, Bergmann M, Bohle RM, Weidner
W and Steger K: Genetic imprinting during impaired spermatogenesis.
Mol Hum Reprod. 12:407–411. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Roberts AR, Blewitt ME, Youngson NA,
Whitelaw E and Chong S: Reduced dosage of the modifiers of
epigenetic reprogramming Dnmt1, Dnmt3L, SmcHD1 and Foxo3a has no
detectable effect on mouse telomere length in vivo. Chromosoma.
120:377–385. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Ray D, Wu A, Wilkinson JE, Murphy HS, Lu
Q, KluveBeckerman B, Liepnieks JJ, Benson M, Yung R and Richardson
B: Aging in heterozygous Dnmt1-deficient mice: Effects on survival,
the DNA methylation genes, and the development of amyloidosis. J
Gerontol A Biol Sci Med Sci. 61:115–124. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Matsuoka T, Kawai K, Ando S, Sugita S,
Kandori S, Kojima T, Miyazaki J and Nishiyama H: DNA
methyltransferase-3 like protein expression in various histological
types of testicular germ cell tumor. Jpn J Clin Oncol hyw012. 2016.
View Article : Google Scholar
|
|
78
|
Vlachogiannis G, Niederhuth CE, Tuna S,
Stathopoulou A, Viiri K, de Rooij DG, Jenner RG, Schmitz RJ and Ooi
SK: The Dnmt3L ADD Domain Controls Cytosine Methylation
Establishment during Spermatogenesis. Cell Rep. 15:S2211–S1247.
2015.
|
|
79
|
Liao HF, Chen WS, Chen YH, Kao TH, Tseng
YT, Lee CY, Chiu YC, Lee PL, Lin QJ, Ching YH, et al: DNMT3L
promotes quiescence in postnatal spermatogonial progenitor cells.
Development. 141:2402–2413. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Yiran Z, Meiling Z, Zhichao Z, Yunjiao Z
and Xin M: Epigenetic regulation of genomic imprinting in germline
cells and preimplantation embryos. Yi Chuan. 38:103–108. 2016.(In
Chinese). PubMed/NCBI
|
|
81
|
von Meyenn F and Reik W: Forget the
Parents: Epigenetic Reprogramming in Human Germ Cells. Cell.
161:1248–1251. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chaillet JR, Vogt TF, Beier DR and Leder
P: Parental-specific methylation of an imprinted transgene is
established during gametogenesis and progressively changes during
embryogenesis. Cell. 66:77–83. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Hajder M, Hajder E and Husic A: The
Effects of Total Motile Sperm Count on Spontaneous Pregnancy Rate
and Pregnancy After IUI Treatment in Couples with Male Factor and
Unexplained Infertility. Medical archives. 70:39–43. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Mintziori G, Kita M, Duntas L and Goulis
DG: Consequences of hyperthyroidism in male and female fertility:
Pathophysiology and current management. J Endocrinol Invest. Mar
8–2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Dupree JM, Dickey RM and Lipshultz LI:
Inequity between male and female coverage in state infertility
laws. Fertil Steril. Mar 5–2016.(Epub ahead of print). View Article : Google Scholar
|
|
86
|
Bolduc S, Fischer MA, Deceuninck G and
Thabet M: Factors predicting overall success: A review of 747
microsurgical vasovasostomies. Can Urol Assoc J. 1:388–394.
2007.PubMed/NCBI
|
|
87
|
Liang J, Zhang Y, Yu Y, Sun W, Jing J and
Liu R: Effect of chromosomal polymorphisms of different genders on
fertilization rate of fresh IVF-ICSI embryo transfer cycles. Reprod
Biomed Online. 29:436–444. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Oldereid NB, Hanevik HI, Bakkevig I,
Romundstad LB, Magnus Ø, Hazekamp J, Hentemann M, Eikeland SN,
Skrede S, Reitan IR, et al: Pregnancy outcome according to male
diagnosis after ICSI with non-ejaculated sperm compared with
ejaculated sperm controls. Reprod Biomed Online. 29:417–423. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Wosnitzer M, Goldstein M and Hardy MP:
Review of Azoospermia. Spermatogenesis. 4:e282182014. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
GuerreroBosagna C and Skinner MK:
Environmentally induced epigenetic transgenerational inheritance of
male infertility. Curr Opin Genet Dev. 26:79–88. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Komiya A, Kawauchi Y, Kato T, Watanabe A,
Tanii I and Fuse H: Sperm nuclear vacuoles in relation to acrosome
reactions and sperm motility. Scientific World Journal.
2014:1789702014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Xu AM, Liu BJ and Wang ZJ: DAZL and male
infertility: an update. Zhonghua Nan Ke Xue. 20:647–650. 2014.(In
Chinese). PubMed/NCBI
|
|
93
|
Khazaie Y and Nasr Esfahani MH: MicroRNA
and Male Infertility: A Potential for Diagnosis. Int J Fertil
Steril. 8:113–118. 2014.PubMed/NCBI
|
|
94
|
Barazani Y, Agarwal A and Sabanegh ES Jr:
Functional sperm testing and the role of proteomics in the
evaluation of male infertility. Urology. 84:255–261. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Komori K, Tsujimura A, Okamoto Y, Matsuoka
Y, Takao T, Miyagawa Y, Takada S, Nonomura N and Okuyama A:
Relationship between substances in seminal plasma and Acrobeads
Test results. Fertil Steril. 91:179–184. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Dada R, Kumar M, Jesudasan R, Fernández
JL, Gosálvez J and Agarwal A: Epigenetics and its role in male
infertility. J Assist Reprod Genet. 29:213–223. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Bhattacharyya T, Gregorova S, Mihola O,
Anger M, Sebestova J, Denny P, Simecek P and Forejt J: Mechanistic
basis of infertility of mouse intersubspecific hybrids. Proc Natl
Acad Sci USA. 110:E468–E477. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Pacheco SE, Houseman EA, Christensen BC,
Marsit CJ, Kelsey KT, Sigman M and Boekelheide K: Integrative DNA
methylation and gene expression analyses identify DNA packaging and
epigenetic regulatory genes associated with low motility sperm.
PLoS One. 6:e202802011. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Soubry A, Hoyo C, Jirtle RL and Murphy SK:
A paternal environmental legacy: Evidence for epigenetic
inheritance through the male germ line. BioEssays. 36:359–371.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Owen CM and Segars JH Jr: Imprinting
disorders and assisted reproductive technology. Semin Reprod Med.
27:417–428. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Childs AJ, Saunders PT and Anderson RA:
Modelling germ cell development in vitro. Mol Hum Reprod.
14:501–511. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Cortessis VK, Thomas DC, Levine AJ, Breton
CV, Mack TM, Siegmund KD, Haile RW and Laird PW: Environmental
epigenetics: Prospects for studying epigenetic mediation of
exposure-response relationships. Hum Genet. 131:1565–1589. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Berthaut I, Montjean D, Dessolle L, Morcel
K, Deluen F, Poirot C, Bashamboo A, McElreavey K and Ravel C:
Effect of temozolomide on male gametes: An epigenetic risk to the
offspring? J Assist Reprod Genet. 30:827–833. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Crews D: Epigenetics and its implications
for behavioral neuroendocrinology. Front Neuroendocrinol.
29:344–357. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Gabory A, Attig L and Junien C: Epigenetic
mechanisms involved in developmental nutritional programming. World
J Diabetes. 2:164–175. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Katari S, Turan N, Bibikova M, Erinle O,
Chalian R, Foster M, Gaughan JP, Coutifaris C and Sapienza C: DNA
methylation and gene expression differences in children conceived
in vitro or in vivo. Hum Mol Genet. 18:3769–3778. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Feuer SK, Camarano L and Rinaudo PF: ART
and health: Clinical outcomes and insights on molecular mechanisms
from rodent studies. Mol Hum Reprod. 19:189–204. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Zama AM and Uzumcu M: Epigenetic effects
of endocrine-disrupting chemicals on female reproduction: An
ovarian perspective. Front Neuroendocrinol. 31:420–439. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Niemitz EL and Feinberg AP: Epigenetics
and assisted reproductive technology: A call for investigation. Am
J Hum Genet. 74:599–609. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
110
|
Lee J and Shinohara T: Epigenetic
modifications and self-renewal regulation of mouse germline stem
cells. Cell Res. 21:1164–1171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Li L, Le F, Wang LY, Xu XR, Lou HY, Zheng
YM, Sheng JZ, Huang HF and Jin F: Normal epigenetic inheritance in
mice conceived by in vitro fertilization and embryo transfer. J
Zhejiang Univ Sci B. 12:796–804. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Wasson JA, Ruppersburg CC and Katz DJ:
Restoring totipotency through epigenetic reprogramming. Brief Funct
Genomics. 12:118–128. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Daxinger L and Whitelaw E:
Transgenerational epigenetic inheritance: More questions than
answers. Genome Res. 20:1623–1628. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Skinner MK: Environmental epigenomics and
disease susceptibility. EMBO Rep. 12:620–622. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kitamura A, Miyauchi N, Hamada H, Hiura H,
Chiba H, Okae H, Sato A, John RM and Arima T: Epigenetic
alterations in sperm associated with male infertility. Congenit
Anom (Kyoto). 55:133–144. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Marques CJ, Costa P, Vaz B, Carvalho F,
Fernandes S, Barros A and Sousa M: Abnormal methylation of
imprinted genes in human sperm is associated with oligozoospermia.
Mol Hum Reprod. 14:67–74. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Montjean D, Ravel C, Benkhalifa M,
CohenBacrie P, Berthaut I, Bashamboo A and McElreavey K:
Methylation changes in mature sperm deoxyribonucleic acid from
oligozoospermic men: Assessment of genetic variants and assisted
reproductive technology outcome. Fertil Steril. 100:1241–1247.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Kobayashi H, Hiura H, John RM, Sato A,
Otsu E, Kobayashi N, Suzuki R, Suzuki F, Hayashi C, Utsunomiya T,
et al: DNA methylation errors at imprinted loci after assisted
conception originate in the parental sperm. Eur J Hum Genet.
17:1582–1591. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Pliushch G, Schneider E, Schneider T, El
Hajj N, Rösner S, Strowski T and Haaf T: In vitro maturation of
oocytes is not associated with altered deoxyribonucleic acid
methylation patterns in children from in vitro fertilization or
intracytoplasmic sperm injection. Fertil Steril. 103:720–727. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Zheng HY, Shi XY, Wang LL, Wu YQ, Chen SL
and Zhang L: Study of DNA methylation patterns of imprinted genes
in children born after assisted reproductive technologies reveals
no imprinting errors: A pilot study. Exp Ther Med. 2:751–755.
2011.PubMed/NCBI
|
|
121
|
Xu J, Zhang A, Zhang Z, Wang P, Qian Y, He
L, Shi H, Xing Q and Du J: DNA methylation levels of imprinted and
nonimprinted genes DMRs associated with defective human
spermatozoa. Andrologia. Jan 25–2016.(Epub ahead of print).
View Article : Google Scholar
|