Introduction
Dengue is the most common arboviral disease that is
caused by dengue virus (1), and
occurs in Southeast Asia, East and West Africa, the Caribbean and
the Americas (2). Dengue fever and
dengue hemorrhagic fever are increasingly recognized diseases in
Asia (2). Various neurologic
complications of dengue viral infection have been reported,
including Guillain-Barré syndrome (GBS), encephalitis,
encephalopathy, myelitis, meningitis, acute disseminated
encephalomyelitis (ADEM), polyneuropathy, and facial and ulnar
mononeuropathy (3–6). However, the involvement of the spinal
cord and thyroid in patients infected with dengue has been rarely
reported. To the best of our knowledge, only 6 cases of transverse
myelitis in association with dengue infection have been previously
reported in the literature, one of which was complicated with
subacute thyroiditis. The present study describes the case of a
65-year-old patient who developed transverse myelitis complicated
with subacute thyroiditis 6 days following dengue infection. In
addition, the current study reviewed the previous relevant cases in
the literature in order to elucidate the pathogenesis of spinal
cord involvement in dengue viral infection.
Case report
A 65-year-old male patient presented at the Fourth
Affiliated Hospital of Guangzhou Medical University (Guangzhou,
China) in October 2014 with acute paraplegia and sensory loss. The
patient had experienced an acute onset of fever (39°C) 6 days
before admission; in addition, he had previously suffered from
myocardial infarction, and had undergone stent implantation 4
months prior to admission. Initial blood count analysis, performed
on admission, showed a normal total leukocyte count, a low platelet
count (98×109 cells/l), and positive dengue antigen and
IgM (Table I). At 4 days before
admission, the fever was resolved and the patient developed acute
paraplegia with sensory loss after 2 days.
 | Table I.Main biochemical results of exams
carried out in a patient with dengue and transverse myelitis. |
Table I.
Main biochemical results of exams
carried out in a patient with dengue and transverse myelitis.
|
|
Days after
admission |
|
|---|
|
|
|
|
|---|
| Parameter | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 12 | 39 | Reference value |
|---|
| Leukocytes,
×109/l | 8.7 | 7.76 | 9.07 | 11.18 | 10.01 | 11.29 | 7.63 | 7.58 | 5.33 | 6.98 | 3.5–9.5 |
| Platelets,
×109/l | 98 | 160 | 171 | 215 | 220 | 226 | 230 | 239 | 204 | 254 | 125–350 |
| Hematocrit, % | 39.7 | 36.5 | 38.8 | 38.3 | 36.2 | 34.4 | 35.3 | 33.6 | 38.5 | 35.7 | 40–50 |
| ALT, U/l | – | 23 | – | – | – | – | 29 | – | 28 |
| 9–60 |
| γ-GT, U/l | – | 46 | – | – | – | – | 28 | – | 35 |
| 10–60 |
| BUN, mmol/l | 4.1 | 2.5 | 3.8 | 4.9 | 5 | 5.7 | 6.4 | 6.8 | 7.1 | 3.8 | 2.86–8.2 |
| Creatinine,
µmol/l | 78 | 56 | 62 | 56 | 56 | 44 | 42.7 | 58 | 52 | 50 | 62–115 |
| Serum GLU,
mmol/l | 6.48 | 6.76 | 11.73 | 9.05 | 7.69 | 9.4 | 7.92 | 7.87 | 4.81 | 7.63 | 3.89–6.11 |
| FT3, pmol/l | 5.10 |
|
|
|
|
|
|
| 3.65 |
| 3.8–6 |
| FT4, pmol/l | 20.13 |
|
|
|
|
|
|
| 23.10 |
| 7.9–14.4 |
| hTSH, pmol/l | 0.09 |
|
|
|
|
|
|
| 0.29 |
| 0.34–5.6 |
| TGAb, % | 49.40 |
|
|
|
|
|
|
|
|
| 0–30 |
| TMAb, % | 31.70 |
|
|
|
|
|
|
|
|
| 0–20 |
| TPOAb, U/ml | 33.77 |
|
|
|
|
|
|
|
|
| 0–34 |
| Tg, ng/ml | 1.72 |
|
|
|
|
|
|
|
|
| 3.5–77 |
| TRAb, U/l | 0.59 |
|
|
|
|
|
|
|
|
| <1.75 |
| TBG, µg/ml | 9.96 |
|
|
|
|
|
|
|
|
| 13–39 |
| DENV-Ag | (+) |
|
|
|
| (−) |
|
| (−) | (−) | Negative |
| DENV-IgM | (+) |
|
| (+) |
|
|
|
| (+) | (+) | Negative |
| DENV-IgG | (−) |
|
|
|
|
|
|
| (+) | (+) | Negative |
| CSF WBC,
×106/l |
|
| 24.8 |
| 8 |
|
|
|
| 1 | 0–8 |
| CSF TP, mg/l |
|
| 791 |
| 303 |
|
|
|
| 386 | 150–450 |
| CSF GLU,
mmol/l |
|
| 4.49 |
| 4.58 |
|
|
|
| 3.23 | 2.5–4.5 |
| CSF ADA, U/l |
|
| 0.2 |
| 0.3 |
|
|
|
| 4.2 | 0–5 |
| CSF DENV-IgM |
|
| (−) |
| (−) |
|
|
|
| (−) | Negative |
| CSF DENV-IgG |
|
| (−) |
| (−) |
|
|
|
| (−) | Negative |
| CSF DENV-Ag |
|
| (−) |
| (−) |
|
|
|
| (−) | Negative |
Neurological evaluation at admission by manual
muscle testing (7), revealed grade
4/5 flaccid paralysis of the lower limbs with an absence of knee
and ankle jerk reflexes. In the 2 days after admission, the patient
developed muscle strength of grade 1/5 in the bilateral lower
limbs, as well as T4-level sensory deficit followed by acute
urinary retention. However, examination of the upper extremities,
cranial nerves, cerebellum and neck showed no remarkable finding.
Weakness of lower limbs was gradually aggravated, reaching grade
0/5 by 4 day of admission.
Serological testing for anti-human immunodeficiency
virus antibodies with the Venereal Disease Research Laboratory test
was negative. Immunological testing for anti-dengue IgM/IgG and
dengue antigen in the serum at admission were positive; however,
these were negative in the cerebrospinal fluid (CSF) on days 2 and
4 after admission. NMDA receptor for encephalitis and aquaporin 4
antibodies were negative in both the serum and CSF. The visual
evoked potential (VEP) was also negative.
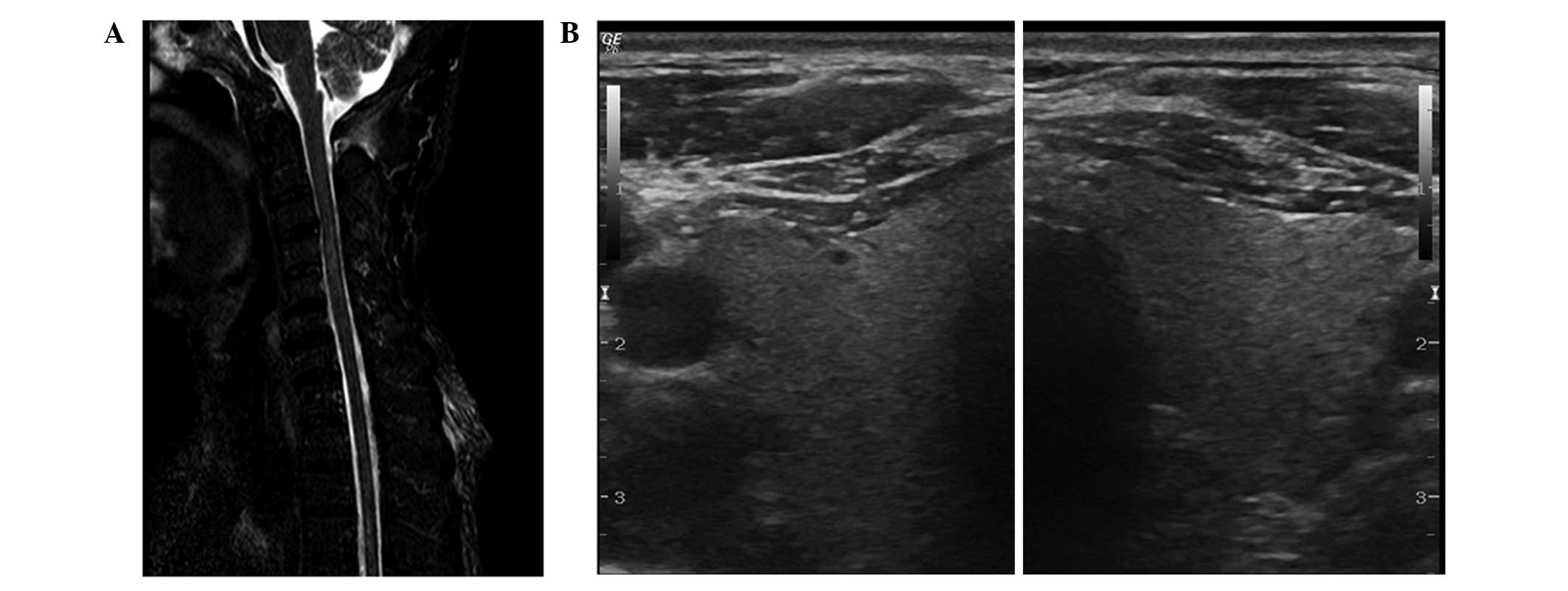
Magnetic resonance imaging (MRI) of the cervical
spinal cord was performed on day 5 after admission and showed
hypersignal intensity on T2 weighted images at C3-C5 (Fig. 1A). CSF analysis on day 2 of admission
revealed a clear fluid with a pressure of 14 cmH2O and a
leukocyte count of 24.8×106 cells/l, including 45%
mononuclear cells and 55% polynuclear cells. In addition, the CSF
glucose and total protein levels were 4.49 mmol/l and 791 mg/l,
respectively. CSF cultures were negative for bacteria and fungi.
Furthermore, serological analyses on admission revealed increased
FT4, thyroglobulin antibody (TGAb) and thyroid microsomal antibody
(TMAb) levels, as well as reduced human thyroid-stimulating hormone
(hTSH), thyroglobulin (Tg) and thyroxine-binding globulin (TBG)
levels. However, no antinuclear, anti-double stranded DNA and
anti-ganglioside antibodies were detected, and a thyroid ultrasound
test, conducted on day 5 of admission, was negative (Fig. 1B).
According to the aforementioned findings, the
patient was diagnosed with acute transverse myelitis complicated
with subacute thyroiditis in association with a dengue viral
infection. The patient was treated with intravenous pulse
methylprednisolone (1 g/day; Pfizer Manufacturing NV, Puurs,
Belgium) and immunoglobulin (20 g/day; Shuanglin Biological
Pharmaceutical Co., Ltd., Zhanjiang, China) for 5 consecutive days
from day 5 of admission. After 1 month of treatment, an MRI scan of
the cervical spinal cord demonstrated a decreased high-intensity
signal (Fig. 2) compared with the
value at admission. CSF analysis showed a leukocyte count of
8×106 cells/l, glucose level of 3.23 mmol/l and total
protein of 386 mg/l.
At 3 months after the onset of symptoms, the
patient's lower limbs were graded as 1/5 after receiving intensive
physiotherapy. The patient presented a T12-level sensory deficit
and the sphincter function was normal; however, little improvement
was observed after 4 months of follow-up.
Written informed consent for this case report was
obtained from the patient's family. Approval for this study was
provided by the Ethics Committee of the Fourth Affiliated Hospital
of Guangzhou Medical University.
Discussion
Dengue is an infectious disease caused by a
flavivirus that results in a spectrum of clinical presentations
from subclinical to dengue hemorrhagic fever, and subsequently
dengue shock syndrome. The neurological complications of dengue
include para-infectious encephalitis, GBS and ADEM; however,
transverse myelitis is rarely involved. In the present study, a
literature review identified 6 reported cases (8–13) of
transverse myelitis attributed to dengue infection between 1996 and
2014, in addition to the present case. Table II provides an overview of the
current and previous cases. The PubMed database (www.ncbi.nlm.nih.gov/pubmed) was searched for
‘transverse myelitis/TM’ and ‘dengue’, and full-text versions of
all cases were carefully analyzed. Studies involving central
nervous neurological disorders that did not report appropriate
medical evidence were excluded. All patients in the current and 6
previous studies had recently experienced dengue infection, with 6
adult and 1 pediatric cases identified (8–13). The
time lag between infection and transverse myelitis symptoms varied
between 3 and 16 days (mean, 7 days). As shown in Table II, among the 6 previous cases, there
were 2 Singaporean patients (8,9), 1 Thai
(10), 1 Malaysian Chinese (11) and 2 Japanese (12,13).
Cases initially considered to be dengue were admitted with various
neurological symptoms, including spastic paraparesis (in 1 case)
and flaccid paraparesis (6 cases). However, not all patients
experienced typical dengue hemorrhagic fever and dengue shock
syndrome prior to the onset of neurological symptoms. A careful
analysis of the reported cases did not reveal any predisposing
factor for the illness. All patients were found to have a low
platelet count and dengue infection. In 4 out of 7 cases [the
current case plus 3 others (9,10,12)] MRI
of the spinal cord was used to confirm the diagnosis, and
hyperintensity in T2-weighted images supported the diagnosis of
transverse myelitis. Furthermore, CSF analysis revealed signs of
inflammation. Intravenously administered Ig methylprednisolone
and/or plasmapheresis were the preferential treatments in 4 of the
7 cases [methylprednisolone in 2 cases (8,10),
plasmapheresis in 1 case (12), and
Ig methylprednisolone plus plasmapheresis in the present case). In
total, 5 patients recovered completely (8–11,13).
However, the case reported in the present study showed a partial
recovery at 3 months post-infection.
 | Table II.Patient demographics in the current
and previous cases of dengue fever with acute transverse myelitis
and subacute thyroiditis. |
Table II.
Patient demographics in the current
and previous cases of dengue fever with acute transverse myelitis
and subacute thyroiditis.
| Authors | Year | Age
(years)/gender | Country | Dengue infection
onset (days)a | Manifestations | MRI | Treatment | Clinical
outcomes | Ref. |
|---|
| Seet et
al | 2006 | 44/F | Singapore | 16 | Spastic paraparesis
(T5 level) | Normal |
Methylprednisolone | Recovery 3 months
later |
(8) |
| Larik et
al | 2012 | 43/M | Singapore | 6 | Flaccid paraparesis
(T4 level) | C2-T9 | IVIg | Recovery 6 weeks
later |
(9) |
| Chanthamat et
al | 2010 | 61/F | Thailand | 6 | Flaccid paraparesis
(T10 level) | T9-10 |
Methylprednisolone | Recovery 1 year
later | (10) |
| Renganathan et
al | 1996 | 14/F | China | 7 | Flaccid paraparesis
(T5-6 level) | Normal | Systemic
treatment | Recovery 2 weeks
later | (11) |
| Kunishige et
al | 2004 | 42/M | Japan | 3 | Flaccid paraparesis
(T6 level) | C6-L2 | IVIg;
plasmapheresis | Improved 2 months
later | (12) |
| Leão et
al | 2002 | 58/M | Japan | 5 | Flaccid paraparesis
(unspecified) | Normal | Ceftriaxone | Recovery 6 months
later | (13) |
| Current case | 2014 | 65/M | China | 6 | Flaccid paraparesis
(T4 level) | C3-5 | IVIg;
methylprednisol; plasmapheresis | Improved 3 months
later | – |
In the current patient, transverse myelitis was
diagnosed based on the following typical symptoms: Transiently
decreased platelet count, positive dengue antigen and IgM/IgG, and
according to the features of an MRI scan of the spinal cord. To the
best of our knowledge, the current study reported the first case
suffering from transverse myelitis combined with dengue fever in
mainland China.
Dengue is endemic in Southeast Asia, East and West
Africa, the Caribbean and the Americas (2). However, all the cases reported in the
literature involve Asian patients. Therefore, the Asian population
appears to be prone to autoimmune injury of the spinal cord.
Thrombocytopenia occurred in all previously reported cases, with
the exception of the case described by Larik et al (9). However, normal leukocyte count was
obtained in 5 cases of transverse myelitis (8,10–12). The
possible pathogenesis may be due to superinfection or co-infection,
including urinary tract infection, blood-stream infection and
pneumonia. Notably, leukocytosis was identified as a sign of severe
dengue infection in a Taiwanese study (14); however, it cannot be ruled out that
spinal cord injury was caused directly by dengue virus. According
to the comparison of cases shown in Table II, para-infectious transverse
myelitis also appears to be associated with flaccid paraparesis,
while post-infectious myelitis may be associated with spastic
paraparesis.
Thyroid involvement in dengue has been rarely
reported. Subacute thyroiditis has been suggested to be a
complication of expanded dengue syndrome (15). The present study detected increased
FT4, TGAb and TMAb levels, as well as reduced hTSH, Tg and TBG
levels in the patient, without any history of thyroiditis, which is
as an autoimmune disease. Transverse myelitis has been shown to be
associated with autoimmune reaction post-infection (3,16).
Furthermore, abnormal thyroid function is presumed to be caused by
viral infection or by an inflammatory process, and multiple cases
have suggested its association with coxsackievirus infection,
mumps, measles, adenovirus and dengue viral infection (17–20).
The mechanisms of viral transmission and neuronal
injury induced by dengue virus are relatively unknown. In the early
stages, a direct pathogenic effect of dengue virus on neural
tissues is indicated by the presence of viral antigen in the CSF
(12). All cases identified by the
literature review, as well as the present case, failed to display
presence of dengue IgM/IgG or antigen in the CSF, with the
exception of the two cases reported by Kunishige et al
(12) and Seet et al
(8). Therefore, direct infection and
post-infectious immune injury in dengue are suggested to be
associated with transverse myelitis. Overall, the current findings
confirm that dengue infection can result in autoimmune diseases,
particularly in the spinal cord and thyroid; the cause-and-effect
association between dengue infection and acute transverse myelitis
was likely established in the present case. However, further
studies are required to elucidate the underlying mechanisms of this
association.
In conclusion, the case presented in the current
study suggests that acute transverse myelitis with subacute
thyroiditis may be a result of dengue infection. This diagnosis
should be considered in patients who develop central nervous system
manifestations during or after the recovery period of dengue
infection. Since methylprednisolone and immunoglobulin are
effective during the active phase, prompt diagnosis and initiation
of treatment are crucial.
References
|
1
|
Murthy JM: Neurological complication of
dengue infection. Neurol India. 58:581–584. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gulati S and Maheshwari A: Atypical
manifestations of dengue. Trop Med Int Health. 12:1087–1095. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Solomon T, Dung NM, Vaughn DW, Kneen R,
Thao LT, Raengsakulrach B, Loan HT, Day NP, Farrar J, Myint KS, et
al: Neurological manifestations of dengue infection. Lancet.
355:1053–1059. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Misra UK, Kalita J, Syam UK and Dhole TN:
Neurological manifestations of dengue virus infection. J Neurol
Sci. 244:117–122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Soares CN, Faria LC, Peralta JM, de
Freitas MR and Puccioni-Sohler M: Dengue infection: Neurological
manifestations and cerebrospinal fluid (CSF) analysis. J Neurol
Sci. 249:19–24. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
de Sousa A Miranda, Puccioni-Sohler M,
Dias Borges A, Adorno L Fernandes, Alvarenga M Papais and Alvarenga
RM Papais: Post-dengue neuromyelitis optica: Case report of a
Japanese-descendent Brazilian child. J Infect Chemother.
12:396–398. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Williams M: Manual muscle testing,
development and current use. Phys Ther Rev. 36:797–805.
1956.PubMed/NCBI
|
|
8
|
Seet RC, Lim EC and Wilder-Smith EP: Acute
transverse myelitis following dengue virus infection. J Clin Virol.
35:310–312. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Larik A, Chiong Y, Lee LC and Ng YS:
Longitudinally extensive transverse myelitis associated with dengue
fever. BMJ Case Rep. 2012.pii:bcr1220115378. 2012.
|
|
10
|
Chanthamat N and Sathirapanya P: Acute
transverse myelitis associated with dengue viral infection. J
Spinal Cord Med. 33:425–427. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Renganathan A, Ng WK and Tan CT:
Transverse myelitis in association with dengue infection. Neurol J
Southeast Asia. 1:61–63. 1996.
|
|
12
|
Kunishige M, Mitsui T, Tan BH, Leong HN,
Takasaki T, Kurane I, Mihara A and Matsumoto T: Preferential gray
matter involvement in dengue myelitis. Neurology. 63:1980–1981.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Leão RN, Oikawa T, Rosa ES, Yamaki JT,
Rodrigues SG, Vasconcelos HB, Sousa MRS, Tsukimata JK, Azevedo RSS
and Vasconcelos PFC: Isolation of dengue 2 virus from a patient
with central nervous system involvement (transverse myelitis). Rev
Soc Bras Med Trop. 35:401–404. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee IK, Liu JW and Yang KD: Fatal dengue
hemorrhagic fever in adults: Emphasizing the evolutionary pre-fatal
clinical and laboratory manifestations. PLoS Negl Trop Dis.
6:e15322012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Assir MZ, Jawa A and Ahmed HI: Expanded
dengue syndrome: Subacute thyroiditis and intracerebral hemorrhage.
BMC Infect Dis. 12:2402012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sindic CJ, Van Antwerpen MP and Goffette
S: The intrathecal humoral immune response: Laboratory analysis and
clinical relevance. Clin Chem Lab Med. 39:333–340. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lazarus JH: Silent thyroiditis and
subacute thyroiditisWerner & Ingbar's The Thyroid: A
Fundamental and Clinical Text. Braverman LE and Utiger RD: 7th.
Lippincott-Raven; Philadelphia, PA: pp. 577–591. 1996
|
|
18
|
Desailloud R and Hober D: Viruses and
thyroiditis: An update. Virol J. 6:52009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Eylan E, Zmucky R and Sheba C: Mumps virus
and subacute thyroiditis; Evidence of a causal association. Lancet.
272:1062–1063. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Felix-Davies D: Autoimmunisation in
subacute thyroiditis. Lancet. 1:880–883. 1958. View Article : Google Scholar : PubMed/NCBI
|