Introduction
Vascular dementia (VD) is the second most common
type of dementia after Alzheimer's disease (1,2). It is
predicted that by the year 2040, the number of people with dementia
worldwide will reach 81.1 million, with the number of dementia
patients in China being the sum of all those in all the developed
countries combined (3). The
progressive nature of VD leads to an unremitting and largely
irreversible deterioration in quality of life, and places a heavy
emotional and economic burden on families (4). However, currently there are no drugs
licensed for the treatment of vascular cognitive impairment. Thus,
there is an urgent requirement to develop therapeutic agents to
prevent vascular dementia.
VD is caused by a reduced blood flow to the brain or
an impaired vascular system (5). As
the population ages and cerebrovascular disease prevalence
increases, the occurrence of VD increases as well (6). Etiopathogenic mechanisms causing VD
include oxidative stress, cytotoxicity of reactive oxygen species,
mitochondrial dysfunction and apoptosis (7,8). The rat
bilateral common carotid artery occlusion (BCCAO) model is the most
common model used to investigate the effect of chronic cerebral
hypoperfusion-induced cognitive dysfunction, and is used to screen
drugs with potential therapeutic value for VD (9). Reduced blood flow can result in
neuronal energy failure and promote the production of reactive
oxygen species, which initiate neuronal apoptosis and lead to the
functional deficits typical of VD (10).
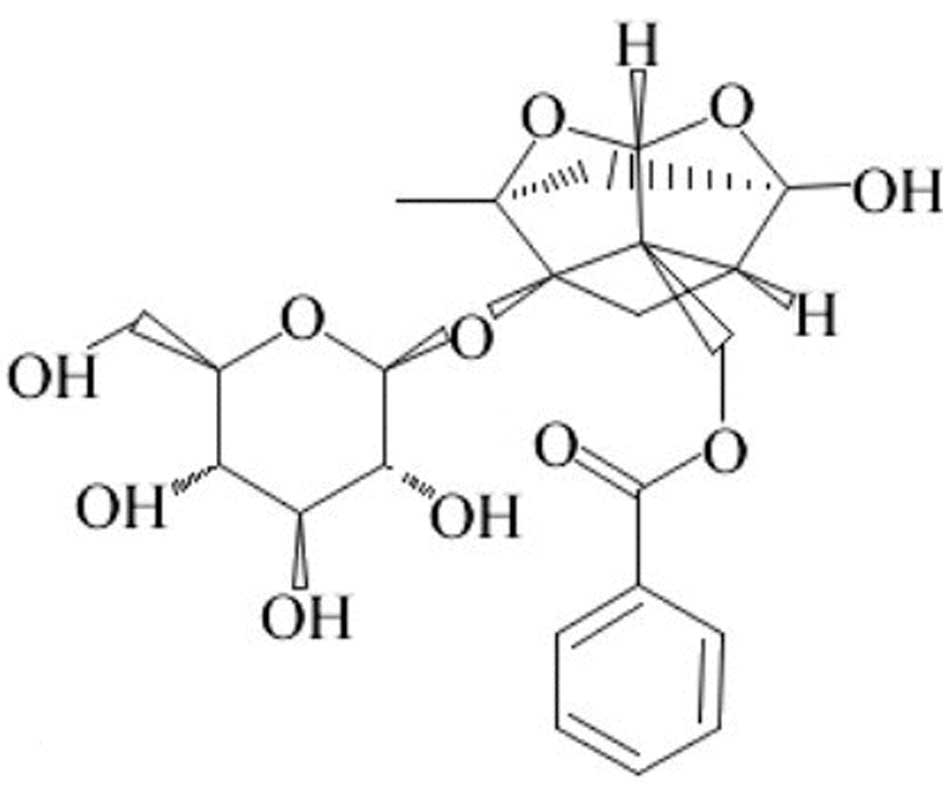
Paeoniflorn (PF) (Fig.
1) is the principal bioactive component of Paeoniae
radix which has been used for >1,000 years in traditional
Chinese medicine (11). In modern
pharmacological studies, PF exhibits numerous pharmacological
effects such as anti-inflammation, antioxidant,
endothelium-dependent vasorelaxation, neuromuscular blocking and
cognition enhancement properties (12,13).
Xiao et al (14) demonstrated
that PF is able to reverse, or alleviate, impairments. such as
cerebral infarction, neurological symptoms, tongue protrusion and
performance in the water maze, at the chronic stage of transient
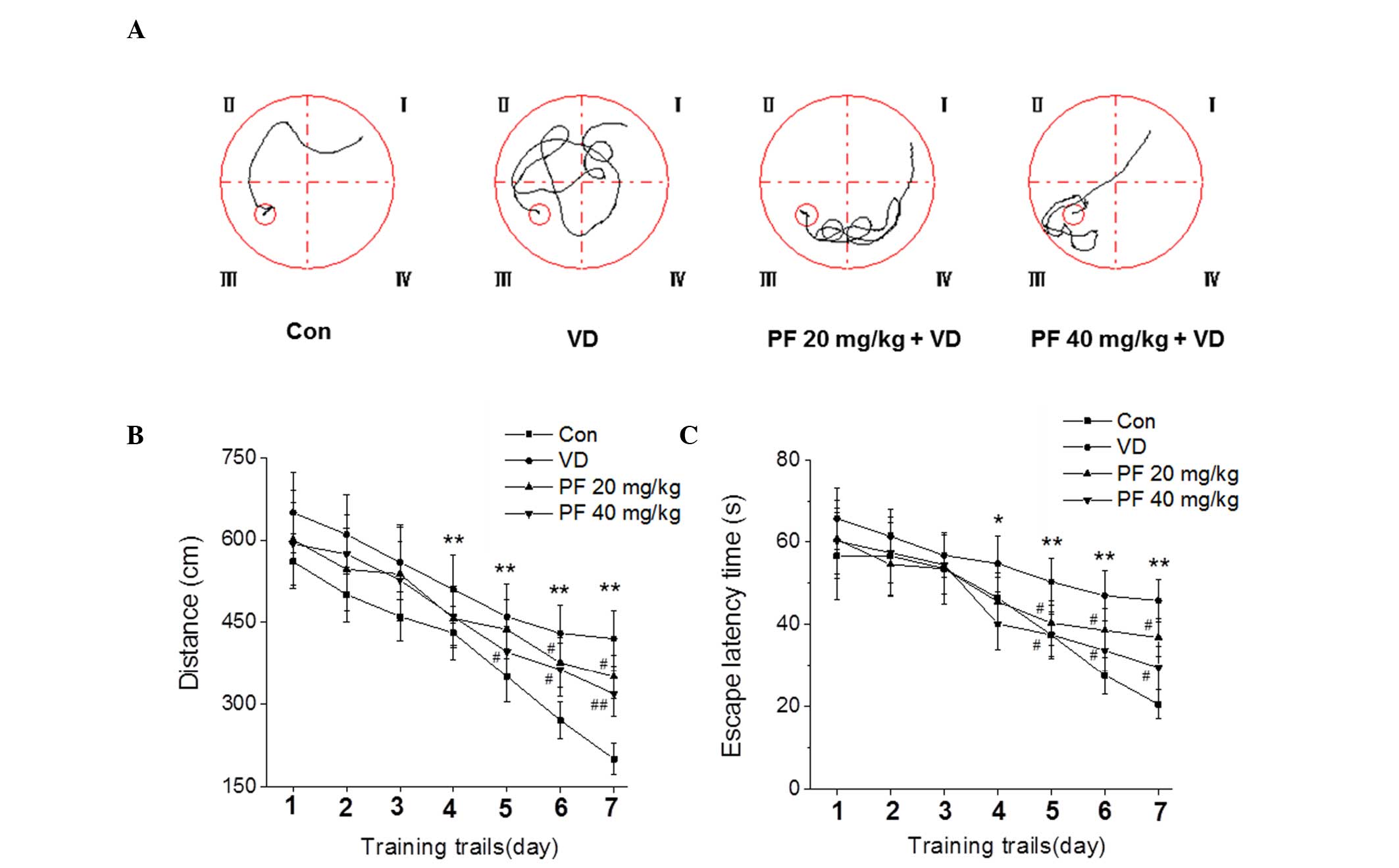
middle cerebral artery occlusion in rats. Our previous studies have
demonstrated that PF significantly attenuates memory impairment in
BCCAO model rats (unpublished; Fig.
2) (15); however, the molecular
mechanisms underlying the protective effects of PF on VD have not
been clearly identified. Therefore, the present study focuses on
evaluating the neuroprotective effect of PF and its relation to
cell apoptosis in a BCCAO rat model.
Materials and methods
Animals
Male Sprague Dawley rats (16–18 months old; 300–450
g body weight) were obtained from the Vital River Laboratories
(Beijing, China). Animals were housed with ad libitum access
to food and water at a temperature of 22±2°C, humidity of 55±5% and
a 12-h light/dark cycle. The study was performed in strict
accordance with the recommendations in the Guide for the Care and
Use of Laboratory Animals of the National Institutes of Health
(16). The protocol was approved by
the Committee on the Ethics of Animal Experiments of the National
Research Institute of Family Planning.
Reagents
PF (purity >98%) was purchased from Shandong
Zhongxing Guangrun Biotechnology Co., Ltd. (Nanjing, China). The
following primary antibodies were used in western blot analysis:
Anti-neuron-specific endolase (NSE) (sc-292097), anti-S100β
(sc-28533), anti-brain-derived neurotrophic factor (BDNF)
(sc-20981), anti-B-cell lymphoma 2 (Bcl-2) (sc-492), anti-Bcl-2
associated X protein (Bax) (sc-493) and anti-cytochrome c
(sc-7159) (all from Santa Cruz Biotechnology, Inc., Dallas, TX,
USA).
Study design
PF and saline were administered by oral gavage daily
for 28 days. Rats were randomized into the following four groups
prior to surgery, according to a computer-generated randomization
schedule (n=10 for each group): i) Control group; ii) VD group: VD
+ saline (2 ml/kg, once daily for 28 days); iii) low dose PF group:
VD + PF (20 mg/kg, once daily for 28 days); and iv) high dose PF
group: VD + PF (40 mg/kg, once daily for 28 days).
Establishment of vascular
dementia
Rats were deeply anesthetized with mebumal sodium
(50 mg/kg) by intraperitoneal injection. A midline incision was
made to expose the bilateral common carotid arteries. The common
carotid arteries were carefully separated from the surrounding
tissues, including the vagus nerve, and ligated with 4-0 silk
suture (Johnson&Johnson Medical Ltd., Wokingham, UK). The
control rats were subjected to the same surgical procedure without
occlusion of the arteries. During surgery, rectal temperatures were
maintained at 37±0.5°C with a thermostatically controlled warming
plate (Harvard Apparatus, Holiston, MA, USA).
Collection and preservation of brain
tissues
After 28 days of BCCAO, the rats were anesthetized
with 10% chloral hydrate (350 mg/kg, i.p.) and then decapitated.
The brain was rapidly removed and dissected on ice to obtain the
hippocampus. All brain tissues were stored at −80°C until further
biochemical analysis.
Western blot analysis
The isolated hippocampus were homogenized in lysis
buffer [10 mM Tris (Tocris Bioscience, Bristol, UK) (pH 7.4), 100
mM NaCl (Sinopharm Chemical Reagent Beijing Co., Ltd., Beijing,
China), 1 mM ethylenediamine-N,N,N',N'-tetraacetic acid (Tocris
Bioscience), 1 mM
ethyleneglycol-bis(2-aminoethyl)-N,N,N',N'-tetraacetic acid (Tocris
Bioscience), 1 mM NaF (Sinopharm Chemical Reagent Beijing Co.,
Ltd.), 20 mM Na4P2O7 (Sinopharm
Chemical Reagent Beijing Co., Ltd.), 2 mM
Na3VO4 (Sinopharm Chemical Reagent Beijing
Co., Ltd.)], 0.1% sodium dodecyl sulfate (SDS), 0.5% sodium
deoxycholate (Sinopharm Chemical Reagent Beijing Co., Ltd.), 1%
Triton-X 100 (Amresco LLC, Clevelan, OH, USA), 10% glycerol
(Sinopharm Chemical Reagent Beijing Co., Ltd.), 1 mM
phenylmethylsulfonyl fluoride (made from a 0.3 M stock in
dimethylsulfoxide; Tocris Bioscience), 60 µg/ml aprotinin (Santa
Cruz Biotechnology Inc.), 10 µg/ml leupeptin (Santa Cruz
Biotechnology Inc.), and 1 µg/ml pepstatin (Santa Cruz
Biotechnology Inc.)] for 30 min. The soluble fraction was obtained
by centrifugation at 3,000 × g for 10 min. Protein concentration
was determined using a bicinchoninic acid protein assay (Pulilai,
Beijing, China). Equal amounts of protein (40 µg) were boiled at
100°C for 10 min in loading buffer (Fermentas, Beijing, China) and
were separated in 8–10% SDS-polyacrylamide gel, and
electrotransferred onto a polyvinylidene difluoride membrane
(Bio-Rad, Hercules, CA, USA). The membrane was blocked with 5%
non-fat milk in 1X Tris-buffered saline [TBS; 10 mM Tris-HCl
(Tocris Bioscience and Sinopharm Chemical Reagent Beijing Co. Ltd.)
(pH 8.0), 150 mM NaCl (Sinopharm Chemical Reagent Beijing Co.,
Ltd.)] and 0.1% Tween-20 (TBST; Santa Cruz Biotechnology Inc.) at
25°C for 1 h and subsequently incubated overnight at 4°C with the
following primary antibodies: Anti-NSE (1:500), anti-S100β (1:500),
anti-BDNF (1:500), anti-Bcl-2 (1:1,000), anti-Bax (1:1,000) and
anti-cytochrome c (1:1,000). The membranes were then washed
twice with TBST and probed with the corresponding secondary
antibodies conjugated with horseradish peroxidase (sc-2004/sc-2005;
HRP; 1:5,000; Santa Cruz Biotechnology Inc.) (anti-mouse/rabbit-HRP
was used at a dilution of 1:5,000) at 25°C for 1 h. Following the
washes, the blots were developed using an enhanced
chemiluminescence system (Amersham ECL plus, GE Healthcare
Bio-Sciences, Pittsburgh, PA, USA). The bands were visualized by
exposure to X-ray film (X-Omat films, Kodak, Rochester, NY, USA).
Anti-β-actin antibody (sc-130656; 1:2,000; Santa Cruz Biotechnology
Inc.) was used as a loading control. All samples were analyzed at
least in triplicate.
Statistical analysis
The Morris water maze (15) was used to evaluate spatial memory
functioning following the treatment. As described in the previous
study (17), the water maze
apparatus was a circular pool (50 cm height, 150 cm diameter) with
a black inner wall, which was filed with water to 28 cm and
maintained at 22–25°C. The pool was divided into four quadrants
(I–IV) according to four equal distance points on the inner wall.
Furthermore, an escape platform painted black (26 cm height, 15 cm
diameter) was submerged 2.0 cm under the water surface. The rats
were given 4 trials per day for 4 days. The trials began as the rat
was placed in the pool facing the side wall at a start position and
ended once the animal found the platform. In cases where the rat
did not find the platform within 90 sec, it was guided there.
Following a period of 20 sec on the platform, the rat was
immediately placed again in the pool at a different starting
position for the next trial. The swimming traces of the rats were
recorded by a camera suspended over the center of the pool. The
escape latency and swimming distance of the rats were monitored by
a computerized tracking system (Chinese Academy of Medical
Sciences, Beijing, China).
The Morris water maze was performed with repeated
measures and analyzed by two-way analysis of variance followed by a
Bonferroni multiple group comparison. Statistical analysis of other
data was performed by one-way analysis of variance followed by a
post-Tukey test. For all statistical analyses, a standard software
package (Statistical Analysis Software, version 10.0; SAS
Institute, Cary, NC, USA) was used. All data are presented as the
mean ± standard error. P<0.05 was considered to indicate a
statistically significant difference.
Results
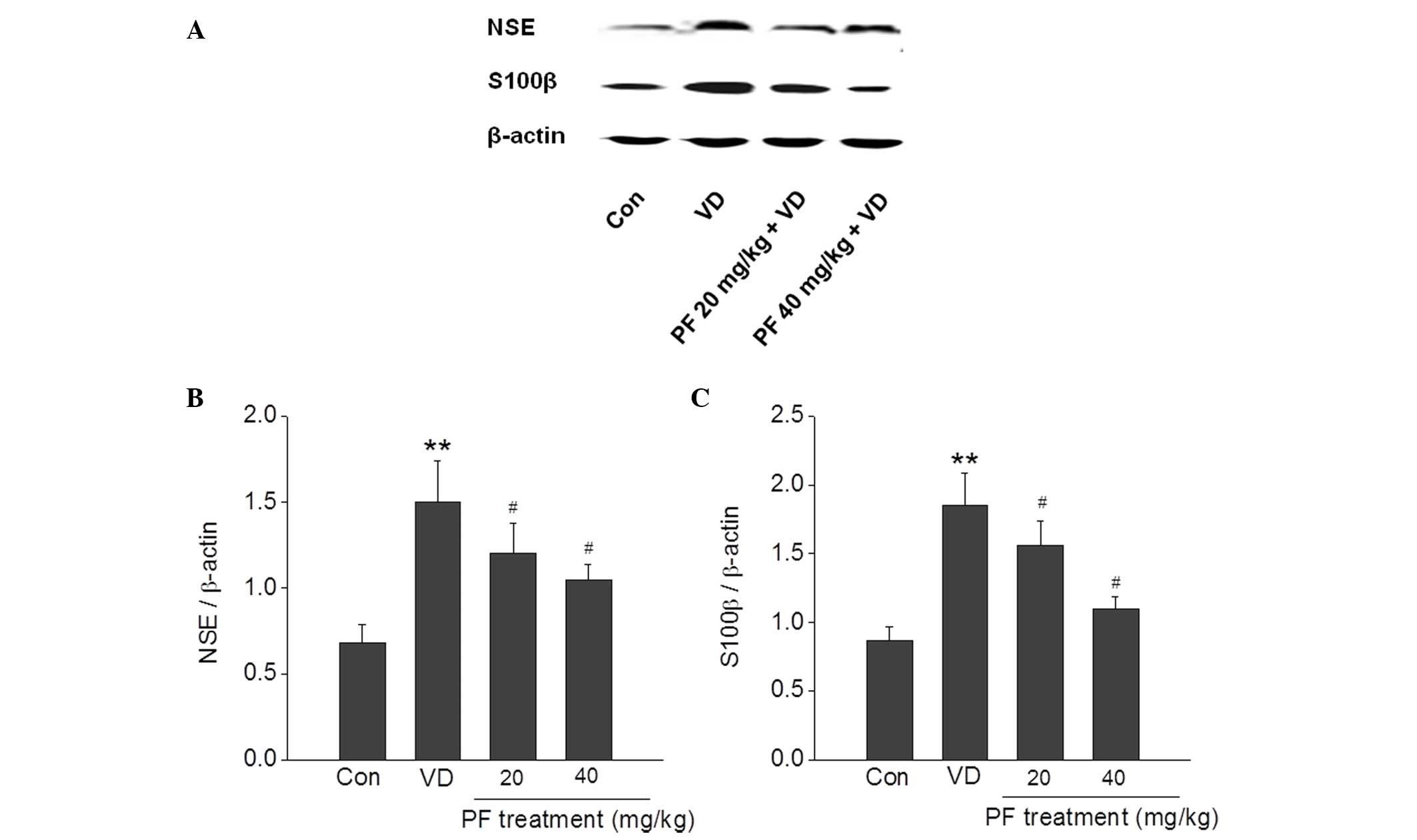
PF prevents NSE and S100β activation
in the hippocampus
A substantial increase in the expression of NSE and
S100β activity following VD has been reported. The results of the
present study demonstrated that NSE and S100β were significantly
increased in the VD group compared with the control group. PF (20
and 40 mg/kg) significantly reversed this increase in expression of
NSE and S100β in the VD group (P<0.05) (Fig. 3).
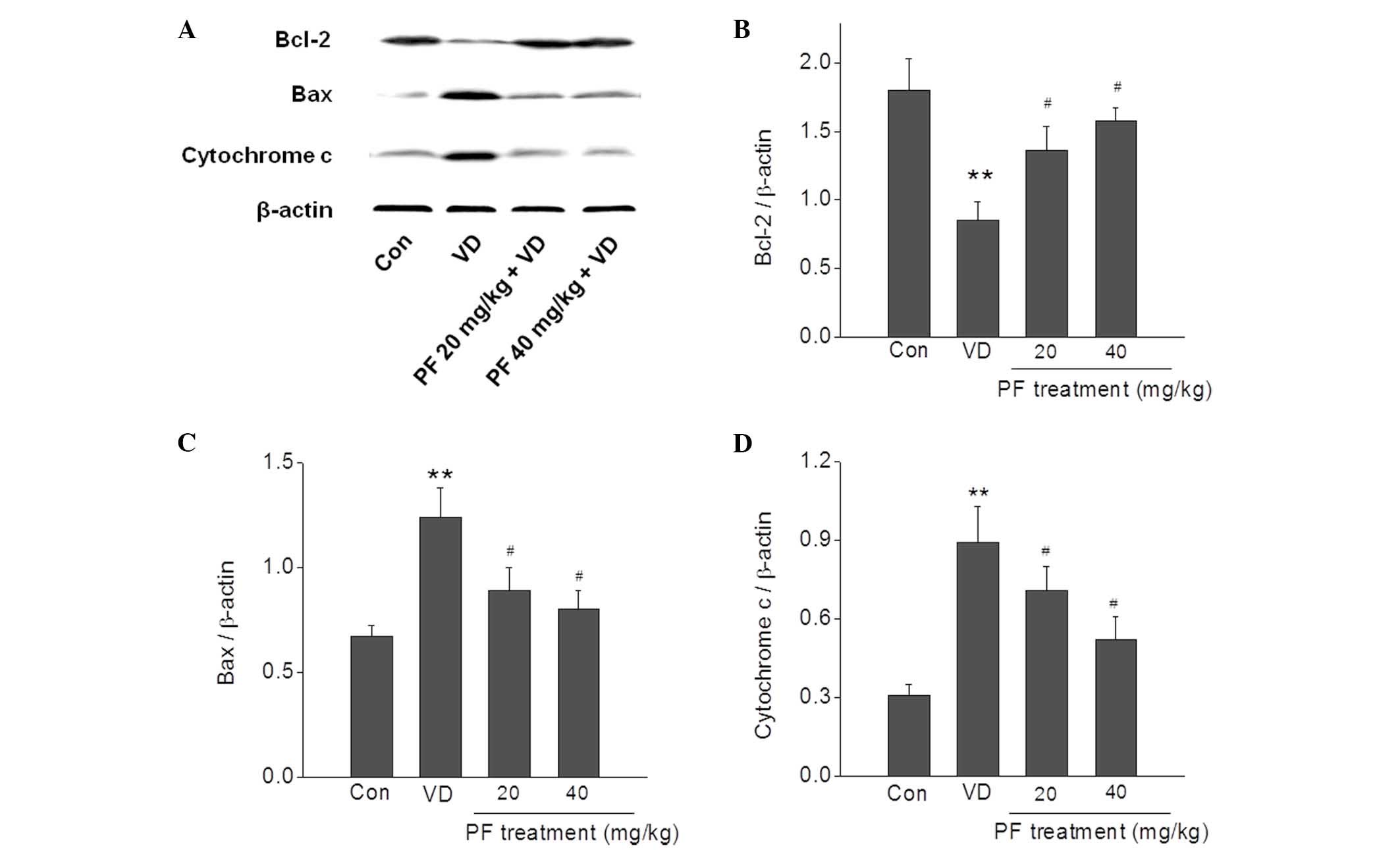
PF regulates apoptosis-related protein
expression in the hippocampus
The effects of PF treatment on VD-induced
apoptosis-related proteins were examined. The expression levels of
Bax and cytochrome c were significantly increased in the VD
group compared with the control group (P<0.01), and this was
significantly reversed by treatment with PF (20 and 40 mg/kg;
P<0.05). In addition, the expression level of Bcl-2 was
significantly decreased in the VD group compared with the control
group (P<0.01), and treatment with PF (20 and 40 mg/kg)
significantly reversed this decrease in expression level
(P<0.05) (Fig. 4).
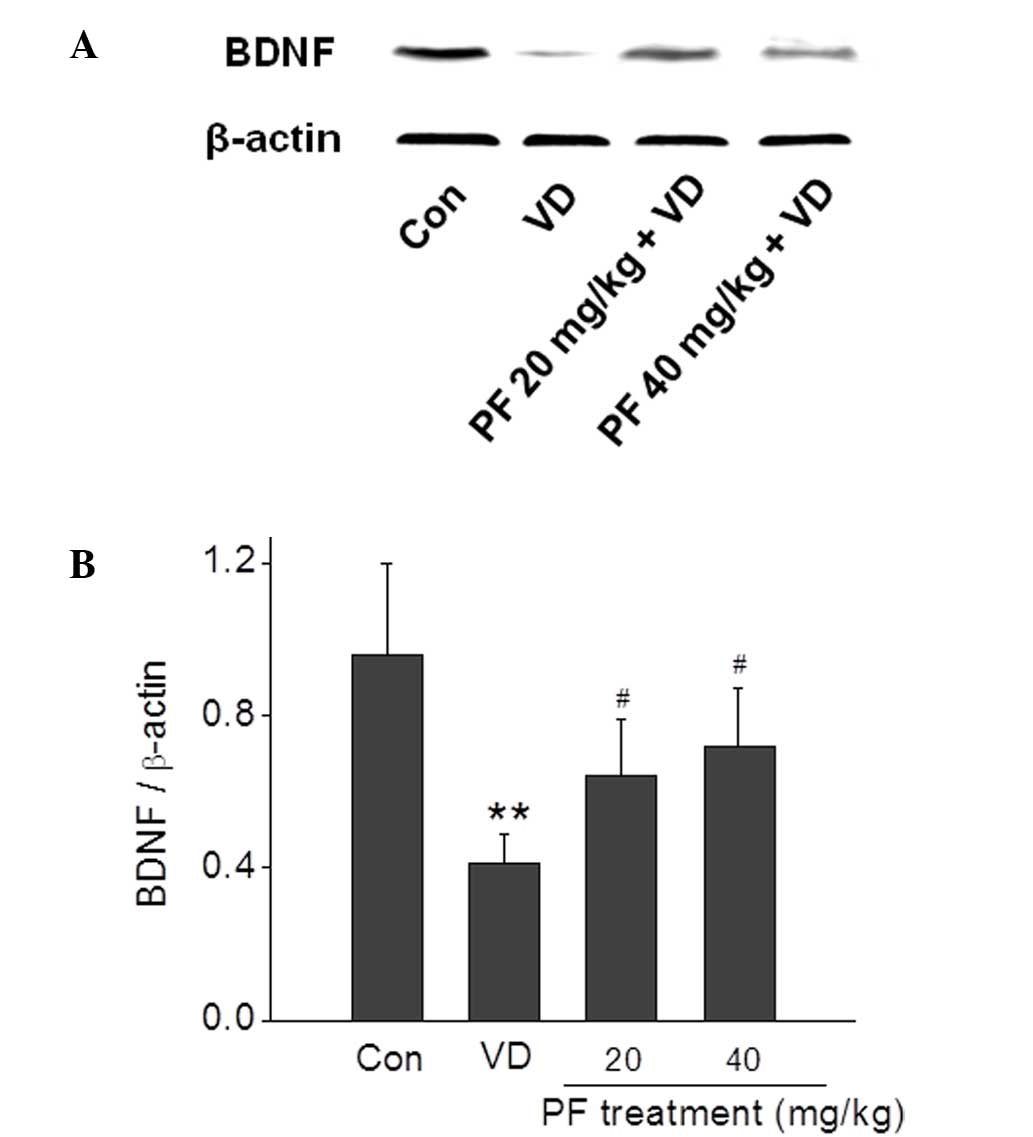
PF upregulates BDNF expression levels
in the hippocampus
BDNF protein expression levels in the hippocampus
were quantified using western blotting (Fig. 5). The results demonstrated that the
BDNF expression level in the VD group was significantly reduced
compared with the control group. Treatment with PF (20 and 40
mg/kg) significantly reversed this decrease in BDNF expression
level (P<0.05).
Discussion
Cognitive impairment is a key feature of VD. The
hippocampus is highly associated with learning and memory, and is
one of the brain regions that is most sensitive to hypoxia and
reactive oxygen species. Therefore, the hippocampus is thought to
be the primary target brain region of BCCAO-induced damage
(18). In the present study, the
effects of PF on molecular changes in the hippocampus of BCCAO rats
was investigated. The results demonstrated that administration of
PF for 28 days significantly decreased the expression levels of NSE
and S100β, both sensitive markers for brain damage, in VD model
rats. In addition, PF inhibited the initiation of apoptotic cell
death, and attenuated the decreased expression of BDNF induced by
BCCAO damage. These results strongly support the potential
therapeutic role of PF in VD.
NSE is a cytoplasmic glycolytic enzyme in neurons,
and is passively released into the extracellular space under
pathological conditions (19). S100β
is a calcium-binding protein primarily expressed and secreted by
astrocyte cells in the central nervous system; acute elevation of
extracellular S100β has been observed in injury conditions
(20). NSE and S100β expression
levels have been considered markers of neurodegeneration and are
thought to be associated with the severity of the disease (21,22). The
changes in NSE and S100β expression levels in the hippocampus of
rats were examined in present study. Experimental data showed that
the expression levels of NSE and S100β proteins were significantly
decreased in PF-treated VD rats compared with VD rats, which
indicates that PF treatment can reverse hippocampus impairment.
Apoptosis is a mode of cell death, and has been
proposed to explain the cell loss observed in numerous neurological
disorders, including VD (23).
Bcl-2 and Bax are two primary genes responsible for
the regulation of apoptotic cell death, and their individual
products possess opposing functions (24). Bcl-2 is functionally characterized as
the apoptosis-suppressing factor, whereas Bax is considered as the
apoptosis-promoting factor (25).
Bcl-2 inhibits cytochrome c release from mitochondria
elicited by the pro-apoptotic molecule Bax, resulting in the
inhibition of caspase activation and apoptotic death (26,27). In
the present study, treatment with PF significantly reduced the
expression levels of Bax and cytochrome c, and increased the
expression levels of Bcl-2 in the hippocampus of rats with VD.
These changes indicate that PF inhibits hippocampal neuron
apoptosis in a rat model of VD.
Accumulating evidence has documented the critical
role of BDNF, a member of the neurotrophin family, in the
regulation of the maintenance, growth and survival of neurons
(28). BDNF enhances synaptic
transmission and neuronal plasticity in the central nervous system
(29), resulting in an increase of
learning ability and memory capability (30). BDNF serum concentrations have been
reported to correlate with the severity of dementia in patients
(31). The results in the current
study demonstrated that the neuroprotective effects of PF in VD
rats possibly occurred through upregulating the expression of BDNF.
BDNF exerts its neuronal protective properties primarily by
activating tropomyosin-related kinase B (TrkB) receptors, thus
protecting neurons from apoptosis (32). The primary downstream signaling
pathways activated by TrkB receptors are phosphatidylinositol
3-kinase/Akt, mitogen-activated protein kinase/Erk or
phosphoinositide phospholipase-γ signaling pathways. Further
studies are required in order to clarify the downstream signaling
pathways.
In conclusion, the results from the present study
demonstrate that PF produces a protective effect in VD rats by
inhibiting the initiation of apoptotic cell death and attenuating
the decreased expression of BDNF induced in the VD model. These
results confirm the neuroprotective effects of PF on VD and provide
a novel insight into the long-term use of PF as a potential
treatment in the early cognitive impairment stages of VD.
Acknowledgements
The present study was supported by the National Key
Grant of Basic Research Project (grant no. 2010CB530403) and the
Capital Medical University National Key Discipline Project (grant
no. CMUNEURO-201403).
References
|
1
|
Ronnemaa E, Zethelius B, Lannfelt L and
Kilander L: Vascular risk factors and dementia: 40-Year follow-up
of a population-based cohort. Dement Geriatr Cogn Disord.
31:460–466. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Malouf R and Birks J: Donepezil for
vascular cognitive impairment. Cochrane Database Syst Rev CD004395.
2004. View Article : Google Scholar
|
|
3
|
Ferri CP, Prince M, Brayne C, Brodaty H,
Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y,
et al: Global prevalence of dementia: A Delphi consensus study.
Lancet. 366:2112–2117. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yang S, Zhou GG, Liu H, et al: Portective
effects of p38 MAPK inhibitor SB202190 against hippocampal
apoptosis and spatial learning and memory deficits in a rat model
of vascular dementia. Biomed Res Int,. 2013:2157982013. View Article : Google Scholar
|
|
5
|
Jellinger KA: The enigma of vascular
cognitive disorder and vascular dementia. Acta Neuropathol.
113:349–388. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Levine DA and Langa KM: Vascular cognitive
impairment: Disease mechanisms and therapeutic implications.
Neurotherapeutics. 8:361–373. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bennett S, Grant MM and Aldred S:
Oxidative stress in vascular dementia and Alzheimer's disease: A
common pathology. J Alzheimers Dis. 17:245–257. 2009.PubMed/NCBI
|
|
8
|
Wang J, Zhang HY and Tang XC: Cholinergic
deficiency involved in vascular dementia: Possible mechanism and
strategy of treatment. Acta Pharmacol Sin. 30:879–888. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gong X, Ma M, Fan X, Li M, Liu Q, Liu X
and Xu G: Down-regulation of IGF-1/IGF-1R in hippocampus of rats
with vascular dementia. Neurosci Lett. 513:20–24. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kasparova S, Brezova V, Valko M, et al:
Study of the oxidative stress in a rat model of chronic brain
hypoperfusion. Neurochem Int. 46:601–611. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nizamutdinoval IT, Jim YC, Kim JS, et al:
Paconol and paconiflorin, the main active principles of
Paconiaalbiflora, protect the heart from myocardial
ischemia/reperfusion injury in rats. Planta Med. 74:14–18. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Watanabe H: Candidates for cognitive
enhancer extracted from medicinal plants: Paeoniflorin and
tetramethylpyrazine. Behav Brain Res. 83:135–141. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tang NY, Liu CH, Hsieh CT and Hsieh CL:
The anti-inflammatory effect of paeoniflorin on cerebral infarction
induced by ischemia-reperfusion injury in Sprague-Dawley rats. Am J
Chin Med. 38:51–64. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiao L, Wang YZ, Liu J, Luo XT, Ye Y and
Zhu XZ: Effects of paeoniflorin on the cerebral infarction,
behavioral and cognitive impairments at the chronic stage of
transient middle cerebral artery occlusion in rats. Life Sci.
78:413–420. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang LG, Wang LJ, Shen QQ, et al:
Paeoniflorin Improves Regional Cerebral Blood Flow and Suppresses
Inflammatory Factors in the Hippocampus of Rats with Vascular
Dementia. Chin J Integr Med. Epub ahead of print.
|
|
16
|
Institute of Laboratory Animal Research,
Commission on Life Sciences, National Research Council, . Guide for
the Care and Use of Laboratory Animals. 7th. National Academy
Press; Washington, D.C.: pp. 56–66. 1996
|
|
17
|
D'Hooge R and De Devn PP: Applications of
the Morris water maze in the study of learning and memory. Brain
Res Brain Res Rev. 36:60–90. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Farkas E, Luiten PG and Bari F: Permanent,
bilateral common carotid artery occlusion in the rat: A model for
chronic cerebral hypoperfusion-related neurodegenerative diseases.
Brain Res Rev. 54:162–180. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Berger RP, Dulani T, Adelson PD, Leventhal
JM, Richichi R and Kochanek PM: Identification of inflicted
traumatic brain injury in well-appearing infants using serum and
cerebrospinal markers: A possible screening tool. Pediatrics.
117:325–332. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gonçalves CA, Leite MC and Nardin P:
Biological and methodological features of the measurement of S100B,
a putative marker of brain injury. Clin Biochem. 41:755–763. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mecocci P, Parnetti L, Romano G, Scarelli
A, Chionne F, Cecchetti R, Polidori MC, Palumbo B, Cherubini A and
Senin U: Serum anti-GFAP and anti-S100 autoantibodies in brain
aging, Alzheimer's disease and vascular dementia. J Neuroimmunol.
57:165–170. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Parnetti L, Palumbo B, Cardinali L, Loreti
F, Chionne F, Cecchetti R and Senin U: Cerebrospinal fluid
neuron-specific enolase in Alzheimer's disease and vascular
dementia. Neurosci Lett. 183:43–45. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sun ZK, Ma XR, Jia YJ, et al: Effects of
resveratrol on apoptosis in a rat model of vascular dementia. Exp
Ther Med. 7:843–848. 2014.PubMed/NCBI
|
|
24
|
Min JJ, Huo XL, Xiang LY, et al:
Protective effect of Dl-3n-butylphthalide on learning and memory
impairment induced by chronic intermittent hypoxia-hypercapnia
exposure. Sci Rep. 4:55552014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hwang L, Choi IY, Kim SE, Ko IG, Shin MS,
Kim CJ, Kim SH, Jin JJ, Chung JY and Yi JW: Dexmedetomidine
ameliorates intracerebral hemorrhage-induced memory impairment by
inhibiting apoptosis and enhancing brain-derived neurotrophic
factor expression in the rat hippocampus. Int J Mol Med.
31:1047–1056. 2013.PubMed/NCBI
|
|
26
|
Shimizu S, Narita M and Tsujimoto Y: Bcl-2
family proteins regulate the release of apoptogenic cytochrome c by
the mitochondrial channel VDAC. Nature. 399:483–487. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kluck RM, Bossy-Wetzel E, Green DR and
Newmeyer DD: The release of cytochrome c from mitochondria: A
primary site for Bcl-2 regulation of apoptosis. Science.
275:1132–1136. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chuang DM: The antiapoptotic actions of
mood stabilizers: molecular mechanisms and therapeutic potentials.
Ann N Y Acad Sci. 1053:195–204. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Schinder AF and Poo M: The neurotrophin
hypothesis for synaptic plasticity. Trends Neurosci. 23:639–645.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mizuno M, Yamada K, Olariu A, Nawa H and
Nabeshima T: Involvement of brain-derived neurotrophic factor in
spatial memory formation and maintenance in a radial arm maze test
in rats. J Neurosci. 20:7116–7121. 2000.PubMed/NCBI
|
|
31
|
Laske C, Stransky E, Leyhe T, Eschweiler
GW, Maetzler W, Wittorf A, Soekadar S, Richartz E, Koehler N,
Bartels M, et al: BDNF serum and CSF concentrations in Alzheimer's
disease, normal pressure hydrocephalus and healthy controls. J
Psychiatr Res. 41:387–394. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Murer MG, Yan Q and Raisman-Vozari R:
Brain-derived neurotrophic factor in the control human brain and in
Alzheimer's disease and Parkinson's disease. Prog Neurobiol.
63:71–124. 2001. View Article : Google Scholar : PubMed/NCBI
|