Introduction
Acute spinal cord injury (ASCI) is a severe type of
high-energy central nervous system (CNS) damage that frequently
leads to devastating neurological deficits and disabilities,
including the loss of sensory and motor capabilities (paraplegia or
tetraplegia). The prevalence of ASCI ranges from 906 to 250 per
million and the annual incidence of ASCI ranges from 8 to 49.1 per
million in different nations (1) and
global prevalence is expected to increase (2). Following ASCI, the spinal cord is
restored for a period of time, however function is markedly damaged
and is often irreversible, leading to delayed death of spinal
neurons and paralysis. There is an increasing body of evidence
regarding the pathophysiology of acute spinal cord injury,
indicating that it involves primary and secondary injury (3–10). The
primary injury directly leads to neuron death, while the secondary
injury's pathological mechanisms encompass excitotoxicity, ionic
imbalances, inflammatory response, lipid peroxidation, free radical
injury and apoptosis (3–7), which induce neuron death. Presently,
stem cell therapy has become one of the current treatments;
however, its application is limited due to ethical aspects
(11). Although great advances in
pharmacotherapy for the purpose of limiting neuronal secondary
injury following ASCI have been achieved, only methylprednisolone
(MP) is used widely (9,12,13). MP
is used to treat ASCI due to its potent anti-inflammatory,
anti-apoptosis and antioxidant properties (9). However, due to the poor side-effects,
such as sepsis, pulmonary embolism, wound infections (14) and gastrointestinal bleeding (2), and controversy over whether or not the
effects are beneficial-previous studies have reported that MP did
not improve motor function scores (2,15)-concerns have been raised due to the
high dosage (30 mg/kg bolus followed by 5.4 mg/kg for 23 h)
(13) required and therefore, its
use in treating ASCI is contentious (9,16). It is
therefore important to investigate other pharmacological agents
that may be combined with MP in order to reduce the dose of MP
required and enhance functional recovery.
Tanshinone IIA (TIIA) is an effective monomer
component purified from the Chinese herb Danshen (Radix Salviae
Miltiorrhiza) and representative liposoluble constituent. It
participates in various biochemical events in organisms and
exhibits bioactivities to antagonize oxidation properties, protect
against inflammation, apoptosis and free radical injury following
CNS injury, as demonstrated in in vitro and in vivo
studies (8,17,18). It
has been demonstrated that TIIA protects rat spinal cord neurons
against ASCI-induced neurotoxicity (8). However, to the best of our knowledge,
there are no studies assessing the effect of combined TIIA with MP
and whether combining TIIA treatment with MP may allow the dose of
MP to be reduced in the treatment of ASCI. The present study
attempted to investigate the effects of combined TIIA with MP to
treat ASCI in vivo and in vitro by measuring
oxidative stress reaction, the expressions of inflammatory factors
and apoptosis-related proteins.
Materials and methods
Animals
All Sprague-Dawley rats were kept in dams in the
Laboratory Animal Services Center with ad libitum access to
food and water and a 12-h light-dark cycle. All rats were
maintained at 22–25°C and 40–60% humidity. A total of 60 adult male
Sprague-Dawley rats (Hubei Provincial Laboratory Animal Public
Service Center, Hubei, China), weighing 240–260 g and aged 6–7
weeks-old, were used in the current study, 12 of which were
selected for sham-surgery and 48 selected for contusive ASCI. A
total of 80 one-day-old male Sprague-Dawley rats (Center for Animal
Experiment of Wuhan University, Wuhan, China) were used for cell
culture in vitro. All rats were maintained in the same
conditions. All procedures were performed in accordance with
guidelines approved by the Animal Ethics Committee of Wuhan General
Hospital of Guangzhou Military Command (Wuhan, China).
Rat ASCI model
All adult animals (n=60) were anaesthetized through
intraperitoneal (i.p.) injection of 10% chloral hydrate (3.5 ml/kg,
i.p.; Hubei Yuancheng Saichuang Technology Co., Ltd., Wuhan,
China). In order to expose the paravertebral muscles, an incision
was made along the back of each rat. A laminectomy was performed at
the T9-T11 level, exposing the cord without damaging the dura. In
order to subject the exposed dorsal surface of the cord to the
weight drop impact, a 10-g metal rod was dropped from a height of
25 mm (19). Subsequently, the
lesioned muscle and skin were sutured in two layers. Each rat was
then administered 1.0 ml saline solution using a subcutaneous
injection, to replace blood volume lost during surgery. Following
surgery, sterile gauze was wrapped around the wound on each rat. A
standard diet and water were provided daily to the rats ad
libitum. A total of 3 to 5 days' post-injury, manual bladder
expression was performed twice a day until the rats were able to
urinate by themselves.
Study design in animal models
In the current study, 60 rats were randomly assigned
into five groups (n=12, each group) and all animals were subjected
to laminectomy: Sham group, animals were only subjected to
laminectomy; ASCI group, animals subjected to ASCI using an
impactor; TIIA treatment group, animals subjected to ASCI using an
impactor and treated with a dosage of 30 mg/kg TIIA per day [chosen
according to previous findings (20)]; MP treatment group, animals subjected
to ASCI using an impactor and treated with 30 mg/kg MP (13) 15 min following the strike; TIIA + MP
treatment group, the animals were subjected to ASCI using an
impactor and treated with 30 mg/kg TIIA per day and a selected low
dose of 20 mg/kg MP 15 min after the strike. The drugs were
administered via intraperitoneal administration. At the planed time
point, rats were anesthetized by intraperitoneal injection of 10%
chloral hydrate (3.5 ml/kg, i.p.) as before and the spinal cord was
immediately exposed from T9 to T11 and 10 mm damaged tissue was cut
at the site of injury. Rats were sacrificed by cervical dislocation
except for the immunofluorescence double labeling experiment at
different time points (4 rats per group), depending on the
parameters measured: Rats undergoing western blot analysis for
nuclear factor (NF)-κB on day 1, measurement of tissue superoxide
dismutase (SOD) and malondialdehyde (MDA) on day 1 and on day 7
following ASCI, immunofluorescent staining on day 3 following ASCI
and western blot analysis for caspase-3, B-cell lymphoma-2 (Bcl-2)
and Bcl-2 associated protein X (Bax) on day 7 following ASCI.
Cell culture and treatment
Primary culture of cortical neurons was isolated and
cultured as previously described (21), with minor modifications. For mixed
glial cell culture, one-day-old Sprague-Dawley rat pups were
sacrificed by cervical dislocation; the skin and skull were
carefully torn with tweezers and brain cortical tissues were
dissected in ice-cold dissection buffer. Following this, the
meninges of the cortex were peeled off and separated from the
olfactory bulb and hippocampus and dissected cortical tissues were
digested with trypsin. Following incubation at 37°C for 15 min to
adhere and eliminate fibroblasts, cells were dissociated and plated
into 75 cm2 tissue culture flasks at a density of
2.0×107 cells/flask. Cells were incubated at 37°C with
Dulbecco's modified Eagle's medium/F12 supplemented with 10% fetal
bovine serum (both Hyclone; GE Healthcare Life Sciences, Logan, UT,
USA) and 1% penicillin-streptomycin medium. Following 24 h,
non-adherent cells were removed by agitating the flask and the
culture medium was replaced. When a confluent layer of glial cells
formed (10 to 14 days), cells were trypsinized (Beyotime Institute
of Biotechnology, Haimen, China) and inoculated. Following the
second passage, cells were seeded into a 6-well cell culture plate
(Nest Biotechnology Co., Ltd., Wuxi, China) for neuron-glia
co-culture. Rat primary spinal cord neuron cultures were derived
from the spinal cord of one-day-old Sprague-Dawley rat pups.
Briefly, spinal cords were dissected and freed of meninges. Cells
were dissociated by trypsinization, followed by triturating and
passing through a 74-mm steel mesh. Cells were incubated at 37°C
for 30 min to allow adherence and eliminate glial cells and
fibroblasts. Neurons (2×105 cells/plate) were plated
onto poly-L-lysine (PLL; Sigma-Aldrich; Merck Millipore, Darmstadt,
Germany) coated 20-mm glass coverslips (NEST, China) for co-culture
experiments and MTT analysis. Neurons were maintained in neurobasal
media (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA), 2%
B27 supplement (Gibco; Thermo Fisher Scientific, Inc.) and 0.5 mM
glutamine (Sigma-Aldrich; Merck Millipore). Neurons on coverslips
at day 6–7 were placed into glia-seeded wells. Neurons and
astrocytes were in close apposition but with no direct cell-cell
contact. For modelling ASCI, neurons and glial cell were subjected
to a cut with a no. 15 scalpel blade (22) with a 1 mm gap. Cultures were
maintained in a 37°C humidified incubator in a 5% CO2 atmosphere.
The cells were treated with TIIA at a concentration of 10 µM
(according to the MTT analysis), MP at a concentration of 1 µM and
combined TIIA 10 µM and MP 0.5 µM, respectively. The incubation was
continued for 24 h and subsequently the cells were trypsinized,
collected and extracted for analysis.
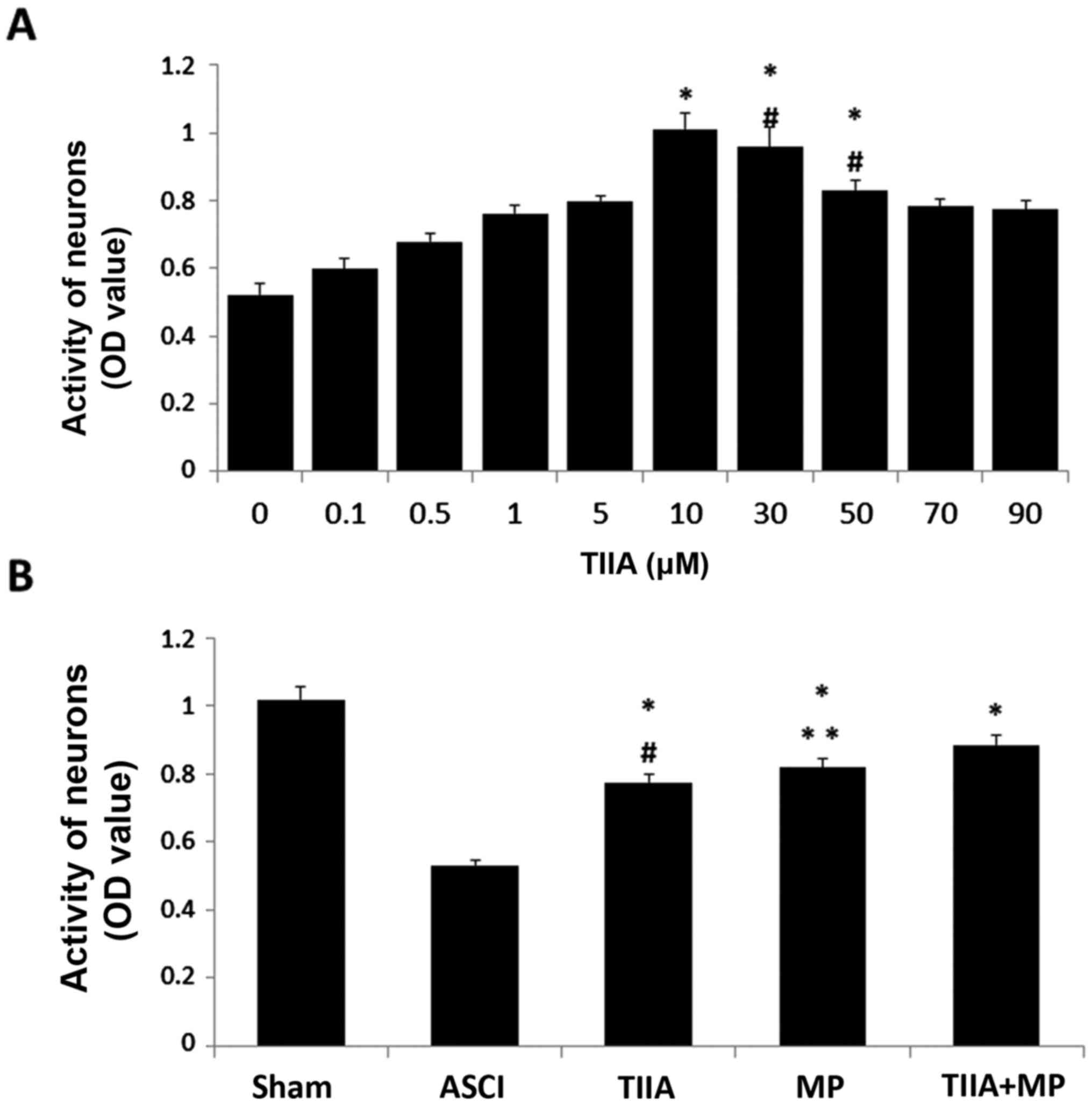
MTT analysis
The neurons' viability was measured by MTT assay for
the optimal concentration of TIIA for neurons. Briefly, the MTT
solution (Beyotime Institute of Biotechnology) was added to 96-well
plates (1×104 neuronal cells/well) at a final
concentration of 500 mg/ml and then incubated for 4 h at 37°C. To
dissolve the formazan, the culture medium was removed and 100 µl
dimethyl sulfoxide was added to each well. The optical density of
each well was measured at 570 nm using a microplate reader. One
culture well with neurons was used for each experimental condition.
Thus, each plate contained multiple wells of each experimental
condition and multiple control wells. This procedure was replicated
for 4 plates per condition. Spinal cord neurons were treated with
various concentrations (0, 0.1, 0.5, 1, 5, 10, 30, 50, 70 and 90
µM) of TIIA for 24 h. Following this, the cells were injured as
previously described. Cell viability was measured using an MTT
assay. Neuron viability treated with TIIA, MP and their combination
was measured by MTT assay too. The MTT data was converted to the
percentage of the respective control groups (untreated spinal cord
neuron cells) after analysis by microplate reader (SM-600, Shanghai
Utrao Medical Devices Co., Ltd, China).
Western blot analysis
Total proteins were extracted separately from the
spinal cord tissues or neurons' cultures. In detail, following
sacrifice and transcardial perfusion with 100 ml 0.9% saline, the
experimental rats' skin and soft tissue on back at T9-T11 were cut
to expose the injured spinal cord, which was harvested (5 mm
rostral and 5 mm caudal from the injury site). The tissue was
homogenized by sonication in radioimmunoprecipitation assay lysis
buffer (Wuhan Boster Biological Technology, Ltd., Wuhan, China),
and neurons were washed three times in Earle's Balance Salt
Solution following trypsinization and kept in serum-free media
(Hyclone; GE Healthcare Life Sciences). The samples were
centrifuged at 12,000 × g for 1 h at 4°C. The protein
content of the lysate samples was determined using a BCA protein
assay kit (Beyotime Institute of Biotechnology). Protein lysates
(35 µg per lane for each sample) were fractioned using 10% SDS-PAGE
and transferred to a nitrocellulose membrane. Membranes were then
blocked with 5% non-fat dry milk at room temperature for 2 h and
incubated for 12 h at 4°C with primary antibodies: Rabbit
anti-β-actin (BA2305; 1:1,000; Wuhan Boster Biological Technology,
Ltd.), rabbit anti-Bcl-2 (15071T; 1:800), rabbit anti-Bax (2772T;
1:800; both Cell Signaling Technology, Inc., Danvers, MA, USA),
rabbit anti-caspase-3 (ab4051; 1:300; Abcam, Cambridge, UK) and
rabbit anti-NF-κBP65 (BA1298; 1:1,000; Wuhan Boster Biological
Technology, Ltd.). Horseradish peroxidase conjugate goat
anti-rabbit immunoglobulin (Ig)G was used as a secondary antibody
(BA1055 1:50,000, Wuhan Boster Biological Technology, Ltd.). The
reaction was developed using enhanced chemiluminescence (ELC)
reagent (Thermo Fisher Scientific, Inc.) and signal density was
measured using ImageJ analysis software v2.1.4.7 (National
Institute of Health, Bethesda, MD, USA) (23). Each group had 4 replicates and the
values were normalized against β-actin.
Immunofluorescence double
labeling
In order to perform immunofluorescence double
labeling for confocal microscopy, rats were sacrificed 3 days
post-injury as described before, and the whole body of the rat was
fixed using transcardial saline infusion followed by 100 ml
paraformaldehyde (4%). Following perfusion, the injured spinal
cords were carefully dissected, as indicated for western blot
analysis, fixed for an additional 2 h in 4% paraformaldehyde at
4°C. The specimens were transferred to a solution containing 30%
sucrose in 0.1 M phosphate buffer (pH 7.4) overnight. Spinal cord
segments from sham-operated or injured animals were embedded in
paraffin and longitudinally sectioned (2-µm thick), prior to
mounting on gelatin-coated slides. The sections were dewaxed with
xylene, permeabilized and blocked with 0.3% Triton X-100 and 10%
normal goat serum (Wuhan Boster Biological Technology, Ltd.) in
0.01 M phosphate-buffered saline for 30 min at 4°C. Mouse anti rat
caspase-3 polyclonal antibody (AB208161; 1:100; Abcam) and rabbit
anti-rat β-III Tubulin (AT809; 1:100; Beyotime Institute of
Biotechnology) primary antibodies were applied to the sections
overnight at 4°C. On the following day, the sections were incubated
with fluorescein isothiocyanate-conjugated goat anti-rabbit
(BA1105; 1:1,000) and indoles cyanine dye (Cy3)-conjugated goat
anti-mouse (BA1032; 1:1,000; both Wuhan Boster Biological
Technology, Ltd.) secondary antibodies at 4°C for 3 h. Slides were
mounted and examined with a BX51 fluorescence microscope (Olympus
Corp., Tokyo, Japan). In control sections, the primary antibody was
substituted with 1% normal goat serum. The colocalisation area was
measured using ImageJ analysis software (v2.1.4.7). R value
represented Mander's overlap coefficient tubulin and caspase-3 in
ImageJ analysis software: Ranges between 1 and 0, with 1 indicating
high colocalisation and 0 indicating low colocalisation.
Behavioral assessments
Behavioral assessments were determined using the
Basso, Beattie, and Bresnahan (BBB) locomotor rating score. Gross
BBB locomotor recovery following contusive spinal cord injury was
scored in an open field according to the locomotor rating scale of
0 (complete paralysis) to 21 (normal locomotion) (24). BBB testing was performed once a day
in double-blind model from day 0 to day 7 following spinal cord
surgery. Each rat was observed for 4 min by two investigators
blinded to the study.
Measurement of SOD and MDA
MDA was measured using an MDA assay kit (Thiobar
bituric acid test method; Beyotime Institute of Biotechnology) and
SOD activities in spinal cord tissues were measured using a
Total-SOD (T-SOD) assay kit (Hydroxylamine method; Nanjing
Jiancheng Bioengineering Institute, Nanjing, China) in accordance
with previous research (20).
Statistical analysis
Data are expressed as the mean ± standard error of
the mean. Statistical significance was determined using Student's
t-test when there were two experimental groups. When more than two
groups were compared, statistical evaluation of the data was
performed using one-way analysis of variance and Dunnett's post-hoc
test. P<0.05 was considered to represent a statistically
significant difference.
Results
Effects on functional recovery
following ASCI
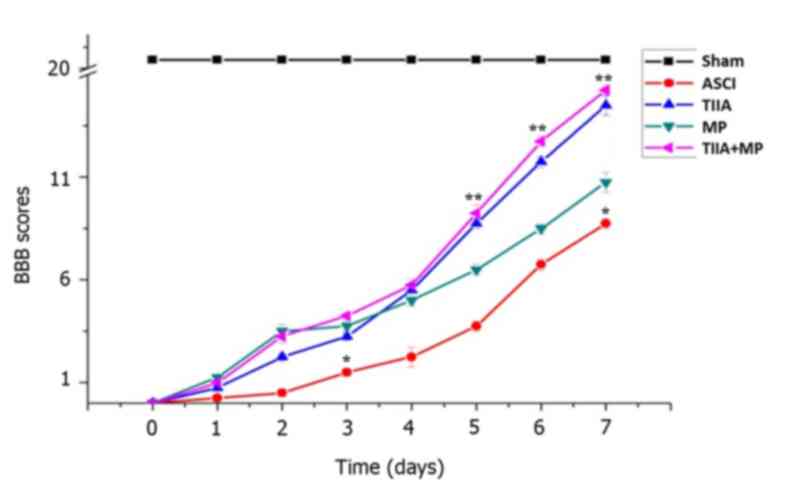
In order to assess the effects of treatment on
functional recovery following ASCI in each group, the BBB locomotor
test was performed every day for 7 days (Fig. 1). On day 0, the BBB score of all rats
was regarded as 0. BBB scores in the treatment groups were
significantly higher than the ASCI group on day 3 and 7
(P<0.05). BBB scores in the TIIA + MP combined group were higher
than the MP group on day 3, but this was not significant
(P>0.05). From day 5 to day 7, the scores in the combined
treatment group were higher than the MP group and the differences
were statistically significant (P<0.05; Fig. 1).
Effect on the expression of apoptosis
factors following ASCI
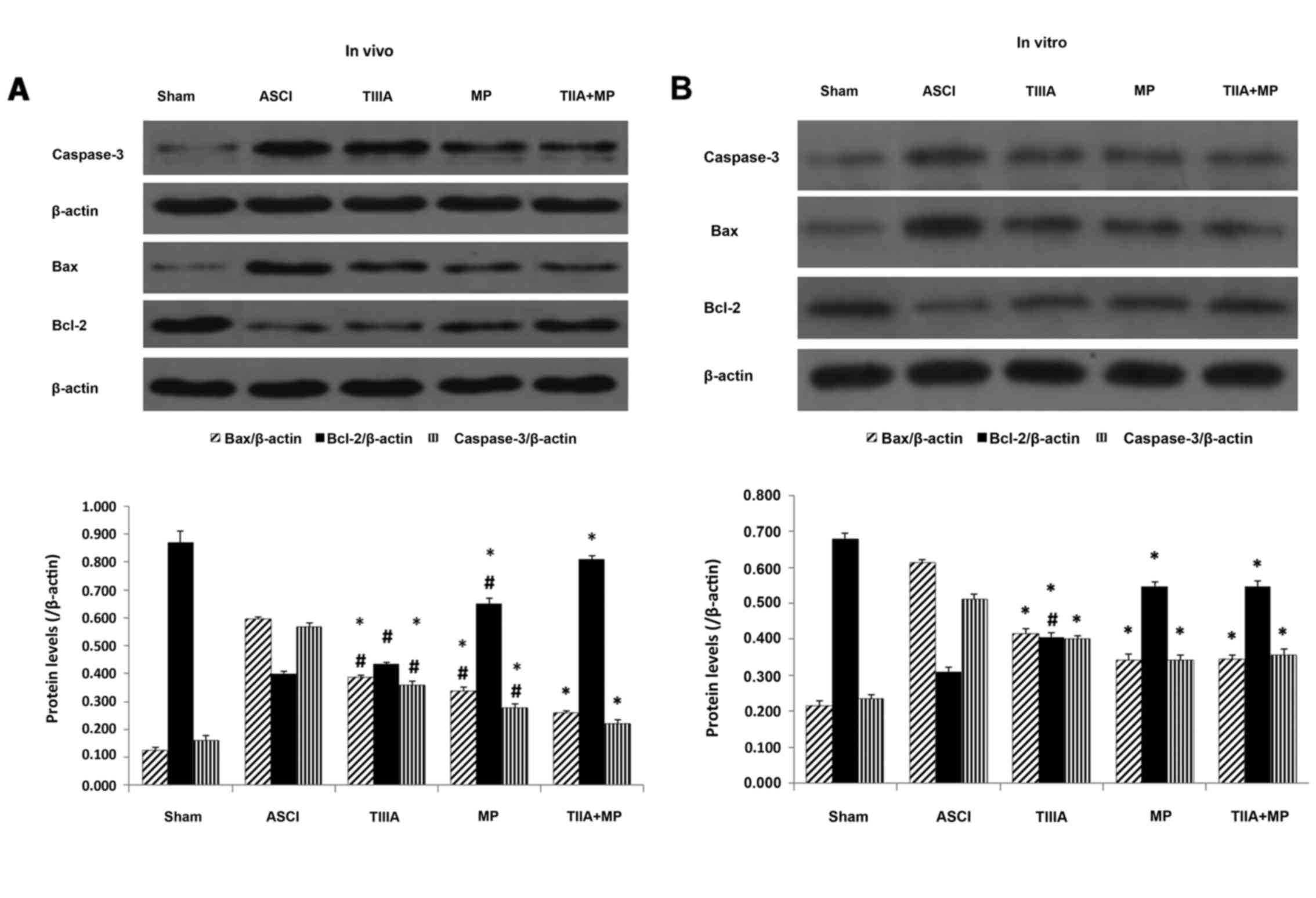
In the present study, the effect of each treatment
on the expression of pro- and anti-apoptotic factors on day 7
following ASCI in rats and 24 h following mechanical injury in
neurons were investigated using western blot analysis. As presented
in Fig. 2A, Bax and caspase-3
expression were appreciably increased in the spinal cords of rats
subjected to ASCI and Bcl-2 expression was decreased compared with
the sham group. However, this state was altered by the drug
treatments. Combined treatment exhibited significant anti-apoptotic
ability compared with that observed in the ASCI group on day 7
after ASCI (P<0.05; Fig. 2A). The
statistical analysis demonstrated that Bcl-2 expression in the
combined treatment group was significantly increased, however,
levels of Bax and caspase-3 were significantly decreased compared
with the MP group (P<0.05; Fig.
2A). In addition, the data in Fig.
2B indicated that combined treatment was significantly more
effective than TIIA treatment alone at reversing the decrease in
Bcl-2 expression induced by mechanical injury in neurons
(P<0.05), although Bax and caspase-3 expression did not differ
significantly. These effects were similar to those observed in the
MP group (P<0.05).
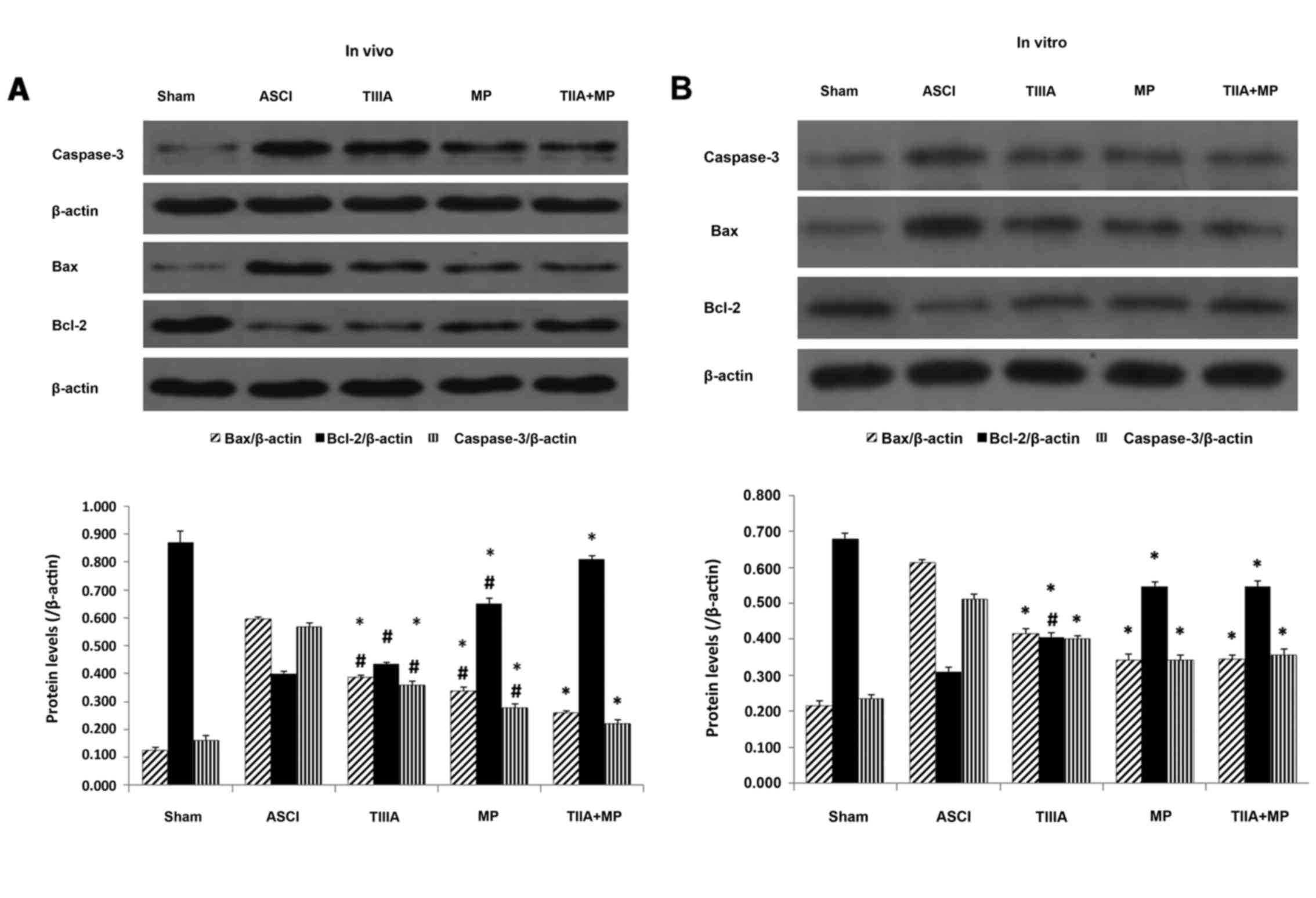 | Figure 2.Expression of Bcl-2, Bax and
Caspase-3 proteins determined by western blot analysis. (A) Results
normalized relative to β-actin in the ASCI rats at day 7 and (B) in
spinal neuron culture scratch models following 24 h culture. Data
are presented as mean ± standard error of the mean, n=4 per group.
(A) *P<0.05 vs. ACSI group; #P<0.05 vs. TIIA + MP group. (B)
*P<0.05 vs. ASCI group; #P<0.05 vs. TIIA + MP group and MP
group. Bcl-2, B-cell lymphoma-2; Bax, Bcl-2 associated protein X;
ASCI, acute spinal cord injury; MP, methylprednisolone; TIIA,
tanshinone IIA; TIIA + MP, TIIA and MP combined treatment; Sham,
sham-operated, no treatment. |
Effect on the expression of
antioxidation molecules following ASCI
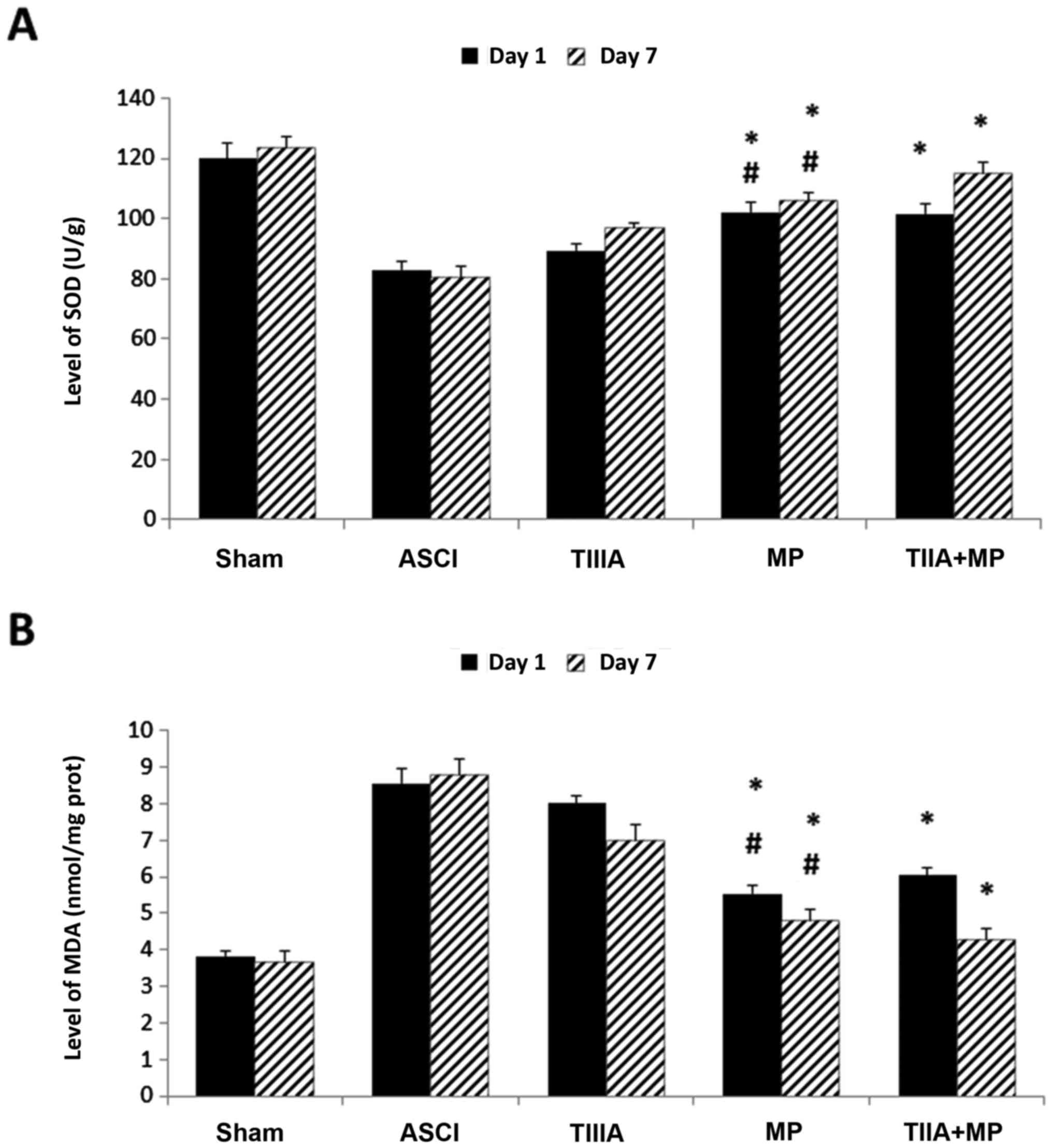
The effect of each treatment on antioxidation was
investigated by measuring the tissue levels of SOD and MDA in the
spinal cord on day 1 and day 7. Levels of SOD were significantly
elevated in the MP group and TIIA + MP group compared with the ASCI
group (P<0.05; Fig. 3A), while
levels of MDA were significantly reduced in the MP group and TIIA +
MP group compared with those of the rats in the ASCI group
(P<0.05; Fig. 3B). However, no
significant differences in SOD and MDA levels were observed between
the MP and combined treatment groups.
Effect on the expression level of
NF-κB in the spinal cord following ASCI
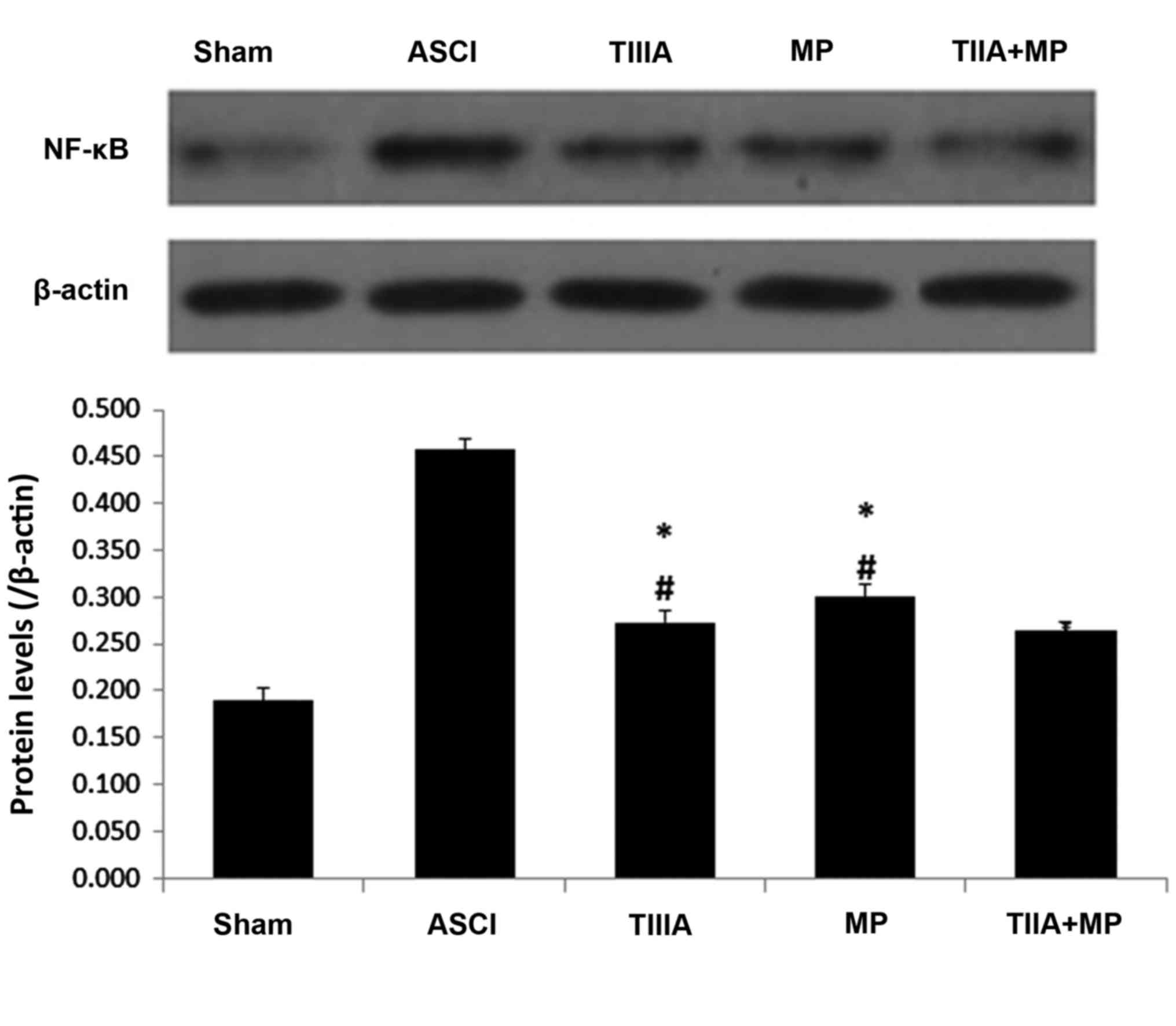
The effect of each treatment on NF-κB expression in
the spinal cord tissue on 1 day following ASCI was detected by
western blot analysis. This was due to the NF-κB associated pathway
that serves a key role in inflammation during secondary injury
following ASCI (25). Substantial
increases in NF-κB levels were identified in spinal cord tissue
samples collected from rats 1 day following ASCI. These increases
were significantly reversed in all treatment groups (P<0.05;
Fig. 4). NF-κB levels detected in
the combined treatment group were lower than in the MP group, but
this difference was not significant.
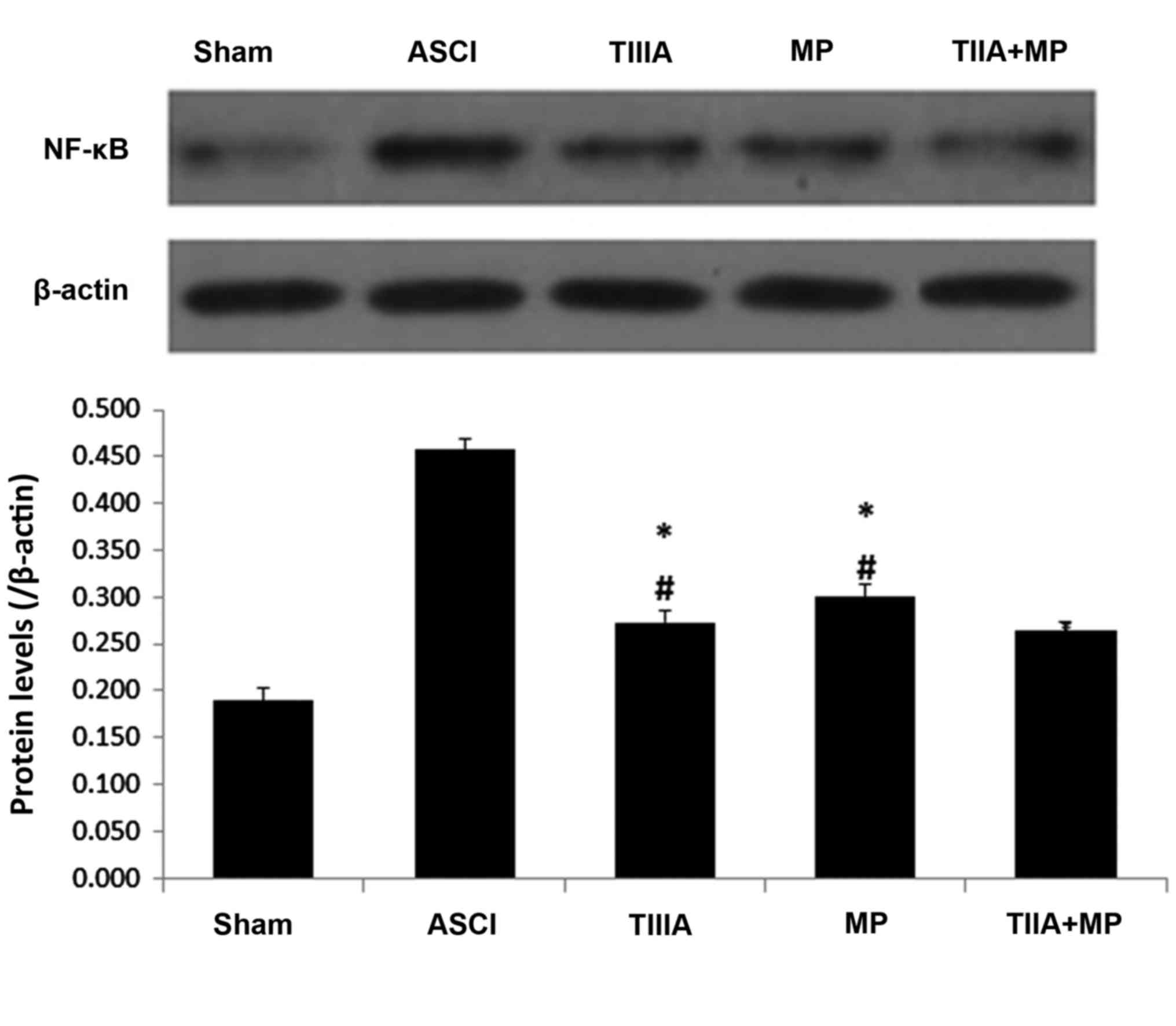 | Figure 4.Expression of NF-κB determined by
western blot analysis, with results normalized relative to β-actin
in spinal neurons culture scratch models following 24 h. Data are
presented as mean ± standard error of the mean, n=4 per group.
*P<0.05 vs. ASCI group, #P>0.05 vs. TIIA + MP
group. NF-κB, nuclear factor-κB; ASCI, acute spinal cord injury;
MP, methylprednisolone; TIIA, tanshinone IIA; TIIA + MP, TIIA and
MP combined treatment; Sham, sham-operated, no treatment. |
Effect on the activity of mechanical
injured neurons following ASCI
To determine the neuroprotective ability of TIIA,
cultured spinal cord neurons were exposed to mechanical injury and
cell viability was assessed by MTT reduction assay after 24 h.
Results are presented as the mean of 5 replicate values in three
independent experiments. Based on the result, 10 µM was selected as
the optimal TIIA concentration for subsequent experiments, as the
increase in neuronal activity was greatest following treatment with
10 µM TIIA (Fig. 5A). In the ASCI
group, the optical density (OD) value decreased 24 h after the
mechanical scratch protocol. Treatment with TIIA, MP and the
combined treatment significantly reversed this decrease in OD value
(P<0.05). Cell viability in the combined treatment group was
higher than in the MP group, however, no significant differences
were observed in cell viability between cells treated with MP alone
and the combined treatment.
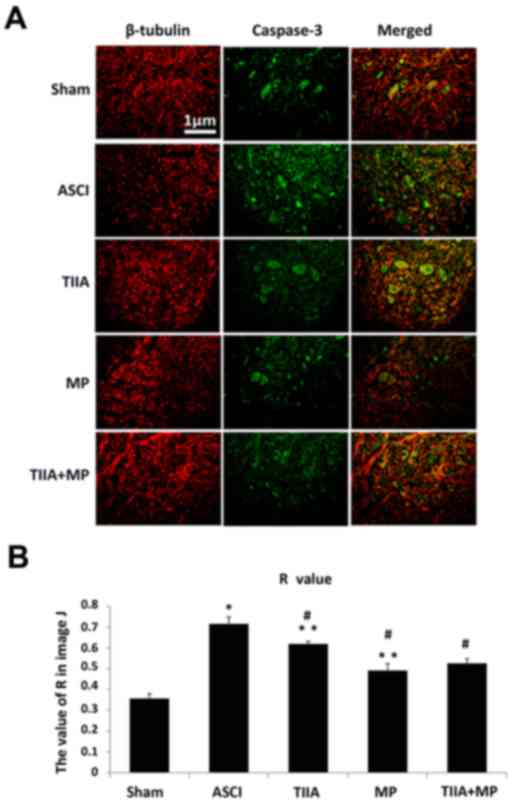
Effect on the expression of caspase-3
in spinal tissues and neurons in vivo by immunohistochemistry
Immunofluorescence double labeling images are
presented in Fig. 6A (red: Tubulin
and green: caspase-3). The results indicated that decreased levels
of caspase-3 expression in neurons were exhibited in treatment
groups when compared with the ASCI group. In Fig. 6B, the R values represent the overlap
coefficient of tubulin and caspase-3 and the results from the
immunohistochemistry experiments revealed that a significant
increase in the immunoreactivity of caspase-3 was observed in ASCI
rats compared with the sham group (P<0.05), which suggested that
there was more caspase-3 present in neurons in the ASCI group
compared with the sham group. Similar to the results from western
blot analysis, TIIA, MP and combined TIIA + MP treatment
significantly reduced the R value compared with the ASCI group,
which indicated that reduced levels of caspase-3 (P<0.05) were
present in the neurons of each group, but there was no significant
difference between the TIIA or MP groups compared with the combined
treatment group (P>0.05).
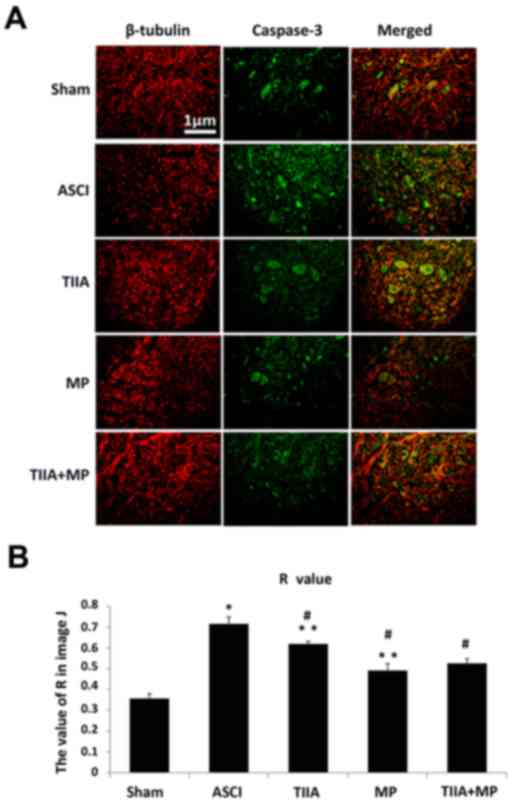 | Figure 6.Immunofluorescence double labeling
images and the R value of Mander's overlap coefficient indicate
that the immunoreactivity of capase-3 increases in ASCI rats and
was reduced following treatment with MP. Scale bar=1 µM. (A)
Expression of caspase-3 in the spinal tissues and neurons in
vivo was determined by immunoreactivity at day 3 (red, β-III
Tubulin and green, caspase-3). (B) Data are presented as mean ±
standard error of the mean, n=5 per group. R value represented
Mander's overlap coefficient tubulin and caspase-3 in ImageJ
analysis software (v2.1.4.7): Ranges between 1 and 0, with 1
indicating high colocalisation (increased levels of caspase-3 in
neurons) and 0 indicating low colocalisation (reduced levels of
caspase-3 in neurons). *P<0.05 vs. Sham group; #P<0.05 vs.
ASCI group; **P>0.05 vs. TIIA + MP group. ASCI, acute spinal
cord injury; MP, methylprednisolone; TIIA, tanshinone IIA; TIIA +
MP, TIIA and MP combined treatment; Sham, sham-operated, no
treatment. |
Discussion
The present study provides evidence that the
combination of TIIA with MP significantly improves motor function
following ASCI and may reduce the dose of MP required to induce the
same anti-apoptosis, antioxidation and anti-inflammatory
efficiency. Furthermore, combined treatment may reduce apoptosis of
neurons following mechanical injury in vitro. Although both
compounds have each been extensively studied (8,26), to
the best of our knowledge, the current study is the first to
identify the neurological outcome from combining TIIA and MP
treatment following ASCI. The viability and regenerative capacity
of neurons in the CNS is supported by the effects of TIIA and MP
combined treatment. This has practical and conceptual implications
due to the anti-apoptosis, antioxidation and anti-inflammatory
efficiency of TIIA and MP combined treatment.
The treatment of ASCI is a major challenge for
physicians due to the complex and progressive nature of the
disease. MP is one of the most investigated agents due to its
neuroprotective potential and remains the only drug used worldwide
to treat ASCI. Although MP is not FDA-approved for use following
ASCI, it is commonly used in this setting based on the results of a
number of randomized controlled trials; furthermore, the beneficial
effect of high-dose MP was initially reported in a series of
National Acute Spinal Cord Injury Studies (NASCIS) (13,27).
Following publication of the NASCIS trials, the regimen of these
trials was rapidly adopted worldwide. As well as the benefits of MP
however, high-dose MP led to a number of side effects developing,
including urinary tract infections, pneumonia, wound infections,
hyperglycemia and gastrointestinal complications (16,28–31).
Therefore, the identification of other pharmacological agents to
combine with MP is required in order to enhance functional recovery
and reduce the dose of MP required and thus, its side effects. A
number of studies demonstrate that TIIA may protect the spinal cord
tissues from ASCI due to its anti-inflammatory, anti-apoptotic and
antioxidant functions (8,17,20,25). The
present study aimed to detect the efficiency of a combined
treatment of TIIA and MP following ASCI. The major finding of the
current study is that combined TIIA and MP has beneficial effects
on contusion acute injury of the spinal cord in rats and mechanical
scratch in neurons.
When the spinal cord is lacerated or macerated by a
sharp penetrating force, or contused or compressed by a blunt
force, it leads to neurological damage occurring in the spinal cord
that is normally referred to as ‘primary injury’. The primary
injury refers to the loss of spinal cord integrity due to
mechanical factors (10). The
mechanical injury leads to a cascade of biological events,
described as ‘secondary injury’ (32,33),
which occurs over a time course of min to weeks and leads to
further neurological damage. Much of the damage that occurs in the
spinal cord following traumatic injury is due to the secondary
effects of a complex array of pathophysiological processes
including ischemia, edema, inflammation, excitotoxicity and
oxidative cell damage, which take part in a spiraling interactive
cascade, ending in neuronal dysfunction and death (10).
Assessment of neurological function is a prevalent
method of accessing the degree of injury and the outcome of a
treatment with medication. In the present study, BBB rating
indicated a significant improvement of locomotion occurring
everyday post-treatment, suggesting that the combined treatment may
improve the behavioral function in animals with ASCI. Notably, the
BBB scores in the MP group were higher than the combined treatment
group 3 days following ASCI, while functional recovery was slower,
taking 4–7 days. This may be because high-dose MP is more effective
in protecting the injured spinal cord in the early phase, while
continuous TIIA treatment may protect the injured spinal cord in
the late phase.
The potential mechanism of ASCI remains unclear.
However, neuronal apoptosis is one of the major pathogenic
mechanisms that govern ASCI. The increased activation of oxidative
stress and a series of apoptosis-associated proteins contribute to
the pathogenic processes of neuronal death following ASCI, which
ultimately lead to cell death (4,7). Cell
apoptosis typically occurs in the ‘secondary injury’ phase
(32). Bcl-2 and Bax are regarded as
regulators of apoptosis, one of their principal roles is the
regulation of the initiation of apoptosis by the mitochondrial
pathway, and specifically, they directly regulate the permeability
of the external mitochondrial membrane, acting in opposition: Bcl-2
inhibits apoptosis and Bax promotes apoptosis (34). The ratio of Bcl-2 to Bax controls the
occurrence of apoptosis, whereby an increased ratio of Bcl-2 to Bax
promotes cell survival and a decreased ratio promotes apoptosis
(35). Caspases are a class of
proteases instrumental in performing a number of cellular functions
including cell differentiation, remodeling and death (36). Caspase-3 is a member of the caspase
family, which regulates the execution of the mammalian apoptotic
cell death program (36,37). Caspase-3 is the primary terminal in
the process of cell apoptosis shear enzyme, an important mechanism
of cell death following ASCI (4).
Caspase-3 associated apoptotic pathways are activated following
traumatic spinal cord injury in rats and occur early in neurons in
the injury site and h to days later in adjacent gliocytes, distant
from the injury site. TIIA may protect damaged neurons and CNS
tissues from apoptosis by regulating the expression of apoptosis
factors, such as Bcl-2, Bax and caspase-3 (8,17,38–40).
In the present study, to investigate the protective
effects of a combination treatment with TIIA and MP on the ASCI
model, the factors associated with apoptosis were investigated. The
data indicated that a combined treatment may markedly reverse the
increase in pro-apoptosis factors Bax and caspase-3, and the
decreased anti-apoptosis factor Bcl-2 protein induced by ASCI in
vivo and in vitro. To the best of our knowledge, this is
the first evidence that TIIA, combined with MP, may confer marked
protection at a molecular level against ASCI in vivo. A
previous study considered that MP may protect the oligodendrocytes
but not neurons following spinal cord injury in vitro and
in vivo (41). However, in
the present study, the double-labeling immunofluorescence indicates
that the expression of caspase-3(+)/β-III Tubulin (+) cells was
significantly lower in the MP group and combined treatment group
than in the ASCI group in vivo. These data demonstrated that
combined treatment may protect neurons from apoptosis following
ASCI with the same effectiveness as MP treatment alone.
Secondary injuries develop hours to days following
primary injuries and involve a number of pathophysiological changes
including ischemia, ion infiltration, production of oxygen free
radicals and lipid peroxidation (7).
The spinal cord consists largely of lipids and is easily damaged by
free radical-induced lipid peroxidation, a major pathophysiological
mechanism of secondary neuronal and glial damage (9). During this process, the balance between
antioxidants and pro-oxidants is disrupted. For example, SOD, which
is a scavenger for reactive oxygen species (ROS), is consumed
during oxidative stress. MDA, formed from the breakdown of
polyunsaturated fatty acids, serves as an important and reliable
index for determining the extent of peroxidation reactions
(42). Oxygen free radicals are
typically produced in the mitochondria and their harmful effects
are eliminated by antioxidant systems. Consistent with previous
studies (43,44), the results of the current study
demonstrated that levels of MDA increased in the ASCI group and
significantly decreased in the MP and combined treatment groups.
However, no significant difference was observed between the
expression of MDA between the combined treatment and MP groups on
day 1 and 7. In addition, SOD levels also decreased in the ASCI
group as compared with the sham group (data not shown) and the
combined treatment and MP groups may increase the level of SOD in
the blunt spinal cord injury tissue in the ASCI group.
NF-κB was key to the inflammatory action due to its
regulatory role on the expression of a variety of cytokines (such
as TNF-α and IL-6) that regulate the inflammatory response
(25,45). As a regulator of death and survival
proteins, NF-κB serves an important role in neuron survival in the
CNS. A previous study revealed that NF-κB expression increased
rapidly following the occurrence of ASCI, exhibiting an effect of
enlarging the inflammatory cascade reaction and programmed cell
death (26). The activation of NF-κB
was closely linked to neuronal death from excitotoxicity and
inhibiting NF-κB activation deterred the process of neural cell
death. The inhibition of inflammatory responses at the early stage
of ASCI may constitute an attractive therapeutic strategy for ASCI.
Similar to previous studies (46,47), the
present study observed that the increase of NF-κB induced in
contusion spinal cord was significantly reversed with the treatment
of TIIA monotherapy, MP monotherapy and the combined treatment.
However, there was no significant difference between the expression
of NF-κB in the combined treatment and MP groups.
In conclusion, the present study demonstrates that
TIIA combined with a low dose of MP may protect the spinal cord
from ASCI due to its antioxidant, anti-inflammatory and
anti-apoptosis properties in the spinal cord tissue following ASCI.
The current study, to the best of our knowledge, is the first to
reveal that TIIA combined with low dose MP therapy has the
equivalent efficiency of a full dose of MP monotherapy in
vivo and in vitro. Even though the present study has
limitations, for example that the dosage of TIIA and MP in
vivo was chosen artificially and the observation time was
short, we believe that the combined treatment of TIIA and MP may be
a promising strategy of pharmacological therapy for rapid
initiation of neuroprotection following ASCI and reduce the dosage
of MP in the treatment of ASCI for the same neuroprotective effect
and further research should focus on exploring the biological and
the long-term effects of combined treatment.
Acknowledgements
The authors would like to thank Dr. Hui Kang (Wuhan
General Hospital of Guangzhou Military Command, Wuhan, China) for
his advice about the experiment design and Professor Yi Zhang
(Wuhan General Hospital of Guangzhou Military Command, Wuhan,
China) for his technical assistance and his assistance with rat
husbandry.
References
|
1
|
Singh A, Tetreault L, Kalsi-Ryan S, Nouri
A and Fehlings MG: Global prevalence and incidence of traumatic
spinal cord injury. Clin Epidemiol. 6:309–331. 2014.PubMed/NCBI
|
|
2
|
Evaniew N, Belley-Côté EP, Fallah N,
Noonan VK, Rivers CS and Dvorak MF: Methylprednisolone for the
treatment of patients with acute spinal cord injuries: A systematic
review and meta-analysis. J Neurotrauma. 33:468–481. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Choi DW and Rothman SM: The role of
glutamate neurotoxicity in hypoxic-ischemic neuronal death. J
Neurotrauma. 13:171–182. 1990.
|
|
4
|
Emery E, Aldana P, Bunge MB, Puckett W,
Srinivasan A, Keane RW, Bethea J and Levi AD: Apoptosis after
traumatic human spinal cord injury. J Neurosurg. 89:911–920. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hall ED and Braughler JM: Free radicals in
CNS injury. Res Publ Assoc Res Nerv Ment Dis. 71:81–105.
1993.PubMed/NCBI
|
|
6
|
Blight AR: Macrophages and inflammatory
damage in spinal cord injury. J Neurotrauma. 9:(Suppl 1). S83–S91.
1992.PubMed/NCBI
|
|
7
|
Lou J, Lenke LG, Ludwig FJ and O'Brien MF:
Apoptosis as a mechanism of neuronal cell death following acute
experimental spinal cord injury. Spinal Cord. 36:683–690. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yin X, Yin Y, Cao FL, Chen YF, Peng Y, Hou
WG, Sun SK and Luo ZJ: Tanshinone IIA attenuates the inflammatory
response and apoptosis after traumatic injury of the spinal cord in
adult rats. PLoS One. 7:e383812012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Silva NA, Sousa N, Reis RL and Salgado AJ:
From basics to clinical: A comprehensive review on spinal cord
injury. Prog Neurobiol. 114:25–57. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kwon BK, Tetzlaff W, Grauer JN, Beiner J
and Vaccaro AR: Pathophysiology and pharmacologic treatment of
acute spinal cord injury. Spine J. 4:451–464. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oh SK and Jeon SR: Current concept of stem
cell therapy for spinal cord injury: A review. Korean J
Neurotrauma. 12:40–46. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bracken MB, Shepard MJ, Collins WF Jr,
Holford TR, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers L, Maroon
JC, Marshall LF, et al: Methylprednisolone or naloxone treatment
after acute spinal cord injury: 1-year follow-up data. Results of
the second national acute spinal cord injury study. J Neurosurg.
76:23–31. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bracken MB, Shepard MJ, Collins WF,
Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers
L, Maroon J, et al: A randomized, controlled trial of
methylprednisolone or naloxone in the treatment of acute
spinal-cord injury. Results of the second national acute spinal
cord injury study. N Engl J Med. 322:1405–1411. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bracken MB, Collins WF, Freeman DF,
Shepard MJ, Wagner FW, Silten RM, Hellenbrand KG, Ransohoff J, Hunt
WE, Perot PL Jr, et al: Efficacy of methylprednisolone in acute
spinal cord injury. JAMA. 251:45–52. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Harrop JS: Spinal cord injury: Debating
the efficacy of methylprednisolone. Neurosurgery. 61:(Suppl 1).
S30–S31. 2014. View Article : Google Scholar
|
|
16
|
Walters BC, Hadley MN, Hurlbert RJ, Aarabi
B, Dhall SS, Gelb DE, Harrigan MR, Rozelle CJ, Ryken TC, Theodore
N, et al: Guidelines for the management of acute cervical spine and
spinal cord injuries: 2013 update. Neurosurgery. 60:(Suppl 1).
S82–S91. 2013. View Article : Google Scholar
|
|
17
|
Liu T, Jin H, Sun QR, Xu JH and Hu HT: The
neuroprotective effects of tanshinone IIA on ß-amyloid-induced
toxicity in rat cortical neurons. Neuropharmacology. 59:595–604.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu Z, Wang J, Huang E, Gao S, Li H, Lu J,
Tian K, Little PJ, Shen X, Xu S and Liu P: Tanshinone IIA
suppresses cholesterol accumulation in human macrophages: Role of
heme oxygenase-1. J Lipid Res. 55:201–213. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yin Y, Sun W, Li Z, Zhang B, Cui H, Deng
L, Xie P, Xiang J and Zou J: Effects of combining
methylprednisolone with rolipram on functional recovery in adult
rats following spinal cord injury. Neurochem Int. 62:903–912. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kaech S and Banker G: Culturing
hippocampal neurons. Nat Protoc. 1:2406–2415. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Boomkamp SD, McGrath MA, Houslay MD and
Barnett SC: Epac and the high affinity rolipram binding conformer
of PDE4 modulate neurite outgrowth and myelination using an in
vitro spinal cord injury model. Br J Pharmacol. 171:2385–2398.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Burnette WN: ‘Western blotting’:
Electrophoretic transfer of proteins from sodium dodecyl
sulfate-polyacrylamide gels to unmodified nitrocellulose and
radiographic detection with antibody and radioiodinated protein A.
Anal Biochem. 112:195–203. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Basso DM, Beattie MS and Bresnahan JC: A
sensitive and reliable locomotor rating scale for open field
testing in rats. J Neurotrauma. 12:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tang Q, Han R, Xiao H, Shen J, Luo Q and
Li J: Neuroprotective effects of tanshinone IIA and/or
tetramethylpyrazine in cerebral ischemic injury in vivo and in
vitro. Brain Res. 1488:81–91. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sun S, Yin Y, Yin X, Cao F, Luo D, Zhang
T, Li Y and Ni L: Anti-nociceptive effects of Tanshinone IIA (TIIA)
in a rat model of complete Freund's adjuvant (CFA)-induced
inflammatory pain. Brain Res Bull. 88:581–588. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu J, Fan G, Chen S, Wu Y, Xu XM and Hsu
CY: Methylprednisolone inhibition of TNF-alpha expression and NF-kB
activation after spinal cord injury in rats. Brain Res Mol Brain
Res. 59:135–142. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
A randomized, controlled trial of
methylprednisolone or naloxone in the treatment of acute
spinal-cord injury. N Engl J Med. 323:1207–1209. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ito Y, Sugimoto Y, Tomioka M, Kai N and
Tanaka M: Does high dose methylprednisolone sodium succinate really
improve neurological status in patient with acute cervical cord
injury? A prospective study about neurological recovery and early
complications. Spine (Phila Pa 1976). 34:2121–2124. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Suberviola B, González-Castro A, Llorca J,
Ortiz-Melón F and Miñambres E: Early complications of high-dose
methylprednisolone in acute spinal cord injury patients. Injury.
39:748–752. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Matsumoto T, Tamaki T, Kawakami M, Yoshida
M, Ando M and Yamada H: Early complications of high-dose
methylprednisolone sodium succinate treatment in the follow-up of
acute cervical spinal cord injury. Spine (Phila Pa 1976).
26:426–430. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chikuda H, Yasunaga H, Takeshita K,
Horiguchi H, Kawaguchi H, Ohe K, Fushimi K and Tanaka S: Mortality
and morbidity after high-dose methylprednisolone treatment in
patients with acute cervical spinal cord injury: A
propensity-matched analysis using a nationwide administrative
database. Emerg Med J. 31:201–206. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lu J, Ashwell KW and Waite P: Advances in
secondary spinal cord injury: Role of apoptosis. Spine (Phila Pa
1976). 25:1859–1866. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mautes AE, Weinzierl MR, Donovan F and
Noble LJ: Vascular events after spinal cord injury: Contribution to
secondary pathogenesis. Phys Ther. 80:673–687. 2000.PubMed/NCBI
|
|
34
|
Kroemer G, Galluzzi L and Brenner C:
Mitochondrial membrane permeabilization in cell death. Physiol Rev.
87:99–163. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Korsmeyer SJ, Shutter JR, Veis DJ, Merry
DE and Oltvai ZN: Bcl-2/Bax: A rheostat that regulates an
anti-oxidant pathway and cell death. Semin Cancer Biol. 4:327–332.
1993.PubMed/NCBI
|
|
36
|
Thornberry NA: The caspase family of
cysteine proteases. Br Med Bull. 53:478–490. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Miller DK: The role of the Caspase family
of cysteine proteases in apoptosis. Semin Immunol. 9:35–49. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Xia WJ, Yang M, Fok TF, Li K, Chan WY, Ng
PC, Ng HK, Chik KW, Wang CC, Gu GJ, et al: Partial neuroprotective
effect of pretreatment with tanshinone IIA on neonatal
hypoxia-ischemia brain damage. Pediatr Res. 58:784–790. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Meng XF, Zou XJ, Peng B, Shi J, Guan XM
and Zhang C: Inhibition of ethanol-induced toxicity by tanshinone
IIA in PC12 cells. Acta Pharmacol Sin. 27:659–664. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Dong H, Mao S, Wei J, Liu B, Zhang Z,
Zhang Q and Yan M: Tanshinone IIA protects PC12 cells from
beta-amyloid(25–35)-induced apoptosis via PI3K/Akt signaling
pathway. Mol Biol Rep. 39:6495–6503. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lee JM, Yan P, Xiao Q, Chen S, Lee KY, Hsu
CY and Xu J: Methylprednisolone protects oligodendrocytes but not
neurons after spinal cord injury. J Neurosci. 28:3141–3149. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ege E, Ilhan A, Gurel A, Akyol O and Ozen
S: Erdosteine ameliorates neurological outcome and oxidative stress
due to ischemia/reperfusion injury in rabbit spinal cord. Eur J
Vasc Endovasc Surg. 28:379–386. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Topsakal C, Erol FS, Ozveren MF, Yilmaz N
and Ilhan N: Effects of methylprednisolone and dextromethorphan on
lipid peroxidation in an experimental model of spinal cord injury.
Neurosurg Rev. 25:258–266. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fu J, Huang H, Liu J, Pi R, Chen J and Liu
P: Tanshinone IIA protects cardiac myocytes against oxidative
stress-triggered damage and apoptosis. Eur J Pharmacol.
568:213–221. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Sadeghi A, Ebrahimi Seyyed SS, Golestani A
and Meshkani R: Resveratrol Ameliorates Palmitate-Induced
inflammation in skeletal muscle cells by attenuating oxidative
stress and JNK/NF-KB pathway in a SIRT1-independent mechanism. J
Cell Biochem. Jan 6–2017.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen Y, Wu X, Yu S, Lin X, Wu J, Li L,
Zhao J and Zhao Y: Neuroprotection of tanshinone IIA against
cerebral ischemia/reperfusion injury through inhibition of
macrophage migration inhibitory factor in rats. PLoS One.
7:e401652012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chengke L, Weiwei L, Xiyang W, Ping W,
Xiaoyang P, Zhengquan X, Hao Z, Penghui Z and Wei P: Effect of
infliximab combined with methylprednisolone on expressions of
NF-κB, TRADD, and FADD in rat acute spinal cord injury. Spine
(Phila Pa 1976). 38:E861–E869. 2013. View Article : Google Scholar : PubMed/NCBI
|