|
1
|
Collins MM, Stafford RS, O'Leary MP and
Barry MJ: Distinguishing chronic prostatitis and benign prostatic
hyperplasia symptoms: Results of a national survey of physician
visits. Urology. 53:921–925. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Roberts RO, Lieber MM, Rhodes T, Girman
CJ, Bostwick DG and Jacobsen SJ: Prevalence of a physician-assigned
diagnosis of prostatitis: The Olmsted County study of urinary
symptoms and health status Among Men. Urology. 51:578–584. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tan JK, Png DJ, Liew LC, Li MK and Wong
ML: Prevalence of prostatitis-like symptoms in Singapore: A
population-based study. Singap Med J. 43:189–193. 2002.
|
|
4
|
Ku JH, Kim ME, Lee NK and Park YH:
Influence of environmental factors on chronic prostatitis-like
symptoms in young men: Results of a community-based survey.
Urology. 58:853–858. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Krieger JN, Riley DE, Cheah PY, Liong ML
and Yuen KH: Epidemiology of prostatitis: New evidence for a
world-wide problem. World J Urol. 21:70–74. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Guo YH and Li HJ: ProstatitisPeople's
Military Medical Press; Beijing; pp. 682007
|
|
7
|
Krieger JN, Nyberg LJ Jr and Nickel JC:
NIH Consensus definition and classification of prostatitis. JAMA.
282:236–237. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Quick ML, Wong L, Mukherjee S, Done JD,
Schaeffer AJ and Thumbikat P: Th1-Th17 cells contribute to the
development of uropathogenic Escherichia coli-induced chronic
pelvic pain. PLoS One. 8:e609872013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang K: Guide for the Diagnosis and
Treatment of Prostatitis. People's Medical Publishing House;
Beijing: 2009
|
|
10
|
Rowe E, Smith C, Laverick L, Elkabir J,
Witherow RO and Patel A: A prospective, randomized, placebo
controlled, double-blind study of pelvic electromagnetic therapy
for the treatment of chronic pelvic pain syndrome with 1 year of
followup. J Urol. 173:2044–2047. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Seethalakshmi L, Bala RS, Malhotra RK,
Austin-Ritchie T, Miller-Graziano C, Menon M and Luber-Narod J: 17
beta-estradiol induced prostatitis in the rat is an autoimmune
disease. J Urol. 156:1838–1842. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mahal BA, Cohen JM, Allsop SA, Moore JB,
Bhai SF, Inverso G and Dimitrakoff JD: The role of phenotyping in
chronic prostatitis/chronic pelvic pain syndrome. Curr Urol Rep.
12:297–303. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wagenlehner FM, Pilatz A, Bschleipfer T,
Diemer T, Linn T, Meinhardt A, Schagdarsurengin U, Dansranjavin T,
Schuppe HC and Weidner W: Bacterial prostatitis. World J Urol.
31:711–716. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cua DJ, Sherlock J, Chen Y, Murphy CA,
Joyce B, Seymour B, Lucian L, To W, Kwan S, Churakova T, et al:
Interleukin-23 rather than interleukin-12 is the critical cytokine
for autoimmune inflammation of the brain. Nature. 421:744–748.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Park H, Li Z, Yang XO, Chang SH, Nurieva
R, Wang YH, Wang Y, Hood L, Zhu Z, Tian Q and Dong C: A distinct
lineage of CD4 T cells regulates tissue inflammation by producing
interleukin 17. Nat Immunol. 6:1133–1141. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Langrish CL, Chen Y, Blumenschein WM,
Mattson J, Basham B, Sedgwick JD, McClanahan T, Kastelein RA and
Cua DJ: IL-23 drives a pathogenic T cell population that induces
autoimmune inflammation. J Exp Med. 201:233–240. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lubberts E, Koenders MI, Oppers-Walgreen
B, van den Bersselaar L, Coenen-de Roo CJ, Joosten LA and van den
Berg WB: Treatment with a neutralizing anti-murine interleukin-17
antibody after the onset of collagen induced arthritis reduces
joint inflammation, cartilage destruction, and bone erosion.
Arthritis Rheum. 50:650–659. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Miller LJ, Fischer KA, Goralnick SJ, Litt
M, Burleson JA, Albertsen P and Kreutzer DL: Nerve growth factor
and chronic prostatitis/chronic pelvic pain syndrome. Urology.
59:603–608. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Arms L, Girard BM, Malley SE and Vizzard
MA: Expression and function of CCL2/CCR2 in rat micturition
reflexes and somatic sensitivity with urinary bladder inflammation.
Am J Physiol Renal Physiol. 305:F111–F122. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Donadio AC and Depiante-Depaoli M:
Inflammatory cells and MHC class II antigens expression in prostate
during time-course experimental autoimmune prostatitis development.
Clin Immunol Immunopathol. 85:158–165. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schmidt R, Schmelz M, Ringkamp M,
Handwerker HO and Torebjörk HE: Innervation territories of
mechanically activated C nociceptor units in human skin. J
Neurophysiol. 78:2641–2648. 1997.PubMed/NCBI
|
|
22
|
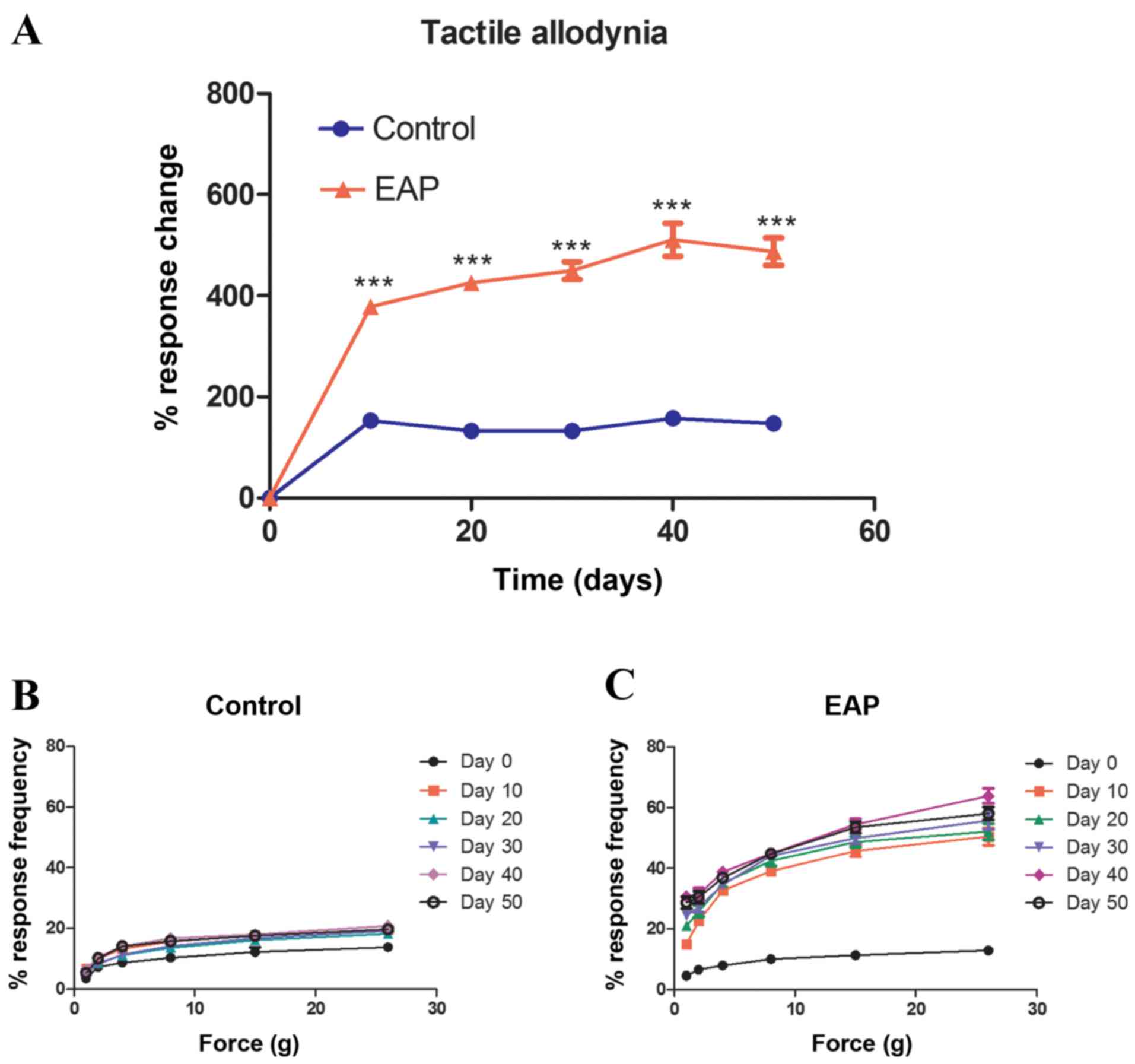
Rudick CN, Schaeffer AJ and Thumbikat P:
Experimental autoimmune prostatitis induces chronic pelvic pain. Am
J Physiol Regul Integr Comp Physiol. 294:R1268–R1275. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fen ZG, Yan WJ, Zhang J and Xu Y: Effects
of Calcium Concentration on the Soluble Gq Protein α Subunit in the
Photoreceptor Cell of Macrobrachium rosenbergi on Light Adaptation
and Dark Adaptation. Zoolog Res. 24:373–376. 2003.
|
|
25
|
Depiante-Depaoli M and Pacheco-Rupil B:
Experimental autoimmunity to rat male accessory glands (MAG):
Circulating antibodies, immunoglobulins bound to target glands, and
immunoglobulins-secreting cells. Am J Reprod Immunol Microbiol.
7:32–38. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schaeffer AJ: Clinical practice. Chronic
prostatitis and the chronic pelvic pain syndrome. N Engl J Med.
355:1690–1698. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
John H, Barghorn A, Funke G, Sulser T,
Hailemariam S, Hauri D and Joller-Jemelka H: Noninflammatory
chronic pelvic pain syndrome: Immunological study in blood,
ejaculate and prostate tissue. Eur Urol. 39:72–78. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pontari MA: Chronic prostatitis/chronic
pelvic pain syndrome in elderly men: Toward better understanding
and treatment. Drugs Aging. 20:1111–1125. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Orhan I, Onur R, Ilhan N and Ardiçoglu A:
Seminal plasma cytokine levels in the diagnosis of chronic pelvic
pain syndrome. Int J Urol. 8:495–499. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Alexander RB, Ponniah S, Hasday J and
Hebel JR: Elevated levels of proinflammatory cytokines in the semen
of patients with chronic prostatitis/chronic pelvic pain syndrome.
Urology. 52:744–749. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhang ZY and Schluesener HJ: HDAC
inhibitor MS-275 attenuates the inflammatory reaction in rat
experimental autoimmune prostatitis. Prostate. 72:90–99. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shahed AR and Shoskes DA: Correlation of
beta-endorphin and prostaglandin E2 levels in prostatic fluid of
patients with chronic prostatitis with diagnosis and treatment
response. J Urol. 166:1738–1741. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Taguchi O and Nishizuka Y: Self tolerance
and localized autoimmunity. Mouse models of autoimmune disease that
suggest tissue-specific suppressor T cells are involved in self
tolerance. J Exp Med. 165:146–156. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Motrich RD, Maccioni M, Riera CM and
Rivero VE: Autoimmune prostatitis: State of the art. Scand J
Innunol. 66:217–227. 2007. View Article : Google Scholar
|
|
35
|
Pacheco-Rupil B, Depiante-Depaoli M and
Casadio B: Experimental autoimmune damage to rat male accessory
glands. II. T cell requirement in adoptive transfer of specific
tissue damage. Am J Reprod Immunol. 5:15–19. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ishigooka M, Zermann DH, Doggweiler R and
Schmidt RA: Similarity of distributions of spinal c-fos and plasma
extravasation after acute chemical irritation of the bladder and
the prostate. J Urol. 164:1751–1756. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Quick ML, Wong L, Mukherjee S, Done JD,
Schaeffer AJ and Thumbikat P: Th 1-Th 17 cells contribute to the
development of uropathogenic Escherichia coli-induced chronic
pelvic pain. PLoS One. 8:e609872013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Day YJ, Liou JT, Lee CM, Lin YC, Mao CC,
Chou AH, Liao CC and Lee HC: Lack of interleukin-17 leads to a
modulated micro-environment and amelioration of mechanical
hypersensitivity after peripheral nerve injury in mice. Pain.
155:1293–1302. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
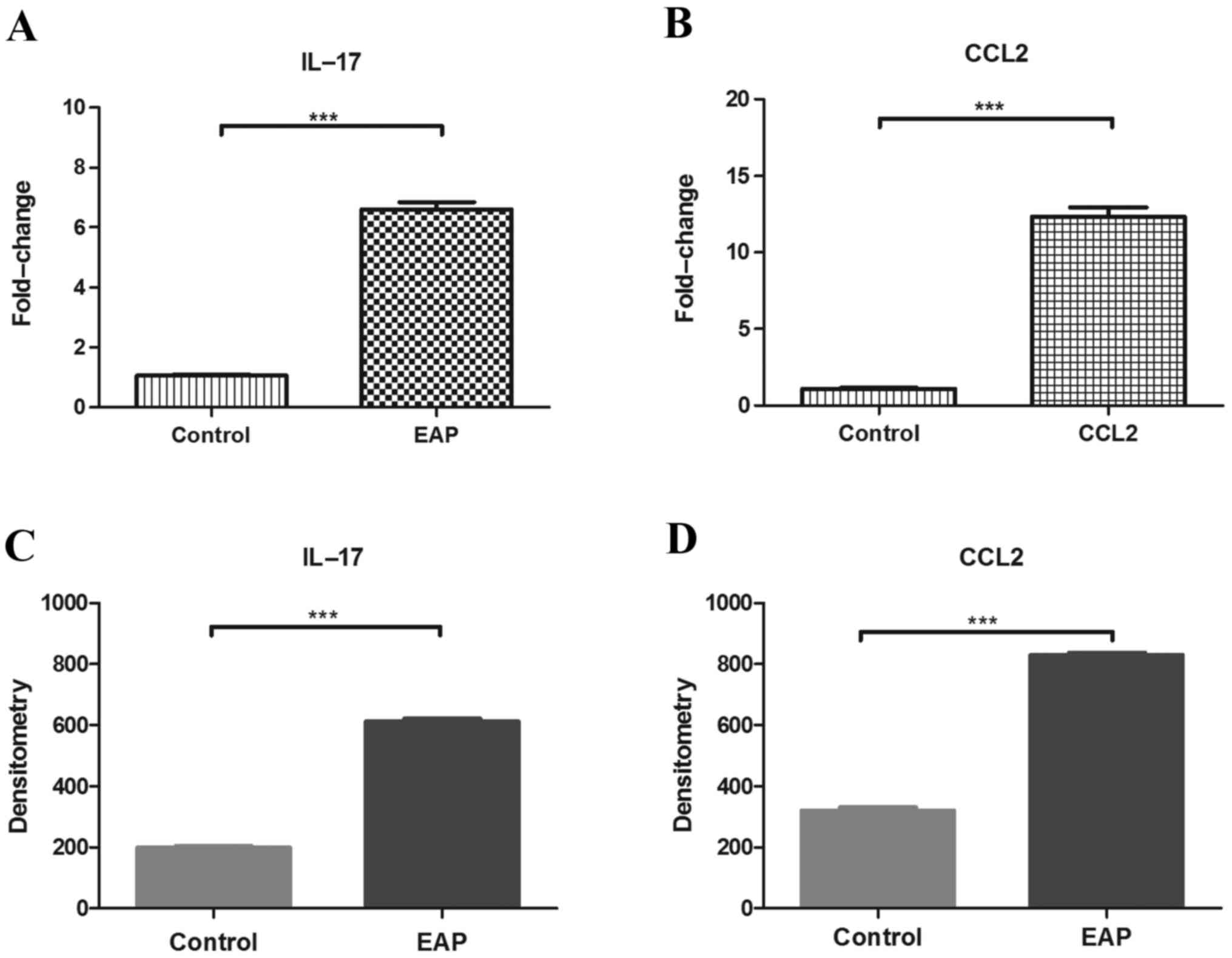
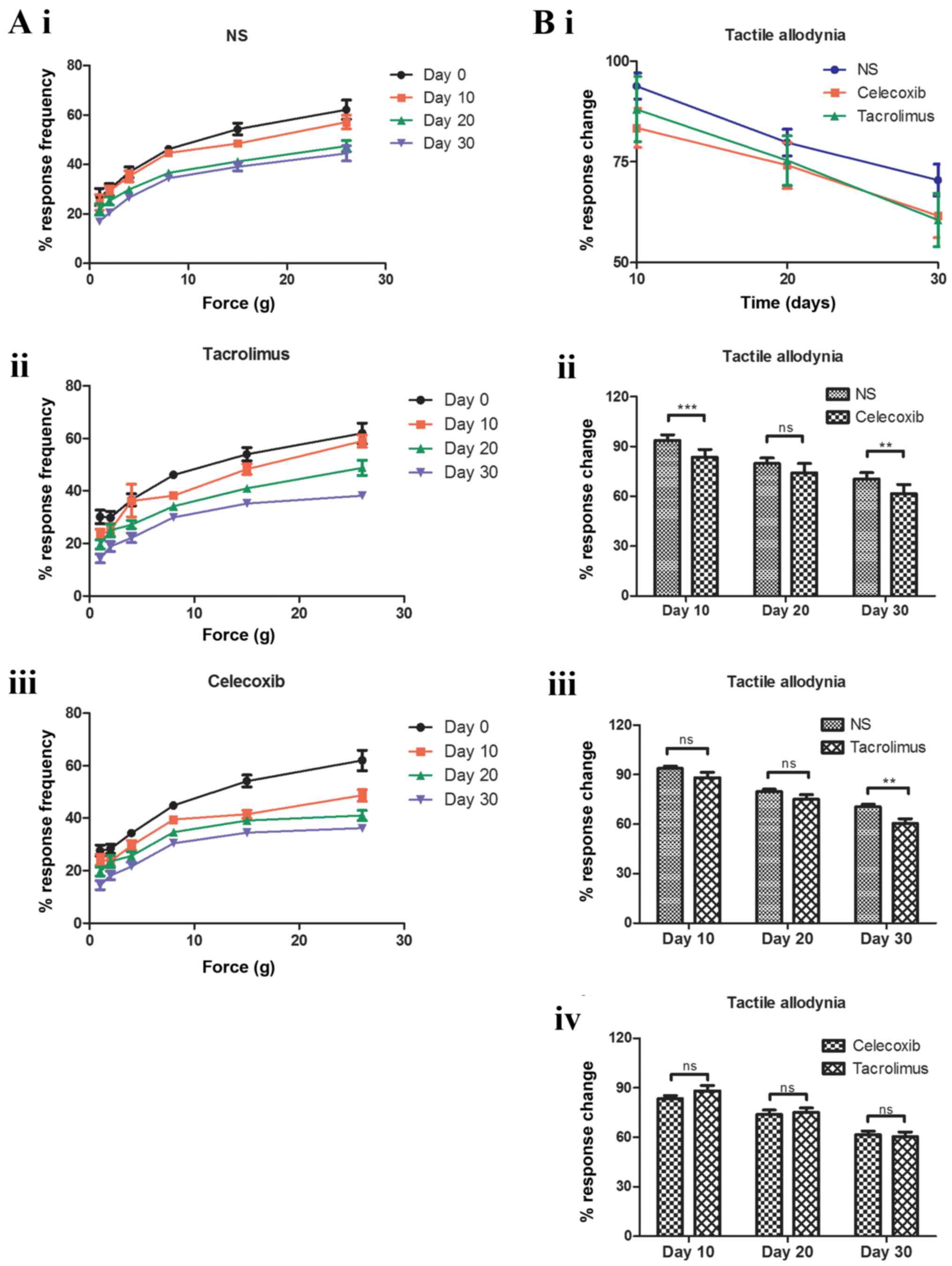
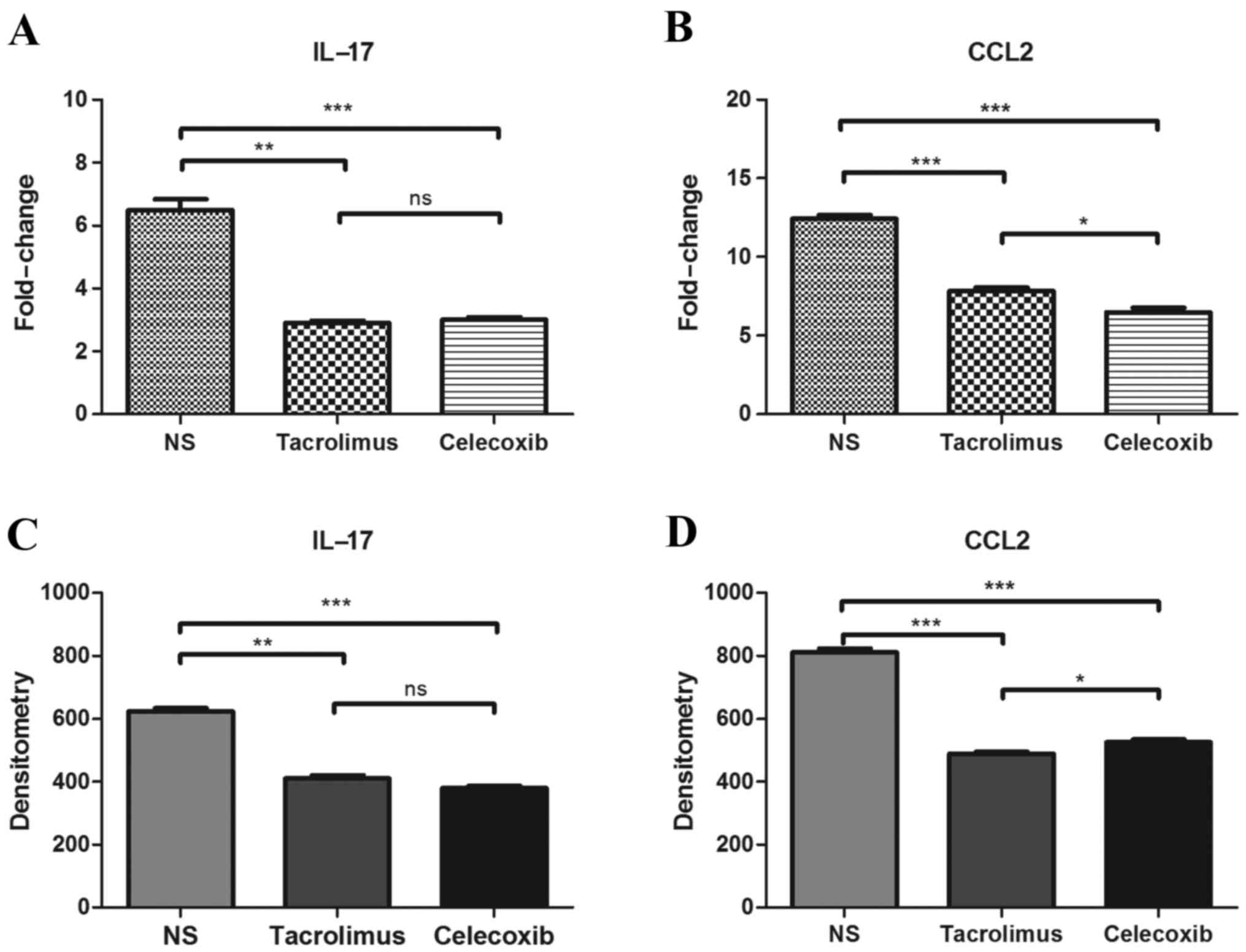
Murphy SF, Schaeffer AJ, Done J, Wong L,
Bell-Cohn A, Roman K, Cashy J, Ohlhausen M and Thumbikat P: IL17
Mediates Pelvic Pain in Experimental Autoimmune Prostatitis (EAP).
PLoS One. 10:e01256232015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Quick ML, Mukherjee S, Rudick CN, Done JD,
Schaeffer AJ and Thumbikat P: CCL2 and CCL3 are essential mediators
of pelvic pain in experimental autoimmune prostatitis. Am J Physiol
Regul Integr Comp Physiol. 303:R580–R589. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Rivero VE, Cailleau C, Depiante-Depaoli M,
Riera CM and Carnaud C: Non-obese diabetic (NOD) mice are
genetically susceptible to experimental autoimmune prostatitis
(EAP). J Autoimmun. 11:603–610. 1998. View Article : Google Scholar : PubMed/NCBI
|