Introduction
As one of the major pathological causes of patellar
dislocation, femoral trochlear dysplasia has an incidence of 85–96%
(1,2), and is typically caused by genetic
factors (3). Under normal
conditions, when a knee joint flexes 20° from the fully extended
position, the patella is only able to shift inward by 5 mm
(4). Only when the flexion reaches
20–30° do the patellofemoral joints align perfectly (4). Morphological changes of the femoral
trochlea in these patients may cause abnormal patella movement and
lead to patella dislocation (5). The
clinical diagnosis of femoral trochlear dysplasia primarily relies
on imaging diagnosis. Historically, plain imaging has been the
major source of diagnosis (6). A
sulcus angle of >150° on an axial radiograph is considered to
indicate femoral trochlear dysplasia (6). However, in axial radiographs, the
trochlear groove displayed is located on the distal side of the
femoral trochlea, which does not represent the true morphology of
the proximal trochlea (6). As such,
the reliability of this method was considerably low (6). Furthermore, in 96% of patients with
trochlear dysplasia, lateral radiography revealed the femoral
trochlear groove crossing through the medial and lateral femoral
condylar bumps, appearing as a ‘crossing sign’ or ‘supratrochlear
spur’ when the medial and lateral femoral condyles overlapped
(7). This imaging method has several
limitations, including the required scanning posture and
difficulties in attaining quantitative measurements (8–10).
A study by Dejour and Le Coultre (7) classified femoral trochlear morphologies
into four types: (A) Normal trochlear shape, but shallow trochlear
groove; (B) markedly flattened or even convex trochlea; (C)
trochlear facet asymmetry, with an overly high lateral facet and a
hypoplastic medial facet; and (D) type C features and vertical
links between facets or cliff pattern. Computed tomography (CT) is
not able to reveal articular cartilage, and so the femoral trochlea
observed on CT images based on the bone landmarks does not reflect
its true morphology. In contrast, magnetic resonance imaging (MRI)
has the advantages of projecting articular cartilage and the
surrounding ligaments and muscles, thus this imaging modality has
become the basic method for evaluating femoral trochlear dysplasia.
However, regardless of whether CT or MRI is used, due to the
variety and complicated morphological structures of the proximal
trochlea, multiple deepest points of the trochlear groove have
often been observed when diagnosing severe trochlear dysplasia
(types B-D), causing difficulties in confirming the desired
anatomical landmarks (8). This
ambiguity reduces measurement reliability and complicates the
preoperative diagnosis. Previous studies have reported multiple
methods by which the deepest point of the trochlear groove may be
located from MRIs (9,11). However, whether these methods are
able to accurately find the anatomic landmark and correctly
diagnose trochlear dysplasia remains uncertain (11). The aim of the present study was to
determine the measurement values of severe trochlear dysplasia
acquired from MRI and to investigate the application values of MRI,
such that more evidence may be gained for clinical assessment, and
to determine the differences in measurements between several
trochlear dysplasia patients and normal subjects.
Subjects and methods
Patients
A total of 59 patients (61 knees) from the Shanghai
Jiao Tong University Affiliated Sixth People's Hospital (Shanghai,
China) who demonstrated symptoms of patellar instability between
January 2013 and May 2014 were enrolled in the present study, and
30 healthy volunteers were enrolled as the control group. The
patient inclusion criteria were a medical history of >1 patellar
dislocation prior to admission and CT images of knees suggesting
severe trochlear dysplasia as Dejour types B-D, which were
determined according to the Dejour trochlear dysplasia system
(7). Exclusion criteria were as
follows: Osteoarthritis, meniscus tears, metabolic bone disease,
rheumatoid arthritis and a history of ipsilateral knee surgery.
There were 19 males and 40 females in the patient groups, with an
age range of 14–44 years (mean, 23.6 years). There were 31 cases in
the left knee and 30 cases in the right knee. The present study was
approved by the Ethics Committee of Shanghai Jiao Tong University
Affiliated Sixth People's Hospital and all patients provided
informed consent.
CT examination
All patients lay on their backs with their knee
fully extended whilst a plain CT scan was performed using a
LightSpeed VCT CT scan system (64 slices; GE Healthcare, Chicago,
IL, USA). The slice thickness and slice spacing were both 5 mm. The
tube current was set to 220 mA, and the tube voltage was set to 120
kV. Slice reconstruction was based on 0.625-mm-thick slices.
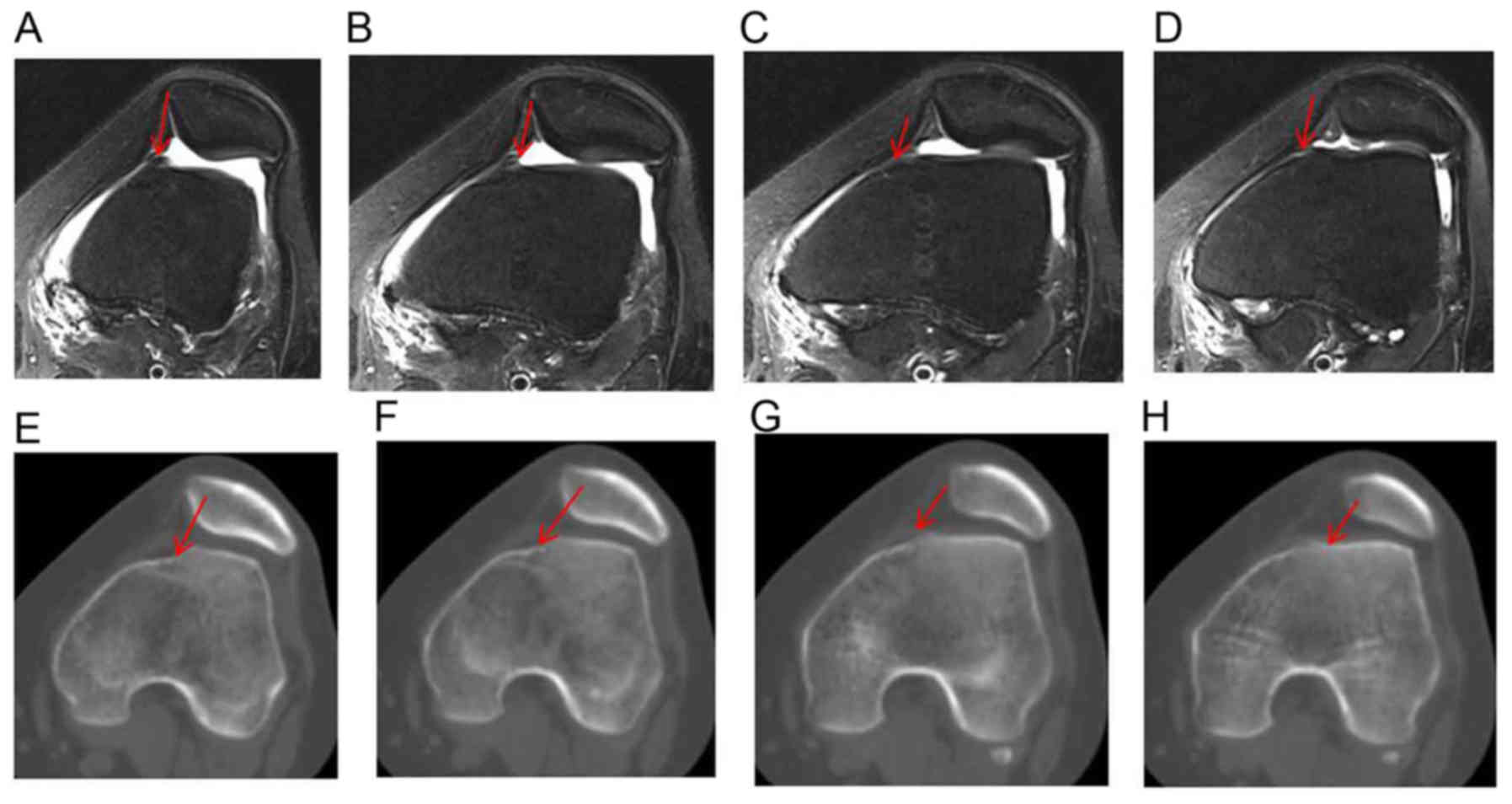
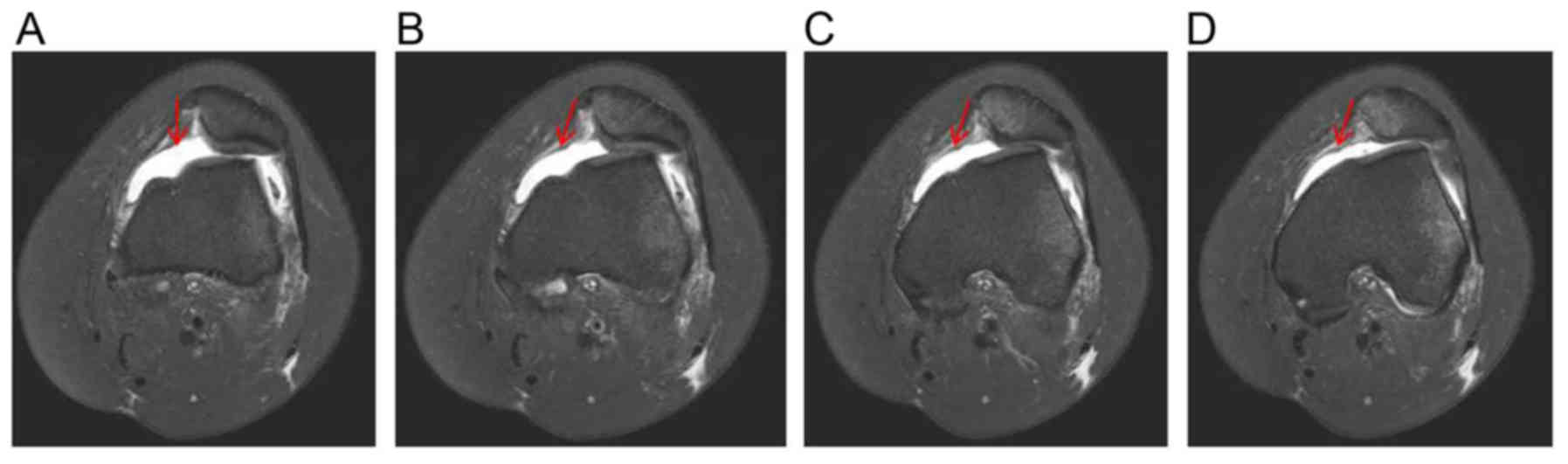
MRI examination and measurement
method
MRI examinations were performed with a Philips
Intera-Achieva 3.0T system with a standard knee coil (Philips
Medical Systems, Inc., Bothell, WA, USA). Patients and healthy
volunteers lay on their backs with knee flexion of 20–30°. The
major imaging techniques included cross sectional fast spin-echo T2
weighted image fat-suppressed sequences, with a slice thickness of
3 mm and a slice spacing of 0.3 mm. The most proximal images
revealing the complete medial and lateral facet cartilage of
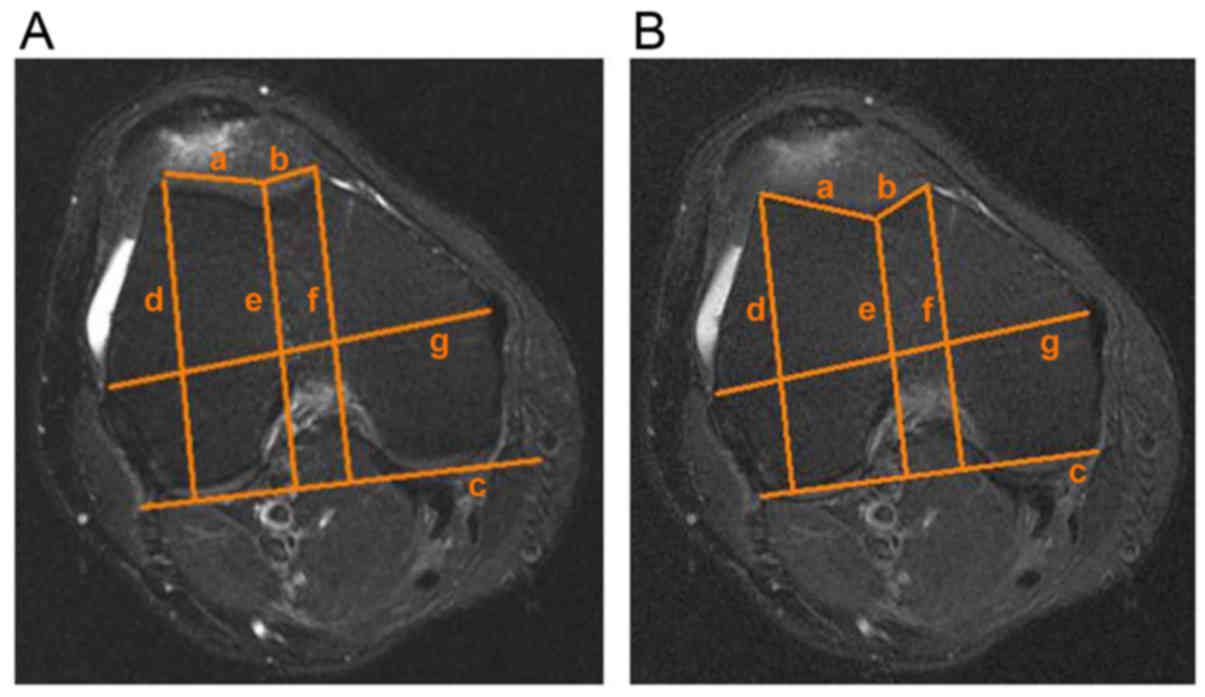
trochlea on craniocaudal MRI slices were selected (Figs. 1 and 2). Cartilage and subchondral bone landmarks
were used to compare a series of measurements, including the
femoral trochlear groove depth, the sulcus angle, the lateral
trochlear inclination, trochlear facet asymmetry, the femoral
medial and lateral condyle symmetry, and the ratios between the
femoral medial/lateral condyles and the maximal trochlear width
(Fig. 3). The following comparisons
were made: i) The differences in measurements between patient and
control groups based on cartilage and subchondral bone landmarks;
ii) differences in measurements based on cartilage and subchondral
bone landmarks within the patient and control groups; and iii)
differences in the sulcus angle, trochlear groove depth, the
lateral trochlear inclination and trochlear facet asymmetry among
patients with types B, C and D trochlear dysplasia. Measurement
values were independently determined by an orthopaedic physician
and a senior musculoskeletal radiologist blinded to patient
clinical data.
Statistical analysis
All statistical analysis was performed using SPSS
19.0 software (IBM Corp., Armonk, NY, USA). All data was
represented as mean ± standard error. Independent sample t-test was
used to compare the difference between the patient group and the
control group. Paired sample t-test was applied to the comparison
between the measurements by cartilage and subchondral bone
landmark. Kruskal-Wallis test was used to compare measurements
among patients with different types of trochlear dysplasia.
Intraclass correlation coefficient was used to compared the
inter-observer reliability (<0.2, poor; 0.2–0.4, moderate;
0.4–0.6, fair; 0.6–0.8, good; 0.8–1.0, very good). P<0.05 was
considered to indicate a statistically significant difference.
Results
Significant differences were observed in the femoral
trochlear groove depth, sulcus angle, lateral trochlear inclination
and trochlear facet asymmetry between the patient and control
groups (P<0.05; Table I).
However, no significant differences were observed between the two
groups in terms of the femoral medial and lateral condyle symmetry
and the ratios between the femoral medial/lateral condyles and the
maximal trochlear width (Table I).
When comparing within-group results, all indices based on the two
landmarks in the patient group, with the exception of the lateral
trochlear inclination (P=0.085), were significantly different
(P<0.05; Table II). All
measurements in the control group were statistically different
(P<0.05; Table II). No
significant differences were observed between patients with Dejour
types B, C and D, in the regard of sulcus angle
(x2=3.348; P=0.187), trochlear groove depth
(x2=1.809; P=0.405), lateral trochlear inclination
(x2=1.921; P=0.383) and trochlear facet asymmetry
(x2=1.363; P=0.506). In the observer credibility
evaluation, the intraclass correlation coefficient of a single
measurement and the mean measurement value was between good and
very good (0.691–0.869; P<0.05).
 | Table I.Intergroup comparisons of measurements
between patient and control groups based on cartilage and
subchondral bone landmarks. |
Table I.
Intergroup comparisons of measurements
between patient and control groups based on cartilage and
subchondral bone landmarks.
|
| Group |
|
|
|---|
|
|
|
|
|
|---|
| Measurements | Patient | Control | t value | P-value |
|---|
| Measurements based on
the cartilage landmark |
|
|
|
|
| Trochlear
groove depth, mm |
2.4±1.1 |
4.2±0.9 | −7.959 | <0.05 |
| Sulcus
angle, degrees |
160.3±8.7 |
146.9±4.1 | 8.03 | <0.05 |
| Trochlear
facet asymmetry |
0.4±0.1 |
0.5±0.1 | −6.377 | <0.05 |
| Lateral
trochlear inclination, degrees |
13.7±5.6 |
20.0±4.4 | −5.371 | <0.05 |
| Femoral
medial and lateral condyle symmetry |
1.1±0.1 |
1.1±0.0 | −0.263 | 0.793 |
| Ratio
between the femoral medial condyle and the maximal trochlear
width |
0.8±0.1 |
0.8±0.1 | 0.884 | 0.379 |
| Ratio
between the femoral lateral condyle and the maximal trochlear
width |
0.8±0.1 |
0.8±0.1 | 1.757 | 0.082 |
| Measurements based on
the subchondral bone landmark |
|
|
|
|
| Trochlear
groove depth, mm |
3.8±0.2 |
6.0±0.2 | −7.477 | <0.05 |
| Sulcus
angle, degrees |
149.2±1.0 |
138.6±1.0 | 7.589 | <0.05 |
| Trochlear
facet asymmetry |
0.4±0.1 |
0.6±0.0 | −6.434 | <0.05 |
| Lateral
trochlear inclination, degrees |
14.3±0.8 |
22.5±0.7 | −7.789 | <0.05 |
| Femoral
medial and lateral condyle symmetry |
1.0±0.0 |
1.0±0.0 | −1.373 | 0.173 |
| Ratio
between the femoral medial condyle and the maximal trochlear
width |
0.7±0.0 |
0.7±0.0 | 1.367 | 0.175 |
| Ratio
between the femoral lateral condyle and the maximal trochlear
width |
0.8±0.0 |
0.8±0.0 | 1.107 | 0.271 |
 | Table II.Intragroup comparisons of
measurements from patient and control groups based on cartilage and
subchondral bone landmarks. |
Table II.
Intragroup comparisons of
measurements from patient and control groups based on cartilage and
subchondral bone landmarks.
|
| Landmark |
|
|
|---|
|
|
|
|
|
|---|
| Measurements | Cartilage | Subchondral
bone | t value | P-value |
|---|
| Measurements within
the patient group |
|
|
|
|
|
Trochlear groove depth,
mm |
2.4±1.1 |
3.8±0.2 | −10.104 | <0.05 |
| Sulcus
angle, degrees |
160.3±8.7 |
149.2±1.0 | 12.075 | <0.05 |
|
Trochlear facet asymmetry |
0.4±0.1 |
0.4±0.1 | −3.522 | 0.001 |
| Lateral
trochlear inclination, degrees |
13.7±5.6 |
14.3±0.8 | −1.751 | 0.085 |
| Femoral
medial and lateral condyle symmetry |
1.1±0.1 |
1.0±0.0 | 6.363 | <0.05 |
| Ratio
between the femoral medial condyle and the maximal trochlear
width |
0.8±0.1 |
0.7±0.0 | 11.491 | <0.05 |
| Ratio
between the femoral lateral condyle and the maximal trochlear
width |
0.8±0.1 |
0.8±0.0 | 18.067 | <0.05 |
| Measurements within
the control group |
|
|
|
|
|
Trochlear groove depth,
mm |
4.2±0.9 |
6.0±0.2 | −8.649 | <0.05 |
| Sulcus
angle, degrees |
146.9±4.1 |
138.6±1.0 | 8.135 | <0.05 |
|
Trochlear facet asymmetry |
0.5±0.1 |
0.6±0.0 | −3.480 | 0.002 |
| Lateral
trochlear inclination, degrees |
20.0±4.4 |
22.5±0.7 | −3.372 | 0.002 |
| Femoral
medial and lateral condyle symmetry |
1.1±0.0 |
1.0±0.0 | 4.148 | <0.05 |
| Ratio
between the femoral medial condyle and the maximal trochlear
width |
0.8±0.1 |
0.7±0.0 | 9.772 | <0.05 |
| Ratio
between the femoral lateral condyle and the maximal trochlear
width |
0.8±0.1 |
0.8±0.0 | 14.299 | <0.05 |
Discussion
Patients with recurrent patellar dislocation often
have pathological origins of patellar instability, including
trochlear dysplasia, increased Tibial Tuberosity-Trochlear Groove
distance, patella alta and patellar tilt (1). Among these pathologies, trochlear
dysplasia has the highest incidence (1). In the present study, the purpose of
acquiring measurements for the femoral trochlea was to clarify the
fundamental factors of patellar dislocation and guide the surgical
method and postoperative follow-up (4). An MRI cross-sectional sequence is
important for the assessment of femoral trochlear dysplasia. A
study by Stefanik et al (12)
performed measurements on sections revealing the maximum posterior
femoral condyle, whereas a study by Keser et al (13) acquired measurements on the section
first revealing the lateral femoral trochlear cartilage on the
craniocaudal image. However, it may be hypothesised that under
normal circumstances the surface cartilage of the femoral trochlea
would align with the cartilage of the patella, thus the observed
cartilage surface may be closer to the true morphology of the
femoral trochlea. We believed that whether or not the surface
cartilage of the femoral trochlea is normal has a more profound
effect on patellofemoral joint function. Therefore, the
cross-section of the femoral trochlea at the craniocaudal positions
of an MRI study that revealed the most proximal complete medial and
lateral cartilage was chosen as the measurement section (14,15).
Unlike with CT imaging, the deepest point of the femoral trochlear
groove and measurement layer is able to be determined based on the
cartilage landmark with MRI in our patient group. In addition, on
this layer, the subchondral bone landmark also displays the deepest
point of the femoral trochlear groove.
The findings of the present study revealed that the
results based on the two landmarks were the same between the
patient and control groups. Except for the femoral medial and
lateral condyle symmetry, and the ratios between the femoral medial
and lateral condyles and the maximal trochlear width, all other
measurements were statistically significant. The sulcus angles of
the patient group measured in the present study were similar to the
MRI results of 162.5° reported in a study by Toms et al
(16). However, the measurement
value reported in a study by van Huyssteen et al (17) was 185°; this difference may be due to
the fact that the authors only chose the layers displaying the
lateral cartilage of the femoral trochlea with minor bumps. The
layer used in the present study was able to reveal both medial and
lateral cartilage, and the cartilage tissue appeared as small
concavities. A femoral trochlear groove depth <4 mm may be
indicative of dysplasia (18). The
measurements acquired in the present study were significantly
smaller than the reference value and were similar to the 2.5±1.38
mm value reported in a study by Köhlitz et al (19). These results suggest that the femoral
trochlear structure is flattened, resulting in poor alignment of
the patellofemoral joint. Measurements of the sulcus angle and
trochlear groove depth may serve as guides for the anteromedial
tibial tubercle transfer technique for the treatment of patellar
dislocation. A smaller sulcus angle and larger groove depth would
be more likely to cause excess medialization of the tibial tubercle
during surgery (19). This problem
may cause a collision between the patella and the medial facet of
the femoral trochlea, inducing pain (7). In the present study, assessment of the
lateral trochlear inclination based on both landmarks yielded
larger values than the results obtained in a study by Kamath et
al (20), which reported values
of 9.4° and 8.8° for the cartilage and subchondral landmarks,
respectively. The reason for this discrepancy may be the different
measurement layers used in these two studies; Kamath et al
(20) used the layer displaying the
maximal height of the lateral femoral condyle for measurements,
whereas the measurements used in the present study were based on
the cartilage landmark, and yielded similar results to those
obtained in a study by Charles et al (18) (13.31±1.36°). This abnormal lateral
trochlear inclination suggests that the antagonizing strength of
the lateral facet of the femoral trochlea against the lateral
translocation of the patella was weakened when the knee flexion
reached 30°, resulting in patellar dislocation (21). A study by Teng et al (22) suggested that the lateral trochlear
inclination was correlated with the incidence of patellar
dislocation and emphasized the significance of the lateral facet of
the trochlea in preventing patellar dislocation.
Studies regarding the association between the
heights of the medial/lateral femoral condyles and femoral
trochlear dysplasia have been rare. A study by Biedert and Bachmann
(15) reported that patients with
trochlear dysplasia had reduced absolute medial femoral condyle
heights. However, the absolute values were significantly different
among individuals. Therefore, in the present study ratios between
the medial/lateral condyle heights were used, the same as the
ratios between the femoral medial/lateral condyles and the maximal
trochlear width, to exclude the interference of differences between
individual cases. The results demonstrated that, in patients with
severe femoral trochlear dysplasia, the lateral condyle was higher
than the medial condyle. The results of the three indices were
similar to those of the control group. These results suggested that
femoral trochlear dysplasia should not alter the heights of the
medial and lateral condyles, as significant changes were not
observed in either height. The abnormal morphology of the joint
facets was suggested as the major pathological appearance of
trochlear dysplasia. A study by Van Haver et al (23) used the semi-automated landmark-based
3D image reconstruction technique and observed a higher medial
condyle in the sagittal position compared with the control group,
whereas the lateral condyle height was not significantly different.
However, the authors selected the sagittal layers through the
medial and lateral condyles of the femur, and so the changes in
medial condyle height in different layers may vary.
In the present study, the proximal medial and
lateral joint facets of the femoral trochlea were found to be
covered in cartilage in the control group. However, in the patient
group, only the lateral facet at the proximal femoral trochlea had
cartilage coverage. In addition, the lateral facet exhibited a bump
and cliff pattern alteration. The medial facet was observed as
cortical bone. The cartilage of the medial facet was gradually
visible distally. The simultaneous appearance of medial and lateral
cartilage joint facets was only observed at the central part of the
femoral trochlea at the craniocaudal position, and cartilage
coverage at the medial facet was rare. At this point, the deepest
point of the femoral trochlear groove could be identified. In
addition, the missing medial cartilage at the proximal trochlea
resulted in a higher position of the patellar joint cartilage
compared with the trochlear joint facet, which is referred to here
as ‘relatively patellar alta’. The ‘relatively patellar alta’
resulted in a malalignment of the patellofemoral joint, which may
induce patellar dislocation under minor external force. In the
present study, the smaller trochlear facet asymmetry of patients
compared with the control group also revealed abnormal morphology
of the femoral trochlea. A study by Nelitz and Lippacher (14) identified a bump pattern in the
proximal femoral trochlea in a comparative study using MRI and
arthroscope techniques to assess patients with severe femoral
trochlear dysplasia. Although the authors did observe a shallow
trochlear groove, the initial position of the groove was near the
far end, and the medial facet was accompanied by medial condylar
dysplasia. Using CT scans, a study by Hing et al (24) also observed a negative correlation
between the distance between the trochlear groove and the lateral
facet, and the stability of the patella. However, MRI was able to
demonstrate that a series of morphological changes were caused by
femoral trochlear dysplasia. In the present study, according to
such characteristic abnormal forms of the femoral trochlear, the
layers displaying the deepest points of the femoral trochlea on MRI
images were also identified on the corresponding CT images.
Intragroup comparisons revealed that, aside from the
lateral trochlear inclination, all other indices based on cartilage
and subchondral bone landmarks exhibited significant differences.
Furthermore, all indices were statistically significant in the
control group. This result confirmed that cartilage and subchondral
bone morphologies were not perfectly matched in the patient or
control groups. Application of the cartilage landmark was able to
reveal the true morphology of the femoral trochlea. In the patient
group, the existence of cartilage rendered the trochlear facet
flatter and straighter, resulting in more severe dysplasia
(17,25). Unlike the results reported by Shih
et al (25), in the present
study the lateral trochlear inclination demonstrated no significant
difference based on the cartilage and subchondral bone landmarks in
the patient group, suggesting that the cartilage and subchondral
bone surfaces on the lateral trochlear facet were almost parallel.
Therefore, if the deepest point of the femoral trochlear groove
determined by MRI was identified on the CT image, the measurement
on the corresponding layer of the CT images may underestimate the
severity of the femoral trochlear dysplasia. However, because the
measurements of bony facets between patients and control groups
were significantly different, this suggests that femoral trochlear
dysplasia may still be determined using CT measurements in the
initial diagnosis.
A further study of the B-D types of severe femoral
trochlear dysplasia revealed no significant differences in the
sulcus angle and trochlear depth, the lateral trochlear inclination
or the medial and lateral joint facet asymmetry between types. This
finding was similar to that reported in a study by Nelitz et
al (9), which is possibly
because the Dejour classification was determined by the
proximal-side morphology of the femoral trochlea. Without complete
cartilage coverage, the proximal trochlear is not able to form the
patellofemoral joint. Therefore, in the present study, the selected
layers were the central part of the trochlear at craniocaudal
position. The different layers were the main reason that no
correlation was observed between measurements acquired and Dejour's
classification. A study by Fucentese et al (26) suggested that the preoperative
classification of femoral trochlear dysplasia may predict the
postoperative recovery of patients. They discovered that patients
with types B and D trochlear dysplasia had better prognoses than
patients with types A and C due to the reduced contact pressure
between the patellofemoral joints in type B and D patients after
surgery. The results of the present study suggested that the
selected MRI image was able to objectively evaluate femoral
trochlear dysplasia but not classify the type of dysplasia. It is
worth noting that measurements of the selected layers may assist in
evaluating trochlear dysplasia rather than replacing the
classification of trochlear dysplasia. During preoperative
assessment, the combination of femoral trochlear measurements and
Dejour classification may provide more assistance in determining a
surgical method and the prognosis.
In the present study, the parameters measured by MRI
were able to reveal the pathological characteristics in patients
with types B-D femoral trochlear dysplasia, including a flattened
trochlear groove, flat joint facets and medial facet dysplasia.
This method assisted with diagnosis and selecting the best surgical
approach. In these patients, isolated force that strengthens the
medial patellofemoral ligament for the medial translocation of the
patella was not sufficient to counter the force of lateral
dislocation caused by trochlear dysplasia. Therefore, combined
femoral trochlear construction and medial patellofemoral ligament
reconstruction were required to correct the dislocation (27,28).
The present study was not without limitations.
Further studies are required to confirm whether the determined
deepest point of the femoral trochlear groove may be used for other
measurements, such as the trochlear congruence angle and the Tibial
Tuberosity-Trochlear Groove distance. In addition, although the
credibility between observers ranged from good to very good in the
present study, a study by Dornacher et al (29) suggested that, for type C and D
patients with trochlear groove dysplasia, the correlation between
the interclass and intraclass observers was not ideal. Therefore,
larger sample sizes and experiments involving multiple institutions
are required to confirm the reliability of these results. Finally,
no comparative measurements were performed between corresponding
layers from CT and MRI images, and it was not clear whether the
results from both techniques were interchangeable.
MRI has unique advantages over X-ray and CT scans,
such as no radiation exposure and the capacity to reveal cartilage
and surrounding muscles and ligaments. The results of the present
study suggested that, for patients with severe femoral trochlear
dysplasia, MRI is able to determine the deepest point of the
femoral trochlea for measurements. Measurements in the patient
group were significantly different compared with the control group.
Within the patient group, measurements based on the cartilage
landmark were different from the measurements based on the
subchondral bone landmark. Therefore, these objective measurements
may assist in clinical assessment and treatment for such patients.
However, the limitation of this method is that measurement values
are unable to be used to determine the classification of the
femoral trochlea, and so MRI measurements should be combined with
morphological classifications.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81171312).
References
|
1
|
Earhart C, Patel DB, White EA, Gottsegen
CJ, Forrester DM and Matcuk GR Jr: Transient lateral patellar
dislocation: Review of imaging findings, patellofemoral anatomy,
and treatment options. Emerg Radiol. 20:11–23. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dejour H, Walch G, Nove-Josserand L and
Guier C: Factors of patellar instability: An anatomic radiographic
study. Knee Surg Sports Traumatol Arthrosc. 2:19–26. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lippacher S, Reichel H and Nelitz M:
Radiological criteria for trochlear dysplasia in children and
adolescents. J Pediatr Orthop B. 20:341–344. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Redziniak DE, Diduch DR, Mihalko WM,
Fulkerson JP, Novicoff WM, Sheibani-Rad S and Saleh KJ: Patellar
instability. Instr Course Lect. 59:195–206. 2010.PubMed/NCBI
|
|
5
|
Botchu R, Obaid H and Rennie WJ:
Correlation between trochlear dysplasia and the notch index. J
Orthop Surg (Hong Kong). 21:290–293. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chhabra A, Subhawong TK and Carrino JA: A
systematised MRI approach to evaluating the patellofemoral joint.
Skeletal Radiol. 40:375–387. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dejour D and Le Coultre B: Osteotomies in
patello-femoral instabilities. Sports Med Arthrosc. 15:39–46. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tecklenburg K, Dejour D, Hoser C and Fink
C: Bony and cartilaginous anatomy of the patellofemoral joint. Knee
Surg Sports Traumatol Arthrosc. 14:235–240. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nelitz M, Lippacher S, Reichel H and
Dornacher D: Evaluation of trochlear dysplasia using MRI:
Correlation between the classification system of Dejour and
objective parameters of trochlear dysplasia. Knee Surg Sports
Traumatol Arthrosc. 22:120–127. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Smith TO, Cogan A, Patel S, Shakokani M,
Toms AP and Donell ST: The intra- and inter-rater reliability of
X-ray radiological measurements for patellar instability. Knee.
20:133–138. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Escala JS, Mellado JM, Olona M, Giné J,
Sauri A and Neyret P: Objective patellar instability: MR-based
quantitative assessment of potentially associated anatomical
features. Knee Surg Sports Traumatol Arthrosc. 14:264–272. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Stefanik JJ, Roemer FW, Zumwalt AC, Zhu Y,
Gross KD, Lynch JA, Frey-Law LA, Lewis CE, Guermazi A, Powers CM
and Felson DT: Association between measures of trochlear morphology
and structural features of patellofemoral joint osteoarthritis on
MRI: The MOST study. J Orthop Res. 30:1–8. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Keser S, Savranlar A, Bayar A, Ege A and
Turhan E: Is there a relationship between anterior knee pain and
femoral trochlear dysplasia? Assessment of lateral trochlear
inclination by magnetic resonance imaging. Knee Surg Sports
Traumatol Arthrosc. 16:911–915. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nelitz M and Lippacher S: Arthroscopic
evaluation of trochlear dysplasia as an aid in decision making for
the treatment of patellofemoral instability. Knee Surg Sports
Traumatol Arthrosc. 22:2788–2794. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Biedert RM and Bachmann M:
Anterior-posterior trochlear measurements of normal and dysplastic
trochlea by axial magnetic resonance imaging. Knee Surg Sports
Traumatol Arthrosc. 17:1225–1230. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Toms AP, Cahir J, Swift L and Donell ST:
Imaging the femoral sulcus with ultrasound, CT, and MRI:
Reliability and generalizability in patients with patellar
instability. Skeletal Radiol. 38:329–338. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
van Huyssteen AL, Hendrix MR, Barnett AJ,
Wakeley CJ and Eldridge JD: Cartilage-bone mismatch in the
dysplastic trochlea. An MRI study. J Bone Joint Surg Br.
88:688–691. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Charles MD, Haloman S, Chen L, Ward SR,
Fithian D and Afra R: Magnetic resonance imaging-based
topographical differences between control and recurrent
patellofemoral instability patients. Am J Sports Med. 41:374–384.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Köhlitz T, Scheffler S, Jung T, Hoburg A,
Vollnberg B, Wiener E and Diederichs G: Prevalence and patterns of
anatomical risk factors in patients after patellar dislocation: A
case control study using MRI. Eur Radiol. 23:1067–1074. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kamath AF, Slattery TR, Levack AE, Wu CH,
Kneeland JB and Lonner JH: Trochlear inclination angles in normal
and dysplastic knees. J Arthroplasty. 28:214–219. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Balcarek P, Jung K, Ammon J, Walde TA,
Frosch S, Schüttrumpf JP, Stürmer KM and Frosch KH: Anatomy of
lateral patellar instability: Trochlear dysplasia and tibial
tubercle-trochlear groove distance is more pronounced in women who
dislocate the patella. Am J Sports Med. 38:2320–2327. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Teng HL, Chen YJ and Powers CM: Predictors
of patellar alignment during weight bearing: An examination of
patellar height and trochlear geometry. Knee. 21:142–146. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Van Haver A, De Roo K, De Beule M, Van
Cauter S, Audenaert E, Claessens T and Verdonk P: Semi-automated
landmark-based 3D analysis reveals new morphometric characteristics
in the trochlear dysplastic femur. Knee Surg Sports Traumatol
Arthrosc. 22:2698–2708. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hing CB, Shepstone L, Marshall T and
Donell ST: A laterally positioned concave trochlear groove prevents
patellar dislocation. Clin Orthop Relat Res. 447:187–194. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shih YF, Bull AM and Amis AA: The
cartilaginous and osseous geometry of the femoral trochlear groove.
Knee Surg Sports Traumatol Arthrosc. 12:300–306. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fucentese SF, Zingg PO, Schmitt J,
Pfirrmann CW, Meyer DC and Koch PP: Classification of trochlear
dysplasia as predictor of clinical outcome after trochleoplasty.
Knee Surg Sports Traumatol Arthrosc. 19:1655–1661. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Howells NR, Barnett AJ, Ahearn N, Ansari A
and Eldridge JD: Medial patellofemoral ligament reconstruction: A
prospective outcome assessment of a large single centre series. J
Bone Joint Surg Br. 94:1202–1208. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dejour D, Byn P and Ntagiopoulos PG: The
Lyon's sulcus-deepening trochleoplasty in previous unsuccessful
patellofemoral surgery. Int Orthop. 37:433–439. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dornacher D, Reichel H and Lippacher S:
Measurement of tibial tuberosity-trochlear groove distance:
Evaluation of inter- and intraobserver correlation dependent on the
severity of trochlear dysplasia. Knee Surg Sports Traumatol
Arthrosc. 22:2382–2387. 2014. View Article : Google Scholar : PubMed/NCBI
|