Introduction
Acute kidney injury (AKI) has been identified as an
independent risk factor for significant increase in incidence rate
and the mortality rate after cardiopulmonary bypass (CPB) with a
complicated pathogenesis, and also a common complication after CPB
(1). Serum creatinine and urinary
volume, as common and non-specific indicators in diagnosis and
staging criteria of AKI, have shown poor sensitivity and are
susceptible to the external factors, thereby decreasing their
capabilities in precise reflection of the slight variations in
renal function and delaying the accurate diagnosis of AKI in
clinical practice (2). Clinically,
there remain no effective indicators for early prediction and
diagnosis of AKI, thereby resulting in a particularly high
incidence rate and mortality rate of AKI after CPB due to delayed
efficient treatment methods. Thus, screening out the indicators for
early diagnosis of AKI can significantly ameliorate the prognosis
of AKI patients through efficient treatment methods in advance and
decrease in mortality rate (3).
Study has shown that urinary interleukin-8 (uIL-8) and urinary
neutrophil gelatinase-associated lipocalin (uNGAL) have promising
sensitivity in early diagnosis of AKI after CPB (4–8). In this
study, we aimed to investigate the application value of uIL-18 and
uNGAL in urine samples in early diagnosis of AKI after CPB through
detecting the dynamic changes in levels of uIL-18 and uNGAL
collected from the clinical data of patients.
Materials and methods
Subjects
A total of 103 patients who underwent CPB between
March and October, 2014 were enrolled as subjects. The criteria for
enrollment of subjects: i) patients without renal and hepatic
dysfunction, tumors, or medication history of nephrotoxic drugs
before CPB; ii) patients without unstable vital signs before CPB;
iii) patients conforming to the diagnostic criteria of AKI, i.e.
the Scr level was >26.5 µM, or exceeded 50% of the baseline
level of Scr (9). This study was
approved by the Ethics Committee of Zhengzhou No. 7 People's
Hospital, and all patients or their family signed the informed
consent.
Methods
We collected the urine samples before and at 2, 4,
6, 8 and 12 h after CPB and the blood samples before and at 12, 24,
48 and 72 h after CPB for centrifugation, and the supernatant was
collected for detecting the levels of uIL-18 and uNGAL in urine
samples and the levels of Scr in blood samples, in which the Scr
level was measured with an Automatic Biochemistry Analyzer, while
uNGAL and uIL-18 levels in urine by enzyme-linked immunosorbent
assay (ELISA). The ELISA kit was purchased from R&D Systems
(Minneapolis, MN, USA).
Statistical analysis
In this study, statistical analysis on experiment
data was performed by SPSS 19.0 software (NDtimes, Beijing, China).
Data in normal distribution are presented as mean ± standard
deviation (mean ± SD). For comparisons of data among groups and
between different time-points, t-test and analysis of variance were
carried out. Receiver operating characteristic (ROC) curve and area
under curve (AUC) were used to evaluate the sensitivity and
specificity of uIL-18 and uNGAL on AKI. P<0.05 suggested that
the difference had statistical significance.
Results
Incidence rate of AKI
Among 103 patients who received the CPB, there were
22 patients (21.4%) with AKI, while remaining 81 patients had no
AKI, indicating that the incidence rate of AKI was 21.4%. Among
those with AKI, there were 10 females and 12 males with an average
age of 59±10.2 years, while in those with no AKI, there were 39
females and 42 males with an average age of 58±7.9 years. We found
no statistically significant difference in comparisons of gender
ratio and age between the two groups.
From 12 h after CPB, the level of Scr in the AKI
group was significantly elevated, and this increasing trend lasted
till 72 h; comparisons with the levels before CPB and in non-AKI
group showed that the differences were statistically significant
(P<0.05). In the non-AKI group, there was no significant
difference in comparison of Scr level before and after CPB, and the
difference had no statistical significance (Table I).
 | Table I.Comparisons of Scr levels at different
time-points in the non-AKI group and the AKI group (Umol/l, mean ±
SD). |
Table I.
Comparisons of Scr levels at different
time-points in the non-AKI group and the AKI group (Umol/l, mean ±
SD).
| Time-point | Non-AKI group | AKI group | P-value | t-test | P-value | F-value |
|---|
| Before CPB |
62.34±11.37 |
65.22±10.46 | 0.2868 | 1.071 |
|
|
| At 2 h after CPB |
63.11±13.89 |
67.78±13.55 | 0.1629 | 1.406 | 0.244 | 1.6781 |
| At 12 h after
CPB |
64.34±15.02 |
85.48±22.47a,b | P<0.05 | 5.468 | P<0.05 | 4.6147 |
| At 24 h after
CPB |
64.17±13.57 |
118.29±34.63a,b | P<0.05 | 11.324 | P<0.05 | 10.9608 |
| At 48 h after
CPB |
61.54±10.44 |
124.61±38.61a,b | P<0.05 | 13.173 | P<0.05 | 13.6250 |
Variations in level of uIL-18
In AKI group, uIL-18 attained the peak level at 2 h
after CPB, and the high level lasted for 10 h, and comparisons with
the levels before CPB and in non-AKI group showed that the
differences had statistical significance (P<0.05); the level of
uIL-18 after CPB in the non-AKI group was slightly higher than that
before CPB, but the difference had no statistical significance
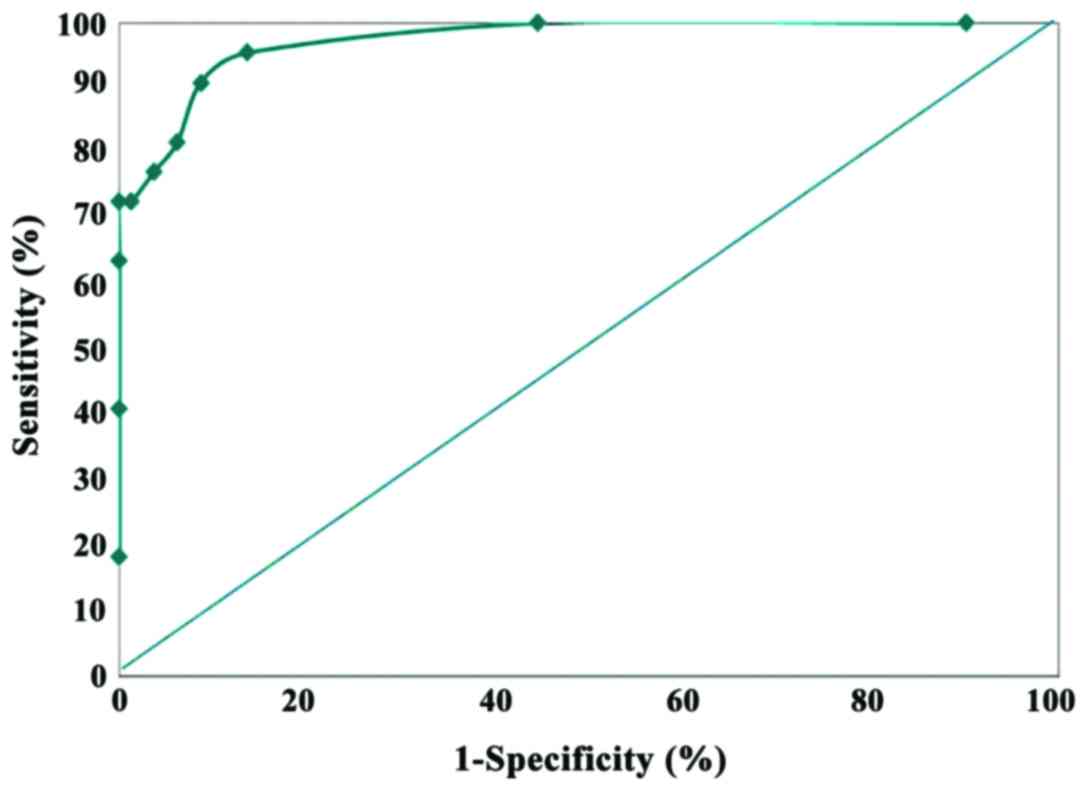
(P>0.05) (Table II). To assess
the diagnostic value of uIL-18 after CPB, the level of uIL-18 at a
certain time-point was adopted for statistical analysis and
preparation of ROC curve. Since uIL-18 attained the peak level at 2
h after CPB, we selected this time-point to perform further study.
At 2 h after CPB, the AUC of ROC curve of uIL-18 was 90.48, and
when the critical value was set as 1.6 µg/l, the sensitivity and
specificity was 90.91 and 91.36%, where the uIL-18 level in most of
the patients in the AKI group was >1.6 µg/l, but there were only
11 patients (11/81) in the non-AKI group with a level >1.6 µg/l
(Table III and Fig. 1).
 | Table II.The levels of uIL-18 at different
time-points in non-AKI group and AKI group (µg/l, mean ± SD). |
Table II.
The levels of uIL-18 at different
time-points in non-AKI group and AKI group (µg/l, mean ± SD).
| Time-point | Non-AKI group | AKI group | P-value | t-test | P-value | F-value |
|---|
| Before CPB |
0.91±0.46 |
0.98±0.32 | 0.4123 | 0.823 |
|
|
| At 2 h after CPB |
0.95±0.51 |
4.89±0.96a,b | P<0.05 | 18.508 | P<0.05 | 9.0000 |
| At 4 h after CPB |
1.13±0.79 |
4.46±1.56a,b | P<0.05 | 13.849 | P<0.05 | 23.7656 |
| At 6 h after CPB |
1.05±0.74 |
4.01±1.21a,b | P<0.05 | 14.330 | P<0.05 | 14.2979 |
| At 8 h after CPB |
1.19±0.67 |
3.79±1.42a,b | P<0.05 | 12.286 | P<0.05 | 19.6914 |
| At 12 h after
CPB |
1.22±0.74 |
3.73±1.61a,b | P<0.05 | 10.586 | P<0.05 | 25.3135 |
 | Table III.Distribution of uIL-18 concentrations
in patients at 2 h after CPB. |
Table III.
Distribution of uIL-18 concentrations
in patients at 2 h after CPB.
|
| AKI | non-AKI |
|---|
|
|
|
|
|---|
| uIL-18 (µg/l) | n | Total | n | Total |
|---|
| >0.1 | 0 | 22 | 8 | 81 |
| >0.6 | 1 | 22 | 37 | 73 |
| >1.1 | 1 | 21 | 25 | 36 |
| >1.6 | 2 | 20 | 4 | 11 |
| >2.1 | 1 | 18 | 2 | 7 |
| >2.6 | 1 | 17 | 2 | 5 |
| >3.1 | 0 | 16 | 2 | 3 |
| >3.6 | 2 | 16 | 1 | 1 |
| >4.1 | 5 | 14 | 0 | 0 |
| >4.6 | 5 | 9 | 0 | 0 |
| >5.1 | 4 | 4 | 0 | 0 |
| Total | 22 |
| 81 |
|
Variations in level of uNGAL
In the AKI group, a significant elevation in uNGAL
level at 2 h after CPB followed by a rapid decrease was seen, and
difference between the level at 2 h after CPB and the level before
CPB as well as that in the non-AKI group had statistical
significance (P<0.05). However, at 12 h after CPB, these
differences had no statistical significance (P>0.05), and in the
non-AKI group, there was no statistically significant difference in
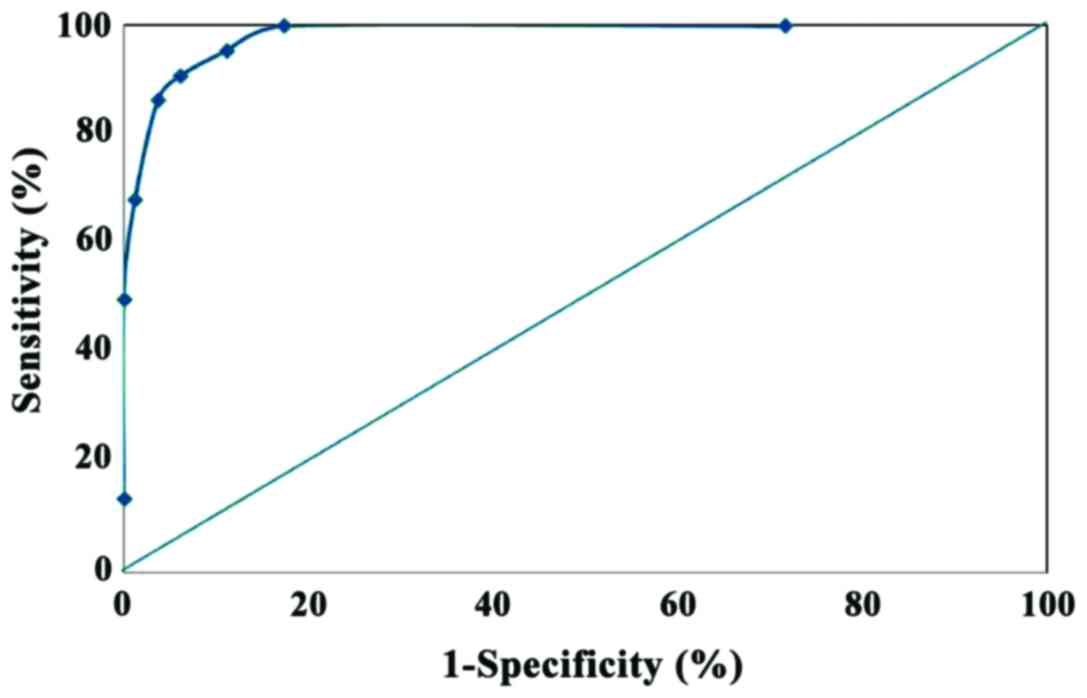
comparison to the uNGAL level before and after CPB (Table IV). To assess the diagnostic value
of uNGAL level after CPB, the level of uNGAL at a certain
time-point was adopted for statistical analysis and preparation of
ROC curve. Since a significant elevation in uNGAL was attained at 2
h after CPB, which was not significantly different from the peak
level attained at 4 h after CPB, we selected this time-point to
perform further study. At 2 h after CPB, the AUC of ROC curve of
uNGAL was 83.25, and when the critical value was set as 100 µg/l,
the sensitivity and specificity, respectively, was 90.91 and
93.83%, where the uNGAL level in most of the patients (20/22) in
the AKI group was >1.6 µg/l, but there were only 7 patients
(7/81) in the non-AKI group with a level >100 µg/l (Table V and Fig.
2).
 | Table IV.The levels of uNGAL at different
time-points in non-AKI group and AKI group (µg/l, mean ± SD). |
Table IV.
The levels of uNGAL at different
time-points in non-AKI group and AKI group (µg/l, mean ± SD).
| Time-point | Non-AKI group | AKI group | P-value | t-test | P-value | F-value |
|---|
| Before CPB |
34.91±9.46 |
36.74±8.02 | 0.4089 |
0.829 |
|
|
| At 2 h after
CPB |
36.91±12.55 |
425.41±18.96a,b | P<0.05 | 114.408 | P<0.05 | 5.5889 |
| At 4 h after
CPB |
35.13±17.42 |
527.47±17.54a,b | P<0.05 | 117.389 | P<0.05 | 4.7831 |
| At 6 h after
CPB |
32.25±11.84 |
358.01±15.9a,b | P<0.05 | 105.935 | P<0.05 | 3.9305 |
| At 8 h after
CPB |
29.48±8.67 |
105.79±21.42a,b | P<0.05 | 25.500 | P<0.05 | 7.1333 |
| At 12 h after
CPB |
30.22±9.74 |
35.03±12.17 | 0.0547 |
1.944 | 0.063 | 2.3027 |
 | Table V.Distribution of uNGAL concentrations
in patients at 2 h after CPB. |
Table V.
Distribution of uNGAL concentrations
in patients at 2 h after CPB.
|
| AKI | non-AKI |
|---|
|
|
|
|
|---|
| uNGAL (µg/l) | n | Total | n | Total |
|---|
| >10 | 0 | 22 | 24 | 81 |
| >30 | 1 | 22 | 44 | 57 |
| >60 | 2 | 21 | 5 | 13 |
| >100 | 1 | 20 | 4 | 8 |
| >200 | 3 | 19 | 2 | 4 |
| >300 | 4 | 15 | 2 | 2 |
| >400 | 8 | 11 | 0 | 0 |
| >500 | 3 | 3 | 0 | 0 |
Discussion
Various factors affect the renal functions in
surgeries, particularly the CPB, which can induce severe
complications, such as acute renal failure that has poor prognosis,
and frequently leads to continuous increased incidence rates and
mortality without immediate intervention and treatment (10,11).
Recently, AKI was put forward by the international nephrology
communication for accurate prediction and early diagnosis and
treatment; the attack of AKI without any effective intervention and
treatment will aggravate the kidney impairment, or even lead to
death (12,13). Thus, early diagnosis of AKI is of
great significance for prognosis of patients. So far, Scr has been
used as a conventional indicator for detection of renal function,
but the obvious increase in content of Scr is usually identified at
12 h after surgery; thus, Scr cannot timely reflect the impairment
of kidney (14). Hence, it is
prioritized to search for biological indicators for early diagnosis
of AKI in clinical practice.
Ischemic reperfusion in kidney is a key factor
inducing the attack of AKI after CPB for it can initiate the
expression of IL-18, thereby resulting in the inflammatory
responses in kidney and AKI (15).
An ischemic AKI experiment has proved that damage to kidney tubules
will give rise to massive release of IL-18 into the urine; thus, we
can detect the content of IL-18 using the urine sample (16); a clinical study confirmed that in
patients with ischemia or late-onset transplantation rejection
after kidney transplantation, a significant elevation is also
identified in the content of uIL-18 (17,18). In
addition, the AKI in patients will facilitate the generation of
NGAL that can protect the renal tissues (19). Study has shown that the expression of
NGAL is quite low in normal renal tissues, but under the kidney
impairment, NGAL will be rapidly secreted by the epithelial cells
of tubules to protect the integrity of tubules, which is usually
accompanied by a quick increase in concentration of NGAL in urine
(6,20). Thus, uIL-18 or uNGAL may be a
candidate for indicators in detection of AKI, and they have become
a research hotspot.
In this study, the results showed that among 103
patients undergoing CPB, there were 22 patients with AKI after CPB,
which coincide with a previous study (16). Compared with the levels before
surgery and those in non-AKI group, a significant elevation was
identified at 12 h after CPB in patients of the AKI group, lasting
till 72 h after CPB, and the differences had statistical
significance (P<0.05), which is also consistent with previous
studies, suggesting that this period is suitable for diagnosis of
AKI using Scr (17). Among the AKI
patients, maximal level of uIL-18 was attained at 2 h after CPB,
and the high level lasted till 12 h; comparisons between the uIL-18
level at this time-point and the level before CPB as well as that
in the non-AKI group showed that the differences had statistical
significance (P<0.05). However, peak level of uNGAL was
identified at 4 h after CPB, which could only be sustained for 8 h
after CPB; the result is also coincident with previous reports
(6,19). Shortly after CPB, a slight increase
was seen in patients of the non-AKI group, which may be caused by
the release of inflammatory factors (15). To provide better clinical service, we
further confirmed the critical values of uIL-18 and uNGAL at 2 h
after CPB with promising sensitivity and specificity, and the
results showed that when the critical values of uIL-18 and uNGAL
were 1.6 and 100 µg/l, respectively, these indicators showed good
sensitivity and specificity; besides, the AUC of ROC was,
respectively, 90.48 and 83.25, suggesting that the results are
reliable. The result of this study also conforms to the reports of
studies by other groups (18,20).
In conclusion, although rapid increases in uIL-18
and uNGAL levels were found in a short time in patients with AKI
after CPB, the emergence of peak value in uIL-18 level after CPB is
earlier than the uNGAL, and the high level of uIL-18 can be
sustained for a long time. Thus, uIL-18 has a better clinical value
for early diagnosis and intervention of the development and
progression of AKI.
References
|
1
|
Reddy SL, Grayson AD, Griffiths EM, Pullan
DM and Rashid A: Logistic risk model for prolonged ventilation
after adult cardiac surgery. Ann Thorac Surg. 84:528–536. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bellomo R, Kellum JA and Ronco C: Defining
acute renal failure: Physiological principles. Intensive Care Med.
30:33–37. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Doddakula K, Al-Sarraf N, Gately K, Hughes
A, Tolan M, Young V and McGovern E: Predictors of acute renal
failure requiring renal replacement therapy post cardiac surgery in
patients with preoperatively normal renal function. Interact
Cardiovasc Thorac Surg. 6:314–318. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Song S, Meyer M, Türk TR, Wilde B,
Feldkamp T, Assert R, Wu K, Kribben A and Witzke O: Serum cystatin
C in mouse models: A reliable and precise marker for renal function
and superior to serum creatinine. Nephrol Dial Transplant.
24:1157–1161. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jin Y, Shao X, Sun B, Miao C, Li Z and Shi
Y: Urinary kidney injury molecule 1 as an early diagnostic
biomarker of obstructive acute kidney injury and development of a
rapid detection method. Mol Med Rep. 15:1229–1235. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Devarajan P: Neutrophil
gelatinase-associated lipocalin (NGAL): A new marker of kidney
disease. Scand J Clin Lab Invest (Suppl). 241:89–94. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mishra J, Dent C, Tarabishi R, Mitsnefes
MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, et al:
Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker
for acute renal injury after cardiac surgery. Lancet.
365:1231–1238. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nguyen MT and Devarajan P: Biomarkers for
the early detection of acute kidney injury. Pediatr Nephrol.
23:2151–2157. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goldstein SL: Pediatric acute kidney
injury: It's time for real progress. Pediatr Nephrol. 21:891–895.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nunag M, Brogan M and Garrick R:
Mitigating contrast-induced acute kidney injury associated with
cardiac catheterization. Cardiol Rev. 17:263–269. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Karkouti K, Wijeysundera DN, Yau TM,
Callum JL, Cheng DC, Crowther M, Dupuis JY, Fremes SE, Kent B,
Laflamme C, et al: Acute kidney injury after cardiac surgery: Focus
on modifiable risk factors. Circulation. 119:495–502. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wu Y, Wang L, Meng L, Cao GK and Zhang Y:
MIP-1α and NF-κB as indicators of acute kidney injury secondary to
acute lung injury in mechanically ventilated patients. Eur Rev Med
Pharmacol Sci. 20:3830–3834. 2016.PubMed/NCBI
|
|
13
|
Nissenson AR: Acute renal failure:
Definition and pathogenesis. Kidney Int (Suppl). 66:S7–S10.
1998.PubMed/NCBI
|
|
14
|
Pirgakis KM, Makris K, Dalainas I, Lazaris
AM, Maltezos CK and Liapis CD: Urinary cystatin C as an early
biomarker of acute kidney injury after open and endovascular
abdominal aortic aneurysm repair. Ann Vasc Surg. 28:1649–1658.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Parikh CR, Jani A, Melnikov VY, Faubel S
and Edelstein CL: Urinary interleukin-18 is a marker of human acute
tubular necrosis. Am J Kidney Dis. 43:405–414. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Melnikov VY, Faubel S, Siegmund B, Lucia
MS, Ljubanovic D and Edelstein CL: Neutrophil-independent
mechanisms of caspase-1- and IL-18-mediated ischemic acute tubular
necrosis in mice. J Clin Invest. 110:1083–1091. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Parikh CR, Mishra J, Thiessen-Philbrook H,
Dursun B, Ma Q, Kelly C, Dent C, Devarajan P and Edelstein CL:
Urinary IL-18 is an early predictive biomarker of acute kidney
injury after cardiac surgery. Kidney Int. 70:199–203. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Han WK, Wagener G, Zhu Y, Wang S and Lee
HT: Urinary biomarkers in the early detection of acute kidney
injury after cardiac surgery. Clin J Am Soc Nephrol. 4:873–882.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bolignano D, Lacquaniti A, Coppolino G,
Donato V, Campo S, Fazio MR, Nicocia G and Buemi M: Neutrophil
gelatinase-associated lipocalin (NGAL) and progression of chronic
kidney disease. Clin J Am Soc Nephrol. 4:337–344. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shemin D and Dworkin LD: Neutrophil
gelatinase-associated lipocalin (NGAL) as a biomarker for early
acute kidney injury. Crit Care Clin. 27:379–389. 2011. View Article : Google Scholar : PubMed/NCBI
|