Introduction
Bone loss is considered to be a disabling
complication of inflammatory bowel disease (IBD) (1). Bone mineral density (BMD) testing
results of patients with IBD from seven medical facilities, ranging
from January 1996 to October 2006, were reviewed to determine the
prevalence rate of osteoporosis (2).
A total of 317 bone density tests were conducted in 2,035 patients,
and osteoporosis was detected in 26% of patients and osteopenia in
48% (2). Another study involving 70
patients with IBD demonstrated that osteoporosis was observed in
13.2% of patients and osteopenia in 46.1% (3). The dominant risk factors leading to
osteoporosis in IBD are considered to be age, intestinal
malabsorption, long-term use of steroids, lack of exercise or
supplementation of calcium and vitamin D, and smoking (4). In addition, inflammation and
proinflammatory cytokines serve a key role in bone loss and
increase the risk of fracture (5),
including interleukin (IL)-6 and tumor necrosis factor (TNF)
(6). However, the published
literature regarding osteoporosis in IBD has associated it with the
aforementioned risk factors. Osteoporosis as a complication is
common in patients with IBD, followed by the above risk factors,
while it rarely presents as a primary manifestation in patients
with Crohn's disease (CD). A previous study observed that severe
osteoporosis presented in a 12-year-old boy with CD, and no history
of steroid use was tracked (7). To
the best of our knowledge, no reports of osteoporosis as an initial
manifestation of IBD in adults exist. The present case report
describes a case of osteoporosis as an initial manifestation in an
adult patient with CD without the aforementioned risk factors.
Notably, using steroids and biological agents ameliorated low back
pain (LBP) in the patient. Considering the relationship between
inflammation and bone loss, it was hypothesized that osteoporosis,
in the present case, is a primary manifestation of CD.
Case report
A 43-year-old male presented at the Second Xiangya
Hospital of Central South University (Changsha, China) with
worsening symptoms of LBP in July 2015 and was compulsively posed
in a lateral position. No abdominal or digestive syndromes were
observed. The dietary intake of the patient had not changed;
however, the patient had lost 15 kg of body weight in 12 months. As
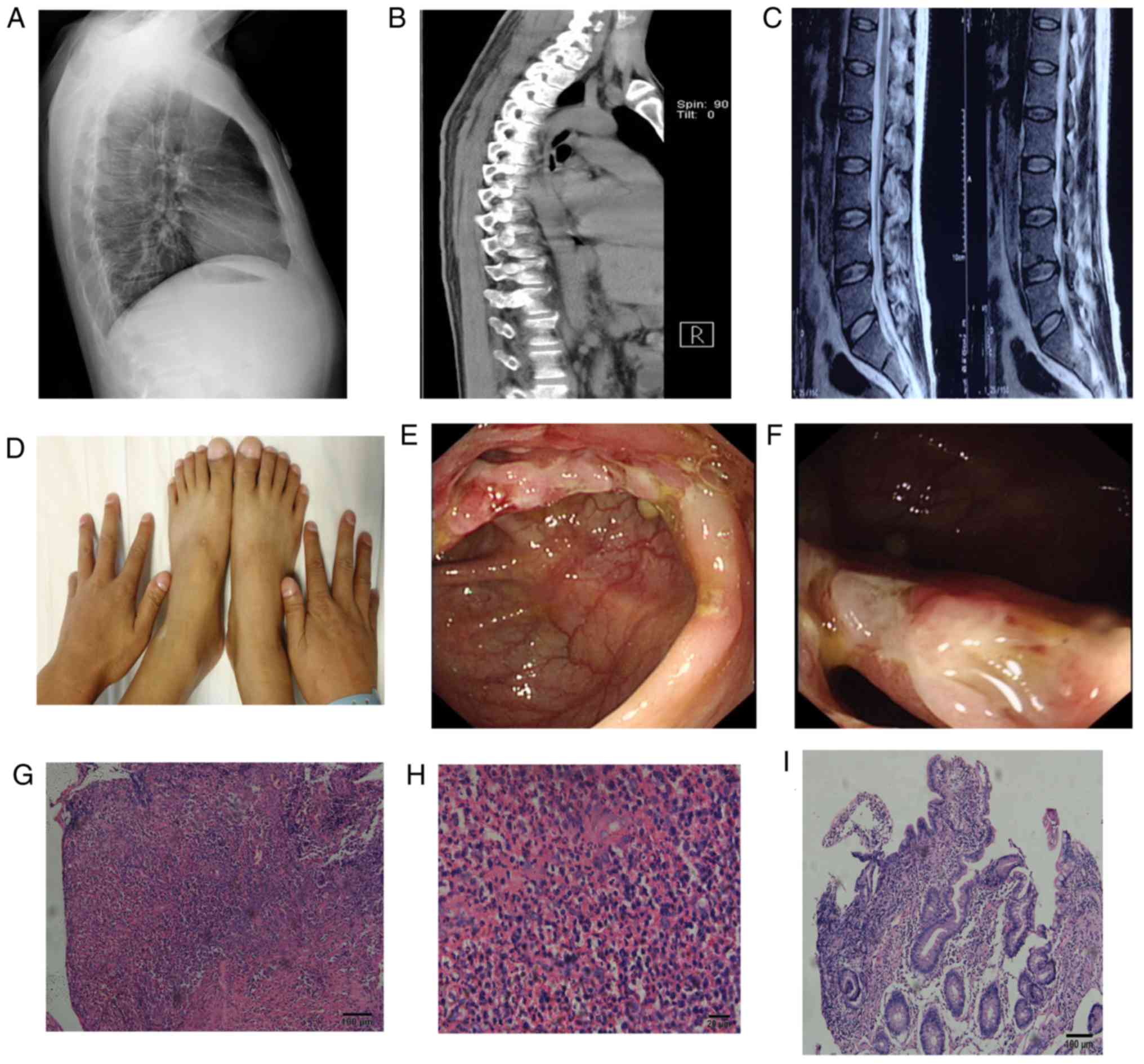
demonstrated in Fig. 1, X-rays
revealed thoracolumbar spine degeneration (Fig. 1A). A 1 year supply of medicinal
calcium preparation (Caltrate®; 600 mg/day orally;
Wyeth; Pfizer, Inc., New York, NY, USA; and 1α-OH vitamin D3; Teva
Pharmaceutical Industries, Ltd., Petach Tikva, Israel; oral soft
capsule, 0.25 µg/day) was unable to improve LBP. A computed
tomography (CT) scan was subsequently performed, revealing
thoracolumbar spine degeneration and mesenteric lymph node
tumescence (Fig. 1B), as did single
photon emission CT (Fig. 1C). The
patient was therefore referred to the Gastroenterology department
in July 2015.
The patient had no history of long-term use of
corticosteroids and no bone fractures, and had a 10-year history of
cigarette smoking at a rate of 6 cigarettes/day. The body weight of
the patient was 71.6 kg and body mass index was 23.92. Physical
examination revealed pressing pain in the cervical, lumbar and
thoracic vertebrae and obvious clubbing of the fingers and feet
(Fig. 1D). Other inspections of the
lung, heart and abdomen proved unremarkable. Laboratory data
revealed a serum hemoglobin (Hb) level of 103 g/l (normal range,
130–175 g/l; Sysmex® XN-Series; Sysmex Corporation,
Kobe, Japan), serum albumin level of 23.9 g/l (normal range, 40–55
g/l; Hitachi Modular 7600 chemistry analyzer; Hitachi, Ltd., Tokyo,
Japan), an erythrocyte sedimentation rate (ESR) of 50 mm/h (normal
range, 1–15 mm/h, automatic ESR analyzer Monitor-100; Vital
Diagnostics, Forli, Italy), C-reactive protein (CRP) level of 63.5
mg/l (normal range, 0–8.0 mg/l; IMMAGE® 800; Beckman
Coulter, Inc., Brea, CA, USA) and reduced serum 25-hydroxy vitamin
D level of 37 nmol/l (normal range, 75–250 nmol/l; ADVIA Centaur XP
chemiluminescence immunoanalyzer; Siemens Healthcare Diagnostics
Manufacturing, Ltd., Dublin, Ireland). No positive results were
identified for serum parathyrin, gonadin, calcium, phosphate,
magnesium, alkaline phosphatase and human leukocyte
antigen-B27.
A dual-energy X-ray absorptionmetry scan (DXA) of
the lumbar spine revealed a severe reduction in BMD (lumbar
Z-score, −2.9 SD; T-score, −3.0 SD). Colonoscopy demonstrated an
inflamed and strictured ileocecal valve, with less inflammation in
the ascending, transverse colon, sigmoid colon and rectum,
compatible with CD; however, the coloscope could not pass through
the restricted ileocecal valve (Fig. 1E
and F). An ileocecal valve biopsy indicated chronic active
colitis with ulcers and inflammatory granulation tissue suggestive
of CD (Fig. 1G and H). The biopsy
tissue was fixed in 4% formaldehyde for 6 h at 35°C, then cut into
4-µm-thick sections and stained with hematoxylin and eosin for 20
min at room temperature. The sections were observed using an
Olympus BX53F light microscope (Olympus Corporation, Tokyo, Japan).
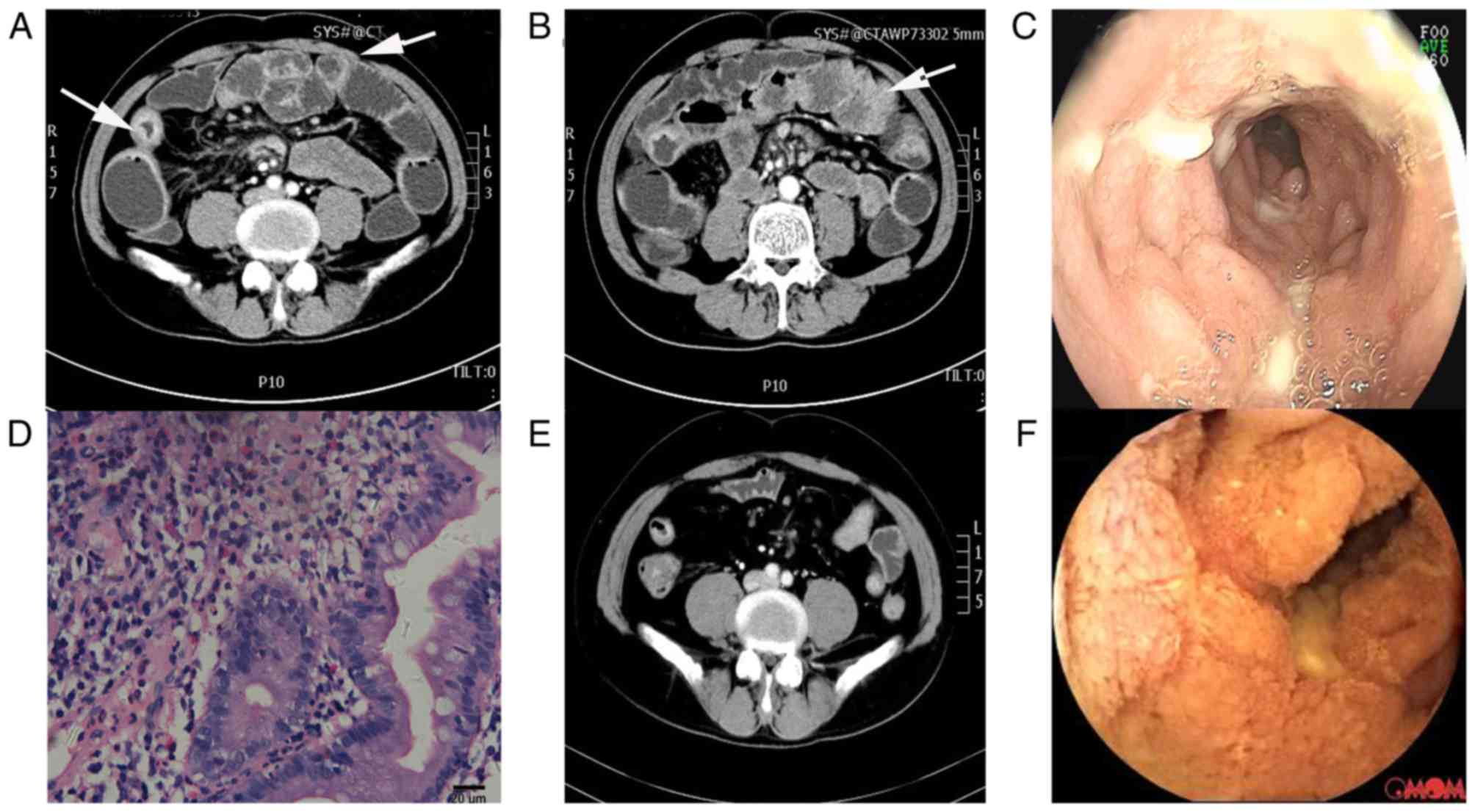
An abdominal CT scan indicated marked symmetric segmental
thickening at the jejunum wall (Fig. 2A
and B). Duodenal-balloon enteroscopy demonstrated segmental
ulceration and stricture in the jejunum (Fig. 2C). A jejunum biopsy revealed chronic
active colitis with necrosis and ulceration (Figs. 1I and 2D). The tissue sections were fixed and
stained as above. After excluding tuberculosis via a chest X-ray
and T-SPOT® (cat. no. TB.300 CN; Oxford Immunotec Global
PLC, Abingdon, UK), the patient was diagnosed with CD according to
World Health Organization criteria (8). The presenting CD activity index (CDAI)
was 231.0 (9).
Prednisone (Zhejiang Xianju Pharmaceutical Co.,
Ltd., Zhejiang, China) 60 mg/day was prescribed with a concomitant
dose of 100 mg azathioprim (Shanghai Xinyi Pharmaceutical Co.,
Ltd., Shanghai, China) daily in September 2015 for 8 months. LBP
began to show improvement 5 days after treatment. However, by April
2016, the CRP level was 57.60 mg/l, the CDAI was 284, and a second
DXA revealed no improvement of BMD (lumbar Z-score, −3.1 SD;
T-score, −3.2 SD). In addition, hypertension, an adverse effect of
prednisone, was tracked. Given this result and the patient's
insensitivity to steroids, prednisone was switched to adalimumab
(Humira®; 40 mg/2 weeks, subcutaneous injection; Vetter
Pharma International GmbH, Ravensburg, Germany) in May 2016. By
November 2016, CRP and ESR were maintained at normal levels (7.12
mg/l and 10 mm/h, respectively), Hb level was 158 g/l and the CDAI
was 148.0. DXA revealed an improved BMD (lumbar Z score, −1.9 SD;
T-score, −2.1 SD) and abdominal CT scan demonstrated improved
mineralization, with sclerosis of vertebral bodies and intestinal
inflammation (Fig. 2E).
Nevertheless, capsule endoscopy indicated no significant
improvement of small intestinal disease (Fig. 2F). The patient is still undergoing
treatment with biological agents and is followed up every 2 months.
The patient provided written informed consent for publication of
the present case report.
Discussion
Reduced bone density is an extra-intestinal
manifestation and a common complication of IBD (10). However, osteoporosis as an initial
symptom of IBD is rare. The present report detailed a case of
osteoporosis as a presenting manifestation of CD, and osteoporosis
was improved following treatment of CD with glucocorticoids.
The possible reasons leading to osteoporosis in IBD
are corticosteroid use, smoking and gut inflammation (10). No history of corticosteroid use and
metabolic bone disease were tracked in the present patient. Smoking
alone did not suitably explain osteoporosis. Therefore, the
inflammatory activity of CD itself may be a main contributor to
osteoporosis (11). One of the
possible mechanisms of osteoposrosis in IBD is malabsorption.
Calcium deficiency and low vitamin D levels occurred as a result of
small intestinal dysfunction in the present patient. A previous
5-year study identified that low vitamin D levels are common in
patients with IBD, and IBD patients with low mean vitamin D levels
demonstrated worse disease activity, worse pain and higher
requirement for steroids (4). The
use of vitamin D may improve osteoporosis (12); however, this was not the case for the
present patient. LBP was not improved following treatment with
calcium and vitamin D. Furthermore, although BMD improved following
steroid and biological treatment, endoscopic performance was not
notably improved in the present case. This phenomenon suggested
that malabsorption may be a partial cause of osteoporosis in CD,
and osteoporosis may be the result of extra-intestinal
inflammation.
In the present case, prednisone and azathioprim were
prescribed, and the LBP began to improve following treatment,
indicating that osteoporosis was associated with inflammation.
Immune-associated inflammation also participated in the genesis of
bone loss, as previously reported (13). T cell reconstitution is accompanied
by increased bone resorption and decreased BMD (14). Proinflammatory cytokines may also
contribute to bone loss and increase the risk of fracture (5). A previous study demonstrated that IL-6
levels were higher in patients with CD than the levels in controls
(15). Thus, steroids were able to
reduce LBP in the present case. Nevertheless, the present patient
suffered from adverse effects and insensitivity to steroids, so
adalimumab, an anti-TNF antibody, was administered, which resulted
in improved BMD and CDAI. TNFs are cytokines that are associated
with bone loss, and the pathway involved is the receptor activator
of nuclear factor-κB, which is expressed on the surface of
osteoblasts (16). Additionally,
interferon regulatory factor-1 (IRF1) is regarded as a genetic risk
for IBD, and a mutant murine model of IRF1−/− indicated
that IRF1 deficiency was related to decreased proliferation of bone
marrow-derived osteoblast precursors and increased mineralization
activity, suggesting its role in regulating bone metabolism
(17). Accordingly, bone loss may be
an initial manifestation of CD.
In conclusion, for bone loss, the possibility of
small intestinal CD should be considered, and CD as the primary
disease should be treated actively. Adequate calcium supplements
should be administered to patients with CD, physical activity
should be encouraged, and smoking or excessive alcoholic intake
should also be avoided.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CO performed endoscopy examination. DP performed the
magnetic resonance imaging and computed tomography scans. FL and HW
collected the data and wrote the manuscript. JZ analyzed the data
and revised the manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
the publication of this case report.
Consent for publication
The patient provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ott C and Schölmerich J: Extraintestinal
manifestations and complications in IBD. Nat Rev Gastroenterol
Hepatol. 10:585–595. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Etzel JP, Larson MF, Anawalt BD, Collins J
and Dominitz JA: Assessment and management of low bone density in
inflammatory bowel disease and performance of professional society
guidelines. Inflamm Bowel Dis. 17:2122–2129. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miznerova E, Hlavaty T, Koller T, Toth J,
Holociova K, Huorka M, Killinger Z and Payer J: The prevalence and
risk factors for osteoporosis in patients with inflammatory bowel
disease. Bratisl Lek Listy. 114:439–445. 2013.PubMed/NCBI
|
|
4
|
Kabbani TA, Koutroubakis IE, Schoen RE,
Ramos-Rivers C, Shah N, Swoger J, Regueiro M, Barrie A, Schwartz M,
Hashash JG, et al: Association of vitamin D level with clinical
status in inflammatory bowel disease: A 5-year longitudinal study.
Am J Gastroenterol. 111:712–719. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Clowes JA, Riggs BL and Khosla S: The role
of the immune system in the pathophysiology of osteoporosis.
Immunol Rev. 208:207–227. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schulte CM, Dignass AU, Goebell H, Röher
HD and Schulte KM: Genetic factors determine extent of bone loss in
inflammatory bowel disease. Gastroenterology. 119:909–920. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Thearle M, Horlick M, Bilezikian JP, Levy
J, Gertner JM, Levine LS, Harbison M, Berdon W and Oberfield SE:
Osteoporosis: An unusual presentation of childhood Crohn's disease.
J Clin Endocrinol Metab. 85:2122–2126. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
APDW2004 Chinese IBD Working Group.
Retrospective analysis of 515 cases of Crohn's disease
hospitalization in China: Nationwide study from 1990 to 2003. J
Gastroenterol Hepatol. 21:1009–1015. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Harvey RF and Bradshaw JM: A simple index
of Crohn's-disease activity. Lancet. 1:5141980. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Targownik LE, Bernstein CN and Leslie WD:
Inflammatory bowel disease and the risk of osteoporosis and
fracture. Maturitas. 76:315–319. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Phan CM and Guglielmi G: Metabolic bone
disease in patients with malabsorption. Semin Musculoskelet Radiol.
20:369–375. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee DY, Jee JH, Cho YY, Jang JY, Yu TY,
Kim TH, Hong YJ, Hong WJ, Jin SM, Hur KY, et al: Serum
25-hydroxyvitamin D cutoffs for functional bone measures in
postmenopausal osteoporosis. Osteoporos Int. 28:1377–1384. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Iseme RA, McEvoy M, Kelly B, Agnew L,
Walker FR and Attia J: Is osteoporosis an autoimmune mediated
disorder? Bone Rep. 7:121–131. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ofotokun I, Titanji K, Vikulina T,
Roser-Page S, Yamaguchi M, Zayzafoon M, Williams IR and Weitzmann
MN: Role of T-cell reconstitution in HIV-1 antiretroviral
therapy-induced bone loss. Nat Commun. 6:82822015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sylvester FA, Wyzga N, Hyams JS and
Gronowicz GA: Effect of Crohn's disease on bone metabolism in
vitro: A role for interleukin-6. J Bone Miner Res. 17:695–702.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ali T, Lam D, Bronze MS and Humphrey MB:
Osteoporosis in inflammatory bowel disease. Am J Med. 122:599–604.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Salem S, Gao C, Li A, Wang H,
Nguyen-Yamamoto L, Goltzman D, Henderson JE and Gros P: A novel
role for interferon regulatory factor 1 (IRF1) in regulation of
bone metabolism. J Cell Mol Med. 18:1588–1598. 2014. View Article : Google Scholar : PubMed/NCBI
|