Introduction
The primary symptoms of insomnia include difficulty
in falling asleep, being easily awoken and unable to fall asleep
again and being kept awake throughout the night (1). In Traditional Chinese Medicine, this
disorder is called ‘Bu Mei’ (2).
Insomnia may negatively impact the quality of the individuals
everyday life (3,4). The prevalence of insomnia disorder is
~10–20% in the USA (5), with ~50% of
cases having a chronic cause. Insomnia may result in a diminished
cognitive ability, including attention deficit, poor memory and
impaired decision making (4).
Insomnia symptoms are characterized by prolonged sleep latency and
difficulty staying asleep as long as desired (4). Benzodiazepines are commonly prescribed
for short-term relief of anxiety and insomnia symptoms, however
certain patients continue taking these drugs and become long-term
benzodiazepine users (6). Compared
with drug therapy, acupuncture has been demonstrated to exhibit
improved effects and cause fewer adverse reactions, however it may
still lead to local allergies, local muscle tension and pain caused
by needling or allergic reactions to the metal used (7,8). The
most common side effects associated with benzodiazepines are
sedation, dizziness, weakness and unsteadiness (9). A previous randomized placebo-controlled
study on the efficacy and safety of acupuncture [at Baihui (GV20),
Yintang (EX-HN3), bilateral ear Shenmen, Sishencong (EX-HN1) and
Anmian (EX)] for the short-term treatment of primary insomnia,
revealed that electroacupuncture was superior to placebo
acupuncture (10). A recent study
has reported that the augmented acupuncture formula (points LI4,
LIV3, EX-HN3, GV20, LU7 and KID6) was more effective for the
treatment of depression and improved the sleep quality in patients
who already had depression, compared with the standard acupuncture
formula (points LI4, LIV3, EX-HN3 and GV20) (11). Based on this GV20 is frequently used
for the acupuncture treatment of insomnia (12). Previous studies of acupuncture
treatment have primarily focused on subjectively reported symptoms
of insomnia. Consequently, they were not able to observe the
mechanisms of acupuncture's effect on insomnia. In the present
study, electroencephalogram (EEG) will be used to assess changes in
the brain activity in real time. These measures will objectively
examine real-time physiological changes due to acupuncture
(13). To explore the mechanism of
GV20 acupuncture treatment on insomnia, a rat model of sleep
deprivation was constructed and the instant effects of acupuncture
at GV20 on EEGs was analyzed by assessing the change of frequency
of EEG α and β waves.
Materials and methods
Experimental animals and grouping
A total of 16 Wistar male rats (age, 12 months;
weight, 340±10 g) were obtained from the Experimental Animal
Research Center of Hubei (Wuhan, China; no. SCXK(E)2008-0005). The
rats were allowed free access to food and water and were housed
under a controlled temperature (23±2°C) and humidity (40–60%), with
12 h of artificial light per day. Following adaptive feeding for 1
week prior to the experiment, all rats were divided into the blank
group, the GV20 group, the sham acupoint group and the model group
(4 rats per group). All experimental procedures complied with the
guidelines of the Principles of Laboratory Animal Care (14) and the legislation of the People's
Republic of China for the Use and Care of Laboratory Animals
(15). The experimental protocols
were approved by the Animal Experimentation Ethics Committee of the
Hubei University of Traditional Chinese Medicine (Wuhan,
China).
Experiment instruments
An MP150 multichannel physiological signal recorder
(Biopac Systems Inc., Goleta, CA, USA) and cuboid-shaped wire mesh
(100×90×15 cm) were used in the present study. A circular sink
(120×80 cm) was purchased from Chengdu Taimeng Technology Co., Ltd.
(Chengdu, China) and an acupuncture needle (0.20×13 mm) was
obtained from Beijing Hanyi Medical Apparatus and Instruments
Center (Beijing, China).
Modeling method
The modified multiple platform method (MMPM) using
the platform technique (16) was
applied in the present experiment, using 12 platforms (17). The cuboid-shaped wire mesh was placed
into a circular sink, and the sink was filled with water until the
water was ~1 cm below the surface of the grid the rats were on. The
12 rats (GV20, sham acupoint and model groups) were settled on the
cross points and were forced to grasp the wire to maintain a
standing position to prevent falling. These rats could freely move
around the sink on the mesh. When the rats fell asleep, they would
immediately fall into the water due to the relaxation in their
muscle tension. As a consequence of this, rats would need to swim
to the wire mesh and stand on it again. The temperature of the room
was maintained at 25±1°C. During the total 72 h of producing the
model, water in the sink was exchanged once every 12 h. While
exchanging water, the rats were placed in cages to be fed. The
feeding time was limited to 1 min and the cages were kept shaking
to prevent the rats from falling to sleep.
The blank group was reared in a normal environment
(temperature, 25±1°C) with a 12 h light/dark cycle. In order to
eliminate the influence of swimming and the limitation of feeding
time, the blank group was also fed once every 12 h, with the
feeding time limited to 1 min. Rats were forced to swim for 10 sec
after every feed.
Intervention methods
Following 72 h of modeling, EEGs of all 16 rats were
measured and recorded immediately (120 sec for each rat).
Subsequently, the acupuncture treatment and synchronized measuring
of EEGs was initiated instantly (within 120 sec of treating and
recording for each rat).
In order to obtain EEG measurements, sterilized
needle electrodes were inserted into the subcutaneous tissues of
rat's heads in an awakened state. The positive electrode was 0.3 cm
to the right of the vertex of parietal bone and the negative
electrode was 0.3 cm to the left of the vertex of parietal bone.
The reference electrode was placed on the subcutaneous tissue of
the neck. During the measurement and the recording, all the rats
were captured and fastened in the same way with homemade
cloths.
For acupuncture treatment, the acupoints were based
on the ‘Map of the Experimental Animal Acupuncture Points,’ which
was formulated by the Experimental Acupuncture Institute of China
Association of Acupuncture and Moxibustion (18). For the GV20 group, the needle was
horizontally inserted at GV20 at the vertex of the rat's parietal
bone (19) via an even
reinforcing-reducing method, as described previously (20). The needle was rotated bidirectionally
within 90° at a speed of 2 Hz. The needle was retained for 120 sec,
and rotated once every 40 sec. For the sham acupoint group, the
needle was inserted at the sham acupoint (0.15 cm to the right of
the vertex of the rat's parietal bone), and the manipulation was
the same as that of the GV20 group.
Statistical analysis
Data were analyzed with the SPSS software, version
20.0 (IBM Corp., Armonk, NY, USA) and expressed as the mean ±
standard deviation. One-way analysis of variance (ANOVA) followed
by Tukey's post hoc test was performed for analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
Behavior observation
During the first 24 h of modeling, the GV20 group,
the sham acupoint group and the model group were acting normally
and rats crept on the wire and reacted strongly when being
captured. Between 25–48 h, the majority of the rats demonstrated
tiredness: Rats crouched and shook instead of creeping and
occasionally fell into the water and had to swim back to the wire.
Furthermore, rats began to show signs of a reduced appetite when
being fed, as they preferred sleeping to eating, their cages had to
be kept shaking to prevent them from sleeping. Between 49–72 h, all
three groups of rats were observed and appeared much thinner
compared with prior to the modeling experiment, their fur was wet
and messy, and their ears, eyes and the extremities of limbs had
turned pink or pale. In addition, the majority of the rats
demonstrated signs of excitement and mania. Rats shook a lot,
tended to fight each other, fiercely struggled when being captured
for feeding and had good appetites when being offered food and
water. During the 72-h modeling period of the three groups, the
rats in the blank group, which were reared under standard
conditions, acted normally.
Within 10 sec of acupuncture treatment, rats in the
GV20 group fell into sleep instantly, breathing stably and were
crouched with their eyes closed. The sham acupoint group remained
awake within 10 sec of the sham acupoint acupuncture treatment and
were still shaking, aggressively; their characteristics were
similar to the model group at the same time.
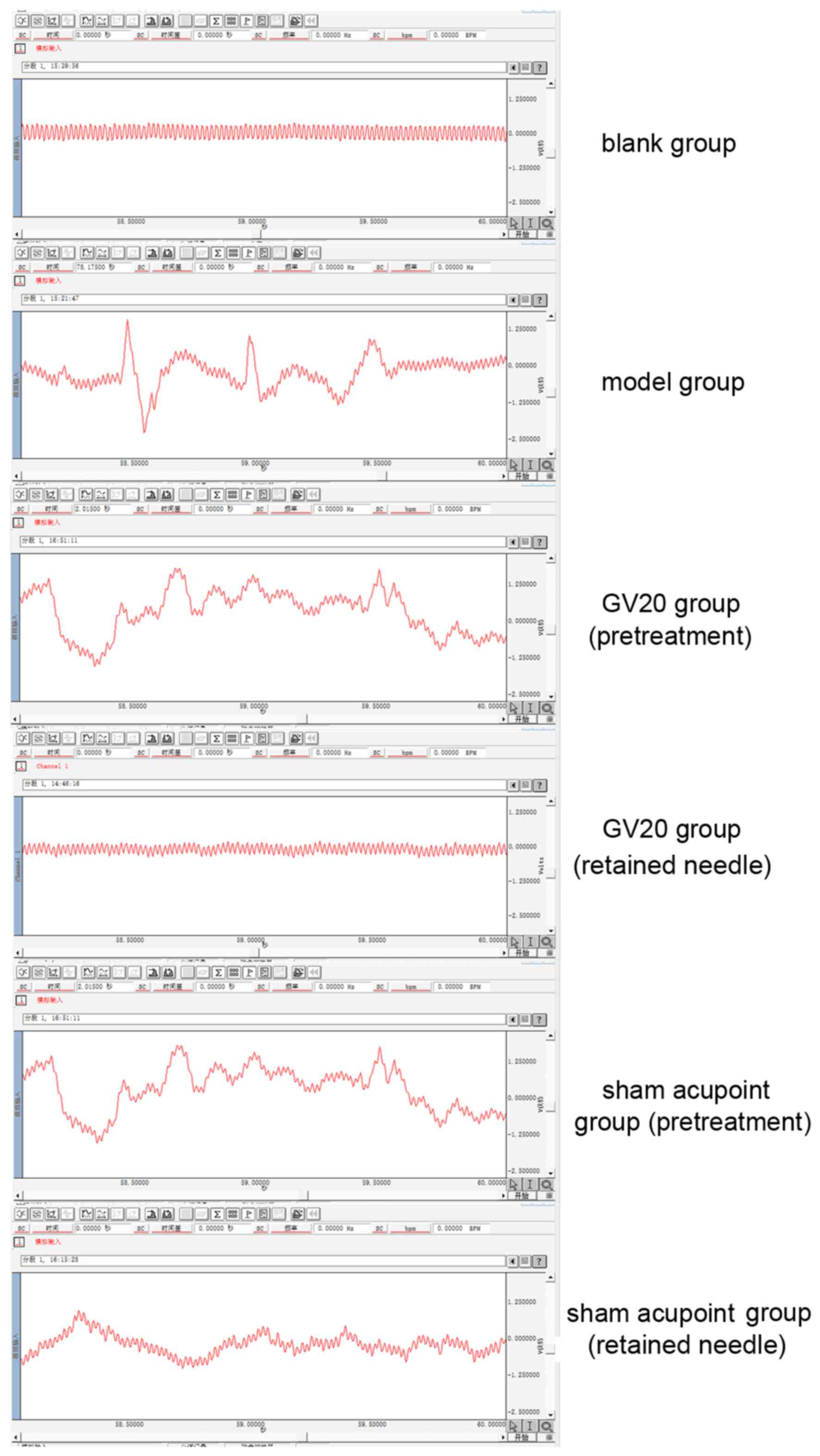
Analysis of EEG
EEGs from all rats and the analysis of the frequency
of α and β waves are demonstrated in Fig. 1 and Tables
I and II. As indicated in
Fig. 1, compared with the blank
group, the model, GV20 (pretreatment) and sham acupoint
(pretreatment) groups demonstrated similar characteristics in their
EEG data. The EEGs indicated relatively disordered shapes,
irregular waves, low amplitude and unclear amplitude modulations,
which were similar to EEGs of panasthenia (21). Paroxysmal spines, sharp waves,
spine-slow synthetical waves and sharp-slow synthesis waves were
observed on the EEGs. The frequency of α and β waves in all four
groups were compared using one-way ANOVA followed by Tukey's post
hoc test. Significant differences among the four groups were
observed (α wave frequency, F=39.919 and P<0.05; β wave
frequency, F=61.170 and P<0.05; Table
I). The frequency of α waves of the GV20 (pretreatment), sham
acupoint (pretreatment) and the model groups were significantly
reduced compared with the blank group (P<0.05). Conversely, the
frequency of β waves of the GV20 (pretreatment), sham acupoint
(pretreatment) and model groups were significantly increased
compared with the blank group (P<0.05). These findings indicated
that the production of the sleep deprivation model was successful.
Comparison of the frequency of α and β waves in the GV20 and sham
acupoint groups (pretreatment and retained needle) using one-way
ANOVA followed by Tukey's post hoc test indicated the differences
among the two groups were statistically significant (α wave
frequency, F=32.225 and P<0.05; β wave frequency, F=53.352,
P<0.05; Table II), allowing a
comparative study for acupuncture treatment to be performed.
 | Table I.Frequency of α and β waves of the
blank, model, GV20 (pretreatment) and sham acupoint (pretreatment)
groups. |
Table I.
Frequency of α and β waves of the
blank, model, GV20 (pretreatment) and sham acupoint (pretreatment)
groups.
|
|
| Wave frequency,
mHz |
|---|
|
|
|
|
|---|
| Group | n | α | β |
|---|
| GV20
(pretreatment) | 4 |
10.1208±0.4955a |
32.3789±0.7171a |
| Sham acupoint
(pretreatment) | 4 |
10.5254±0.4064a |
32.6520±2.1659a |
| Model | 4 |
10.0009±0.0857a |
33.0258±0.7713a |
| Blank | 4 | 12.2918±0.1842 | 21.5471±0.7273 |
 | Table II.Frequency of α and β waves in the GV20
and sham acupoint groups. |
Table II.
Frequency of α and β waves in the GV20
and sham acupoint groups.
|
|
| Wave frequency,
mHz |
|---|
|
|
|
|
|---|
| Group | Time at which
measurement taken | α | β |
|---|
| GV20 |
|
|
|
| Rat
1 | Pretreatment | 10.1936 | 32.6975 |
|
| Retained needle | 12.2616a | 25.4447a |
| Rat
2 | Pretreatment | 10.5781 | 32.6994 |
|
| Retained needle | 12.2057a | 23.0262a |
| Rat
3 | Pretreatment | 10.2926 | 32.9251 |
|
| Retained needle | 12.3499a | 22.8959a |
| Rat
4 | Pretreatment | 9.4188 | 31.1205 |
|
| Retained needle | 12.2616a | 22.9197a |
| Sham acupoint |
|
|
|
| Rat
1 | Pretreatment | 10.5558 | 31.9311 |
|
| Retained
needle |
10.7676b |
31.5172b |
| Rat
2 | Pretreatment | 10.8959 | 29.7769 |
|
| Retained
needle |
10.4773b |
29.3446b |
| Rat
3 | Pretreatment | 10.6971 | 35.6291 |
|
| Retained
needle |
10.2877b |
36.3446b |
| Rat
4 | Pretreatment | 9.9528 | 33.2436 |
|
| Retained
needle | 9.6955b |
33.4247b |
For the GV20 group, the differences in frequency of
α and β waves at pretreatment compared with frequencies when the
needle was retained at GV20 were statistically significant
(Pα=0.003 and Pβ=0.001), and when the needle
was retained, the EEG frequency of α waves was significantly
increased whereas the frequency of β waves was significantly
decreased. In the sham acupoint group, the differences in the
frequency of α and β waves between pretreatment and when the
needled was retained were not statistically significant
(Pα=0.237 and Pβ=0.966). These results
indicated that the acupuncture treatment at GV20 was able to
relieve the central excitement of insomnia in rats, improve the
frequency of α waves and decrease the frequency of β waves,
providing an instant sedative effect. Conversely, sham acupuncture
treatment demonstrated no notable curative effect.
Discussion
GV20 is located on the vertex of the body and is
also called the ‘intersection point of Three Yang and Five
Channels’ because GV20 is the intersection point of Governor
vessel, foot-taiyang meridian, foot-shaoyang meridian,
hand-shaoyang meridian and foot-jueyin meridian (22). Various studies support the sedative
effects of GV20 in treating insomnia and relieving symptoms
(23,24). A previous study has indicated that
treatment using GV20 regulates the body state in patients with
insomnia by repairing neurons, regulating the content of
5-hydroxyidnoleacetic acid, improving the blood supplement to the
brain and enhancing the activity of acetylcholinesterase in the
brain (25).
As an objective index in evaluating brain function,
EEG is an intuitive, sensitive, specific and easy method for
analysis, which makes it a popular method in research and for the
diagnosis of mental disorders and central nervous system diseases
(26). In addition, EEG is generally
applied in the study of psychology, scientific research and the
detection of anesthesia (27). In
literature regarding sleep disorders, EEGs are typically used. For
example, polysomnography is an important detection method with EEG
being its most important index (28). Currently, EEG is used in comparing
changes in patients with insomnia before and after their treatment
to determine the clinical effects (29). In cases where the normal conscious
body is in a quiet and relaxed state, predominantly α waves of 8–13
Hz are indicated in EEGs (30).
However, in cases where the body is in an anxious, nervous or manic
state, β waves of 14–30 Hz are primarily observed (31). In conscious patients with insomnia,
the EEG data may indicate the phenomena of slowing α waves, lower
amplitude and a lack of amplitude modulation, in addition to
increased β wave rhyme (32–36). Therefore, the increase in the
proportion of α waves is a valuable index in evaluating the change
of insomnia symptoms, and changes in β waves may be used in
determining anxiety and mania in patients with insomnia.
In the present study, when sleep deprivation was
achieved, the frequency of α waves in the GV20 (pretreatment), sham
acupoint (pretreatment) and model groups were decreased compared
with the blank group. However, the frequency of β waves in the GV20
(pretreatment), sham acupoint (pretreatment) and model groups were
increased compared with the blank group. Results demonstrated that
after 72 h of sleep deprivation, rats with insomnia were anxious
and excited. When the needle was retained at GV20, the frequency of
α waves were improved and the frequency of β waves was decreased,
which suggested this treatment provided an instant sedative
effect.
In conclusion, the present findings indicated that
acupuncture treatment at GV20 may be an effective application in
treating insomnia symptoms, such as anxiety and mania. The present
study may be meaningful for designing clinical acupuncture
treatment plans for patients with insomnia.
Acknowledgements
The present study was supported by Hubei Province
Scientific and Technological Research Projects (grant nos. 20162006
and 2016CFB221).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ohayon MM: Epidemiology of insomnia: What
we know and what we still need to learn. Sleep Med Rev. 6:97–111.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Deng A, Jiang Re and Ma Z: Literature
study on distribution features of tcm syndromes and syndrome
elements of insomnia. Chin Med Mod Dis Education China. 13:147–149.
2015.(In Chinese).
|
|
3
|
Mishima K, DiBonaventura Md and Gross H:
The burden of insomnia in Japan. Nat Sci Sleep. 7:1–11.
2015.PubMed/NCBI
|
|
4
|
Buysse DJ: Insomnia. JAMA. 309:706–716.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Burman D: Sleep disorders: Insomnia. FP
Essent. 460:22–28. 2017.PubMed/NCBI
|
|
6
|
Kaufmann CN, Spira AP, Depp CA and
Mojtabai R: Long-term use of benzodiazepines and nonbenzodiazepine
hypnotics, 1999–2014. Psychiatr Serv. 69:235–238. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xie ZY and Wu Xi: Observation on the
efficacy of acupoint massage plus moxibustion for refractory
insomnia. J Acupuncture Tuina Sci. 13:44–48. 2015.(In Chinese).
View Article : Google Scholar
|
|
8
|
Sok SR, Erlen JA and Kim KB: Effects of
acupuncture therapy on insomnia. J Adv Nurs. 44:375–384. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Uzun S, Kozumplik O, Jakovljević M and
Sedić B: Side effects of treatment with benzodiazepines. Psychiatr
Danub. 22:90–3. 2010.PubMed/NCBI
|
|
10
|
Yeung WF, Chung KF, Zhang SP, Yap TG and
Law AC: Electroacupuncture for primary insomnia: A randomized
controlled trial. Sleep. 32:1039–1047. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wen X, Wu Q, Liu J, Xu Z, Fan L, Chen X,
He Q, Ma R, Wu Y, Jiang S, et al: Randomized single-blind
multicenter trial comparing the effects of standard and augmented
acupuncture protocols on sleep quality and depressive symptoms in
patients with depression. Psychol Health Med. 23:375–390. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kalavapalli R and Singareddy R: Role of
acupuncture in the treatment of insomnia: A comprehensive review.
Complement Ther Clin Pract. 13:184–193. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Han KH, Kim SY and Chung SY: Effect of
acupuncture on patients with insomnia: Atudy protocol for a
randomized controlled trial. Trials. 15:4032014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bayne K: Revised guide for the care and
use of laboratory animals available. american physiological
society. Physiologist. 39(199): 208–211. 1996.
|
|
15
|
Kong Q and Qin C: Analysis of current
laboratory animal science policies and administration in China.
ILAR J. 51:e1–e11. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cohen HB and Dement WC: Sleep: Changes in
threshold to electroconvulsive shock in rats after deprivation of
‘paradoxical’ phase. Science. 150:1318–1319. 1995. View Article : Google Scholar
|
|
17
|
Machado RB, Hipólide DC, Benedito-Silva AA
and Tufik S: Sleep deprivation induced by the modified multiple
platform technique: Quantification of sleep loss and recovery.
Brain Res. 1004:45–51. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yin CS, Jeong HS, Park HJ, Baik Y, Yoon
MH, Choi CB and Koh HG: A proposed transpositional acupoint system
in a mouse and rat model. Res Vet Sci. 84:159–65. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yin CS, Jeong HS, Park HJ, Baik Y, Yoon
MH, Choi CB and Koh HG: A proposed transpositional acupoint system
in a mouse and rat model. Res Vet Sci. 84:159–65. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ding N, Jiang J, Lu M, Hu J, Xu Y, Liu X
and Li Z: Manual acupuncture suppresses the expression of
proinflammatory proteins associated with the nlrp3 inflammasome in
the hippocampus of samp8 mice. Evid Based Complement Alternat Med.
2017:34358912017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Neznamov GG, Bochkarev VK, Siuniakov SA
and Grishin SA: Characteristics of ladasten effect in neurasthenia
patients with various eeg parameters. Eksp Klin Farmakol. 71:18–25.
2008.(In Russian). PubMed/NCBI
|
|
22
|
Shen EY, Chen FJ, Chen YY and Lin MF:
Locating the acupoint baihui (GV20) beneath the cerebral cortex
with MRI reconstructed 3D neuroimages. Evid Based Complement
Alternat Med. 2011:3624942011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Montakab H and Langel G: The effect of
acupuncture in the treatment of insomnia. Clinical study of
subjective and objective evaluation. Schweiz Med Wochenschr Suppl.
62:49–54. 1994.(In French). PubMed/NCBI
|
|
24
|
Spence DW, Kayumov L, Chen A, Lowe A, Jain
U, Katzman MA, Shen J, Perelman B and Shapiro CM: Acupuncture
increases nocturnal melatonin secretion and reduces insomnia and
anxiety: A preliminary report. J Neuropsychiatry Clin Neurosci.
16:19–28. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jiang YJ: Electro acupuncture Du20 and
Du24 on Cognitive Impairment after Stoke (unpublished PhD
thesis)Fujian University of Chinese Medicine. Fuzhou: 2011,
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fu K, Qu J, Chai Y and Zhou T: Hilbert
marginal spectrum analysis for automatic seizure detection in EEG
signals. Biomedical Signal Processing Control. 18:179–185. 2015.
View Article : Google Scholar
|
|
27
|
Zhang C: Analysis of electrocephalogram
and electrocephafulctuo technology on ‘rigid-gentle syndrome
differentiation’ of psychosomatic diseases (unpublished PhD
thesis). China Academy of Chinese Medicine Science. 2013.
|
|
28
|
Kempfner J, Sorensen GL, Sorensen HB and
Jennum P: Automatic REM sleep detection associated with idiopathic
rem sleep Behavior Disorder. Conf Proc IEEE Eng Med Biol Soc.
2011:6063–6. 2011.PubMed/NCBI
|
|
29
|
Perlis ML, Kehr EL, Smith MT, Andrews PJ,
Orff H and Giles DE: Temporal and stagewise distribution of high
frequency EEG activity in patients with primary and secondary
insomnia and in good sleeper controls. J Sleep Res. 10:93–104.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Coll MP, Press C, Hobson H, Catmur C and
Bird G: Crossmodal classification of mu rhythm activity during
action observation and execution suggests specificity to
somatosensory features of actions. J Neurosci. 37:5936–5947. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li N, Wang P, Deng B, Wei XL, Che YQ, Jia
CH, Guo Y and Chao W: Influence of acupuncture of Zusanli (ST 36)
on connectivity of brain functional network in healthy subjects.
Zhen Ci Yan Jiu. 36:278–87. 2011.(In Chinese). PubMed/NCBI
|
|
32
|
Perlis ML, Merica H, Smith MT and Giles
DE: Beta EEG activity and insomnia. Sleep Med Rev. 5:363–374. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Perlis ML, Smith MT, Andrews PJ, Orff H
and Giles DE: Beta/Gamma EEG activity in patients with primary and
secondary insomnia and good sleeper controls. Sleep. 24:110–117.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Krystal AD, Edinger JD, Wohlgemuth WK and
Marsh GR: NREM sleep EEG frequency spectral correlates of sleep
complaints in primary insomnia subtypes. Sleep. 25:630–640.
2002.PubMed/NCBI
|
|
35
|
Goljahani A, Bisiacchi P and Sparacino G:
An EEGLAB plugin to analyze individual EEG alpha rhythms using the
‘channel reactivity-based method’. Comput Methods Programs Biomed.
113:853–861. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Merica H, Blois R and Gaillard JM:
Spectral characteristics of sleep EEG in chronic insomnia. Eur J
Neurosci. 10:1826–1834. 1998. View Article : Google Scholar : PubMed/NCBI
|