Introduction
Myocardial infarction is one of the leading causes
of death in patients (1). The
tissues release a variety of chemokines and cytokines after
infarction, which leads to the accumulation of inflammatory cells
and induces inflammation, resulting in fibrosis of myocardial
tissues and cardiac remodeling (2).
This causes heart failure due to a reduction in the cardiac
function (3–5). Regulating post-infarction inflammatory
response can improve cardiac remodeling after myocardial
infarction. This enhances cardiac function and reduces
mortality.
Atorvastatin is currently one of the most commonly
used drugs in clinic for the treatment of coronary heart disease
and is mainly used for the control of risk factors in coronary
heart disease as well as in the improvement of prognosis. As a
result, the incidence of myocardial infarction is reduced (6). Recent findings have shown that
atorvastatin can improve cardiac function after myocardial
infarction (7), but its specific
mechanism remains to be determined. The effects of atorvastatin on
myocardial remodeling after myocardial infarction in rats were
discussed in this study mainly from the aspect of inflammation.
Materials and methods
Reagents and instruments
Chloral hydrate (Wuhan Yuancheng Technology
Development Co., Ltd., Hubei, China), small animal ventilator and
BL-420 biological signal collection system (both from Chengdu TME
Technology Co., Ltd., Sichuan, China), radioimmunoprecipitation
assay (RIPA) lysis buffer (Beyotime Institute of Biotechnology,
Haimen, China) were used in the present study. Hematoxylin and
eosin (H&E), and triphenyl tetrazolium chloride (TTC) staining
was carried out (both purchased from Nanjing Jiancheng
Bioengineering Institute, Jiangsu, China). Masson's trichrome
staining was performed using a Masson Stain kit (D026) (Nanjing
Jiancheng Bioengineering Institute). Color Doppler ultrasonic
diagnostic apparatus (Mindray North America, Mahwah, NJ, USA), as
well as rabbit anti-rat p38 mitogen-activated protein kinase and
phosphorylated p38 polyclonal antibodies (all purchased from Cell
Signaling Technology, Danvers, MA, USA) were used in the study.
Horseradish peroxidase-labeled goat anti-rat antibodies and
diaminobenzidine (DAB) coloration reagent kits were used (both from
Beyotime Institute of Biotechnology). In addition, we used
atorvastatin calcium tablets (Pfizer, Inc., New York, NY, USA),
total cholesterol (TC), low-density lipoprotein cholesterol
(LDL-C), triglyceride (TG) and high-density lipoprotein cholesterol
(HDL-C) test kits (all from Nanjing Jiancheng Bioengineering
Institute). Further reagents and instruments used were: Protease
inhibitor (Roche Diagnostics, Basel, Switzerland), protein
electrophoresis apparatus (Bio-Rad Laboratories, Inc., Hercules,
CA, USA), rapid tissue cell cracker (Wuxi Voshin Instruments Co.,
Ltd., Jiangsu, China), protein loading buffer (Beyotime Institute
of Biotechnology), pre-stained protein marker (Thermo Fisher
Scientific, Inc., Waltham, MA, USA), and fluorescence microscope
(IX73; Olympus Corporation, Tokyo, Japan).
Modeling
Chloral hydrate (300–350 mg/kg) was administered by
intraperitoneal injection. The rats were connected with the
ventilator and BL-420 bioinformation collection system was used
after anesthesia. The thoracic cavity was opened from the 3rd and
4th intercostal space of the left thoracic cavity in rats. Anterior
descending arteries of the rats in the medication and myocardial
infarction groups were ligated with a 6-0 suture. The rats in the
sham operation group were threaded but not ligated. Following
surgery, the chest was closed and erythromycin ointment was
applied. The intratracheal catheter was removed after the rats woke
up from anesthesia, and they were returned to the rearing cage for
a 4-week rearing. Signs of successful myocardial infarction
modeling included: i) Electrocardiogram showed elevated ST segment
and ii) the ligation site and the heart tissue at the cardiac apex
were whitened. The modeling was considered successful when the
aforementioned two requirements were met (8).
Laboratory animals and grouping
A total of 43 male Sprague-Dawley rats (~200 g) were
provided by the Laboratory Animal Center of Hubei Medical
University (cat. no. SCXK E 2016–0008). The study was approved by
the Ethics Committee of Xiangyang No. 1 People's Hospital
(Xiangyang, China). The rats were kept in cage at temperature of
22–25°C and humidity 53–60%. The animals had access to food and
water ad libitum. The rats that were modeled successfully
were divided into four groups using a random number table: i) The
control group (10 rats), rats were fed normally; ii) the sham group
(11 rats), rats were given 2 ml normal saline by gavage every 24 h
continuously for 4 weeks; iii) the non-medication group (11 rats),
rats were given 2 ml normal saline by gavage every 24 h
continuously for 4 weeks and iv) the medication group (11 rats),
atorvastatin was dissolved in the normal saline, and 2 ml
atorvastatin (drug dose: 10 mg/kg) (9–11) was
given to the rats by gavage every 24 h continuously for 4 weeks
after successful modeling.
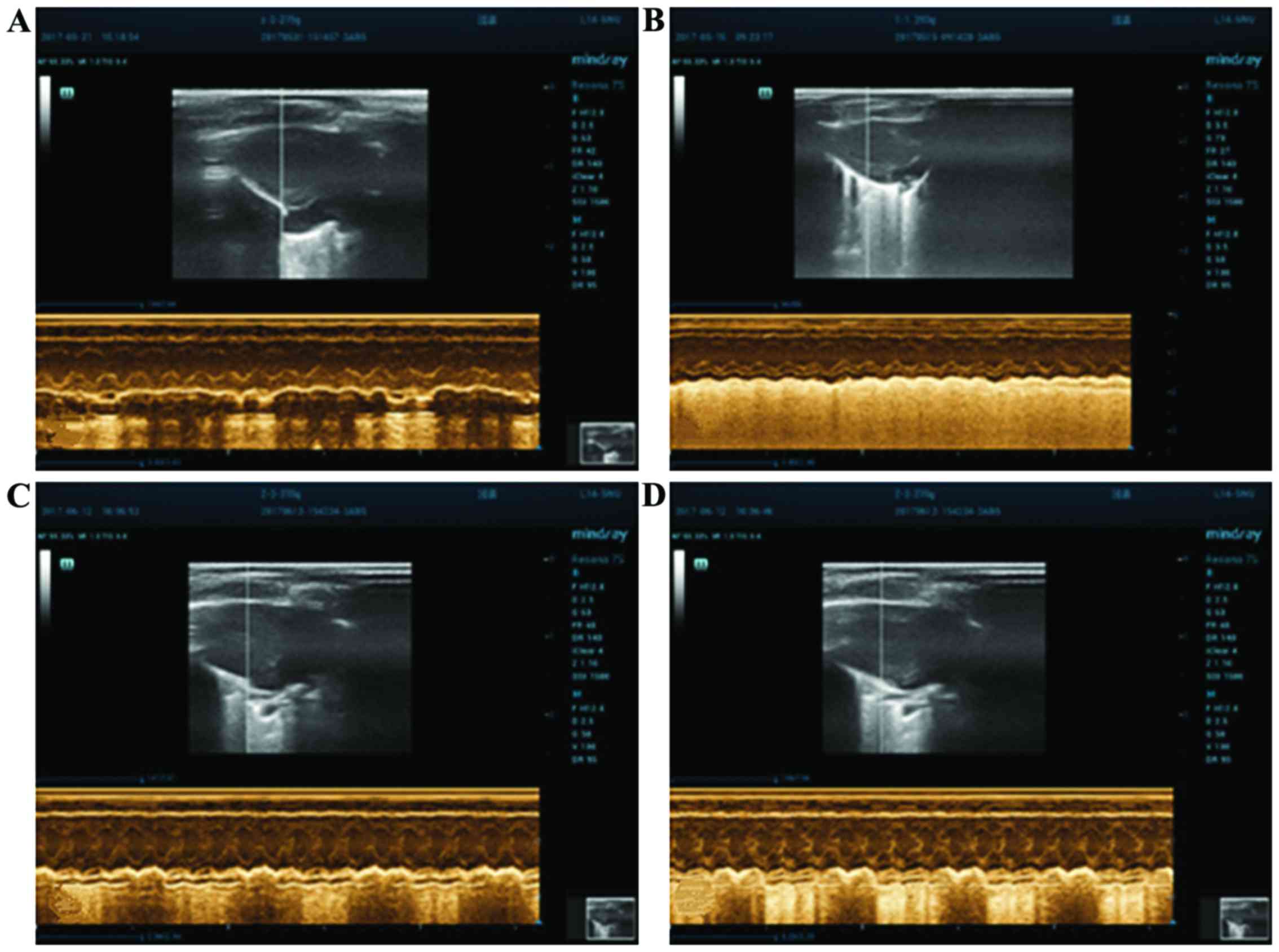
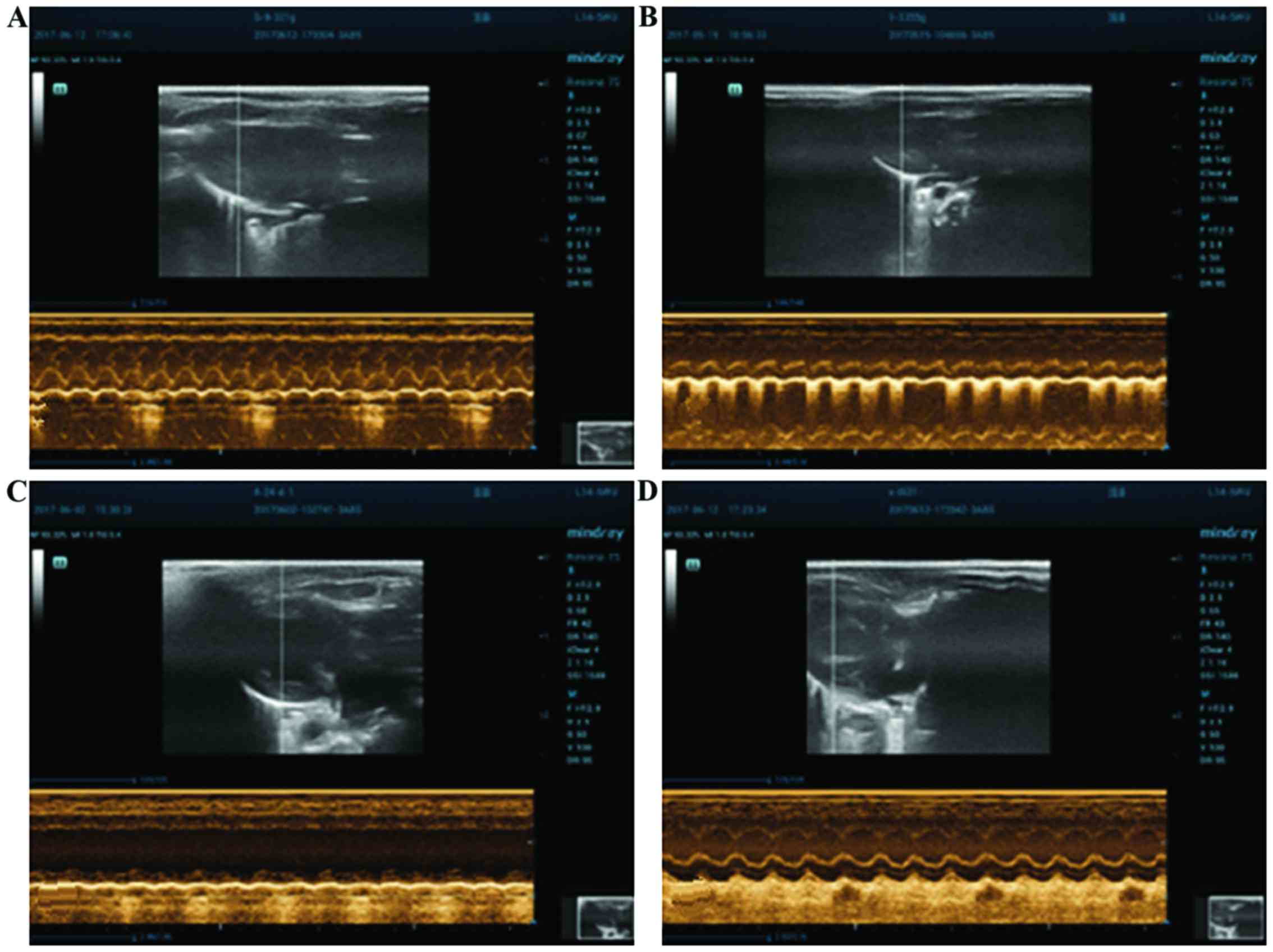
Measurement of cardiac function via
echocardiography
Left ventricular ejection fraction (LVEF),
shortening fraction (SF), left ventricular end-systolic diameter
(LVESD) and left ventricular end-diastolic diameter (LVEDD) of the
rats in each group were measured via color Doppler ultrasonic
diagnostic apparatus before and at 4 weeks after modeling.
Measurement of blood lipids in each
group
Four weeks later, the rats were anesthetized using
chloral hydrate (300–350 mg/kg) via intraperitoneal injection.
Blood (4 ml) was drawn from the abdominal aorta and the plasma was
frozen at −80°C. The concentrations of TC, TG, HDL-C and LDL-C were
detected using the reagent kits.
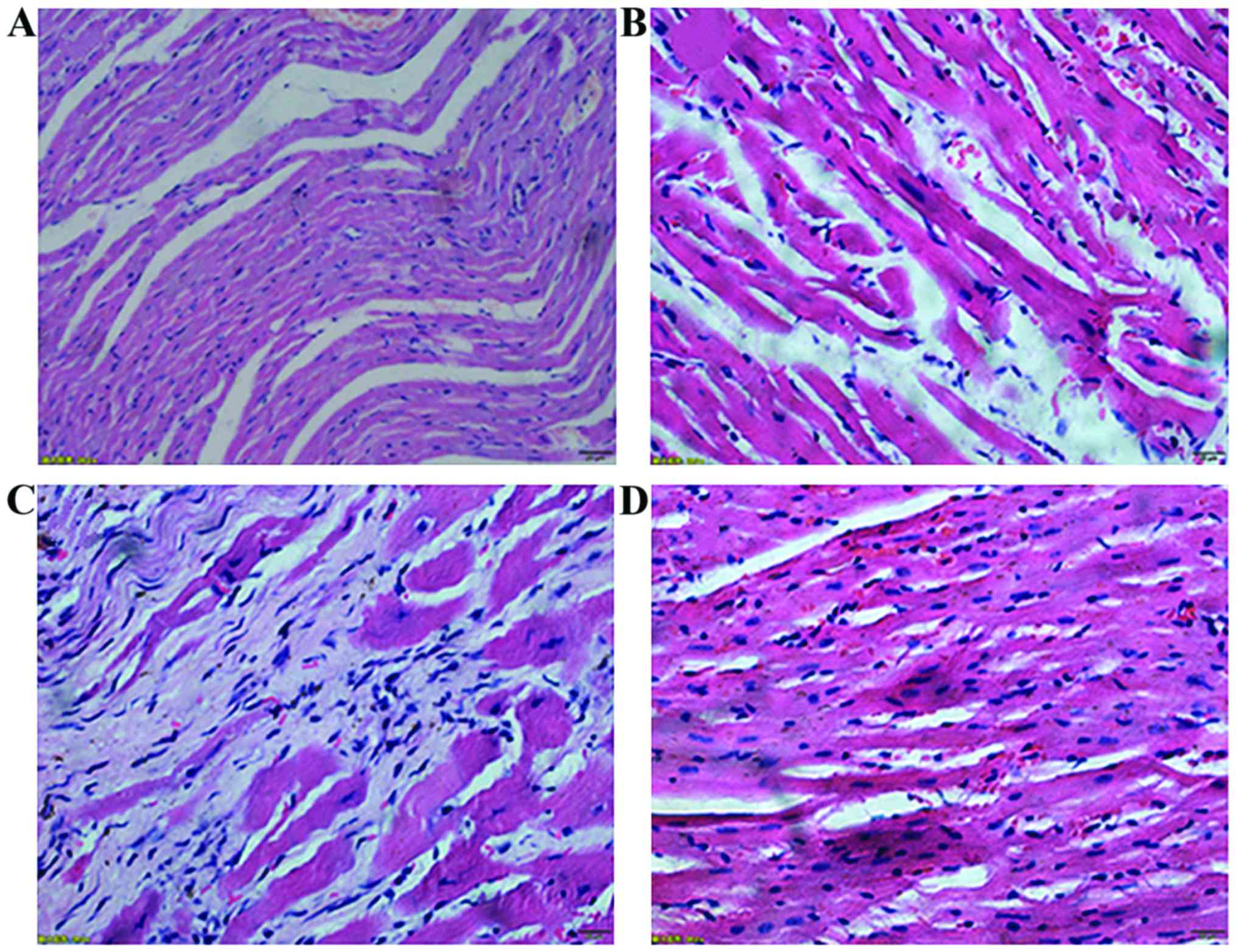
Left ventricular H&E staining
The anterior wall of the left ventricle of the rats
in each group was sampled and fixed in 4% paraformaldehyde. The
samples were embedded with paraffin the next day to produce
paraffin sections. After H&E staining, the samples were placed
under the fluorescence microscope to observe the morphological
changes of the cells.
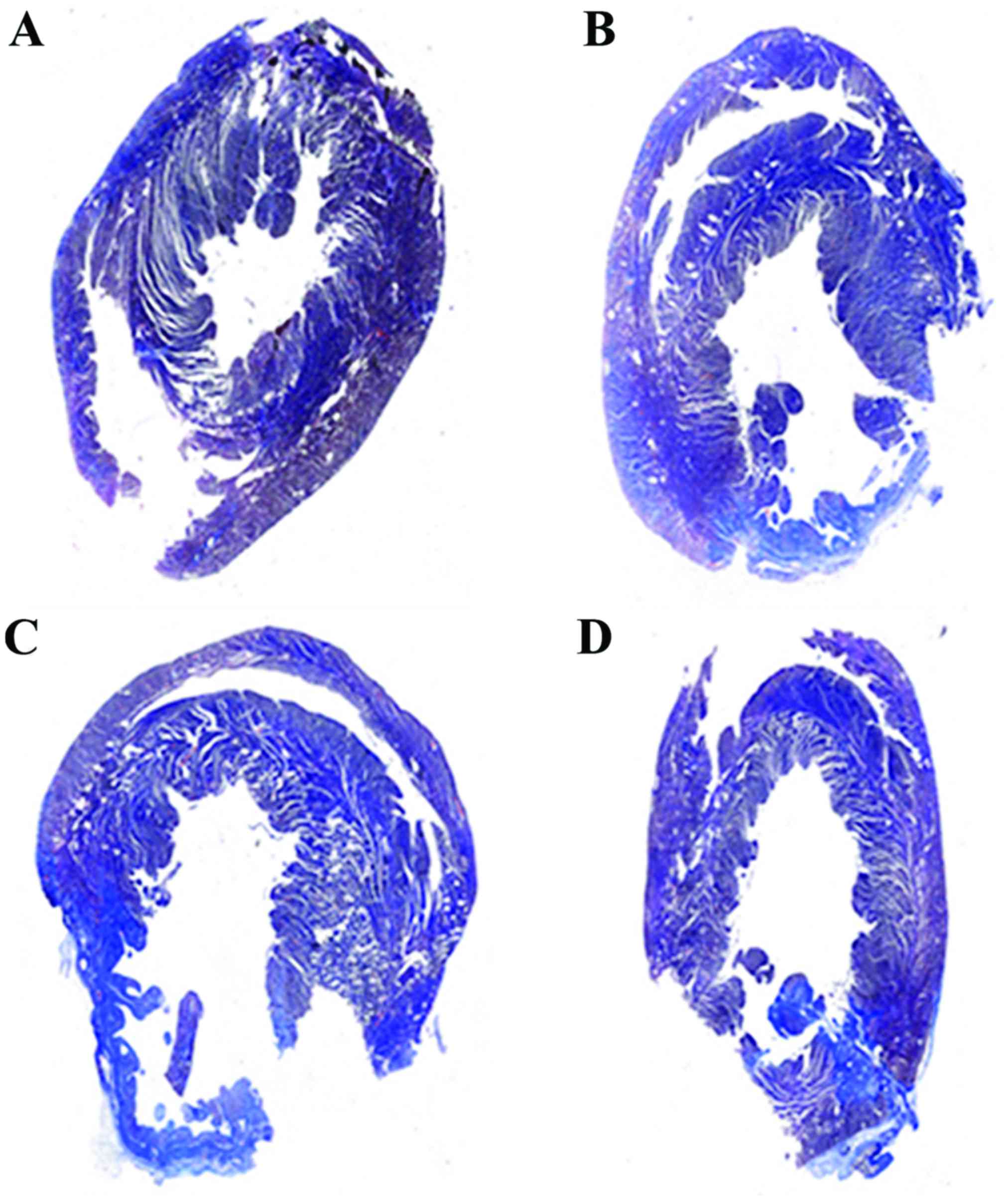
Masson staining
The hearts of the rats were removed and washed
repeatedly with normal saline, then fixed in 4% paraformaldehyde.
Serial sectioning (5 times in total) was conducted for the hearts
of the rats in each group to produce paraffin sections. Masson
staining was performed according to the kit instructions after
dewaxing. The fibrosis area of each group was analyzed using ImageJ
software (National Institutes of Health, Bethesda, MD, USA).
TTC staining
The hearts were removed, washed repeatedly and
placed in the heart cutting slot (RWD Life Science Co., Ltd.,
Shenzhen, China). Then, they were placed in the refrigerator at
−20°C for 2 h. Heart sectioning was conducted in the unit of 2 mm
and placed in TTC dye liquor for incubation at 37°C for 30 min. The
results were observed, and the myocardial infarction size was
measured using ImageJ software (National Institutes of Health).
Western blot analysis
The left ventricles of the rats were excised and cut
into pieces in the size of rice (12). An appropriate amount of RIPA lysis
buffer and protease inhibitors were added. The tissues were
pulverized using a rapid tissue cell cracker and centrifuged at
13,500 × g for 5 min at 4°C. The supernatant was removed and an
appropriate amount of protein loading buffer was added. Then, it
was boiled for 5 min and frozen at −20°C. SDS-PAGE with 5%
concentration and 12% separation gel was used. Pre-stained protein
marker was added to the first well, and 30 µg protein samples were
added to the remaining wells. Electrophoresis was stopped when the
bromophenol blue reached the bottom of the gel. Membrane transfer
was performed at 4°C for 2 h at 200 mA. The wells were eluted with
Tris-buffered saline containing Tween-20 (TBST) and blocked for 2 h
with 5% skimmed milk powder (4% bovine serum albumin was used for
phosphorylated antibodies). Rabbit anti-rat α-tubulin, p38,
phospho-p38 primary polyclonal antibodies (1:500; cat. nos. 2144,
9212 and 9211; Cell Signaling Technology, Danvers, MA, USA) and
rabbit anti-rat TNF-α primary polyclonal antibody (1:500; cat. no.
ARC3012; Thermo Fisher Scientific, Inc.) was added and incubated
overnight at 4°C. Then they were eluted with TBST. Goat anti-rabbit
secondary polyclonal antibody (1:1,000; cat. no. 7074; Cell
Signaling Technology) was added and incubated for 1 h at room
temperature. Finally, they were eluted with TBST, and DAB
coloration reagent kits were used for color development for several
minutes. They were scanned and the images were saved. Gray value
was measured using ImageJ software (National Institutes of
Health).
Statistical analysis
SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) was used
for result processing. A t-test was used for the comparison of
enumeration data between two groups, and analysis of variance with
the Bonferroni's post hoc test was used for comparison among
multiple groups. The data were expressed as mean ± standard
deviation (SD). P<0.05 was considered to indicate a
statistically significant difference.
Results
Effect of atorvastatin on improving
the cardiac function of the rats
LVEDD, LVESD, LVEF and SF in each group did not show
significant differences between groups before modeling (p>0.05,
Table I). The ventricular wall
movement of the rats in the non-medication group was obviously
reduced in comparison with that of the rats in the medication
group. Four weeks after modeling LVEF and SF in the medication
group were significantly higher than those in the non-medication
group (P<0.05). LVESD and LVEDD in the medication group were
obviously lower than those in the non-medication group (P<0.05)
(Figs. 1 and 2, Tables I
and II).
 | Table I.Cardiac function in each group before
modeling (mean ± SD). |
Table I.
Cardiac function in each group before
modeling (mean ± SD).
| Groups | LVEDD (cm) | LVESD (cm) | LVEF (%) | SF (%) |
|---|
| Control | 0.62±0.08 | 0.32±0.08 | 85.75±7.85 | 57.60±7.98 |
| Sham operation | 0.62±0.11 | 0.32±0.10 | 85.33±8.90 | 57.00±8.78 |
| Non-medication | 0.61±0.11 | 0.31±0.11 | 86.75±7.96 | 58.11±7.88 |
| Medication | 0.62±0.07 | 0.32±0.08 | 83.88±8.56 | 60.19±8.13 |
 | Table II.Cardiac function in each group at 4
weeks after modeling (mean ± SD). |
Table II.
Cardiac function in each group at 4
weeks after modeling (mean ± SD).
| Groups | LVEDD (cm) | LVESD (cm) | LVEF (%) | SF (%) |
|---|
| Control | 0.60±0.08 | 0.30±0.75 | 82.20±7.54 | 56.10±9.40 |
| Sham operation | 0.72±0.10 | 0.45±0.70 | 85.75±7.85 | 51.44±9.15 |
| Non-medication |
1.07±0.12a |
0.76±0.11a |
49.13±9.03a |
32.88±9.16a |
| Medication |
0.69±0.09b |
0.39±0.09b |
64.00±8.37b |
49.89±7.51b |
Measurement of blood lipids in each
group 4 weeks later
HDL-C and TG of each group had no statistical
differences (P>0.05). The contents of TC and LDL-C in the blood
of the rats in the medication group were obviously decreased
(P<0.05) (Table III).
 | Table III.Blood lipids in each group 4 weeks
later (mean ± SD) (mmol/l). |
Table III.
Blood lipids in each group 4 weeks
later (mean ± SD) (mmol/l).
| Groups | TC | TG | HDL-C | LDL-C |
|---|
| Control | 2.49±0.18 | 1.35±0.14 | 1.46±0.17 | 0.71±0.15 |
| Sham operation | 2.49±0.19 | 1.48±0.14 | 1.53±0.18 | 0.67±0.17 |
| Non-medication | 2.80±0.28 | 1.35±0.18 | 1.40±0.22 | 0.70±0.13 |
| Medication |
1.78±0.26a | 1.33±0.18 | 1.52±0.19 |
0.43±0.09a |
Comparison of cell morphology of the
rats in each group
The non-medication group showed a large area of
fibrous tissue hyperplasia. There were only a small number of
normal cardiac tissues with incomplete capsule, nuclear
fragmentation and dissolution. Cardiac tissues with clear texture
could be seen in the sections of the rats in the control group. The
capsule was complete, the cell nucleus was blue and the cytoplasm
was red. In addition, the medication group showed a small amount of
fibrous tissue hyperplasia. Necrotic myocardial cells were
significantly reduced, and the texture of the myocardial cells was
still visible. The sham operation group showed a small amount of
fibrous tissue hyperplasia. Necrotic myocardial cells were rarely
observed, and the texture of the myocardial cells was still evident
(Fig. 3).
Comparison of the myocardial fibrosis
area of the rats in each group after medication
The proportion of fibrosis in each group was
significantly different (P<0.05), and the myocardial fibrosis
area in the medication group was significantly lower than that in
the non-medication group (P<0.05) at 4 weeks after myocardial
infarction in rats (Fig. 4 and
Table IV).
 | Table IV.The area of infarction and fibrosis 4
weeks later (mean ± SD). |
Table IV.
The area of infarction and fibrosis 4
weeks later (mean ± SD).
| Groups | Proportion of
myocardial infarction size | Proportion of
cardiac fibrosis area |
|---|
| Control | 0±0 | 0.01±0.004 |
| Sham operation | 0.11±0.05 | 0.06±0.007 |
| Non-medication |
0.32±0.05a |
0.20±0.019a |
| Medication |
0.22±0.09b |
0.11±0.016b |
Effect of atorvastatin on reducing the
myocardial infarction size
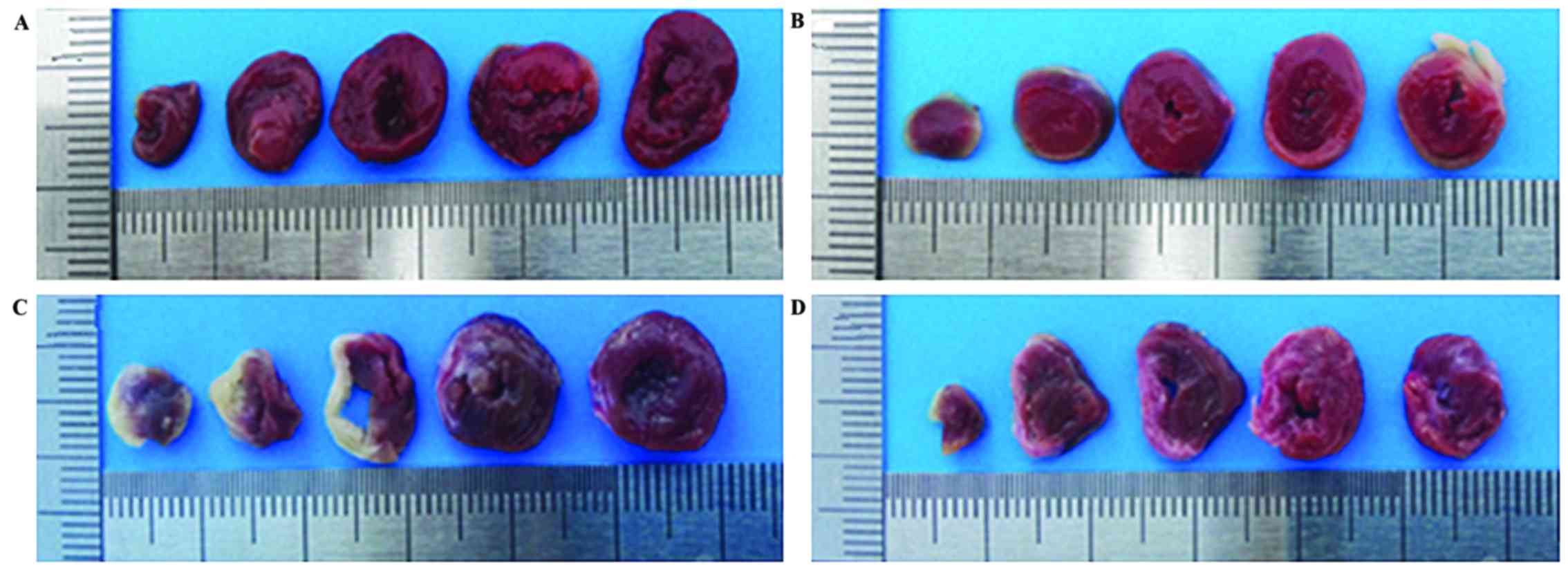
The proportion of fibrosis in each group was
significantly different (P<0.05), and the myocardial infarction
size of the rats in the medication group was significantly lower
than that of the rats in the non-medication group (P<0.05) after
the 4-week experiment (Fig. 5 and
Table IV).
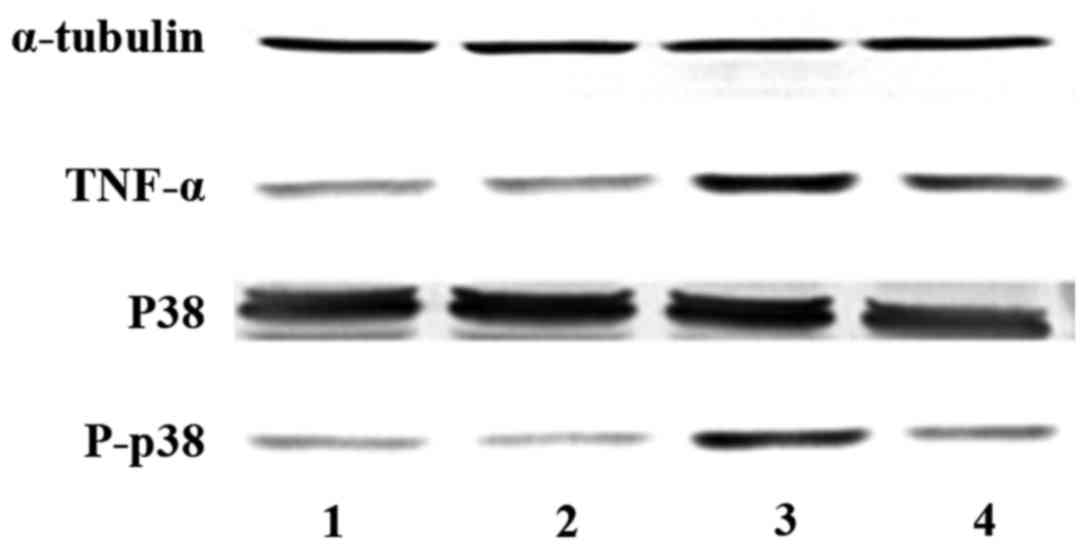
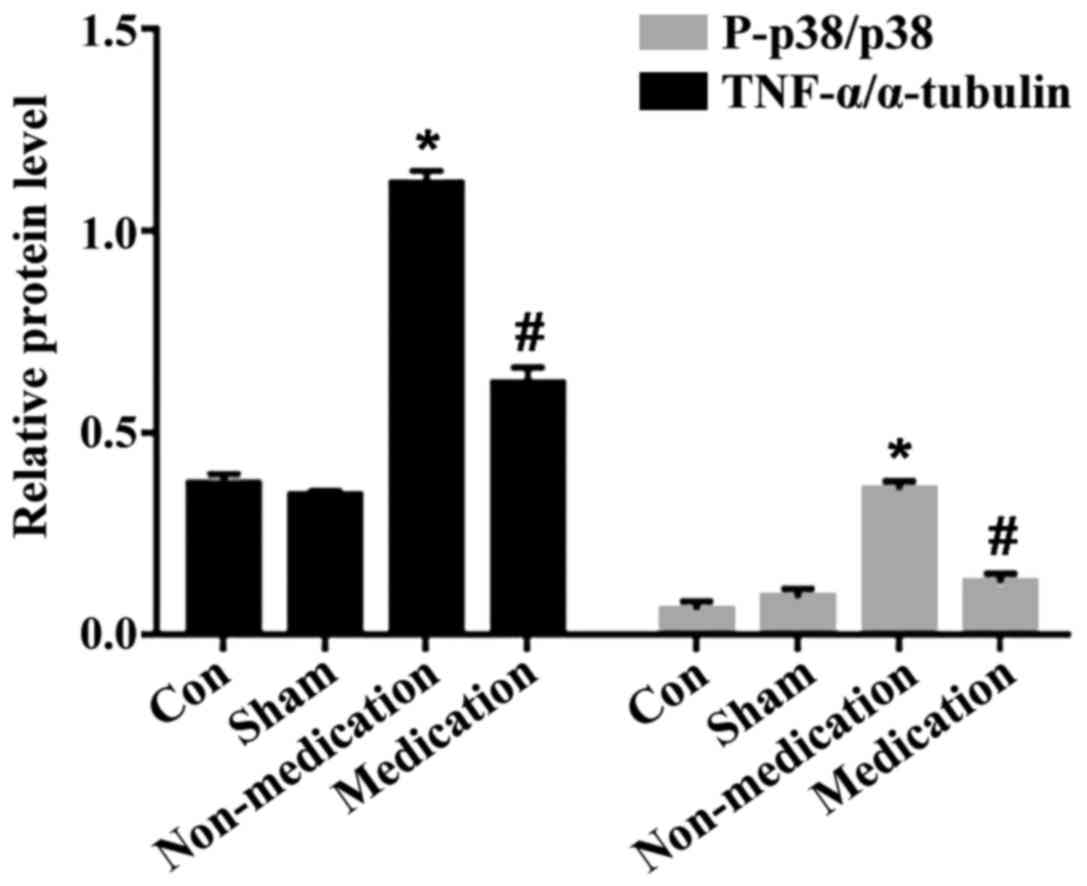
Protein expression in each group
The cardiac protein expression of the rats in each
group was significantly different 4 weeks after successful
modeling. Phosphorylated p38 and TNF-α in the non-medication group
were obviously increased compared to those in the control group
(P<0.05), while they were obviously reduced in the medication
group compared with those in the non-medication group (P<0.05)
(Figs. 6 and 7).
Discussion
Myocardial infarction is the necrosis of myocardial
cells in the heart caused by ischemia and hypoxia (13). An inflammatory reaction is caused by
the accumulation of various inflammatory cells after infarction.
The accumulation of inflammatory cells and release of inflammatory
cytokines lead to post-infarction cardiac remodeling (2). The expansion of the central cavity,
decrease of cardiac function, apoptosis of the myocardial cells and
proliferation of fibrous tissues are observed during cardiac
remodeling (14). Early remodeling
changes the adaptation of the heart. Long-term staying in this
state leads to increased cardiac load, decreased cardiac function
and heart failure (15). Therefore,
the study of the treatment method for cardiac modeling after
myocardial infarction is of great importance.
Atorvastatin has the function of regulating lipids.
Some scholars believe that atorvastatin can resist inflammation,
oxidation and arrhythmia, and improve cardiac remodeling. The
long-term administration of atorvastatin can improve patient
prognosis and reduce the incidence of adverse events (7,16).
However, the exact mechanism is unknown. In the present study, the
left ventricular cardiac function, myocardial fibrosis,
morphological changes of the myocardial cells and expression of
phosphorylated p38 and TNF-α in the rats were detected at 4 weeks
after myocardial infarction in order to study the possible
mechanism of atorvastatin in improving cardiac remodeling. The
results of the experiment showed that the 4-week continuous
administration of atorvastatin could improve the left ventricular
function of the rats. LVEF and SF were increased compared with
those in the non-medication group (P<0.05 for both items), while
LVESD and LVEDD were decreased compared with those in the
non-medication group (P<0.05 for both items). The myocardial
infarction size and fibrosis area in the medication group were
significantly reduced compared with those in the non-medication
group (P<0.05 for both items). The morphological structure of
the myocardial cells was more complete. Necrotic cells were
decreased, and the outline of the myocardial cells was clearly
visible. The contents of phosphorylated p38 and TNF-α in the left
ventricle were significantly decreased (P<0.05 for both items).
It indicated that atorvastatin can improve cardiac remodeling after
myocardial infarction in rats. Therefore, its action of mechanism
may be related to its inhibition of p38 phosphorylation and its
decrease of TNF-α expression.
p38 includes 4 subtypes, namely p38α, p38β, p38γ and
p38δ (17). p38β, p38γ and p38δ are
expressed in the brain, skeletal muscle and pancreas, respectively
(17). However, p38α is expressed in
any tissue. Its molecular weight is 38 kDa. Endogenous response can
be caused by tyrosine site phosphorylation (18). Heat shock protein (HSP) 27 is a
target of action at the downstream of p38α. Upon oxidative stress,
the activation of HSP27 can convert the actin into a fibrous
tissue, in which the p38/MK2/HSP29 pathway plays an important role
(18). TNF-α is mainly secreted by
macrophages (19), which can cause
inflammatory immune response and induce the secretion of various
cytokines. It also plays an important role in ischemic
cardiomyopathy (20). TNF-α is
expressed in large numbers after myocardial infarction in rats
(21) and acts on the extracellular
matrix (22), leading to myocardial
remodeling due to an increased expression of matrix
metalloproteinases (23). On the one
hand, inflammatory cytokines can activate inducible nitric oxide
synthase and increase its activity. On the other hand, it can
activate renin-angiotensin-aldosterone system to participate in
myocardial remodeling. TNF-α can promote apoptosis (14). The interaction of apoptosis, necrosis
and proliferation of fibrous tissues further aggravates myocardial
remodeling, which further deteriorates cardiac function. Therefore,
reduction of the level of inflammatory cytokines is essential for
improving cardiac remodeling after myocardial infarction.
In summary, the findings have shown that the
function of atorvastatin on improving cardiac remodeling after
myocardial infarction in rats may be associated with its inhibition
of p38 phosphorylation and its reduction of TNF-α expression, which
provides a basis for clarifying the mechanism of atorvastatin in
cardiac remodeling after the treatment of myocardial infarction and
lays a foundation for the discovery of subsequent new therapeutic
targets.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ML was responsible for the implementation of the
project, the establishment of animal models, the test of indexes,
and the wrote the study. FL, the chief executive of the project,
provided ideas of selecting topics, conducted experiments and
statistical methods and revised the paper. MS collected the data,
modificated the pictures and statistical analysis. XS was
responsible for the whole experimental methodology. LL was
responsible for the production of animal models, animal husbandry
and gavage. XW collected and stored the animal specimens. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Xiangyang No.1 People's Hospital (Xiangyang, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen J, Cao W, Asare PF, Lv M, Zhu Y, Li
L, Wei J, Gao H, Zhang H, et al: Amelioration of cardiac
dysfunction and ventricular remodeling after myocardial infarction
by danhong injection are critically contributed by
anti-TGF-β-mediated fibrosis and angiogenesis mechanisms. J
Ethnopharmacol. 194:559–570. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kumagai S, Nakayama H, Fujimoto M, Honda
H, Serada S, Ishibashi-Ueda H, Kasai A, Obana M1, Sakata Y, et al:
Myeloid cell-derived LRG attenuates adverse cardiac remodelling
after myocardial infarction. Cardiovasc Res. 109:272–282. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Velasquez LS, Sutherland LB, Liu Z,
Grinnell F, Kamm KE, Schneider JW, Olson EN and Small EM:
Activation of MRTF-A-dependent gene expression with a small
molecule promotes myofibroblast differentiation and wound healing.
Proc Natl Acad Sci U S A. 110:16850–16855. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sobirin MA, Kinugawa S, Akahashi M,
Fukushima A, Homma T, Ono T, Hirabayashi K, Suga T, Azalia P, et
al: Activation of natural killer T cells ameliorates postinfarct
cardiac remodeling and failure in mice. Circ Res: Aug 10, 2012
(Epub ahead of print). https://doi.org/10.1161/CIRCRESAHA.112.270132
|
|
5
|
Qi HP, Wang Y, Zhang QH, Guo J, Li L, Cao
YG, Li SZ, Li XL, Shi MM, et al: Activation of peroxisome
proliferator-activated receptor γ (PPARγ) through NF-κB/Brg1 and
TGF-β1 pathways attenuates cardiac remodeling in
pressure-overloaded rat hearts. Cell Physiol Biochem. 35:899–912.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Berwanger O, de Barros E, Silva PG,
Barbosa RR, Precoma DB, Figueiredo EL, Hajjar LA, Kruel CD, Alboim
C, Almeida AP, Dracoulakis MD, et al: Atorvastatin for high-risk
statin-naïvepatients undergoing noncardiac surgery: The lowering
the risk of operative complications using atorvastatin loading dose
(LOAD) randomized trial. Am Heart J. 184:88–96. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Reichert K, Pereira do Carmo HR, Galluce
Torina A, Diógenes de Carvalho D, Carvalho Sposito A, de Souza
Vilarinho KA, da Mota Silveira-Filho L, Martins de Oliveira PP and
Petrucci O: Atorvastatin improves ventricular remodeling after
myocardial infarction by interfering with collagen metabolism. PLoS
One. 11:e01668452016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Puhl SL, Müller A, Wagner M, Devaux Y,
Böhm M, Wagner DR and Maack C: Exercise attenuates inflammation and
limits scar thinning after myocardial infarction in mice. Am J
Physiol Heart and Circ Physiol. 309:345–359. 2015.https://doi.org/10.1152/ajpheart.00683.2014
View Article : Google Scholar
|
|
9
|
Song XJ, Yang CY, Liu B, Wei Q, Korkor MT,
Liu JY and Yang P: Atorvastatin inhibits myocardial cell apoptosis
in a rat model with post-myocardial infarction heart failure by
downregulating ER stress response. Int J Med Sci. 8:564–572. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
An Z, Yang G, He YQ, Dong N, Ge LL, Li SM
and Zhang WQ: Atorvastatin reduces myocardial fibrosis in a rat
model with post-myocardial infarction heart failure by increasing
the matrix metalloproteinase-2/tissue matrix metalloproteinase
inhibitor-2 ratio. Chin Med J (Engl). 126:2149–2156.
2013.PubMed/NCBI
|
|
11
|
Tang XL, Sanganalmath SK, Sato H, Bi Q,
Hunt G, Vincent RJ, Peng Y, Shirk G, Dawn B and Bolli R:
Atorvastatin therapy during the peri-infarct period attenuates left
ventricular dysfunction and remodeling after myocardial infarction.
PLoS One. 6:e253202011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Song MA, Dasgupta C and Zhang L: Chronic
losartan treatment up-regulates AT1R and increases the heart
vulnerability to acute onset of ischemia and reperfusion injury in
male rats. PLoS One. 10:e01327122015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Thygesen K, Alpert JS and White HD; Joint
ESC/ACCF/AHA/WHFTask Force for the redefinition of myocardial
infarction: Universal definition of myocardial infarction. J Am
Coll Cardiol. 50:2173–2195. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fan Z, Fu M, Xu Z, Zhang B, Li Z, Li H,
Zhou X, Liu X, Duan Y, Lin PH, et al: Sustained release of a
peptide-based MatrixMetalloproteinase-2 inhibitor to attenuate
adverse cardiac remodeling and improve cardiac function following
myocardial infarction. Biomacromolecules. 18:2820–2829. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Heeger CH, Jaquet K, Thiele H, Zulkarnaen
Y, Cuneo A, Haller D, Kivelitz D, Schmidt T, Krause K, Metzner A,
et al: Percutaneous, transendocardial injection of bone
marrow-derived mononuclear cells in heart failure patients
following acute ST-elevation myocardial infarction: ALSTER-Stem
Cell trial. EuroIntervention. 8:732–742. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ma H, Liu Y, Xie H, Zhang G, Zhan H, Liu
Z, Wang P, Geng Q and Guo L: The renoprotective effects of
simvastatin and atorvastatin in patients with acute coronary
syndrome undergoing percutaneous coronary intervention: An
observational study. Medicine. 96:e73512017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Remy G, Risco AM, Iñesta-Vaquera FA,
González-Terán B, Sabio G, Davis RJ and Cuenda A: Differential
activation of p38MAPK isoforms by MKK6 and MKK3. Cell Signal.
22:660–667. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Corre I, Paris F and Huot J: The p38
pathway, a major pleiotropic cascade that transduces stress and
metastatic signals in endothelial cells. Oncotarget. 8:55684–55714.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Udalova I, Monaco C, Nanchahal J and
Feldmann M: Anti-TNF therapy. Microbiol Spectr. 4:2016.doi:
10.1128/microbiolspec. MCHD-0022-2015. PubMed/NCBI
|
|
20
|
Zhang P, Wu X, Li G, He Q, Dai H, Ai C and
Shi J: Tumor necrosis factor-alpha gene polymorphisms and
susceptibility to ischemic heart disease: A systematic review and
meta-analysis. Medicine (Baltimore). 96:e65692017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen H, Xu Y, Wang J, Zhao W and Ruan H:
Baicalin ameliorates isoproterenol-induced acute myocardial
infarction through iNOS, inflammation and oxidative stress in rat.
Int J Clin Exp Pathol. 8:10139–10147. 2015.PubMed/NCBI
|
|
22
|
Chen WL, Sheu JR, Chen RJ, Hsiao SH, Hsiao
CJ, Chou YC, Chung CL and Hsiao G: Mycobacterium tuberculosis
upregulates TNF-α expression via TLR2/ERK signaling and induces
MMP-1 and MMP-9 production in human pleural mesothelial cells. PLoS
One. 10:e01379792015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sato F, Kohsaka A, Takahashi K, Otao S,
Kitada Y, Iwasaki Y and Muragaki Y: Smad3 and Bmal1 regulate p21
and S100A4 expression in myocardial stromal fibroblasts via TNF-α.
Histochem Cell Biol. 148:617–624. 2017. View Article : Google Scholar : PubMed/NCBI
|