Introduction
The diagnosis of unidentified pleural effusions is
one of the most difficult and complicated tasks in respiratory
medicine (1). Prior to the
application of thoracoscopy, hydrothorax exfoliative cytologic
examination and closed pleural biopsy were the two methods
typically used; however, these methods have a low positive
diagnostic rate (2). The clinical
application of thoracoscopy thus provides a novel diagnostic method
for undiagnosed pleural effusions. Compared to conventional closed
pleural biopsy, the thoracoscopy has notable advantages. It
overcomes the blindness of closed pleural biopsy and markedly
improves diagnostic accuracy of pleural effusions, and therefore
improves the positive diagnostic rate of pleural diseases (3–5). It has
been reported that the overall positive diagnostic rate with
thoracoscopy may reach 71–100% (6–8). For
example, a retrospective study by Hansen et al (9) investigated the diagnostic value of
thoracoscopy in 146 patients with pleural effusions, and the
positive diagnostic rate reached 90.4%. Among these patients, 136
had negative results through three cytological and microbiological
examinations (9).
The present retrospective study included 86 patients
with pleural effusions who received medical thoracoscopy
examination at Shaanxi Provincial People's Hospital (Xi'an, China).
A diagnosis rate of 91.9% was identified and it was demonstrated
that malignant tumors were the most common cause of pleural
effusion in the 36–65 and 65 years and above age groups, while
tuberculous pleuritis was the most common cause in the
16–35-year-old age group. Sex and smoking-history had little impact
on diagnosis distribution.
Patients and methods
Patients
A retrospective study was conducted on clinical data
of 86 patients (50 males and 36 females; age range, 17–84 years;
mean, 58±15 years) with pleural effusions who received medical
thoracoscopy in the Endoscopy Center of Shaanxi Provincial People's
Hospital between May 2012 to November 2013. The indication of
medical thoracoscopy was undiagnosed pleural effusion, which
referred to the situation that the cause of disease could not be
identified through routine examination of pleural fluid,
biochemical tests, bacteriology, exfoliative cytology as well as
closed pleural biopsy examination. No contraindication had been
demonstrated for any patients receiving medical thoracoscopy. The
procedure was approved by the Ethics Committee of Shaanxi
Provincial People's Hospital. All patients and family members were
informed of the surgical procedure and signed an informed consent
form prior to the procedure.
Medical thoracoscopy procedure
A bent-type electronic thoracoscope (Olympus BF-240)
with EVIS-260 light-source and video camera system (Olympus
Corporation, Tokyo, Japan) was used for the thoracoscopy procedure.
Routine blood tests, bleeding and clotting time tests, and
electrocardiograms were performed prior to examination. Artificial
pneumothorax on the affected side was set up prior to surgery. The
whole procedure was conducted in the endoscope room. Heart rate,
breathing frequency, blood pressure, oxygen saturation and
consciousness were closely monitored. Each patient was placed in a
lateral decubitus position with the affected side up. The
thoracoscope was inserted into the pleural cavity at the midpoint
between the 6 and 7th ribs along the midaxillary line or axillary
line, through a 1–2-cm cut under local anesthesia. If there was no
pleural adhesion observed, the trocar was inserted vertically and
put into the thoracoscope. The pleural effusion was examined and
drawn out as much as possible to obtain satisfactory exposure. The
changes of parietal and visceral pleura were examined carefully. If
abnormal pleural nodules, pleural congestion, thickening, adhesion
and ulcers were observed under the thoracoscope, 5–10 pieces of
tissue were collected under direct vision via a protractor.
Following surgery, all fluid and air inside the pleural cavity were
drawn out as much as possible and the closed drainage trocars was
left inside. Diagnosis of tumor, tuberculosis or other pleural
lesions was performed according to histological and cytological
changes, as previously described in the British thoracic society
guidelines (10). Histological
analysis was performed following standard protocol. In brief,
tissue samples were fixed in 10% neutral buffered formalin
overnight at room temperature and subsequently embedded in paraffin
blocks. Sections were cut to 6-µm thick and stained with a
commercial hematoxylin and eosin staining kit (haematoxylin for 4
min and eosin for 2 min, at room temperature). Slides were examined
under standard bright-field microscope with a ×10 or ×20 object
lens.
Results
Medical thoracoscopy examination
delivers a high diagnosis rate
Among the 86 patients with undiagnosed pleural
effusions, 50 were males and 36 were females. Their age range was
17–84 years with an average of 58±15 years. Among them, 2 patients
had pleural effusion with a little peritoneal effusion, and 6
patients had pleural effusion with a small amount of pericardial
effusion. Clinical features of these patients were summarized in
Table I. The thoracoscopy
examination took 15–120 min with an average of 35 min. In 86
patients receiving thoracoscopy, 79 were given clear diagnosis and
5 remained undiagnosed. Examination failed only in 2 patients: 1
patient had their diaphragm muscle obviously moved up and the
thoracoscope went into peritoneal cavity by mistake due to pleural
adhesions; the other patient had serious pleural thickening and
adhesion making it difficult for the thoracoscope to enter the
pleural cavity for observation. Altogether, the positive diagnosis
rate was 91.9% (79/86).
 | Table I.Patient features of the study group
(n=86). |
Table I.
Patient features of the study group
(n=86).
| Clinical
features | Average value or
number of cases |
|---|
| Age, years | 58.0±15.0
(17–84)a |
| Sex
(male/female) | 50/36 |
| Position of pleural
effusion (left/right/both sides) | 36/40/10 |
|
Smoker/non-smoker | 48/38 |
Among the 86 patients receiving thoracoscopy, the
largest group of patients were diagnosed with pleura cancer
metastasis (37/86; 43.0%), the second largest group of patients
were diagnosed with tuberculous pleuritis (20/86; 23.3%), while
third largest group of patients was diagnosed with non-specific
pleuritis (13/86; 15.1%). The detailed results of the pathological
examination were demonstrated in Table
II. Among the 13 patients with non-specific pleuritis, 6 were
considered as tuberculous pleuritis and given tentative
anti-tuberculosis treatment following pleural effusion absorption.
In 1 suspicious patient, it was confirmed that they did not have
pleural mesothelioma at the 6-month follow-up visit for pleural
effusion absorption. Furthermore, 1 patient with a liver abscess,
pneumonia and pleural effusion, was considered as parapneumonic
effusion and given anti-infective treatment following effusion
absorption. Among the 5 patients whose diseases were not clearly
diagnosed, 1 was diagnosed later on with poorly differentiated
adenocarcinoma from bilateral ovaries; 1 was diagnosed with
immature teratoma through an exploratory laparotomy; 1 was
diagnosed with malignant schwannoma through a thoracotomy and
pathological analysis; the remaining 2 patients remained
undiagnosed (data not shown).
 | Table II.Results of pleura pathological
examination for 86 patients with pleural effusions. |
Table II.
Results of pleura pathological
examination for 86 patients with pleural effusions.
| Pathological
results | n (%) |
|---|
| Pleura cancer
metastasis | 37 (43.0) |
| Lung
adenocarcinoma metastasis | 26 (30.2) |
| Lung
squamous cell cancer metastasis | 6 (6.9) |
| Breast
cancer metastasis | 1 (1.1) |
|
Alimentary canal tumor
metastasis | 2 (2.3) |
| Malignant
tumor source unidentified | 2 (2.3) |
| Pleural
mesothelioma | 3 (3.5) |
| Tuberculous
pleuritis | 20 (23.3) |
| Non-specific
pleuritis | 13 (15.1) |
| Parapneumonic
effusion | 4 (4.7) |
| Secondary fetal
hydrothorax after pneumothorax | 1 (1.1) |
| Secondary fetal
hydrothorax of chronic cholecystitis | 1 (1.1) |
| Undiagnosed by
pathology | 5 (5.8) |
| Failed
examination | 2 (2.3) |
Different causes of pleural effusion
present different manifestations under the thoracoscope
A thorough understanding of these manifestations
will substantially improve the positive diagnostic rate of biopsy.
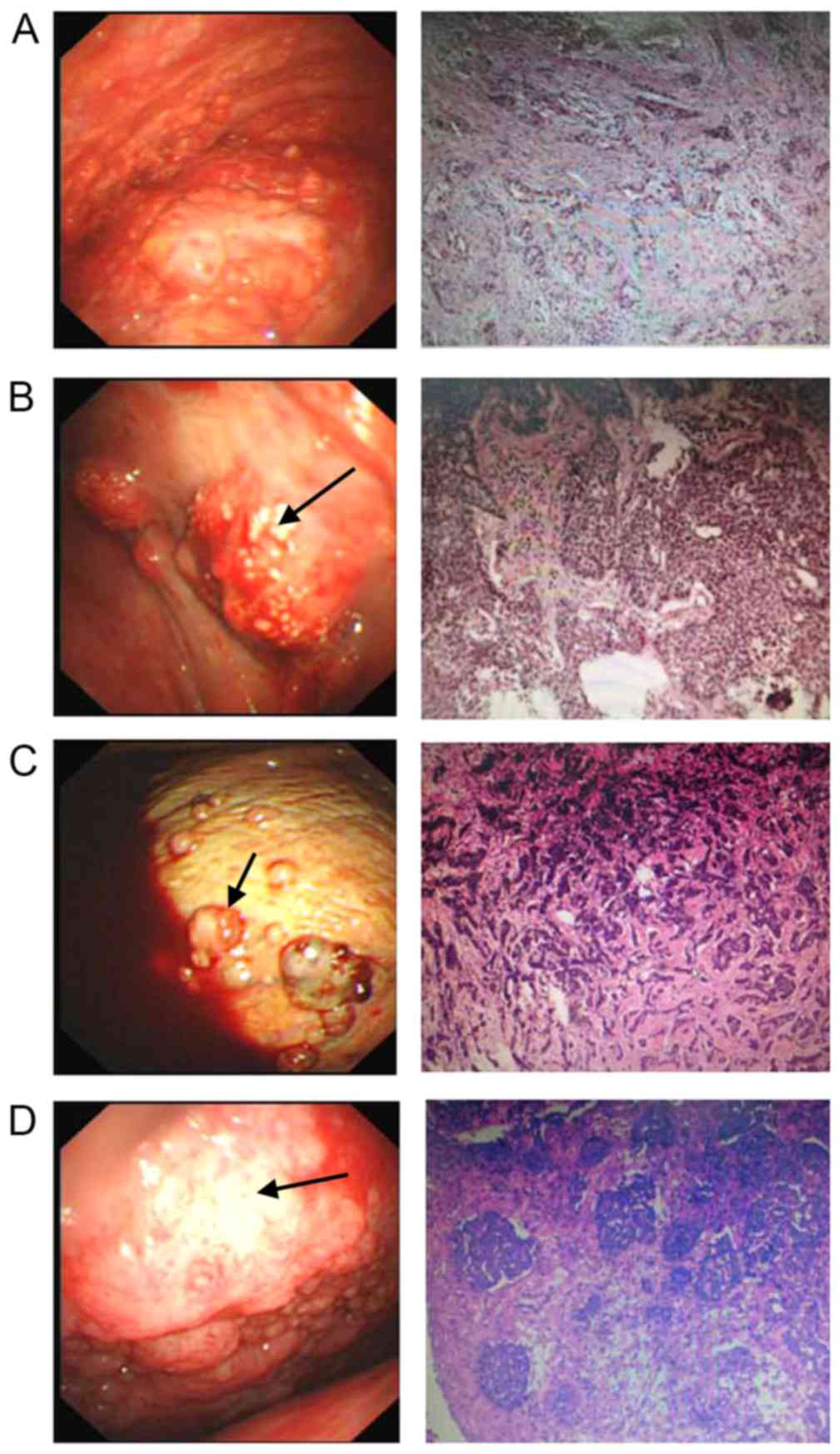
Malignant tumor metastasis pleural effusions (Fig. 1) were predominantly bloody pleural
fluid, and there were numerous grey-white nodules or lumps with
different sizes on parietal and visceral pleura, which had a
well-defined boundary and friable nature and were relatively easy
to biopsy. Additionally, the nodules or lumps were prone to bleed
following biopsy (Fig. 1A-C). For
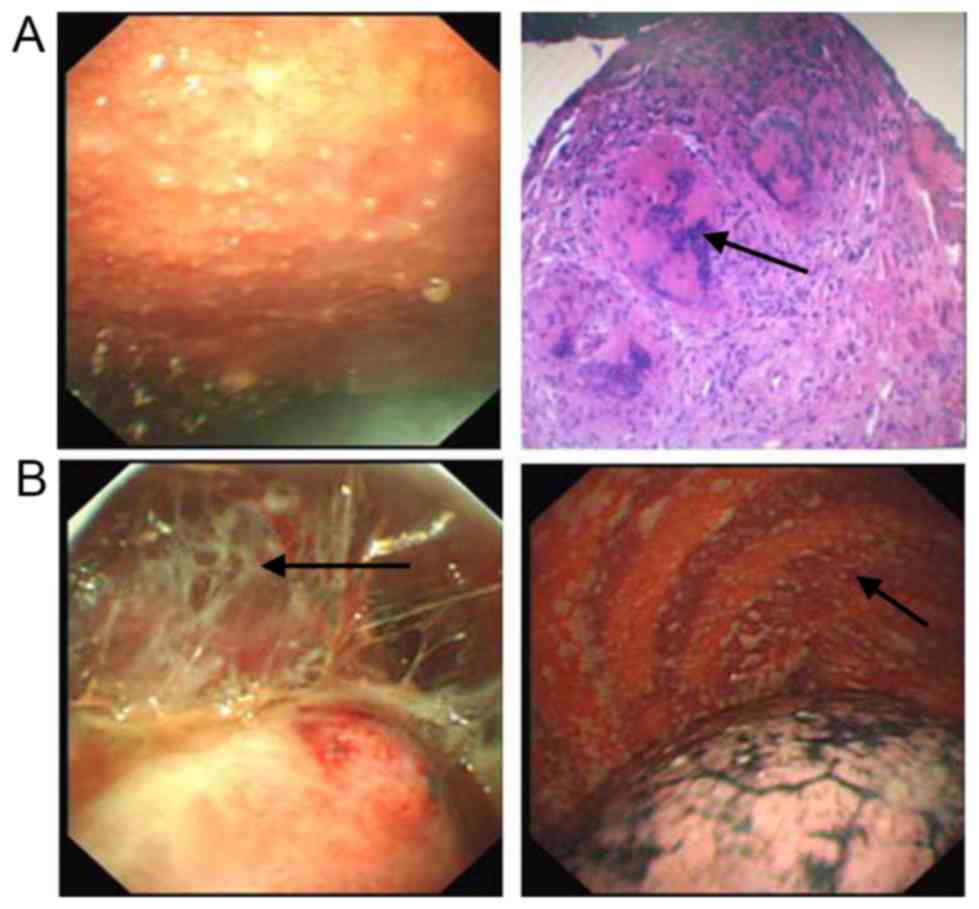
tuberculous pleuritis, the pleura was observed with obvious
congestion and edema, and hatpin-sized grey-white or light-yellow
nodules were often seen scattering or gathering on the pleura,
accompanied with a lot of fibrin and cord-like adhesions (Fig. 2). The pleural mesothelioma was
manifested by numerous lumpy or flat lesions on the parietal
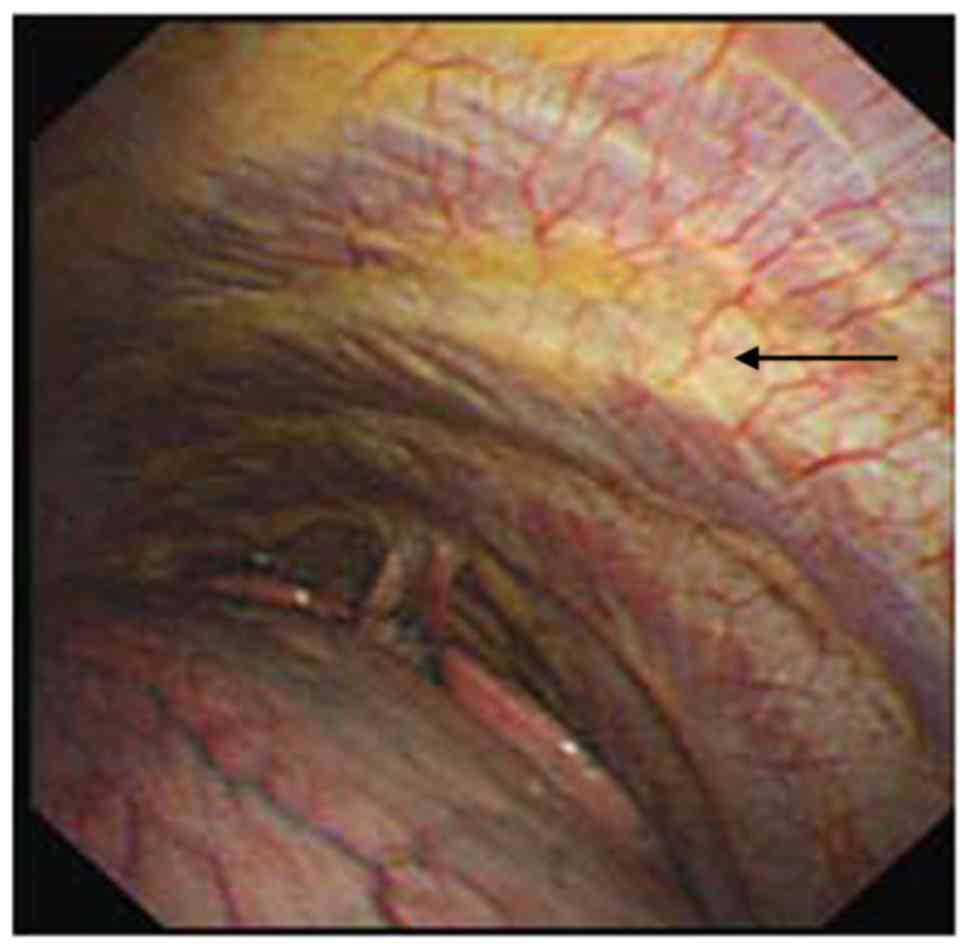
pleura, and they did not tend to bleed following biopsy (Fig. 1D). The non-specific pleuritis was
manifested with diffusive or limited congestion, edema and
thickening on parietal pleura (Fig.
3). Overall, we recommend selecting fragile and rubbery tissue
lesions for biopsy, and testing as many lesions as possible to
avoid incorrect diagnosis.
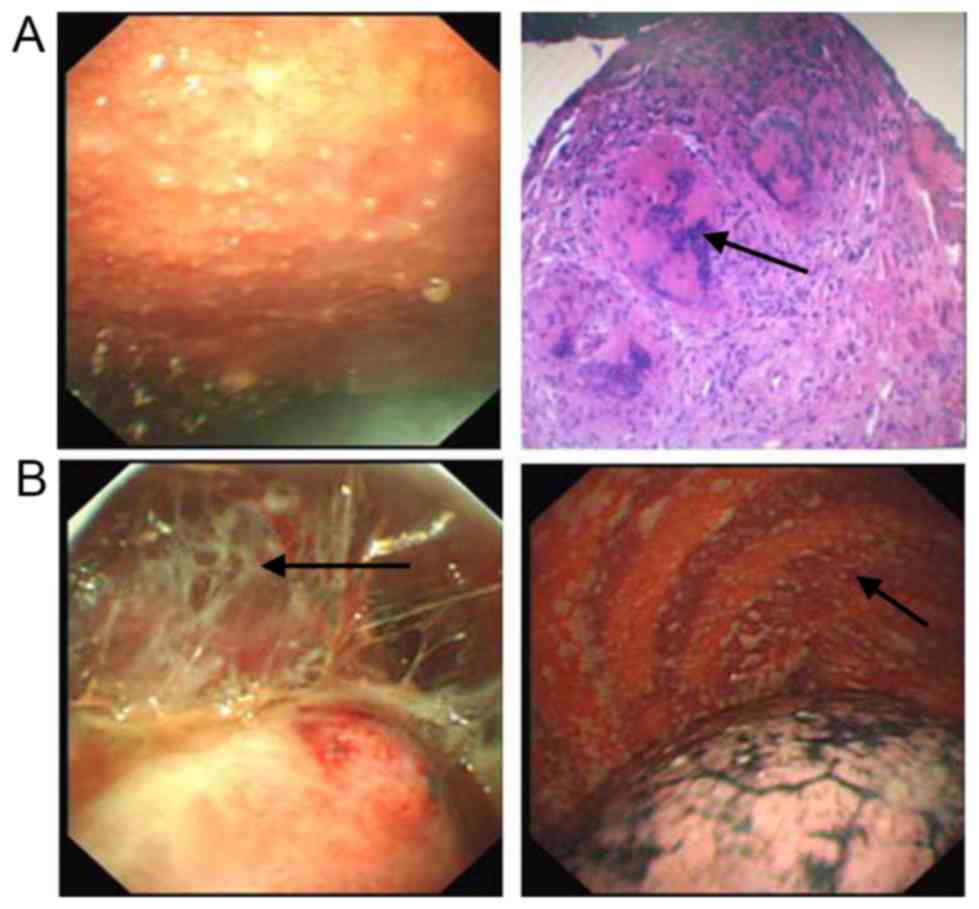 | Figure 2.Patients with pleural effusion
diagnosed with tuberculous pleuritis. (A) Acute stage. Images are
thoracoscopy view (500K CCD, Olympus, left penal) and pathological
section view (hematoxylin and eosin staining; magnification, ×50,
right panel). (B) Chronic stage (500K CCD, Olympus, both panels).
Tuberculous pleuritis was often diagnosed based on diffuse
congestion and thickening of the pleural wall or diaphragmatic
pleura, with miliary and popular nodules. At the chronic stage,
fibrous adhesions (B, black arrow) were often observed while
caseating sphacelus (A, black arrow) was occasionally seen. |
Diagnosis distribution of pleural
effusions is linked to age but not sex or smoking-history
The undiagnosed pleural effusions had different
clinical causes at different ages (Table III). In the present study,
tuberculosis was often observed in 16–35-year-old patients (13/23;
56.5%), while malignant tumors became the major cause in
36–65-year-old patients (24/35; 68.6%) and patients who were 65
years old and above (8/12; 66.7%). Among the malignant tumors, lung
cancer with pleural metastasis was the most common type (32/37;
86.5%), and the majority of these patients had metastatic lung
adenocarcinoma (data not shown).
 | Table III.Diagnosis distribution of patients
with pleural effusions to three major categories (age, sex and
smoking history). |
Table III.
Diagnosis distribution of patients
with pleural effusions to three major categories (age, sex and
smoking history).
|
| Diagnosis |
|---|
|
|
|
|---|
| Group | Malignant tumor, n
(%) | Tuberculosis, n
(%) | Non-specific
pleuritis, n (%) | Total (%) |
|---|
| Age, years |
|
|
|
|
|
16–35 | 5 (21.7) | 13 (56.5) | 5 (21.7) | 23 (100.0) |
|
36–65 | 24 (68.6) | 5 (14.3) | 6 (17.1) | 35 (100.0) |
| 65 and
above | 8 (66.7) | 2 (16.7) | 2 (16.7) | 12 (100.0) |
| Smoking history |
|
|
|
|
|
Smoker | 23 (56.1) | 12 (29.3) | 6 (14.6) | 41 (100.0) |
|
Non-smoker | 14 (48.3) | 8 (27.6) | 7 (24.1) | 29 (100.0) |
| Sex |
|
|
|
|
| Male | 26 (61.9) | 11 (26.2) | 5 (11.9) | 42 (100.0) |
|
Female | 11 (39.3) | 9 (32.1) | 8 (28.6) | 28 (100.0) |
| Total (%) | 37 (52.9) | 20 (28.6) | 13 (18.6) | 70 (100.0) |
Notably, smoking history and sex had no notable
impact on the distribution of diagnosis. It is well known that lung
cancer is closely related to cigarette smoking (11); however, the diagnosis of malignant
tumors was only slightly higher in smokers than non-smokers (56.1
vs. 48.3%, respectively). This may be due to the fact that
secondhand smoke has been a severe social problem in China in past
years (12). Similarly, the
diagnosis of malignant tumors was also slightly higher in males
than females (61.9 vs. 39.3%, respectively), given that the
population of male smokers is much higher than female smokers in
China (13). However, a larger
sample size is required to reach a conclusion with statistical
significance.
Potential complications of
thoracoscopy examination
The most common complication following thoracoscopy
examination was chest pain (47/86; 54.7%). Other complications
included subcutaneous emphysema (16 cases accounting for 18.6%),
pleural hemorrhage (8 cases accounting for 9.3%), low-grade fever
(5 cases accounting for 5.8%), light nausea (4 cases accounting for
4.7%) and re-expansion pulmonary edema (1 case accounting for
1.2%). All symptoms disappeared within 1–3 days, and no mortality
occurred (data not shown).
Although medical thoracoscopy is considered as a
minimally invasive procedure, it is still possible to cause
intraoperative hemorrhage, re-expansion pulmonary edema, secondary
infection, chest pain, fever and other complications. Among the 84
patients receiving the thoracoscopy procedure in our facility, only
1 developed re-expansion pulmonary edema following surgery, and
this was relieved quickly under standard care. Aside from that, the
most common complications were chest pain, often found following
pleural atresia surgery, as well as fever (mostly low-grade fever),
which disappeared within 1–3 days without any special treatment
(9).
Discussion
Pleural effusion is a clinical feature of various
diseases, and currently, it is sometimes difficult to diagnose the
causes of clinical pleural effusions (1). There are 20–25% of cases whose causes
cannot be determined with the existing routine methods (10). The medical thoracoscopy developed in
recent years is an invasive surgical technique that may be
accomplished independently by a pulmonary physician under local
anesthesia. Research has demonstrated that medical thoracoscopy is
able to markedly increase the positive diagnostic rate of
undiagnosed pleural effusions (3).
The present retrospective study included the clinical data of 86
patients with undiagnosed pleural effusions who had received
medical thoracoscopy, in order to investigate the diagnostic value
of medical thoracoscopy in diagnosis of undiagnosed pleural
effusions. The diagnosis rate of thoracoscopy in the present study
reached as high as 91.9%, which is comparable with what has been
reported in previous studies (6–8).
Malignant tumors represent the top cause of clinical
pleural effusions in general, and lung adenocarcinoma is frequently
observed in these patients (14).
However, there is regional discrepancy regarding the primary
non-malignant cause, particularly in terms of tuberculous pleuritis
(15). Tuberculosis is the third
most common cause of pleural effusions in Spain, while it is not a
major cause in the United States (16). In the present study, tuberculosis was
diagnosed in 23.3% of the patients following thoracoscopy. The
early diagnosis made it possible for us to apply pleural drainage
at the acute stage of tuberculous pleuritis, which effectively
prevented chronic changes and reduced the length of
hospitalization. At the chronic stage, such as separated and
encircled pleura, we used biopsy forceps to remove the adhesive
band, sphacelus, as well as encapsulated effusion resulting from
earlier clamping, thus improving the therapeutic effect.
In the present study, malignant tumors and
tuberculous pleuritis accounted for 43.0 and 23.3% of the causes of
undiagnosed pleural effusions, respectively. These are also the two
most common causes of pleural effusions in China (10). The third cause was non-specific
pleuritis, which accounted for 15.1% of cases and, in these
patients, tuberculous pleuritis was frequently found at the
6–18-month follow-ups. A study by Venekamp et al (17) also reported that, from 75 patients
who were diagnosed with non-specific pleuritis under thoracoscopy
in 2005, 91.77% had a benign process and only 8.3% evolved into
tumor according to a 3-year follow-up study. Thus, when a patient
is diagnosed with non-specific inflammation under thoracoscopy, the
clinician should still conduct dynamic observation and whole-body
screening to determine the cause.
Pleural mesothelioma is a rare tumor that originates
from pleural mesothelium tissue or sub-pleural interstitial tissue
(18). The positive diagnostic rate
is usually low by a pleural effusion cytologic examination, and it
has been reported to be only 0–22% (19). This is likely due to the fact that
there are very few mesothelial cells falling off in pleural
effusion and sometimes it is difficult to conduct a qualitative
analysis with a single cell; or it is because the cell has been
kept in pleural effusion for a long time and has lost its features
due to degeneration, therefore it is not easily distinguished from
normal mesothelial cells (18). The
closed pleural biopsy has a positive diagnostic rate of 60% because
the lesion of pleura is not evenly distributed (18). With thoracoscopy, it is possible to
examine the whole pleural cavity to discover early lesions and
conduct biopsy under visual inspection, therefore the positive
diagnostic rate of pleural mesothelioma may reach 91–100% (20). Thus, it is necessary to conduct
thoracoscopy as early as possible for patients with undiagnosed
pleural effusions.
In conclusion, medical thoracoscopy is a useful tool
for diagnosing pleural effusions with unidentified causes, and it
markedly improves the positive diagnostic rate of pleural
effusions. This procedure has the advantages of visual inspection,
easy procedure, high safety and few complications, and has an
important application value for the diagnosis of pleural effusions
with unidentified causes, particularly for pleural metastatic
tumors, tuberculous pleuritis and pleural mesothelioma.
References
|
1
|
McGrath EE and Anderson PB: Diagnosis of
pleural effusion: A systematic approach. Am J Crit Care.
20:119–128. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Prakash UB and Reiman HM: Comparison of
needle biopsy with cytologic analysis for the evaluation of pleural
effusion: Analysis of 414 cases. Mayo Clin Proc. 60:158–164. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kendall SW, Bryan AJ, Large SR and Wells
FC: Pleural effusions: Is thoracoscopy a reliable investigation? A
retrospective review. Respir Med. 86:437–440. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rodriguez-Panadero F, Janssen JP and
Astoul P: Thoracoscopy: General overview and place in the diagnosis
and management of pleural effusion. Eur Respir J. 28:409–422. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tassi GF and Tschopp JM: The centenary of
medical thoracoscopy. Eur Respir J. 36:1229–1231. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sakuraba M, Masuda K, Hebisawa A, Sagara Y
and Komatsu H: Diagnostic value of thoracoscopic pleural biopsy for
pleurisy under local anaesthesia. ANZ J Surg. 76:722–724. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Blanc FX, Atassi K, Bignon J and Housset
B: Diagnostic value of medical thoracoscopy in pleural disease: A
6-year retrospective study. Chest. 121:1677–1683. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee P, Hsu A, Lo C and Colt HG:
Prospective evaluation of flex-rigid pleuroscopy for indeterminate
pleural effusion: Accuracy, safety and outcome. Respirology.
12:881–886. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hansen M, Faurschou P and Clementsen P:
Medical thoracoscopy, results and complications in 146 patients: A
retrospective study. Respir Med. 92:228–232. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maskell NA and Butland RJ; Pleural
Diseases Group, Standards of Care Committee, British Thoracic
Society, : BTS guidelines for the investigation of a unilateral
pleural effusion in adults. Thorax. 58 Suppl 2:ii8–i17. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murray JF and Mason RJ: Murray and Nadel's
textbook of respiratory medicine. Saunders/Elsevier; Philadelphia,
PA: 2010, View Article : Google Scholar
|
|
12
|
Taylor R, Najafi F and Dobson A:
Meta-analysis of studies of passive smoking and lung cancer:
Effects of study type and continent. Int J Epidemiol. 36:1048–1059.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li Q, Hsia J and Yang G: Prevalence of
smoking in China in 2010. N Engl J Med. 364:2469–2470. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boutin C, Viallat JR, Cargnino P and
Farisse P: Thoracoscopy in malignant pleural effusions. Am Rev
Respir Dis. 124:588–592. 1981.PubMed/NCBI
|
|
15
|
Porcel JM and Vives M: Differentiating
tuberculous from malignant pleural effusions: A scoring model. Med
Sci Monit. 9:CR175–CR180. 2003.PubMed/NCBI
|
|
16
|
Baumann MH, Nolan R, Petrini M, Lee YC,
Light RW and Schneider E: Pleural tuberculosis in the United
States: Incidence and drug resistance. Chest. 131:1125–1132. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Venekamp LN, Velkeniers B and Noppen M:
Does ‘idiopathic pleuritis’ exist? Natural history of non-specific
pleuritis diagnosed after thoracoscopy. Respiration. 72:74–78.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Barreiro TJ and Katzman PJ: Malignant
mesothelioma: A case presentation and review. J Am Osteopath Assoc.
106:699–704. 2006.PubMed/NCBI
|
|
19
|
Renshaw AA, Dean BR, Antman KH, Sugarbaker
DJ and Cibas ES: The role of cytologic evaluation of pleural fluid
in the diagnosis of malignant mesothelioma. Chest. 111:106–109.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Boutin C, Rey F, Gouvernet J, Viallat JR,
Astoul P and Ledoray V: Thoracoscopy in pleural malignant
mesothelioma: A prospective study of 188 consecutive patients. Part
1: Diagnosis. Cancer. 72:394–404. 1993. View Article : Google Scholar : PubMed/NCBI
|