Introduction
Colorectal carcinoma (CRC) is currently the third
most prevalent cancer type worldwide. It has a complex etiology
that is influenced by both environmental and genetic factors
(1). Colorectal cancer patients in
the high-risk late stage (stage II or III) are treated with
adjuvant chemotherapy in combination with fluoropyrimidine
monotherapy, which reduces the risk of recurrence and death by
approximately 20–30% compared with fluoropyrimidine monotherapy
(2,3). Addition of oxaliplatin to this
treatment regimen has been reported to improve disease-free
survival in three individual landmark trials (4). Nevertheless, the side effects of this
treatment have limited its application (5). Thus, there is an urgent requirement to
explore novel therapeutic strategies against CRC. In the present
study, an immunological treatment approach against CRC was
investigated.
Immunization-based therapy that utilizes
antigen-presenting cells (APCs) to enhance efficacy is considered
to be a promising approach for the treatment of cancer (6). Dendritic cells (DCs) serve prominent
roles in various immunization therapies by activating cytotoxic
T-lymphocytes (CTLs) (7,8). The key role of DCs in cell-mediated
immunity serves as the basis for the development of effective DC
vaccines for immunization therapies against tumors (9,10). This
approach may induce certain immunological responses in cancer
patients with prostate cancer (11),
lymphoma (12), melanoma, bladder
transitional cancer (13) and
non-small cell lung carcinoma (14).
A sufficient number of functioning DCs that are able to activate
T-cells is important for the efficacy of DC vaccines (15). Specific carrier proteins, cytokines,
immunological adjuvants and transgenic viruses have been
demonstrated to influence the immune response activation by DCs
(16). Previous studies have
reported that non-methylated cytosine-guanine (CpG) motifs may act
as adjuvants for boosting tumor immunity by activating DCs.
Treatment in which CpG motifs are applied may be achieved via
upregulation of Th1 cytokines, soluble growth factors and primary
DC surface markers (17,18).
Antigen 85A (Ag85A) is involved in acid synthesis
(19). Accumulating evidence has
indicated that Ag85A may promote extensive proliferation of Th
cells and the production of Th1 cytokines in mice and
mycobacterium-infected humans (20,21).
Laboratory rats injected with plasmid DNA harboring the Ag85A gene
exhibited increased generation of interleukin (IL)-2 and interferon
(IFN)-γ and increased CTL activity in response to mycobacterium
proteins in the Bacillus Calmette-Guérin vaccine (22,23).
Furthermore, injection with the Ag85A-mixed plasmid DNA vaccine
protected mice from infection by Mycobacterium tuberculosis
and resulted in stronger CTL activities (24). Immunization with DCs engineered with
Mycobacterium Ag85A generated a distinct immune reaction
profile, including CTL activity in response to antigenic
determinants of Ag85A (25).
Melanocytes collected from Ag85A-transfected B16-F10 mice were
identified to inhibit tumorigenic effects and tumor progression
(26). These findings demonstrate
the potential use of Ag85A as an effective auxiliary agent for
enhancing the immune response. However, the antitumor effects of
Ag85A-mixed DCs against colorectal carcinoma remain unclear.
Therefore, the present study examined whether treatment with
Ag85A-transfected DC 2.4 cells could enhance the immunological
response to colorectal cancer.
Materials and methods
Mice and cells
DC 2.4 cells were collected from C57BL/6 mice and
infected with GM-CSF-transfected medullary cells with myc/raf
oncogenes, as previously described (27). CT26 colorectal carcinoma (American
Type Culture Collection, Manassas, VA, USA) and DC 2.4 cell lines
were cultivated in RPMI 1640 (Gibco; Thermo Fisher Scientific,
Inc., Waltham, MA, USA) at 37°C in an incubator under humid
conditions with 50 ml/l CO2. C57BL/6 mice (n=6; male)
aged 6–8 weeks (weight, 18–20 g) were obtained from the Chinese
Academy of Science Shanghai Laboratory Animal Center (Shanghai,
China). Animal experiments in this study were conducted in
accordance with the internationally accepted principles for
laboratory animal use and care. The study was approved by the
Committee on the Ethics of Animal Experiments of China Medical
University (Shenyang, China).
Ag85A plasmid transfection
Cells were transfected with 1 µg Ag85A and pc-DNA3.1
(Shanghai GenePharma Co., Ltd., Shanghai, China) using
Lipofectamine 2000 transfection reagent (Invitrogen; Thermo Fisher
Scientific, Inc.). The pcDNA3.1+/Ag85A plasmid was incubated with
Lipofectamine reagent for 20 min and subsequently added to the RPMI
1640 suspension containing DC 2.4 cells without antibiotics. The
pcDNA3.1 vector without Ag85A served as the negative control. The
Ag85A-DCs and mock-DCs were harvested at 48 h
post-transfection.
Quantification of Ag85A mRNA
expression
Total RNA was extracted from Ag85A-DCs using TRIzol
reagent (Invitrogen; Thermo Fisher Scientific, Inc.). Reverse
transcription (RT) was conducted using a Takara Prime Script RT
reagent kit (Takara Biotechnology Co., Ltd., Dalian, China).
Quantitative polymerase chain reaction (qPCR) was conducted using
the Qiagen Quanti Tect SYBR Green PCR kit (Qiagen GmbH, Hilden,
Germany) on an ABI 7300 Real-Time PCR system (Applied Biosystems;
Thermo Fisher Scientific, Inc.). The thermocycling conditions were
as follows: 3 min at 95°C, followed by 45 cycles of 95°C for 15 sec
and 60°C for 60 sec. GAPDH served as the control for qPCR
amplification. Analysis was performed in triplicate, and
experiments were conducted at least three times. Analysis of
relative gene expression was performed using the 2−∆∆Cq
method (28). The following primers
were used: GAPDH, sense, 5′-CAAAAGGGTCATCATCTCC-3′ and antisense,
5′-CCCCAGCATCAAAGGTG-3′; Ag85A, sense, 5′-CAAAGTGGTGGTGCCAACTC-3′
and antisense, 5′-CTCGCTGGTCAGGAAGGTCT-3′.
Assessment of primary surface
markers
DCs were blocked using 5% bovine serum albumin
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at room temperature
for 1 h and incubated with CD16 and 32 mAb (cat. nos. 2.4G2 and
565,502; 1:1,000; BD Biosciences, Franklin Lakes, NJ, USA) at 4°C
for 15 min. Next, DCs were incubated in saturated
PE-anti-MHC-II/CD80&86 mAb (cat. no. 565157; 1:1,000; BD
Biosciences) at 4°C for 30 min. Cells were examined using a flow
cytometer and were analyzed using FlowJo software 7.6.1 (FlowJo,
LLC, Ashland, OR, USA).
Cytokine analysis
For measurement of cytokine production, the
CD3+ T cells (purity, >90%) were isolated from the
spleen of mice incubated with CT26 cells (1×106) for 21
days, as described previously (29).
CD3+ T cells were sorted via negative selection using
MACS CD3 MicroBeads (Miltenyi Biotec, Inc., Cambridge, MA, USA).
Subsequently, 5×106 T cells were incubated with
5×105 Ag85A-DCs, mimic-DCs or no DCs in CT26-lysate for
2 days at 37°C. The resulting solution was treated with Brefeldin A
(10 µg/ml) for 5 h at 37°C. Cells were cultured with anti-CD4/CD8
mAbs (cat. no. 23–2615; 1:1,000; BD Biosciences) for 30 min at 4°C.
The intracellular analysis was conducted using a flow cytometer
(FACSCalibur; BD Biosciences). Data were analyzed using FlowJo
software 7.6.1 (FlowJo, LLC, Ashland, OR, USA).
Cell proliferation assessment
To determine cell proliferation of Ag85A-DCs, cells
were treated with 25 µg/ml mitomycin C at 37°C for 30 min. Mimic-DC
and non-transfected DC groups were used as controls. Cells were
washed with PBS, following which cells were added to RPMI medium.
Plates containing allogeneic CD3+ T cells
(2×105 cells/100 µl/well, >90% pure), collected from
C57BL/6 mice via negative selection using MACS CD3 MicroBeads were
originally incubated. T-cell proliferation was measured at 1, 2 and
3 days by Cell Counting Kit 8 (CCK8) analysis. CCK8 was added to
each well and cells were incubated for 4 h at 37°C. The absorbance
at 570 nm was measured using a microplate reader.
DCs pulsed with cancer cell
lysate
Ag85A-DCs were incubated with tumor cell lysates
through repeated freezing-thawing cycles. CT26 cells
(5×107/500 µl) were lysed by rapid freezing in liquid
nitrogen for 10 min, followed by rapid thawing at 37°C water to
dissolve the cells. This step was conducted in triplicate.
Ag85A-DCs (1×106 cells/ml) were cultivated in plates in
RPMI-1640 with 10% fetal calf serum (Gibco; Thermo Fisher
Scientific, Inc.) and 200 µl of CT26 lysate was added, to obtain
2×107 cells. Cells were cultured for 2 days at 37°C and
CO2 concentration of 50 ml/l. The CT26 lysate alone
served as the negative control.
Evaluation of cytotoxic T-lymphocytes
in vitro
To verify the in vitro production of
cancer-specific CTLs, CD3+ T cells were cultivated in
RPMI with IL-2. Primed T-cells and CT26 tumor cells were used as
effector cells and target cells, respectively. After 21 days of
incubation, the target cell suspension (4×105 cells/ml)
was added to the plates, while the effector cells were prepared in
various dilutions (effector-to-target ratio, 50:1). The supernatant
was harvested after 20 h (5,000 × g; 5 min; 20°C). Cytolytic
activities against CT26 cancer cells were determined using a
cytotoxicity measurement kit (HY-K0301; Beyotime Institute of
Biotechnology, Haimen, China). CD8+ T-cells releasing
IFN-γ were determined via flow cytometry (FCM), and the amount of
IFN-γ produced was measured using the mouse IFN-γ Quantikine ELISA
kit (MIF00; R&D Systems, Inc., Minneapolis, MN, USA).
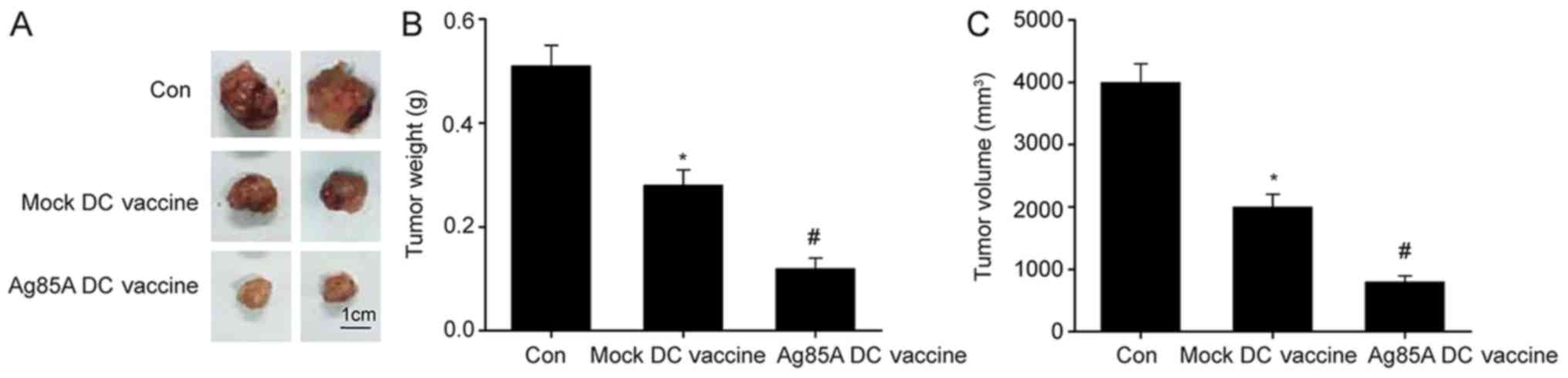
Tumor assessment
First, 1×106 CT26 cells/100 µl were
injected into each C57BL/6 mouse (n=6, male) on the right back. DC
vaccines were then administered at 1, 7 and 14 days after injection
with cancerous cells. Mice were administered with CT26
lysate-pulsed Ag85A-DCs (Ag85A-DC vaccine), CT26 lysate-pulsed
mimic-DCs (mimic-DC vaccine), or CT26 lysate (control) into the
tumors. Length, width and height (mm) of the tumor was measured
with a caliber every 3 days and the volume of tumors was calculated
using the formula as previously (29): V (mm3)=0.52 × length ×
width × height. The corresponding tumor weights were measured
following sacrifice.
Statistical analysis
Data are presented as the mean ± standard error of
the mean. Significant differences among groups were evaluated by
one-way analysis of variance, followed by Tukey's post-hoc test
using SPSS software 17.0 (SPSS, Inc., Chicago, IL, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
Ag85A-transfected DCs
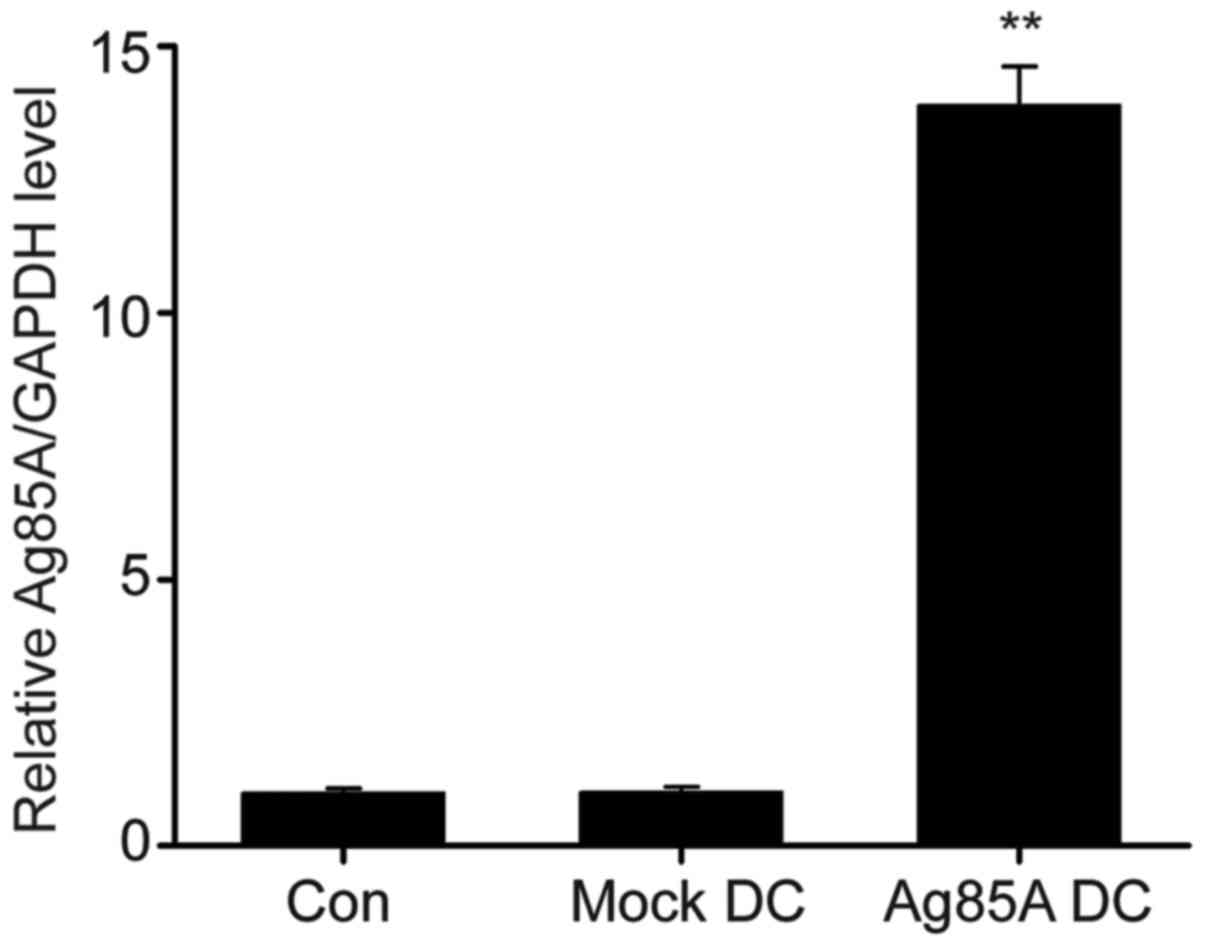
Transfection of DCs with Ag85A DNA was determined to
be successful by RT-qPCR. As indicated in Fig. 1, Ag85A mRNA levels were significantly
upregulated in Ag85A-transfected DCs compared with negative
controls.
Ag85A transfection promotes the
expression of primary surface markers in DCs
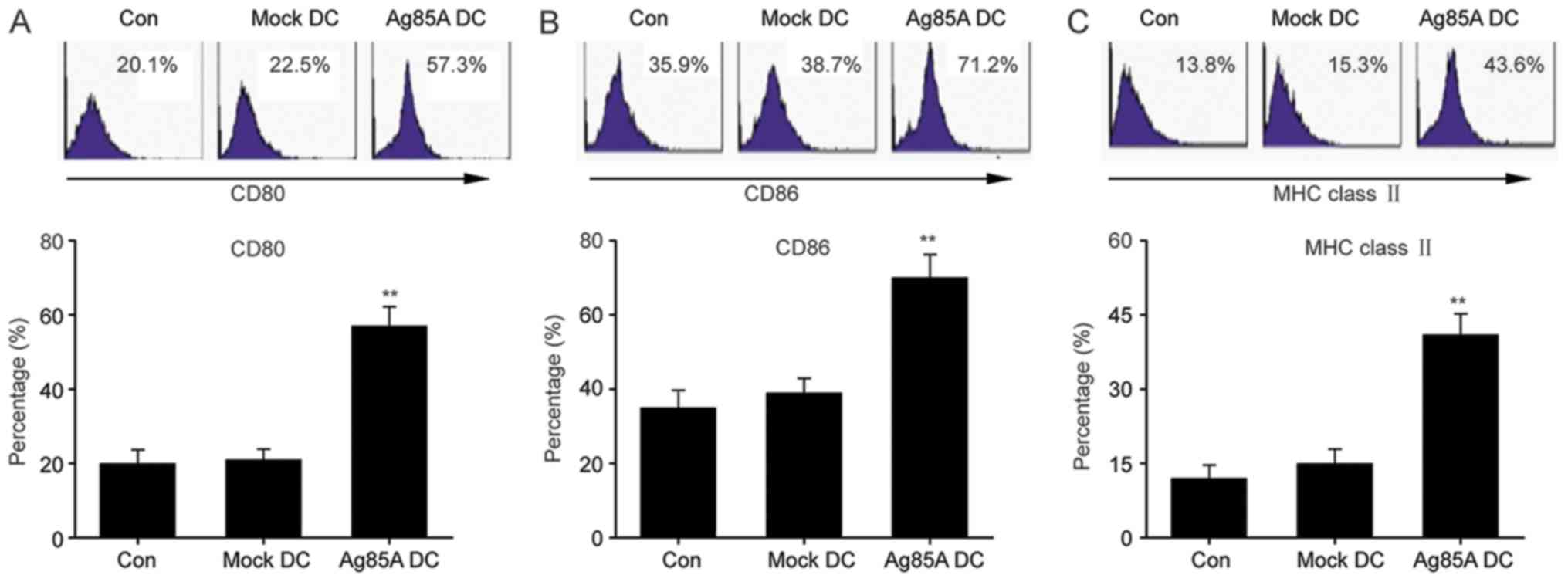
To fully understand the effects of Ag85A on DCs, the
expression of primary surface markers was first evaluated in
Ag85A-transfected DCs. FCM results revealed that the
Ag85A-transfected DCs exhibited significantly increased expression
of MHC class II, CD80 and CD86 compared with the mock-DCs or
negative control DCs (Fig. 2). These
findings indicated that Ag85A transfection promotes the expression
level of primary surface markers in DCs.
Ag85A transfection promotes T-cell
proliferation
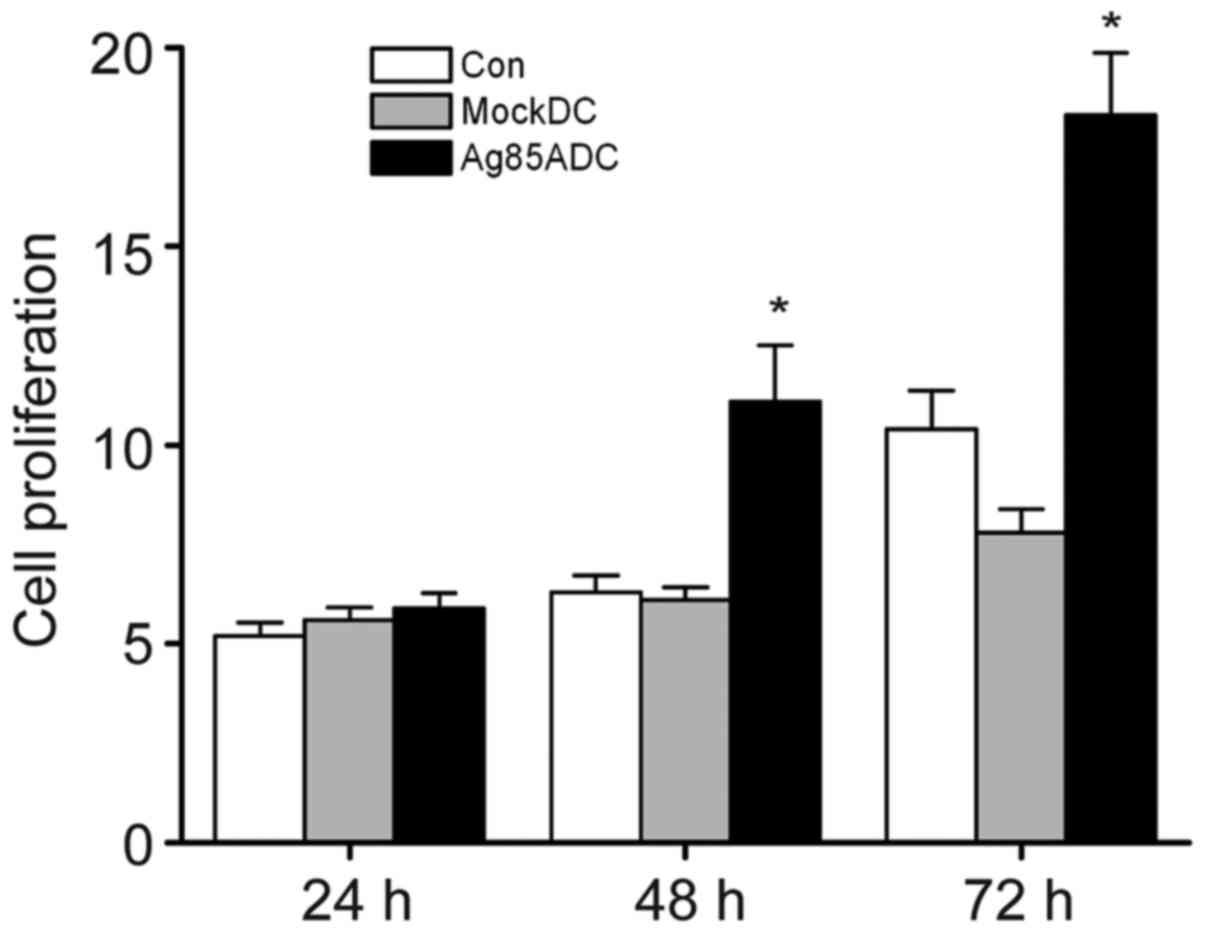
Ag85A-transfected DCs were identified to be more
effective in inducing allogeneic T-cell proliferation compared with
negative control DCs and mock-DCs. Ag85A-DC-induced T-cell
proliferation was significantly increased at 48 and 72 h compared
with mock-DCs and negative control DCs (Fig. 3). These findings suggested that
Ag85A-DCs could trigger T-cell activation.
Ag85A transfection increases
tumor-specific cytotoxicity of T-cells in vitro
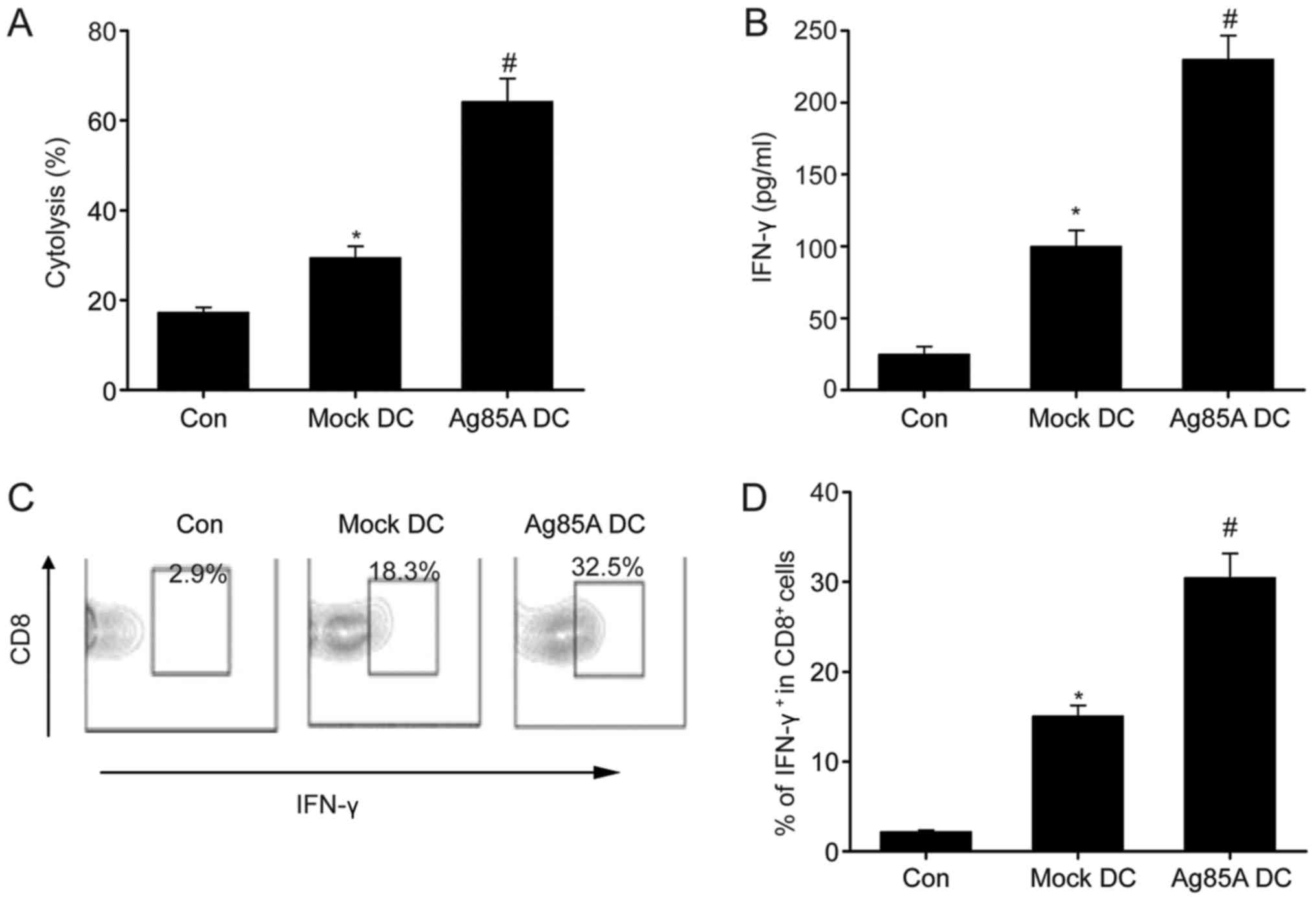
T-cells incubated with CT26 lysate-pulsed Ag85A-DCs
exhibited significantly enhanced cytolytic effects compared with
those incubated with mock-DCs (Fig.
4A). Furthermore, Ag85A-DCs exhibited significantly increased
IFN-γ production compared with the CT26 lysate-pulsed mock-DCs and
CT26 lysate alone (Fig. 4B).
Furthermore, the proportion of IFN-γ-producing CD8+
T-cells was investigated. As indicated in Fig. 4C, the proportion of IFN-γ+
CD8+ cells was considerably higher in cells primed by
CT26 lysate-pulsed Ag85A-DCs compared with cells primed by CT26
lysate alone or CT26 lysate-pulsed mock-DCs. These data
demonstrated the potential of Ag85A-DCs to induce the activation of
certain cytotoxic T-cells in vitro.
Intratumorally injected Ag85A-DC
vaccine suppresses tumor development in mice
Finally, the effect of Ag85A-DCs on colorectal
cancer growth was examined. As depicted in Fig. 5, mice administered with the Ag85A-DC
vaccine had significantly smaller tumor weights and volumes
compared with those administered with the mock-DCs vaccine. These
findings indicate that the Ag85A-DCs vaccine effectively inhibited
tumor growth in vivo.
Discussion
The current findings revealed that Ag85A-transfected
DCs upregulated the expression of MHC-II, CD80 and CD86. Ag85A-DCs
promoted allogeneic T-cell proliferation, elicited stronger
activities against CT26 tumor cells and increased IFN-γ production.
In addition, treatment with the Ag85A-DCs vaccine considerably
suppressed tumor progression in mice. Therefore, it was concluded
that Ag85A-transfected DCs enhanced immunity against colorectal
carcinoma. The current results provided valuable insights and
highlighted the potential use of Ag85A-transfected DC vaccines as
an immunotherapeutic strategy for cancer treatment.
DCs are potentially effective for T-cell immunity.
DCs primed with antigens migrate to lymphoid tissues to prime
T-cells and activate the immune response by expressing
co-stimulating and adhesive cell surface molecules. Host APCs play
crucial roles in tumor antigen presentation (30). Nevertheless, various factors limit
APC maturation and penetration into tumor tissues (31,32). A
previous study demonstrated that production and maturation of DCs
are inhibited by multiple agents in patients with colorectal
carcinoma (33). In the present
study, it was demonstrated that Ag85A-transfected DCs strongly
induced expression of primary surface markers, including MHC-II,
CD80 and CD86, indicating that Ag85A promoted DC generation and
maturation and enhanced anti-tumor immunity.
Ag85A is a key secretory protein in mycobacteria and
thus acts as an effective stimulator of cell-regulated immunity
(34,35). Reorganized Ag85A DNA was demonstrated
to trigger strong immune reactions, leading to dramatic
upregulation of Th1 cytokines (IFN-γ and IL-2), which are crucial
mediators of immunity. In turn, the Th1 cytokines functioned by
stimulating cytotoxic cells and eliminating infected cells
(36–38). In the current study, it was observed
that Ag85A-DCs promoted allogeneic T-cell proliferation and
increased IFN-γ production. DCs transfected with Ag85A exhibited
faster maturation both in terms of phenotype and function.
Ag85A-DCs could effectively induce the activation of original
T-cells, thereby acting as mediators between the internal and
external immunities. Therefore, Ag85A-DCs represent a promising
vaccine for immunotherapy of tumors and other diseases.
The application of DC-dependent tumor vaccination is
effective as an auxiliary agent to stimulate cancer-specific
immunity and represents a promising treatment strategy for
cancerous diseases (39).
Considering the development of drug resistance in late-stage tumor
patients subjected to chemotherapy, the current findings contribute
to the development of an alternative therapeutic strategy against
tumors (40). DCs could be incubated
with synthetic polypeptides and proteins derived from tumors.
Whereas vaccines are developed to target one specific tumor
antigen, antigens derived from tumor cell lysates can trigger a
wide range of T-cell responses against various tumor-related
antigens (41). Vaccines containing
DCs primed with tumor cell lysates have demonstrated strong potency
against various tumor types in both laboratory and clinical
settings (42,43). In the current experiments, Ag85A-DCs
and mock-DCs incubated with CT26 lysates triggered T-cell
activation against certain tumors and induced cytolytic activities
targeting CT26 tumor cells. Furthermore, T-cells primed with CT26
lysate-pulsed Ag85A-DCs exhibited increased tumor-specific CTL
activities compared with T-cells primed with mock-DCs.
Intratumorally injected Ag85A-DC vaccines significantly inhibited
tumor development in mice.
In conclusion, the current study demonstrated that
Ag85A-DCs promoted DC maturation, triggered the activation of
cancer-specific T-cells and promoted anti-tumor cytolytic
activities, thereby contributing to tumor growth inhibition. DCs in
combination with the Ag85A gene could reinforce anti-colorectal
carcinoma immunity. Ag85A-DC vaccines could serve as effective
immunity activators and thus contribute to the development of
therapies against cancers.
Acknowledgements
Not applicable.
Funding
This study was supported financially by grants from
the National Natural Science Foundation of China (grant no.
31270972) and Characteristic Cross Disciplinary Construction
Project of Inner Mongolia University for the Nationalities ‘Study
on the prevention and therapy of brucellosis of Mongolian Medicine’
in 2017 (grant no. MDXK007).
Availability of data and materials
All data generated or analyzed during this study are
included in this article.
Authors' contributions
JZ and WG conceived the project, designed and
performed the experiments, analyzed the data and wrote the
manuscript. LZ performed experiments and analyzed the data. ZG and
XJ performed the in vivo experiments. CL conceived the
project, designed the experiments and revised the manuscript. All
authors read and approved the final version of the document.
Ethics approval and consent to
participate
The animals used in our study were treated in
accordance with protocols approved by the Committee on the Ethics
of Animal Experiments of China Medical University (Shenyang,
China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Miyamoto Y, Zhang W and Lenz HJ: Molecular
landscape and treatment options for patients with metastatic
colorectal cancer. Indian J Surg Oncol. 8:580–590. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bogach J, Levine O, Parpia S, Valencia M,
Ruo L and Serrano P: Does the addition of biologic agents to
chemotherapy in patients with unresectable colorectal cancer
metastases result in a higher proportion of patients undergoing
resection? A systematic review and meta-analysis. J Gastrointest
Surg. 22:523–528. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kwakman JJM, Vink G, Vestjens JH,
Beerepoot LV, de Groot JW, Jansen RL, Opdam FL, Boot H, Creemers
GJ, van Rooijen JM, et al: Feasibility and effectiveness of
trifluridine/tipiracil in metastatic colorectal cancer: Real-life
data from The Netherlands. Int J ClinOncol. 23:482–489. 2018.
|
|
4
|
Meyer B and Are C: Current status and
future directions in colorectal cancer. Indian J Surg Oncol.
8:455–456. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mohammadian M, Zeynali S, Azarbaijani AF,
Khadem AM and Kheradmand F: Cytotoxic effects of the
newly-developed chemotherapeutic agents 17-AAG in combination with
oxaliplatin and capecitabine in colorectal cancer cell lines. Res
Pharm Sci1. 12:517–525. 2017. View Article : Google Scholar
|
|
6
|
Sun X, Han X, Xu L, Gao M, Xu J, Yang R
and Liu Z: Surface-engineering of red blood cells as artificial
antigen presenting cells promising for cancer immunotherapy. Small.
13:2017. View Article : Google Scholar
|
|
7
|
Richaud M and Bendriss-Vermare N: Cancer
immunotherapy via systemic RNA delivery to dendritic cells. Med Sci
(Paris). 33:852–856. 2017.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brown MC, Holl EK, Boczkowski D, Dobrikova
E, Mosaheb M, Chandramohan V, Bigner DD, Gromeier M and Nair SK:
Cancer immunotherapy with recombinant poliovirus induces
IFN-dominant activation of dendritic cells and tumor
antigen-specific CTLs. Sci Transl Med. 9(pii): eaan42202017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gilboa E: DC-based cancer vaccines. J Clin
Invest. 117:1195–1203. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chang WT, Chen HM, Yin SY, Chen YH, Wen
CC, Wei WC, Lai P, Wang CH and Yang NS: Specific
dioscoreaphytoextracts enhance potency of TCL-loaded DC-based
cancer vaccines. Evid Based Complement Alternat Med.
2013:9320402013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Draube A, Klein-González N, Mattheus S,
Brillant C, Hellmich M, Engert A and von Bergwelt-Baildon M:
Dendritic cell based tumor vaccination in prostate and renal cell
cancer: A systematic review and meta-analysis. PLoS One.
6:e188012011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hsu FJ, Benike C, Fagnoni F, Liles TM,
Czerwinski D, Taidi B, Engleman EG and Levy R: Vaccination of
patients with B-cell lymphoma using autologous antigen-pulsed
dendritic cells. Nat Med. 2:52–58. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakai N, Asai J, Ueda E, Takenaka H, Katoh
N and Kishimoto S: Vaccination of Japanese patients with advanced
melanoma with peptide, tumor lysate or both peptide and tumor
lysate-pulsed mature, monocyte-derived dendritic cells. J Dermatol.
33:462–472. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fong L, Hou Y, Rivas A, Benike C, Yuen A,
Fisher GA, Davis MM and Engleman EG: Altered peptide ligand
vaccination with Flt3 ligand expanded dendritic cells for tumor
immunotherapy. Proc Natl Acad Sci USA. 98:8809–8814. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brody JD and Engleman EG: DC-based cancer
vaccines: Lessons from clinical trials. Cytotherapy. 6:122–127.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Engleman EG: Dendritic cell-based cancer
immunotherapy. Semin Oncol. 30(3): Suppl 8:S23–S29. 2003.
View Article : Google Scholar
|
|
17
|
Jakob T, Walker PS, Krieg AM, Udey MC and
Vogel JC: Activation of cutaneous dendritic cells by CpG-containing
oligodeoxynucleotides: A role for dendritic cells in the
augmentation of Th1 responses by immunostimulatory DNA. J Immunol.
161:3042–3049. 1998.PubMed/NCBI
|
|
18
|
Sparwasser T, Koch ES, Vabulas RM, Heeg K,
Lipford GB, Ellwart JW and Wagner H: Bacterial DNA and
immunostimulatory CpG oligonucleotides trigger maturation and
activation of murine dendritic cells. Eur J Immunol. 28:2045–2054.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Belisle JT, Vissa VD, Sievert T, Takayama
K, Brennan PJ and Besra GS: Role of the major antigen of
Mycobacterium tuberculosis in cell wall biogenesis. Science.
276:1420–1422. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lozes E, Huygen K, Content J, Denis O,
Montgomery DL, Yawman AM, Vandenbussche P, Van Vooren JP, Drowart
A, Ulmer JB and Liu MA: Immunogenicity and efficacy of a
tuberculosis DNA vaccine encoding the components of the secreted
antigen 85 complex. Vaccine. 15:830–833. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huygen K, Content J, Denis O, Montgomery
DL, Yawman AM, Deck RR, DeWitt CM, Orme IM, Baldwin S, D'Souza C,
et al: Immunogenicity and protective efficacy of a tuberculosis DNA
vaccine. Nat Med. 2:893–898. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yuan W, Dong N, Zhang L, Liu J, Lin S,
Xiang Z, Qiao H, Tong W and Qin C: Immunogenicity and protective
efficacy of a tuberculosis DNA vaccine expressing a fusion protein
of Ag85B-Esat6-HspX in mice. Vaccine. 30:2490–2497. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tanghe A, Denis O, Lambrecht B, Motte V,
van den Berg T and Huygen K: Tuberculosis DNA vaccine encoding
Ag85A is immunogenic and protective when administered by
intramuscular needle injection but not by epidermal gene gun
bombardment. Infect Immun. 68:3854–3860. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Denis O, Tanghe A, Palfliet K, Jurion F,
van den Berg TP, Vanonckelen A, Ooms J, Saman E, Ulmer JB, Content
J and Huygen K: Vaccination with plasmid DNA encoding mycobacterial
antigen 85A stimulates a CD4+ and CD8+ T-cell epitopic repertoire
broader than that stimulated by Mycobacterium tuberculosis H37Rv
infection. Infect Immun. 66:1527–1533. 1998.PubMed/NCBI
|
|
25
|
Nakano H, Nagata T, Suda T, Tanaka T,
Aoshi T, Uchijima M, Kuwayama S, Kanamaru N, Chida K, Nakamura H,
et al: Immunization with dendritic cells retrovirally transduced
with mycobacterial antigen 85A gene elicits the specific cellular
immunity including cytotoxic T-lymphocyte activity specific to an
epitope on antigen 85A. Vaccine. 24:2110–2119. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tarrant JP, Walsh MJ, Blanchard MC, Lee
TD, Hoskin DW and Giacomantonio CA: Reduced tumorigenicity of
B16-F10 mouse melanoma cells transfected with mycobacterial antigen
85A. Int J Oncol. 25:1693–1699. 2004.PubMed/NCBI
|
|
27
|
Shen Z, Reznikoff G, Dranoff G and Rock
KL: Cloned dendritic cells can present exogenous antigens on both
MHC class I and class II molecules. J Immunol. 158:2723–2730.
1997.PubMed/NCBI
|
|
28
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhang P, Wang J, Wang D, Wang H, Shan F,
Chen L, Hou Y, Wang E and Lu CL: Dendritic cell vaccine modified by
Ag85A gene enhances anti-tumor immunity against bladder cancer. Int
Immunopharmacol. 14:252–260. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Okada H, Tahara H, Shurin MR, Attanucci J,
Giezeman-Smits KM, Fellows WK, Lotze MT, Chambers WH and Bozik ME:
Bone marrow-derived dendritic cells pulsed with a tumor-specific
peptide elicit effective anti-tumor immunity against intracranial
neoplasms. Int J Cancer. 78:196–201. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Koirala P, Roth ME, Gill J, Piperdi S,
Chinai JM, Geller DS, Hoang BH, Park A, Fremed MA, Zang X and
Gorlick R: Immune infiltration and PD-L1 expression in the tumor
microenvironment are prognostic in osteosarcoma. Sci Rep.
6:300932016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Eruslanov E, Daurkin I, Vieweg J, Daaka Y
and Kusmartsev S: Aberrant PGE(2) metabolism in bladder tumor
microenvironment promotes immunosuppressive phenotype of
tumor-infiltrating myeloid cells. Int Immunopharmacol. 11:848–855.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Liu KJ, Wang CC, Chen LT, Cheng AL, Lin
DT, Wu YC, Yu WL, Hung YM, Yang HY, Juang SH and Whang-Peng J:
Generation of carcinoembryonic antigen (CEA)-specific T-cell
responses in HLA-A*0201 and HLA-A*2402 late-stage colorectal cancer
patients after vaccination with dendritic cells loaded with CEA
peptides. Clin Cancer Res. 10:2645–2651. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Meshkat Z, Teimourpour A, Rashidian S,
Arzanlou M and Teimourpour R: Immunogenicity of a DNA vaccine
encoding Ag85a-Tb10.4 antigens from Mycobacterium tuberculosis.
Iran J Immunol. 13:289–295. 2016.PubMed/NCBI
|
|
35
|
Mancha-Agresti P, de Castro CP, Dos Santos
JSC, Araujo MA, Pereira VB, LeBlanc JG, Leclercq SY and Azevedo V:
Recombinant invasive Lactococcus lactis carrying a DNA vaccine
coding the Ag85A antigen increases INF-γ, IL-6 and TNF-α cytokines
after intranasal immunization. Front Microbiol. 8:12632017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Poecheim J, Barnier-Quer C, Collin N and
Borchard G: Ag85A DNA vaccine delivery by nanoparticles: Influence
of the formulation characteristics on immune responses. Vaccines
(Basel). 4(pii): E322016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Stylianou E, Griffiths KL, Poyntz HC,
Harrington-Kandt R, Dicks MD, Stockdale L, Betts G and McShane H:
Improvement of BCG protective efficacy with a novel chimpanzee
adenovirus and a modified vaccinia Ankara virus both expressing
Ag85A. Vaccine. 33:6800–6808. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Metcalfe HJ, Steinbach S, Jones GJ,
Connelley T, Morrison WI, Vordermeier M and Villarreal-Ramos B:
Protection associated with a TB vaccine is linked to increased
frequency of Ag85A-specific CD4(+) T cells but no increase in
avidity for Ag85A. Vaccine. 34:4520–4525. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Chang CN, Huang YC, Yang DM, Kikuta K, Wei
KJ, Kubota T and Yang WK: A phase I/II clinical trial investigating
the adverse and therapeutic effects of a postoperative autologous
dendritic cell tumor vaccine in patients with malignant glioma. J
Clin Neurosci. 18:1048–1054. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lou Q, Conway TJ Jr, Egilmez NK, Loyall
JL, Bernstein SH, Kelleher RJ Jr and Bankert RB: B cell tumor
vaccine enhanced by covalent attachment of immunoglobulin to
surface proteins on dendritic cells. Clin Immunol. 118:66–76. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Fields RC, Shimizu K and Mulé JJ: Murine
dendritic cells pulsed with whole tumor lysates mediate potent
antitumor immune responses in vitro and in vivo. Proc Natl Acad Sci
USA. 95:9482–9487. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Dauer M, Herten J, Bauer C, Renner F,
Schad K, Schnurr M, Endres S and Eigler A: Chemosensitization of
pancreatic carcinoma cells to enhance T cell-mediated cytotoxicity
induced by tumor lysate-pulsed dendritic cells. J Immunother.
28:332–342. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Schnurr M, Galambos P, Scholz C, Then F,
Dauer M, Endres S and Eigler A: Tumor cell lysate-pulsed human
dendritic cells induce a T-cell response against pancreatic
carcinoma cells: an in vitro model for the assessment of tumor
vaccines. Cancer Res. 61:6445–6450. 2001.PubMed/NCBI
|