Introduction
Dislocation or subluxation of the intraocular lens
(IOL)-capsular bag (CB)-capsular tension ring (CTR) complex is a
serious complication of cataract surgery (1). Spontaneous late in-the-bag IOL
dislocation is commonly caused by trauma or pseudoexfoliation
(1–5). Although the implantation of a CTR
relieves zonular tension, the IOL-CB-CTR complex is also
susceptible to dislocation and subluxation. The rate of surgical
correction for dislocation or subluxation of the IOL-CB-CTR complex
is 0.76% with an interval of 92.7±23.4 months between the initial
and reparative surgery (6).
Traditionally, dislocation of the IOL-CB-CTR complex
has been treated by explanting the IOL-CTR through an incision in
the scleral tunnel or corneal limbus, followed by implantation of a
new IOL (7). However, several
inherent problems are associated with IOL explantation and
replacement. The lens extraction incision must be 3–5 mm in length,
and the IOL and CTR must be removed independently of each other.
During the procedure, if either the IOL or CTR is dislocated
posteriorly into the vitreous cavity, a vitrectomy may be necessary
and a new IOL may be required be implanted at low intraocular
pressure (8). Furthermore, IOL
extraction and replacement is technically challenging and
time-consuming. Complications accompanying this procedure include
massive retinal hemorrhage, retinal detachment and intraocular
infection.
The ideal surgical approach to correct dislocation
or subluxation of the IOL-CB-CTR complex avoids any requirement for
extraction of the IOL-CB-CTR complex, by resolving the subluxation
with a small corneal incision (1).
The method proposed by the present study is quick,
simple and minimally invasive. It involves the repositioning and
fixation of the IOL through sutures. This may reduce intraocular
pressure and prevent post-operative complications. The present
study describes a simple and efficient technique for suturing the
dislocated IOL-CB-CTR complex on the sclera, using 1-mm
corneoscleral limbus incisions.
Case study and surgical technique
The current case study is a representative case.
Five years and 10 months prior to presentation, a 59-year-old man
with a history of chronic obstructive pulmonary disease was treated
with phacoemulsification of the right eye, with an implantation of
a CTR and an IOL (19.5 D; AR40E; Abbott Medical Optics Inc., Santa
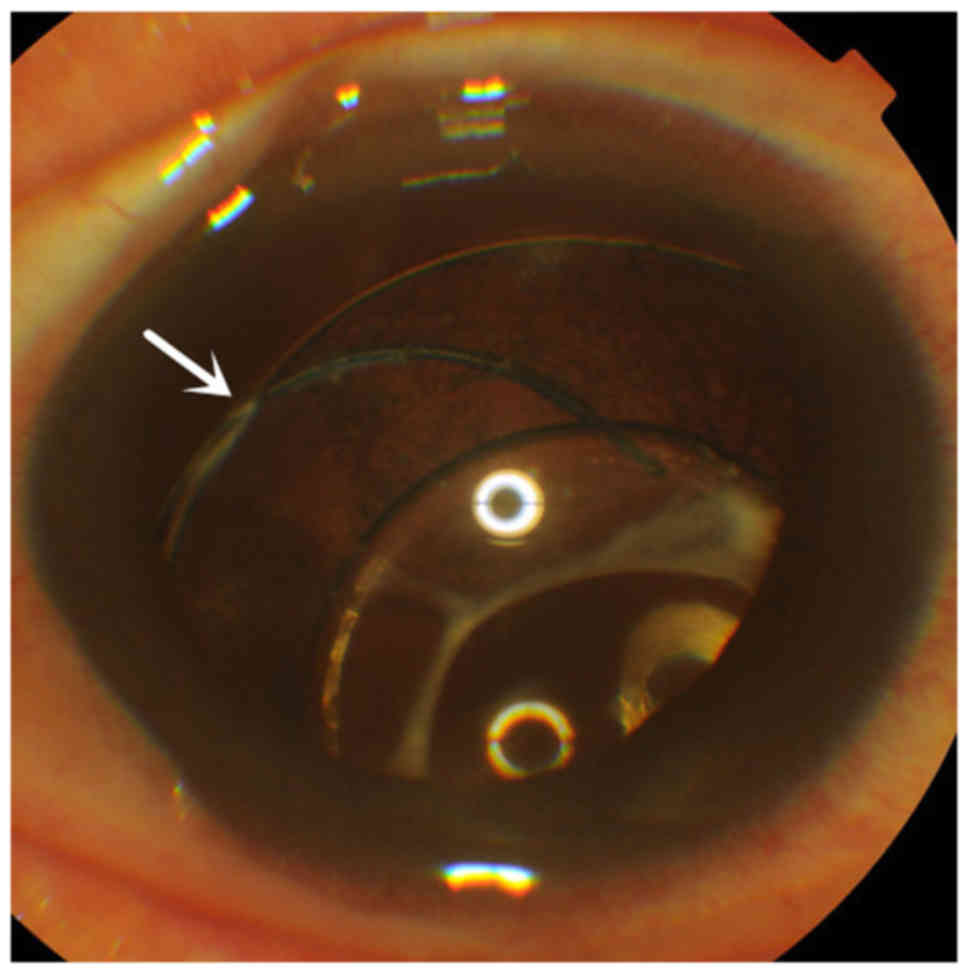
Ana, CA, USA) in the lens capsule. In March 2011, this patient
presented with acute vision decline accompanied by intense coughing
and sneezing. Upon ophthalmologic examination, the patient was
determined to have a bitemporal-upper quadrant dislocation of the
IOL-CTR (Fig. 1). Zonular disruption
was observed between the 9 and 2 o'clock positions, suggesting a
subluxation of the IOL-CB-CTR complex. At presentation, the
patient's vision was 0.2 and intraocular pressure was 15 mmHg.
For this patient, repositioning of the IOL by
bilaterally suturing the complex to the ciliary groove was
proposed. As the patient was placed in a supine position on the
operating table, the dislocated IOL-CB-CTR complex migrated to the
center of the pupillary axis. The lens dislocation was
significantly more pronounced when the patient was in a sitting
position compared to that observed in a supine position.
Manipulation of the position of the head did not
cause any excessive frontal-temporal offset of the IOL-CB-CTR
complex. No fractures were present inferior to the nasal zonules
and the position of the capsular bag was maintained. The right
pupil was dilated by tropicamide, and retrobulbar anesthesia
consisting of 2 cc lidocaine and 2 cc bupivacaine was then injected
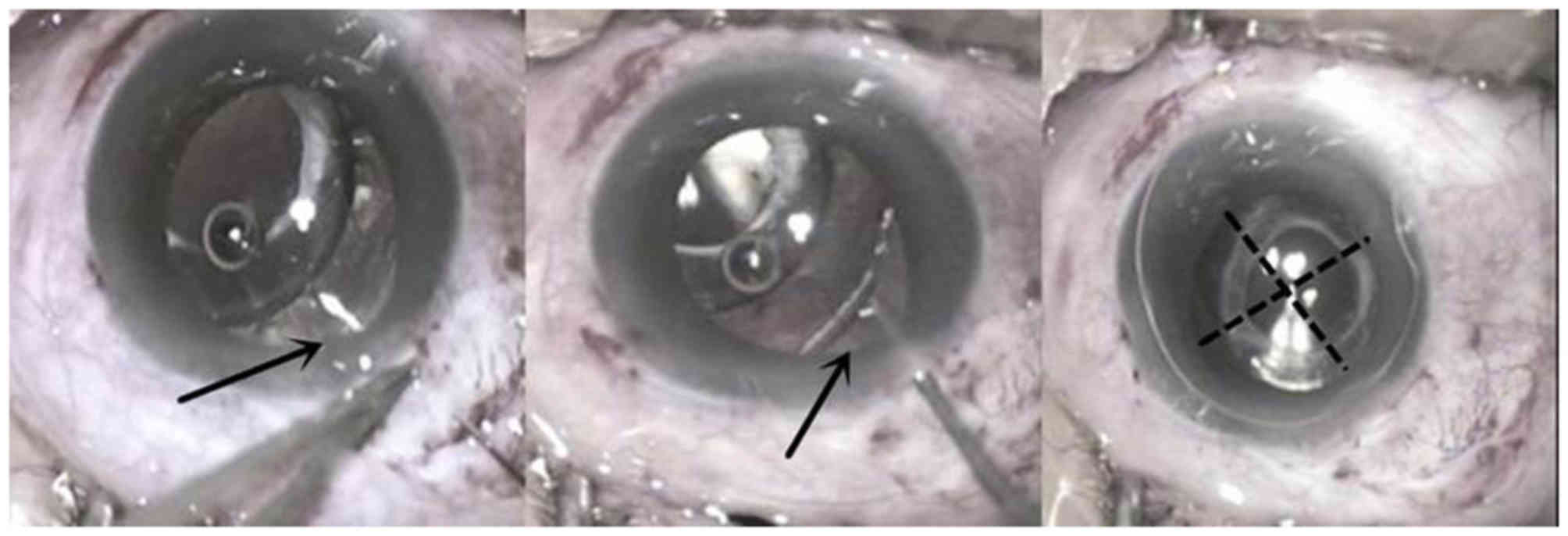
into the retrobulbar space. Subsequently, two 1-mm corneoscleral
incisions were made at the 11 and 3 o'clock positions. Sodium
hyaluronate (1%) was then injected and allowed to move through the
vitreous fluid into the posterior chamber. The IOL-CB-CTR complex
was moved nasally to expose the tension ring and IOL haptics. A
fornix-based conjunctival flap was made. A partial-thickness
triangular scleral flap was made 2.0–2.5 mm posterior to the
surgical limbus. A Z-suture was placed on the sclera 4 mm from the
corneoscleral limbus. In this position, one double-curved 10–0
polypropylene (Prolene) suture was passed through the sclera into
the posterior chamber, penetrating the posterior capsules and
wrapping perpendicularly around the tangential contact point
between the IOL haptics and the CTR, and finally passing through
the anterior capsules into the anterior chamber (Fig. 2). The polypropylene suture was passed
over and under the CTR, which was then retracted through the
sclera. The 10-0 polypropylene suture was pulled to provide
adequate tension for the CB centration.
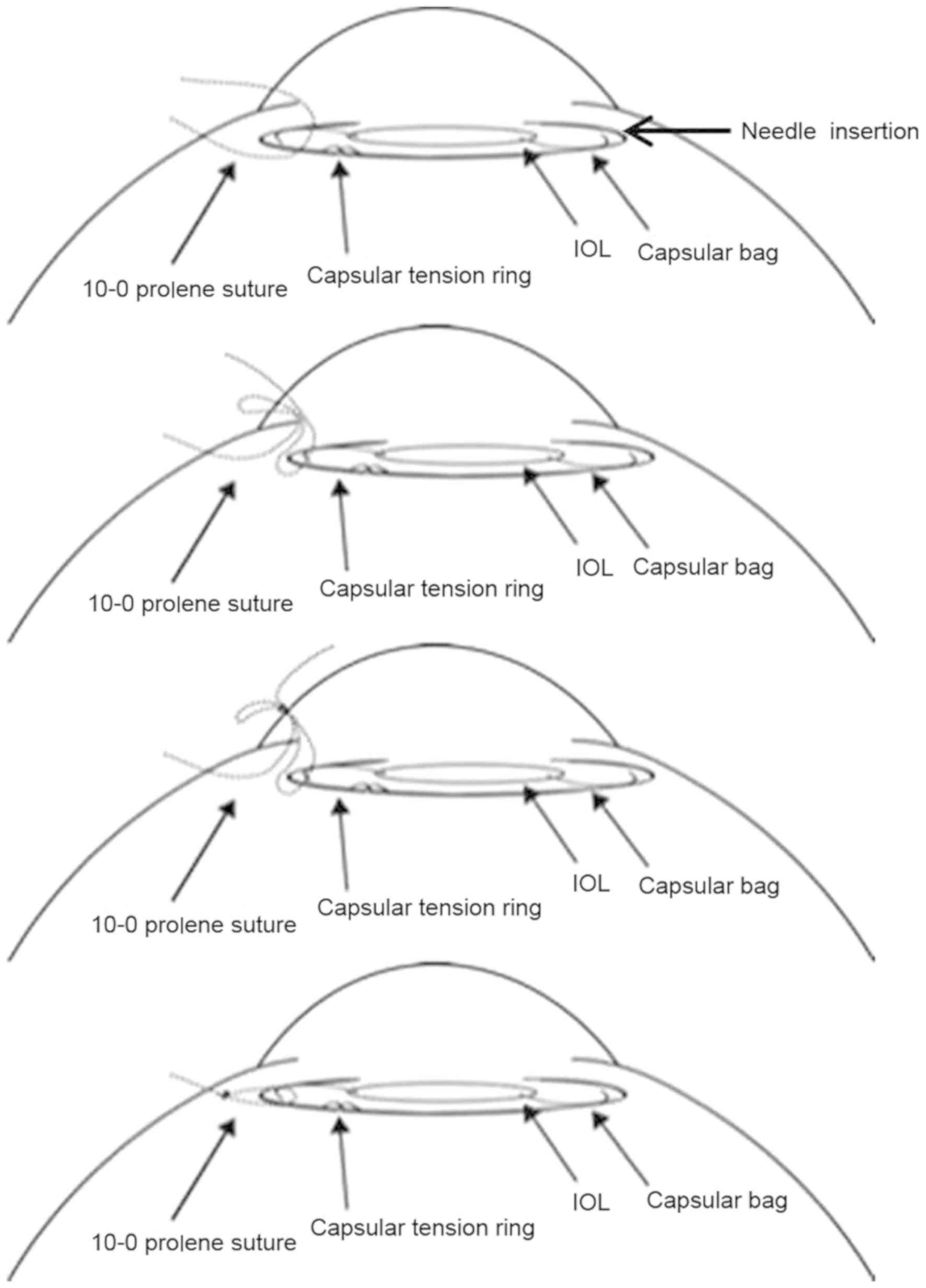
From the 3 o'clock corneoscleral limbus incision,
the stitches were cut from the incision suture and the broken ends
were pulled out. The thread was cut near the needle and then pulled
out from the incision. The suture lines were pulled out from the
anterior and posterior surfaces of the IOL-CB-CTR complex, and a
knot was tied 1 mm away from the corneoscleral incision. The knot
was buried in the scleral bed and covered with the scleral flap and
conjunctiva. After the sutures were cut, the IOL-CB-CTR complex was
repositioned to the center by pulling the suture line (Fig. 3; Video S1).
It is standard knowledge that intact zonules provide
support and circular contour to the capsular bag. In the present
study, the position of the CTR-CB-IOL complex was maintained
through a unilateral suture fixation. No sutures were made on the
contralateral side. The last procedure was an anterior vitrectomy,
which consisted of the removal of the sac and the structures
surrounding the anterior chamber.
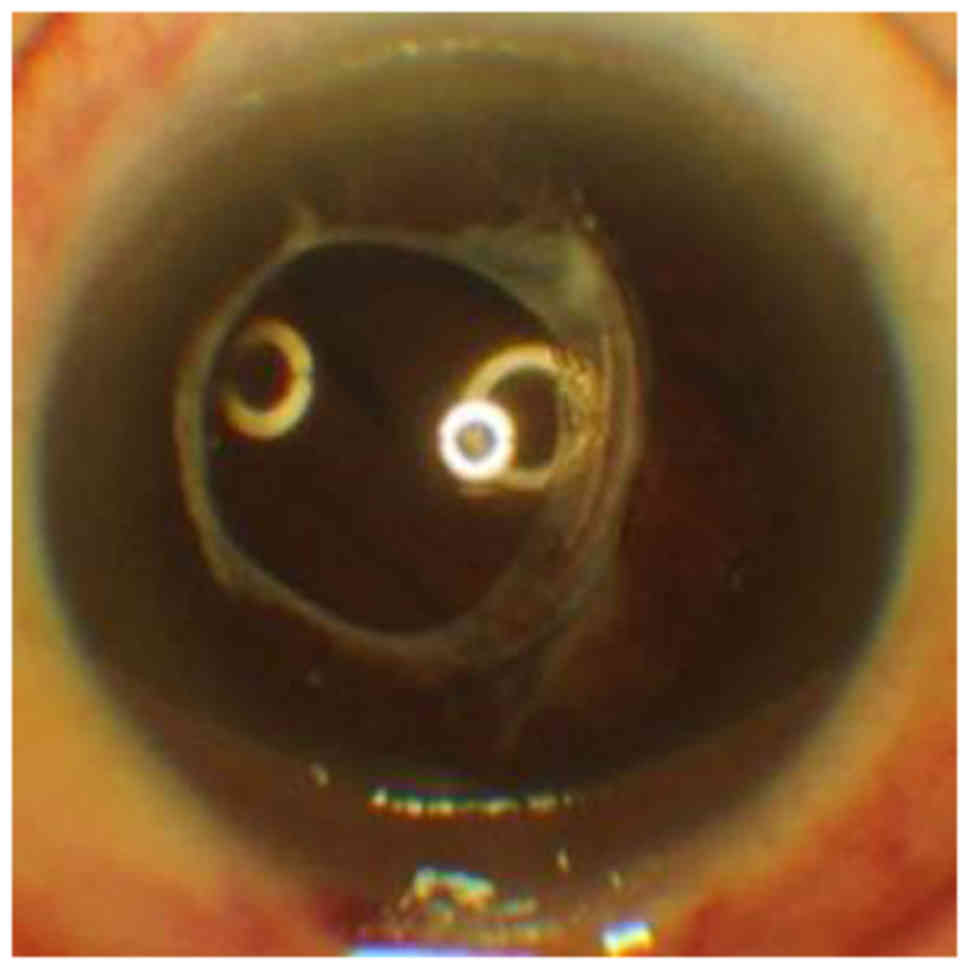
One day after the procedure, the patient's vision
was 0.4 and the CTR-CB-IOL complex remained centered, with minor
bleeding visible in the vitreous space. At two weeks after the
procedure, the hematoceles had been reabsorbed. At the one-year
follow-up, the patient's vision was 0.8 and the IOL-CB-CTR complex
remained centered (Fig. 4).
Discussion
The present study described a novel method to
correct a dislocation and subluxation of an IOL-CTR that avoided
explantation of the IOL. Rather, the IOL-CB-CTR complex was simply
and effectively immobilized.
Suture immobilization of a subluxated or dislocated
IOL is not a novel technique, but it has been underutilized
(1). A similar operation was
described in one case of CTR-CB-IOL dislocation repair, in which
two sutures were placed 180 degrees apart to reposition the
IOL-CB-CTR complex (1). By contrast,
the present procedure used a single suture through the IOL-CB-CTR
complex and the remaining ciliary fibers to provide contralateral
support. Oner et al (9)
reported a IOL-CB-CTR subluxation suture repair technique involving
the transscleral placement of two 10-0 polypropylene sutures over
and under the CTR through the anterior and posterior capsular
surfaces to secure the CTR. This was then retracted and sutured
through the sclera. The present technique involves fewer traumatic
needle paths and smaller incisions.
The path of the suture is crucial for determining
the degree of scleral penetration, which may be associated with
hemorrhage of the ciliary bodies (10,11).
Favorable suture paths are only one of the advantages of the
present technique. In published reports, at least two punctures
were performed in the sclera. However, in our case report, the
sclera is penetrated only once. Less amount of penetration avoids
any repeated perforations and reduces the risk of hemorrhage. The
suture is tied faster than in corresponding techniques (7,11,12). The
final fixed position of the IOL-CB-CTR complex is similar to the
anatomical position.
As the ideal result, the haptics of the IOL and the
tension ring would be fixed precisely within the ciliary groove.
The Z-suture between the sclera has sufficient tension to fix the
complex, and the inflammatory adhesion produced by the suture and
sclera supports this. Using the present method the creation of
partial-thickness triangular scleral flaps with low intraocular
pressure is not required, thereby reducing the time of the
procedure, which may in turn reduce the rate of complications and
endophthalmitis. This method may prevent future dislocations of the
IOL-CB-CTR complex, as the tension of the suture may be adjusted
even after the suture has been knotted. In this way, the present
technique simplifies the repositioning of the IOL-CB-CTR complex.
Another advantage of this technique is the minimally invasive 1-mm
corneoscleral limbus incision, which reduces the risk of
astigmatism. The small incision keeps the anterior chamber stable
and prevents partial or complete movement during suturing of the
complex.
Regardless of the type of suture, the position of
the suture that penetrates the capsule and its relative orientation
with the IOL-CTR contact point determine the success of the
procedure. The tension ring and IOL haptics are independent
circular structures and physically meet nearly tangentially inside
the capsular bag. The suture should penetrate the capsule through a
point perpendicular to the tangential IOL-CTR contact point. Based
on the authors' experience, if the suture is inserted away from
this point, the capsule may be torn by the suture, bearing a risk
of spillage of the IOL into the vitreous cavity. If the suture only
secures the CTR, it cannot adequately support the stability of the
entire complex, as the tension of the suture is unbalanced. Of
note, pre-operative evaluation of the zonules should be performed
to determine whether unilateral or bilateral suturing is
required.
In conclusion, suturing the CTR-CB-IOL complex is
simple and effective. It secures the position of the IOL and
prevents any requirement for the explantation of the complex or
suturing of a new IOL onto the sclera, increasing the work
efficiency of the surgery.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The data and materials in this study are available
from the corresponding author on reasonable request.
Authors' contributions
LG collected, collated and classified the
experimental data, and wrote the manuscript. XY responsible for the
application of experimental ethics. CW performed the surgeries. All
three authors designed the current study, and analysed and
interpreted the data.
Ethical approval and consent to
participate
The present study was approved by the Ethics
Committee of Xi'an No. 4 Hospital, Affiliated GuangRen Hospital,
School of Medicine, Xi'an Jiao Tong University (Xi'an, China).
Patient consent for publication
The patient provided informed consent for the
publication of the intra-operative images/video.
Competing interests
None of the authors has any conflicts of interest to
declare.
References
|
1
|
Moreno-Montañés J, Heras H and
Fernández-Hortelano A: Surgical treatment of a dislocated
intraocular lens-capsular bag-capsular tension ring complex. J
Cataract Refract Surg. 31:270–273. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bhattacharjee H, Bhattacharjee K, Das D,
Jain PK, Chakraborty D and Deka S: Management of a posteriorly
dislocated endocapsular tension ring and a foldable acrylic
intraocular lens. J Cataract Refract Surg. 30:243–246. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gross JG, Kokame GT and Weinberg DV;
Dislocated In-The-Bag Intraocular Lens Study Group: In-the-bag
intraocular lens dislocation. Am J Ophthalmol. 137:630–635. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Scherer M, Bertelmann E and Rieck P: Late
spontaneous in-the-bag intraocular lens and capsular tension ring
dislocation in pseudoexfoliation syndrome. J Cataract Refract Surg.
32:672–675. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ahmed II, Chen SH, Kranemann C and Wong
DT: Surgical repositioning of dislocated capsular tension rings.
Ophthalmology. 112:1725–1733. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Werner L, Zaugg B, Neuhann T, Burrow M and
Tetz M: In-the-bag capsular tension ring and intraocular lens
subluxation or dislocation: A series of 23 cases. Ophthalmology.
119:266–271. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tribus C, Alge CS, Haritoglou C,
Lackerbauer C, Kampik A, Mueller A and Priglinger SG: Indications
and clinical outcome of capsular tension ring (CTR) implantation: A
review of 9528 cataract surgeries. Clin Ophthalmol. 1:65–69.
2007.PubMed/NCBI
|
|
8
|
Lang Y, Fineberg E and Garzozi HJ:
Vitrectomy to remove a posteriorly dislocated endocapsular tension
ring. J Cataract Refract Surg. 27:474–476. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oner FH, Kocak N and Saatci AO:
Dislocation of capsular bag with intraocular lens and capsular
tension ring. J Cataract Refract Surg. 32:1756–1758. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang CS and Chao YJ: Long-term outcome of
combined vitrectomy and transscleral suture fixation of posterior
chamber intraocular lenses in the management of posteriorly
dislocated lenses. J Chin Med Assoc. 79:450–455. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Banaee T and Sagheb S: Scleral fixation of
intraocular lens in eyes with history of open globe injury. J
Pediatr Ophthalmol Strabismus. 48:292–297. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
John T, Tighe S, Hashem O and Sheha H: New
use of 8-0 polypropylene suture for four-point scleral fixation of
secondary intraocular lenses. J Cataract Refract Surg.
44:1421–1425. 2018. View Article : Google Scholar : PubMed/NCBI
|