Introduction
Prolonged glucocorticoid administration causes two
common and irreversible skeletal problems, namely
glucocorticoid-induced osteoporosis and osteonecrosis of the
femoral head (1). Osteonecrosis of
the femoral head, which is characterized by degeneration and
destruction, involves both the articular cartilage and the
subchondral bone. However, the area most vulnerable to steroid use
remains uncertain. It is unclear whether articular cartilage and
subchondral bone of the knee joint are also affected by excessive
glucocorticoid use, in addition to the femoral head. In patients
receiving glucocorticoid therapy, the incidence of osteonecrosis
ranges from 9–40% and is reportedly increasing (2,3).
Long-term low-dose use or short-term exposure to large doses of
glucocorticoids can potentially lead to osteonecrosis of the
femoral head even in the absence of osteoporosis (4). Published reports suggest that
osteonecrosis of the femoral head can occur as early as 36 days
after steroid use even though, in most cases, osteoporosis often
appears after 3 months of glucocorticoid use (5). Thus, it appears that osteonecrosis
develops prior to osteoporosis and that pathological changes occur
before osteonecrosis symptoms manifest themselves (6). It is known that pathological changes
during osteonecrosis of the femoral head include reduced
subchondral trabecular bone mass, deteriorated trabecular
microstructure, thinning and degenerating of the articular
cartilage, and eventual collapse of the femoral head and joint
dysfunction (7,8). The knee joint is similar in structure
to the articular cartilage and the subchondral bone. Nevertheless,
few reports have described the histopathological and bone
remodeling changes in the cartilage and the subchondral bone of the
knee.
Therefore, the aim of the current study was to
investigate the changes in morphology and microstructure of the
articular cartilage and to assess bone remodeling of the
subchondral trabecular bone in the proximal tibia due to prolonged
glucocorticoid treatment at three different doses using an
experimental rat model.
Materials and methods
Animal model and grouping
The current study was performed according to the
guidelines for the Care and Use of Laboratory Animals of the
Guangdong Laboratory Animal Monitoring Institute (Guangzhou, China)
and were approved by the Academic Committee on the Ethics of Animal
Experiments of Guangdong Medical University (Zhanjiang, China) with
permit number SYXK (Guangdong) A2008036. A total of 30 female
Sprague-Dawley rats (age, 3 months; weight, 180–200 g) were
provided by the animal center at Guangdong Medical University
(Zhanjiang, China). All rats were housed under identical conditions
with controlled temperature (24–28°C), relative humidity (50–70%)
and 12-h light/dark cycle with free access to fresh water and a
normal diet.
All rats were divided into the following four groups
(mean body weight, 180–200 g): Vehicle control (Cont, saline alone,
n=7) or dexamethasone (Dex) sodium phosphate (provided by the
College of Pharmacy, University of Nebraska, Omaha, NE, USA) at
doses of 1.0 (Dex1.0, n=7), 2.5 (Dex2.5, n=8), and 5.0 mg/kg
(Dex5.0, n=8). Dex sodium phosphate was dissolved in saline and was
injected intramuscularly (1 ml/kg) twice/week for 8 weeks. The Dex
dose and administration route were selected based on published
literature (9).
Histopathology and evaluation of bone
remodeling characteristics
At the end of the experiment, all tibias were
harvested. Before subjecting them to gradient dehydration and
methyl methacrylate resin embedding, the proximal tibia with an
intact lateral plateau of articular cartilage was stripped of soft
tissues and sawed on the frontal plane using an IsoMet precision
bone saw (Buehler, Lake Bluff, IL, USA) to expose the marrow
cavity. Next, undecalcified bone plastic blocks were sliced at
thicknesses of 9 and 4 µm on a hard tissue microtome (Leica RM2255,
Leica Microsystems GmbH, Wetzlar, Germany). The unstained 9-µm
thick sections were directly processed for histomorphometry, while
the 4 µm sections were stained using the Masson-Goldner trichrome
staining technique (10) (CAS
Hematoxylin 517-28-2, Ponceau 2R 3761-53-3, Acid Fuchsin 3244-88-0,
Orange G 1936-15-8, Light green SF yellowish 5141-20-8;
Sigma-Aldrich; Merck KGaA). Sections were analyzed on a graphics
tablet (DTZ-2100D, Wacom Co., Ltd., Kazo, Japan) connected to a
semi-automatic digitizing image analysis system using the DP72
Olypus camera and a light microscope (BX43; Olympus Corporation,
Tokyo, Japan) with a measurement software program (OsteoMeasure
3.1, Osteometrics, Inc., Decatur, GA, USA).
The thickness of the articular cartilage, including
the superficial, transitional and radial zones, as well as the
thickness of the subchondral zone, including the calcified zone and
the subchondral cortical plate, were measured. Additionally,
chondrocyte volume, size, shape and arrangement and blood vessel
number were recorded and compared among the Dex groups and
controls. Histomorphometric parameters in the subchondral
trabecular bone area between the proximal tibial growth cartilage
and the subchondral cortical plate were also analyzed. The
abbreviations of the parameters used follow the recommendations of
the Histomorphometric Nomenclature Committee and have been used in
previous studies (11). The
microarchitecture parameters analyzed were trabecular thickness
(Tb.Th), trabecular number (Tb.N) and trabecular spacing (Tb.Sp).
Dynamic measurement parameters, ratio of mineralizing surface to
bone surface (MS/BS), bone formation rate per unit of bone surface
(BFR/BS) and bone formation rate per unit of bone volume (BFR/BV)
were analyzed under ultraviolet light. The number of osteoblast
surfaces per bone surface (Ob.S/BS), osteoclast surfaces per bone
surface (Oc.S/BS) and osteocyte lacuna volume (Osteocyte.V/BV) were
also measured.
Fluorochrome labeling analysis
For double labeling in vivo, rats were
administered a subcutaneous injection of tetracycline (40 mg/kg,
Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) on days 13 and 14,
and calcein (10 mg/kg, Sigma-Aldrich; Merck KGaA) on days 3 and 4
prior to sacrifice. Rats were euthanized by intraperitoneal
injection of sodium pentobarbital (1.2 mg/kg) and 8–10 ml blood was
obtained by cardiac puncture. The left proximal tibias were
harvested, as described above. Fluorescence was visualized using a
fluorescence microscope (magnification, ×10; Olympus
Corporation).
Statistical analysis
Data are presented as the mean ± standard deviation.
The statistical differences among groups were evaluated by analysis
of variance with Fisher's least significant difference test using
SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
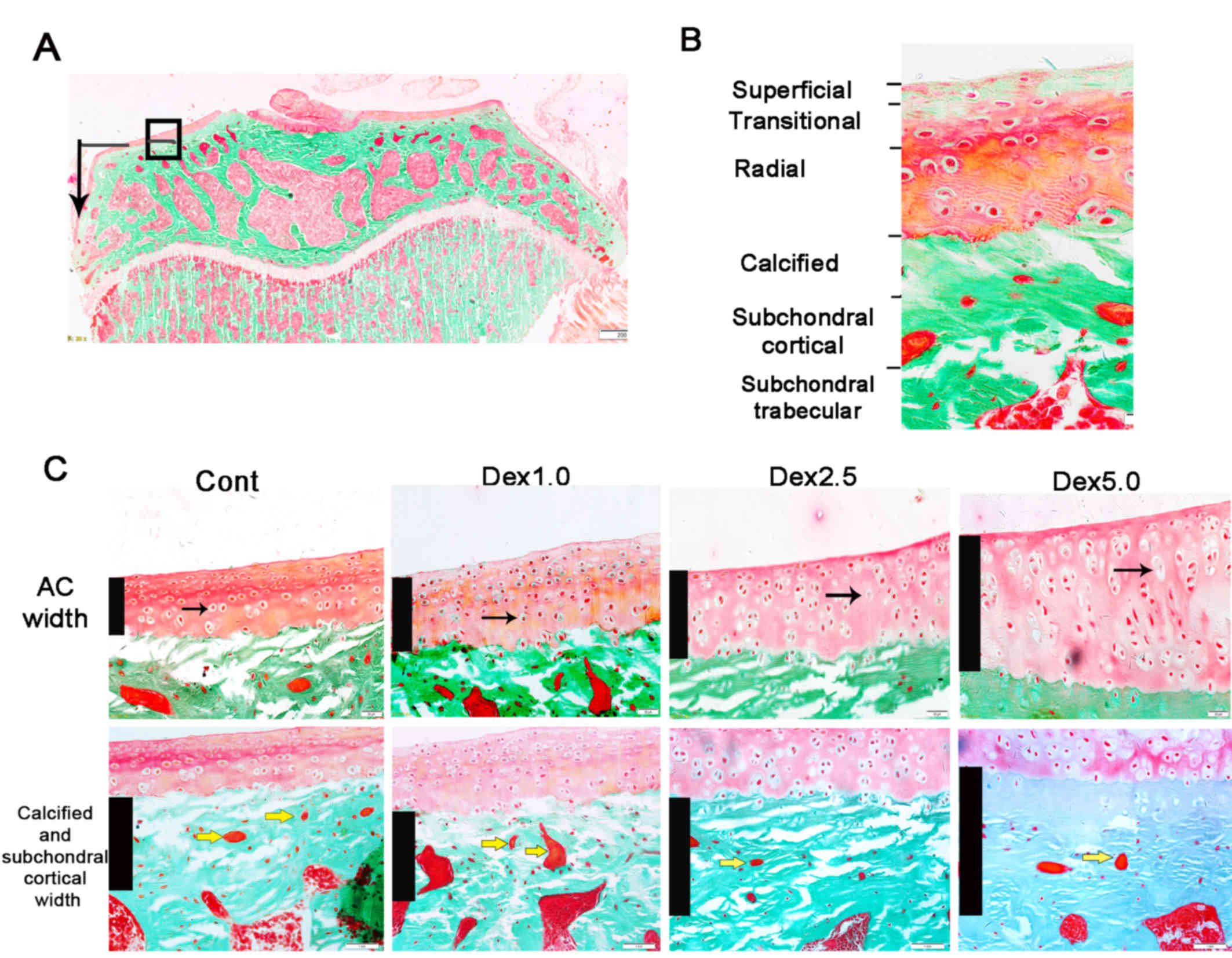
Representative images indicating the thickness and
morphology of the articular cartilage and the subchondral zone are
presented in Fig. 1 and
quantification of the associated parameters is presented in
Fig. 2. There were no obvious
differences between the control and Dex1.0 groups. When compared
with the control and Dex1.0 groups, the total width of the
articular cartilage was significantly higher in the Dex2.5 group
due to greater thickness of the transitional and radial zones.
Similarly, the width of the entire articular cartilage had
significantly expanded in the Dex5.0 group when compared with the
control and Dex1.0 groups and is attributable to the thickening of
the radial and transitional zone, which countered a reduction in
the superficial zone (Fig. 2A).
Chondrocytes within the articular cartilage were either spherical
or elliptical in shape in the normal and the Dex1.0 groups with
uniform and rich cytoplasm. In contrast, in the Dex2.5 and Dex5.0
groups, chondrocytes were triangular or spindle-like with denser
cytoplasm and apoptotic chondrocytes (Fig. 1), and demonstrated a significantly
lower cell/matrix volume ratio in the articular cartilage (Fig. 2B). The width of the subchondral zone,
including the calcified zone and the subchondral cortical plate was
larger, but the blood vessel number within the cortical plate was
lower in the Dex2.5 and Dex5.0 groups compared with the Dex1.0 and
control group (Fig. 2C and D).
 | Figure 1.Morphology of the AC and subchondral
zone from rats treated with vehicle or three doses of Dex. Staining
was performed using the Masson-Goldner trichrome bone stain
technique. (A) Image of the proximal tibial epiphyseal area with an
intact lateral plateau of AC. Magnification, ×4. The black frame
and corner arrow in indicate the observed and measured site of AC
and subchondral zone, which is magnified and shown separately in
panel C. (B) Enlarged section indicating the AC layers and
subchondral zone shown in panel C. Original magnification, ×40. (C)
AC and subchondral zone in each group. Black columns indicate the
width of either AC or subchondral zone. Black arrows point to
chondrocytes in the AC. Chondrocytes are normal in the Cont and
Dex1.0 mg groups but are triangular or spindle-like with large
vacuoles in the Dex2.5 and Dex5.0 groups. Yellow arrows point to
blood vessels within the subchondral cortical plate. Magnification,
×20. Dex, dexamethasone; Cont, control group, Dex1.0, Dex 1.0 mg/kg
group; Dex2.5, Dex 2.5 mg/kg group; Dex5.0, Dex 5.0 mg/kg group;
AC, articular cartilage. |
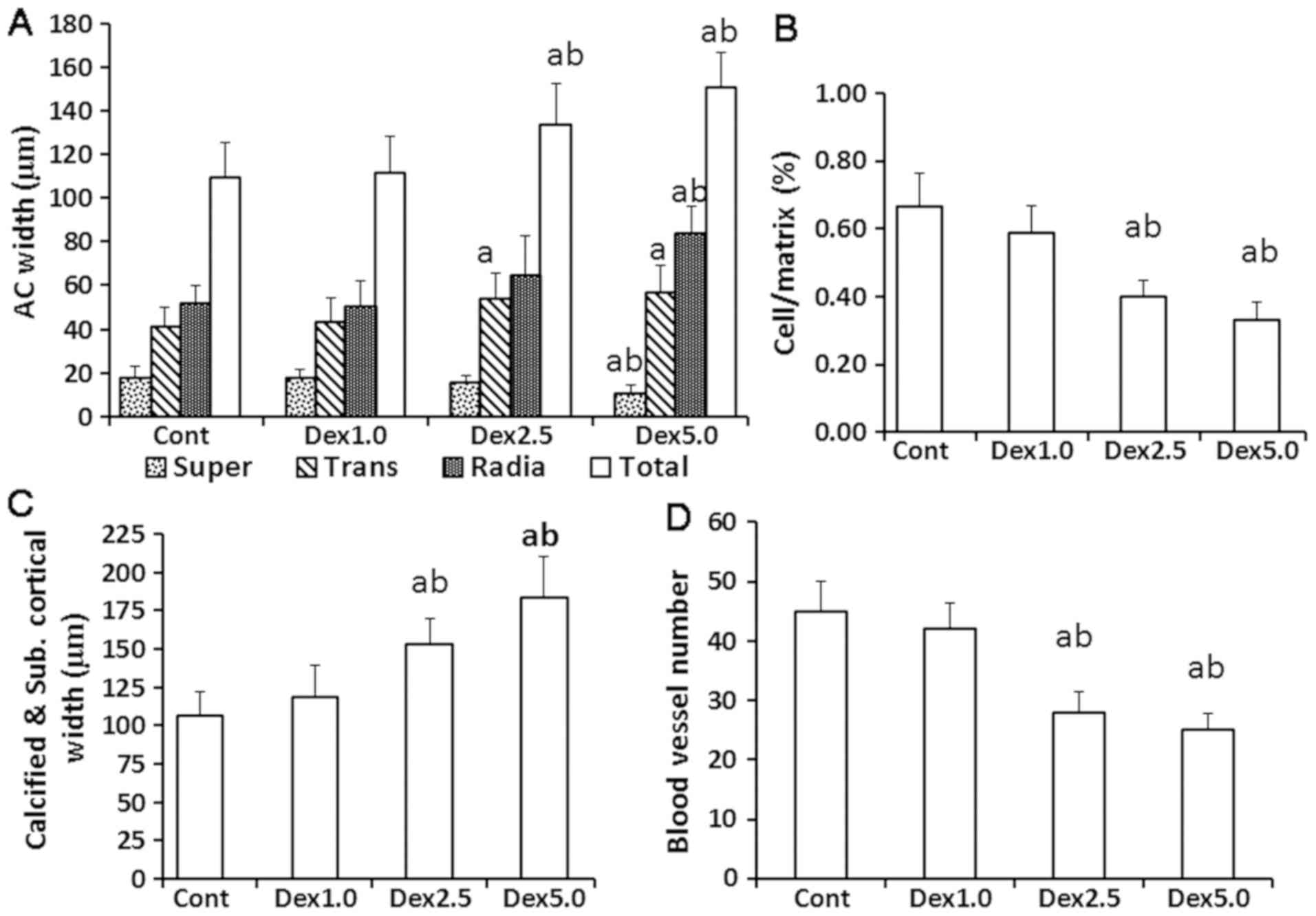
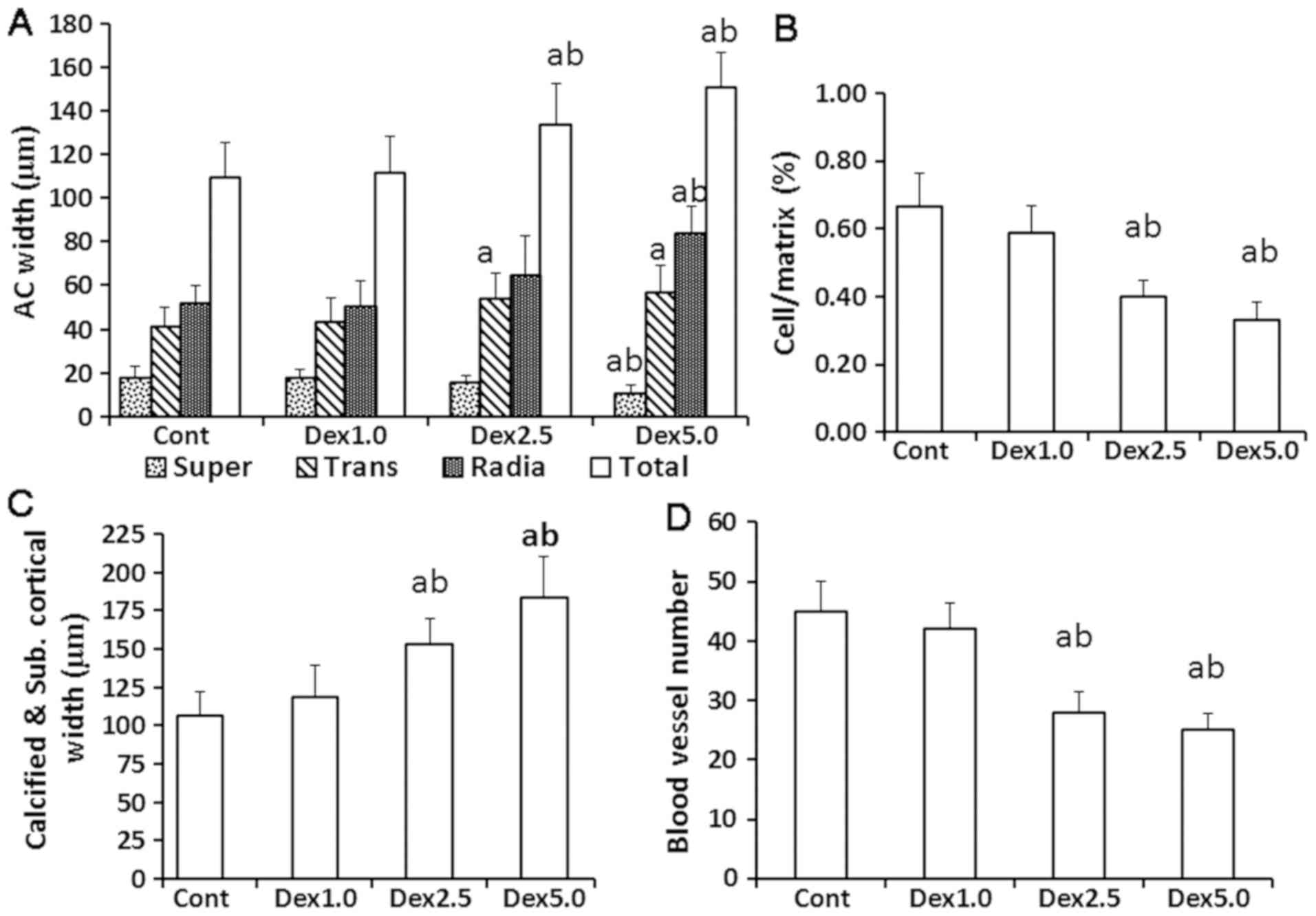 | Figure 2.Parameters of the AC and subchondral
zone from rats treated with vehicle or three doses of Dex. (A)
Comparison of the AC width in each group. (B) Cell/matrix volume
ratio of the AC zones in each group. (C) Calcified and subchondral
cortical plate width changes in the subchondral zone in each group.
(D) Number of blood vessels within the subchondral cortical plate
in each group. aP<0.05 vs. Cont;
bP<0.05 vs. Dex1.0. Dex, dexamethasone; Cont, control
group; Dex1.0, Dex 1.0 mg/kg group; Dex2.5, Dex 2.5 mg/kg group;
Dex5.0, Dex 5.0 mg/kg group; Super, superficial zone, Trans,
transitional zone; Radia, radial zone; Total, total AC width; AC,
articular cartilage. |
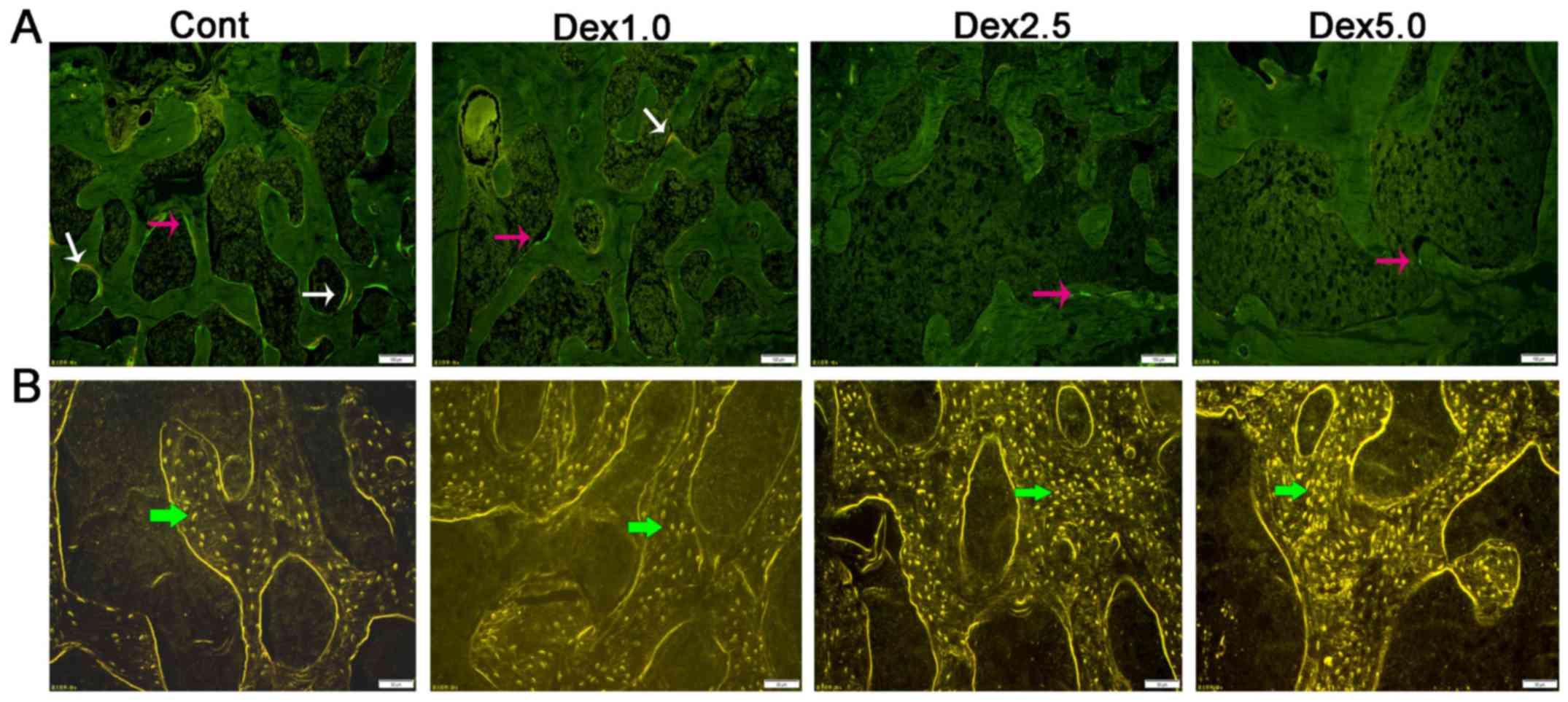
Representative images of subchondral trabecular
morphology are presented in Fig. 3.
Related parameters are presented in Table I. BV/TV, Tb.N and Tb.Th were
decreased, while Tb.Sp of the trabecular epiphysis was increased in
the Dex5.0 group compared with the control group, but Dex1.0 and
Dex2.5 were not observed to affect these parameters. BFR was
significantly and dose-dependently lower in all Dex groups. Ob.S/BS
decreased and osteocyte lacuna volume increased in the Dex2.5 and
Dex5.0 groups compared with the control group, and a greater effect
was observed for Dex5.0 compared with Dex1.0. Furthermore, Oc.S/BS
was significantly lower in the Dex5.0 group compared with the
control group. MS/BS and BFR were dose-dependently and
significantly reduced in all Dex groups compared with the control
groups. As indicated in Fig. 4, the
morphology of the osteoblasts became slender, flat and inactive
with irregular shaped giant osteoclasts, which appeared due to
increasing doses of Dex.
 | Table I.Histomorphometric parameters of the
epiphyseal trabecular bone of the tibia in rats treated with
vehicle or Dex. |
Table I.
Histomorphometric parameters of the
epiphyseal trabecular bone of the tibia in rats treated with
vehicle or Dex.
| Parameter | Cont | Dex1.0 | Dex2.5 | Dex5.0 |
|---|
| BV/TV (%) | 35.65±4.41 | 35.19±4.54 | 34.57±3.61 |
30.47±3.24a,c |
| Tb.N (N/mm) | 3.87±0.54 | 3.62±0.52 | 3.35±0.59 |
3.19±0.46a,c |
| Tb.Sp (µm) | 181.45±29.29 | 184.55±22.22 | 198.91±26.31 |
208.95±27.70a |
| Tb.Th (µm) | 102.81±7.75 | 98.93±4.54 | 95.67±7.84 |
87.56±5.19a,c |
| MS/BS (%) | 17.40±2.52 |
11.24±4.52b |
7.81±2.84b,c |
5.70±2.01b,d |
| BFR/BS
(µm)/d*100) | 19.15±2.73 |
12.65±4.74b |
7.62±2.55b,c |
5.48±2.06b,d |
| BFR/TV (%/year) | 48.85±8.97 |
33.64±12.12b |
22.90±6.58b,c |
15.45±4.01b,d |
| Ob.S/BS | 0.87±0.12 | 0.71±0.11 |
0.55±0.08a |
0.32±0.05b,d |
| Oc.S/BS | 0.88±0.15 | 0.75±0.16 | 0.65±0.17 |
0.62±0.20a |
| Osteocyte.V/TV | 2.11±0.02 | 3.04±0.05 |
7.56±0.10b,c |
8.45±0.14b,d |
Discussion
Osteoporosis and osteonecrosis of the femoral head
are the two most common adverse reactions associated with
glucocorticoid use (12). Currently,
it is accepted that glucocorticoids directly and simultaneously
influence articular cartilage as well as bone tissue, as it has
been demonstrated that both structures have glucocorticoid
receptors (13,14). Both the articular cartilage and its
adjacent bone are inevitably damaged during osteonecrosis of the
femoral head. The current results indicate that Dex has a
dose-dependent detrimental effect on the articular cartilage of the
knee and the subchondral bone. At a given level of glucocorticoid
exposure, the degree of damage to the articular cartilage was lower
compared with that observed in subchondral bone and did not show
obvious degeneration. In addition, the subchondral bone underwent
unbalanced remodeling and osteopenia resulting from severely
impeded bone formation that exceeded the reduction in bone
resorption.
Articular cartilage, similar to bone, is essential
for the normal functioning of joints and the skeletal system
(15). The tibia articular cartilage
is divided into four zones. While the superficial zone provides a
gliding function and behaves as a visco-elastic and hyper-elastic
material going through fast deformations during loading, the
transitional and radial zones support weight and distribute stress
across the cartilage to the subchondral bone (16,17). The
calcified cartilage zone, the thickness of which is linearly
related to the degree of degeneration of the non-calcified zone,
undergoes a transition that transforms the shear force into
pressure and tension and then spreads it to the subchondral layer
(18). Previous studies have
demonstrated that excessive glucocorticoid treatment alters the
cartilage chondrocyte metabolism, induces apoptosis and changes the
intra-articular environment, in addition to inhibiting the
synthesis of the extracellular matrix (19). However, the current study revealed
that a greater thickness of the articular cartilage attributed to a
greater proportion of extracellular matrix in the transitional and
radial zones, as the cell/matrix volume ration in the articular
cartilage was decreased. This observation implies that the increase
in extracellular matrix may be a compensatory mechanism that serves
to maintain joint function while redistributing stress across the
cartilage (20,21), rather than a direct reaction to
glucocorticoid therapy. Extracellular matrix is mainly secreted by
chondrocytes. As the main cells of the articular cartilage,
chondrocytes with similar cell and matrix morphologies perform
similar biomechanical functions. Previous results have indicated
that glucocorticoids inhibit the differentiation and proliferation
of chondrocytes and promote their apoptosis (22). Chondrocytes in the hypertrophic or
deep zone are most vulnerable to attack as the effects of
glucocorticoids highly depend on the activation and differential
stage of the cells targeted in the joint (23). In the current study, the
morphological changes of the radial layer chondrocytes were
observed, which supported this theory. Another reasonable
explanation for thicker articular cartilage is that extracellular
matrix has not yet calcified, which corresponds well with the
observed decrease in blood vessels in the subcostal cortical plate.
Decreased angiogenesis is considered an important pathological
change and an etiological factor during the development of
osteonecrosis of the femoral head (24,25). The
reduction in nutrient supply to the calcified layer of the
articular cartilage would also lead to articular cartilage
degeneration.
At an identical dose of Dex, damage to the
subchondral bone was greater than that observed in the articular
cartilage. Furthermore, bone formation was the most sensitive
indicator of bone reaction to glucocorticoid. A previous study
demonstrated that the role of the subchondral bone during
development of osteonecrosis of the femoral head has been
underestimated, since a subchondral bone lesion is the first event
that leads to the subsequent collapse of the femoral head (26). In osteonecrosis, cells of the
trabecular bone, including osteoblasts, osteocytes and osteoclasts,
spontaneously die, resulting in fracture and collapse of the
articular surface in the femoral head (27). Both in vivo and in
vitro experiments have corroborated that glucocorticoids
directly inhibit osteoblast differentiation and function, and
induce osteoblast apoptosis, which results in rapid and profound
suppression of bone formation (28,29).
Glucocorticoids also directly act on osteoclasts (30). Furthermore, the altered shape of
osteoclast resorption cavities profoundly reduces bone strength,
while the total eroded surface area remains constant (31). Osteocytes, the most abundant bone
cell type, are closely associated with systemic circulation through
the lacunar-canalicular network and play a vital role in
osteonecrosis of the femoral head (7,32).
Glucocorticoid-induced osteocyte apoptosis results in the
disruption of bone vascularity and a decrease in bone hydraulic
support, which causes a greater decline in bone strength compared
with that due to loss of bone mass. These may be important
mechanisms that underpin osteonecrosis (33). Notable, the current observations of
altered morphology of osteoblasts and osteoclasts, along with
inhibited bone turnover and an increase in osteocyte lacunae, are
all consistent with the concepts outlined above. It was
demonstrated in the current study that these developments result in
unbalanced remodeling, stressed lacunar-canalicular network and a
weakened bone microstructure.
The current study has certain limitations. First,
Dex administration was limited to only one period of 8 weeks
instead of a shorter or longer period of treatment. Second, further
experiments are required to elucidate the mechanism of articular
cartilage thickening. For instance, the expression of matrix
metalloproteinase-13, type II collagen and proteoglycans in
articular cartilage could be evaluated by immunohistochemistry or
other molecular biology methods. Furthermore, the use of
glucocorticoid antagonists, or evaluating simultaneous changes of
articular cartilage and subchondral bone in both the femoral head
and knee joint, could provide further insight into the mechanism by
which glucocorticoid influences cartilage.
In conclusion, bone formation was inhibited at a low
dose of glucocorticoid exposure, while bone resorption was reduced
at higher levels of glucocorticoid treatment in rats during a
period of 8 weeks. The latter effect was accompanied by an
increased number of apoptotic osteocytes and resulted in unbalanced
remodeling and weakened microstructure of the subchondral bone.
Damage to the articular cartilage was to a lesser degree compared
with in the subchondral bone, but morphological changes in
chondrocytes and decreased angiogenesis were indicators of
degradation of the articular cartilage.
Acknowledgements
Not applicable.
Funding
This project was funded in part by the Science and
Technology Planning Project of Guangdong Province, China (grant no.
2015A030302077).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YC conceived the study, performed the animal
experiments, analyzed data and prepared the manuscript. JZ
contributed to the animal experiments and histomorphometry
analyses. LH prepared the un-decalcified bone tissue sections. All
authors read and approved the final manuscript for publication.
Ethics approval and consent to
participate
All animal experiments were approved by the Academic
Committee on the Ethics of Animal Experiments of the Guangdong
Medical University, Zhanjiang, China [permit no. SYXK (GUANGDONG)
A2008036].
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Whittier X and Saag KG:
Glucocorticoid-induced osteoporosis. Rheum Dis Clin North Am.
42177–189. (x)2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cao H, Guan H, Lai Y, Qin L and Wang X:
Review of various treatment options and potential therapies for
osteonecrosis of the femoral head. J Orthop Translat. 4:57–70.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gong LL, Fang LH, Wang HY, Peng JH, Si K,
Zhu J, Han FF, Wang YH, Du GH, Pei LX and Liu LH: Genetic risk
factors for glucocorticoid-induced osteonecrosis: A meta-analysis.
Steroids. 78:401–408. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xie XH, Wang XL, Yang HL, Zhao DW and Qin
L: Steroid-associated osteonecrosis: Epidemiology, pathophysiology,
animal model, prevention, and potential treatments (an overview). J
Orthop Translat. 3:58–70. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Weinstein RS: Glucocorticoid-induced
osteonecrosis. Endocrine. 41:183–190. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu R, Liu Q, Wang K, Dang X and Zhang F:
Comparative analysis of gene expression profiles in normal hip
human cartilage and cartilage from patients with necrosis of the
femoral head. Arthritis Res Ther. 18:982016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Weinstein RS, Hogan EA, Borrelli MJ,
Liachenko S, O'Brien CA and Manolagas SC: The pathophysiological
sequence of glucocorticoid-induced osteonecrosis of the femoral
head in male mice. Endocrinology. 158:3817–3831. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dong YL, Zhou L, Li YL, Xiao K and Weng
XS: Establishment and assessment of rat models of
glucocorticoid-induced osteonecrosis. Zhongguo Yi Xue Ke Xue Yuan
Xue Bao. 37:152–156. 2015.PubMed/NCBI
|
|
9
|
Wang D, Miller SC, Liu XM, Anderson B,
Wang XS and Goldring SR: Novel dexamethasone-HPMA copolymer
conjugate and its potential application in treatment of rheumatoid
arthritis. Arthritis Res Ther. 9:R22007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rentsch C, Schneiders W, Manthey S,
Rentsch B and Rammelt S: Comprehensive histological evaluation of
bone implants. Biomatter 4. pii. e279932014.
|
|
11
|
Dempster DW, Compston JE, Drezner MK,
Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR
and Parfitt AM: Standardized nomenclature, symbols, and units for
bone histomorphometry: A 2012 update of the report of the ASBMR
histomorphometry nomenclature committee. J Bone Miner Res. 28:2–17.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Moghadam-Kia S and Werth VP: Prevention
and treatment of systemic glucocorticoid side effects. Int J
Dermatol. 49:239–248. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tu J, Stoner S, Fromm PD, Wang T, Chen D,
Tuckermann J, Cooper MS, Seibel MJ and Zhou H: Endogenous
glucocorticoid signaling in chondrocytes attenuates joint
inflammation and damage. FASEB J. 32:478–487. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gu Y, Zhou J, Wang Q, Fan W and Yin G:
Ginsenoside Rg1 promotes osteogenic differentiation of rBMSCs and
healing of rat tibial fractures through regulation of GR-dependent
BMP-2/SMAD signaling. Sci Rep. 6:252822016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goetzen M, Hofmann-Fliri L, Arens D,
Zeiter S, Stadelmann V, Nehrbass D, Richards RG and Blauth M: Does
metaphyseal cement augmentation in fracture management influence
the adjacent subchondral bone and joint cartilage?: An in vivo
study in sheep stifle joints. Medicine (Baltimore). 94:e4142015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Neumann AJ, Gardner OF, Williams R, Alini
M, Archer CW and Stoddart MJ: Human articular cartilage progenitor
cells are responsive to mechanical stimulation and
adenoviral-mediated overexpression of bone-morphogenetic protein 2.
PLoS One. 10:e01362292015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Grogan SP, Duffy SF, Pauli C, Koziol JA,
Su AI, D'Lima DD and Lotz MK: Zone-specific gene expression
patterns in articular cartilage. Arthritis Rheum. 65:418–428. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Findlay DM and Kuliwaba JS: Bone-cartilage
crosstalk: A conversation for understanding osteoarthritis. Bone
Res. 4:160282016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu N, Wang W, Zhao Z, Zhang T and Song Y:
Autophagy in human articular chondrocytes is cytoprotective
following glucocorticoid stimulation. Mol Med Rep. 9:2166–2172.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tomaszewska E, Dobrowolski P and Puzio I:
Morphological changes of the cartilage and bone in newborn piglets
evoked by experimentally induced glucocorticoid excess during
pregnancy. J Anim Physiol Anim Nutr (Berl). 97:785–796. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Grogan SP, Duffy SF, Pauli C, Koziol JA,
Su AI, D'Lima DD and Lotz MK: Zone-specific gene expression
patterns in articular cartilage. Arthritis Rheum. 65:418–428. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang M, Shi CY, Zhou ZL and Hou JF: Bone
characteristics, histopathology, and chondrocyte apoptosis in
femoral head necrosis induced by glucocorticoid in broilers. Poult
Sci. 96:1609–1614. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Madsen SH, Andreassen KV, Christensen ST,
Karsdal MA, Sverdrup FM, Bay-Jensen AC and Henriksen K:
Glucocorticoids exert context-dependent effects on cells of the
joint in vitro. Steroids. 76:1474–1482. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang YL, Yin JH, Ding H, Zhang W, Zhang
CQ and Gao YS: Vitamin K2 prevents glucocorticoid-induced
osteonecrosis of the femoral head in rats. Int J Biol Sci.
12:347–358. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Weinstein RS, Wan C, Liu Q, Wang Y,
Almeida M, O'Brien CA, Thostenson J, Roberson PK, Boskey AL,
Clemens TL and Manolagas SC: Endogenous glucocorticoids decrease
skeletal angiogenesis, vascularity, hydration, and strength in aged
mice. Aging Cell. 9:147–161. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang L, Zhang L, Pan H, Peng S, Zhao X and
Lu WW: Abnormal subchondral bone microstructure following steroid
administration is involved in the early pathogenesis of
steroid-induced osteonecrosis. Osteoporos Int. 27:153–159. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Briot K and Roux C: Glucocorticoid-induced
osteoporosis. RMD Open. 1:e0000142015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Z, Xue J, Shen T, Ba G, Yu D and Fu
Q: Curcumin alleviates glucocorticoid-induced osteoporosis by
protecting osteoblasts from apoptosis in vivo and in vitro. Clin
Exp Pharmacol Physiol. 43:268–276. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Koromila T, Baniwal SK, Song YS, Martin A,
Xiong J and Frenkel B: Glucocorticoids antagonize RUNX2 during
osteoblast differentiation in cultures of ST2 pluripotent
mesenchymal cells. J Cell Biochem. 115:27–33. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Teitelbaum SL: Glucocorticoids and the
osteoclast. Clin Exp Rheumatol 33 (4 Suppl 92). S37–S39. 2015.
|
|
31
|
Vanderoost J, Søe K, Merrild DM, Delaissé
JM and van Lenthe GH: Glucocorticoid-induced changes in the
geometry of osteoclast resorption cavities affect trabecular bone
stiffness. Calcif Tissue Int. 92:240–250. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yao W, Dai W, Jiang JX and Lane NE:
Glucocorticoids and osteocyte autophagy. Bone. 54:279–284. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jia J, Yao W, Guan M, Dai W, Shahnazari M,
Kar R, Bonewald L, Jiang JX and Lane NE: Glucocorticoid dose
determines osteocyte cell fate. FASEB J. 25:3366–3376. 2011.
View Article : Google Scholar : PubMed/NCBI
|