Introduction
Organizing pneumonia (OP) is a pulmonary disorder
that is associated with nonspecific clinical presentations, chest
radiographic findings and pulmonary function results (1). OP is divided into primary and
secondary OP based on etiology. Primary OP is referred to as
cryptogenic organizing pneumonia (COP) and classified as an
idiopathic interstitial pneumonia (1,2).
Secondary OP is associated with a number of entities, including
drugs, infections, malignancies, connective tissue diseases, organ
transplantation, radiotherapy and the inhalation of harmful gases.
COP mainly involves the alveoli, alveolar ducts and small airways;
however, the lung interstitium may also be involved. It is
considered as an inflammatory disease and diagnosed based on the
clinical, radiographic and pathological findings following the
exclusion of diseases associated with secondary OP (3). Glucocorticoids are effective in the
treatment of COP. However, glucocorticoids usually take a longer
time to take effect, and this results in severe side-effects.
Macrolides, a class of antimicrobial agents first
isolated from Streptomyces erythreus more than five decades
ago, are widely used to treat infectious respiratory diseases in
humans (4). In addition to the
anti-infectious effect, macrolides have been reported to have
anti-inflammatory effects on certain inflammatory respiratory
diseases, including asthma, bronchiectasis and cystic fibrosis (CF)
(4). Studies have shown low-dose
macrolides to be efficient in the treatment of COP (5–7).
However, those studies are limited to case-based reports. There is
a lack of controlled comprehensive clinical trials and definitive
recommendations. The present study reports a case of COP that was
effectively treated with azithromycin in combination with a
glucocorticoid. A search of the literature was carried out in
Medline, using the keywords ‘macrolide OR azithromycin OR
erythromycin OR roxithromycin OR clarithromycin’ AND ‘cryptogenic
organizing pneumonitis OR bronchiolitis obliterating organizing
pneumonia’. A total of 35 articles were retrieved by December 2012.
After excluding unrelated and repetitive articles, eight papers
were selected for analysis. A review of 35 cases of
OP/COP/bronchiolitis obliterans organizing pneumonia (BOOP) treated
with macrolide antibiotics, from these papers and including the
current case, was conducted.
Case report
A 58 year-old female patient was admitted to the
Affiliated Hospital of Ningbo University School of Medicine
(Ningbo, China) with a nine-month history of concurrent cough,
intermittent mild fever and fatigue. Prior to coming to the
hospital, the patient had been treated with cephalosporins,
quinolones and macrolides in other hospitals and the symptoms had
not improved. The patient had been hypertensive for more than 10
years and was taking nifedipine orally to maintain a normal blood
pressure. Physical examination revealed crackles in both lungs. The
examination was otherwise normal, with no signs of connective
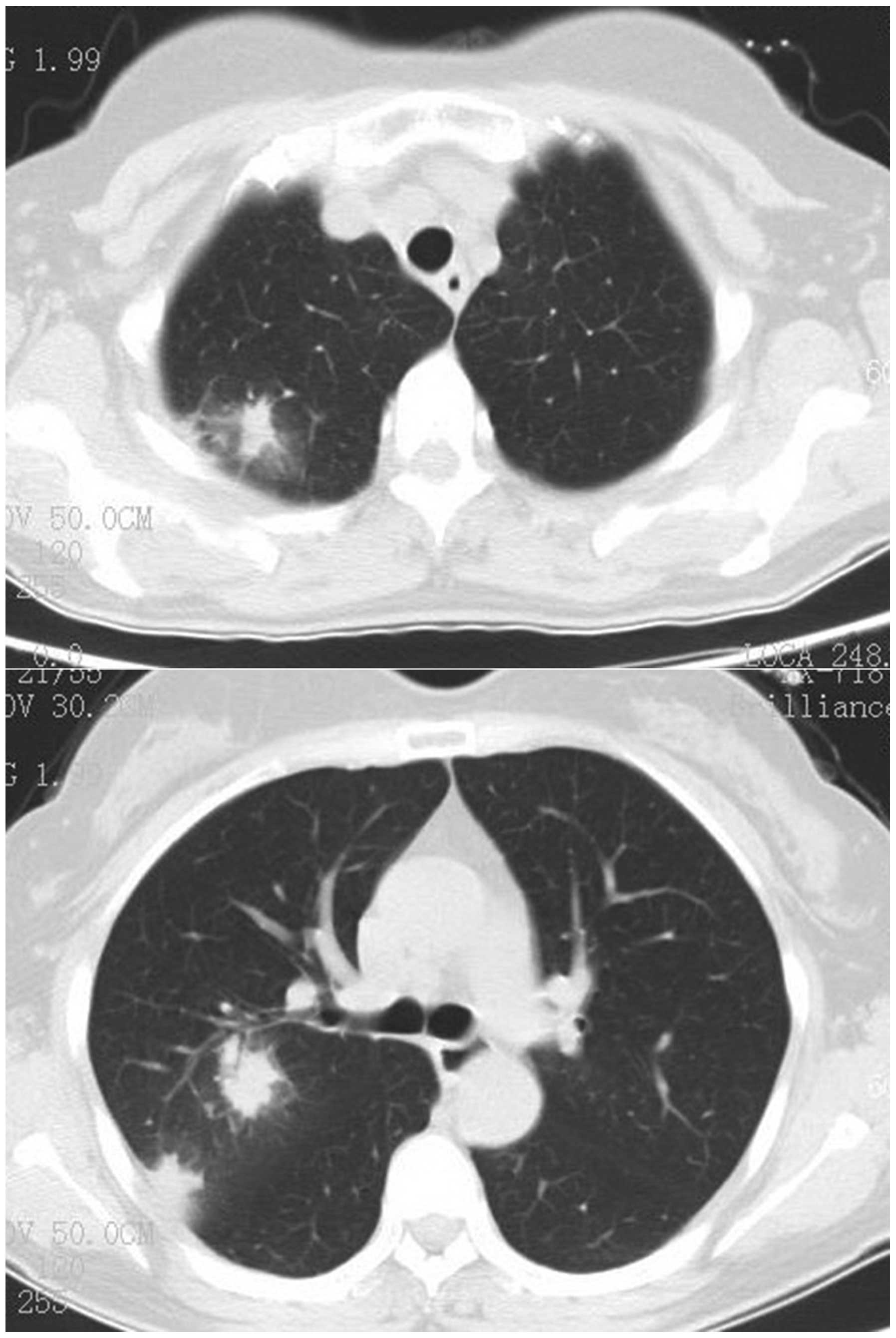
tissue disorders. Chest computed tomography (CT) scanning showed
bilateral nodular, patchy alveolar opacities, prominently in the
right lung, and thickened pleura (Fig.
1). Laboratory tests showed a white blood cell (WBC) count of
8.3×109/l, a neutrophil percentage of 63%, eosinophil
percentage of 0.7%, red blood cell count of 4.46×1012/l,
hemoglobin concentration of 116 g/l, platelet count of
369×109/l, erythrocyte sedimentation rate of 112 mm/h
and C-reactive protein level of 9.1 mg/l. Hepatic and renal
function were normal. The serum anti-mycoplasma antibody titer was
1:80. The anti-double stranded DNA titer was 136 μg/l, the
immunoglobulin E level was 41.58 kIU/l and the anti-paragonimiasis
antibody test was negative. Immunological examinations were all
normal. Perinuclear anti-neutrophil cytoplasmic antibody (P-ANCA)
and cytoplasmic-ANCA tests were negative, and the tumor markers
CA19-9, CA-125, carcinoembryonic antigen, neuron-specific enolase
and CYFRA21-1 were normal. The blood gas pH was 7.41, the partial
pressure of CO2 in arterial blood (PaCO2) was
39 mmHg, the PaO2 was 96 mmHg and the arterial oxygen
saturation (SaO2) was 98%. Sputum culture was negative.
Pulmonary function tests indicated small airway dysfunction.
Bronchoscopy revealed a normal tracheal mucosa and lumen. A test of
bronchoalveolar lavage fluid (BALF) showed no exfoliated cells. The
cell types were 2.4% neutrophils, 0% eosinophilic granulocytes,
82.3% macrophages and 15.3% lymphocytes. Transbronchial needle
aspiration did not detect cancer cells. The patient was initially
considered to have community acquired pneumonia and was treated
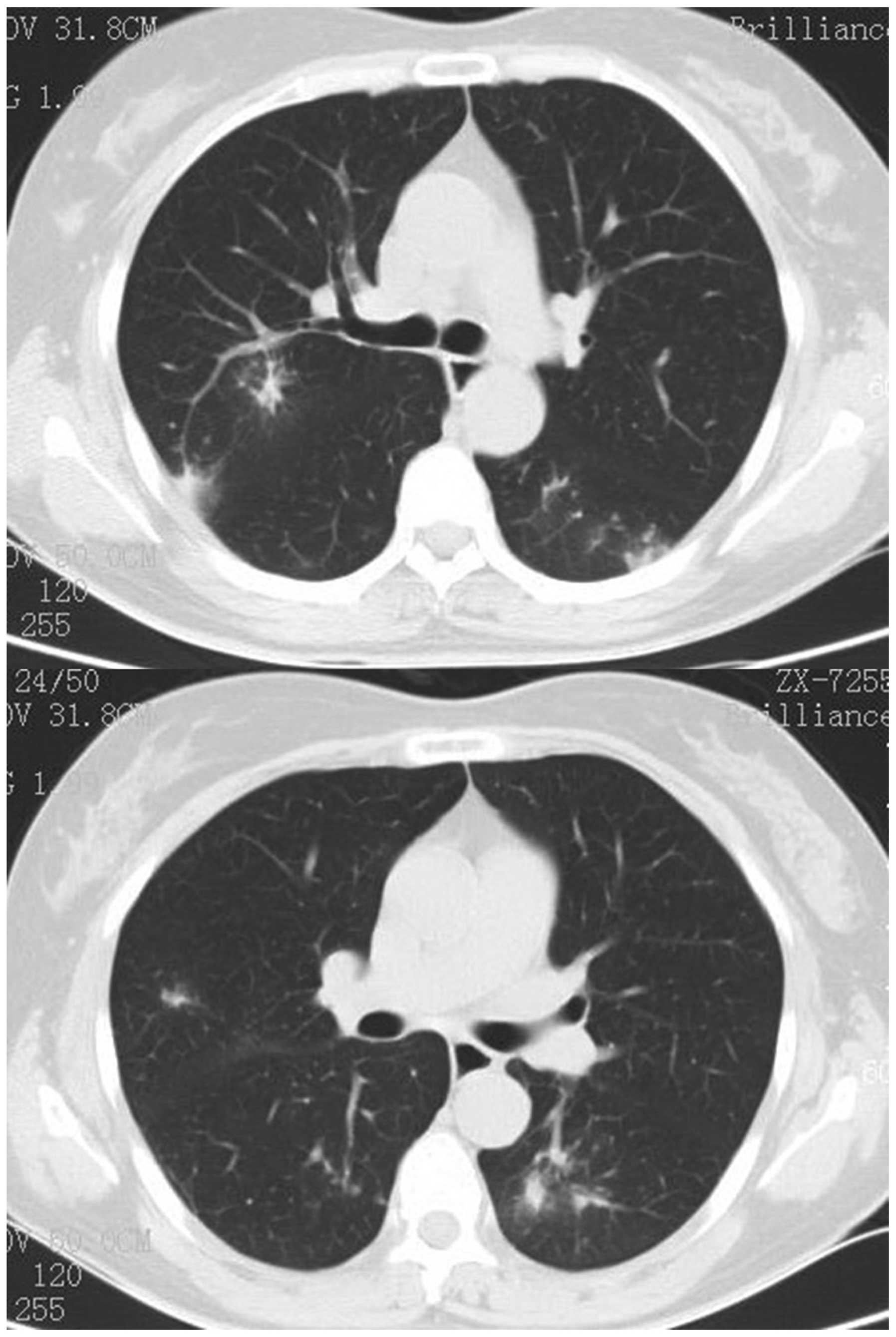
with moxifloxacin (0.4 g, intravenous drip, daily). Ten days later,
a chest CT scan demonstrated that the lesions on the right upper
lung were slightly absorbed; however, there were new nodular and
patchy ground glass opacities in the left lung (Fig. 2). A percutaneous lung biopsy in the
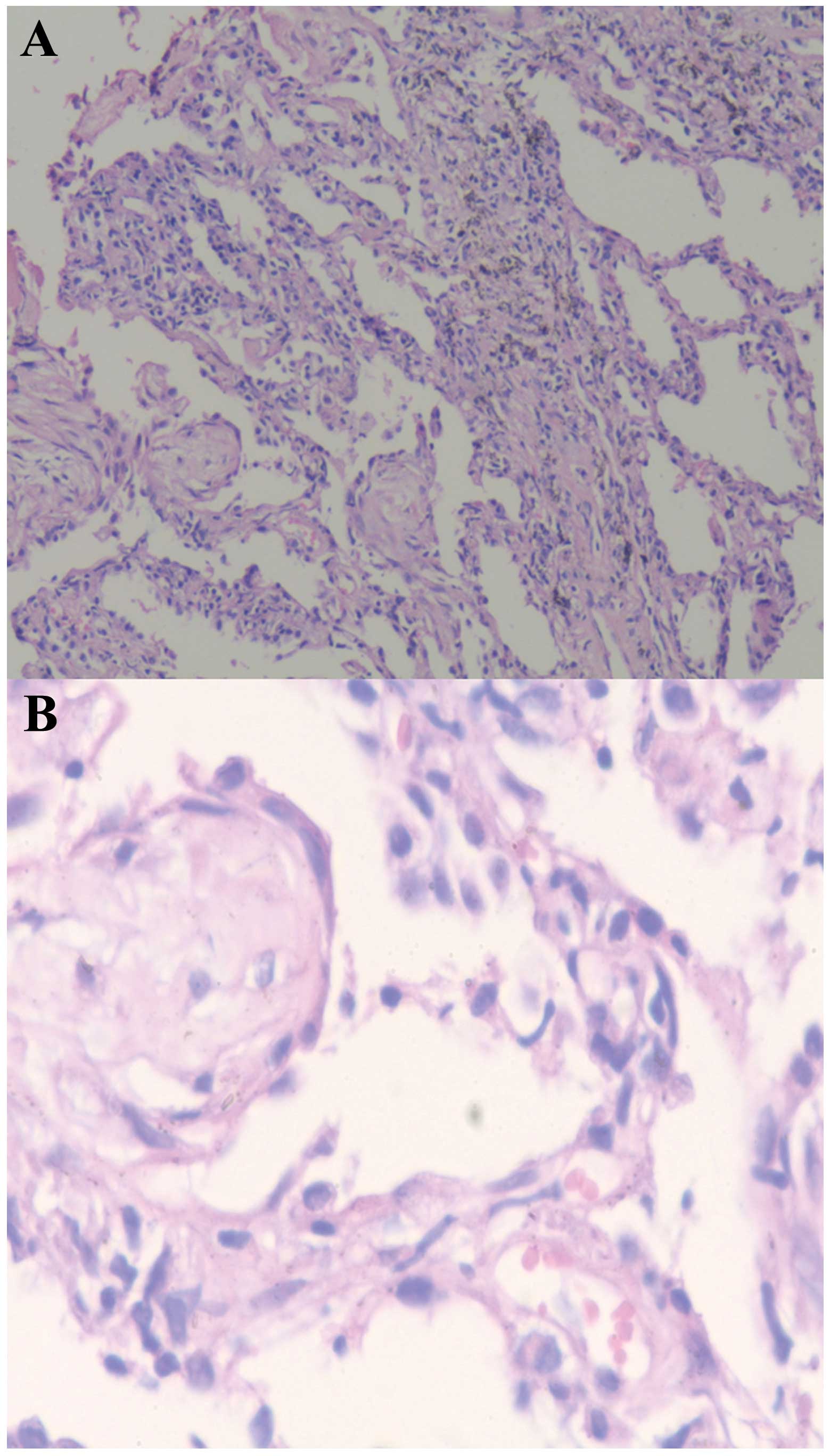
lower left lung was performed. The pathologic examination
identified typical characteristics of OP. The alveoli and alveolar
ducts were filled with plugs of granulation tissue composed of
fibroblasts. Chronic inflammatory cell infiltration and a few
scattered giant cells were found in these tissue sections (Fig. 3). The patient was treated with 0.75
mg/kg/day of prednisone orally. Two weeks later, respiratory
symptoms disappeared and chest radiographic abnormalities were
improved. After another 2 weeks of prednisone treatment, the
patient complained of gastrointestinal discomfort. Thus, 500 mg/day
of azithromycin was added to the treatment, and the dose of
prednisone was gradually reduced. Three months later, prednisone
was completely withdrawn. The patient was continually given
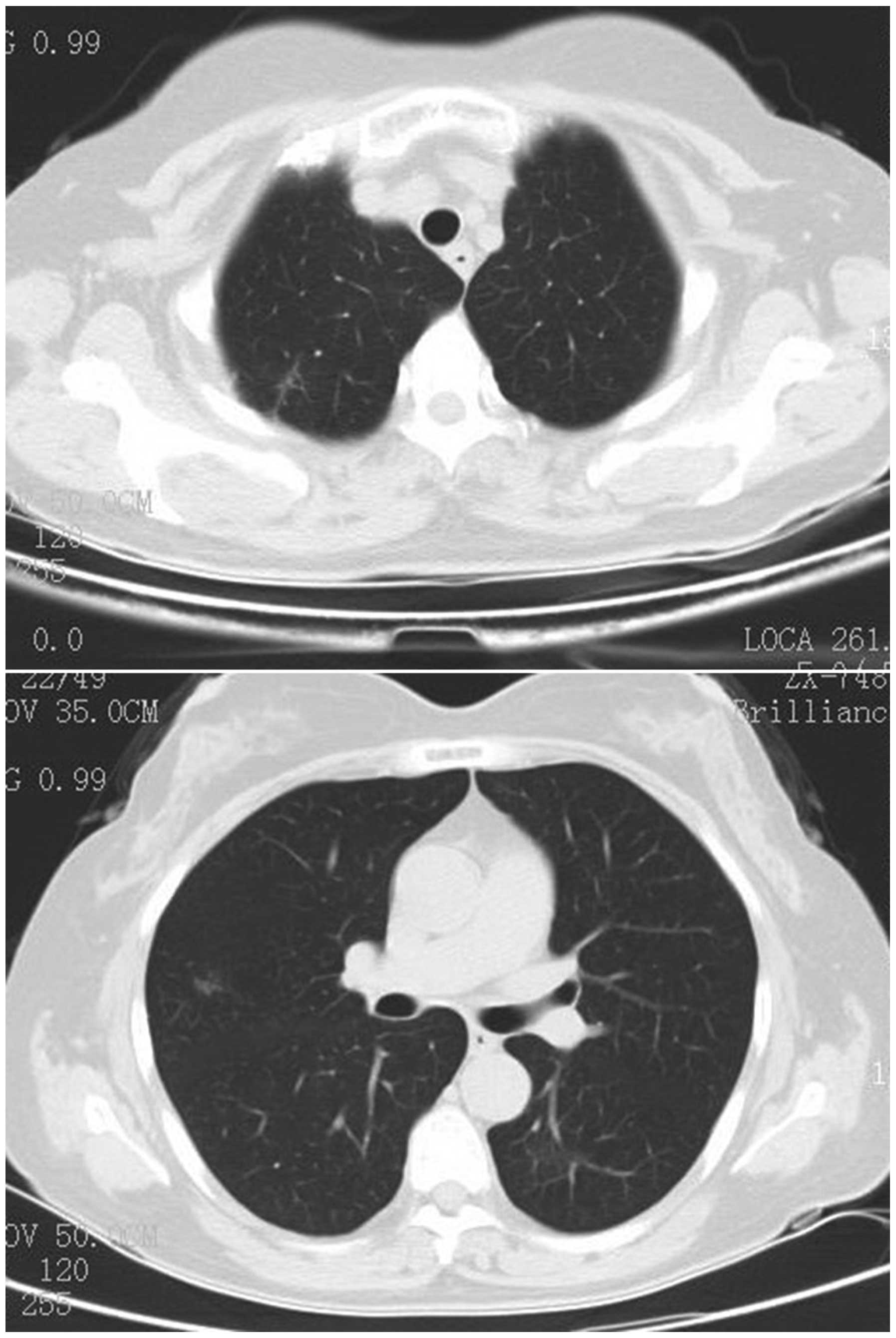
azithromycin at 500 mg/day for another three months. A chest CT
scan showed a complete resolution of the previous bilateral patchy,
nodular consolidations in both lungs (Fig. 4). The patient was followed-up for
one year, and the disease did not relapse. Informed consent was
obtained from the patient.
Discussion
COP is a type of organizing pneumonia without the
presence of evident pathogens, such as infection, or other
associated diseases, such as connective tissue disease. COP is
commonly observed in the non-smoking population and predominantly
in female patients. In the present review of 35 cases of
OP/COP/BOOP, there were 12 male and 23 female patients. Their ages
were between 13 and 83 years. Radzikowska et al (6) reported that 10/12 patients were
non-smokers, and 9/12 were female patients. In the cases covered in
the current review, there were two smokers, four ex-smokers and 14
non-smokers; the smoking history of the remaining nine patients was
not mentioned in the papers. There were 23 cases of primary COP and
six cases of secondary COP. Three cases were associated with
radiotherapy, and the other three cases were associated with
amiodarone, chemotherapy and bone marrow transplantation,
respectively. None of them had family history of COP.
COP patients usually do not show unique clinical
presentations. Among the 35 reviewed cases, 29 patients had certain
types of symptoms; the symptoms of the other six patients were not
specified. The most common symptoms were cough (24/29), shortness
of breath (18/29), light fever (16/29), fatigue (15/29), weight
loss (11/29) and night sweats (6/29; Table I). The complications included
pneumothorax in one case (5), and
mediastinal emphysema and pneumothorax in one case (4). The interval time from onset of
symptoms to diagnosis was variable, with the longest being a 5-year
medical history for a 60-year-old female patient. During these 5
years, the patient repeatedly presented with fever, cough and
shortness of breath. The patient was initially diagnosed with
asthma, and was pathologically diagnosed with COP through
percutaneous lung biopsy (7).
Physical examinations were usually normal in these patients. Nine
out of 29 patients had lung wheezing, and two had lung crackles.
The majority of the patients had mild illnesses; only one patient
had acute onset of illness, and the illness rapidly progressed
following prednisone treatment, and had complications of
pneumomediastinum and pneumothorax. The disease was improved after
the patient was given macrolide in combination with
methylprednisolone and cyclosporine (8).
 | Table IClinical characteristics of patients
with COP. |
Table I
Clinical characteristics of patients
with COP.
| Characteristics | No. of cases | Percentage of
totala |
|---|
| Gender |
| Male | 12 | |
| Female | 23 | |
| Age |
| 13–83 years | 35 | |
| Smoking |
| Never | 14/20 | 70 |
| Ex-smoker | 4/20 | 20 |
| Smoker | 2/20 | 10 |
| COP |
| Primary | 24 | 82.8 |
| Secondary | 5 | 17.2 |
| Symptoms |
| Cough | 24 | 82.8 |
| Dyspnea | 18 | 62.1 |
| Low-grade fever | 16 | 55.2 |
| Weight loss | 11 | 37.9 |
| Fatigue | 15 | 51.7 |
| Night sweats | 6 | 20.7 |
| Lung signs |
| Crackles | 2 | 6.9 |
| Wheezing | 9 | 31 |
| Chest radiograph |
| Normal | | 6 |
| Abnormal | | 29 |
| Patchy
consolidation | 21 | 72.4 |
| Bilateral | 28 | 96.6 |
| Multiple
nodules | 5 | 17.2 |
| Pleural
effusion | 2 | 6.9 |
| Migratory
lesions | 11 | 37.9 |
| Ground glass
opacities | 5 | 17.2 |
| Air bronchogram | 16 | 55.2 |
| Lung biopsy |
| TBLB | 13 | 44.8 |
| Thoracoscopy | 5 | 17.3 |
| Percutaneous lung
biopsy | 4 | 13.8 |
| Surgery | 7 | 24.1 |
| Macrolide |
| Alone | 5 | 82.8 |
| Adjunctive | 24 | 17.2 |
| Efficacy |
| Effective | 24 | 82.8 |
| Invalid | 5 | 17.2 |
The majority of the patients had abnormal chest
radiographic findings. The most common manifestations were multiple
patchy opacities (21/29), air bronchogram (16/29), multiple lung
nodules (5/29), ground glass opacity (5/29), multiple consolidation
(2/29) and single consolidation (3/29; Table I). The most common feature in the
chest radiography of patients with COP was a migratory pattern. It
existed in 9/12 patients in a single study (75%) (6). In the present review, it was observed
in 37.9% of patients (11/29). The majority of the lesions involved
bilateral lungs; both right and left lungs were involved in 28
cases. Pleural effusion and lymphadenopathy were rare. The
radiographic findings were variable in OP, and the differentiation
of OP from other pulmonary diseases is challenging. Lung biopsy is
extremely important to the diagnosis of OP. All 35 patients were
diagnosed by either cytology or pathology. Transbronchial lung
biopsy (TBLB) was the most frequently used technique, and it had
the highest diagnostic value among all methods. Thirteen out of 15
patients were diagnosed through TBLB. TBLB failed to diagnose the
remaining two cases, which were diagnosed through thoracoscopy.
Four cases were diagnosed through percutaneous lung biopsy, one of
them was confirmed at the second examination. Seven patients were
confirmed by surgery and three were confirmed by thoracoscopy.
Surgical intervention is not recommended as the first choice due to
its invasiveness. TBLB is strongly recommended as a routine
diagnostic technique for COP patients.
COP is considered to be an inflammatory disease.
BALF cytological examination demonstrated increased lymphocyte
counts, decreased CD4/CD8 ratio and increased
CD8+CD11b− cell levels (9). In this review, BALF cytological
classification was dominated by lymphocytes (8/16; 50%). Cai et
al (10) observed that the
cytokines interleukin (IL)-6, -8, and -10, interferon-γ-inducible
protein 10, tumor necrosis factor (TNF)-α, soluble TNF receptor 1
(STNFR1) and STNFR2 in BALF were significantly increased in COP
patients, and macrolides significantly decreased their levels. The
proportions of lymphocytes, neutrophils and
CD8+CD11b− cells were significantly decreased
following macrolide treatment (10). This suggests that increased
lymphocyte counts and numbers of CD8+CD11b−
cells in BALF have diagnostic implications for COP.
Glucocorticoids are traditionally a first-line agent
for treating COP. The majority of patients respond well to
treatment (3). However, one study
reported that 10–15% of patients were resistant to treatment and
the disease progressed rapidly (11). A total of 13–58% of patients had
recurrent disease during the reduction of glucocorticoids or
following drug discontinuation (11). Macrolides, as regulators of immune
responses, have been widely used in bronchial asthma,
bronchiectasis, diffuse panbronchiolitis and other diseases. They
have also been reported to effectively treat COP (6–8,10,12–14).
In the current review, all 35 patients received macrolide
treatment, including six cases with unknown clinical efficacy. The
efficacy was assessed in the remaining 29 patients. Twenty patients
initially received macrolide as a single agent. Four-fifths of the
patients (16 cases) were cured with the medication after 3–14
months; however, the improvement took a longer time than that of
glucocorticoids. It usually took 2–3 weeks for symptom improvement
and 1 month for radiological improvement on chest images. One-fifth
of the patients (four cases) had no improvement following macrolide
treatment for 1 month and had to switch to glucocorticoids or a
combination treatment with glucocorticoids. After that, the disease
was well-controlled. The most commonly used macrolide was
clarithromycin (19 cases), the second was erythromycin (seven
cases), and the next was azithromycin (two cases). The type of
macrolide used was undocumented in one case. Nine patients were
later treated with macrolide due to poor efficacy or side-effects
from glucocorticoids. Following the addition of macrolide, the
symptoms in these patients were significantly improved (Table II). There was one patient with
severe COP in whom the disease continued to deteriorate during
glucocorticoid treatment. Following treatment with a combination of
cytotoxic drugs and macrolide, the disease attenuated rapidly
(8). Side-effects of macrolide
treatment were rare. There was only one patient who had a skin rash
resulting from clarithromycin, and later this drug was stopped
(14).
 | Table IICases of OP/COP/BOOP treated with
macrolide. |
Table II
Cases of OP/COP/BOOP treated with
macrolide.
| Reference | Year | No. of patients | Gender | Age (years) | Diagnosis | Macrolide | Regimen | Efficacy |
|---|
| Cai et al
(10) | 2013 | 6 | 1F/5M | 64±2 | BOOP | CAM or AZM | Unknown | Unknown |
| Chang et al
(5) | 2012 | 1 | F | 37 | COP | CAM | Adjunctive | Effective |
| Vaz et al
(7) | 2011 | 1 | F | 60 | COP | AZM | Adjunctive | Effective |
| Lee et al (8) | 2011 | 1 | F | 38 | COP | Macrolide | Adjunctive | Effective |
| Radzikowska et
al (6) | 2008 | 12 | 9F/3M | 44–71 | OP | CAM | Single | Effective 9;
invalid 3 |
| Stover et al
(14) | 2005 | 6 | M | 72 | OP | CAM | Single | Effective |
| | | M | 76 | OP | CAM | Single | Effective |
| | | F | 65 | OP | CAM | Single | Invalid |
| | | F | 56 | BOOP | CAM | Single | Effective |
| | | F | 62 | BOOP | CAM | Single | Effective |
| | | M | 67 | BOOP | CAM | Single | Invalid |
| Ishii et al
(13) | 2000 | 1 | M | 13 | BOOP | EM | Adjunctive | Effective |
| Ichikawa et
al (12) | 1993 | 6 | | 52±21.8 | | | | |
| | | F | 47 | BOOP | EM | Single | Effective |
| | | F | 57 | BOOP | EM | Single | Effective |
| | | F | 64 | BOOP | EM | Single | Effective |
| | | F | 83 | BOOP | EM | Single | Effective |
| | | F | 43 | BOOP | EM | Single | Effective |
| | | F | 18 | BOOP | EM | Single | Effective |
| Present case | 2013 | 1 | F | 58 | COP | AZM | Adjunctive | Effective |
The molecular mechanism of macrolides in the
treatment of COP is not fully understood. Pathologically, COP is
mainly manifested as a polypoid granulation hyperplasia in the
small airway and alveolar respiratory bronchioles. The granulation
tissue is composed of fibroblasts/myofibroblasts, infiltrated with
inflammatory cells, including monocytes, macrophages, mast cells, a
few eosinophils and neutrophils, particularly in the early stage of
the disease. Studies have shown that macrolides exhibit
anti-inflammatory effects (15–20).
They have been widely used in a variety of acute and chronic
respiratory diseases and are effective in treating these diseases.
Kudoh (21) suggested that
erythromycin significantly improved the survival rate of patients
with diffuse panbronchiolitis. Itkin and Menzel (22) demonstrated that macrolides could
lower airway hyper-responsiveness and reduce the amount of
corticosteroid used in patients with asthma. These lines of
evidence support the anti-inflammatory effect of macrolides in the
treatment of COP. The efficacy of a macrolide not only relies on
its treatment time but also its molecular structure. The 14- and
15-membered ring antibiotics have been reported to have
anti-inflammatory effects, and these antibiotics include macrolides
such as erythromycin, clarithromycin and azithromycin (23).
Based on the present analysis, it is recommended
that macrolides may be used as first-line therapeutic agents in
patients with mild COP. For patients with recurrent COP or during
the reduction of glucocorticoid dosing, it is suggested that
macrolides may be combined with steroids as an adjuvant therapy.
Prior to any definitive recommendations being made, large-scale
randomized controlled clinical trials are required.
References
|
1
|
Drakopanagiotakis F, Paschalaki K, et al:
Cryptogenic and secondary organizing pneumonia: clinical
presentation, radiographic findings, treatment response and
prognosis. Chest. 139:893–900. 2011. View Article : Google Scholar
|
|
2
|
American Thoracic Society and European
Respiratory Society. American Thoracic Society/European Respiratory
Society International Multidisciplinary Consensus Classification of
the Idiopathic Interstitial Pneumonias. This joint statement of the
American Thoracic Society (ATS) and the European Respiratory
Society (ERS) was adopted by the ATS board of directors, June 2001
and by the ERS Executive Committee, June 2001. Am J Respir Crit
Care Med. 165:277–304. 2002.
|
|
3
|
Drakopanagiotakis F, Polychronopoulos V
and Judson MA: Organizing pneumonia. Am J Med Sci. 335:34–39. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hatipoglu U and Rubinstein I: Low-dose,
long-term macrolide therapy in asthma: An overview. Clin Mol
Allergy. 2:42004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang WJ, Lee EJ, Lee SY, In KH, Kim CH,
Kim HK and Park S: Successful salvage treatment of
steroid-refractory bronchiolar COP with low-dose macrolide. Pathol
Int. 62:144–148. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Radzikowska E, Wiatr E, Gawryluk D, et al:
Organizing pneumonia - clarithromycin treatment. Pneumonol Alergol
Pol. 76:334–339. 2008.(In Polish).
|
|
7
|
Vaz AP, Morais A, Melo N, et al:
Azithromycin as an adjuvant therapy in cryptogenic organizing
pneumonia. Rev Port Pneumol. 17:186–189. 2011.(In Portuguese).
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee J, Cha SI, Park TI, Park JY, Jung TH
and Kim CH: Adjunctive effects of cyclosporine and macrolide in
rapidly progressive cryptogenic organizing pneumonia with no prompt
response to steroid. Intern Med. 50:475–479. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mukae H, Kadota J, Kohno S, Matsukura S
and Hara K: Increase of activated T-cells in BAL fluid of Japanese
patients with bronchiolitis obliterans organizing pneumonia and
chronic eosinophilic pneumonia. Chest. 108:123–128. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cai M, Bonella F, Dai H, Sarria R, Guzman
J and Costabel U: Macrolides inhibit cytokine production by
alveolar macrophages in bronchiolitis obliterans organizing
pneumonia. Immunobiology. 218:930–937. 2013. View Article : Google Scholar
|
|
11
|
Yousem SA, Lohr RH and Colby TV:
Idiopathic bronchiolitis obliterans organizing
pneumonia/cryptogenic organizing pneumonia with unfavorable
outcome: pathologic predictors. Mod Pathol. 10:864–871.
1997.PubMed/NCBI
|
|
12
|
Ichikawa Y, Ninomiya H, Katsuki M, Hotta
M, Tanaka M and Oizumi K: Low-dose/long-term erythromycin for
treatment of bronchiolitis obliterans organizing pneumonia (BOOP).
Kurume Med J. 40:65–67. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ishii T, Manabe A, Ebihara Y, Ueda T,
Yoshino H, Mitsui T, et al: Improvement in bronchiolitis obliterans
organizing pneumonia in a child after allogeneic bone marrow
transplantation by a combination of oral prednisolone and low dose
erythromycin. Bone Marrow Transplant. 26:907–910. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Stover DE and Mangino D: Macrolides: a
treatment alternative for bronchiolitis obliterans organizing
pneumonia? Chest. 128:3611–3617. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ianaro A, Ialenti A, Maffia P, Sautebin L,
Rombolà L, Carnuccio R, et al: Anti-inflammatory activity of
macrolide antibiotics. J Pharmacol Exp Ther. 292:156–163. 2000.
|
|
16
|
Luisi F, Gandolfi TD, Daudt AD, Sanvitto
JP, Pitrez PM and Pinto LA: Anti-inflammatory effects of macrolides
in childhood lung diseases. J Bras Pneumol. 38:786–796. 2012.
View Article : Google Scholar
|
|
17
|
Zarogoulidis P, Papanas N, Kioumis I,
Chatzaki E, Maltezos E and Zarogoulidis K: Macrolides: from in
vitro anti-inflammatory and immunomodulatory properties to clinical
practice in respiratory diseases. Eur J Clin Pharmacol. 68:479–503.
2012. View Article : Google Scholar
|
|
18
|
Wagner T and Burns JL: Anti-inflammatory
properties of macrolides. Pediatr Infect Dis J. 26:75–76. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Langelot M, Cellerin L and Germaud P:
Anti-inflammatory effects of macrolides: applications in lung
disease. Rev Pneumol Clin. 62:215–222. 2006.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Davidson R and Peloquin P:
Anti-inflammatory effects of the macrolides. J Otolaryngol.
31(Suppl 1): 38–40. 2002. View Article : Google Scholar
|
|
21
|
Kudoh S: Erythromycin treatment in diffuse
panbronchiolitis. Curr Opin Pulm Med. 4:116–121. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Itkin IH and Menzel ML: The use of
macrolide antibiotic substances in the treatment of asthma. J
Allergy. 45:146–162. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sharma S, Jaffe A and Dixon G:
Immunomodulatory effects of macrolide antibiotics in respiratory
disease: therapeutic implications for asthma and cystic fibrosis.
Paediatr Drugs. 9:107–118. 2007. View Article : Google Scholar : PubMed/NCBI
|