Introduction
Bronchiolitis obliterans (BO) is an inflammatory
disease of the small airways that is caused by an insult to the
lower respiratory tract. The presence of inflammation and fibrosis
of the terminal and respiratory bronchioles leads to a narrowing or
full obliteration of the airway lumen, and subsequently to the
chronic obstruction of airflow. BO is characterized by the presence
of intraluminal granulation tissue in the airways or peribronchial
fibrosis and lumen narrowing, resulting in scarring and obstruction
(1).
BO is diagnosed according to a variety of factors,
including the history of insult to the lower respiratory tract
(usually caused by infection), persistent symptoms that do not
respond to the administration of bronchodilators for two weeks,
computed tomographic (CT) findings and the exclusion of other
diseases (2). However, BO is often
undiagnosed or misdiagnosed as other childhood lung diseases, such
as wheezing syndromes.
Epidemiological factors, treatment and disease
prognosis should be clearly defined in order to reduce the
morbidity and mortality rates of the disease. The aim of the
present study was to describe the clinical and radiological
findings, and the treatment protocols, during the follow-up of
patients with BO in the Pediatric Department of the Second Hospital
of Tianjin Medical University (Tianjin, China).
Increasing evidence has demonstrated that macrolide
antibiotics exert immune-modifying properties, in addition to their
role as antimicrobials (3).
Azithromycin has been reported to be effective for long-term use in
the treatment of several chronic conditions, including
mycobacterial diseases, cystic fibrosis and asthma (4). A previous study demonstrated that
following three months of treatment with azithromycin, airway
neutrophilia was shown to decrease in patients with BO syndrome
(BOS) that had undergone a lung transplantation (5). Therefore, long-term low-dose
azithromycin therapy may offer a novel, safe therapy for patients
with BOS who have undergone a lung transplantation. To the best of
our knowledge, the present study was the first long-term study
investigating azithromycin treatment for patients with
post-infectious BO (PIBO).
Subjects and methods
Subjects
This retrospective study reviewed the clinical
records of children diagnosed with PIBO at the Second Hospital of
Tianjin Medical University between August 2010 and March 2013.
Patient gender, age at diagnosis, imaging features, etiology,
clinical course, treatment and prognosis were analyzed. The current
study was conducted in accordance with the Declaration of Helsinki
and with approval from the Ethics Committee of the Second Hospital
of Tianjin Medical University. Written informed consent was
obtained from the parents/guardians of the participants.
Clinical criteria
The clinical criteria for a diagnosis of PIBO were
as follows (6): i) Persistent
dyspnea for >6 weeks following an acute infection or acute lung
injury; ii) unresolved wheezing or a cough with no reaction to
bronchiectasis agents; iii) respiratory symptoms that were severely
disproportionate to the chest X-ray findings; iv) bronchial wall
thickening, bronchiectasis, pulmonary atelectasis or mosaic
perfusion, as observed on a pulmonary high-resolution CT (HRCT)
scan; v) obstructive ventilatory disorder observed using lung
function tests; vi) unilateral hyperlucent lung observed via a
chest radiography examination; and vii) exclusion of other
obstructive pulmonary pathologies, such as asthma, primary ciliary
dyskinesia syndrome, immune deficiency or pancreatic fibrocystic
changes.
Results
Clinical features
A total of 16 children with PIBO were identified.
All 16 cases occurred following moderate-severe pneumonia. Table I presents the clinical features of
the patients with PIBO. Of the 16 cases, 13 were male and three
were female. The median age of the patients was 20.0 months, and
ranged between 3.0 months and 6.0 years. The mean hospital stay was
28.25 days (range, 15–57 days). The initial clinical manifestations
were repeated coughing, wheezing and tachypnea following a
respiratory infection. The 16 patients exhibited varying degrees of
tachypnea; moist rales and wheezing were heard in the lung field. A
severe cough and wheezing were observed in 12 patients at the time
of admission. In addition, 14 patients had a high fever, and six
patients had a transcutaneous blood oxygen saturation of 86–91%.
The children had no family history of asthma. The disease course
varied between 7 and 31 months.
 | Table I.Clinical features of 16
post-infectious pediatric patients with bronchiolitis
obliterans. |
Table I.
Clinical features of 16
post-infectious pediatric patients with bronchiolitis
obliterans.
|
|
|
|
|
| Treatment |
|
|
|
|---|
|
|---|
| Patient | Age (month) | Gender | Predisposing
factors | Diagnostic
method | Steroid | Azithromycin | Hospital stay
(days) | Disease course
(months) | Outcomes |
|---|
| 1 | 24 | M | Mycoplasma
pneumoniae | HRCT | + | + | 39 | 20 | Exacerbation |
| 2 | 12 | M | Mycoplasma
pneumoniae | HRCT | + | + | 33 | 17 | No improvement |
| 3 | 7 | M | Adenovirus | HRCT | + | + | 54 | 13 | Improved |
| 4 | 7 | M | Adenovirus | HRCT | + | + | 57 | 13 | Improved |
| 5 | 3 | M | Adenovirus | HRCT | + | + | 22 | 13 | Improved |
| 6 | 5 | M | Unknown | HRCT | + | + | 26 | 14 | Improved |
| 7 | 36 | M | Mycoplasma
pneumoniae | HRCT | + | + | 23 | 10 | No improvement |
| 8 | 24 | M | Epstein-Barr
virus | HRCT | + | + | 19 | 7 | Improved |
| 9 | 51 | F | Mycoplasma
pneumoniae | HRCT | + | + | 16 | 26 | Improved |
| 10 | 30 | F | Mycoplasma
pneumoniae | HRCT | + | + | 15 | 12 | Improved |
| 11 | 10 | M | Adenovirus | HRCT | + | + | 28 | 18 | No improvement |
| 12 | 72 | F | Mycoplasma
pneumoniae | HRCT | + | + | 20 | 22 | Improved |
| 13 | 8 | M | Unknown | HRCT | + | + | 21 | 12 | Improved |
| 14 | 16 | M | Adenovirus | HRCT | + | + | 23 | 18 | No improvement |
| 15 | 5 | M | Adenovirus | HRCT | + | + | 30 | 31 | Exacerbation |
| 16 | 13 | M | Unknown | HRCT | + | + | 26 | 19 | Improved |
Etiological agents
The initial event that led to BO in the majority of
the children was pneumonia. The causal agent in 13 of the cases was
identified using an immunofluorescence detection kit (Thermo Fisher
Scientific, Waltham, MA, USA) on nasal-pharynx secretions at
initial events or by determining specific serum antibodies during
the later stages of the disease using a Mycoplasma
pneumoniae antibody ELISA kit (Shanghai Tong Wei Industrial
Co., Ltd.). The causal agent in three cases remained unknown.
Adenovirus and Mycoplasma pneumoniae were the most common
etiological agents (12/16), with six cases caused by adenovirus,
six cases associated with Mycoplasma pneumoniae, and one
case associated with Epstein-Barr virus.
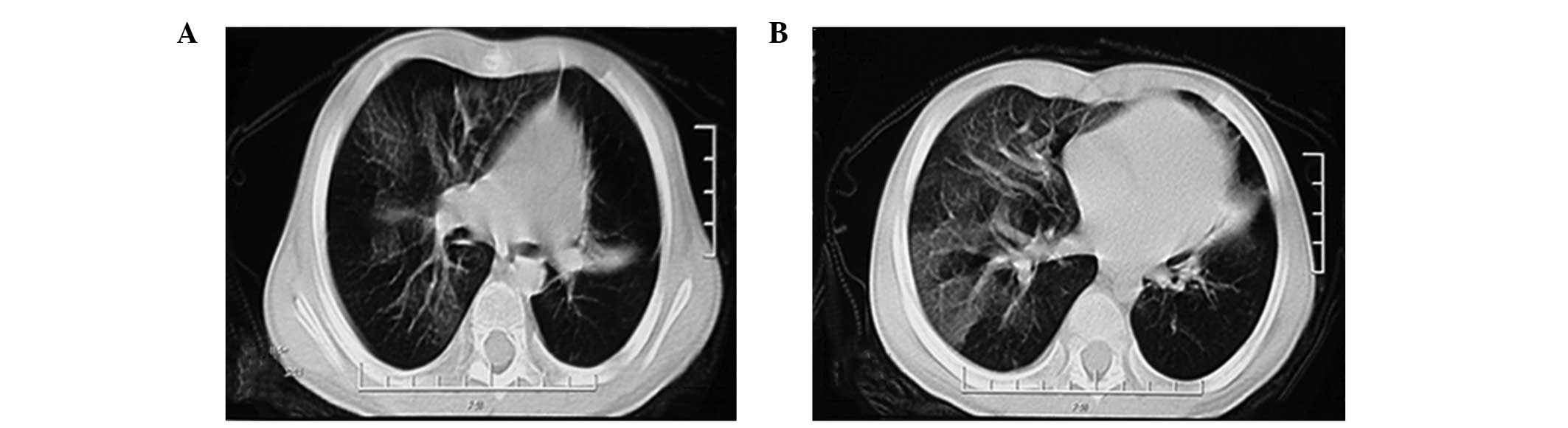
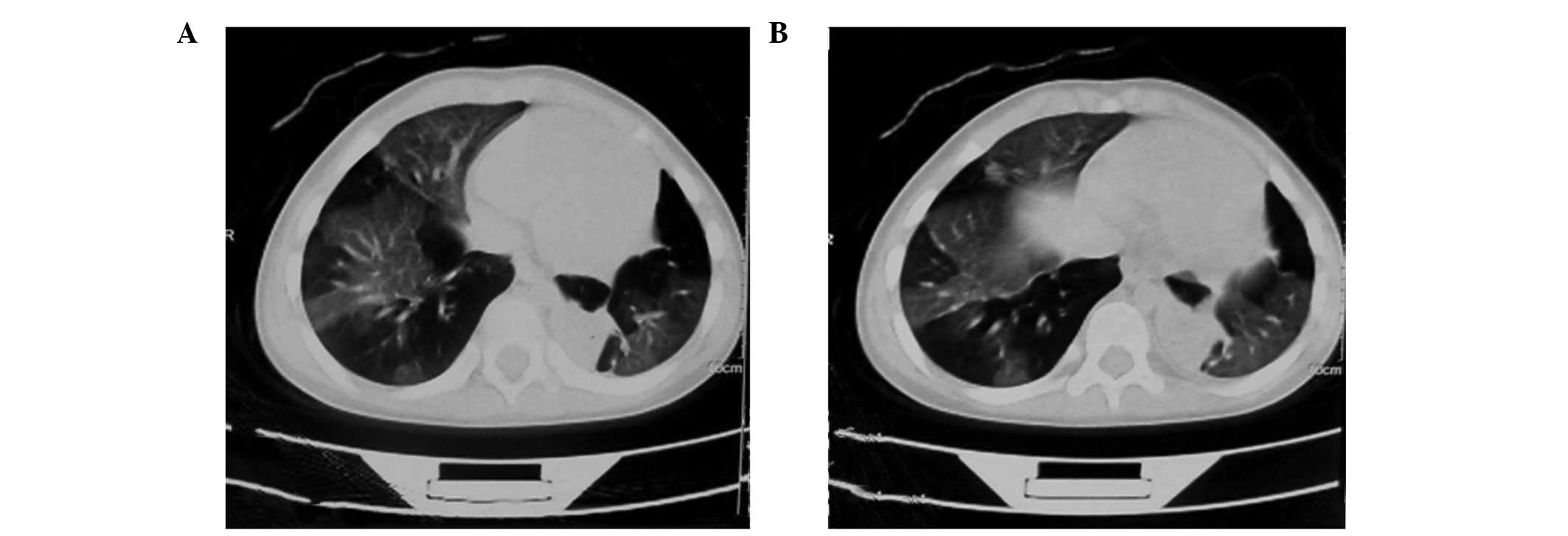
Imaging findings
Chest X-rays, performed using a SOMATOM Definition
64 CT scanner (Siemens Healthcare, Erlangen, Germany), revealed
that 12 patients had excessive ventilation and 10 patients
exhibited patchy ground-glass opacity. The HRCT scans showed patchy
ground-glass opacity and mosaic perfusion in all 16 cases;
bronchial wall thickening and bronchiectasis were observed in eight
cases; pulmonary atelectasis was noted in two cases; and a
unilateral hyperlucent lung was observed in two cases (typical
cases are shown in Figs. 1 and
2). Lung perfusion scans were
performed in two patients and revealed segmental perfusion defects,
which correlated with the abnormalities observed on the chest
radiographs.
Treatment following discharge
When discharged, the patients received supportive
treatment, which included inhaled bronchodilators, chest
physiotherapy and empiric antibiotics when required for acute
respiratory infections. Systemic corticosteroid therapy
(prednisolone, 1 mg/kg/day; Tianjin Lisheng Pharmaceutical Co.,
Ltd., Tianjin, China) and azithromycin (7.5 mg/kg, twice weekly;
Hisun-Pfizer Pharmaceuticals Ltd., Shanghai, China) were used
administered to all 16 patients with a dose reduction of 1.25
mg/month. The treatment period for azithromycin and prednisone
therapy ranged between 6 and 27 months, and the patients underwent
follow-up examinations for various time periods, ranging between 7
and 31 months. Clinical symptoms and HRCT observations were
significantly improved in 10 cases, whereas the HRCT features and
patient condition showed no significant improvement in four cases.
Six months after discharge, the clinical symptoms became more
serious in two patients, who discontinued the prednisone therapy;
HRCT scans revealed a unilateral hyperlucent lung.
Discussion
BO is a chronic obstruction of the airflow
associated with inflammatory lesions of the small airways (1). The condition is divided into two types
depending on the basis of the histological features, namely
proliferative bronchiolitis and obstructive or constrictive
bronchiolitis. The latter form is predominant (7). Constrictive bronchiolitis has a range
of morphological abnormalities, from bronchiolar to peribronchiolar
inflammation, and the condition can lead to complete obstruction of
the bronchioles through submucosal fibrosis (8).
The clinical manifestations of BO are usually
continuous or repeated coughing and wheezing, and a poor exercise
tolerance. Distinguishing BO from ordinary bronchiolitis or viral
pneumonia through observation of the symptoms is challenging;
however, delaying treatment may result in aggravated respiratory
tract infections or even mortality due to respiratory failure in a
period of one to two years (2).
BO has a number of causes, including infection,
connective tissue disorders, bone marrow or lung transplantation
and severe mucocutaneous allergic disorders, such as
Stevens-Johnson syndrome, or the inhalation of toxic substances
(9–11). BO following a severe infectious lung
disease is the most common form reported in children (12). The causal agents of BO include
adenovirus, influenza virus, measles virus and Mycoplasma
pneumoniae (13). Adenovirus is
the leading infectious cause of BO worldwide (14). In the present study, 37.5% of
patients (6/16) were infected with adenovirus. An
additional major infectious agent is Mycoplasma pneumoniae,
which accounted for 37.5% of patients in the present study. The
increased percentage of cases with Mycoplasma pneumoniae as
a causal agent may be associated with the increased incidence of
Mycoplasma pneumonia in China.
Respiratory signs and symptoms of acute viral
bronchiolitis disappear within a few days. Therefore, in children
with acute lower respiratory tract infections, BO must be
considered if wheezing and respiratory distress do not resolve
within the expected time frame, particularly in those with severe
adenovirus infections. Further diagnosis is imperative (15).
With regard to diagnosis, PIBO has no specific signs
and symptoms. Ideally, the diagnosis requires histopathological
confirmation; however, the irregular distribution of the lesions
results in sample collection being challenging (16). Therefore, clinical and imaging
criteria are combined with laboratory tests for agent
identification and to eliminate other forms of chronic lung
disease. Imaging techniques, particularly HRCT, play an important
role in the diagnosis of PIBO (17,18). A
number of characteristics are observed on PIBO-positive HRCT scans,
including patchy ground-glass opacity, air retention, bronchial
wall thickening, bronchiectasis, mosaic perfusion and a unilateral
hyperlucent lung (19). Air
retention syndrome has the highest sensitivity and accuracy in the
diagnosis of BO. Leung et al (20) reported that the sensitivity of air
retention syndrome in HRCT was 91%, with a specificity of 80% and
an accuracy of 86%. The expiratory phase of respiration is
important in diagnosing air retention, particularly in less severe
cases where the inspiratory phase may miss or underestimate this
important characteristic (21).
Acquiring scans of the two respiratory phases may be a challenge in
uncooperative pediatric patients; therefore, more attention should
be paid to ground-glass opacity features. In the current study, the
HRCT results from 10 patients revealed ground-glass opacity.
In the study by Colom and Teper (22), the following scoring method was
proposed: Typical medical history (4 points); adenovirus infection
(3 points) and HRCT showing mosaic perfusion syndrome (4 points). A
score of >7 points indicated a diagnosis of BO, with a
specificity of 100% and a sensitivity of 67%.
PIBO is a rare disease, which has limited the
opportunity for proper randomized clinical trials focused on its
treatment; thus, therapeutic decisions are empirically based
(23,24). The drug treatments for PIBO include:
i) Oral or inhaled corticosteroids aimed at reducing the
inflammatory component; ii) hydroxychloroquine and high-dose pulses
of methylprednisolone for treating severe or prolonged obstruction;
iii) short and long-acting bronchodilators or inhaled
anticholinergic agents for cases of symptomatic wheezing; and iv)
antibiotics, orally or intravenously administered, for the
treatment of patients with frequent infections (25).
Oxygen supplementation may also be used in addition
to drug treatment, particularly during the first few years of the
disease. In the majority of cases, subsequent clinical improvement
leads to the complete weaning off of oxygen. The requirement for
supplemental oxygen at night is a concern; however, only in severe
cases have patients demonstrated significant desaturation during
sleep (26).
Although inflammation plays a prominent role in the
pathogenesis of BO, the use of corticosteroid drug treatment
remains controversial due to the side effects. Certain studies have
suggested that steroids may slow down the progression of bronchiole
fibrosis (27). In the current
study, the patients were administered an initial dose of prednisone
of 1 mg/kg/day. The dose was gradually reduced after 3 months, with
the overall course duration varying between 6 and 27 months, or
longer. A previous study used steroid therapy, for a period ranging
between 1 and 60 months, in children receiving different BO
treatments, including bronchodilators, azithromycin and oxygen
therapy (28). Among these patients,
>80% exhibited rapid improvement in disease symptoms when
medicated using steroids.
Azithromycin is a macrolide antibiotic that has been
demonstrated in prospective, double-blind, placebo-controlled
trials to be effective for the treatment of diffuse
panbronchiolitis and cystic fibrosis. The efficacy of azithromycin
has been hypothesized to be a result of its anti-inflammatory
effects (29).
In addition, a previous study in patients with BOS
following a lung transplant have demonstrated an improvement in the
forced expiratory volume in 1 sec following a prolonged course of
oral azithromycin (250 mg three times per week) (30). Although no previous studies have been
performed with azithromycin in children with PIBO, oral
azithromycin should be considered as a therapeutic option for these
patients due to the efficacy demonstrated in the present study.
In conclusion, the results of the current study
indicate that a typical clinical history and patchy ground-glass
opacity features on HRCT scans can be used as screening indices to
predict BO development. Steroid therapy is the cornerstone of BO
treatment; however, azithromycin is also indispensable in the
treatment of this disease.
References
|
1
|
Lino CA, Batista AK, Soares MA, et al:
Bronchiolitis obliterans: clinical and radiological profile of
children followed-up in a reference outpatient clinic. Rev Paul
Pediatr. 31:10162013.(In English and Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Champs NS, Lasmar LM, Camargos PA, Marguet
C, Fischer GB and Mocelin HT: Post-infectious bronchiolitis
obliterans in children. J Pediatr (Rio J). 87:187–198.
2011.PubMed/NCBI
|
|
3
|
Friedlander AL and Albert RK: Chronic
macrolide therapy in inflammatory airways diseases. Chest.
138:1202–1212. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hickey AJ, Lu D, Ashley ED and Stout J:
Inhaled azithromycin therapy. J Aerosol Med. 19:54–60. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Verleden GM, Vanaudenaerde BM, Dupont LJ
and Van Raemdonck DE: Azithromycin reduces airway neutrophilia and
interleukin-8 in patients with bronchiolitis obliterans syndrome.
Am J Respir Crit Care Med. 174:566–570. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Teper A, Fischer GB and Jones MH:
Respiratory sequelae of viral diseases: from diagnosis to
treatment. J Pediatr (Rio J). 78 (Suppl 2):S187–S194. 2002.(In
Portuguese). View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lynch JP III, Weigt SS, Der Hovanessian A,
Fishbein MC, Gutierrez A and Belperio JA: Obliterative
(constrictive) bronchiolitis. Semin Respir Crit Care Med.
33:509–532. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mauad T and Dolhnikoff M: São Paulo
Bronchiolitis Obliterans Study Group: Histology of childhood
bronchiolitis obliterans. Pediatr Pulmonol. 33:466–474. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Blic J, Deschildre A and Chinet T:
Post-infectious bronchiolitis obliterans. Rev Mal Respir.
30:1521602013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Weigt SS, DerHovanessian A, Wallace WD,
Lynch JP III and Belperio JA: Bronchiolitis obliterans syndrome:
the Achilles' heel of lung transplantation. Semin Respir Crit Care
Med. 34:336–351. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dogra S, Suri D, Saini AG, Rawat A and
Sodhi KS: Fatal bronchiolitis obliterans complicating
Stevens-Johnson syndrome following treatment with nimesulide: a
case report. Ann Trop Paediatr. 31:259–261. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mattiello R, Mallol J, Fischer GB, Mocelin
HT, Rueda B and Sarria EE: Pulmonary function in children and
adolescents with postinfectious bronchiolitis obliterans. J Bras
Pneumol. 36:4534592010.(In English and Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hayes D Jr, Mansour HM, Kirkby S and
Phillips AB: Rapid acute onset of bronchiolitis obliterans syndrome
in a lung transplant recipient after respiratory syncytial virus
infection. Transpl Infect Dis. 14:548–550. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Vu DL, Bridevaux PO, Aubert JD, Soccal PM
and Kaiser L: Respiratory viruses in lung transplant recipients: a
critical review and pooled analysis of clinical studies. Am J
Transplant. 11:1071–1078. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Murtagh P, Giubergia V, Viale D, Bauer G
and Pena HG: Lower respiratory infections by adenovirus in
children. Clinical features and risk factors for bronchiolitis
obliterans and mortality. Pediatr Pulmonol. 44:450–456. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jones KD and Urisman A: Histopathologic
approach to the surgical lung biopsy in interstitial lung disease.
Clin Chest Med. 33:27–40. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee JW, Lee KS, Lee HY, et al: Cryptogenic
organizing pneumonia: serial high-resolution CT findings in 22
patients. AJR Am J Roentgenol. 195:916–922. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Devakonda A, Raoof S, Sung A, Travis WD
and Naidich D: Bronchiolar disorders: a clinical-radiological
diagnostic algorithm. Chest. 137:938–951. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hochhegger B, Irion KL, Marchiori E, Bello
R, Moreira J and Camargo JJ: Computed tomography findings of
postoperative complications in lung transplantation. J Bras
Pneumol. 35:2662742009.(In English and Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Leung AN, Fisher K, Valentine V, et al:
Bronchiolitis obliterans after lung transplantation: detection
using expiratory HRCT. Chest. 113:365–370. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen DH, Lin YN, Lan SL, et al: Clinical
characteristics of bronchiolitis obliterans in pediatric patients.
Zhonghua Er Ke Za Zhi. 50:981022012.(In Chinese). PubMed/NCBI
|
|
22
|
Colom AJ and Teper AM: Clinical prediction
rule to diagnose post-infectious bronchiolitis obliterans in
children. Pediatr Pulmonol. 44:1065–1069. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lenney W, Boner AL, Bont L, et al:
Medicines used in respiratory diseases only seen in children. Eur
Respir J. 34:531–551. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vega-Briceno LE and Zenteno AD: Clinical
guide for diagnosis and care of children and adolescents with
post-infectious bronchiolitis obliterans. Rev Chil Enf Resp.
25:141–163. 2009.
|
|
25
|
Yuksel H, Yilmaz O, Urk V, et al: Clinical
significance of lung perfusion defects in children with
post-infectious bronchiolitis obliterans. Tuberk Toraks.
57:376–382. 2009.PubMed/NCBI
|
|
26
|
Adde FV, Alvarez AE, Barbisan BN and
Guimarães BR: Recommendations for long-term home oxygen therapy in
children and adolescents. J Pediatr (Rio J). 89:6–17. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yalcin E, Doğru D, Haliloğlu M, Ozcelik U,
Kiper N and Gocmen A: Postinfectious bronchiolitis in children:
Clinical and radiological profile and prognostic factors.
Respiration. 70:371–375. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kim TO, Oh IJ, Kang HW, et al:
Temozolomide-associated bronchiolitis obliterans organizing
pneumonia successfully treated with high-dose corticosteroid. J
Korean Med Sci. 27:450–453. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Vos R, Vanaudenaerde BM, Verleden SE, et
al: Anti-inflammatory and immunomodulatory properties of
azithromycin involved in treatment and prevention of chronic lung
allograft rejection. Transplantation. 94:101–109. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Aguerre V, Castanos C, Pena HG, Grenoville
M and Murtagh P: Postinfectious bronchiolitis obliterans in
children: clinical and pulmonary function findings. Pediatr
Pulmonol. 45:1180–1185. 2010. View Article : Google Scholar : PubMed/NCBI
|