Introduction
Breast cancer is the most common malignancy
diagnosed among women worldwide; in the United States (1), more than 1 million new cases of
breast cancer were diagnosed in 2010 (2). The majority of breast cancer-related
deaths are due to the development of distant metastases, for which
there are no effective treatments (3,4).
Although many chemotherapeutic reagents are available for the
treatment of cancer metastasis, the median survival duration has
not improved, and the molecular events that are associated with
disease progression to metastasis are not yet fully understood
(5). Tumor invasion and
metastasis is an integrated process; intriguingly, chemotherapeutic
reagents may be one of the many contributors to cancer metastasis,
and it is believed that occurs through the activation of
endoplasmic reticulum (ER) stress and heparanase by these agents
(6).
Heparan sulfate (HS) proteoglycan (HSPG) (7) is an important component of the
extracellular matrix (ECM) and basement membrane (BM). The
degradation of HSPG is achieved through the cleavage of a
glycosidic bond by heparanase, using a hydrolase mechanism. In
addition, heparanase plays a significant role in cancer metastasis
and invasion (8). Heparanase can
be regulated by glucose, promoter methylation, p53, estrogen, tumor
necrosis factor-α and interferon-γ (9–11).
Its HS degradation activity can be inhibited by the heparanase
inhibitors, OGT2115, and low molecular weight heparin (LMWH)
(12,13).
Chemotherapeutic reagents have been shown to induce
ER stress. In this study, we used two reagents to induce ER stress,
the chemotherapeutic drug, adriamycin (ADM), and the ER stress
inducer, tunicamycin (TM). Invasion and metastasis appear during
the long-term cancer treatment process, prompting us to speculate
that these events may be associated with the increased ER stress. A
number of factors, such as hypoxia, nutritional deficiency,
oxidative stress, chemo- and radiotherapy, calcium metabolism
disorders, and defects in protein expression can cause ER stress
(14,15). The ER responds to stress
conditions by activating a range of stress response signaling
pathways to alter transcriptional and translational programs, which
couple the ER protein folding load with the ER protein folding
capacity. This process is termed the unfolded protein response
(UPR) (16) and the marker
protein is glucose-regulated protein 78 (GRP78). UPR can protect
the ER and minimize damage to other organelles, and it may protect
cells by promoting metastasis (17).
The aim of this study was to investigate the
correlation between ER stress and the increased invasion and
migration of cancer cells. Furthermore, we provide evidence that
the invasion and migration induced by chemotherapeutic reagents
occurs due to the activation of heparanase under ER stress.
Materials and methods
Reagents and antibodies
TM was purchased from Sigma Chemical Co. (Castle
Hill, NSW, Australia). OGT2115 was purchased from Tocris Bioscience
(Bristol, UK). ADM was purchased from Pharmacia & Upjohn SpA
and LMWH was purchased from Sanofi-Aventis Pharmaceutical Co., Ltd.
(Beijing, China), for clinical use. The rabbit monoclonal antibody
(mAb) against GRP78, heparanase, and β-actin antibody were
purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA,
USA). Human heparanase enzyme-linked immunosorbent assay (ELISA)
kit was obtained from R&D Systems (Minneapolis, MN, USA).
Matrigel was purchased from BD Biosciences (Bedford, MA, USA). The
24-well Transwell insert (8 μm) was obtained from Corning Inc.
(Corning, NY, USA).
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
was purchased from Sigma Chemical Co. Dulbecco’s modified Eagle’s
medium (DMEM), fetal bovine serum (FBS) and phosphate-buffered
saline (PBS) were purchased from Gibco (Grand Island, NY, USA).
Cell lines
The breast cancer cell lines, MDA-MB-231 and
MDA-MB-435, were obtained from the American Type Culture Collection
(ATCC). Cells were routinely cultured in DMEM supplemented with 10%
FBS and 100 U of penicillin-streptomycin with 5% CO2 in
a humidified incubator at 37°C. All cell lines were tested every
month for mycoplasma contamination, used only at low passage, and
were regularly examined under a microscope for phenotypic changes
prior to use.
Cell viability assay
The cytotoxic effect of OGT2115 and ADM on breast
cancer cells was determined using the MTT assay as previously
described. MTT is a yellow tetrazolium dye that responds to
metabolic activity. Reductase enzymes in living cells reduce MTT
from a pale yellow color to dark blue formazan crystals. Cells were
plated at 7,000/well in 96-well plates and cultured in a humidified
5% CO2 atmosphere at 37°C. At 24, 48 and 72 h, the wells
were incubated with MTT (5 mg/ml) in PBS for 4 h at 37°C. After 4
h, the MTT solution was removed and replaced with 150 μl of
dimethyl sulfoxide (DMSO). The plate was further incubated for 0.5
h at room temperature, and the optical density (OD) of the wells
were determined using a plate reader at a test wavelength of 570
nm. Each test was performed in triplicate.
Cell invasion assay
The invasion assay was performed using a 24-well
cell culture plate with 8.0-μm pore membrane inserts. Breast cancer
cells were starved in serum-free medium overnight, and
5×104 cells were resuspended in 100 μl serum-free medium
and placed in the upper chambers. The membrane undersurface was
coated with 50 μl Matrigel from BD Biosciences mixed with RPMI-DMEM
serum free medium at a 1:8 dilution for 30 min at 37°C. The lower
well of each chamber was filled with 600 μl DMEM supplemented with
10% FBS and incubated for 48 h. Reagents were added to the upper
chambers, and 48 h after treatment, the cells on the upper surface
of the membrane were removed by cotton buds, and the cells on the
lower chamber were incubated with paraformaldehyde in PBS buffer
and stained with 0.1% crystal violet. Five visual fields were
randomly selected for each insert and photographed under a light
microscope at ×400 magnification. The number of cells was then
counted and analyzed for statistically significant differences.
Each condition was assayed in triplicate, the experiments were
performed independently at least three times, and the results are
expressed as the number of cells/field. A one-way analysis of
variance was used to determine statistical significance.
Cell migration assay
Migration assay was performed using a 24-well cell
culture plate with 8.0-μm pore membrane inserts without Matrigel.
MDA-MB-435 and MDA-MB-231 cells (5×104) were added to
the upper wells, and the chambers were incubated for 24 h at 37°C.
The lower chamber was filled with 600 μl 10% FBS as the
chemoattractant. After 24 h in normoxic conditions the cells that
had migrated were stained and photographed under a light microscope
at ×200 magnification. The number of cells that had migrated was
counted from five randomly selected fields. Each condition was
assayed in triplicate, the experiments were performed independently
at least three times, and the results are expressed as the number
of cells/field. A one-way analysis of variance was used to
determine statistical significance.
Wound healing assay
Cells were plated on six-well plates at
5×105 cells/well. The following day, the cells were
washed with PBS and wounds were created by scraping with a
sterilized pipette tip. The cells were then washed twice with PBS,
and incubated in RPMI-DMEM. The wound closure was monitored for
0–48 h. The wound areas were observed under an inverted microscope
and measured by imaging at the relevant fields for the calculation
of the healing percentages. Each test was performed in
triplicate.
Western blot analysis
Cells were washed three times with cold PBS and
lysed on ice in radioimmunoprecipitation assay (RIPA) buffer with
protease inhibitors. The protein concentrations were determined
using the BCA method. A total of 80 μg of protein was separated by
10% SDS-PAGE and electro-blotted onto PVDF membranes using a
semi-dry blotting apparatus. After blocking in 5% non-fat milk, the
membranes were incubated overnight at 4°C with the primary
antibodies. The membranes were then incubated in the secondary
antibodies for 2 h at room temperature on a shaker. The bands were
visualized using Western Lightning ECL Pro with horseradish
peroxidase (HRP). β-actin was used as a loading control.
ELISA
Utilizing the ELISA method for the detection and
quantification of heparanase, we were able to monitor changes in
heparanase activity. Cells were plated on 24-well plates at
5×104/well and incubated in DMEM containing 10% FBS.
After 24 h, we extracted the cell culture medium for the detection
of heparanase activity. The microtiter plate provided with the kit
was pre-coated with an antibody specific to heparanase. Standards
or samples were then added to the appropriate microtiter plate
wells containing a biotin-conjugated polyclonal antibody to
heparanase. Avidin conjugated to HRP was then added to each
microplate well and incubated. Tetramethylbenzidine (TMB) substrate
solution was then added to each well. Only those wells that
contained heparanase, biotin-conjugated antibody and
enzyme-conjugated avidin exhibited a change in color. The
enzyme-substrate reaction was terminated by the addition of
sulphuric acid solution and the color change was measured
spectrophotometrically at a wavelength of 450±2 nm. The
concentration of heparanase in the samples was then determined by
comparing the OD.
Results
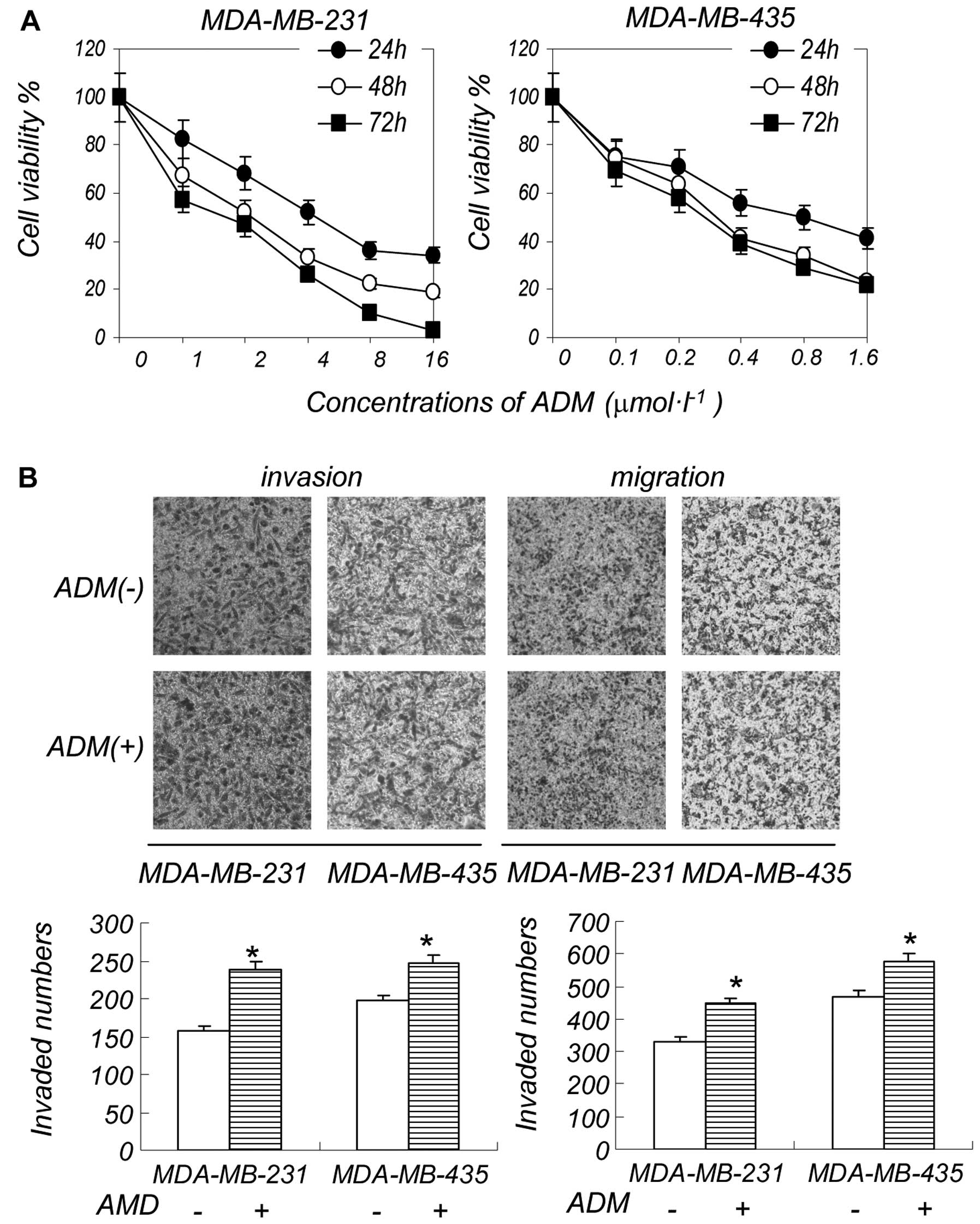
A low concentration of ADM increases the
invasion and migration ability of breast cancer cells
We first examined the effect of ADM on the viability
of the breast cancer cell lines, MDA-MB-231 and MDA-MB-435. ADM
significantly inhibited the growth of MDA-MB-231 cells at an
IC50 of 1 μM. The IC50 of ADM was 0.6 μM in
the MDA-MB-435 cells (Fig. 1A).
We examined the effects of various concentrations of ADM on cell
invasion and migration, and found the IC50 of ADM had
almost no effect on cell invasion and migration (data not shown).
However, a low concentration of ADM (0.2 μM) did not have a
significant effect on cell death, but increased cell invasion and
migration to a certain extent (Fig.
1B). Consistent with cancer metastasis data in clinical
practice, a high concentration of ADM suppressed cell
proliferation, but a low concentration induced breast cancer cell
metastasis. A low degree of ER stress can protect cells but induces
apoptosis when the ER response is strong enough. Metastasis is
likely associated with the induction of ER stress by low
concentrations of chemotherapeutic reagents, which can protect
cancer cells. In order to verify our assumption, we conducted the
following experiments.
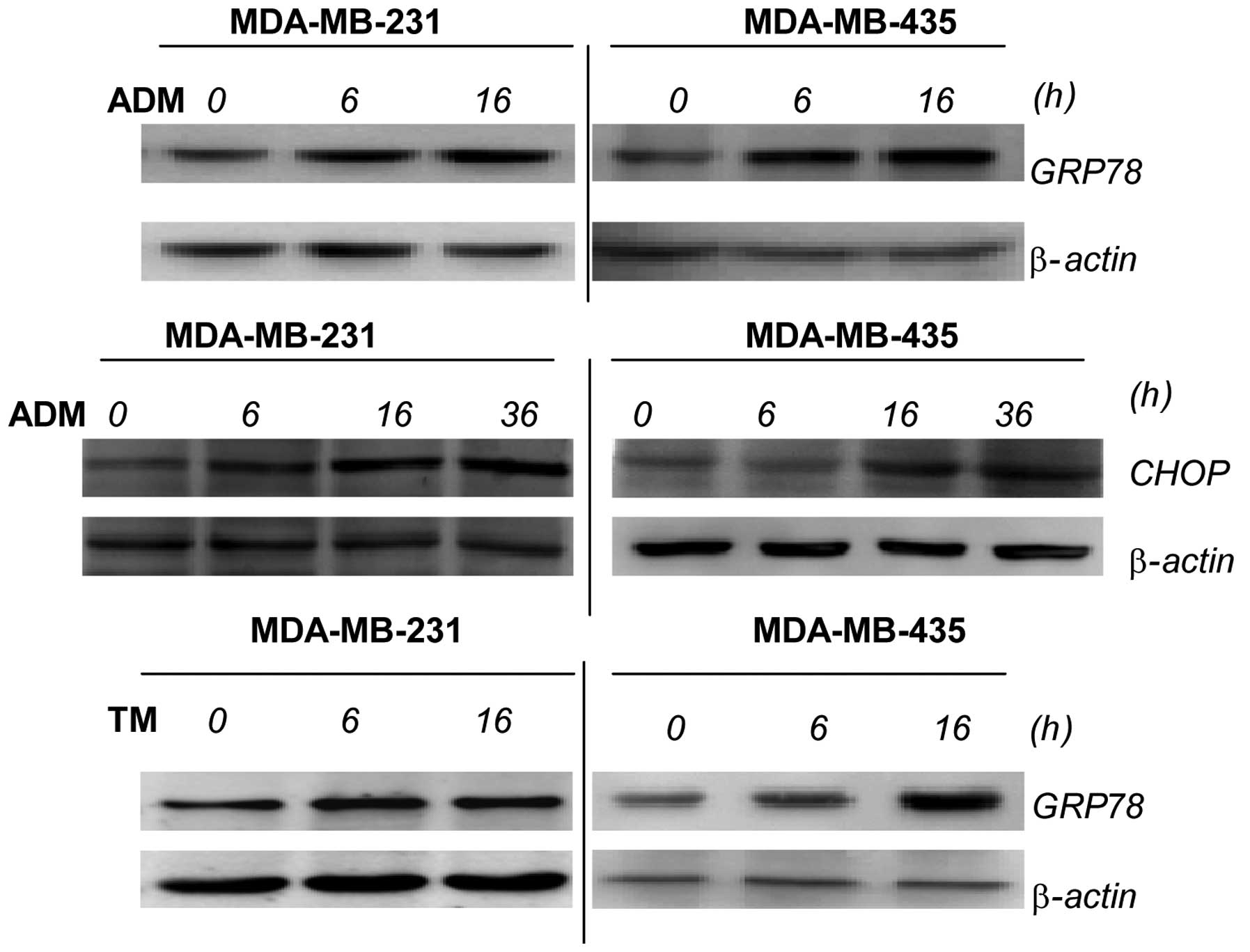
TM and ADM induce ER stress in breast
cancer cells
ADM is a chemotherapeutic reagent which can induce
ER stress. Using ADM, we examined whether the increase in the
invasion and migration of breast cancer cells is due to the
induction of ER stress. To monitor ER stress induction, we detected
the expression of GRP78 and C/EBP homologous protein (CHOP) in the
breast cancer cells following treatment with ADM by western blot
analysis. GRP78 is an indicator of ER stress, and ER stress
transducers are kept in an inactive state through binding to the ER
chaperone, GRP78 (18); treatment
with ADM increases the levels of GRP78 and CHOP. To further verify
that the increase in invasion and migration is indeed caused by ER
stress, we used the ER stress inducer, TM. The results showed that
the cells exposed to TM expressed higher levels of GRP78 (Fig. 2).
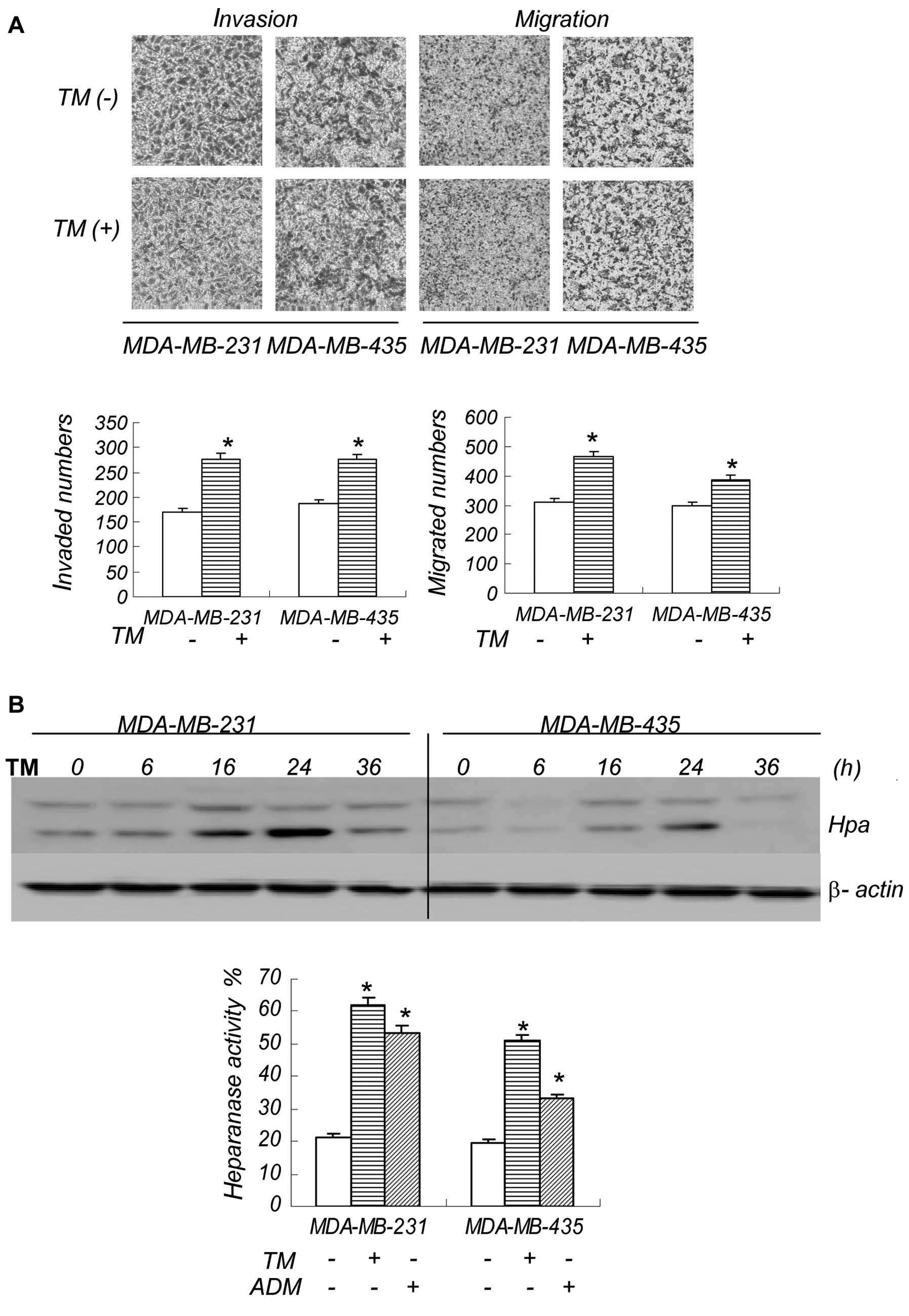
ER stress activates heparanase in breast
cancer cells
We then exposed the breast cancer cells to TM, and
consistent with our findings using ADM, a low concentration of TM
also increased cell invasion and migration. The number of cells
that underwent invasion and migration, and the speed of this
process are shown in Figs. 3A and
4D. Since TM is an ER stress
inducer, combined with the ADM results, we believe that the
invasion and metastasis observed is associated with ER stress.
Heparanase plays a major role in tumor metastasis, and to determine
whether ER stress induces heparanase activation in breast cancer
cells, we performed western blot analysis and ELISA to detect the
expression and activity of heparanase (Fig. 3B). The western blot analysis
results revealed a change in the bands from 50 to 65 kDa,
indicating the activation of heparanase. In addition, the increased
signal shown by ELISA also reflected changes in heparanase
activity. The results demonstrate that the ER stress inducer, TM,
activates heparanase in breast cancer cells. Heparanase activity
increased at 16 and 24 h, causing a series of after-effects and
cell invasion and migration.
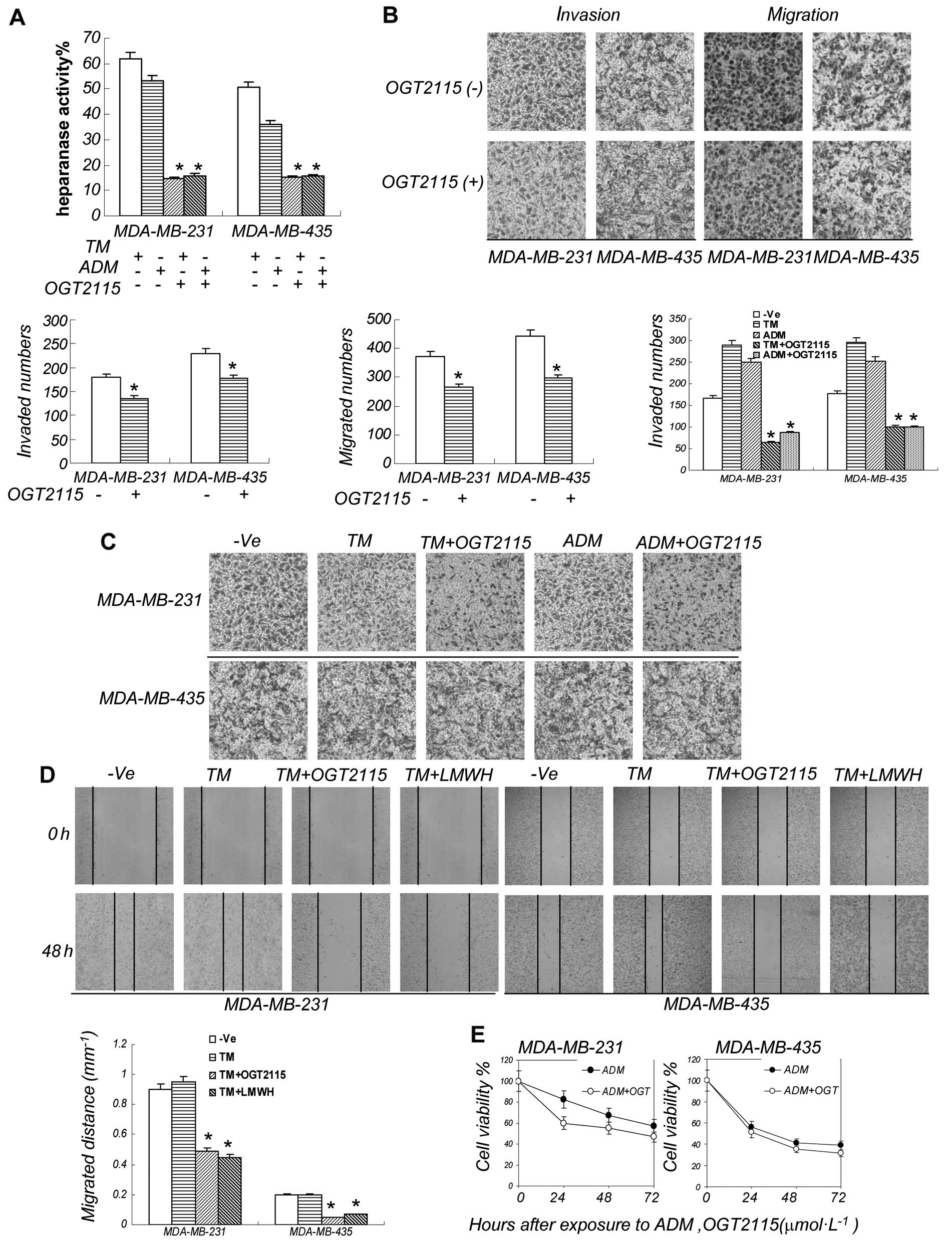
Heparanase inhibitor decreases the
invasion and migration induced by ER stress
As heparanase promotes tumor cell invasion and
migration, we then examined whether the ER stress-induced cell
invasion and migration occurs through the induction of heparanase.
In order to prove that heparanase plays a decisive role in
enhancing cell invasion under ER stress, we used OGT2115 to inhibit
heparanase activity. OGT2115 is a heparanase inhibitor that
exhibits anti-angiogenic properties in vitro by directly
suppressing heparanase activity. First, we determined whether
OGT2115 can inhibit heparanase. Our ELISA results confirmed that
OGT2115 suppressed heparanase activity (Fig. 4A). Since TM enhances cell invasion
and migration when administered at a low concentration, we then
examined whether OGT2115 can alter the effects of TM on cell
invasion and migration. OGT2115 suppressed the invasion and
migration of breast cancer cells, although not significantly
(Fig. 4B). However, compared with
the control group, the number and rate of migrated cells were
significantly reduced following the exposure of the cells to TM +
OGT2115. OGT2115 significantly inhibited the invasion and migration
induced by ADM (Fig. 4C and D).
Furthermore, the MTT assay results showed that OGT2115 did not
decrease the anti-proliferative effect of ADM, thus preserving the
strong antitumor activity of the chemotherapeutic drug (Fig. 4E).
LMWH decreases the invasion and migration
induced by ER stress
In order to validate the above results, we also
selected another heparanase inhibitor in the following experiments.
LMWH as an exogenous supplement of heparins is susceptible to
cleavage by heparanase in vitro, and this cleavage
significantly neutralizes the anti-coagulant properties of these
polysaccharides (19). LMWH
exhibited a moderate antitumor activity and decreased the
heparanase activity induced by ADM or TM (Fig. 5A and B). However, it significantly
reduced cell invasion and migration when used in combination with
TM (Fig. 5C and 4D). We used LMWH in combination with
ADM, and similar to the results obtained from the combination of
LMWH and TM, LMWH significantly reduced the cell migration and
invasion induced by ADM (Fig.
5D). The results of the migration of MDA-MB-435 cells are not
shown. Thus, heparanase inhibitors play a significant role in
decreasing cell invasion and migration induced by ER stress.
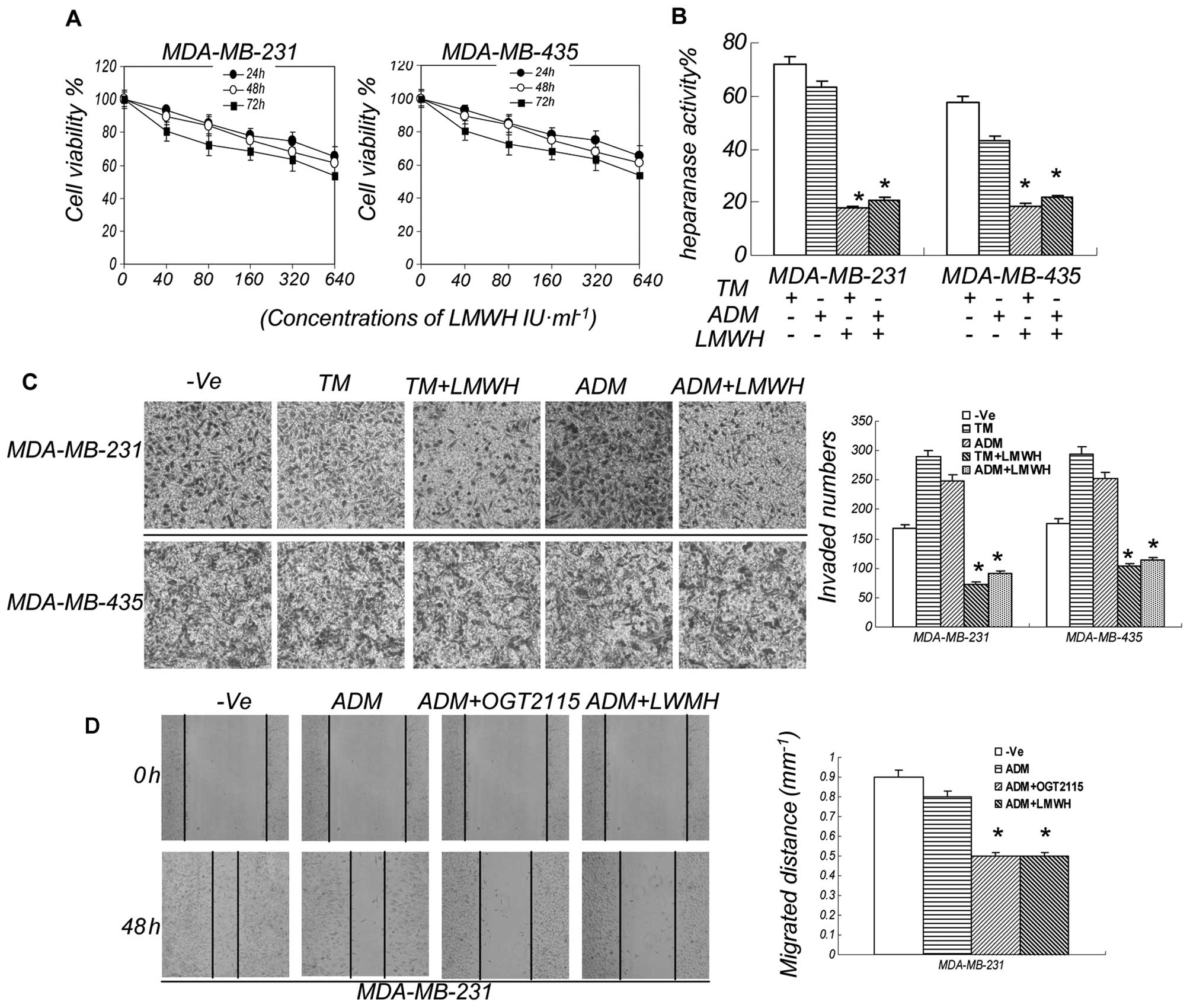
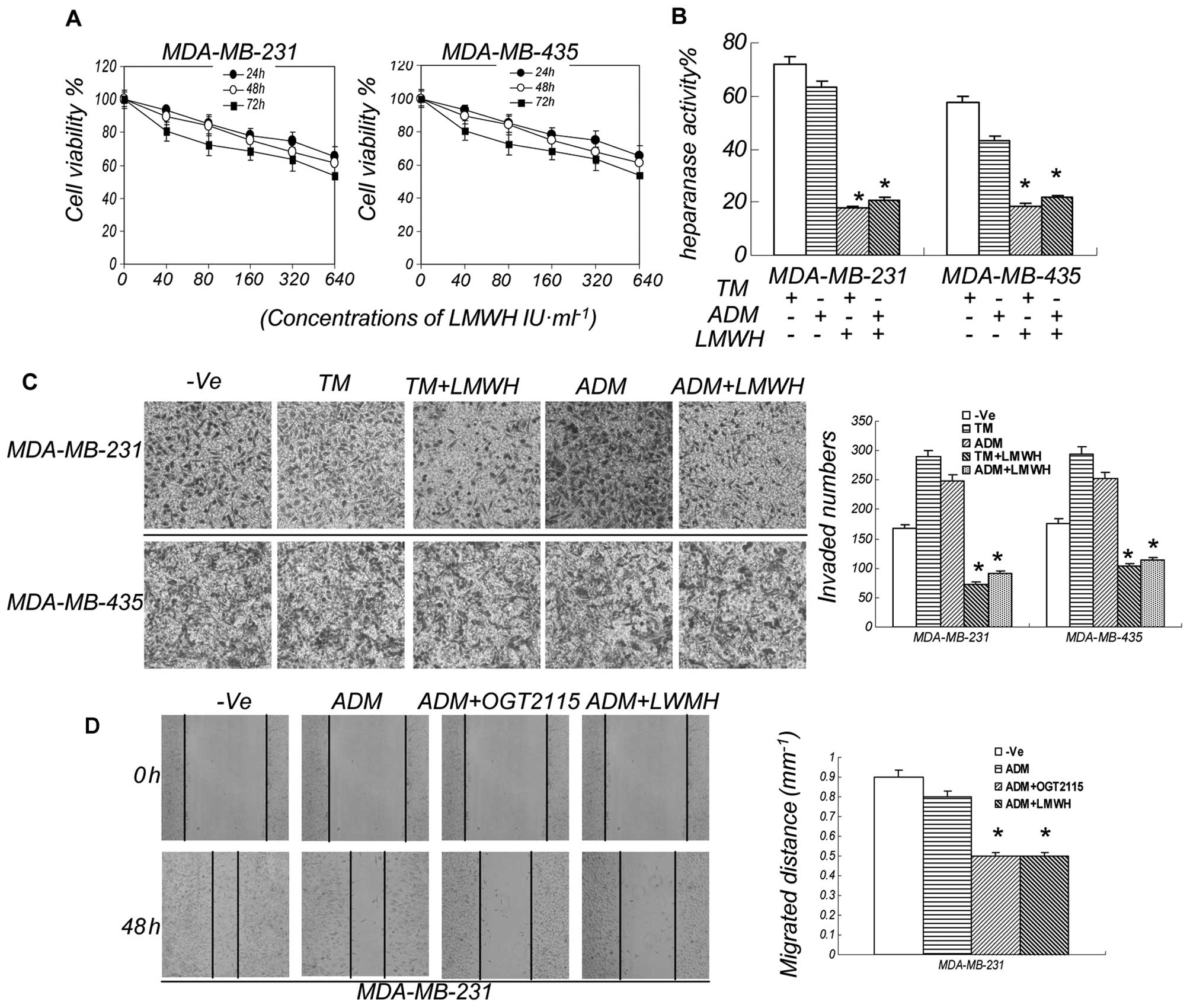 | Figure 5LMWH decreases the invasion and
migration induced by ER stress. (A) LMWH moderately inhibited the
growth of breast cancer cells. The breast cell lines, MDA-MB-435
and MDA-MB-231, were treated with LMWH at various concentrations
and measured after three days in culture. The results are expressed
as a percentage of the control levels. Data are presented as the
means ± SEM, n=3. *P<0.05 compared to the controls.
(B) LMWH suppressed the heparanase activity induced by ER stress.
The breast cancer cell lines, MDA-MB-231 and MDA-MB-435, were
treated for 24 h with TM at 0.75 μM, ADM at 0.2 μM and LMWH at 500
IU/ml. Cell lysates were then prepared and examined for heparanase
enzyme activity. (C) Invasion of the cancer cells were decreased by
LMWH. Following treatment with ADM at 0.2 μM, TM at 0.75 μM and
LMWH at 500 IU/ml for 48 h, we observed that LWMH decreased the
invasion induced by ADM or TM. *P<0.05 compared to
the controls. −Ve, vehicle control. (D) Migration of the cancer
cells were decreased by OGT2115/LMWH. Following treatment with ADM
at 0.2 μM, OGT2115 at 0.8 μM and LMWH at 500 IU/ml for 48 h, we
observed that OGT2115/LMWH decreased the migration induced by ADM.
*P<0.05 compared to the controls. −Ve, vehicle
control. |
Discussion
In breast cancer, metastasis is an end result of a
long selection process of clinical treatments spanning decades, in
which the most adaptable cancer cells persist. More
chemotherapeutic reagents, as well as radiation therapy are being
included in cancer therapeutic regimens; however, in actual
clinical practice, these reagents may increase the incidence of
cancer cell metastasis (20). The
reasons for the progression to metastasis for some patients during
clinical treatment are unclear (10,21). As reported in the literature, we
know that heparanase is an important contributor to tumor invasion
and metastasis (22). It has been
reported that ionizing radiation promotes pancreatic cancer
aggressiveness through the upregulation of heparanase expression
(23). Our results suggest a
correlation between ER stress-induced metastasis and
heparanase.
HSPGs interact through specific attachment sites
with the main protein components of BM and ECM, and only heparanase
can degrade HSPG. This degradation is associated with the invasion,
angiogenic and metastatic potential of diverse malignant tumors and
cell lines. We used Matrigel cell invasion assay; Matrigel enables
an environment conducive to cell invasion in vitro and the
main ingredients of Matrigel are HSPG, laminin, collagen IV,
nidogen and others. At room temperature, Matrigel automatically
gathers to become a matrix material which is similar to the
mammalian cell BM and ECM; it can produce the biological activity
and analog cell BM structure in vivo. The expression of
heparanase in tumor cells correlates with the increased metastatic
potential (24). In addition, HS
moieties in the ECM are responsible for the binding of
heparin-binding growth factors, which are thereby protected,
stabilized and sequestered from their site of action, but upon the
enzymatic degradation of HS can be readily mobilized to induce
growth factor-dependent processes. Thus, the cleavage of HS by
heparanase enables cell invasion, the release of HS-bound
angiogenic and growth factors from the ECM depots, and the
generation of bioactive HS fragments which promote growth
factor-receptor binding, dimerization and signaling (25,26). Direct evidence for heparanase
promoting the progression of many cancers is provided by the
demonstration that the overexpression of heparanase accelerates
primary tumor growth and increases the metastatic ability of
melanoma and prostate carcinoma cells (27). By contrast, heparanase silencing
markedly decreases the metastatic potential of cancer cells.
ER is a central organelle responsible for lipid
synthesis, calcium homeostasis, protein folding and maturation.
Previous studies have focused on the roles of ER stress in the
inhibition of apoptosis and chemotherapy resistance in human
cancers, and certain studies have reported that ER stress is
involved in the regulation of tumor invasion and metastasis.
However, it remains unclear whether ER stress is involved in the
regulation of tumor invasion and metastasis (28). Only properly folded proteins are
allowed to reach their final destination, whereas unfolded and
misfolded proteins are exported or dislocated from the ER and
degraded by cytoplasmic proteasomes (29). When the homeostasis of the ER is
disturbed, unfolded or misfolded proteins accumulate in the ER
lumen, resulting in ER stress. In response to ER stress, cells
activate a set of tightly controlled regulatory programs, known as
UPR, to restore the normal function of the ER. However, if ER
stress is sustained and the adaptive UPR fails to eliminate
unfolded or misfolded proteins, apoptosis will occur to remove the
stressed cells. There are three branches of UPR that are initiated
by distinct ER stress transducers located on the ER membrane:
protein kinase RNA-like endoplasmic reticulum kinase (PERK),
inositol-requiring enzyme-1 (IRE-1) (16) and activating transcription
factor-6 (ATF-6) (30). All three
ER stress transducers are kept in an inactive state through binding
to the ER chaperone GRP78 (31),
which is also known as immunoglobulin-binding protein. The exact
mechanism underlying the switch of the UPR from a prosurvival
mechanism to a proapoptotic response is unclear. Therefore, the UPR
can be considered as a safeguard for protein synthesis,
post-translational modifications, folding and secretion, calcium
storage and signaling and lipid biosynthesis. The UPR initially
tries to restore the normal function of the cell by halting protein
translation and activating the signaling pathways that lead to the
increase in the production of molecular chaperones involved in
protein folding. If these objectives are not achieved within a
certain period of time or the disruption is prolonged, the UPR
tries to turn on the apoptotic pathway (32,33). We demonstrated that
chemotherapeutic reagents can promote ER stress and the activation
of the UPR, which confers a survival advantage to the tumor cells,
promoting their migration and invasion ability, and these effects
are associated with the activation of heparanase.
We provide evidence that ER stress inducers can
activate heparanase, and this activation results in the increased
invasion and migration of breast cancer cells. The purpose of the
UPR is to protect the ER and limit damage to other organelles,
helping cells to leave the original stressed environment and thus
enabling cells to survive. Our findings indicate that the
heparanase inhibitor, OGT2115, and LMWH can suppress metastasis
induced by ER stress in breast cancer cells. The degradation of
LMWH by heparanase in vivo may be relevant in situations in
which heparanase is overexpressed, and treatment with LMWH composed
of non-anticoagulant species of heparin and various sulfated
polysaccharides which inhibit experimental metastasis, also
inhibited heparanase activity in the tumor cells (34). However, the precise molecular
mechanisms responsible for heparanase regulation have not yet been
fully elucidated. HSPG contains sulfate groups and a sugar chain
and is negatively charged. These biological or chemical
characteristics can inhibit metastasis. According to its basic
chemical composition, heparanase inhibitors can be divided into
sugars, nucleotides and amino acids, such as oligomannurarate
sulfate (35), laminarin sulfate,
phosphomannopentaose sulfate (36), LMWH and others. Heparanase
inhibitors do not decrease the anti-proliferative effect of
chemotherapeutic reagents, and they also inhibit the invasion and
migration of cancer cells under ER stress. Our findings may prove
to be clinically significant, since we show that ER stress is a
pivotal contributor in chemotherapy-mediated tumor metastasis. In
addition, since GRP78 and heparanase play roles in the
chemotherapy-induced increase in invasion or migration, the
mechanism behind the ER stress-induced invasion and migration may
be through the activation of heparanase. However, the inhibition of
heparanase activity did not completely suppress cell invasion,
suggesting that other factors may also contribute to the ER
stress-induced increase in cell invasion and metastasis following
chemotherapy.
In conclusion, to our knowledge, we demonstrate for
the first time in this study that ER stress increases the invasion
and migration of breast cancer cells through the activation of
heparanase. This may occur through the activation of the UPR which
plays an important role in the protection of cells against the
cytotoxic effects of low-dose chemotherapy. It is essential to
elucidate the molecular mechanisms that underlie the increase in
cancer metastasis induced by chemotherapy. Our results suggest that
heparanase is involved in chemotherapy-induced tumor metastasis,
and that inhibiting heparanase activity may prove to be a promising
therapeutic strategy for the treatment of metastatic breast cancer.
In our study, cell invasion and migration were suppressed by the
inhibition of heparanase and this finding may have a significant
impact on the development of heparanase-based therapy for
metastasis under ER stress (37,38).
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (no. 81000992 and 81072207),
the Natural Science Foundation of Anhui Province (no. 090413135)
and the Key Project of the Natural Science Foundation of the
Department of Education, Anhui Province, China (no.
KJ2012A202).
References
|
1
|
Qin XJ and Ling BX: Proteomic studies in
breast cancer (Review). Oncol Lett. 3:735–743. 2012.PubMed/NCBI
|
|
2
|
Spinelli GP, Russo LG, Miele E, et al:
Breast cancer metastatic to the pituitary gland: a case report.
World J Surg Oncol. 10:1372012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gnant M, Balic M, Petru E, et al:
Treatment of bone metastases in patients with advanced breast
cancer. Breast Care (Basel). 7:92–98. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Breidenbach M, Rein DT, Schondorf T, et
al: A new targeting approach for breast cancer gene therapy using
the heparanase promoter. Cancer Lett. 240:114–122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Coleman RE: Clinical features of
metastatic bone disease and risk of skeletal morbidity. Clin Cancer
Res. 12:6243–6249. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fux L, Ilan N, Sanderson RD and Vlodavsky
I: Heparanase: busy at the cell surface. Trends Biochem Sci.
34:511–519. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vlodavsky I, Elkin M, Pappo O, et al:
Mammalian heparanase as mediator of tumor metastasis and
angiogenesis. Isr Med Assoc. 2:37–45. 2000.PubMed/NCBI
|
|
8
|
Yang Y, Macleod V, Bendre M, et al:
Heparanase promotes the spontaneous metastasis of myeloma cells to
bone. Blood. 105:1303–1309. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Baraz L, Haupt Y, Elkin M, Peretz T and
Vlodavsky I: Tumor suppressor p53 regulates heparanase gene
expression. Oncogene. 25:3939–3947. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cohen I, Maly B, Simon I, et al: Tamoxifen
induces heparanase expression in estrogen receptor-positive breast
cancer. Clin Cancer Res. 13:4069–4077. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang F, Wang Y, Kim MS, et al:
Glucose-induced endothelial heparanase secretion requires cortical
and stress actin reorganization. Cardiovasc Res. 87:127–136. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vitale FV, Rotondo S, Sessa E, et al: Low
molecular weight heparin administration in cancer patients with
hypercoagulability-related complications and carrying brain
metastases: a case series study. J Oncol Pharm Pract. 18:10–16.
2011. View Article : Google Scholar
|
|
13
|
Gandhi NS, Freeman C, Parish CR and
Mancera RL: Computational analyses of the catalytic and
heparin-binding sites and their interactions with
glycosaminoglycans in glycoside hydrolase family 79
endo-β-D-glucuronidase (heparanase). Glycobiology. 22:35–55.
2012.PubMed/NCBI
|
|
14
|
Schroder M and Kaufman RJ: The mammalian
unfolded protein response. Annu Rev Biochem. 74:739–789. 2005.
View Article : Google Scholar
|
|
15
|
Takada A, Miki T, Kuno A, et al: Role of
ER stress in ventricular contractile dysfunction in type 2
diabetes. PLoS One. 7:e398932012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li N, Zoubeidi A, Beraldi E and Gleave ME:
GRP78 regulates clusterin stability, retrotranslocation and
mitochondrial localization under ER stress in prostate cancer.
Oncogene. June 11–2012.(Epub ahead of print).
|
|
17
|
Dong D, Ni M, Li J, et al: Critical role
of the stress chaperone GRP78/BiP in tumor proliferation, survival,
and tumor angiogenesis in transgene-induced mammary tumor
development. Cancer Res. 68:498–505. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Weng WC, Lee WT, Hsu WM, Chang BE and Lee
H: Role of glucose-regulated Protein 78 in embryonic development
and neurological disorders. J Formos Med Assoc. 110:428–437. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nasser NJ, Sarig G, Brenner B, et al:
Heparanase neutralizes the anticoagulation properties of heparin
and low-molecular-weight heparin. J Thromb Haemost. 4:560–565.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liang Y, O’Driscoll L, McDonnell S, et al:
Enhanced in vitro invasiveness and drug resistance with altered
gene expression patterns in a human lung carcinoma cell line after
pulse selection with anticancer drugs. Int J Cancer. 111:484–493.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bruzzi P, Del Mastro L, Sormani MP, et al:
Objective response to chemotherapy as a potential surrogate end
point of survival in metastatic breast cancer patients. J Clin
Oncol. 23:5117–5125. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ilan NM, Elkin and Vlodavsky I:
Regulation, function and clinical significance of heparanase in
cancer metastasis and angiogenesis. Int J Biochem Cell Biol.
38:2018–2039. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Meirovitz A, Hermano E, Lerner I, et al:
Role of heparanase in radiation-enhanced invasiveness of pancreatic
carcinoma. Cancer Res. 71:2772–2780. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nasser NJ: Heparanase involvement in
physiology and disease. Cell Mol Life Sci. 65:1706–1715. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Theocharis AD, Skandalis SS, Tzanakakis GN
and Karamanos NK: Proteoglycans in health and disease: novel roles
for proteoglycans in malignancy and their pharmacological
targeting. FEBS J. 277:3904–3923. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fan L, Wu Q, Xing X, Liu Y and Shao Z:
Targeted silencing of heparanase gene by small interfering RNA
inhibits invasiveness and metastasis of osteosarcoma cells. J
Huazhong Univ Sci Technolog Med Sci. 31:348–352. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vlodavsky I, Beckhove P, Lerner I, et al:
Significance of heparanase in cancer and inflammation. Cancer
Microenviron. 5:115–132. 2011. View Article : Google Scholar
|
|
28
|
Su R, Li Z, Li H, et al: Grp78 promotes
the invasion of hepatocellular carcinoma. BMC Cancer. 10:202010.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Scull CM and Tabas I: Mechanisms of ER
stress-induced apoptosis in atherosclerosis. Arterioscler Thromb
Vasc Biol. 31:2792–2797. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nishitoh H: CHOP is a multifunctional
transcription factor in the ER stress response. J Biochem.
151:217–219. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang KH, Kuo KL, Chen SC, et al:
Down-regulation of glucose-regulated protein (GRP) 78 potentiates
cytotoxic effect of celecoxib in human urothelial carcinoma cells.
PLoS One. 7:e336152012. View Article : Google Scholar
|
|
32
|
Feng X, Krishnan K, Richie DL, et al:
HacA-independent functions of the ER stress sensor IreA synergize
with the canonical UPR to influence virulence traits in
Aspergillus fumigatus. PLoS Pathog. 7:e10023302011.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Fribley AM, Miller JR, Reist TE, Callaghan
MU and Kaufman RJ: Large-scale analysis of UPR-mediated apoptosis
in human cells. Methods Enzymol. 491:57–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fiamoli V, Blatny J, Zapleta O, Kohlerova
S and Janousova E: Treatment of deep vein thrombosis with
continuous IV infusion of LMWH: a retrospective study in 32
children. Thrombosis. 2011:9814972011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhao H, Liu H, Chen Y, et al:
Oligomannurarate sulfate, a novel heparanase inhibitor
simultaneously targeting basic fibroblast growth factor, combats
tumor angiogenesis and metastasis. Cancer Res. 66:8779–8787. 2006.
View Article : Google Scholar
|
|
36
|
Basche M, Gustafson DL, Holden SN, et al:
A phase I biological and pharmacologic study of the heparanase
inhibitor PI-88 in patients with advanced solid tumors. Clin Cancer
Res. 12:5471–5480. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Xu YZ, Zhu Y, Shen ZJ, et al: Significance
of heparanase-1 and vascular endothelial growth factor in
adrenocortical carcinoma angiogenesis: potential for therapy.
Endocrine. 40:445–451. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sanderson RD and Iozzo RV: Targeting
heparanase for cancer therapy at the tumor-matrix interface. Matrix
Biol. 31:283–284. 2012. View Article : Google Scholar : PubMed/NCBI
|