Introduction
Myocardial infarction is a major public health
concern, and is one of the primary causes of mortality worldwide
(1). Thrombolysis, primary
angioplasty, and cardiac surgery are all effective therapeutic
methods to restore cardiac blood flow to the ischemic myocardium
(2), which is aimed at promptly
resuming blood supply to the ischemic myocardium and these methods
are frequently used in clinical practice. However, reperfusion
paradoxically results in insufficient protection of the myocardium
and various disorders, including inflammation, apoptosis, oxidative
stress injury and calcium overload. These pathological mechanisms
underlie the myocardial ischemic/reperfusion (MI/R) injury
(3,4), and severely influence surgical
treatment and postoperative long-term recovery. Previous studies
have demonstrated that hydrogen (H2) exerts an effective
therapeutic role in a variety of I/R injury diseases, including
MI/R (5,6), intestinal I/R injury (7), renal I/R injury (8), hepatic I/R injury (9) and retinal I/R injury (10). Hydrogen has been demonstrated to
exhibit anti-inflammation, anti-apoptosis and anti-oxidative
properties (5-9,11-13). Numerous studies have reported that
hydrogen exerts a protective role in myocardial related diseases
(6,11,14).
I/R induced-inflammatory reaction is one of the most
important elements in myocardial I/R (MI/R) injury (15). The main pathological process
consists of the release of inflammatory cytokines and the
aggregation and infiltration of inflammatory cells upon the
inflammatory response (16).
During the process of inflammation, inflammatory cells are
stimulated and various cytokines are released, including tumor
necrosis factor α (TNF-α), interleukin (IL)-6 and IL-8 (17). In addition, myocardial apoptosis
is also associated with MI/R injury (12). Myocardial apoptosis is considered
to be one of the key pathological processes in MI/R injury, and may
be associated with heart failure, the amount of which is determined
by the severity of MI/R injury (18). During MI/R injury, myocardial
apoptosis leads to myocardial contractile dysfunction, compensatory
hypertrophy and reparative fibrosis, further increasing myocardial
injury, which ultimately develops into cardiac dysfunction and
failure (19).
Autophagy contributes to normal cardiac homeostasis,
and impeding the autophagy process can lead to severe consequences
for the heart, such as the accumulation of protein aggregates and
dysfunctional organelles, generating cellular dysfunction and
cardiac failure (20). Nakai
et al (20) reported that
constitutive autophagy is a homeostatic mechanism for maintaining
cardiomyocyte size and normal cardiac structure and function. Of
note, mitophagy was activated and served a crucial role in
cardioprotection in different models of cardiac injury (21,22). The PTEN-induced kinase 1
(PINK1)/Parkin pathway exerts pivotal functions in the clearing of
defective mitochondria via autophagy in cells (23). It has also been reported that
Parkin functions as a regulator, and activates mitochondrial
autophagy for mitochondrial degradation in cardiac myocytes
(24). A recent study suggested
that PINK1/Parkin-induced mitophagy regulated mitochondrial
dynamics and function in myocytes (25). The absence of Parkin resulted in
accumulated dysfunctional mitochondria in the myocardium with age,
which led to oxidative damage and mitochondrial respiration
dysfunction (26,27).
Consequently, it was hypothesized that
PINK1/Parkin-mediated autophagy participated in the myocardial
inflammation response and apoptosis in MI/R injury, and that
hydrogen may alleviate the MI/R injury via PINK1/Parkin-mediated
autophagy. To examine this hypothesis, the present study
investigated the effect of hydrogen on myocardial inflammation
response and apoptosis in MI/R injury in vivo and in
vitro. In addition, the role of PINK1/Parkin-induced mitophagy
was explored in the hydrogen-mediated myocardial protection.
Materials and methods
Animals
A total of 72 Wistar male adult rats (age, 8-10
weeks; weight, 200-250 g) were obtained from the Laboratory Animal
Center of the Academy of Military Medical Sciences (Beijing,
China). Rats were acclimated for 1 week prior to experiments. The
rats were housed at a temperature-controlled (25°C) room under a
12-h light/dark cycle to mimic the normal physiological day-night
cycle. Standard chow and water were freely available to rats
following sterilization. All experimental protocols were approved
by the Institutional Animal Care and Use Committee of Tianjin
Medical University and were conducted in strict accordance with the
National Institutes of Health guidelines for the use of
experimental animals.
Rat MI/R model
The MI/R injury model was induced according to
previous research with some minor modifications (28). The rats were anesthetized with
sodium pentobarbital (60 mg/kg, intraperitoneally) and the thoracic
cavity was opened by left thoracotomy. After the pericardium was
incised to expose the left anterior descending coronary artery
(LAD), a 6-0 ligature was passed underneath the LAD and was tied to
produce an occlusion. Thereafter, the artery was occluded by
applying tension to the ligature. A successful ischemia was
confirmed by persistent ST segment elevation on the
electrocardiogram. After 30 min of ischemia, the ligature was
removed. Reperfusion was confirmed by visible restoration of color
in the ischemic tissue and inversion of the T wave on the
electrocardiogram. The chest and skin were closed, and the rats
were resuscitated by appropriate fluid replacement and placed on a
37°C heating pad until they were awake. The sham operation included
all procedures except ligation of the LAD.
Cell culture and hypoxia/reoxygenation
(H/R) injury
H9C2 myocardial cells were maintained in our
laboratory and obtained from the American Type Culture Collection.
Cells were grown in DMEM (Invitrogen; Thermo Fisher Scientific,
Inc.) supplemented with 10% heat-inactivated FBS (Invitrogen;
Thermo Fisher Scientific, Inc.), 100 U/ml penicillin and 100
µg/ml streptomycin, and cultured at 37°C with 5%
CO2 in a humidified atmosphere. The medium was replaced
every 2-3 days. Confluent cells were used for subsequent
experiments at 80-90% confluence, between the 4 and 6th passages.
The cells were seeded at a density of 1×106
cells/ml.
To mimic ischemic injury in vitro, the
process of H/R injury was performed as previously published
(29). Cells were cultured in
serum-free DMEM (glucose-free) in a humidified environment with 95%
N2 and 5% CO2 for hypoxic conditions.
Following a 4-h incubation, cells were transferred to normal
culture conditions with routine culture medium in a normal oxygen
environment for 24 h for reoxygenation.
Hydrogen treatment for rats in vivo
According to a previous study (6), hydrogen was dissolved in 0.9% saline
for 6 h under high pressure (0.4 MPa) to a supersaturated level by
using a hydrogen producing apparatus. Hydrogen-rich saline was
stored under an atmospheric pressure at 4°C in an aluminum bag with
no dead volume, sterilized by gamma radiation, which was freshly
prepared once a week to ensure that the concentration was
maintained at 0.6 mmol/l. A needle-type hydrogen sensor (Unisense
A/S) was used to detect the hydrogen concentration of the media,
according to the protocol described in our previous study (13). The hydrogen-rich saline was
administered via intraperitoneal injection at a dose of 10 ml/kg
and at 5 min prior to reperfusion, as described in a previous study
(30).
Hydrogen treatment for cells in
vitro
According to our previously study (13), hydrogen was diluted in normal
medium (or as indicated) to prepare 0.6 mmol/l hydrogen-rich
culture medium, using a hydrogen producing apparatus in our
department, following the same protocols as for the preparation of
hydrogen-rich saline. To ensure a 0.6 mmol/l concentration,
hydrogen-rich medium was freshly prepared each week. In the
H2 group, hydrogen-rich medium was used to culture the
cells instead of normal medium.
PINK1 small interfering (si) RNA
transfection
The PINK1-targeting siRNA and the scramble siRNA
were designed and synthesized by Santa Cruz Biotechnology, Inc.
Transfection was performed according to the manufacturer's
protocol. The sequences were: Scramble siRNA, 5′-UUC UCC GAA CGU
GUC ACG UTT-3′; and PINK1 siRNA, 5-GCC AUC UUG AAC ACA AUG ATT-3.
H9C2 cells were seeded in 6-well plates overnight, and then
transfected with PINK1 siRNA (50 nM) and scramble siRNA (50 nM)
using siRNA Lipofectamine™ 2000 transfection reagent (Invitrogen;
Thermo Fisher Scientific, Inc.).
Experiment 1: Effect of hydrogen on
infarction size of hearts and cardiac function in rats induced by
MI/R
A total of 24 rats were randomly divided into four
groups (n=6 rats per group): Control (Con), control + hydrogen
(Con+H2), MI/R (I/R), and MI/R + hydrogen
(I/R+H2) groups. MI/R injury was performed by surgical
ligation of the left coronary artery. At 24 h following
reperfusion, infarction size of hearts and cardiac function
[maximum rate of increase of left ventricular pressure
(±dp/dtmax), left ventricular ejection fraction (LVEF),
left ventricular end-diastolic pressure (LVEDP), heart rate (HR),
systolic blood pressure (SBP), diastolic blood pressure (DBP) and
mean arterial pressure (MAP)] were detected, and blood samples were
collected for the detection of creatinine kinase-muscle/brain
(CK-MB) and cardiac troponin I (cTnI) levels in the four
groups.
Experiment 2: Effect of hydrogen on
cytokines and autophagy in rats induced by MI/R
Another 24 rats were randomly divided into four
groups (n=6 rats per group). The grouping method and experimental
protocols were the same as experiment 1. At 24 h following
reperfusion, heart tissues were collected for the detection of
cytokine levels [TNF-α, IL-1β, IL-6 and high mobility group box 1
(HMGB1)] by ELISA. Apoptosis-related proteins (cleaved caspase-3,
Bcl-2 and Bax) and autophagy-associated proteins
[microtubule-associated protein 1 light chain 3α (LC3),
autophagy-related protein (ATG) 5, ATG12, Beclin1, PINK1 and
Parkin] were detected by western blotting.
Experiment 3: Effect of hydrogen on cell
viability and lactate dehydrogenase (LDH) release in H9C2 cells
stimulated by H/R in vitro
H9C2 cells were divided into four groups (n=6):
Control (Con), control + hydrogen (Con+H2), H/R
treatment (H/R), and H/R + hydrogen (H/R+H2) groups.
H9C2 cell injury was performed by hypoxia and reoxygenation, as
aforementioned. The C+H2 and I/R+H2 groups
were cultured using hydrogen-rich medium throughout both the
hypoxia and the reoxygenation. At 4 h following hypoxia and 24 h of
reoxygenation, cells were harvested to detect cell viability by the
MTT assay and LDH activity.
Experiment 4: Effect of hydrogen on
autophagy-related proteins in H9C2 cells stimulated by H/R in
vitro
H9C2 cells were divided into four groups (n=6). The
grouping method and experimental protocols were the same as
described in experiment 3. At 4 h following hypoxia and 24 h of
reoxygenation, cells were collected to detect the protein
expression levels of LC3, ATG5, ATG12, Beclin1, PINK1 and Parkin by
western blot analysis.
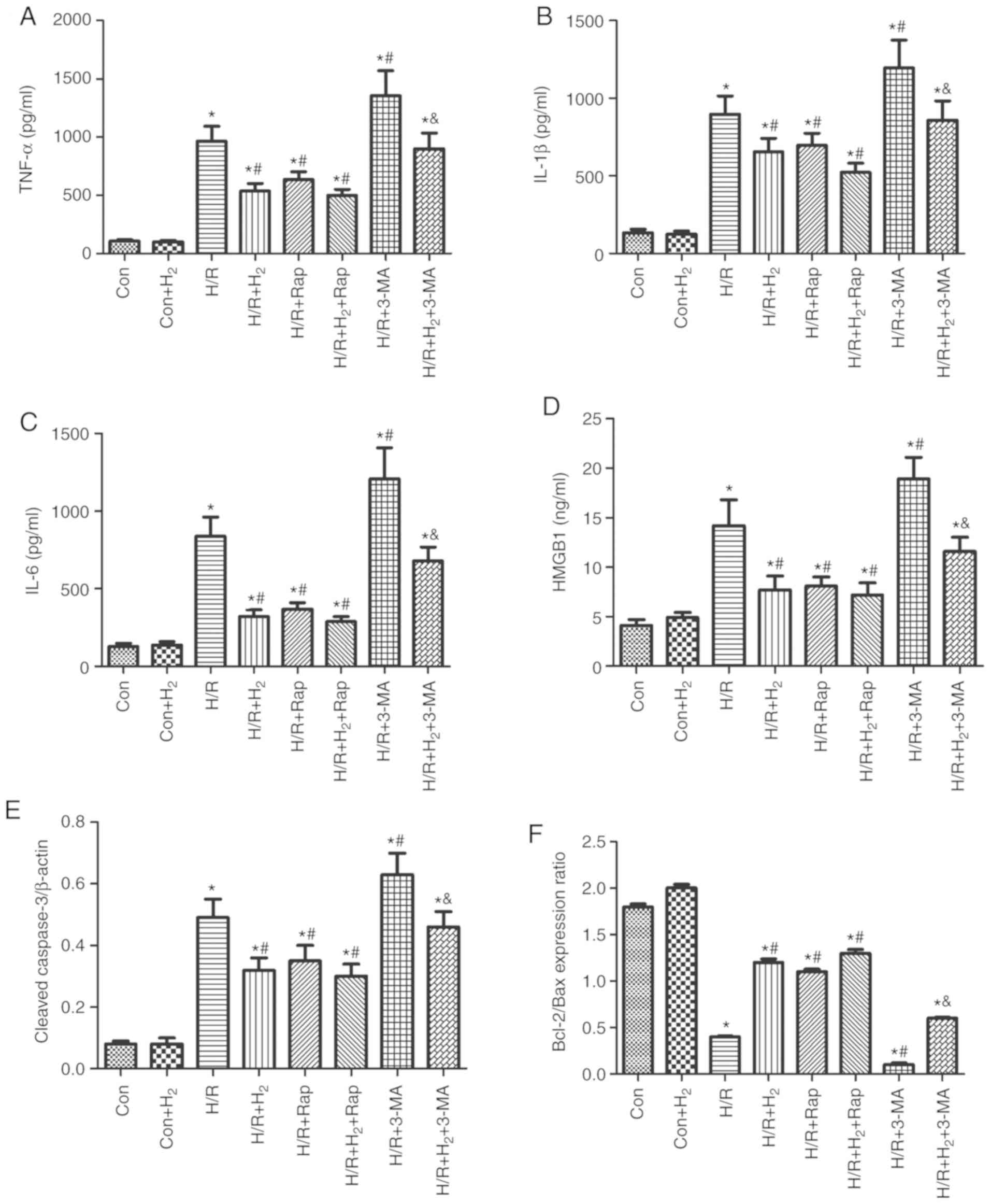
Experiment 5: Effect of autophagy on
cytokine levels and apoptosis in H9C2 cells treated with hydrogen
and H/R in vitro
H9C2 cells were divided into eight groups (n=6):
Control (Con), control + hydrogen (Con+H2), H/R
treatment (H/R), H/R + hydrogen (H/R+H2), H/R treatment
+ autophagy inducer rapamycin (H/R+Rap), H/R treatment + autophagy
inhibitor 3-MA (H/R+3-MA), H/R treatment + hydrogen + autophagy
inducer rapamycin (H/R+H2+Rap), and H/R treatment +
hydrogen+ autophagy inhibitor 3-MA (H/R+H2+3-MA) groups.
Rap (20 µM; Sigma-Aldrich; Merck KGaA) and 3-MA (1 mM;
Sigma-Aldrich; Merck KGaA) were added to the medium 2 h prior to
the experiment. Then, hydrogen, 3-MA and/or Rap were administered
throughout the hypoxia and the reoxygenation phases. At 4 h
following hypoxia and 24 h of reoxygenation, the cells were
collected to detect cytokine levels (TNF-α, IL-1β, IL-6 and HMGB1)
by ELISA and expression levels of apoptosis-related proteins
(cleaved caspase-3, Bcl-2, Bax) by western blotting.
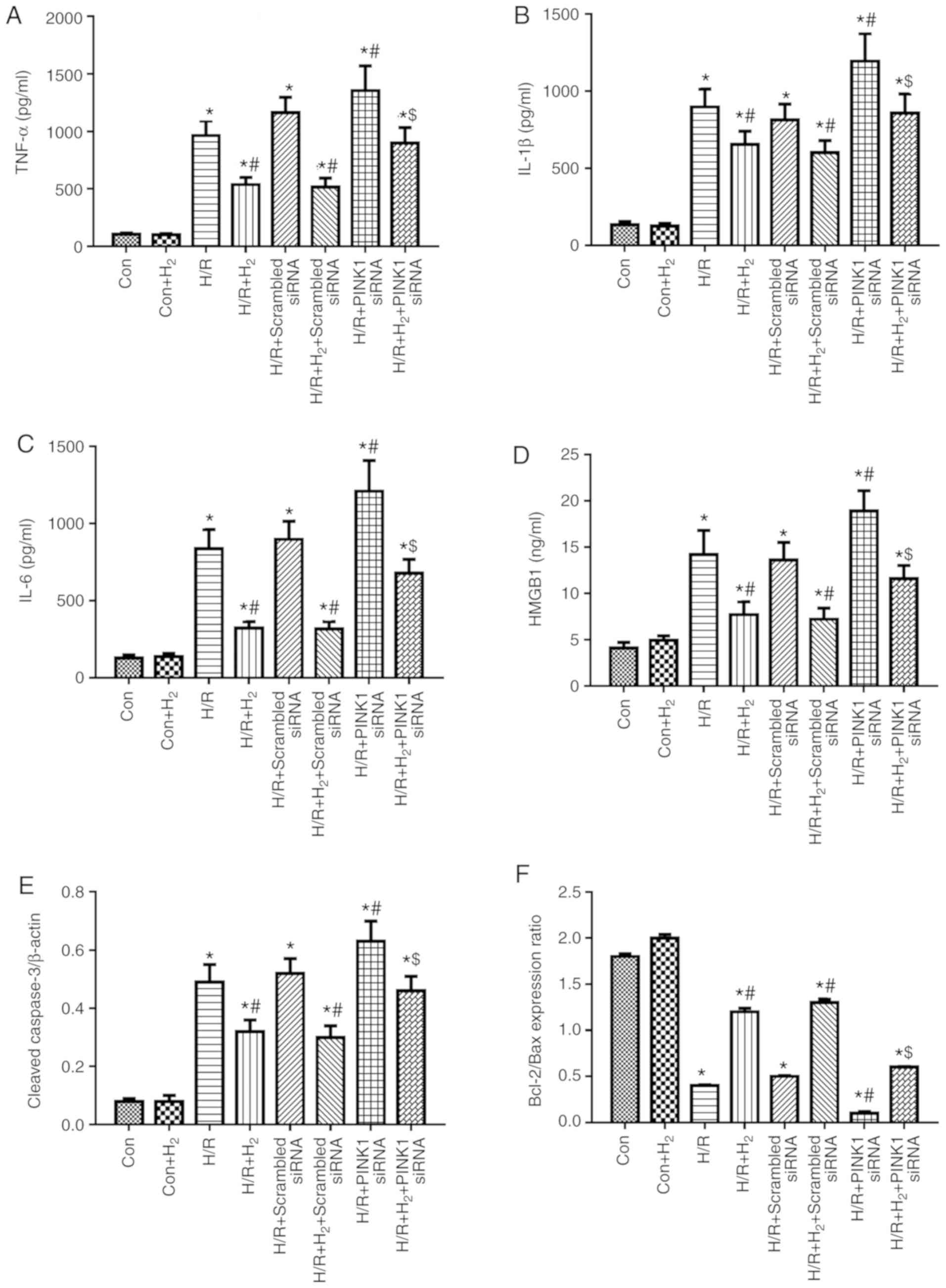
Experiment 6: Effect of PINK silencing on
cytokine levels and apoptosis in H9C2 cells treated with hydrogen
and H/R in vitro
H9C2 cells were divided into eight groups (n=6):
Control (C), control + hydrogen (C+H2), H/R treatment
(H/R), H/R treatment + hydrogen (H/R+H2), H/R treatment
+ scramble siRNA (H/R+scramble siRNA), H/R treatment + hydrogen +
scramble siRNA (H/R+H2+scramble siRNA), H/R treatment +
PINK siRNA (H/R+PINK1 siRNA), and H/R treatment + hydrogen + PINK
siRNA (H/R+H2+PINK1 siRNA) groups. At 4 h following
hypoxia and 24 h reoxygenation, cells were collected to detect
cytokine levels (TNF-α, IL-1β, IL-6 and HMGB1) by ELISA and
expression levels of apoptosis-related proteins (cleaved caspase-3,
Bcl-2 and Bax) by western blotting.
Detection of cardiac function and
hemodynamic change
Following 1 h reperfusion, a fluid-filled latex
balloon connected to a Millar transducer (pressure sensor) was
inserted into the left ventricle as described previously (14), and ±dp/dtmax, LVEF,
LVEDP, HR, SBP, DBP and MAP were measured.
Determination of myocardial infarct
size
The hearts were rapidly excised and frozen at −20°C.
The left ventricles were cut into 5 transverse slices, which were
incubated in 2% triphenyltetrazolium chloride (TTC) solution in
phosphate buffer (pH 7.4, at 37°C) in the dark for 20 min. The
slices were subsequently photographed and measured to delineate the
area of infarct size (IS; TTC-negative) and area at risk (AAR;
TTC-stained). The images were captured using a light microscope
(magnification, ×4; Leica Microsystems GmbH). Myocardial infarct
sizes (IS/AARx100%) were calculated by Image-Pro Plus software
(Media Cybernetics, Inc.).
Detection of apoptosis by TUNEL
After the experiments were performed, the heart
tissue was collected to detect apoptosis by using an in situ Cell
Death Detection kit (Roche Diagnostics), according to the
manufacturer's protocol. The heart tissue was perfused with 10%
formalin and placed in 10% formalin for 24 h in room temperature,
embedded in paraffin, and sectioned into 5-µm thickness
slices. Paraffin sections of heart tissue were stained with the
TUNEL kit, which results in the nuclei of apoptotic cells to be
stained red. Total DNA in all cell nuclei was counterstained blue
with DAPI. The apoptosis rate was calculated as the ratio of red to
blue stained nuclei and relative to the control group.
Detection of CK-MB and cTnI release in
serum
After the measurement of hemodynamics and cardiac
function parameters, blood samples were collected from the heart.
The serum was separated by centrifugation at 3,000 × g for 15 min
at 4°C, aliquoted, and stored at −20°C until subsequent
experimentation. The levels of CK-MB and cTnI were detected using
commercially available ELISA kits on a microplate reader (cat. no.
AKC0305 for CK-MA; cat. no. MA1-20112. for cTnI; Thermo Fisher
Scientific, Inc.). All procedures were performed in accordance with
the manufacturer's protocol.
Cytokine detection by ELISA
Following 1 h of reperfusion or 24 h of
reoxygenation, heart tissues and culture media were collected for
the detection of cytokine levels by ELISA. Heart tissues were
homogenized and centrifuged at 10,000 × g for 20 min at 4°C, and
the cell culture media was collected and centrifuged at 3,000 × g
for 10 min at 4°C. The supernatants were harvested and stored at
−20°C until detection of the cytokines TNF-α (cat. no. RTA00;
R&D Systems, Inc.), IL-1β (cat. no. RLB00; R&D Systems,
Inc.), IL-6 (cat. no. R6000B; R&D Systems, Inc.) and HMGB1
(cat. no. ST51011; IBL International GmbH) by ELISA, according to
the manufacturer's protocol.
Analysis of cell viability and LDH
activity
H9C2 cells were seeded in a 96-well plate for at
least 12 h at a density of 1×104 cells/well and then
were subjected to the different treatments. Cell viability was
determined by the MTT assay, and cytotoxicity was detected by an
LDH assay. Briefly, after 24 h of reoxygenation, MTT (5 mg/ml) was
added to the medium supplemented with 10% FBS for 4 h at 37°C, then
the medium was discarded, and formazan blue was dissolved in 100
µl of DMSO. The absorbance was detected at 490 nm using a
microplate reader. Relative cell viability was quantified relative
to the control group. The cells in the control group were
considered 100% viable.
Cardiomyocyte injury was measured by LDH release. At
24 h following reoxygenation, the supernatant was harvested to
detect LDH activity, according to the manufacturer's protocol (cat.
no. 04744926001; Roche Diagnostics GmbH). LDH activity was
expressed as a percentage relative to the control cell
cultures.
Western blot analysis
Following 1 h of reperfusion or 24 h of
reoxygenation, heart tissue and H9C2 cells were collected for the
detection of caspase-3, Bcl-2, Bax, ATG5, ATG12, Beclin1, PINK1 and
Parkin by western blotting. Heart tissue or H9C2 cells were
resuspended in radioimmunoprecipitation assay (RIPA) lysis buffer
(Beyotime Institute of Biotechnology) on ice for 30 min. The
samples were centrifuged at 15,000 × g for 20 min at 4°C, and the
supernatants were collected and boiled for 5 min. Protein
concentrations were quantified using the Bradford protein assay
(Thermo Fisher Scientific, Inc.). Denatured proteins (15 µg)
were separated by 12% SDS-PAGE and then electrotransferred onto
polyvinylidene difluoride membranes (EMD Millipore). Following
blocking with 5% non-fat milk blocking buffer for 1 h at room
temperature, the membranes were incubated with primary antibodies
(all from Abcam) against cleaved caspase-3 (cat. no. ab13847;
1:500), Bcl-2 (cat. no. ab196495; 1:1,000), Bax (cat. no. ab32503;
1:2,000), LC3 (cat. no. ab48394; 1:1,000), ATG5 (cat. no. ab108327;
1:2,000), ATG12 (cat. no. ab155589; 1:1,000), Beclin1 (cat. no.
ab62557; 1:1,000), PINK1 (cat. no. ab23707; 1:500) and Parkin (cat.
no. ab77924; 1:500) and β-actin (cat. no. ab8227; 1:1,000)
overnight at 4°C. The membranes were subsequently washed with PBS
three times and incubated with secondary antibodies (cat. nos.
ab6721 and ab6728; 1:5,000; Abcam) at room temperature for 1 h. The
labeled bands were visualized with an enhanced chemiluminescence
reagent using the Bio-Rad Gel Doc 2000 system (Bio-Rad
Laboratories, Inc.), and quantified with the QuantityOne software
(v4.6; Bio-Rad Laboratories, Inc.). Protein expressions were
normalized to β-actin.
Statistical analysis
All data are presented as the mean ± standard error
of the mean. Statistical analysis was performed using GraphPad
Prism 5 (GraphPad Software, Inc.). Differences between groups were
evaluated by one-way analysis of variance followed by Tukey's post
hoc test. P<0.05 was considered to indicate a statistically
significant difference.
Results
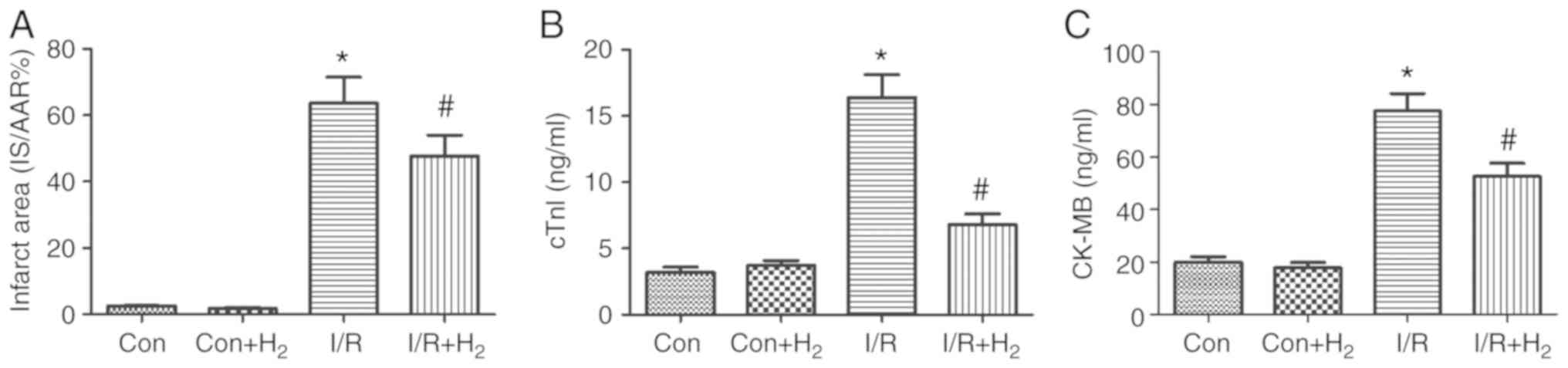
Hydrogen alleviates myocardial infarction
size of hearts
MI/R leads to myocardial cell injury (31). To investigate the effect of
hydrogen on myocardial injury, TTC staining was performed to
analyze the infarct area, and cTnI and CKMB levels were detected in
the hearts of MI/R-treated rats. Compared with the control group,
myocardial infarct, cTnI and CKMB were significantly elevated in
the I/R group (P<0.05; Fig.
1A-C). Compared with the I/R group, these indicators of
myocardial injury were significantly attenuated in the
IR+H2 group (P<0.05; Fig. 1A-C). These results indicated that
hydrogen alleviated myocardial injury induced by I/R.
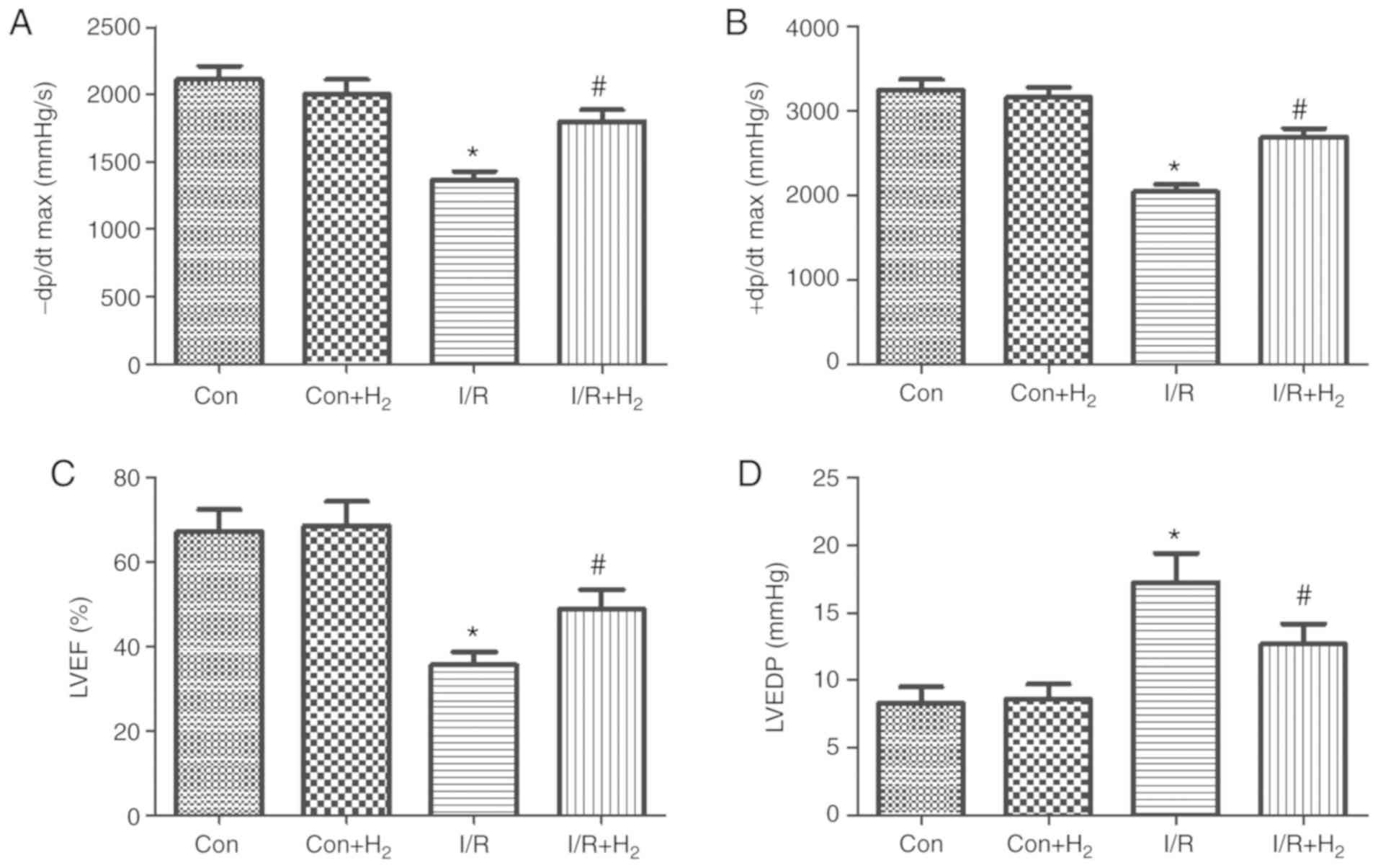
Effect of hydrogen-rich saline on cardiac
function
To investigate the effect of hydrogen on cardiac
function, the present study measured cardiac function and
hemodynamic indexes in MI/R-treated rats, namely
±dp/dtmax, LVEF, LVEDP, HR, SBP, DBP and MAP. Compared
with the control group, ±dp/dtmax and LVEF at the end of
the reperfusion period were significantly decreased, and LVEDP was
increased, in the I/R group (P<0.05; Fig. 2A-D). Treatment with hydrogen
significantly increased the value of ±dp/dtmax and LVEF,
and decreased LVEDP at the end of the reperfusion period in the
I/R+H2 group (P<0.05; Fig. 2A-D).
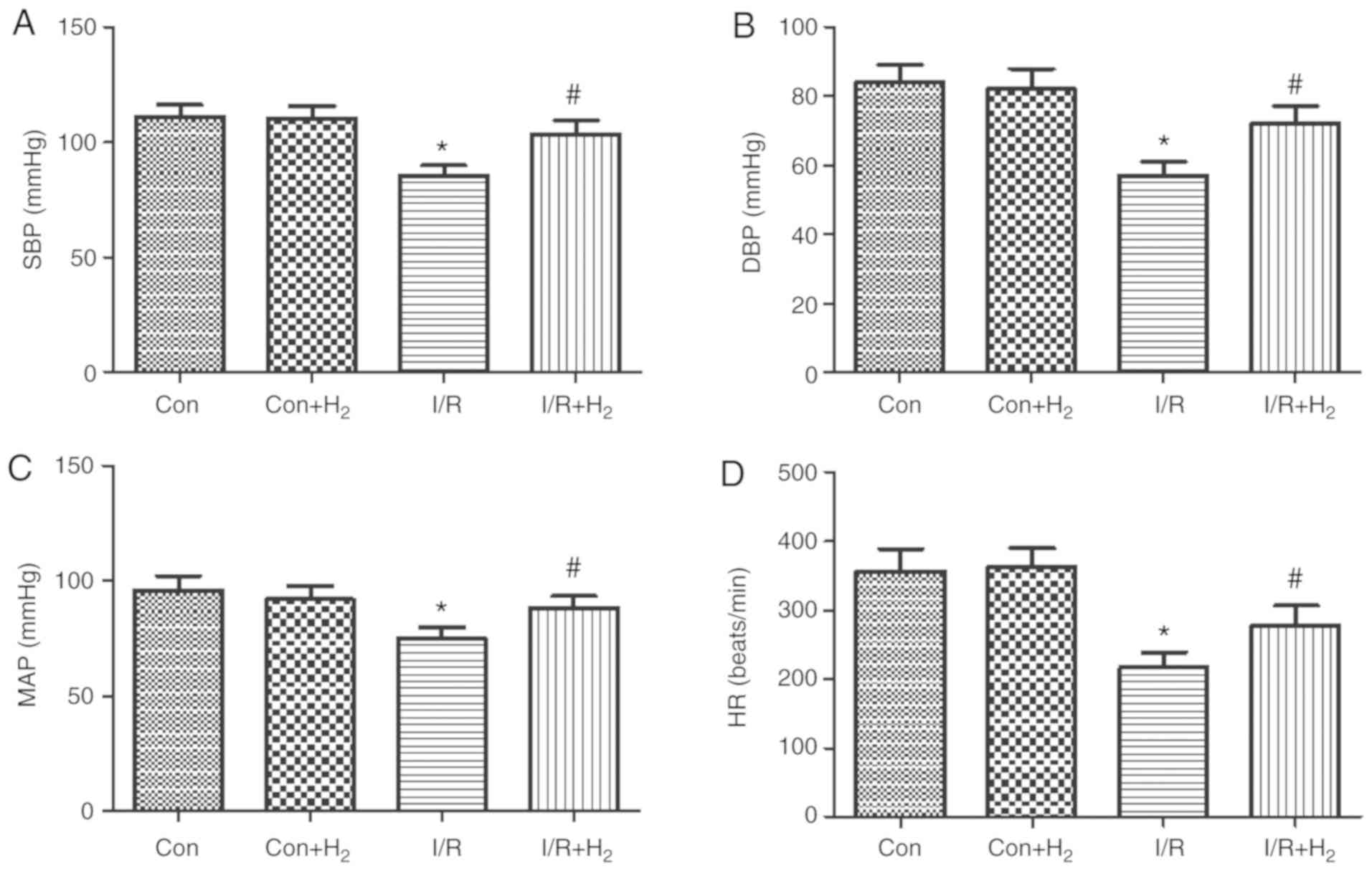
MI/R induced deterioration of the hemodynamic
indexes (HR, SBP, DBP and MAP) in the I/R group compared with the
control group (P<0.05; Fig.
3A-D). Compared with the I/R group, hydrogen-rich saline
administration improved the absolute values of HR, SBP, DBP and MAP
in the I/R+H2 group (P<0.05; Fig. 3A-D). Taken together, these results
indicated that hydrogen-rich saline contributed to the recovery of
cardiac function and hemodynamic change and improved the tolerance
of hearts against I/R injury.
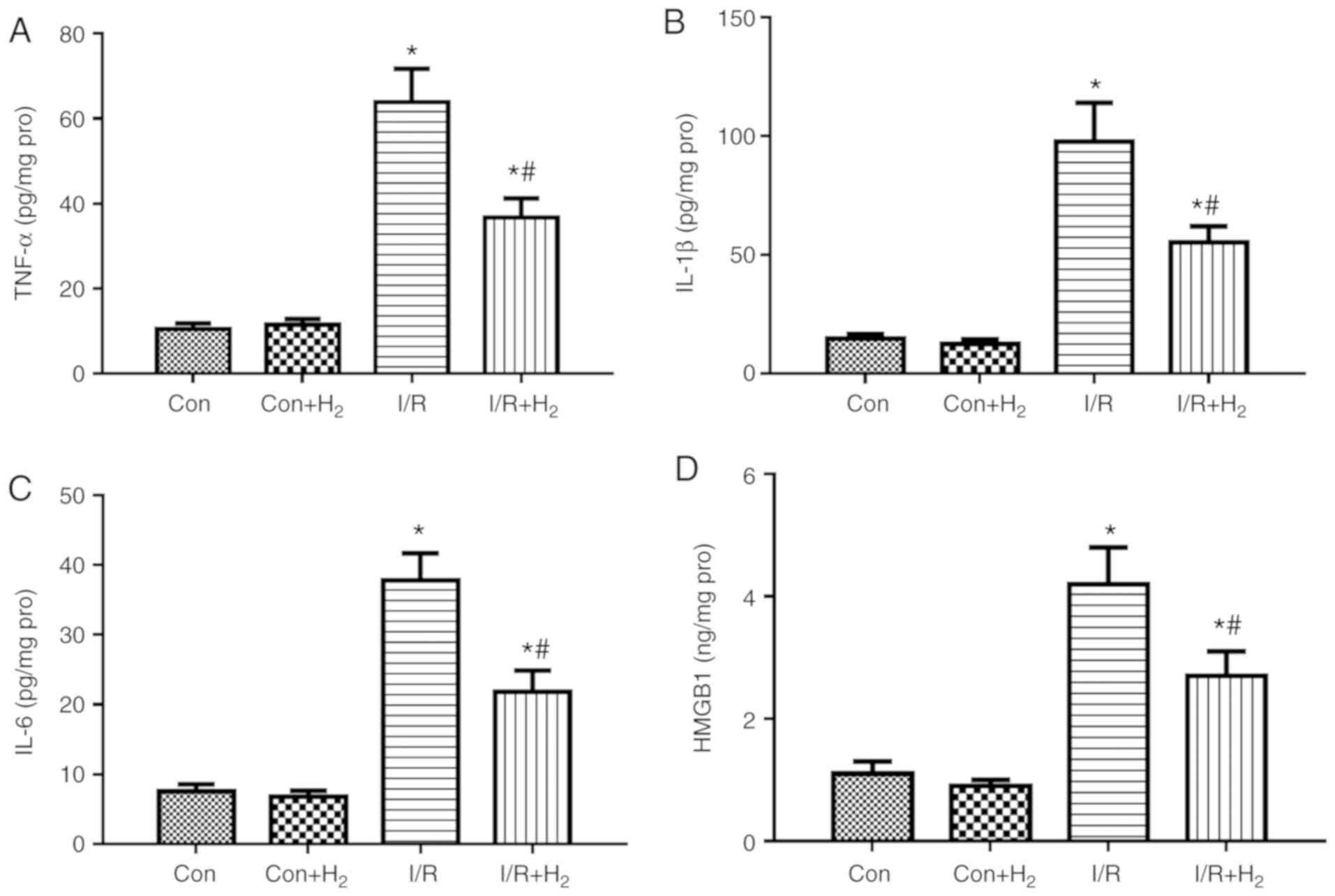
Hydrogen attenuates the expression of
cytokines and apoptosis-related proteins following MI/R in
rats
Inflammatory reaction is an integral part of the
immune response to myocardial I/R injury (31). Markers of inflammation, such as
TNF-α and IL-6, are usually present at undetected levels in the
normal heart; however, they are upregulated under stressful
conditions, such as MI/R injury (32). To examine the effect of hydrogen
on cytokine production in MI/R rats, the present study detected the
levels of TNF-α, IL-1β, IL-6 and HMGB1 in the hearts of the rats at
the end of reperfusion. The results demonstrated that the release
of TNF-α, IL-1β IL-6 and HMGB1 was significantly increased in the
I/R group compared with the control group, while treatment with
hydrogen-rich saline significantly downregulated the levels of the
inflammatory markers in the I/R+H2 group (P<0.05;
Fig. 4A-D).
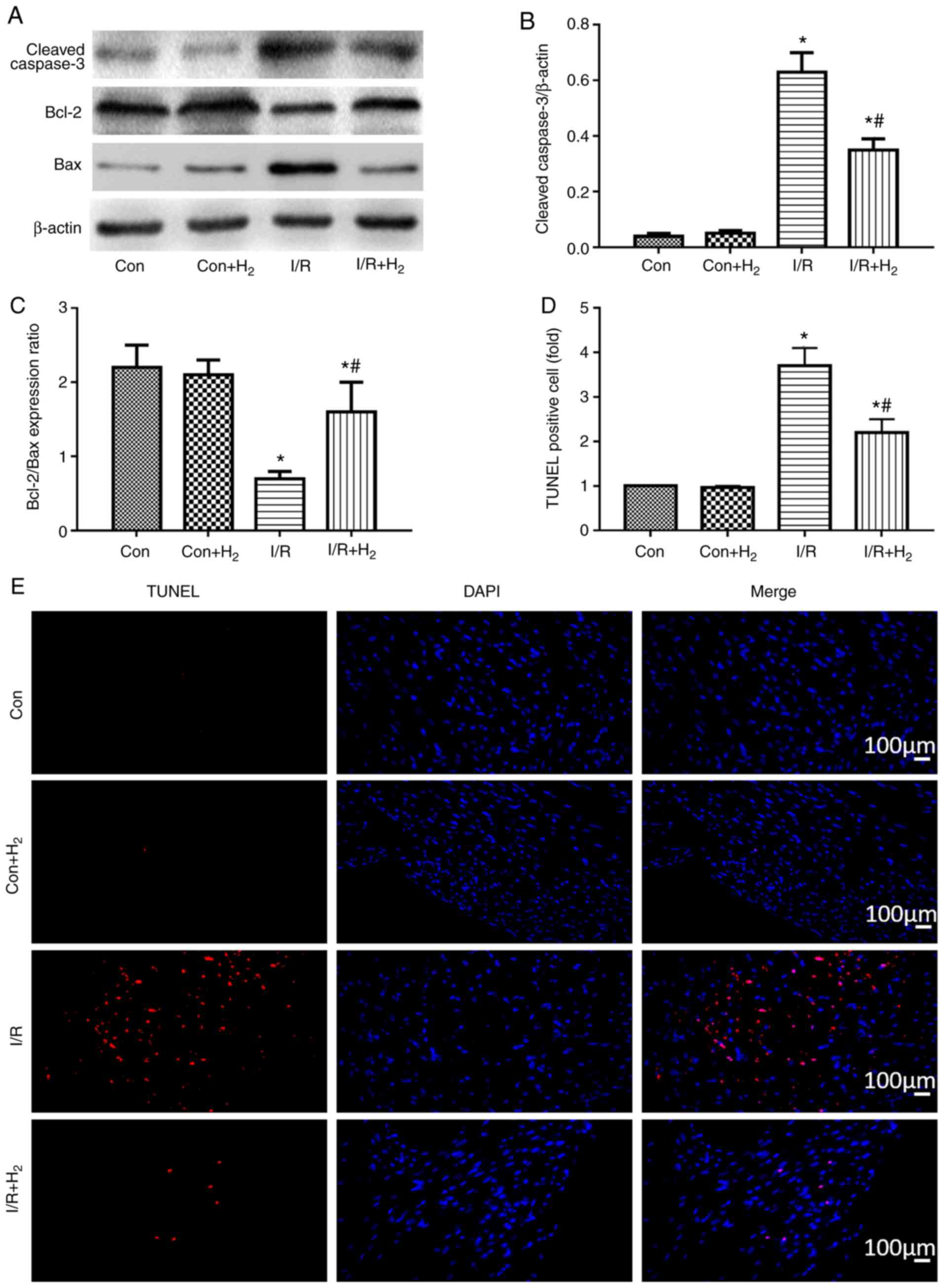
The present study then investigated whether hydrogen
regulated myocardial apoptosis induced by I/R injury, by detecting
the expression levels of the cleaved caspase-3, Bcl-2 and Bax
proteins in myocardial rat tissues using western blotting.
Caspase-3 and Bax are proapoptotic proteins, while Bcl-2 is
anti-apoptotic (33). Caspase-3
levels were higher and Bcl-2/bax ratio was lower in the I/R group,
compared with the control group (P<0.05; Fig. 5A-C). Compared with the I/R group,
caspase-3 expression was reduced, while the Bcl-2/bax ratio was
increased, in the I/R+H2 group (P<0.05; Fig. 5A-C). Apoptosis rates were further
confirmed in the myocardial tissues by TUNEL staining. I/R
treatment increased the number of apoptotic cells in the heart
sections compared with the control group, while administration of
hydrogen-rich saline markedly reversed this I/R-induced effect
(Fig. 5D and E). These results
indicated that hydrogen administration improved myocardial cell
apoptosis following reperfusion.
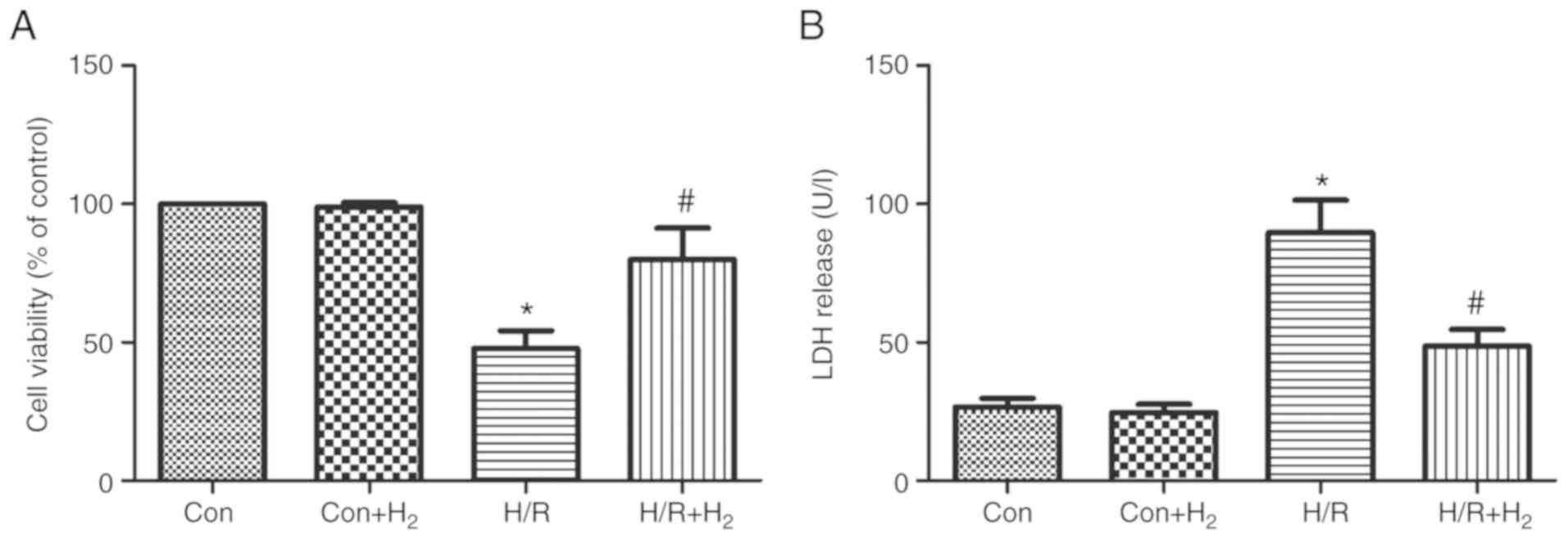
Effect of hydrogen on cell viability and
LDH release following hypoxia and reoxygenation in myocardial
cells
The present study used the MTT assay to assess the
effect of hydrogen on cell viability following H/R in myocardial
cells. The results revealed that cell viability was reduced
following H/R in myocardial cells compared with the control group
(P<0.05; Fig. 6A); however,
hydrogen significantly increased the cell viability in the
H/R+H2 group compared with the H/R group (P<0.05;
Fig. 6A). The present study also
investigated the cell toxicity by measuring the release of LDH. H/R
induced LDH increase in the H/R group compared with the control
group (P<0.05; Fig. 6B). LDH
release was significantly decreased in the H/R+H2 group
compared with the H/R group (P<0.05; Fig. 6B).
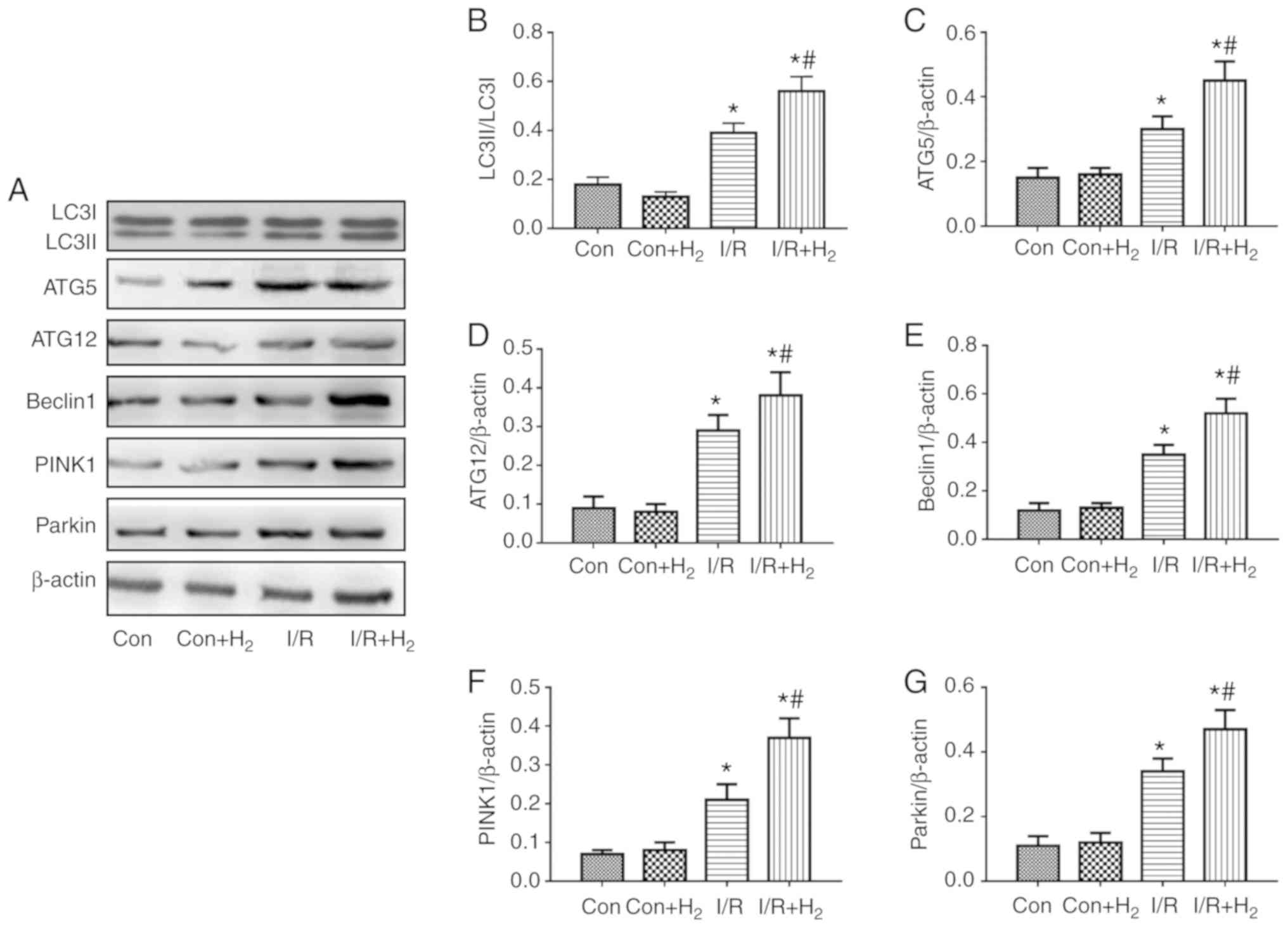
Expression of autophagy-related proteins
following treatment with hydrogen in injury induced by I/R and H/R
in vivo and in vitro
To examine the effects in autophagy in myocardial
cells, the present study measured the protein expression levels of
ATG5, ATG12 and Beclin1 by western blotting in injured myocardial
cells induced by I/R in vivo and H/R in vitro. The
results demonstrated that the ratio of LC3II/LC3I, ATG5, ATG12 and
Beclin1 expression levels were increased in the I/R group compared
with the control group, while hydrogen further augmented these
effects in the I/R+H2 group when compared with the I/R
group (P<0.05; Fig. 7A-E). The
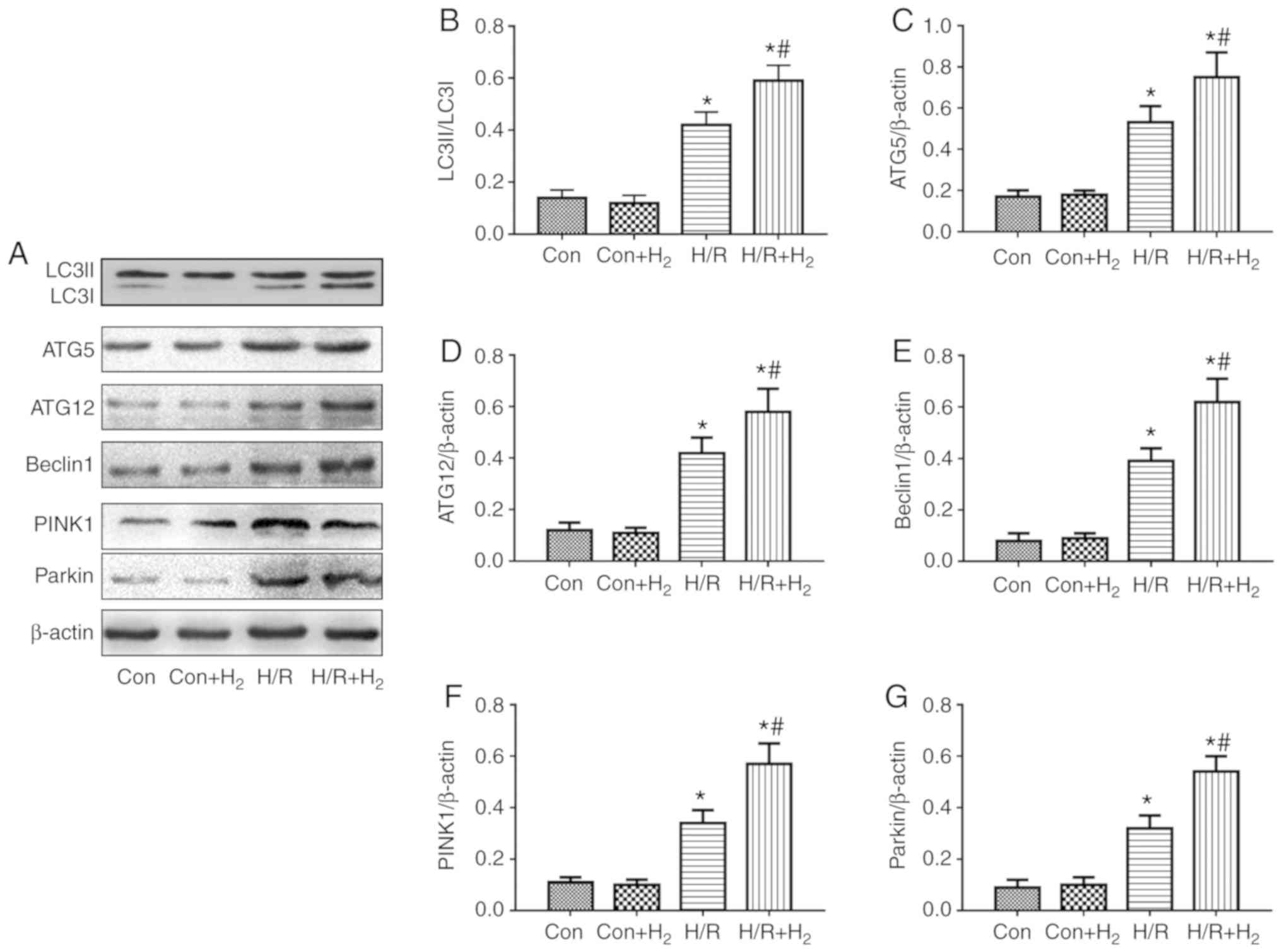
results from the in vitro experiments were consisted with
the in vivo protein expression; H/R induced an increase in
the ratio of LC3II/LC3I, and in ATG5, ATG12 and Beclin1 protein
expression compared with the control group, and hydrogen further
increased these effects (Fig.
8A-E).
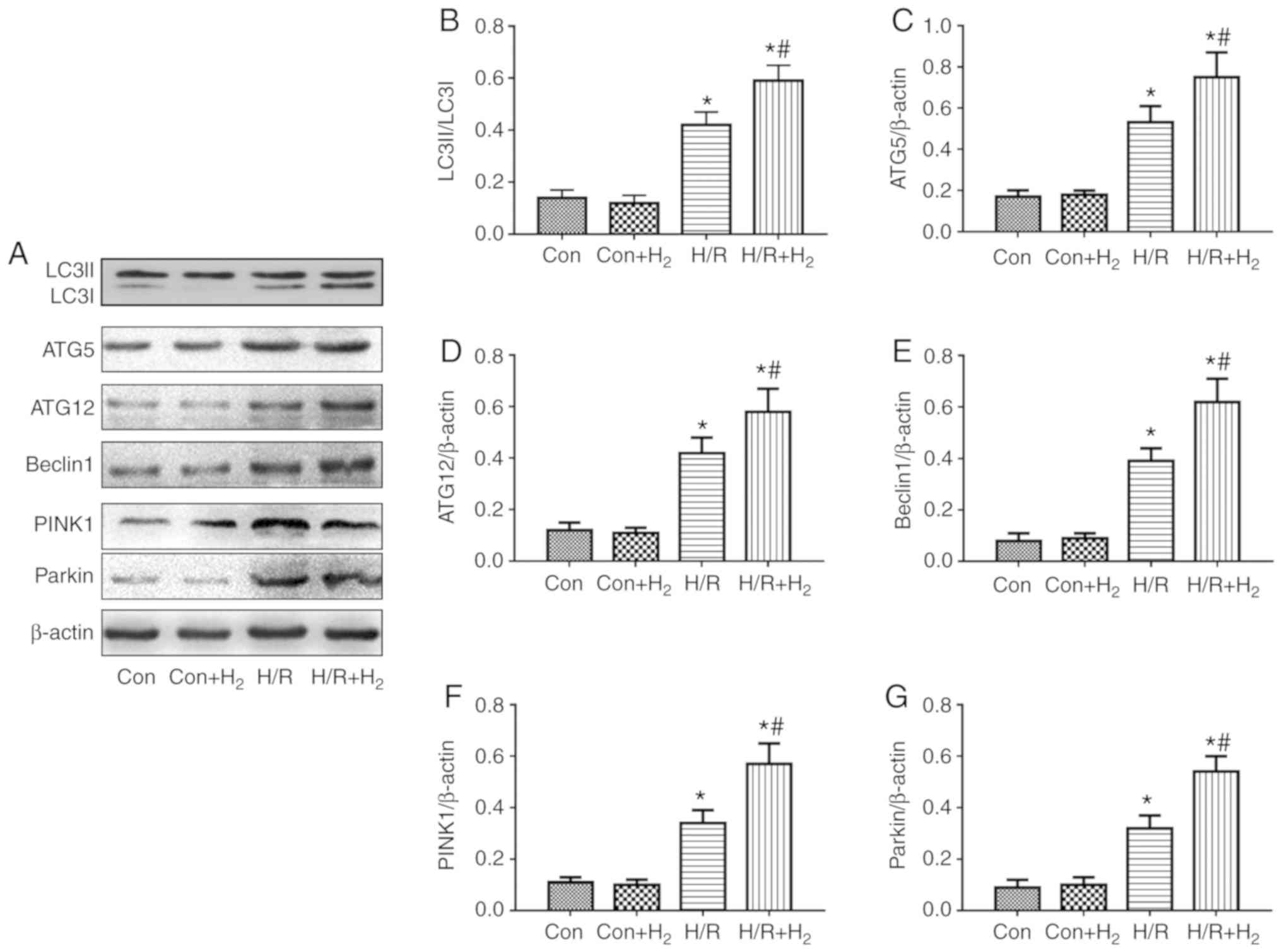 | Figure 8Effect of hydrogen on
autophagy-associated protein expression following cell injury
induced by H/R in H9C2 cells. Myocardial injury in vitro was
induced by hypoxia followed by reoxygenation. Following a 4 h
hypoxia, normal medium was replaced with hydrogen-rich medium in
the Con+H2 and H/R+H2 groups. At 24 h
following reoxygenation, cells were harvested to detect the
expression levels of autophagy-associated proteins by western
blotting. (A) Representative blot images. (B) Quantification of
LC3, (C) ATG5, (D) ATG2, (E) Beclin1, (F) PINK1 and (G) Parkin
levels. Values are presented as the mean ± standard error of the
mean (n=6). *P<0.05 vs. control group; and
#P<0.05 vs. H/R group. H/R, hypoxia/reoxygenation;
Con, control; LC3, microtu-bule-associated protein 1 light chain
3α; ATG, autophagy-related protein; PINK1, PTEN-induced kinase
1. |
Mitophagy mediated by PINK1/Parkin exerts a crucial
function in the degradation process of injured mitochondria
(34). The results of the present
study demonstrated that PINK1 and Parkin were increased in the I/R
group in vivo compared with the control group, and treatment
with hydrogen enhanced the expressions of PINK1 and Parkin in
myocardial tissue in the I/R+H2 group (P<0.05;
Fig. 7A,F and G). These results
were also observed in vitro. Compared with the control
group, H/R induced the expressions of PINK1 and Parkin in
myocardial cells, while a further increase was observed following
hydrogen treatment (P<0.05; Fig.
8A,F and G).
Hydrogen treatment improves cytokines
release and apoptosis via autophagy in H/R-induced myocardial cell
injury in vitro
The aforementioned results demonstrated that
hydrogen exerted an anti-inflammatory response via decreasing the
level of cytokines and an anti-apoptotic effect via increasing the
Bcl-2/bax ratio and reducing caspase-3 in rats with I/R injury. In
addition, it was observed that treatment with hydrogen improved the
expression of proteins associated with autophagy in I/R rats. In
order to investigate whether hydrogen regulated inflammation and
apoptosis via autophagy in myocardial cells, the present study
investigated the effect of autophagy, using rapamycin or 3-MA to
induce or inhibit the autophagy process, respectively.
The present results demonstrated that H/R induced
the release of the cytokines TNF-α, IL-1β, IL-6 and HMGB1, and
enhanced the expression of caspase-3 in H9C2 cells (P<0.05;
Fig. 9A-E). In addition, the
Bcl-2/Bax ratio was decreased in myocardial cells stimulated by H/R
compared with the control group (P<0.05; Fig. 9F). Treatment with hydrogen
alleviated the excessive release of the cytokines, increased the
expression of caspase-3, and decreased the Bcl-2/Bax ratio in the
H/R+H2 group, compared with the H/R group (P<0.05;
Fig. 9A-F). Similarly, in
comparison to the H/R group, there was a decrease in cytokine and
caspase-3 expression levels, and an increase in the Bcl-2/Bax
ratio, in the H/R+Rap and H/R+H2+Rap groups (P<0.05;
Fig. 9A-F). Treatment with 3-MA
partly reversed the inhibitory effect of hydrogen and Rap on
cytokine expression, caspase-3 and promotion of the Bcl-2/Bax ratio
in H/R myocardial cells (Fig.
9A-F).
Hydrogen exerts anti-inflammatory and
anti-apoptotic effects in myocardial cells induced by H/R via
PINK/Parkin-mediated autophagy
Autophagy, especially mitophagy, is a critical
process of elimination of damaged organelles in the cells process
during MI/R injury (35,36). PINK1/Parkin serve a key regulatory
role in autophagy and mitophagy (24). Our previous research demonstrated
that hydrogen could regulate PINK1 and Parkin in myocardial cells
induced by H/R. The present study used a PINK1-specific siRNA to
knock down its expression in myocardial cells, and successful
knockdown was confirmed (Fig.
S1). Compared with the H/R or H/R+H2 groups, there
was not a significant difference in TNF-α, IL-1β, IL-6 and HMGB1,
caspase-3, Bcl-2/Bax ratio in H/R+scramble siRNA group or
H/R+H2+scramble siRNA group, respectively (P<0.05;
Fig. 10A-F). However, compared
with the H/R or H/R+H2 groups, levels of TNF-α, IL-1β,
IL-6 and HMGB1 were increased, caspase-3 expression was enhanced
and the Bcl-2/Bax ratio was decreased in the H/R+PINK1siRNA or
HR+H2+PINK1siRNA groups, respectively (P<0.05;
Fig. 10A-F). These results
indicated that PINK silencing reversed the anti-inflammatory and
anti-apoptotic effects of hydrogen in myocardial cells induced by
H/R.
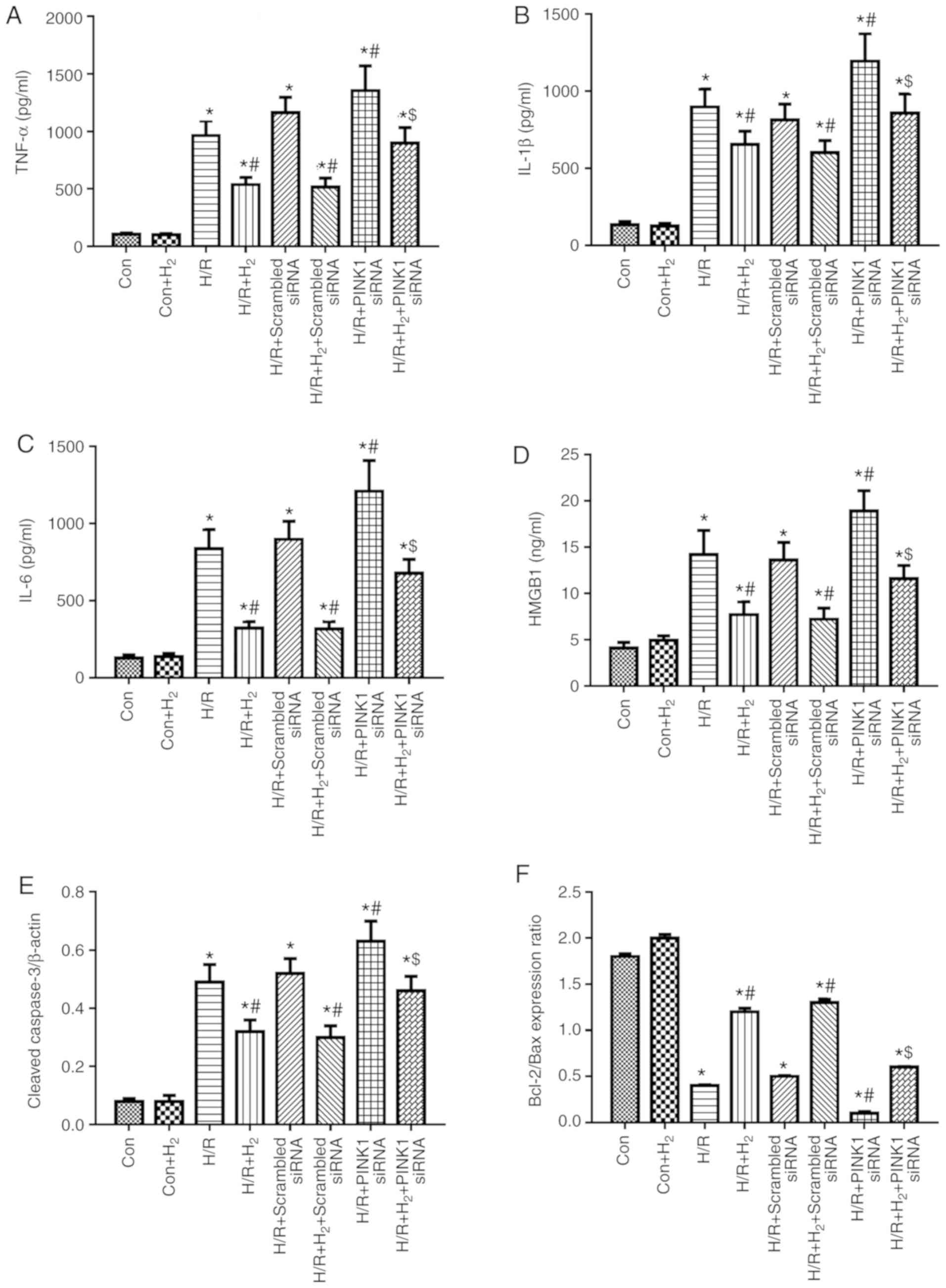 | Figure 10Effect of hydrogen on cytokine levels
and apoptosis induced by H/R in H9C2 cells. Prior to the
experiment, scramble control siRNA and PINK1-specific siRNA were
transfected into H9C2 cells. Myocardial injury and hydrogen
treatment were described in Fig.
6. At 24 h following reoxygenation, cells were harvested to
detect the levels of (A) TNF-α, (B) IL-1β, (C) IL-6 and (D) HMGB1
by ELISA. (E) The expression levels of cleaved caspase-3 and (F)
the Bcl-2/Bax ratio were detected by western blotting. Values are
presented as the mean ± standard error of the mean (n=6).
*P<0.05 vs. control group; #P<0.05 vs.
H/R group; and $P<0.05 vs. H/R+H2 group.
H/R, hypoxia/reoxygenation; siRNA, small interfering RNA; PINK1,
PTEN-induced kinase 1; TNF, tumor necrosis factor; IL, interleukin;
HMGB1, high mobility group box 1; Con, control. |
Discussion
Myocardial infarction is one of the main causes of
mortality, and its incidence continues to increase worldwide, while
the early restoration of coronary blood flow is conducive to
attenuate myocardial tissue injury (1). However, reperfusion may lead to
further myocardial injury, including inflammation response
(37), apoptosis (38) and oxidative damage (39). Hydrogen has been observed to exert
an anti-inflammatory, anti-apoptotic and anti-oxidative injury
effect, and has a protective role in heart diseases (6). In the present study, the effect of
hydrogen on MI/R injury was investigated, and the mechanism
associated with I/R injury in myocardial cells in vivo and
in vitro was discussed. The results demonstrated that
hydrogen-rich saline attenuated the myocardial infarction size and
improved cardiac dysfunction, and exerted anti-inflammatory and
anti-apoptotic effects in the heart tissues in vivo.
Treatment with hydrogen-rich media also reduced myocardial cell
injury in vitro. In addition, myocardial cell injury
contributed to the activation of autophagy, which was evidenced by
an increase in the protein expression levels of LC3, ATG-5, ATG12,
Beclin1, PINK1 and Parkin in vivo and in vitro;
hydrogen could affect the expression of these proteins in
vivo and in vitro, via the PINK1/Parkin pathway. These
findings indicated that hydrogen regulated the process of autophagy
and further alleviated the inflammation response and apoptosis in
myocardial cell injury.
Therapy for myocardial ischemic disease depends on
myocardial reperfusion treatment; however, this process not only
has complex obstacles for effective treatment, but also induces
cardiac dysfunction (40). For
the recovery of cardiac function, myocardial enzyme release and
infarct size measurement have been considered as endpoints for I/R
injury evaluation (41). Nandi
et al (42) reported that
MI/R led to cardiac dysfunction and NaHS had a protective role. It
has previously been reported that hydrogen exerts myocardial
protection from heart diseases via inhibiting oxidative injury,
apoptosis and cytokines release (6,11,43,44). In addition, hydrogen protected
from MI/R injury via regulating the glycogen synthase kinase 3β
(GSK3β) and autophagy signaling pathways (45,46). The present study predominantly
focused on hydrogen treatment on MI/R injury and the mechanism of
PINK1-mediated autophagy. The present results demonstrated that
MI/R deteriorated the myocardial infarction size, and the markers
±dp/dtmax, LVEF and LVEDP and HR, SBP, DBP and MAP in
MI/R injured rats. According to previously published research
(47,48), 10 ml/kg hydrogen-rich saline was
safe and had a positive therapeutic effect on MI/R injury.
Similarly, the present study found that hydrogen improved
myocardial infarction size, cardiac function and hemodynamic
changes following reperfusion of cardiac blood flow. In addition,
in the in vitro experiments, hydrogen ameliorated the LDH
release and increased the cell viability in myocardial cell injury
stimulated by H/R. These results were consistent with the finding
that hydrogen-rich saline improved the hemodynamic parameters LVSP,
+(dP/dt)max, and -(dP/dt)max and infarct size
in MI/R-treated rats (11).
Apoptosis is a major cause of tissue damage, second
only to reperfusion injury following ischemia (47). It has recently been reported that
myocardial apoptosis is initiated by ischemia and amplified by
reperfusion, which partially contributes to myocardial dysfunction
and cardiomyocyte death and even heart failure (48,49). Caspase-3 exerts a pivotal role in
the process of cell apoptosis, which is downstream of the Bcl-2
family (50). The Bcl-2 family
includes the anti-apoptotic Bcl-2 and the pro-apoptotic Bax, and an
increased Bcl-2/Bax ratio represents a protective effect of cells
against apoptosis (50). In the
process of apoptosis, Bcl-2 is capable of forming a heterodimer
with Bax, thereby preventing Bax homodimerization and the
sequential activation of caspase-3 (51). Numerous studies have demonstrated
that MI/R or H/R induce myocardial apoptosis in in vivo and
in vitro experiments (52,53). Sun et al (11) reported that I/R led to myocardial
cell apoptosis by detection of caspase-3 and TUNEL and that
hydrogen attenuated apoptosis in myocardial cells. This was
corroborated by the findings of the present study. Treatment with
hydrogen obviously inhibited apoptosis, by mitigating caspase-3
expression and alleviating the Bcl-2/bax ratio in MI/R-treated
heart tissues, and hydrogen administration in vitro
attenuated apoptosis in myocardial cell injury induced by H/R.
Myocardial apoptosis triggers the inflammatory response and the
release of excessive cytokines from the infarcted myocardium after
acute myocardial infarction, consequently the secreted cytokine
TNF-α further stimulates infiltrating leukocytes and endothelial
cells to release proinflammatory cytokines, such as IL-1β and IL-6,
which then initiates the inflammation cascade, inflammation
response, and the subsequent myocardial dysfunction (54-57). Downregulation of HMGB1 was
reported to partially reduce myocardial I/R injury (58). In the present study, I/R or H/R
injury caused the excessive release of TNF-α, IL-1β, IL-6 and HMGB1
in myocardium tissues and cells, and treatment with hydrogen
significantly inhibited these effects.
Numerous studies have reported that under conditions
of cellular stress, autophagy is increased in the myocardium, which
is initially a protective response activated by the cells (20,23,35). ATG5, ATG12, beclin1 and LC3 are
key regulatory proteins of autophagy in cells (59). Decreased mitochondrial autophagy
(termed mitophagy) can cause inflammation and cell death, which
results in degenerative diseases (60). The PINK1/Parkin pathway is
associated with marking dysfunctional mitochondria for clearance by
autophagy (61). PINK1-deficiency
increased the susceptibility of the heart to I/R injury ex
vivo (62). PINK1-deficiency
in mice contributed to heart failure more rapidly in response to
pressure overload compared with wild-type mice (63). It has previously been reported
that hydrogen-rich saline exerts a protective role in myocardial
I/R injury via anti-oxidative, anti-apoptosis and anti-inflammation
mechanisms, which inhibit endoplasmic reticulum stress, regulate
Akt and GSK3β protein expression and the expressions of the
autophagy-related proteins mammalian target of rapamycin (mTOR),
Beclin1 and LC3, and mitochondrial-associated protein expression
(30,44,64). Based on this previous literature,
the present study focused on the mechanisms associated with
autophagy, and then further examined the effect of
PINK1/Parkin-mediated autophagy. The results of the present study
indicated that MI/R or myocardial H/R induced mitophagy by
increasing the expression levels of LC3, ATG5, ATG12, beclin1,
PINK1 and Parkin in vitro and in vivo, which are
markers of mitophagy activity in cells. To further investigate the
effect PINK1/Parkin-mediated autophagy on the hydrogen-treated
myocardial H/R injury, specific siRNAs were used to silence the
expression PINK1 in myocardial cells. Compared with the H/R group,
PINK1 silencing elevated the expression levels of the cytokines
TNF-α, IL-1β, IL-6 and HMGB1, elevated caspase-3 expression, and
decreased the Bcl-2/Bax ratio following H/R in myocardial cells.
Therefore, PINK1 silencing partly reversed the protective effect of
hydrogen on inflammation response and apoptosis in
vitro.
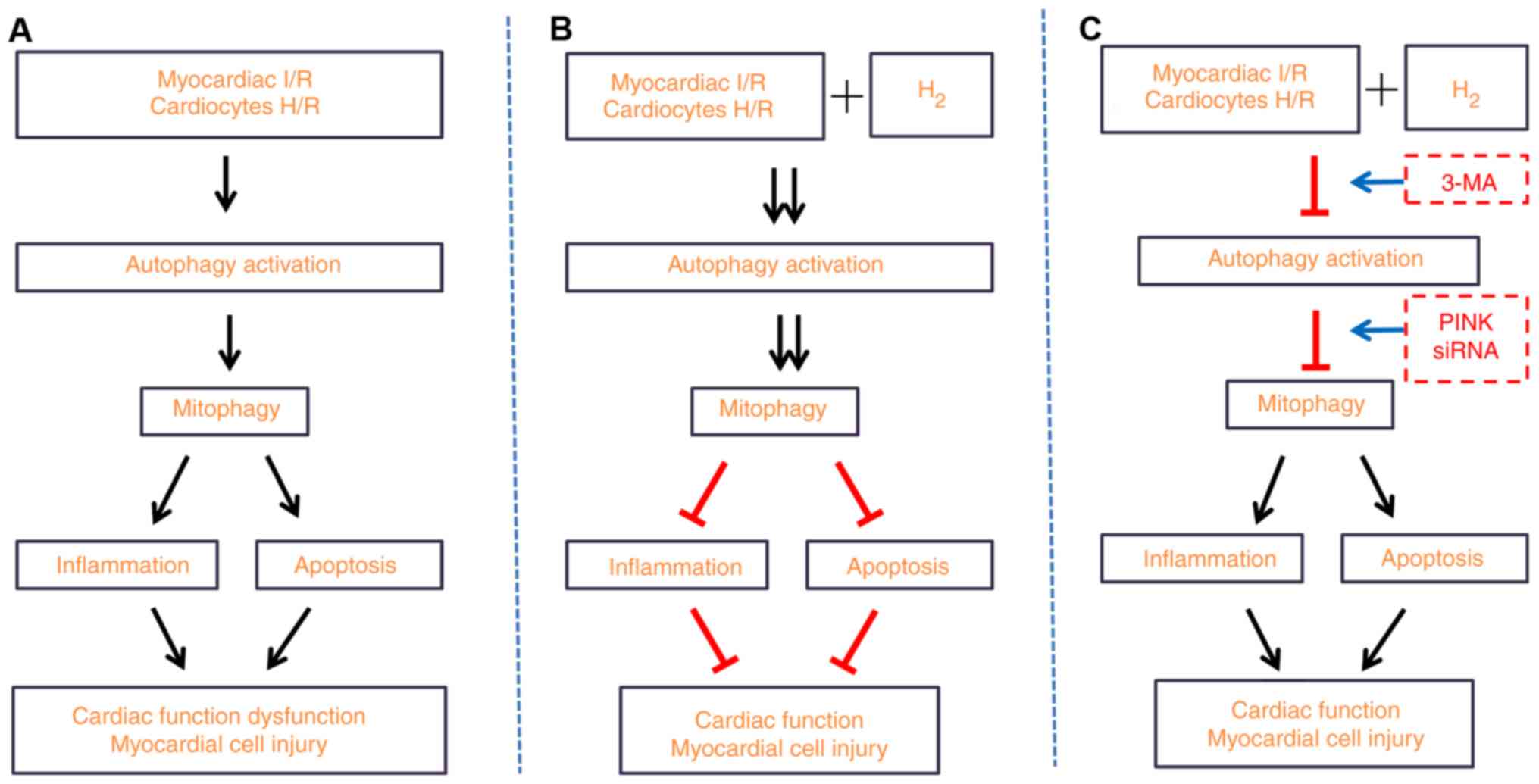
In summary, the results of the present study
demonstrated that hydrogen-rich saline alleviated the inflammatory
response and apoptosis induced by MI/R or H/R, and contributed to
the increased expression of proteins associated with autophagy.
These findings suggested that hydrogen-rich saline alleviated the
inflammatory response and apoptosis via PINK1/Parkin-mediated
mitophagy. The present study also elucidated the detailed mechanism
by which hydrogen protected myocardial injury from the inflammation
response and apoptosis (Fig.
11). Since the present study provides a novel hypothesis for
the mechanisms of hydrogen therapy, further studies will be needed
in the future to fully elucidate the underlying mechanisms of
hydrogen treatment in disease.
Supplementary Materials
Funding
This study was supported by the National Nature
Science Foundation of China (grant no. 81601667).
Availability of data and materials
The datasets used and analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LY, KX designed the research and revised the
manuscript. LY, HC and KX performed the experiments and drafted the
manuscript. QW performed data analysis. LY and HC revised the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All experimental protocols were approved by the
Institutional Animal Care and Use Committee of Tianjin Medical
University and were conducted in strict accordance with the
National Institutes of Health guidelines for the use of
experimental animals.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Acknowledgments
Not applicable.
References
|
1
|
Yellon DM and Hausenloy DJ: Myocardial
reperfusion injury. N Engl J Med. 357:1121–1135. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ding S, Yang Y and Mei J: Protective
effects of L-malate against myocardial ischemia/reperfusion injury
in rats. Evid Based Complement Alternat Med. 2016:38036572016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Heusch G, Musiolik J, Gedik N and
Skyschally A: Mitochondrial STAT3 activation and cardioprotection
by ischemic postconditioning in pigs with regional myocardial
ischemia/reperfusion. Circ Res. 109:1302–1308. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang Z, Wang Y, Ye J, Lu X, Cheng Y, Xiang
L, Chen L, Feng W, Shi H, Yu X, et al: BFGF attenuates endoplasmic
reticulum stress and mitochondrial injury on myocardial
ischaemia/reperfusion via activation of PI3K/Akt/ERK1/2 pathway. J
Cell Mol Med. 19:595–607. 2015. View Article : Google Scholar
|
|
5
|
Pan Z, Zhao Y, Yu H, Liu D and Xu H:
Effect of hydrogen-rich saline on cardiomyocyte autophagy during
myocardial ischemia-reperfusion in aged rats. Zhonghua Yi Xue Za
Zhi. 95:2022–2026. 2015.In Chinese. PubMed/NCBI
|
|
6
|
Zhang Y, Sun Q, He B, Xiao J, Wang Z and
Sun X: Anti-inflammatory effect of hydrogen-rich saline in a rat
model of regional myocardial ischemia and reperfusion. Int J
Cardiol. 148:91–95. 2011. View Article : Google Scholar
|
|
7
|
Shigeta T, Sakamoto S, Li XK, Cai S, Liu
C, Kurokawa R, Nakazawa A, Kasahara M and Uemoto S: Luminal
injection of hydrogen-rich solution attenuates intestinal
ischemia-reperfusion injury in rats. Transplantation. 99:500–507.
2015. View Article : Google Scholar
|
|
8
|
Li J, Hong Z, Liu H, Zhou J, Cui L, Yuan
S, Chu X and Yu P: Hydrogen-rich saline promotes the recovery of
renal function after ischemia/reperfusion injury in rats via
anti-apoptosis and anti-inflammation. Front Pharmacol. 7:1062016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shimada S, Wakayama K, Fukai M, Shimamura
T, Ishikawa T, Fukumori D, Shibata M, Yamashita K, Kimura T, Todo
S, et al: Hydrogen gas ameliorates hepatic reperfusion injury after
prolonged cold preservation in isolated perfused rat liver. Artif
Organs. 40:1128–1136. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang R, Wu J, Chen Z, Xia F, Sun Q and Liu
L: Postconditioning with inhaled hydrogen promotes survival of
retinal ganglion cells in a rat model of retinal
ischemia/reperfusion injury. Brain Res. 1632:82–90. 2016.
View Article : Google Scholar
|
|
11
|
Sun Q, Kang Z, Cai J, Liu W, Liu Y, Zhang
JH, Denoble PJ, Tao H and Sun X: Hydrogen-rich saline protects
myocardium against ischemia/reperfusion injury in rats. Exp Biol
Med (Maywood). 234:1212–1219. 2009. View Article : Google Scholar
|
|
12
|
Cabigas EB, Somasuntharam I, Brown ME, Che
PL, Pendergrass KD, Chiang B, Taylor WR and Davis ME:
Over-expression of catalase in myeloid cells confers acute
protection following myocardial infarction. Int J Mol Sci.
15:9036–9050. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen H, Xie K, Han H, Li Y, Liu L, Yang T
and Yu Y: Molecular hydrogen protects mice against polymicrobial
sepsis by ameliorating endothelial dysfunction via an Nrf2/HO-1
signaling pathway. Int Immunopharmacol. 28:643–654. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Qi L, Pan H, Li D, Fang F, Chen D and Sun
H: Luteolin improves contractile function and attenuates apoptosis
following ischemia-reperfusion in adult rat cardiomyocytes. Eur J
Pharmacol. 668:201–207. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xiong J, Xue FS, Yuan YJ, Wang Q, Liao X
and Wang WL: Cholinergic anti-inflammatory pathway: A possible
approach to protect against myocardial ischemia reperfusion injury.
Chin Med J (Engl). 123:2720–2726. 2010.
|
|
16
|
Speyer CL and Ward PA: Role of endothelial
chemokines and their receptors during inflammation. J Invest Surg.
24:18–27. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Naidu BV, Farivar AS, Woolley SM, Grainger
D, Verrier ED and Mulligan MS: Novel broad-spectrum chemokine
inhibitor protects against lung ischemia-reperfusion injury. J
Heart Lung Transplant. 23:128–134. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Konstantinidis K, Whelan RS and Kitsis RN:
Mechanisms of cell death in heart disease. Arterioscler Thromb Vasc
Biol. 32:1552–1562. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Movassagh M and Foo RS: Simplified
apoptotic cascades. Heart Fail Rev. 13:111–119. 2008. View Article : Google Scholar
|
|
20
|
Nakai A, Yamaguchi O, Takeda T, Higuchi Y,
Hikoso S, Taniike M, Omiya S, Mizote I, Matsumura Y, Asahi M, et
al: The role of autophagy in cardiomyocytes in the basal state and
in response to hemodynamic stress. Nat Med. 13:619–624. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang H, Liu B, Li T, Zhu Y, Luo G, Jiang
Y, Tang F, Jian Z and Xiao Y: AMPK activation serves a critical
role in mitochondria quality control via modulating mitophagy in
the heart under chronic hypoxia. Int J Mol Med. 41:69–76. 2018.
|
|
22
|
Bian X, Teng T, Zhao H, Qin J, Qiao Z, Sun
Y, Liun Z and Xu Z: Zinc prevents mitochondrial superoxide
generation by inducing mitophagy in the setting of
hypoxia/reoxygenation in cardiac cells. Free Radic Res. 52:80–91.
2018. View Article : Google Scholar
|
|
23
|
Eiyama A and Okamoto K:
PINK1/Parkin-mediated mitophagy in mammalian cells. Curr Opin Cell
Biol. 33:95–101. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kubli DA, Cortez MQ, Moyzis AG, Najor RH,
Lee Y and Gustafsson AB: PINK1 is dispensable for mitochondrial
recruitment of parkin and activation of mitophagy in cardiac
myocytes. PLoS One. 10:pp. e01307072015, View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dorn GN III: Parkin-dependent mitophagy in
the heart. J Mol Cell Cardiol. 95:42–49. 2016. View Article : Google Scholar :
|
|
26
|
Hoshino A, Mita Y, Okawa Y, Ariyoshi M,
Iwai-Kanai E, Ueyama T, Ikeda K, Ogata T and Matoba S: Cytosolic
p53 inhibits Parkin-mediated mitophagy and promotes mitochondrial
dysfunction in the mouse heart. Nat Commun. 4:23082013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kubli DA, Zhang X, Lee Y, Hanna RA,
Quinsay MN, Nguyen CK, Jimenez R, Petrosyan S, Murphy AN and
Gustafsson AB: Parkin protein deficiency exacerbates cardiac injury
and reduces survival following myocardial infarction. J Biol Chem.
288:915–926. 2013. View Article : Google Scholar :
|
|
28
|
Yang Y, Ma Z, Hu W, Wang D, Jiang S, Fan
C, Di S, Liu D, Sun Y and Yi W: Caveolin-1/-3: Therapeutic targets
for myocardial ischemia/reperfusion injury. Basic Res Cardiol.
111:452016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mao X, Wang T, Liu Y, Irwin MG, Ou JS,
Liao XL, Gao X, Xu Y, Ng KF, Vanhoutte PM and Xia Z:
N-acetylcysteine and allopurinol confer synergy in attenuating
myocardial ischemia injury via restoring HIF-1alpha/HO-1 signaling
in diabetic rats. PLoS One. 8. pp. e689492013, View Article : Google Scholar
|
|
30
|
Pan Z, Zhao Y, Yu H, Liu D and Xu H:
Effect of hydrogen-rich saline on cardiomyocyte autophagy during
myocardial ischemia-reperfusion in aged rats. Zhonghua Yi Xue Za
Zhi. 95:2022–2026. 2015.In Chinese. PubMed/NCBI
|
|
31
|
Rossello X, Lobo-Gonzalez M and Ibanez B:
Pathophysiology and therapy of myocardial ischaemia/reperfusion
syndrome. Eur Heart J Acute Cardiovasc Care. Jun 7–2019, Epub ahead
of print. View Article : Google Scholar
|
|
32
|
Hinojar R, Foote L, Ucar EA, Dabir D,
Schnackenburg B, Higgins DM, Schaeffter T, Nagel E and Puntmann V:
Myocardial T2 mapping for improved detection of inflammatory
myocardial involvement in acute and chronic myocarditis. J
Cardiovasc Magn Reson. 16(Suppl 1): pp. O632014, View Article : Google Scholar :
|
|
33
|
Xu P, Cai X, Zhang W, Li Y, Qiu P, Lu D
and He X: Flavonoids of Rosa roxburghii Tratt exhibit
radioprotection and anti-apoptosis properties via the
Bcl-2(Ca(2+))/caspase-3/PARP-1 pathway. Apoptosis. 21:1125–1143.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Narendra DP, Jin SM, Tanaka A, Suen DF,
Gautier CA, Shen J, Cookson MR and Youle RJ: PINK1 is selectively
stabilized on impaired mitochondria to activate Parkin. PLoS Biol.
8:pp. e10002982010, View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Moyzis AG, Sadoshima J and Gustafsson AB:
Mending a broken heart: The role of mitophagy in cardioprotection.
Am J Physiol Heart Circ Physiol. 308:H183–H192. 2015. View Article : Google Scholar :
|
|
36
|
Li T, Jiao YR, Wang LH, Zhou YH and Yao
HC: Autophagy in myocardial ischemia reperfusion injury: Friend or
foe? Int J Cardiol. 239:102017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Toldo S, Marchetti C, Mauro AG, Chojnacki
J, Mezzaroma E, Carbone S, Zhang S, Van Tassell B, Salloum FN and
Abbate A: Inhibition of the NLRP3 inflammasome limits the
inflammatory injury following myocardial ischemia-reperfusion in
the mouse. Int J Cardiol. 209:215–220. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yu H, Zhang H, Zhao W, Guo L, Li X, Li Y,
Zhang X and Sun Y: Gypenoside protects against myocardial
ischemia-reperfusion injury by inhibiting cardiomyocytes apoptosis
via inhibition of chop pathway and activation of PI3K/Akt pathway
in vivo and in vitro. Cell Physiol Biochem. 39:123–136. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ge M, Yao W, Yuan D, Zhou S, Chen X, Zhang
Y, Li H, Xia Z and Hei Z: Brg1-mediated Nrf2/HO-1 pathway
activation alleviates hepatic ischemia-reperfusion injury. Cell
Death Dis. 8:pp. e28412017, View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ma L, Liu H, Xie Z, Yang S, Xu W, Hou J
and Yu B: Ginsenoside Rb3 protects cardiomyocytes against
ischemia-reperfusion injury via the inhibition of JNK-mediated
NF-κB pathway: A mouse cardiomyocyte model. PLoS One. 9:pp.
e1036282014, View Article : Google Scholar
|
|
41
|
Yu J, Wang L, Akinyi M, Li Y, Duan Z, Zhu
Y and Fan G: Danshensu protects isolated heart against ischemia
reperfusion injury through activation of Akt/ERK1/2/Nrf2 signaling.
Int J Clin Exp Med. 8:14793–14804. 2015.PubMed/NCBI
|
|
42
|
Nandi S, Ravindran S and Kurian GA: Role
of endogenous hydrogen sulfide in cardiac mitochondrial
preservation during ischemia reperfusion injury. Biomed
Pharmacother. 97:271–279. 2018. View Article : Google Scholar
|
|
43
|
Chi J, Li Z, Hong X, Zhao T, Bie Y, Zhang
W, Yang J, Feng Z, Yu Z, Xu Q, et al: Inhalation of hydrogen
attenuates progression of chronic heart failure via suppression of
oxidative stress and P53 related to Apoptosis pathway in rats.
Front Physiol. 9:10262018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yue L, Li H, Zhao Y, Li J and Wang B:
Effects of hydrogen-rich saline on Akt/GSK3beta signaling pathways
and cardiac function during myocardial ischemia-reperfusion in
rats. Zhonghua Yi Xue Za Zhi. 95:1483–1487. 2015.In Chinese.
PubMed/NCBI
|
|
45
|
Pan Z, Zhao Y, Yu H, Liu D and Xu H:
Effect of hydrogen-rich saline on cardiomyocyte autophagy during
myocardial ischemia-reperfusion in aged rats. Zhonghua Yi Xue Za
Zhi. 95:2022–2026. 2015.In Chinese. PubMed/NCBI
|
|
46
|
Yue L, Li H, Zhao Y, Li J and Wang B:
Effects of hydrogen-rich saline on Akt/GSK3β signaling pathways and
cardiac function during myocardial ischemia-reperfusion in rats.
Zhonghua Yi Xue Za Zhi. 95:1483–1487. 2015.In Chinese. PubMed/NCBI
|
|
47
|
Guo J, Wang SB, Yuan TY, Wu YJ, Yan Y, Li
L, Xu XN, Gong LL, Qin HL, Fang LH and Du GH: Coptisine protects
rat heart against myocardial ischemia/reperfusion injury by
suppressing myocardial apoptosis and inflammation. Atherosclerosis.
231:384–391. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Fliss H and Gattinger D: Apoptosis in
ischemic and reperfused rat myocardium. Circ Res. 79:949–956. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Anselmi A, Abbate A, Girola F, Nasso G,
Biondi-Zoccai GG, Possati G and Gaudino M: Myocardial ischemia,
stunning, inflammation, and apoptosis during cardiac surgery: A
review of evidence. Eur J Cardiothorac Surg. 25:304–311. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Vukojevic K, Carev D, Sapunar D, Petrovic
D and Saraga-Babic M: Developmental patterns of caspase-3, bax and
bcl-2 proteins expression in the human spinal ganglia. J Mol
Histol. 39:339–349. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Dong JW, Zhu HF, Zhu WZ, Ding HL, Ma TM
and Zhou ZN: Intermittent hypoxia attenuates ischemia/reperfusion
induced apoptosis in cardiac myocytes via regulating Bcl-2/Bax
expression. Cell Res. 13:385–391. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Li R, Geng HH, Xiao J, Qin XT, Wang F,
Xing JH, Xia YF, Mao Y, Liang JW and Ji XP: MiR-7a/b attenuates
post-myocardial infarction remodeling and protects H9c2
cardiomyoblast against hypoxia-induced apoptosis involving Sp1 and
PARP-1. Sci Rep. 6:290822016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Jiang YQ, Chang GL, Wang Y, Zhang DY, Cao
L and Liu J: Geniposide prevents hypoxia/reoxygenation-induced
apoptosis in H9c2 cells: Improvement of mitochondrial dysfunction
and activation of GLP-1R and the PI3K/AKT signaling pathway. Cell
Physiol Biochem. 39:407–421. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Bao W, Hu E, Tao L, Boyce R, Mirabile R,
Thudium DT, Ma XL, Willette RN and Yue TL: Inhibition of Rho-kinase
protects the heart against ischemia/reperfusion injury. Cardiovasc
Res. 61:548–558. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sun D, Huang J, Zhang Z, Gao H, Li J, Shen
M, Cao F and Wang H: Luteolin limits infarct size and improves
cardiac function after myocardium ischemia/reperfusion injury in
diabetic rats. PLoS One. 7:pp. e334912012, View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Ahn J and Kim J: Mechanisms and
consequences of inflammatory signaling in the myocardium. Curr
Hypertens Rep. 14:510–516. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Woldbaek PR, Tønnessen T, Henriksen UL,
Florholmen G, Lunde PK, Lyberg T and Christensen G: Increased
cardiac IL-18 mRNA, pro-IL-18 and plasma IL-18 after myocardial
infarction in the mouse; a potential role in cardiac dysfunction.
Cardiovasc Res. 59:122–131. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang JJ, Peng K, Zhang J, Meng XW and Ji
FH: Dexmedetomidine preconditioning may attenuate myocardial
ischemia/reperfusion injury by down-regulating the HMGB1
TLR4-MyD88-NF-κB signaling pathway. PLoS One. 12:pp. e01720062017,
View Article : Google Scholar
|
|
59
|
Cao QH, Liu F, Yang ZL, Fu XH, Yang ZH,
Liu Q, Wang L, Wan XB and Fan XJ: Prognostic value of autophagy
related proteins ULK1, Beclin 1, ATG3, ATG5, ATG7, ATG9, ATG10,
ATG12, LC3B and p62/SQSTM1 in gastric cancer. Am J Transl Res.
8:3831–3847. 2016.PubMed/NCBI
|
|
60
|
de Vries RL and Przedborski S: Mitophagy
and Parkinson's disease: Be eaten to stay healthy. Mol Cell
Neurosci. 55:37–43. 2013. View Article : Google Scholar
|
|
61
|
Narendra D, Tanaka A, Suen DF and Youle
RJ: Parkin is recruited selectively to impaired mitochondria and
promotes their autophagy. J Cell Biol. 183:795–803. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lee Y, Lee HY, Hanna RA and Gustafsson AB:
Mitochondrial autophagy by Bnip3 involves Drp1-mediated
mitochondrial fission and recruitment of Parkin in cardiac
myocytes. Am J Physiol Heart Circ Physiol. 301:H1924–H931. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Billia F, Hauck L, Konecny F, Rao V, Shen
J and Mak TW: PTEN-inducible kinase 1 (PINK1)/Park6 is
indispensable for normal heart function. Proc Natl Acad Sci USA.
108:9572–9577. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zhao Y, Tang Y, Suo C, Liu D, Li S and Li
H: Effects of hydrogen-rich saline on endoplasmic reticulum stress
during myocardial ischemia-reperfusion in rats. Zhonghua Yi Xue Za
Zhi. 94:3024–3028. 2014.In Chinese. PubMed/NCBI
|