Introduction
Early gastric cancer (EGC) is defined as the
presence of a lesion confined to the mucosa or submucosa,
regardless of the presence of regional lymph node metastasis, and
has a good prognosis with appropriate treatment (1). Although the outcome of patients with
EGC following curative surgery is excellent, cancer recurrence is a
rare event and could occur even after curative gastrectomy with an
incidence of 1.4–2.7% (2–5).
Endoscopic resection with endoscopic mucosal
resection (EMR) or endoscopic submucosal dissection (ESD) is widely
accepted as the standard treatment for EGC without lymph node
metastasis and enables a clinician to resect a target lesion en
bloc (6,7). Most EGC confined to the mucosa can be
curatively treated by endoscopic resection, since lymph node
metastasis is rare in such cases. Endoscopic resection is currently
considered appropriate for the treatment of intestinal-type gastric
cancer cases without central ulceration that are <2 cm in
diameter, according to guidelines for EMR/ESD established by the
Japanese Gastric Cancer Association (7). However, gastrectomy with lymph node
dissection should be performed in patients with submucosal invasion
with or without margin involvement following endoscopic resection
(8,9).
In this study, a case of metachronous liver and bone
metastasis after laparoscopy-assisted distal gastrectomy is
described, following initial treatment by ESD for small EGC without
lymph node metastasis, showing human epidermal growth factor
receptor 2 (HER2) overexpression. All diagnostic procedures and
therapy concerning the patient were performed after obtaining
written informed consent.
Case report
A 65-year-old man was referred to our hospital for
examination of gastric cancer initially diagnosed by medical
check-up. The patient’s medical and family history were
unremarkable. The laboratory findings were almost within normal
range, as were levels of serum carcinoembryonic antigen and cancer
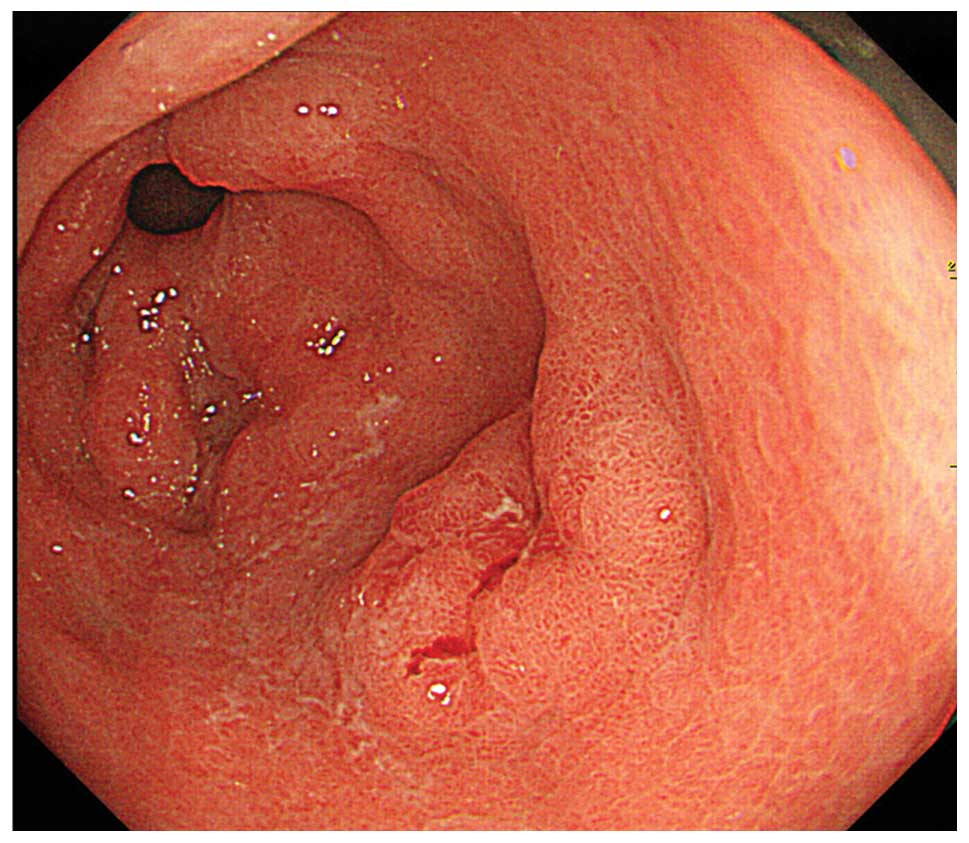
antigen 19-9. Esophagogastroduodenoscopy (EGD) demonstrated a
superficial depressed-type gastric cancer in the antrum that proved
to be a well-differentiated adenocarcinoma on biopsy (Fig. 1). Abdominal computed tomography
(CT) demonstrated no evidence of distant metastases and endoscopic
ultrasound (EUS) identified tumor invasion of the antral
mucosa.
Following a clinical diagnosis of EGC confined to
mucosa, ESD was performed. The macroscopic findings of the resected
specimen showed that the tumor was an irregularly shaped depressed
lesion, 11 mm in diameter (Fig.
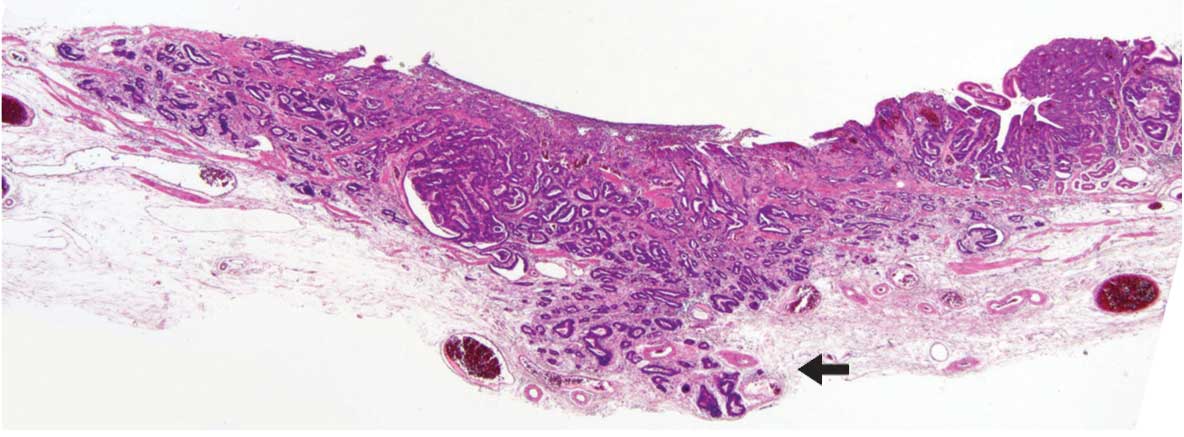
2). Histological analyses revealed that the tumor was a
well-differentiated adenocarcinoma that had invaded the submucosal
layer to a depth of >500 μm at the center of the lesion
with positive lymphatic and negative venous invasion (Fig. 3). Therefore, according to the
extended criteria for endoscopic resection, the patient underwent
laparoscopy-assisted distal gastrectomy with regional lymph node
dissection, resulting in no residual carcinoma and no lymph node
metastasis. The post-operative course was uneventful, and the
patient was discharged on post-operative day 14.
The patient underwent periodic follow-up physical
examinations, and 1 year after the operation, abdominal CT showed a
ring-enhanced, well-defined mass measuring 4.8 cm in diameter
located in the liver (Fig. 4).
Since there was no evidence of further metastatic lesions in other
organs, the patient underwent surgical resection of the liver
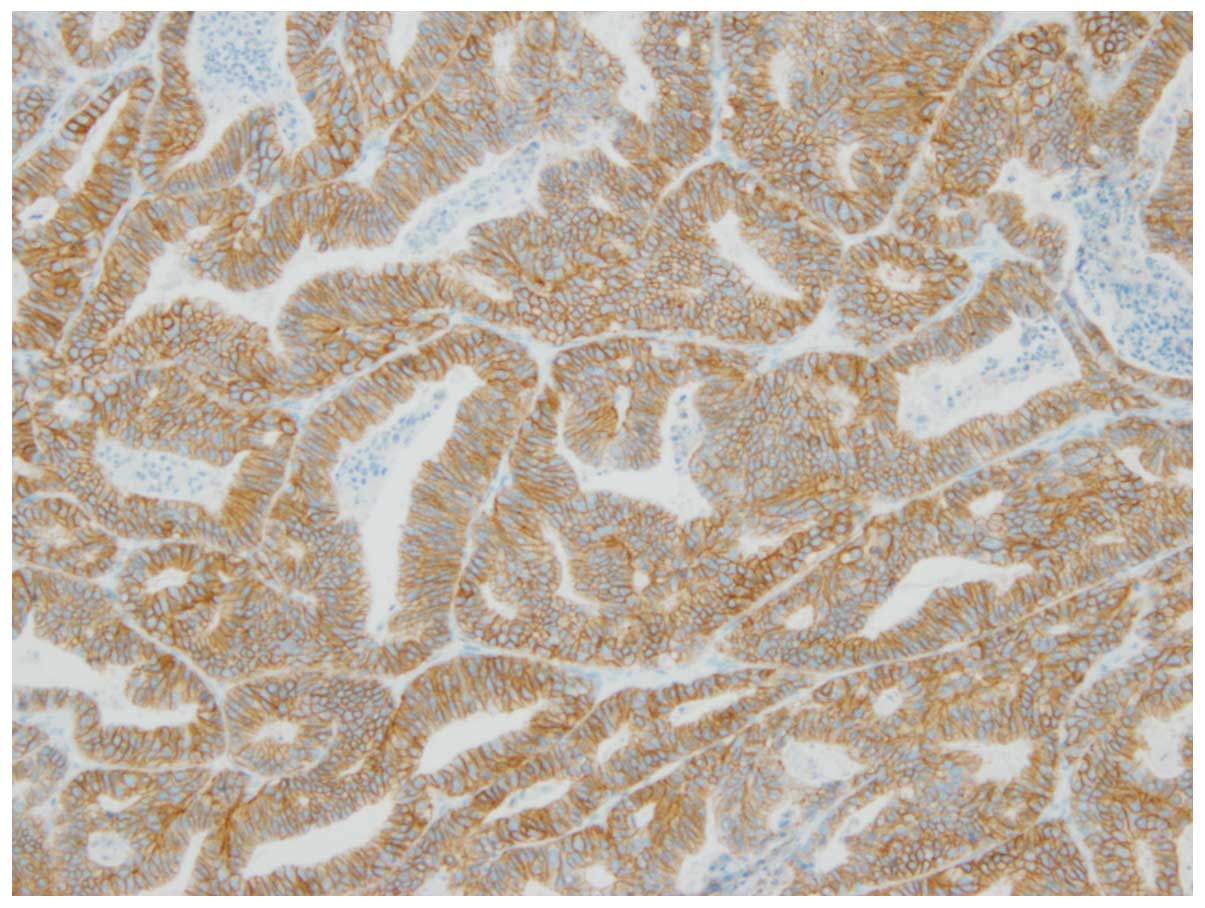
tumor. Histological examination confirmed the diagnosis of a
well-differentiated adenocarcinoma originating from the previous
gastric cancer and immunohistochemical analysis of the tumor showed
strong reactivity for HER2 (Fig.
5). Therefore, the patient was administered trastuzumab in
combination with chemotherapy consisting of capecitabine plus
cisplatin.
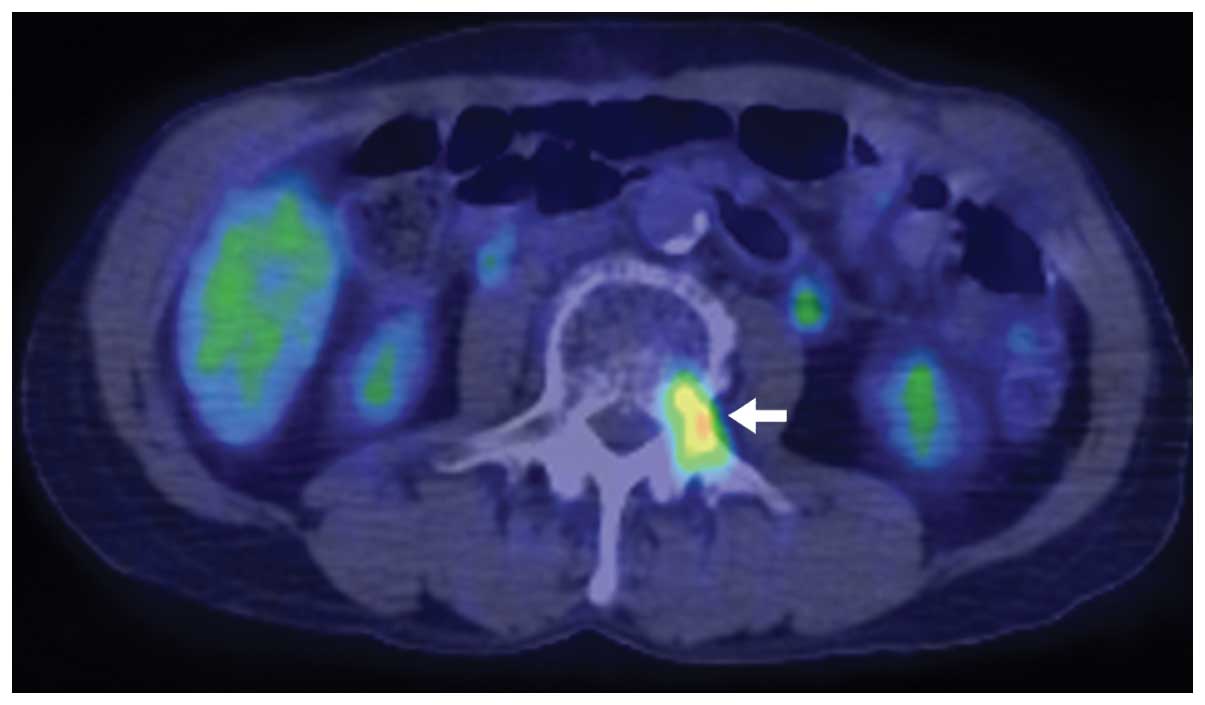
However, eight months after the second operation,
the patient developed metastasis of the third lumbar vertebrae,
which was detected using 18F-2-deoxy-2-fluoro-D-glucose
positron emission tomography combined with CT imaging (FDG-PET/CT)
(Fig. 6). Therefore, the patient
was treated with trastuzumab plus irinotecan/docetaxel and was
alive 12 months after the second operation.
Discussion
Solitary liver metastasis from EGC after curative
gastrectomy is rare, with a reported incidence of 0.4–0.7%. A
significant correlation between liver metastasis from gastric
cancer that has invaded the submucosal layer and venous invasion
has been reported (2,3,11).
This clinical case emphasizes the risk of metachronous distant
metastasis even after curative treatment for small EGC infiltrating
the submucosa.
In the patient reported in this study, microscopic
examination of a resected specimen by gastrectomy showed no
residual cancer. Since endoscopic resection is generally performed
using a coagulating device, the presence of cancer cells at the
margins of the coagulated tissue, within the resected specimen and
residual organ site, is unlikely. Therefore, in the present case,
it is unlikely that cancer cells were present in the resected
stomach following ESD. It has been reported that the rate of the
residual tumor was 11.1% among cases where there was incomplete
resection due to a positive vertical margin with submucosal
invasion (10).
In general, lymph node metastasis is reported to be
the most significant risk factor for the recurrence of EGC
(2,3,11).
Regarding the risk factors for liver metastasis, it has been
reported that vascular involvement in the submucosal layer is
significantly more important compared with nodal and lymphatic
involvement (11,12). Furthermore, lymphatico-portal
venous anastomosis due to mesenteric lymphatic occlusion is
reportedly an important factor in the occurrence of liver
metastasis of gastric cancer (13). Additional factors associated with
cancer recurrence include lymphatic invasion, submucosal invasion,
large tumor size, and a superficial spreading type (2,5,11).
In contrast to these risk factors, the present EGC case was a small
tumor of 11 mm in diameter without lymph node metastasis or venous
invasion, although lymphatic invasion was positive. Despite the
fact that these characteristics likely indicate a good prognosis,
the overexpression of HER2 observed in this case may have increased
the risk of metastasis, thus contributing to a poor prognosis.
Although HER2 overexpression has been reported to
correlate with aggressive biological behavior and poor prognosis,
there have been no universal conclusions regarding its significance
as a prognostic factor (14–16).
While certain studies have reported that HER2 overexpression is
associated with a poor prognosis in gastric cancer, the impact of
HER2 expression on patient survival is limited, particularly in
earlier stages of the disease (17,18).
The present case emphasizes the need for including HER2 status as a
risk factor for tumor recurrence even in EGC cases.
The recent development of chemotherapy and
administration of novel molecular-targeted drugs for advanced-stage
gastric cancer has provided clinical benefits and improved the
survival rate of patients (19–21).
Trastuzumab is the current standard of care for the treatment of
HER2-positive early and advanced breast cancer (22). In a recent international phase III
randomized controlled trial, the addition of trastuzumab to
chemotherapy significantly improved overall survival compared with
chemotherapy alone in patients with advanced gastric cancer
(21). Therefore, trastuzumab in
combination with chemotherapy could be considered as a novel
standard option for patients with HER2-positive advanced or
recurrent gastric cancer.
Liver resection for hepatic metastases from gastric
carcinoma is, however, not a common procedure due to poor
prognosis. Therefore, there is still no widespread agreement
regarding surgical resection of synchronous or metachronous liver
metastases from gastric cancer (23,24).
In the present case, as the first recurrence was limited to the
liver, surgical resection was the chosen treatment, followed by a
chemotherapy regimen consisting of trastuzumab in combination with
capecitabine plus cisplatin. However, in the present case, bone
metastasis appeared despite complete removal and disappearance of
the liver metastasis. Additional case reports are therefore needed
in order for the poor prognosis of EGC recurrence to be
improved.
Despite the generally excellent outcome of EGC
patients following curative surgery, a strong malignancy potential
remains, which is associated with an extremely poor prognosis even
in cases of small-sized tumors. Therefore, clinicians should take
this possibility into consideration in follow-up management after
curative treatment to treat recurrent disease earlier.
Determination of the HER2 expression status in addition to
conventional pathological diagnoses, such as lymph node metastasis
as well as lymphatic and venous involvement may be helpful in
predicting the risk of EGC recurrence.
References
|
1
|
Japanese Gastric Cancer Association:
Japanese Classification of Gastric Carcinoma - 2nd English edition.
Gastric Cancer. 1:10–24. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Youn HG, An JY, Choi MG, Noh JH, Sohn TS
and Kim S: Recurrence after curative resection of early gastric
cancer. Ann Surg Oncol. 17:448–454. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saka M, Katai H, Fukagawa T, Nijjar R and
Sano T: Recurrence in early gastric cancer with lymph node
metastasis. Gastric Cancer. 11:214–218. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sano T, Sasako M, Kinoshita T and Maruyama
K: Recurrence of early gastric cancer. Follow-up of 1475 patients
and review of the Japanese literature. Cancer. 72:3174–3178. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Namikawa T, Kitagawa H, Iwabu J, et al:
Clinicopathological properties of the superficial spreading type
early gastric cancer. J Gastrointest Surg. 14:52–57. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ono H, Kondo H, Gotoda T, et al:
Endoscopic mucosal resection for treatment of early gastric cancer.
Gut. 48:225–229. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gotoda T: Endoscopic resection of early
gastric cancer. Gastric Cancer. 10:1–11. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Song KY, Hyung WJ, Kim HH, et al: Is
gastrectomy mandatory for all residual or recurrent gastric cancer
following endoscopic resection? A large-scale Korean multi-center
study. J Surg Oncol. 98:6–10. 2008. View Article : Google Scholar
|
|
9
|
Nagano H, Ohyama S, Fukunaga T, et al:
Indications for gastrectomy after incomplete EMR for early gastric
cancer. Gastric Cancer. 8:149–154. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee HJ, Jang YJ, Kim JH, et al: Clinical
outcomes of gastrectomy after incomplete EMR/ESD. J Gastric Cancer.
11:162–166. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ishida M, Morita S, Saka M, Fukagawa T,
Taniguchi H and Katai H: Metachronous liver metastasis from early
gastric cancer. J Gastrointest Surg. 16:837–841. 2012. View Article : Google Scholar
|
|
12
|
Hyung WJ, Lee JH, Choi SH, Min JS and Noh
SH: Prognostic impact of lymphatic and/or blood vessel invasion in
patients with node-negative advanced gastric cancer. Ann Surg
Oncol. 9:562–567. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamagata K and Kumagai K: Experimental
study of lymphogenous peritoneal cancer dissemination: migration of
fluorescent-labelled tumor cells in a rat model of mesenteric lymph
vessel obstruction. J Exp Clin Cancer Res. 19:211–217. 2000.
|
|
14
|
Hofmann M, Stoss O, Shi D, et al:
Assessment of a HER2 scoring system for gastric cancer: results
from a validation study. Histopathology. 52:797–805. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grabsch H, Sivakumar S, Gray S, Gabbert HE
and Müller W: HER2 expression in gastric cancer: rare,
heterogeneous and of no prognostic value - conclusions from 924
cases of two independent series. Cell Oncol. 32:57–65.
2010.PubMed/NCBI
|
|
16
|
Barros-Silva JD, Leitão D, Afonso L, et
al: Association of ERBB2 gene status with histopathological
parameters and disease-specific survival in gastric carcinoma
patients. Br J Cancer. 100:487–493. 2009. View Article : Google Scholar
|
|
17
|
Park DI, Yun JW, Park JH, et al: HER-2/neu
amplification is an independent prognostic factor in gastric
cancer. Dig Dis Sci. 51:1371–1379. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim KC, Koh YW, Chang HM, et al:
Evaluation of HER2 protein expression in gastric carcinomas:
comparative analysis of 1,414 cases of whole-tissue sections and
595 cases of tissue microarrays. Ann Surg Oncol. 18:2833–2840.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Boku N, Yamamoto S, Fukuda H, et al:
Fluorouracil versus combination of irinotecan plus cisplatin versus
S-1 in metastatic gastric cancer: a randomised phase 3 study.
Lancet Oncol. 10:1063–1069. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Koizumi W, Narahara H, Hara T, et al: S-1
plus cisplatin versus S-1 alone for first-line treatment of
advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet
Oncol. 9:215–221. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bang YJ, Van Cutsem E, Feyereislova A, et
al: Trastuzumab in combination with chemotherapy versus
chemotherapy alone for treatment of HER2-positive advanced gastric
or gastrooesophageal junction cancer (ToGA): a phase 3, open-label,
randomised controlled trial. Lancet. 376:687–697. 2010. View Article : Google Scholar
|
|
22
|
Boekhout AH, Beijnen JH and Schellens JH:
Trastuzumab. Oncologist. 16:800–810. 2011. View Article : Google Scholar
|
|
23
|
Sakamoto Y, Sano T, Shimada K, et al:
Favorable indications for hepatectomy in patients with liver
metastasis from gastric cancer. J Surg Oncol. 95:534–539. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Munekage M, Okabayashi T, Hokimoto N, et
al: A case with synchronous multiple liver metastases from gastric
carcinoma: postoperative long-term disease-free survival.
Langenbecks Arch Surg. 394:749–753. 2009. View Article : Google Scholar : PubMed/NCBI
|