Introduction
Angiosarcoma is a rare aggressive malignant tumor of
vascular endothelial origin (1) that
mainly causes cutaneous lesions. Angiosarcoma originating in the
omentum is extremely rare, with only few previous reported cases
(2–5). Here, we report a case of angiosarcoma
of the greater omentum arising in a prior radiation field 7 years
after concurrent chemoradiotherapy for cervical cancer.
Case report
A 38-year-old female visited our outpatient clinic
complaining of abdominal pain and distension. She had a history of
concurrent chemoradiotherapy for squamous cell carcinoma of the
cervix 7 years ago, which had led to complete clinical remission.
The prior treatment included whole pelvic irradiation (50.4
Gy/28Fr), intracavitary brachytherapy (18 Gy/3Fr), and three
courses of systemic cisplatin administration. She had no other
relevant medical history and familial history.
On presentation, the patient was generally ill and
had a markedly distended abdomen. The pelvic examination was normal
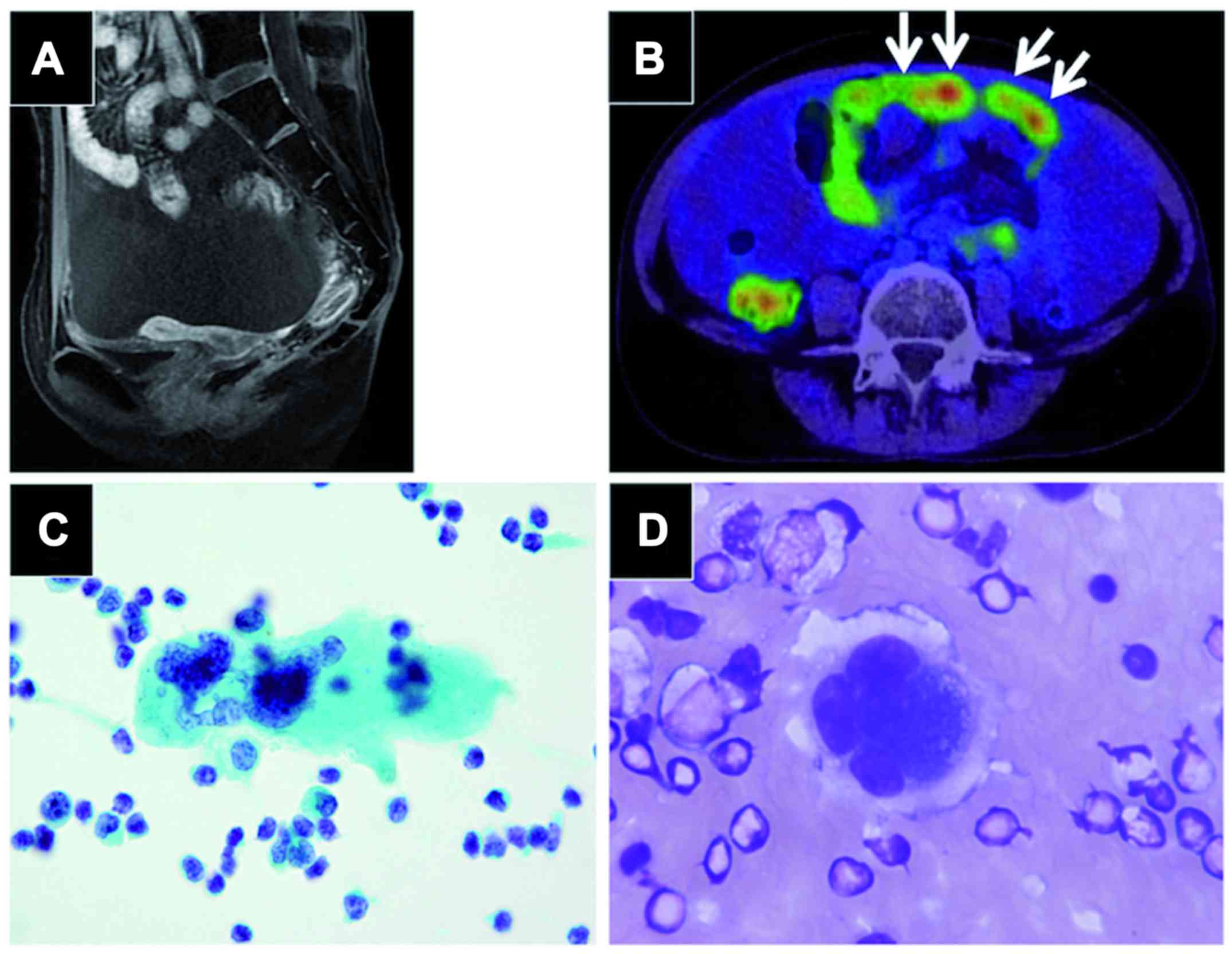
and pelvic MRI scan showed an atrophic but otherwise normal uterus
and bilateral adnexa (Fig. 1A).
Positron emission tomography CT scans revealed an omental mass with
prominent FDG uptake, massive bloody ascites, and signs suspicious
of peritonitis carcinomatosis (Fig.
1B). Gastroscopy and colonoscopy findings were unremarkable.
Cervical and endometrial cytology were negative for malignancy.
Ascites cytology obtained by paracentesis revealed solitary,
scattered multinucleated giant cells with prominent nucleoli
(Fig. 1C,d); however, the findings
did not prove malignancy due to the small number of suspicious
cells. CA125 was elevated (237 mIU/ml), while other tumor markers
(SCC, CEA and CA19-9) were negative.
Intra-abdominal cancer of unknown primary origin was
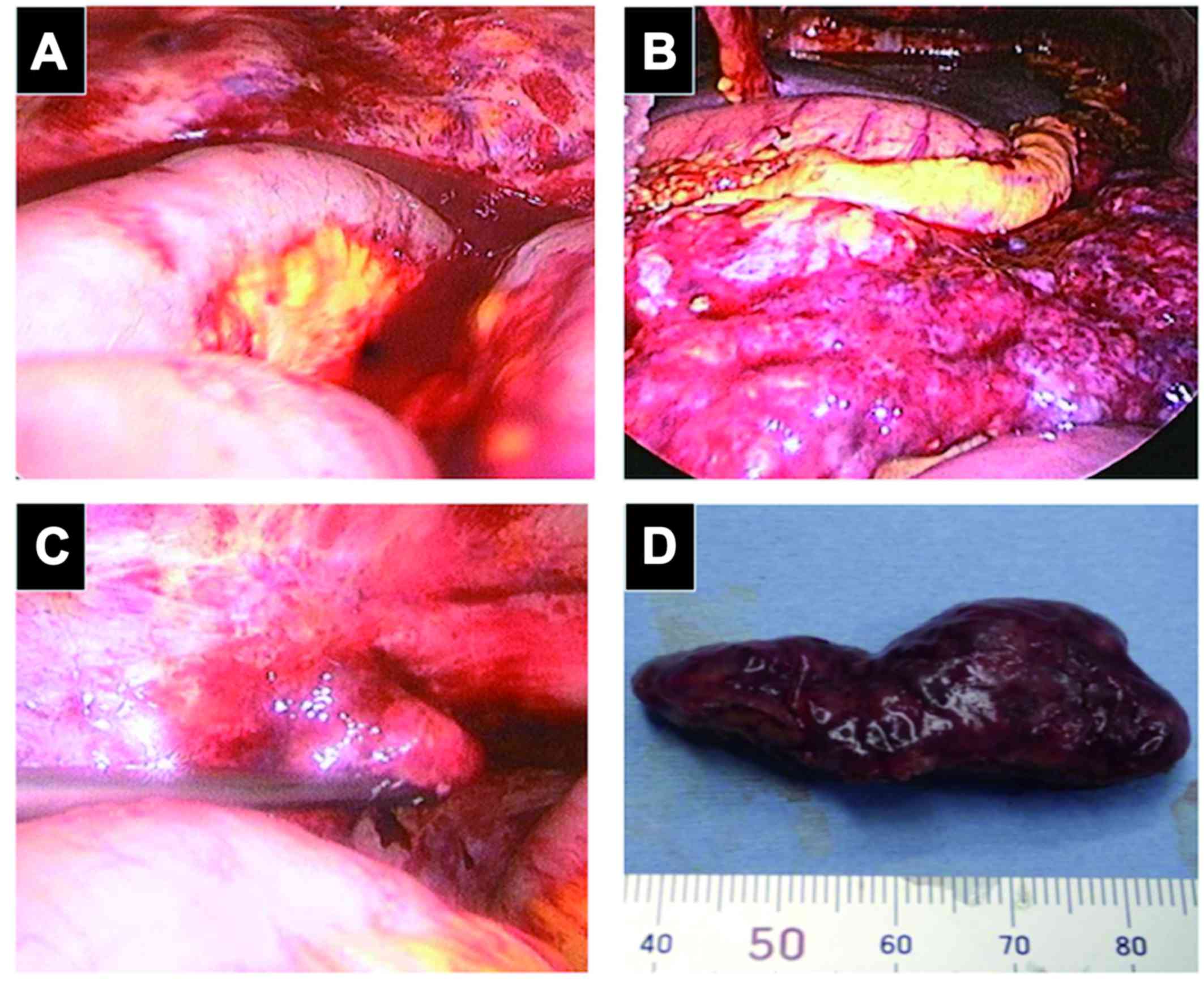
suspected and diagnostic laparoscopy was performed. Laparoscopic
examination revealed intensive peritoneal inflammation, massive
bloody ascites (Fig. 2A) and a
congested greater omental mass of 15 cm in diameter (Fig. 2B). This mass reached the splenic
flexure and had invaded close to the splenic hilum. There was a
small papillary lesion on the surface of the left ovary, which was
suspicious for dissemination (Fig.
2C). The right adnexa (Fig. 2D)
and the uterus were atrophic and adhered to the peritoneal wall
with no apparent lesion. Biopsy of the omental mass, bilateral
partial oophorectomy and right salpingectomy were performed. A
frozen section of the omental mass was diagnosed as poorly
differentiated malignant tumor. The operation time was 65 min and
blood loss was 1,150 ml.
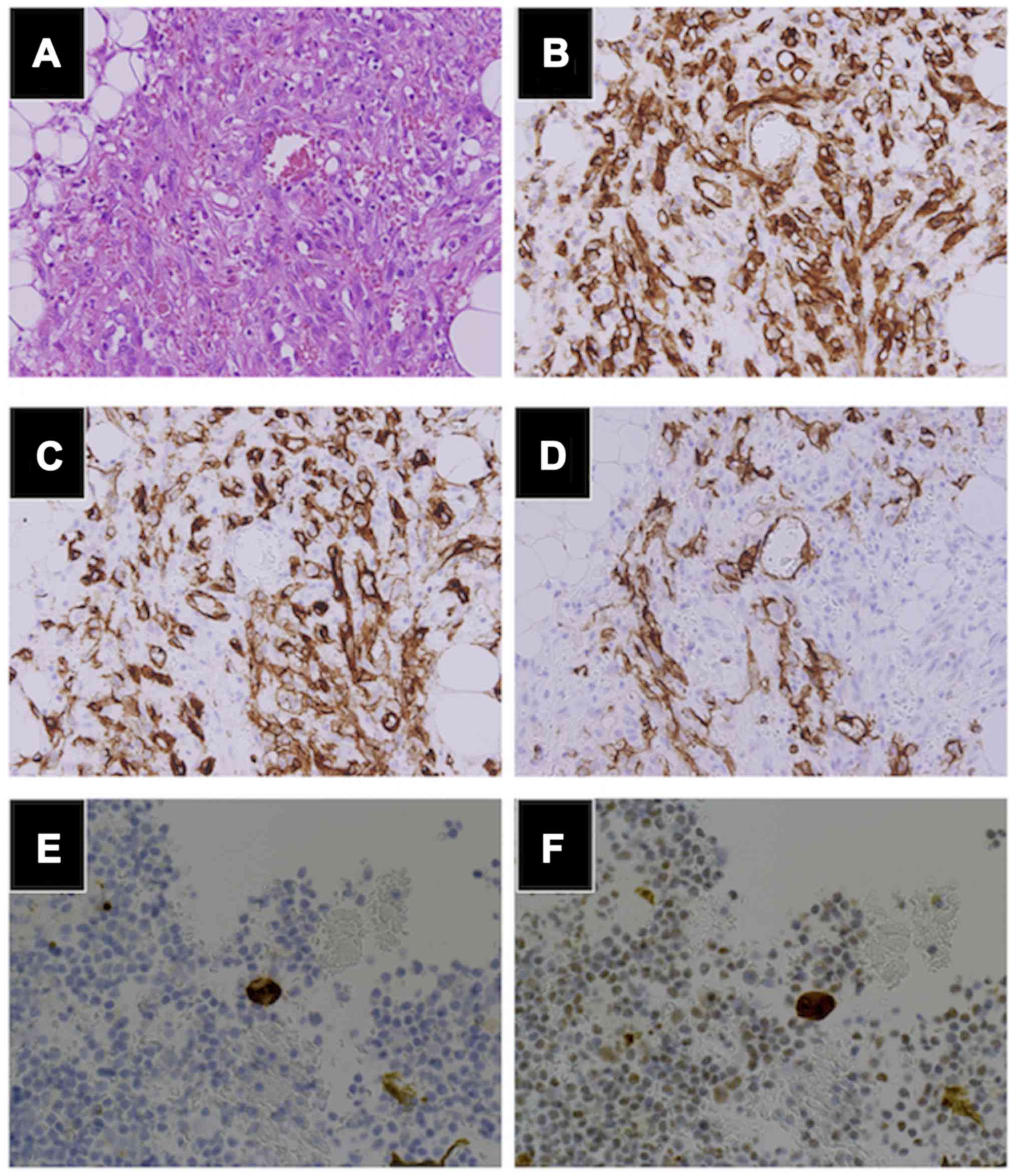
Microscopically, the tumors were composed of
high-grade malignant cells with frequent mitosis, forming irregular
anastomosing vascular channels containing erythrocytes (Fig. 3A). The same findings were present in
the left Fallopian tube, indicating dissemination.
Immunohistochemistry revealed positive staining for endothelial
markers CD31 (Fig. 3B), CD34
(Fig. 3C) and ERG. The lymphatic
endothelial marker D2-40 (Fig. 3D)
was positive, whereas cytokeratin (AE1/AE3), estrogen receptor,
progesterone receptor and WT-1 were negative. The cell block
technique for ascites revealed a few cells positive for CD34
(Fig. 3E) and ERG (Fig. 3F).
The diagnostic criteria for radiation-induced
sarcoma include pathologically proven sarcoma developing in a prior
radiation field, normal findings prior to radiotherapy, and at
least a three-year period after radiotherapy (6). Fulfilling the above criteria, the
clinical and pathological findings led to the diagnosis of
radiation-induced angiosarcoma of the greater omentum. The advanced
tumor was unresectable; therefore, weekly paclitaxel (100
mg/m2 on days 1, 8, 15, 22, 29, 36 in a 7-week cycle, as
approved in Japan) was started 11 days after surgery, which lead to
complete response after six courses, and complete cytoreductive
surgery was performed consequently. Currently, the patient remains
disease free 3 months post surgery.
Discussion
Angiosarcoma is a rare, aggressive malignant tumor
of vascular endothelial origin (1)
that comprises approximately 2% of soft-tissue sarcomas. The most
common site is the head and neck in elderly patients, whereas cases
of intraperitoneal origin are extremely rare. The prognosis of
angiosarcoma is generally poor, 19-43.9% of cases present with
advanced disease (7,8) and the median survival period is 7–12
months (7,8).
Secondary soft tissue sarcoma is an uncommon but
important adverse event following radiation therapy. As the
importance of radiation therapy in cancer treatment has grown over
the years, the number of recognized radiation-induced sarcomas is
also growing. In a study of 4,884 adult patients with soft tissue
sarcoma, 2.5% were diagnosed as radiation-induced, of which 15%
were patents with angiosarcoma (9).
Radiation-induced angiosarcoma accounts for 3–12.2% of all
angiosarcomas (7), and among
patients who received radiotherapy for primary cancer, the
standardized incidence ratio of angiosarcoma was 6.0 (95% CI
2.7–11), compared to patients who received other treatment
(10). Compared to other subtypes,
radiation-induced angiosarcoma has a particularly poor prognosis;
even local lesions recur in 87.5% of cases, and the median survival
period is 7–8 months (7).
The patient described herein developed angiosarcoma
in a prior radiation field 7 years after cervical cancer treatment,
and in this respect this is a typical case of radiation-induced
angiosarcoma. However, most radiation-induced angiosarcomas occur
in the skin of patients after radiation treatment for breast cancer
(7). Only four previous cases of
angiosarcoma originating in the greater omentum have been reported,
all of which were consequences of radiation therapy for gynecologic
cancer (2–5) (Table I).
All cases presented with advanced disease, which were complicated
with massive hemorrhagic ascites and peritoneal dissemination.
While the cases receiving palliative care described the rapidly
progressing character of the disease (3,5),
Chudecha-Glaz et al reported the achievement of partial
response by platinum-based chemotherapy, which lead to
cytoreductive surgery and control of the disease at least
temporarily (4). Swiftly making the
diagnosis and enabling chemotherapy administration seems to be the
key in controling the disease.
 | Table I.Radiation-induced angiosarcoma arising
in the omentum. |
Table I.
Radiation-induced angiosarcoma arising
in the omentum.
| Authors (year) | Age | Sex | Previous
malignancy | Radiation to
onset | Intra-peritoneal
hemorrhage | Treatment | Prognosis | (Refs.) |
|---|
| Westenberg et
al (1989) | 59 | F | Cervical cancer | 8 years | + | Unknown | Unknown | (7) |
| Sakemi et al
(2011) | 74 | F | Cervical cancer | 5 years | + | Palliative | 34 days died | (8) |
| Chudecka-Glaz et
al (2014) | 55 | F | Ovarian cancer | 20 years | + | Chemotherapy,
Surgery | 16 months died | (9) |
| Narayanan et
al (2015) | 77 | F | Cervical cancer | Unknown | + | Surgery, palliative
care | Unknown | (10) |
| Present case | 38 | F | Cervical cancer | 7 years | + | Chemotherapy,
surgery | Currently disease
Free (8 months) |
|
Due to the low prevalence and lack of specific
markers, prompt diagnosis of intraperitoneal angiosarcoma is a
challenge. Our current experience suggests the clinical usefulness
of diagnostic laparoscopy. The importance of diagnostic laparoscopy
is emerging for intraperitoneal cancer of unknown primary origin,
where minimal invasiveness is required for high-risk patients. This
method permits precise evaluation of the cancer origin,
determination of the feasibility of complete cytoreduction, and
conversion to laparotomy as needed. Further, for an unresectable
tumor, diagnostic laparoscopy allows sufficient biopsy for
pathological examination with permissive complications (11). With use of diagnostic laparoscopy, we
were able to initiate systemic treatment only 11 days
postoperatively in the current case.
For advanced stage angiosarcoma, systemic cytotoxic
chemotherapy is the treatment of choice. Due to the lack of
clinical trials for angiosarcoma patients, anthracycline- and
ifosfamide-based regimens have been considered as first line
chemotherapy following the results of clinical trials for other
soft tissue sarcomas (12,13). However, recently, few studies have
shown the efficacy of taxane-based therapy for angiosarcoma. In a
retrospective study in 32 patients with angiosarcoma who received
triweekly or weekly paclitaxel, the EORTC soft tissue and bone
group found a response rate of 62% and a median time to progression
of 7.6 months (12). In the ANGIOTAX
phase II trial (14), weekly
paclitaxel (80 mg/m2 on days 1, 8, and 15 of a 4-week
cycle) was administered to 30 patients with unresectable
angiosarcoma. The response rate was 19% after 6 courses, but the
regimen achieved a relatively high non-progression rate (75% at 3
months and 24% at 6 months), and the median progression free
survival (PFS) and overall survival (OS) were 4 and 8 months,
respectively. Taking these studies into account, the NCCN
guidelines currently recommend weekly paclitaxel as first line
chemotherapy for angiosarcoma; however, further clinical trials are
needed to optimize standard therapy.
Herein, we have reported a case of radiation-induced
angiosarcoma originating in the greater omentum in a 38-year-old
female. Radiation-induced angiosarcoma following treatment of
gynecologic cancer is clearly a rare complication, but should be
considered, especially with the increasing importance of radiation
therapy for treatment of invasive cervical cancer.
Acknowledgements
Written informed consent was obtained from the
patient for the publication of this case report, and ethics
approval was given from the ethical committee of our institute
(approval nο. 20070081). We thank the patient for allowing
discussion of her case with the academic community.
References
|
1
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Westenberg AH, Wiggers T, Henzen-Logmans
SC, Verweij J, Meerwaldt JA and van Geel AN: Post-irradiation
angiosarcoma of the greater omentum. Eur J Surg Oncol. 15:175–178.
1989.PubMed/NCBI
|
|
3
|
Sakemi M, Sakemi R, Harada M, So S,
Uchiyama D, Morimitsu Y, Kakiuchi S, Ishihara Y, Kubo Y, Matsugaki
S, et al: A case of postirradiation angiosarcoma of the greater
omentum with hemorrhage. Clin J Gastroenterol. 4:302–306. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chudecka-Głaz A, Menkiszak J, Kuźniak S,
Lewandowska M, Burak M and Walecka A: A rare case of peritoneal
disseminated angiosarcoma 20 years after ovarian cancer diagnosis.
Gynecol Obstet Invest. 77:68–72. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Narayanan S, Parker M, Shayo J, Zheng M,
Matulewicz T and Parker G: The Impact of Radiation on an Unusual
Case of Omental Epithelioid Angiosarcoma. Case Rep Surg.
2015:8490592015.PubMed/NCBI
|
|
6
|
Arlen M, Higinbotham NL, Huvos AG, Marcove
RC, Miller T and Shah IC: Radiation-induced sarcoma of bone.
Cancer. 28:1087–1099. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abraham JA, Hornicek FJ, Kaufman AM,
Harmon DC, Springfield DS, Raskin KA, Mankin HJ, Kirsch DG,
Rosenberg AE, Nielsen GP, et al: Treatment and outcome of 82
patients with angiosarcoma. Ann Surg Oncol. 14:1953–1967. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fayette J, Martin E, Piperno-Neumann S, Le
Cesne A, Robert C, Bonvalot S, Ranchère D, Pouillart P, Coindre JM
and Blay JY: Angiosarcomas, a heterogeneous group of sarcomas with
specific behavior depending on primary site: A retrospective study
of 161 cases. Ann Oncol. 18:2030–2036. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cha C, Antonescu CR, Quan ML, Maru S and
Brennan MF: Long-term results with resection of radiation-induced
soft tissue sarcomas. Ann Surg. 239:903–910. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Virtanen A, Pukkala E and Auvinen A:
Angiosarcoma after radiotherapy: A cohort study of 332,163 Finnish
cancer patients. Br J Cancer. 97:115–117. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Marmor RA, Kelly KJ, Lowy AM and
Baumgartner JM: Laparoscopy is safe and accurate to evaluate
peritoneal surface metastasis prior to cytoreductive surgery. Ann
Surg Oncol. 23:1461–1467. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schlemmer M, Reichardt P, Verweij J,
Hartmann JT, Judson I, Thyss A, Hogendoorn PC, Marreaud S, Van
Glabbeke M and Blay JY: Paclitaxel in patients with advanced
angiosarcomas of soft tissue: A retrospective study of the EORTC
soft tissue and bone sarcoma group. Eur J Cancer. 44:2433–2436.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Agulnik M, Yarber JL, Okuno SH, von Mehren
M, Jovanovic BD, Brockstein BE, Evens AM and Benjamin RS: An
open-label, multicenter, phase II study of bevacizumab for the
treatment of angiosarcoma and epithelioid hemangioendotheliomas.
Ann Oncol. 24:257–263. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Penel N, Bui BN, Bay JO, Cupissol D,
Ray-Coquard I, Piperno-Neumann S, Kerbrat P, Fournier C, Taieb S,
Jimenez M, et al: Phase II trial of weekly paclitaxel for
unresectable angiosarcoma: The ANGIOTAX Study. J Clin Oncol.
26:5269–5274. 2008. View Article : Google Scholar : PubMed/NCBI
|