Introduction
As the survival of patients with brain tumors has
increased with the advances in radiotherapy or intensive
chemotherapy, the risk of secondary brain tumors has also increased
significantly. Glioblastoma multiforme (GBM) is a high-grade glioma
that may develop from several other tumors, such as medulloblastoma
(MB), germinomas and Burkitt's lymphoma, after radiation therapy
(1). The first case of
radiation-induced GBM developing from MB following radiotherapy of
the central nervous system (CNS) was reported by Kleriga et
al in 1978 (2). Several similar
cases have since been reported. The majority of radiation-induced
glioblastomas (RIGs) may develop after a long latency period, and
appear more frequently in the same location as the irradiation
field. Furthermore, previous studies on RIGs report a more
aggressive course and poorer prognosis compared with typical
GBM.
Glioblastoma with rhabdoid characteristics was first
described by Wyatt-Ashmead in 2001 (3) as an extremely rare occurrence. An
increasing number of previous reports indicated that glioblastoma
with rhabdoid components exhibited a highly aggressive course and
often tended to occur in younger patients compared with typical
GBM.
We herein report a case of RIG with rhabdoid
characteristics in a 13-year-old boy who had received CNS
radiotherapy for MB of the posterior fossa 8 years earlier.
Case report
A 4-year-old boy was first admitted to the hospital
in April 2009 with headache, vomiting and gait disturbance. None of
his family members had any known genetic diseases predisposing to
cancer. Magnetic resonance imaging (MRI) of brain revealed an
enhanced space-occupying lesion in the fourth ventricle. This
lesion was completely resected, and was diagnosed as MB in April
2009 by postoperative histological examination. Postoperative
radiotherapy was performed, with a dose of 30.6 Gy delivered to the
craniospinal region and an additional delivery of 54 Gy to the
posterior fossa after craniospinal irradiation. Follow-up MRI or CT
scans were regularly performed thereafter, and revealed no evidence
of recurrence over the next 8 years.
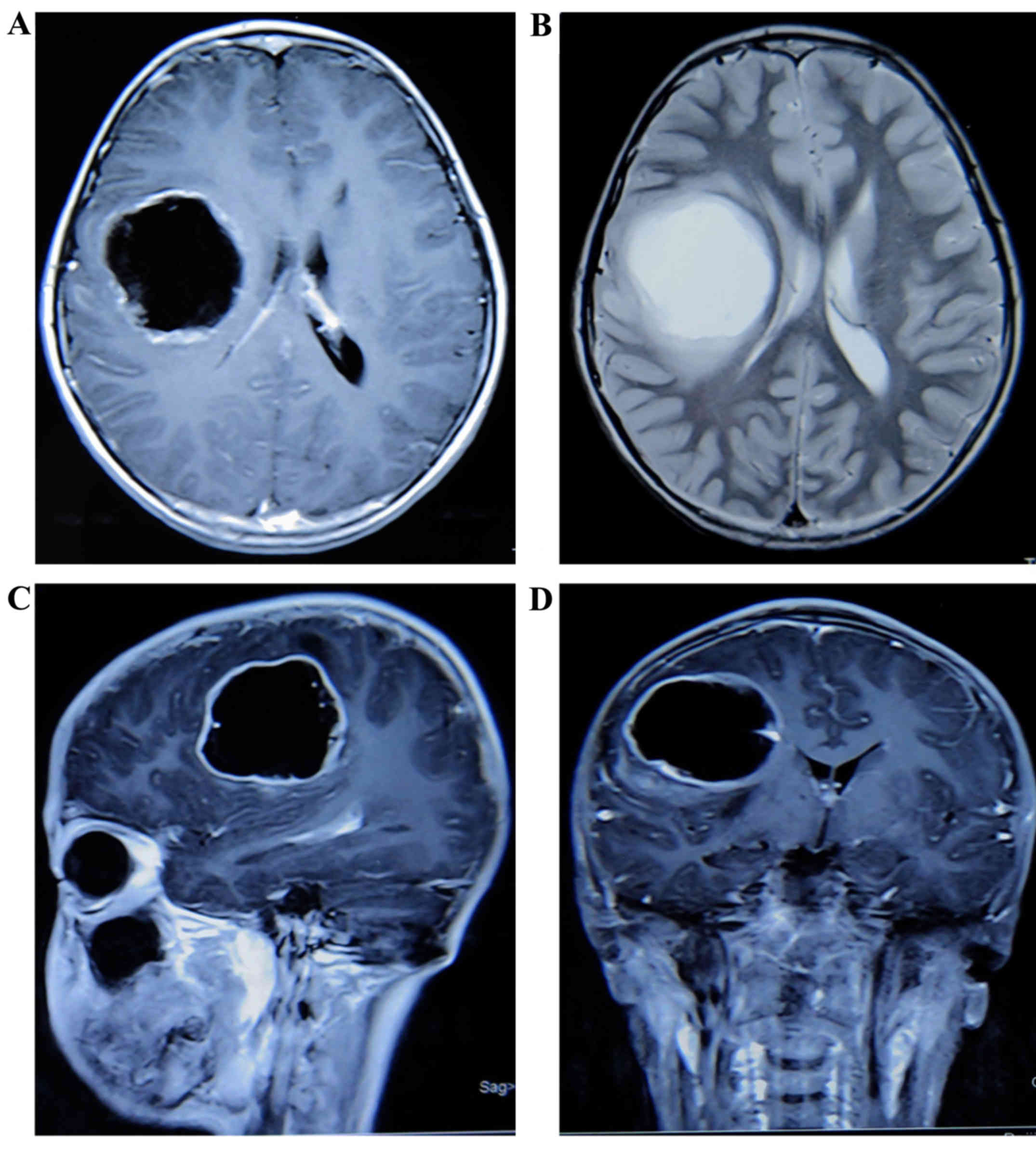
On January 2017, the patient was readmitted with
weakness of the distal left limbs without objective loss of
sensation, gait disturbance and ipsilateral angular salivation.
Subsequently, a brain MRI revealed a quasi-circular cystic lesion
with a significantly enhanced capsule in the right frontal lobe.
The lesion was poorly circumscribed, without obvious peritumoral
edema. The cystic component displayed inhomogeneous low signal on
T1-weighted images, and inhomogeneous hyperintense signal on
T2-weighted images. On February 2017, the patient underwent
surgical resection, and the subsequent histological diagnosis was
GBM. Intraoperatively, the main component of the lesion was cystic,
and the wall of the cystic lesion exhibited inhomogeneous
thickness. After surgery, the weakness of the left limbs worsened
and 2 months later the patient was readmitted with paroxysmal
headache. A brain MRI revealed multiple enhanced tissues adjacent
to the tumor bed in the right frontal lobe (Fig. 1). Subsequently, the patient received
4 cycles of chemotherapy with nimotuzumab, bevacizumab and
irinotecan (dosage records unavailable), following which there
remained no evidence, from regular reexaminations, to indicate
tumor progression.
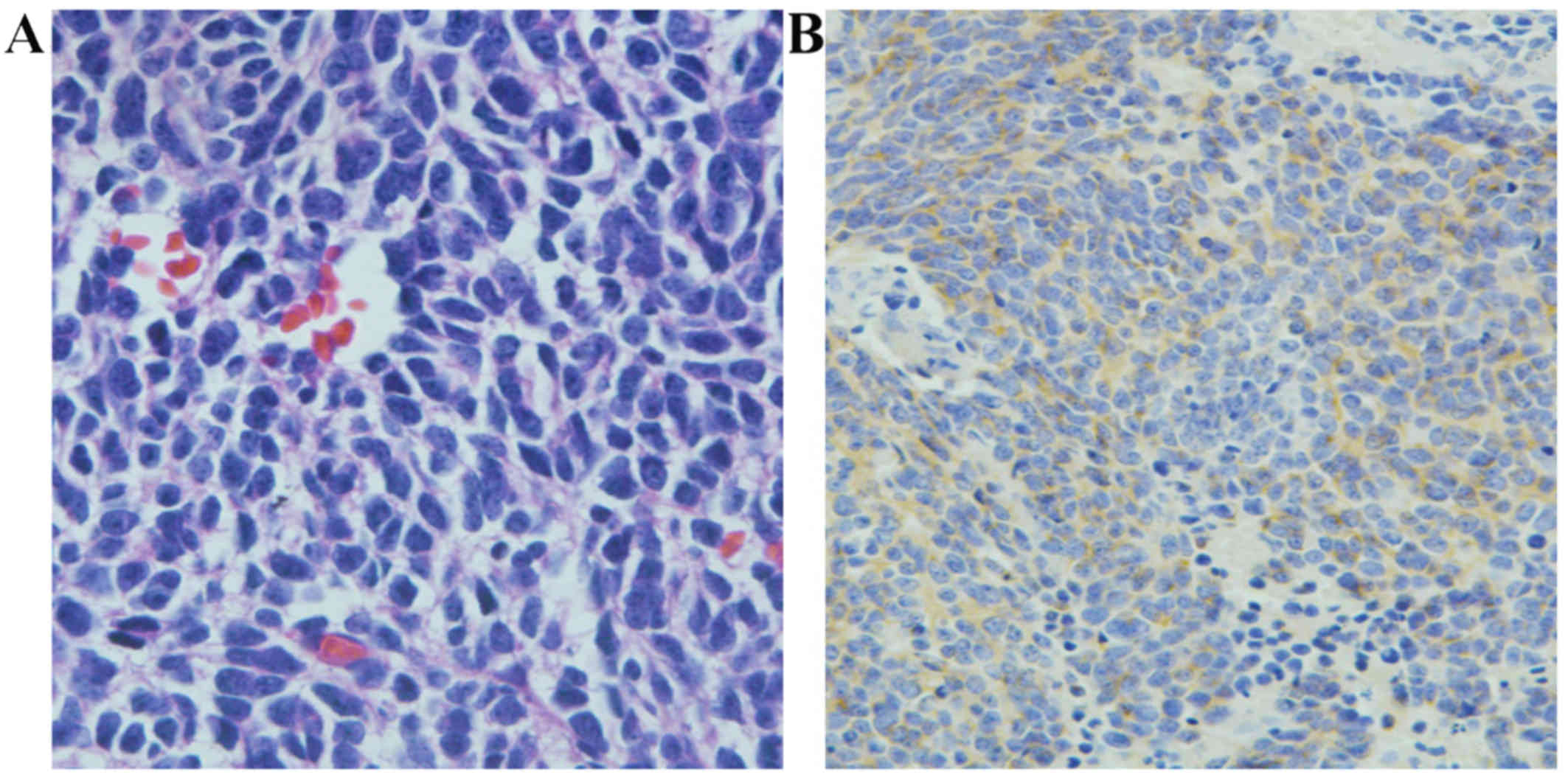
The first diagnosed tumor displayed characteristics
typical of MB: Pleomorphic tumor cells with sparse cytoplasm,
hyperchromatic nuclei, extensive presence of apoptosis/necrosis and
mitotic figures, with Homer-Wright rosettes (Fig. 2A). Immunohistochemical examination
revealed expression of synaptophysin (Syn) in the cytoplasm of some
MB cells (Fig. 2B). However,
neurofilament protein, S-100 and vimentin (Vim) were not expressed
in the tumor tissue.
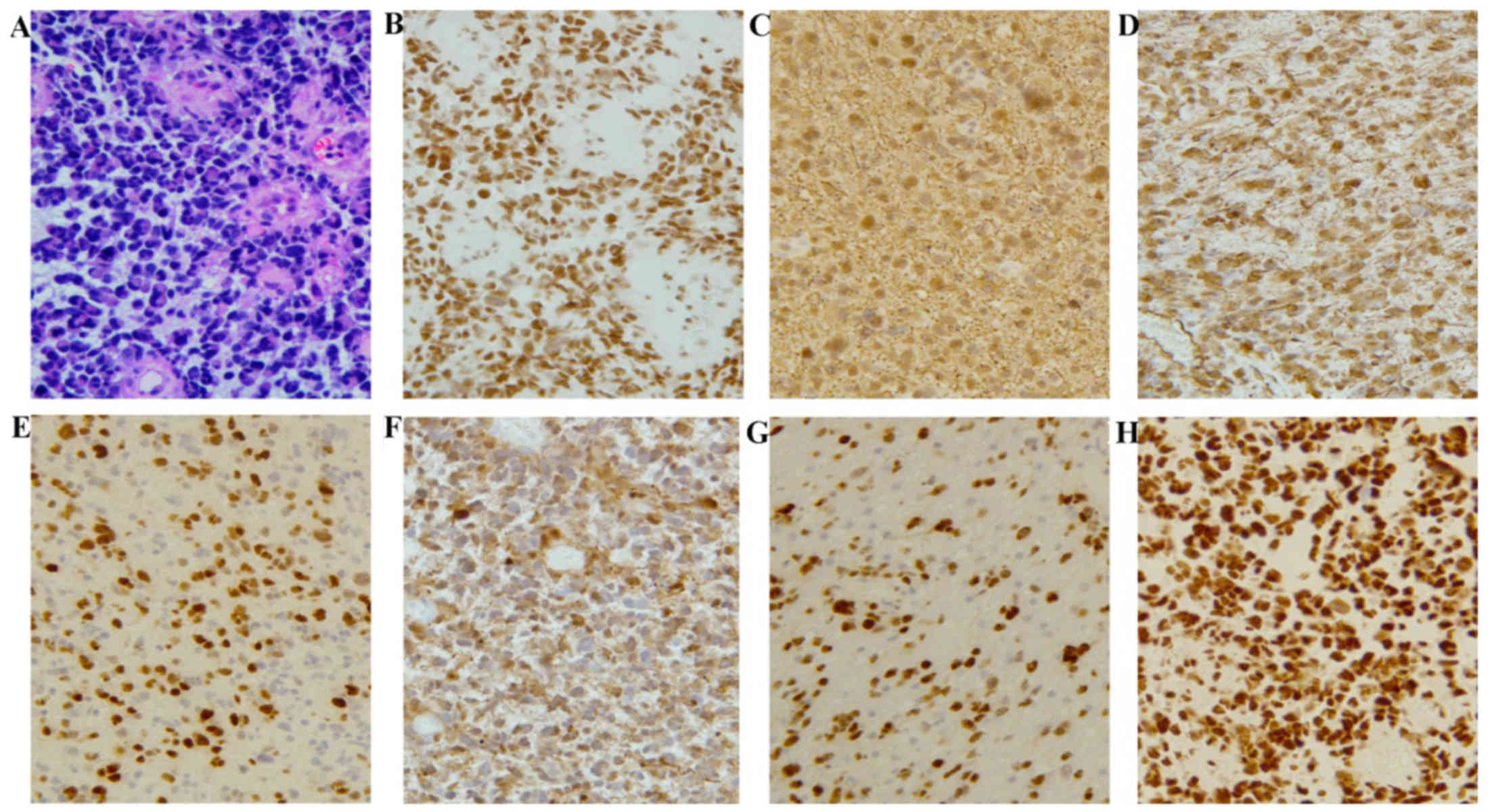
Histological examination of the secondary tumor
revealed that the neoplastic cells exhibited characteristics of
both glioblastoma and rhabdoid tumor cells. The majority of the
tumor cells exhibited microvascular proliferation, obvious atypia,
abundant cytoplasm, extensive apoptosis and mitotic figures, as
well as patchy necrosis. A few cells were characterized by
eccentric nuclei with prominent nucleoli. Furthermore, scattered
giant cells were identified. Immunohistochemically, the tumor cells
were strongly positive for glial fibrillary acidic protein (GFAP),
Vim and Olig-2. In addition, S-100, p53, isocitrate dehydrogenase 1
and α-thalassemia/mental retardation syndrome X-linked (ATRX) were
also expressed by these tumor cells, and smooth muscle actin (SMA)
was focally positive, reflecting the loss of integrase interactor-1
(INI-1) protein. However, there were no observations indicating
primitive neuroectodermal tumor in this case. The molecular
pathology revealed ATRX mutation and
O6-methylguanine-DNA-methyltransferase promoter
methylation. Examination by fluorescence in situ
hybridization demonstrated that there was no loss of heterozygosity
on chromosome 1p19q. The Ki-67 index (Ki 67-positive cells) was
~30–40% (Fig. 3). Unfortunately, the
patient died 1 year following the secondary recurrence.
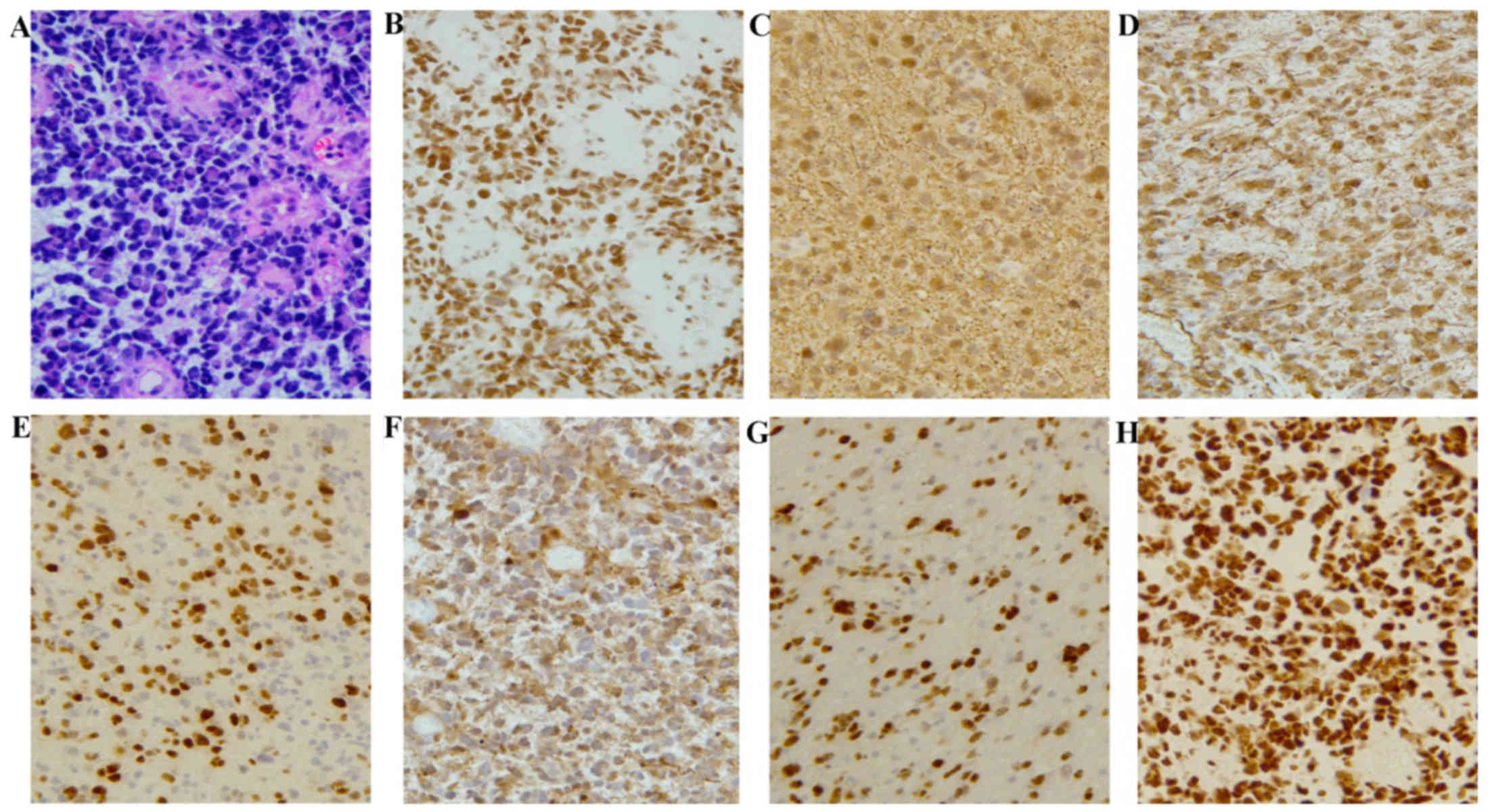 | Figure 3.Histological and immunohistochemical
characteristics of glioblastoma multiforme. (A) The histological
characteristics of the secondary tumor were obviously different
from those of the original tumor. Glioblastoma cells exhibited
microvascular proliferation, obvious atypia, abundant cytoplasm,
extensive apoptosis/necrosis and mitotic figures, as well as patchy
necrosis. A few cells were characterized by eccentrically located
nuclei with prominent nucleoli (hematoxylin and eosin staining;
magnification, ×200). (B) The tumor cell bearing characteristics of
rhabdoid cells exhibited loss of the INI-1 protein compared with
the surrounding INI-1-expressing cells (magnification, ×200). (C-H)
Immunohistochemically, the tumor cells highly expressed (C) GFAP,
(D) vimentin and (E) Olig-2. (F) S-100, (G) p53, and (H) ATRX were
also expressed in those tumor cells (magnification, ×200). INI-1,
integrase interactor 1; GFAP, glial fibrillary acidic protein;
ATRX, α-thalassemia/mental retardation syndrome X-linked. |
Discussion
Glioblastoma is a high-grade glioma that may develop
as a secondary tumor following radiation therapy. As reported in
the first animal experiment conducted by Haymaker et al in
1972 (4), glioblastoma was induced
by radiation in a monkey. Over the last 45 years, ~296 cases of
radiation-induced brain tumors, such as meningiomas, sarcomas and
gliomas, have been reported. The criteria of radiation-induced
glioblastoma established by Cahan et al (5) were as follows: i) The phenotypes of the
primary and secondary tumors were distinctly different; ii) the
site of the secondary tumor was within the field of irradiation;
iii) the secondary tumor should be histologically diagnosed; iv)
there should be a prolonged latency period between the treatment of
the primary and the appearance of the secondary tumor. The case in
our report was diagnosed as glioblastoma by histological
examination 8 years after radiotherapy for MB.
In a study by Minniti et al (6), the risk of secondary brain tumor
following conservative surgery and radiotherapy for pituitary
adenoma was 2.4% in 20 years. Similar to these results, scientists
in Margaret Hospital reported that the estimated cumulative risk
for RIG was 1.7–2.7% at 15 years after radiation therapy (7). RIG may develop from primary tumors such
as hematological malignancies, MB, pituitary adenoma, low-grade
glioma and craniopharyngioma. As demonstrated by previous data, MB
accounts for 12.8% of primary tumors (8).
The majority of radiation-induced brain tumors
(RIBTs) are reported in children who were aged <10 years when
they initially received radiotherapy. The first case of RBIT
reported by Kleriga et al (2), was a patient treated for MB at the age
of 10 months and developed a malignant astrocytoma in the same
location 11 years after radiotherapy. You et al reported 5
cases of secondary brain tumors; all these cases were irradiated at
an age of <10 years (1). The age
of patients who develop RIGs is frequently lower compared with that
of spontaneous high-grade gliomas. The case of RIG reported herein
had a history of radiotherapy for MB at the age of 4 years. These
findings indicate that patient age at first radiotherapy may be an
important factor in the development of RIBTs. Another factor
affecting the development of RIGs is irradiation volume. The
incidence of RIGs increased with increasing irradiation volume.
According to a review of patients with secondary brain tumors
induced by radiation therapy, the proportion of radiation-induced
malignant gliomas was 75% among patients receiving initial
radiotherapy of craniospinal or whole-brain fields (7). Our patient was treated with
craniospinal irradiation at first admission and the secondary tumor
occurred 8 years later within the radiation field.
A study by Yang et al (9) reported that the secondary tumor
exhibited strong immunoreactivity for both GFAP and p53. These
histological characteristics were also described in a case reported
by Donson et al (10).
Although p53 mutations were not detected, strong immunoreactivity
for p53 is frequently associated with gene mutations of p53. p53
gene mutations have been identified in radiation-induced tumors
(11,12); thus, they may play a relevant role in
the development of RIGs. However, the association between p53 gene
mutations and the occurrence of secondary tumors remains largely
unexplored.
In the present case, in addition to the strong
expression of GFAP and p53, Vim, Syn and epithelial membrane
antigen (EMA) were also expressed. As previously reported, Vim,
SMA, EMA and Syn were mostly expressed in the secondary
epithelioid/rhabdoid glioblastoma (13,14).
Furthermore, focal loss of the INI-1 protein was observed in
rhabdoid tumor cells, which were characterized by eccentric nuclei
with prominent nucleoli. Focal loss of the INI-1 protein was also
observed in cases reported by Sugimoto et al (15). Similar findings were also reported by
a study on four cases of rhabdoid glioblastoma (16). Unfortunately, all these cases had a
poor prognosis, with a median survival from the time of diagnosis
of rhabdoid glioblastoma of only ~4.9 months (16,17).
The present case represents a rare occurrence of RIG
with the characteristics of rhabdoid glioblastoma following CNS
radiotherapy. Due to the extremely poor prognosis, this type of
tumor should be further investigated and more studies are required
to determine its relevance to irradiation.
Acknowledgements
Not applicable.
Funding
This manuscript was supported by the National
Keypoint Research and Invention Program (grant no.
2016YFC0105705).
Availability of data and materials
All data generated during this study are included in
this published article.
Authors' contributions
YW, SJS, ZW and XS conceived and designed the study.
ZW, YW and ZD drafted the manuscript. JW, DC, YR, JF, QW and YS
critically revised the manuscript for content. All authors approved
the manuscript for submission.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient's parents provided written informed
consent for the publication of the case details and associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
You SH, Lyu CJ, Kim DS and Suh CO: Second
primary brain tumors following cranial irradiation for pediatric
solid brain tumors. Child's Nerv Syst. 29:1865–1870. 2013.
View Article : Google Scholar
|
|
2
|
Kleriga E, Sher JH, Nallainathan SK, Stein
SC and Sacher M: Development of cerebellar malignant astrocytoma at
site of a medulloblastoma treated 11 years earlier. Case report. J
Neurosurg. 49:445–449. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wyatt-Ashmead J, Kleinschmidt-De Masters
BK, Hill DA, Mierau GW, McGavran L, Thompson SJ and Foreman NK:
Rhabdoid glioblastoma. Clin Neuropathol. 20:248–255.
2001.PubMed/NCBI
|
|
4
|
Haymaker W, Rubinstein LJ and Miquel J:
Brain tumors in irradiated monkeys. Acta neuropathologica.
20:267–277. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cahan WG, Woodard HQ, Higinbotham NL,
Stewart FW and Coley BL: Sarcoma arising in irradiated bone: Report
of eleven cases. 1948. Cancer. 82:8–34. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Minniti G, Traish D, Ashley S, Gonsalves A
and Brada M: Risk of second brain tumor after conservative surgery
and radiotherapy for pituitary adenoma: Update after an additional
10 years. J Clin Endocrinol Metab. 90:800–804. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Paulino AC, Mai WY, Chintagumpala M, Taher
A and Teh BS: Radiation-induced malignant gliomas: is there a role
for reirradiation? Int J Radiat Oncol Biol Phys. 71:1381–1387.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yamanaka R, Hayano A and Kanayama T:
Radiation-induced gliomas: A comprehensive review and
meta-analysis. Neurosurg Rev. 5:2016.(Epub ahead of print).
|
|
9
|
Yang SY, Wang KC, Cho BK, Kim YY, Lim SY,
Park SH, Kim IH and Kim SK: Radiation-induced cerebellar
glioblastoma at the site of a treated medulloblastoma: Case report.
J Neurosurg. 102 4 Suppl:1–422. 2005.
|
|
10
|
Donson AM, Erwin NS,
Kleinschmidt-DeMasters BK, Madden JR, Addo-Yobo SO and Foreman NK:
Unique molecular characteristics of radiation-induced glioblastoma.
J Neuropathol Exp Neurol. 66:740–749. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gessi M, Maderna E, Guzzetti S, Cefalo G,
Massimino M, Solero CL, Finocchiaro G and Pollo B:
Radiation-induced glioblastoma in a medulloblastoma patient: a case
report with molecular features. Neuropathology. 28:633–639.
2008.PubMed/NCBI
|
|
12
|
Brachman DG, Hallahan DE, Beckett MA,
Yandell DW and Weichselbaum RR: p53 gene mutations and abnormal
retinoblastoma protein in radiation-induced human sarcomas. Cancer
Res. 51:6393–6396. 1991.PubMed/NCBI
|
|
13
|
Nagai S, Kurimoto M, Ishizawa S, Hayashi
N, Hamada H, Kamiyama H and Endo S: A rare astrocytic tumor with
rhabdoid features. Brain Tumor Pathol. 26:19–24. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mutou J, Hirose Y, Ikeda E, Yoshida K,
Nakazato Y and Kawase T: Malignant brain tumor with rhabdoid
features in an adult. Neurol Med Chir (Tokyo). 51:449–454. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sugimoto K, Ideguchi M, Kimura T, Kajiwara
K, Imoto H, Sadahiro H, Ishii A, Kawano H, Ikeda E and Suzuki M:
Epithelioid/rhabdoid glioblastoma: A highly aggressive subtype of
glioblastoma. Brain Tumor Pathol. 33:137–146. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Babu R, Hatef J, McLendon RE, Cummings TJ,
Sampson JH, Friedman AH and Adamson C: Clinicopathological
characteristics and treatment of rhabdoid glioblastoma. J
Neurosurg. 119:412–419. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Byeon SJ, Cho HJ, Baek HW, Park CK, Choi
SH, Kim SH, Kim HK and Park SH: Rhabdoid glioblastoma is
distinguishable from classical glioblastoma by cytogenetics and
molecular genetics. Hum Pathol. 45:611–620. 2014. View Article : Google Scholar : PubMed/NCBI
|