Introduction
Okino et al (1) introduced the concept of
electrochemotherapy (ECT), on the basis of electroporation, in
1992. Electric pulses with a long length (ms–μs) have been shown to
induce a transient rearrangement of the lipid bilayer of cells and
form aqueous channels in the cell membrane, this is termed
electroporation (2). Hofmann et
al (3) and Dev et al
(4) applied electrochemotherapy in
conjunction with bleomycin, to treat cancers, this strategy
significantly reduced the side effects of the drug. Electric pulses
with a short duration (ns–ps) have been shown to mainly affect
intracellular organelles and cause apoptosis, as well as
cytoskeletal, nuclear membrane and DNA damage, whilst maintaining
an intact plasma membrane (5–7).
According to the time-domain theory (8), psPEF has a wealth of ultra-wideband
(UWB) spectrum (almost from direct current up to GHz), therefore it
has a higher time and spatial resolution, with little distortion of
the signal. If psPEF may be used to target deeper target lesions,
without harming the normal tissues, a non-invasive treatment for
tumors may be achieved (9).
Mitochondrial transmembrane potential has a crucial role in
apoptosis. A lower mitochondrial membrane potential induces the
release of cytochrome C and activates the caspase family, which
ultimately leads to apoptosis (10).
Previous results have indicated that microsecond PEF
(μsPEF) and nanosecond PEF (nsPEF) may induce apoptosis of SKOV3
and HeLa cells, through the mitochondrial and endoplasmic reticulum
pathways (11–15). The aim of the present study was to
evaluate the efficacy of psPEF on a cervical cancer xenograft. A
cervical cancer xenograft was generated in nude mice as a model,
and the effectiveness of certain psPEF parameters on the tumor was
investigated in vivo.
Materials and methods
Chemicals and reagents
RPMI-1640 media and fetal bovine serum (FBS) were
purchased from Gibco Life Technologies (Carlsbad, CA, USA); the
Terminal Deoxynucleotidyl-transferase-mediated dUTP Nick End
Labeling (TUNEL) Detection kit was obtained from Roche Diagnostics
(Basel, Switzerland). The Mitochondria Isolation kit, Mitochondrial
Membrane Potential Assay kit with JC-1, and Caspase-3, -8 and -9
Activity Assay kits were purchased from Beyotime Institute of
Biotechnology (Haimen, China). A Bradford Protein Assay kit was
purchased from Comwin Biotech Co., Ltd. (Beijing, China), and the
Caspase-12 Quantification kit was purchased from Genmed
Scientifics, Inc., USA (Shanghai, China).
Cells
The HeLa human cervical cancer cells (Cell bank of
Committee on Type Culture Collection of Chinese Academy of
Sciences, Wuhan, China) were cultured in RPMI-1640, supplemented
with 10% FBS, 100 U/ml penicillin and 100 μg/ml streptomycin, at
37°C and in an atmosphere containing 5% CO2. The cells
were digested with trypsin, and 2×107 cells/ml were
prepared for subcutaneous injection.
Tumor models
The female nude mice were obtained from the
Laboratory Animal Center of Chongqing Medical University,
(Chongqing, China), aged six weeks. The mice were fed under
specific pathogen-free conditions, and were randomly divided into
four groups (six mice per group). A HeLa cell/Matrigel mixture of
0.2 ml was injected into the dorsal subcutis of the nude mice. The
psPEF treatment was performed once the xenograft had reached a
diameter of 0.8–1.0 cm (~2 weeks). Ethical approval of animal
procedures was obtained from the Second Affiliated Hospital of
Chongqing Medical University.
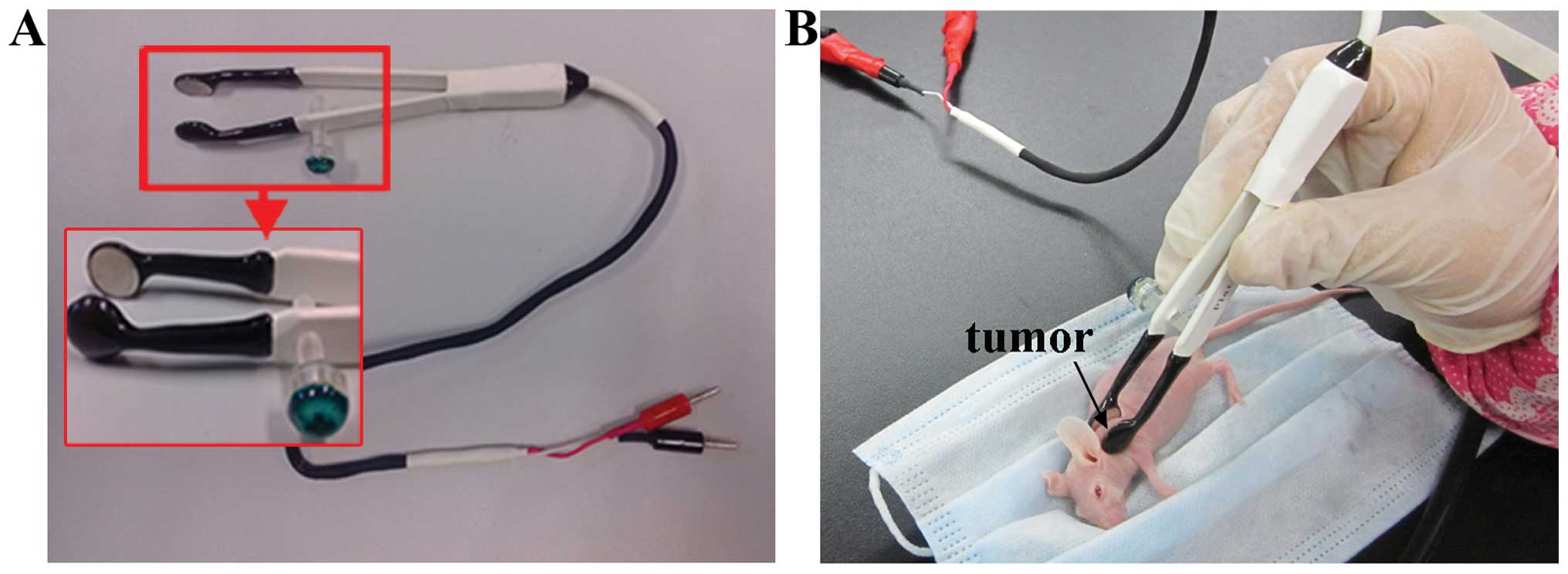
Exposure to electrical pulses
Following anesthesia by intraperitoneal injection of
0.7 ml 10% chloral hydrate, the tumor was placed closely and
non-invasively between the tweezer-electrodes (Fig. 1), and exposed to 2,000 pulses, at a
3 Hz frequency for 800 psec, with 120–140 kV/cm strength. The
electric field amplitude and pulse width were monitored throughout
the procedures using a DP04054 oscilloscope (Tektronix, Inc.,
Beaverton, OR, USA). The control mice were not treated, and the
tumor tissues were harvested once the tumor had reached a diameter
of 0.8–1.0 cm. In the experimental 6 h group, the mice were
sacrificed and the xenografts were harvested 6 h following
electrical pulse exposure. In the 12 h group, the nude mice were
sacrificed by cervical dislocation 12 h following electrical pulse
exposure and the tumors were harvested. In the 24 h group, the nude
mice were sacrificed and the tumors were harvested 24 h following
electrical pulse exposure.
Ultrastructural study
The tumors were fixed in cacodylate-buffered 1%
osmium tetroxide, dehydrated, and embedded in Epon 812 for
ultra-thin sectioning. The tissue sections were stained with uranyl
acetate and lead citrate and observed under a transmission electron
microscope (TEM; H-7500; Hitachi Ltd., Tokyo, Japan).
TUNEL assay
The tissue sections were incubated in terminal
deoxynucleotidyly-transferase (TdT) buffer and TdT reaction
solution mixture. Briefly, the sections were soaked in 2X saline
sodium citrate solution for 10 min, in order to terminate the
reaction. The sections were then incubated in Chain-avidin-marked
horseradish peroxidase enzyme for 30 min, and stained with 0.04%
DAB for 5–10 min and hematoxylin for 3–5 min. The sections were
processed using a TUNEL Detection kit, according to the
manufacturer’s instructions. The TUNEL-positive cells, per field,
were counted in 10 random fields, and the counts were averaged.
Apoptotic index = (number of apoptotic cells/number of all tumor
cells) × 100%.
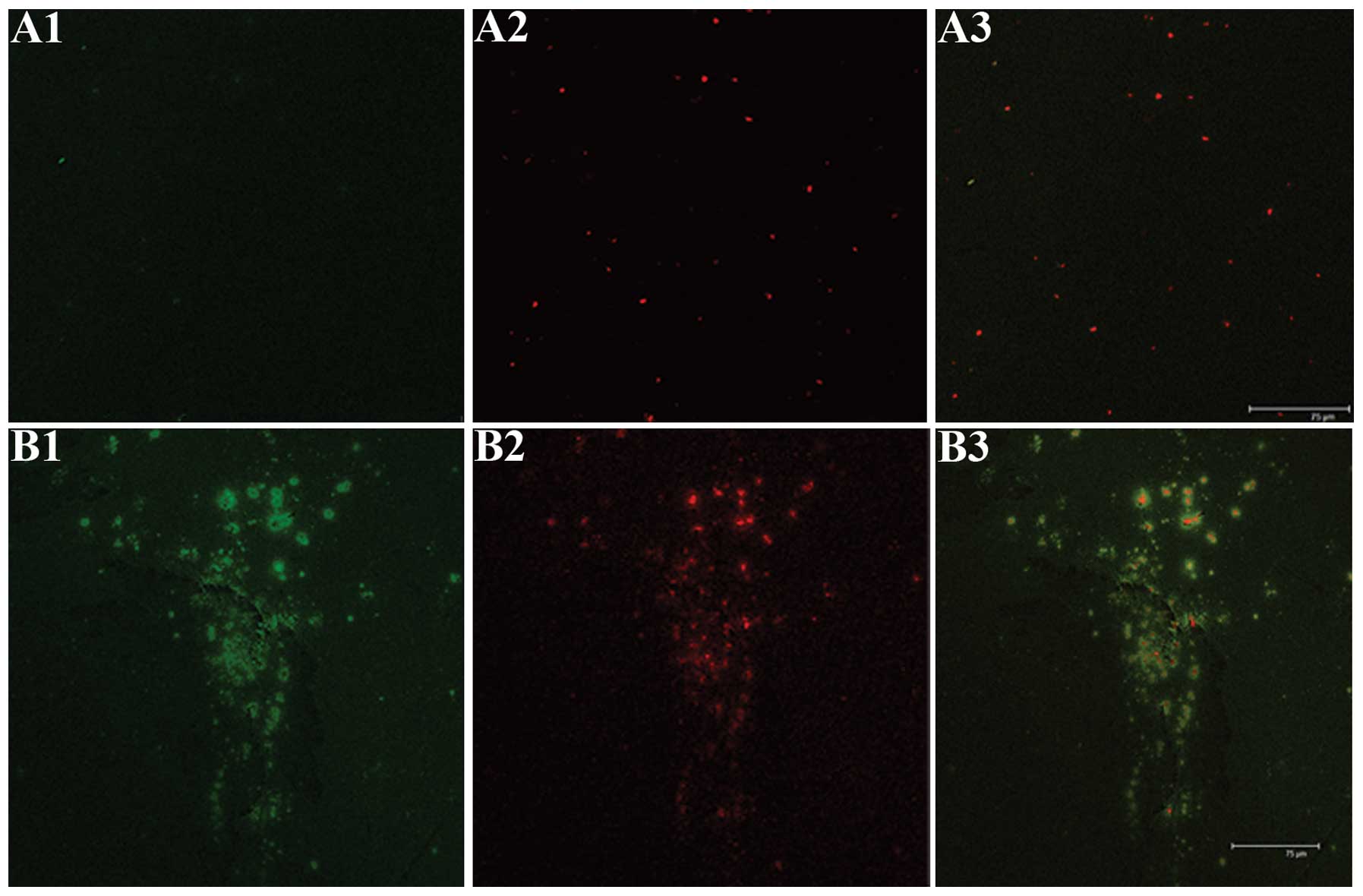
Laser scanning confocal microscopy (LSCM)
evaluation of mitochondrial transmembrane potential
The tumor tissues were homogenized in Mitochondria
Isolation Reagent A and the homogenates were centrifuged at 600 × g
for 5 min, at 4°C. The sediment was then stained using the
ΔΨm-specific probe JC-1 for 5–10 min. The samples were visualized
using LSCM (TCS-SP2; Leica, Wetzlar, Germany) with fluorescein
isothiocyanate (green) and rhodamine isothiocyanate (red) channels.
Red fluorescence was considered to represent a higher mitochondrial
membrane potential, whereas green fluorescence was considered to
represent a lower mitochondrial membrane potential. The two
fluorescent images (green and red) were analyzed using confocal
software (PCS-SP2 confocal laser fluorescence semi-quantitative
analysis software; Leica) which allowed for the quantification of
the intensity of green and red fluorescence.
Caspase-3, -8 and -9 activity assay
The activity of caspase-3, -8 and -9 was measured
using commercially available kits. Briefly, the tumor samples were
homogenized in lysis buffer and the homogenates were centrifuged at
16,000 × g, for 15 min at 4°C. The supernatants were collected and
the protein concentrations were determined using the Bradford
Protein Assay. Caspase-3, -8, and -9 activity was measured using
substrate peptides Ac-DEVD-pNA. The absorbance was measured at a
wavelength of 405 nm, using an EXL 800 Universal Microplate Reader
(BioTek Instruments Inc., Winooski, VT, USA).
Caspase-12 activity assay
The frozen tumor was ground to a powder and
transferred to a tube containing 150 μl lysis buffer. The tissue
was homogenized and centrifuged at 16 × g for 10–15 min, at 4°C.
The supernatant was transferred to a new tube and incubated for 90
min. The absorbance was measured at a wavelength of 405 nm using
the EXL 800 Universal Microplate Reader.
Inhibition rate
The nude mice were sacrificed and the tumor samples
were harvested. The inhibitory rate was subsequently calculated on
the seventh day following psPEF treatment. Inhibition rate (%) = (1
− average weight of the tumor in the treated group/average weight
of tumor in the untreated group) × 100%.
Statistical analysis
All of the data were processed using the statistical
software SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). The
student’s t-test, a one-way analysis of variance and a
χ2 test were used to determine the statistical
significance of the differences between the groups. A P<0.05 was
considered to indicate a statistically significant difference.
Results
Histology
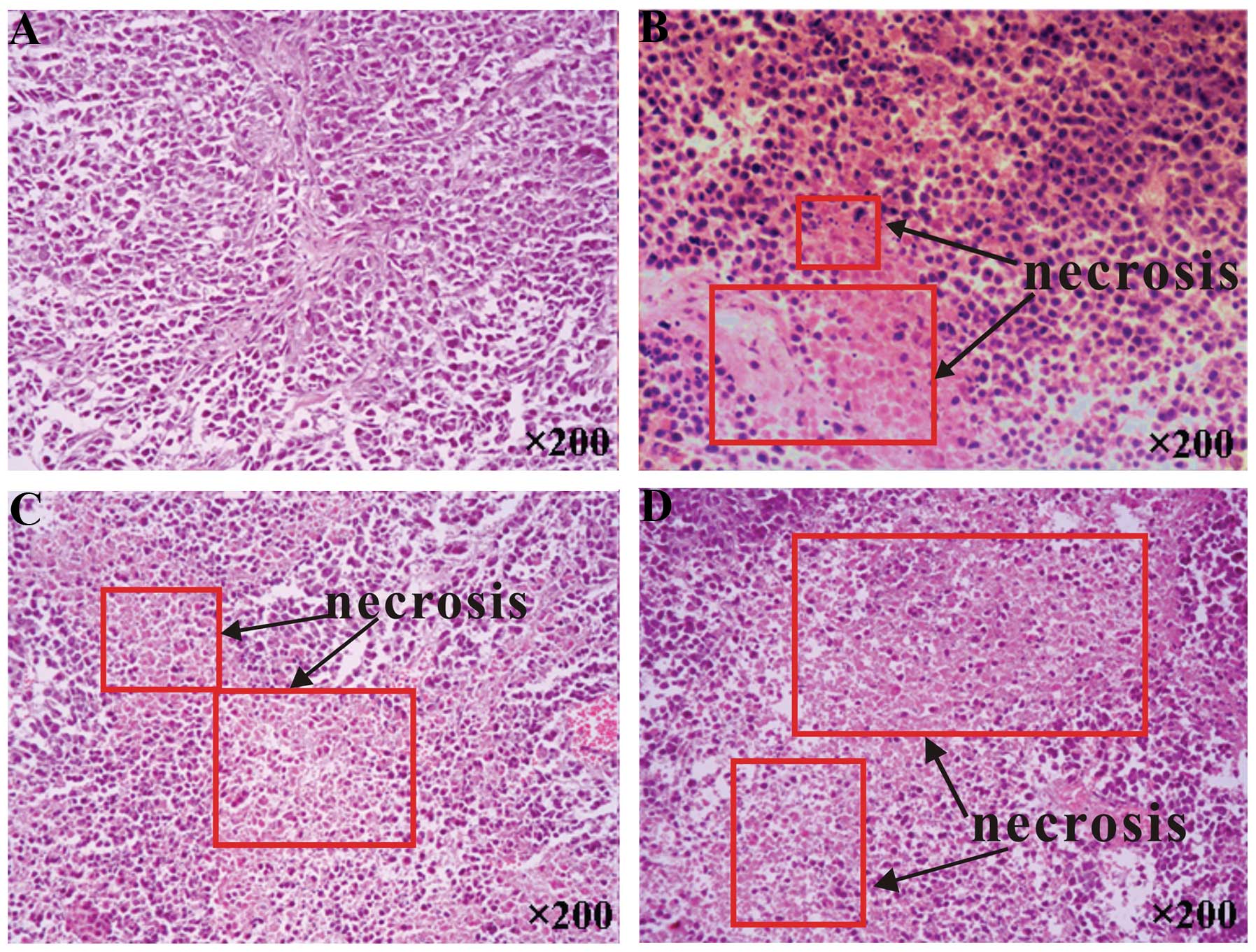
In the pathological examinations, necrosis was not
observed to be present in the control tumors, whereas psPEF
treatment led to cell necrosis (Fig.
2B), which was most notable in the 24 h group (Fig. 2D). The TEM demonstrated that the
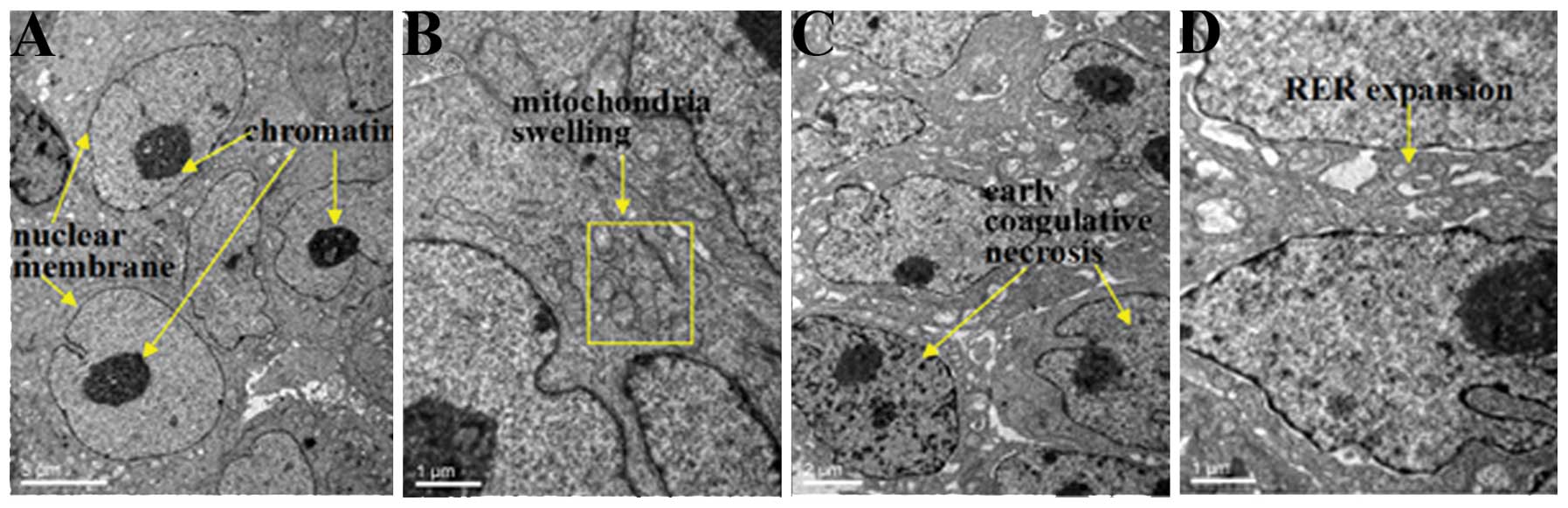
control tumors exhibited mild mitochondrial swelling (Fig. 3A and B). The tumors that underwent
psPEF treatment showed early coagulative necrosis in the 6 h group
(Fig. 3C and D); notable
coagulative necrosis (Fig. 3E) and
numerous apoptotic bodies (Fig.
3F) in the 12 h group; and severe coagulative necrosis
(Fig. 3G) and few apoptotic bodies
(Fig. 3H) in the 24 h group.
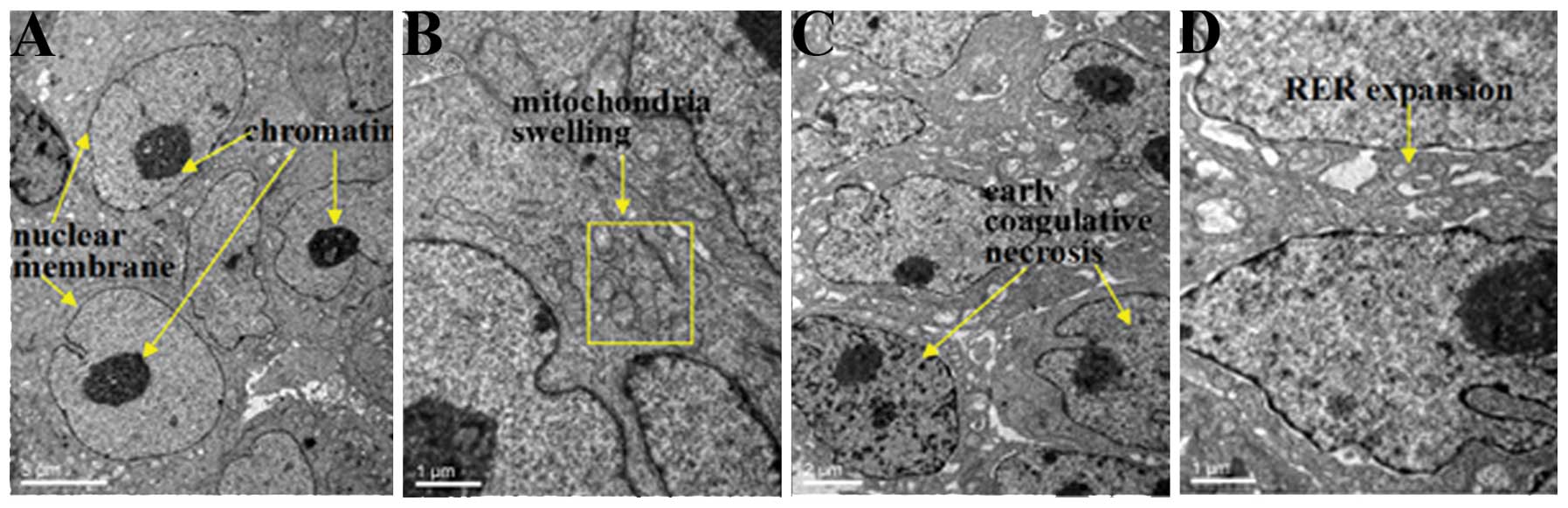 | Figure 3Ultrastructure of the human cervical
carcinoma in the nude mice xenograft model under transmission
electron microscopy. (A and B) Controls, not treated with
picosecond pulsed electric fields (psPEF), and the cells at (C and
D) 6 h, (E and F) 12 h and (G and H) 24 h following exposure to
psPEF treatment. The cells of the control group were intact, with
(A) well distributed chromatin, a clear nuclear membrane, and (B)
mild mitochondrial swelling. However, the cells of the 6 h group
demonstrated (C) early coagulative necrosis with (D) rough
endoplasmic reticulum expansion. The 12 h group had (E) notable
coagulative necrosis but the cell outline remained visible, a
segmentally fractured plasma membrane and (F) numerous apoptotic
bodies. The 24 h group had (G) severe coagulative necrosis, in
which the cell outline disappeared, and there were (H) few
apoptotic bodies. Following the psPEF treatment, apoptotic bodies
appeared, which were markedly evident in the 12 h group, and
necrosis of the cells increased which was most notable in the 24 h
group. Magnification: A, ×4,000; B,:x15,000; C, ×7,000; D, ×15,000;
E,:x15,000; F, ×7,000; G, ×7,000; H, ×15000. |
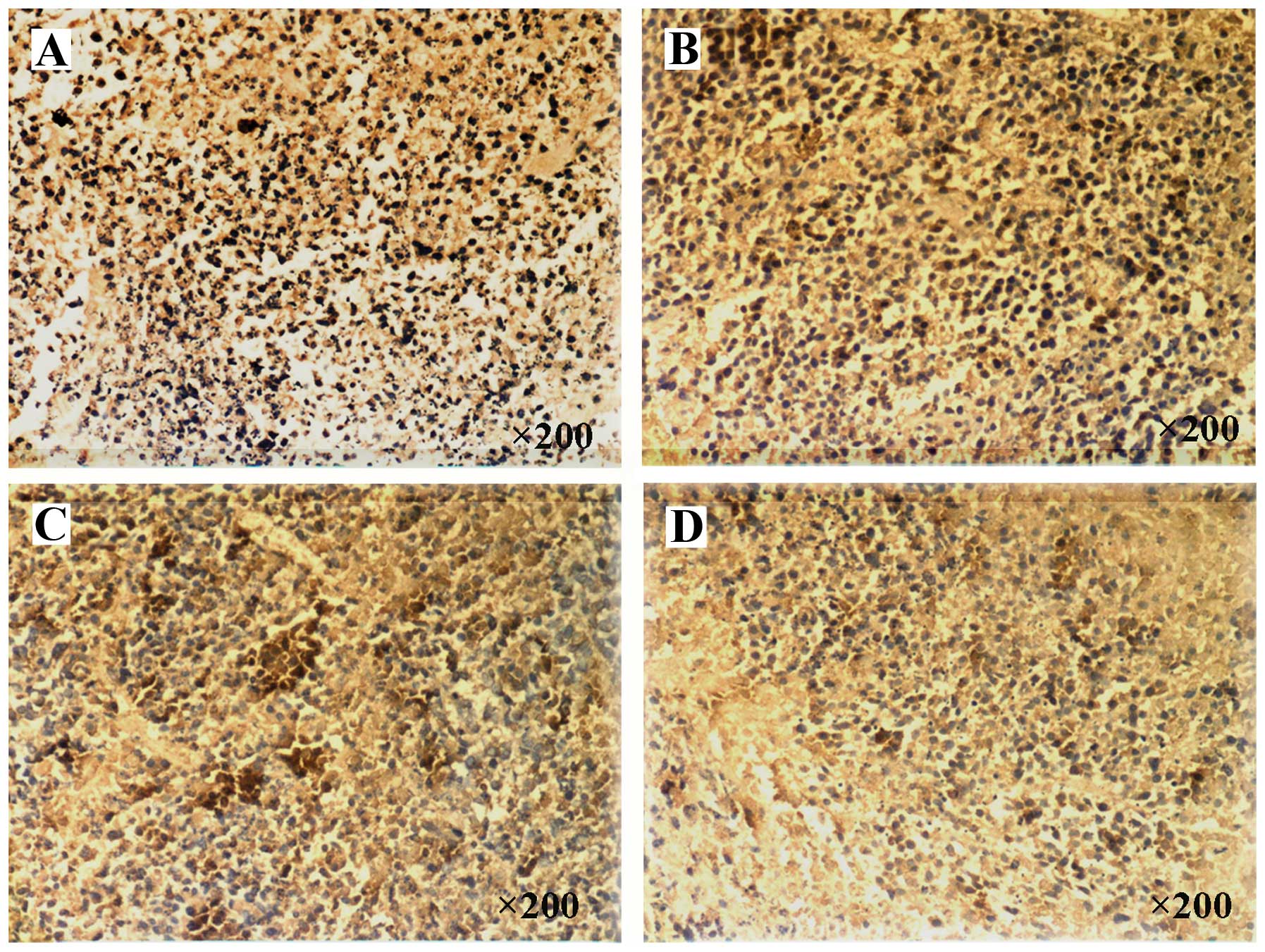
Rate of apoptosis
There was an increased rate of apoptosis in all of
the treatment groups, as compared with the control group
(P<0.01; Fig. 4E). The
apoptotic rate of the 12 h group was significantly higher, as
compared with the other treatment groups (P<0.01; Fig. 4E). However, there were no
statistical differences between the 6 and 24 h groups.
Mitochondrial transmembrane
potential
When stained with the mitochondria-specific probes
JC-1, the mitochondria of tumor cells may emit red and green
fluorescence. The experimental 6 and 12 h groups presented a
reduced red fluorescence and increased green fluorescence, as
compared with the untreated controls (Fig. 5A–C). However, the experimental 24 h
group presented weak red and green fluorescence, as compared with
the 6 and 12 h groups (Fig.
5D).
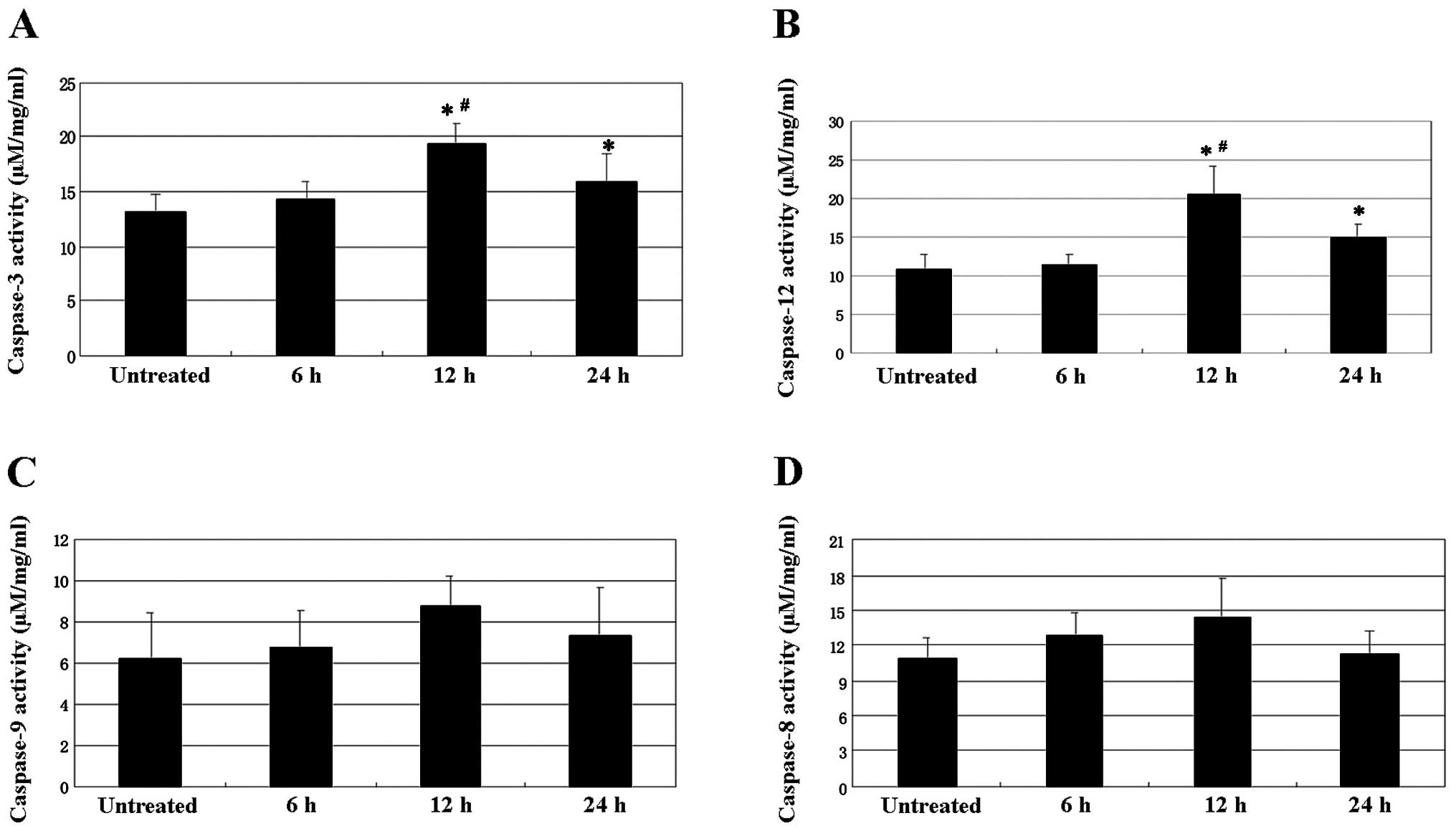
Caspase-3, -8, -9 and -12 activity
The activity of caspase-3 and caspase-12 was
increased in the tumors, following exposure to psPEF. Caspase-3
activity in the various groups had the following hierarchical
pattern: 12 h>24 h>6 h=control group (P<0.05; Fig. 6A). Caspase-12 activity in the
various groups had the following hierarchical pattern: 12 h>24
h>6 h=control group (P<0.01; Fig. 6B). However, caspase-8 and -9
activity were not affected by exposure to psPEF (Fig. 6C and D).
Inhibition rate
The rate of inhibition was 9.11% at the seventh day
following exposure to psPEF. This demonstrated that, to some
extent, picosecond pulsed electric fields are able to inhibit tumor
growth in a xenograft tumor model of cervical cancer.
Discussion
The results of the present study suggest that psPEF
may induce cellular apoptosis of a cervical cancer xenograft, by
activation of the endoplasmic reticulum stress signaling
pathway.
For the purpose of preserving fertility, an
effective and non-invasive therapy for cervical carcinoma is
required. PEF is a novel technique. psPEF may be transferred to
non-invasive target deep tissue (8,16),
thus resulting in non-invasive treatment. Previous studies have
demonstrated that psPEF is an efficient apoptosis-inducing agent in
HeLa cells, through the endoplasmic reticulum stress and
caspase-dependent signaling pathways (15). However, there are differences
between cellular in vitro and in vivo experiments.
Cell activity is affected by humoral regulation and other factors
in vivo. The presence of both cervical cancer and normal
tissue may have an effect on the efficacy of psPEF in vivo.
Therefore, a study determining the effects of psPEF on a cervical
cancer xenograft was required, which is more relevant for clinical
applications. The present study demonstrated that psPEF is
effective on cervical carcinoma in vivo. psPEF led to tumor
cell death in a cervical carcinoma xenograft, which gradually
increased with prolonged exposure, during which there was
significant tumor cell apoptosis. These results suggest that
apoptosis has an important role in tumor cell death. Also, LSCM
showed that the mitochondrial membrane potential of the tumor
decreased following psPEF treatment, and the number of mitochondria
in the 24 h treatment group was reduced, as compared with the 12 h
group. These results indicate that some apoptotic tumor cells may
die and be subsequently cleared away. Furthermore, the tumor
inhibition rate suggested that psPEF could effectively inhibit
tumor growth in vivo.
The alterations to cellular protein activation
associated with psPEF stimulation may provide valuable information
to determine the occurrence of stress, and also to help elucidate
the mechanisms of action of pulses on cervical carcinoma in
vivo. The present study suggested that psPEF induced tumor cell
apoptosis through the endoplasmic reticulum stress and
caspase-dependent signaling pathways.
In conclusion, the present study demonstrated the
efficacy of psPEF on cervical carcinoma in vivo. These
findings may be used to develop a non-invasive therapeutic
strategy. A future study may include a larger sample size and
modified psPEF parameters. Additional studies on the safety of
psPEF in vivo are currently underway.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (no. 81172123).
References
|
1
|
Okino M, Tomie H, Kanesada H, et al:
Optimal electric conditions in electrical impulse chemotherapy. Jpn
J Cancer Res. 83:1095–1101. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weaver JC: Electroporation: a general
phenomenon for manipulating cells and tissues. J Cell Biochem.
51:426–435. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hofmann GA, Dev SB, Dimmer S and Nanda GS:
Electroporation therapy: a new approach for the treatment of head
and neck cancer. IEEE Trans Biomed Eng. 46:752–759. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dev SB, Rabussay DP, Widera G and Hofmann
GA: Medical applications of electroporation. IEEE Trans Plasma Sci.
28:206–223. 2000. View Article : Google Scholar
|
|
5
|
Stacey M, Stickley J, Fox P, et al:
Differential effects in cells exposed to ultra-short, high
intensity electric fields: cell survival, DNA damage and cell cycle
analysis. Mutat Res. 542:65–75. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Craviso GL, Chatterjee P, Maalouf G, et
al: Nanosecond electric pulse-induced increase in intracellular
calcium in adrenal chromaffin cells triggers calcium-dependent
catecholamine release. IEEE Trans Dielectr Electri Insul.
16:1294–1301. 2009. View Article : Google Scholar
|
|
7
|
Stacey M, Fox P, Buescher S and Kolb J:
Nanosecond pulsed electric field induced cytoskeleton, nuclear
membrane and telomere damage adversely impact cell survival.
Bioelectrochemistry. 82:131–134. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baum CE, Stone AP and Tyo JS:
Ultra-wideband, short-pulse electromagnetics. 8. Springer Press;
New York, NY, USA: 2007
|
|
9
|
Long Z, Yao C, Li C, Mi Y and Sun C:
Focusing properties of picosecond electric pulses in non-invasive
cancer treatment. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi.
27:1128–1132. 2010.(In Chinese). PubMed/NCBI
|
|
10
|
Jeong SY and Seol DW: The role of
mitochondria in apoptosis. BMB Rep. 41:11–22. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yao CG, Guo F, Wang J, Li CX, Wen YQ and
Tang JY: Study of tumor cell mitochondrial apoptosis signaling
pathway induced by nanosecond pulsed electric fields. Chin J Biomed
Eng. 29:724–730. 2010.
|
|
12
|
Liu LJ, Zhao DY, Wang J, et al:
Ca2+ is an important mediator of nanosecond steep
pulse-induced apoptosis in human ovarian cancer SKOV3 cells. Nan
Fang Yi Da Xue Xue Bao. 31:772–776. 2011.(In Chinese).
|
|
13
|
Tang JY, Wu XJ, Yao CG, Yao ZW and Sun CX:
The effects of nanosecond steep pulse on apoptosis and the
concentration of intracellular calcium of human ovarian carcinoma
cell line SKOV3. Prog Obstet Gynecol. 16:827–831. 2007.
|
|
14
|
Hua YY, Wang XS, Zhang Y, et al: Intense
picosecond pulsed electric fields induce apoptosis through a
mitochondrial-mediated pathway in HeLa cells. Mol Med Rep.
5:981–987. 2012.PubMed/NCBI
|
|
15
|
Chen WJ, Xiong ZA, Zhang M, et al:
Picosecond pulsed electric fields induce apoptosis in HeLa cells
via the endoplasmic reticulum stress and caspase-dependent
signaling pathways. Int J Oncol. 42:963–970. 2013.PubMed/NCBI
|
|
16
|
Bajracharya C, Shu X, Baum CE and
Schoenbach KH: Target detection with impulse radiating antenna.
IEEE Antennas Wireless Propag Lett. 10:496–499. 2011. View Article : Google Scholar
|