Introduction
Diabetes is a chronic metabolic syndrome caused by
insulin deficiency and resistance. There are 200 million diabetic
individuals in the world, with only approximately one-half being
diagnosed, and these numbers are expected to double by 2030. The
disease often results in long-term microvascular, neurological, and
macrovascular complications, including retinopathy, nephropathy,
neuropathy, and increased risk of cardiovascular disease. Excessive
activation of angiotensin II (AngII) is an important underlying
mechanism for the development of diabetes, and Ang (1-7) is
hypothesized to counteract it. Furthermore, the renin-angiotensin
system (RAS) is significantly involved in the development of
diabetes and its complications. The activation of RAS causes
pancreatic β cell dysfunction by suppressing pro-insulin
biosynthesis, glucose-stimulated insulin secretion (GSIS) and first
phase insulin secretion (1–2), as
well as by increasing islet fibrosis (3) and oxidative stress (4). The angiotensin-converting enzyme 2
(ACE2)-angiotensin (1-7) [Ang (1-7)]-Mas axis is suggested to have
an antagonistic effect on the RAS, while Ang (1-7) is the main
antagonist of AngII. Angiotensin-converting enzyme inhibitor (ACEI)
and angiotensin receptor antagonist (ARB) can alleviate these
pathological changes (3,5–7).
Also, several clinical experiments have demonstrated the
effectiveness of RAS blockade in reducing the onset of diabetes
(8–11).
In 2006, it was demonstrated that patients with
Severe Acute Respiratory Syndrome (SARS) were more inclined to
exhibit higher blood glucose (12), and this may be partly due to the
fact that ACE2 is a functional receptor for the SARS coronavirus
(13). Thus we hypothesized that
the ACE2-Ang (1-7)-Mas axis has a protective effect on pancreatic β
cell function. Our previous study demonstrated for the first time
that loss of ACE2 led to impaired glucose homeostasis in mice. In
addition, ACE2 knockout (ACE2-/y) mice exhibit progressive
impairments in glucose tolerance and reduced first-phase insulin
secretion (14). The present study
aimed to investigate the underlying molecular mechanisms of these
effects. Accordingly, ACE2 gene therapy improved glycemic control
in diabetic mice via Ang (1-7) (15). Ang (1-7) is hypothesized to exhibit
antioxidant effects in diabetic nephropathy, hypertension,
cardiovascular diseases and in the brain (16–19).
These data confirm the protective role of the ACE2-Ang (1-7)-Mas
axis in the pancreas and establish a novel target for the treatment
of type 2 diabetes mellitus.
Oxidative stress is one of the most important
factors in β cell loss (20).
However, little is known regarding the correlation between Ang
(1-7) and oxidative stress in the pancreas. In the present study,
the protective effect of Ang (1-7) on oxidative β cell damage was
investigated. The protective effect was shown to occur by improving
GSIS, glucose stimulated calcium (GSCa) responses and the
mitochondrial membrane potential (MMP), which was demonstrated
previously (21), and reducing the
production of reactive oxygen species (ROS). The selective receptor
antagonist A779 was used to confirm the protective role of Ang
(1-7).
Materials and methods
Cell culture
INS-1 insulinoma cells were a gift from Professor
Liu Yong (Shanghai Institutes for Biological Science, Chinese
Academy of Sciences, Shanghai, China), which were originally
supplied by Dr Claes Wollheim, University Medical Center (Geneva,
Switzerland). The culture medium consisted of RPMI-1640 (Hyclone,
Logan, UT, USA) with 11.1 mmol/l D-glucose supplemented with 10%
fetal bovine serum (Hyclone), 100 U/ml penicillin, 100 µg/ml
streptomycin (both from Invitrogen; Thermo Fisher Technology, Inc.,
Waltham, MA, USA), 10 mmol/l HEPES, 2 mmol/l L-glutamine, 1 mmol/l
sodium pyruvate and 50 µmol/l mercaptoethanol, in 5%
CO2 at 37°C.
Oxidative stress model
INS-1 cells were incubated with 0, 50, 100, 150,
250, 300, and 350 µM H2O2 for 15 min
and cell viability was evaluated using the 3-(4,5)-dimethylthiahiazo
(-z-y1)-3,5-di-phenytetrazoliumromide test (Beyotime Institute of
Biotechnology, Beijing, China). INS-1 cell viability decreased in a
dose-dependent manner following H2O2
stimulation. The INS-1 cell vitality was reduced to ~70% with the
stimulation of 250 µM H2O2 for 15 min.
Thus, oxidative stress was induced by treatment with 250 µM
H2O2 for 15 min for the experiments in the
present study.
Insulin secretion stimulated by
H2O2
GSIS was measured in INS-1 cells, which were grown
for 2 days in 96-well plates, balanced in Krebs-Ringer Bicarbonate
Buffer (KRBB) [129 mM NaCl; 4.7 mM KCl; 1.2 mM
KH2PO4; 1.2 mM MgSO4; 2.5 mM
CaCl2; 5 mM NaHCO3; 10 mM HEPES
(Sigma-Aldrich, St. Louis, MO, USA); and 0.1% bovine serum albumin
(Sigma-Aldrich; pH 7.4)] containing 3.3 mM glucose for 1 h, and
were then incubated in 3.3 and 16.7 mM glucose KRBB, respectively,
at 37°C for 2 h.
To determine the effect of
H2O2, INS-1 cells were grown for 48 h and
subsequently incubated under basal conditions or in the presence of
either 10−8 mol/l Ang (1-7) (Sigma-Aldrich),
10−6 mol/l A779 (Sigma-Aldrich) or Ang (1-7) and A779
together, for 2 h. H2O2 at a final
concentration of 250 µM was added in the final 15 min.
Untreated cells served as a control. The cell supernatant was
rapidly removed and rinsed twice with phosphate-buffered saline
(PBS; Hyclone). Insulin secretion was determined at 16.7 mM glucose
KRBB and insulin levels were measured using an insulin
enzyme-linked immunosorbent assay kit (EMD Millipore, Billerica,
MA, USA).
Intracellular Ca2+
measurement
INS-1 cells were loaded with 5 µmol/l
Fluo-3AM (Biotium, Hayward, CA, USA) in a 40-min incubation at 37°C
in 3.3 mmol/l KRBB following pretreatment with Ang (1-7) or A779
for 2 h and then, in the last 15 min, H2O2
was added at a 250-µM concentration. Cellular
Ca2+ signaling was determined with confocal microscopy
(Leica TCS SP5; Leica Microsystems GmbH, Wetzlar, Germany). Images
were collected using 488 nm excitation (em) and the emission (em)
was determined at >505 nm.
ROS determination
INS-1 cells were grown in RPMI-1640 in 6-well plates
for 48 h, followed by incubation with Ang (1-7) or A779 for 2 h,
then a concentration of 250 µM H2O2
was added in the last 15 min. Cells were loaded with 5
µmol/l dihydroethidium (DHE) ROS (Vigorous Biotechnology
Co., Ltd.; Beijing, China) detection and suspended in PBS for 20
min at 37°C in the dark. The cells were rinsed twice in PBS and
collected with 0.05% trypsin (Hyclone; GE Healthcare Life Sciences,
Logan, UT, USA). Following centrifugation at 140 × g for 5 min,
pellets were resuspended in 500 µl PBS. ROS was determined
using intracellular ROS capture DHE with flow cytometry (BD
FACSCalibur; BD Biosciences, Franklin Lakes, NJ, USA). Briefly, an
ex wavelength of 480–535 nm was used to determine em >590–610
nm. Cells were then divided into two subgroups: ROS-negative cells,
which exhibit a very low fluorescence intensity and ROS-positive
cells, which emit red fluorescence. Ten-thousand events per sample
were collected.
MMP
MMP was assessed using JC-1 (Beyotime Institute of
Biotechnology) in INS-1 cells. Cells grown in 6-well plates were
incubated with 1 ml JC-1 (2 mg/ml) for 20 min at 37°C. The cells
were centrifuged at 1,000 × g for 5 min, while the pellets were
resuspended in 500 µl PBS. Carbonyl cyanide
M-chlorophenylhydrazone (CCCP; Beyotime Institute of
Biotechnology), a mitochondrial electron transport chain inhibitor,
served as a positive control. CCCP (10 M) was added to the cells
for 20 min. In total, 10,000 cells from each well were analyzed by
flow cytometry (ex, 490 nm, em, 590 nm). Color change from green to
red indicated an increase in the MMP or the improvement of
mitochondrial function.
Statistical analysis
Statistical analyses were performed using GraphPad
Prism 5 (http://www.graphpad.com/), and data are
expressed as means ± standard error of the mean. One-way analysis
of variance followed by Tukey's or Dunnett's tests were used to
compare all groups or selected groups to the control and P<0.05
was considered to indicate a statistically significant
difference.
Results
Insulin release
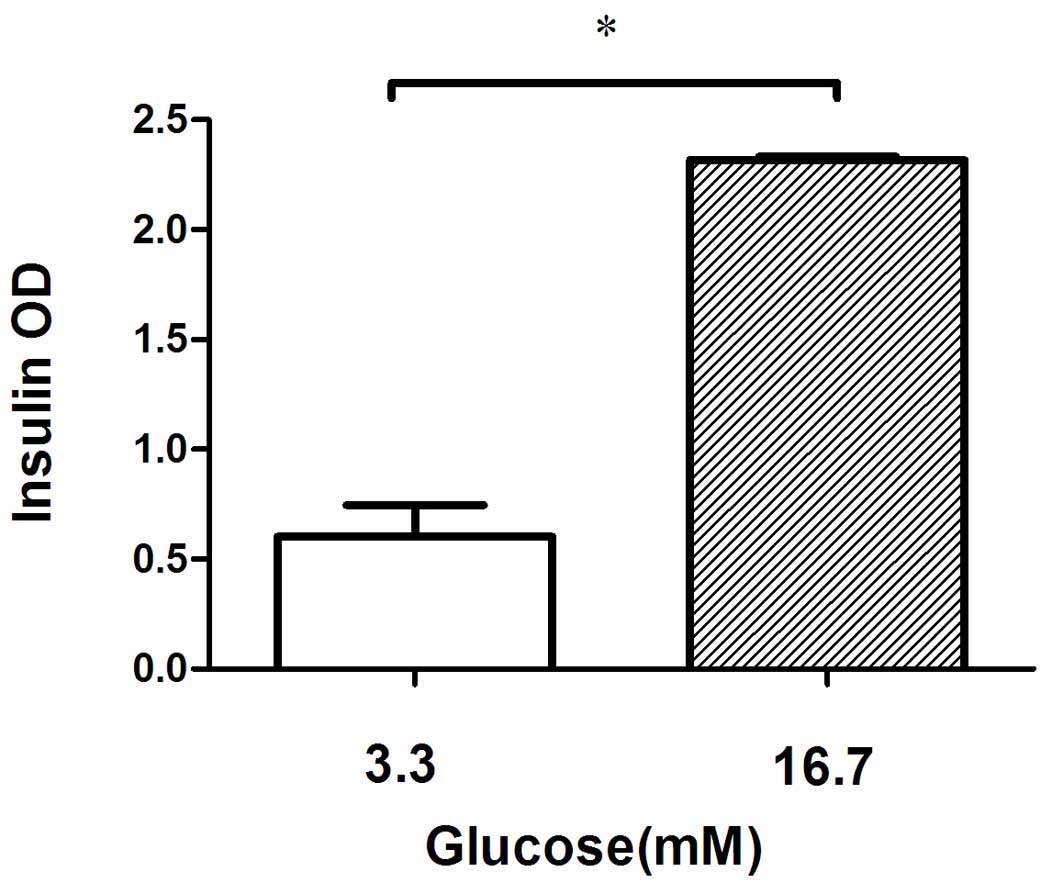
The quantity of insulin released from the INS-1
cells was significantly increased, as expected, when the glucose
concentration in the incubation medium was increased from 3.3 to
16.7 mmol/l (Fig. 1).
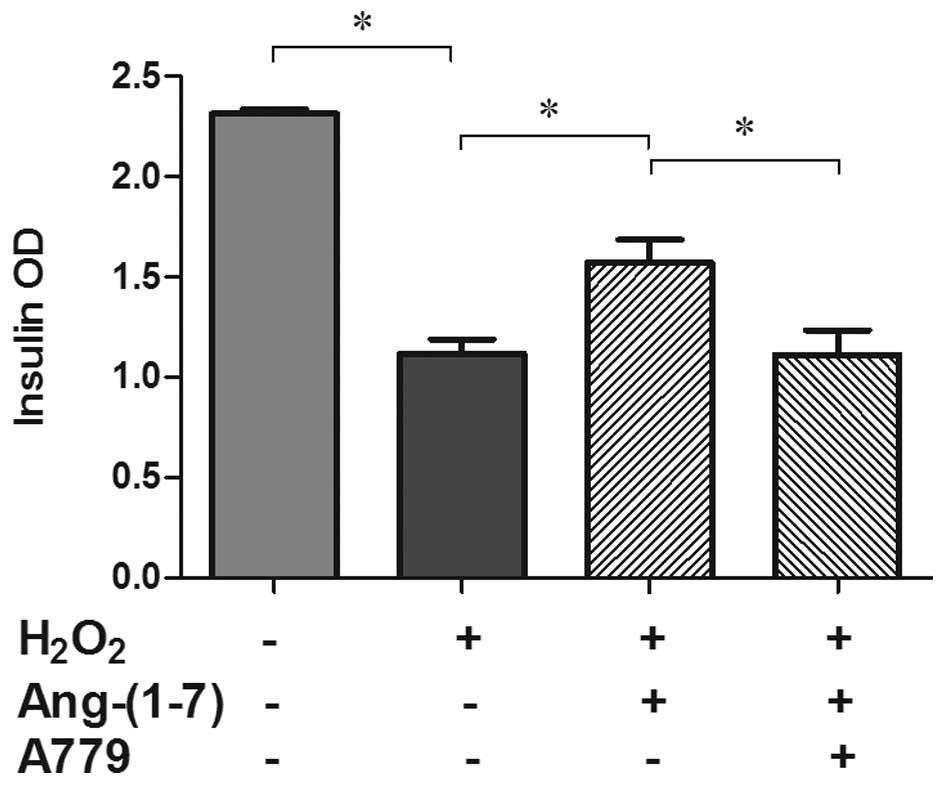
Ang (1-7) restored GSIS in the presence
of H2O2
Groups treated with H2O2
exhibited significantly impaired insulin secretion (51.8%) compared
with the control groups. Pre-treatment with 10−8 mol/l
Ang (1-7) prior to the addition of H2O2 can
restore insulin secretion significantly, although not to basal
levels (26.1%; P<0.05), and its antagonist A779 can inhibit this
restorative effect (P<0. 05; Fig.
2).
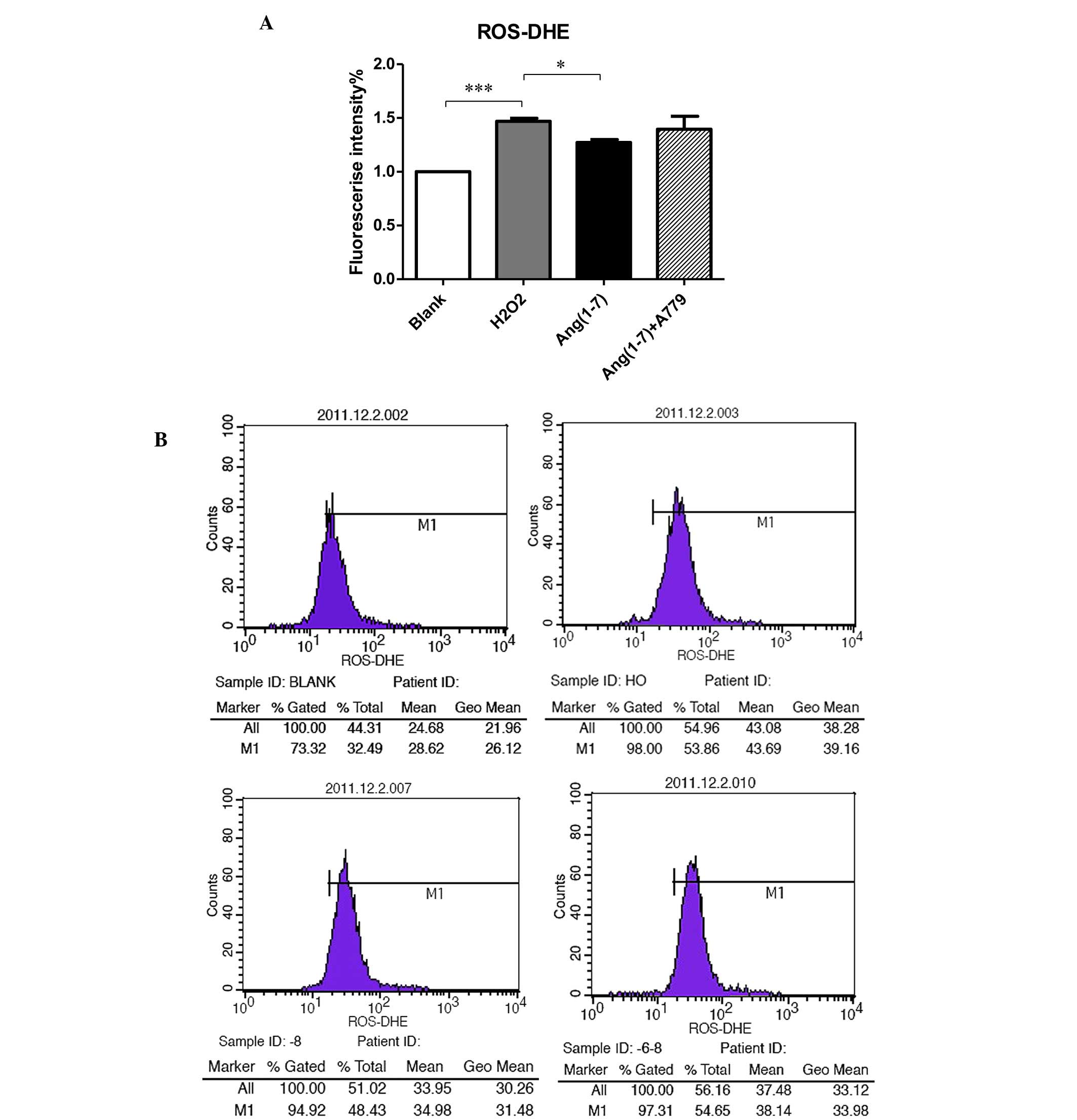
Generation of intracellular ROS
To determine the potential antioxidant role of Ang
(1-7) in pancreatic β cells, INS-1 cells were used to measure the
level of ROS. As shown in Fig. 3,
adding 250 µmol/l H2O2 for 15 min to
the INS-1 cells clearly increased the production of ROS compared
with the control groups at 16.7 mM glucose. Pre-treatment with
10−8 mol/l Ang (1-7) for 2 h prior to adding
H2O2 reduced the level of ROS (P<0.05),
while treatment with 10−8 mol/l for 2 h A779 selectively
inhibited this effect (Fig.
3).
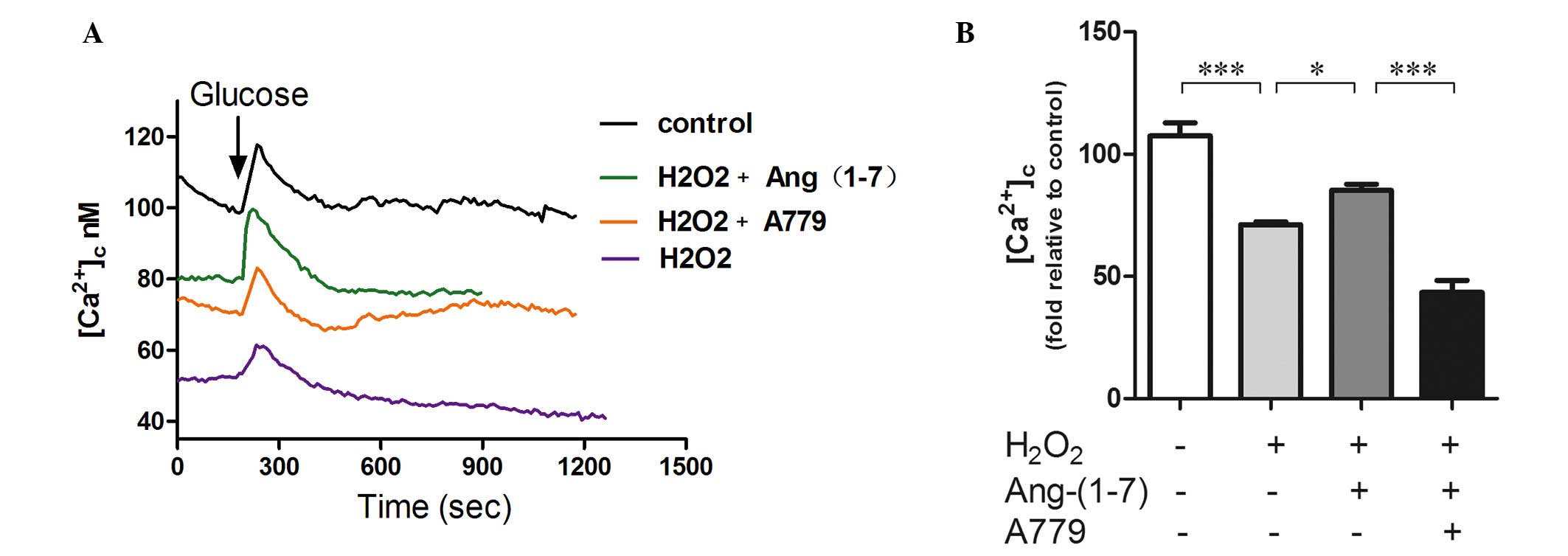
Intracellular Ca2+ imaging of
GSCa
GSCa responses are one of the most commonly used
indexes of β cell function. They can provide real-time results of β
cell function. As shown in Fig. 4,
GSCa signaling in INS-1 cells consists of three phases: Phase 0,
the initial dip below baseline due to calcium uptake by the
endoplasmic reticulum; phase 1, the rapid rise to peak calcium
level concomitant with the release of pre-docked insulin granules;
and phase 2, the elevated plateau. Addition of 250 µmol/l
H2O2 for 15 min to INS-1 cells decreased the
fluorescence intensity compared with the control group.
Pre-treatment with a 10−8 mol/l Ang (1-7) for 2 h prior
to adding H2O2 upregulated calcium
fluorescence by 25%, and A779 can selectively inhibited this
effect. Furthermore, pre-incubation with Ang (1-7) restored the
amplitude of calcium in phase 1 and A779 blocked this effect
(Fig. 4).
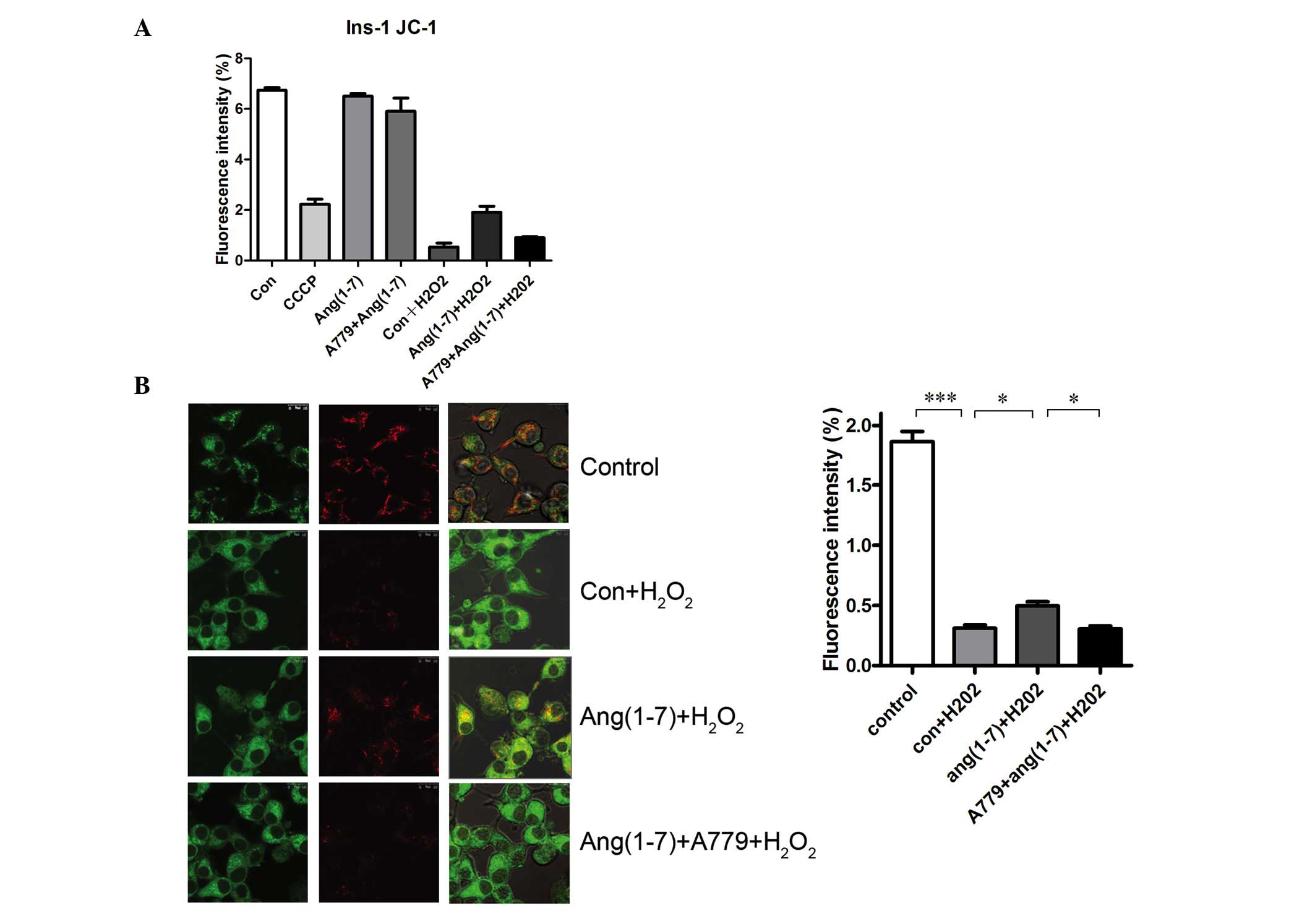
Ang (1-7) restores mitochondrial function
in the presence of H2O2
JC-1 was used to detect the MMP to evaluate the
potential antioxidant effect of Ang (1-7) on mitochondrial function
in INS-1 cells. Analysis of fluorescence intensity by flow
cytometry revealed a significant increase in MMP in Ang
(1-7)-treated INS-1 cells (Fig.
5A), which was inhibited by treatment with A779. Furthermore,
the red fluorescence, which indicates greater MMP, increased
significantly following the addition of Ang (1-7), which was
blocked by A779 treatment, as demonstrated by a significant
increase in green fluorescence (Fig.
5B). As shown in Fig. 5, INS-1
cells treated with 250 µmol/l H2O2 for
15 min exhibited a decrease in the level of MMP caused by CCCP
compared with that in the controls at 16.7 mM glucose.
Pre-treatment with a 10−8 mol/l Ang (1-7) for 2 h prior
to adding H2O2 increased the level of MMP
significantly. Treatment with 10−8 mol/l A779 for 2 h
inhibited this effect.
Discussion
The present study demonstrated that Ang (1-7) can
partially restore insulin secretion from INS-1 cells (which is
reduced by oxidative stress injury) and reduce the level of
intracellular ROS. This protective effect was associated with the
change in cellular calcium signaling and mitochondrial function.
Ang (1-7) can restore early phase calcium signaling and
mitochondrial membrane potential, and has a protective effect on
mitochondrial function; however, Ang-(1-7) protective effects could
be blockaded by its specific inhibitor, A779. To the best of our
knowledge, this is the first study to confirm the antioxidant
effect of Ang (1-7) in INS-1 β cells.
Oxidative stress results in an increase in the
production of ROS and a reduction of the scavenging mechanisms. It
has been well-documented that ROS exhibits an important role in the
development of diabetes. As the end products of oxidative stress, a
certain level of ROS is required for glucose homeostasis (22). However, excess ROS leads to β cell
dysfunction by promoting β cell apoptosis and inactivating genes
involved in insulin synthesis, such as v-maf avian
musculoaponeurotic fibrosarcoma oncogene homolog A and pancreatic
and duodenal homeobox 1 (23). In
addition, hyperactivity of RAS leads to the development of β cell
dysfunction by increasing oxidative stress and fibrosis (3–4). Ang
(1-7) is considered to be an important antagonist of AngII and it
has been shown to be able to reduce oxidative stress in the
kidneys, cardiovascular system and neural system; however, the
effects of Ang (1-7) in pancreatic β cell remains unknown.
We hypothesized that the effects of Ang (1-7) occur
via the same mechanisms in pancreatic β cells. As shown in the
present study, Ang (1-7) reduced the intracellular ROS levels in
INS-1 cells and had a protective effect on β cell function. Bindom
et al (15) found that ACE2
overexpression in the pancreas of diabetic rats improves the
function of β cells. Furthermore, the protective effect can be
blocked by its specific inhibitor A779, which suggested that this
effect was mediated by Ang (1-7) (15) and is consistent with the findings
of the present study. In addition, chronic injection of Ang (1-7)
improves insulin sensitivity in rats with a high-fructose diet
(24), Mas receptor knockout mice
exhibited decreased insulin sensitivity, impaired glucose tolerance
and glucose uptake (25). These
studies demonstrated the protective role of Ang (1-7) in the
development of diabetes and metabolic syndrome. In addition, a
number of studies in other systems supported the idea that the
protective role of Ang (1-7) occurs by reducing oxidative stress.
ACE2 overexpression results in a reduction of ROS formation in the
brain (17). Furthermore,
continuous intravenous infusion of Ang (1-7) restores vasodilation
and protects the myocardium via inhibition of oxidative stress
(24).
In pancreatic β cells, the regulation of
intracellular calcium is crucial to the processes of insulin
secretion (26); thus, analyzing
GSCa responses can provide information regarding the viability and
function of pancreatic β cells. GSCa results can be obtained
rapidly and at a lower cost than GSIS (27). In addition, the calcium curve
directly reflects the changes in insulin secretion within the first
15 min following the addition of glucose. In the present study, it
was observed that the intracellular calcium fluorescence intensity
and the amplitude of insulin secretion in the first phase
significantly decreased following treatment with
H2O2. This result is consistent with the
insulin secretion experiment, which suggests that the reduction of
insulin secretion is correlated with a decrease in intracellular
calcium. Ang (1-7) can restore the calcium fluorescent intensity
and the signaling peak of first phase insulin secretion. Moreover,
A779 can block this effect. This study confirmed that oxidative
stress can cause a decline in intracellular calcium, which results
in the reduction of first phase insulin secretion in pancreatic
cells, and Ang-(1-7) can restore this early β cell dysfunction
associated with calcium levels. Our previous study showed that ACE2
knockout mice exhibited progressive impairments in glucose
tolerance and reduced first-phase insulin secretion (14); thus, in vivo and in
vitro experiments were consistent. These results demonstrated
the importance of the ACE2-Ang (1-7)-Mas axis in the early stages
of diabetes and its protective role in the early treatment of
diabetes, as well as the correlation with Ang (1-7) and oxidative
stress in INS-1 cells.
Islet β cells detect changes in blood glucose and
maintain glucose homeostasis. The mitochondrial energy metabolism
conditions in pancreatic β cells are crucial for the capacity of
sensing blood glucose levels (28). The importance of mitochondria in
type 2 diabetes has been demonstrated by the identification of
causal mutations in the mitochondrial DNA in pancreatic β cells
(29,30). Excessive AngII can increase
mitochondrial ROS production, and reduce the mitochondrial membrane
potential and respiratory control ratio (21). Recent studies have shown that AT1R
blockers can protect the mitochondria in the kidney in a type 1
diabetes mouse model. In the present study, Ang (1-7) restored the
impaired MMP and exhibited protective effects on mitochondrial
function. The protective effect on mitochondrial function is likely
to be one of the mechanisms underlying the antioxidant effect of
Ang (1-7) in pancreatic β cells.
In conclusion, to the best of our knowledge, the
present study was the first to demonstrate the antioxidant effect
of Ang (1-7) in the INS-1 pancreatic cell line and the restorative
effects of Ang (1-7) on insulin secretion. This was associated with
restoration of calcium signaling, reduction of ROS generation and
restoration of the impaired mitochondrial function in oxidative
stress conditions. The effects observed following treatment with
Ang (1-7) were inhibited by its specific antagonist, A779. This
study demonstrated that reducing ROS production and restoring
mitochondrial function are likely to be the mechanisms underlying
the protective effects of Ang (1-7) on pancreatic β cell function
under oxidative stress. Notably, this experiment confirms the
importance of Ang (1-7) in the early stages of diabetes. These
findings may assist with the treatment of diabetes in future,
potentially during the development of novel therapeutic
strategies.
Acknowledgments
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81070644, 30871187
and 30671001).
References
|
1
|
Lau T, Carlsson PO and Leung PS: Evidence
for a local angiotensin-generating system and dose-dependent
inhibition of glucose-stimulated insulin release by angiotensin II
in isolated pancreatic islets. Diabetologia. 47:240–248. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Favre GA, Esnault VL and Van Obberghen E:
Modulation of glucose metabolism by the
renin-angiotensin-aldosterone system. Am J Physiol Endocrinol
Metab. 308:E435–E449. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ko SH, Kwon HS, Kim SR, Moon SD, Ahn YB,
Song KH, Son HS, Cha BY, Lee KW, Son HY, et al: Ramipril treatment
suppresses islet fibrosis in otsuka long-evans tokushima fatty
rats. Biochem Biophys Res Commun. 316:114–122. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakayama M, Inoguchi T, Sonta T, Maeda Y,
Sasaki S, Sawada F, Tsubouchi H, Sonoda N, Kobayashi K, Sumimoto H
and Nawata H: Increased expression of NAD (P)H oxidase in islets of
animal models of Type 2 diabetes and its improvement by an AT1
receptor antagonist. Biochem Biophys Res Commun. 332:927–933. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tikellis C, Wookey PJ, Candido R,
Andrikopoulos S, Thomas MC and Cooper ME: Improved islet morphology
after blockade of the renin-angiotensin system in the ZDF rat.
Diabetes. 53:989–997. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cheng Q, Law PK, de Gasparo M and Leung
PS: Combination of the dipeptidyl peptidase IV inhibitor LAF237
[(S)-1-[(3-hydroxy-1-adamantyl)ammo]acetyl-2-cyanopyrrolidine] with
the angiotensin II type 1 receptor antagonist valsartan
[N-(1-oxopentyl)-N-[[2′-(1H-tetrazol-5-yl)-[1,1′-biphenyl]-4-yl]
methyl]-L-valine] enhances pancreatic islet morphology and function
in a mouse model of type 2 diabetes. J Pharmacol Exp Ther.
327:683–691. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Frantz ED, Crespo-Mascarenhas C,
Barreto-Vianna AR, Aguila MB and Mandarim-de-Lacerda CA:
Renin-angiotensin system blockers protect pancreatic islets against
diet-induced obesity and insulin resistance in mice. PLoS One.
8:e671922013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Braga MF and Leiter LA: Role of
renin-angiotensin system blockade in patients with diabetes
mellitus. Am J Cardiol. 104:835–839. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scheen AJ: Renin-angiotensin system
inhibition prevents type 2 diabetes mellitus. Part 1. A
meta-analysis of randomised clinical trials. Diabetes Metab.
30:487–496. 2004. View Article : Google Scholar
|
|
10
|
Scheen AJ: Renin-angiotensin system
inhibition prevents type 2 diabetes mellitus. Part 2. Overview of
physiological and biochemical mechanisms. Diabetes Metab.
30:498–505. 2004. View Article : Google Scholar
|
|
11
|
Califf RM, Boolell M, Haffner SM, Bethel
M, McMurray J, Duggal A and Holman RR; NAVIGATOR Study Group:
Prevention of diabetes and cardiovascular disease in patients with
impaired glucose tolerance: Rationale and design of the nateglinide
and valsartan in impaired glucose tolerance outcomes research
(NAVIGATOR) Trial. Am Heart J. 156:623–632. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ,
Wu BY, Sun GZ, Yang GR, Zhang XL, Wang L, et al: Plasma glucose
levels and diabetes are independent predictors for mortality and
morbidity in patients with SARS. Diabet Med. 23:623–628. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li W, Moore MJ, Vasilieva N, Sui J, Wong
SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough
TC, et al: Angiotensin-converting enzyme 2 is a functional receptor
for the SARS coronavirus. Nature. 426:450–454. 2003. View Article : Google Scholar
|
|
14
|
Niu MJ, Yang JK, Lin SS, Ji XJ and Guo LM:
Loss of angiotensin-converting enzyme 2 leads to impaired glucose
homeostasis in mice. Endocrine. 34:56–61. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bindom SM, Hans CP, Xia H, Boulares AH and
Lazartigues E: Angiotensin I-converting enzyme type 2 (ACE2) gene
therapy improves glycemic control in diabetic mice. Diabetes.
59:2540–2548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Benter IF, Yousif MH, Cojocel C,
Al-Maghrebi M and Diz DI: Angiotensin-1-7 prevents diabetes-induced
cardiovascular dysfunction. Am J Physiol Heart Circ Physiol.
292:H666–H672. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xia H, Suda S, Bindom S, Feng Y, Gurley
SB, Seth D, Navar LG and Lazartigues E: ACE2-mediated reduction of
oxidative stress in the central nervous system is associated with
improvement of autonomic function. PLoS One. 6:e226822011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dhaunsi GS, Yousif MH, Akhtar S, Chappell
MC, Diz DI and Benter IF: Angiotensin-1-7 prevents diabetes-induced
attenuation in PPAR-gamma and catalase activities. Eur J Pharmacol.
638:108–114. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xue B, Zhang Z, Beltz TG, Guo F, Hay M and
Johnson AK: Estrogen regulation of the brain renin-angiotensin
system in protection against angiotensin II-induced sensitization
of hypertension. Am J Physiol Heart Circ Physiol. 307:H191–H198.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Drews G, Krippeit-Drews P and Düfer M:
Oxidative stress and beta-cell dysfunction. Pflugers Arch.
460:703–718. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dikalov SI and Nazarewicz RR: Angiotensin
II-induced production of mitochondrial reactive oxygen species:
Potential mechanisms and relevance for cardiovascular disease.
Antioxid Redox Signal. 19:1085–1094. 2013. View Article : Google Scholar :
|
|
22
|
Pi J, Bai Y, Zhang Q, Wong V, Floering LM,
Daniel K, Reece JM, Deeney JT, Andersen ME, Corkey BE and Collins
S: Reactive oxygen species as a signal in glucose-stimulated
insulin secretion. Diabetes. 56:1783–1791. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Robertson RP: Chronic oxidative stress as
a central mechanism for glucose toxicity in pancreatic islet beta
cells in diabetes. J Biol Chem. 279:42351–42354. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Giani JF, Mayer MA, Muñoz MC, Silberman
EA, Höcht C, Taira CA, Gironacci MM, Turyn D and Dominici FP:
Chronic infusion of angiotensin-1-7 improves insulin resistance and
hypertension induced by a high-fructose diet in rats. Am J Physiol
Endocrinol Metab. 296:E262–E271. 2009. View Article : Google Scholar
|
|
25
|
Santos SH, Fernandes LR, Mario EG,
Ferreira AV, Pôrto LC, Alvarez-Leite JI, Botion LM, Bader M,
Alenina N and Santos RA: Mas deficiency in FVB/N mice produces
marked changes in lipid and glycemic metabolism. Diabetes.
57:340–347. 2008. View Article : Google Scholar
|
|
26
|
Satin LS: Localized calcium influx in
pancreatic beta-cells: Its significance for
Ca2+-dependent insulin secretion from the islets of
Langerhans. Endocrine. 13:251–262. 2000. View Article : Google Scholar
|
|
27
|
Carter JD, Dula SB, Corbin KL, Wu R and
Nunemaker CS: A practical guide to rodent islet isolation and
assessment. Biol Proced Online. 11:3–31. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Matschinsky FM, Magnuson MA, Zelent D,
Jetton TL, Doliba N, Han Y, Taub R and Grimsby J: The network of
glucokinase-expressing cells in glucose homeostasis and the
potential of glucokinase activators for diabetes therapy. Diabetes.
55:1–12. 2006. View Article : Google Scholar
|
|
29
|
Silva JP, Köhler M, Graff C, Oldfors A,
Magnuson MA, Berggren PO and Larsson NG: Impaired insulin secretion
and beta-cell loss in tissue-specific knockout mice with
mitochondrial diabetes. Nat Genet. 26:336–340. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Maassen JA, 'T Hart LM, Van Essen E, Heine
RJ, Nijpels G, Jahangir Tafrechi RS, Raap AK, Janssen GM and Lemkes
HH: Mitochondrial diabetes: Molecular mechanisms and clinical
presentation. Diabetes. 53(Suppl 1): S103–S109. 2004. View Article : Google Scholar : PubMed/NCBI
|