Introduction
Diabetic nephropathy (DN) is one of the most
frequent microvascular complications in patients with diabetes and
often leads to end-stage renal disease (1). Albuminuria is a common clinical
manifestation of DN and may be associated with kidney disease and
its progression (2). Routine
therapeutic agents such as angiotensin II receptor blockers and
angiotensin-converting enzyme inhibitors reduce urine protein
levels and confer limited benefits for the renal function of
patients with DN (3,4). However, these therapeutic agents are
not sufficient for the prevention of kidney damage. Therefore, it
is imperative to identify novel therapeutic targets for DN.
Podocytes are specialized epithelial cells, which
are key glomerular endothelial cells and form a major component of
the glomerular filtration barrier. Structural and functional
alterations in these cells are crucial for the development of
albuminuria (5).
Epithelial-mesenchymal transition (EMT) is a biological
characteristic of epithelial cells under physiological and
pathological conditions, which is important during DN. Podocytes
undergoing EMT lose the phenotypic characteristics of epithelial
cells, including reduced P-cadherin, nephrin and podocin expression
levels and express phenotypic markers of mesenchymal cells,
including α-smooth muscle actin (α-SMA) and fibronectin (6). However, the mechanisms underlying the
EMT of podocytes under high glucose (HG) conditions remain to be
elucidated.
Glycogen synthase kinase-3β (GSK-3β), a serine
(Ser)/threonine (Thr) kinase, is ubiquitously expressed in
eukaryotic cells and is hypothesized to act on signal transduction
proteins, structural proteins and transcription factors to regulate
cell differentiation, proliferation and apoptosis (7). GSK-3β has two phosphorylation sites,
one is a Ser9 inhibition site and the other a tyrosine (Tyr)216
activation site (8). GSK-3β is
also suggested to participate in the Wnt/β-catenin pathway, which
is important for podocyte EMT (9).
The objective of the present study was to
investigate the function of GSK-3β in podocyte EMT and barrier
dysfunction under HG conditions in order to identify a novel
therapeutic target for DN. Podocytes were transfected with
GSK-3β small interfering RNA (siRNA) or treated with lithium
chloride (LiCl), a selective inhibitor of GSK-3β (7,10),
to inhibit the GSK-3β expression and activity. The alterations in
the phenotypic characteristics and barrier function of podocytes
following treatment were observed. The results of the present study
indicate that GSK-3β is required for HG-induced EMT and barrier
dysfunction in podocytes, implying GSK-3β is a novel potentially
therapeutic target for the treatment of DN.
Materials and methods
Podocyte cell culture and
transfection
Conditionally immortalized mouse podocytes were
provided by Professor Nie Jing (Southern Medical University,
Guangzhou, China). Undifferentiated podocytes were cultured and
differentiated in Roswell Park Memorial Institute (RPMI) 1640
medium (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA)
containing 10% fetal bovine serum (FBS; Gibco; Thermo Fisher
Scientific, Inc.), 5.6 mM glucose (Dingguo Changsheng Biotechnology
Co., Ltd., Beijing, China) and 10 U/ml recombinant mouse
interferon-γ (Shanghai Sangon Biotech Co., Ltd., Shanghai, China),
in an incubator at 33°C in 5% CO2. Following differentiation,
podocytes were cultured at 37°C in RPMI 1640 medium without
recombinant mouse interferon-γ. They were cultured for 12–14 days
with the medium replaced every 1–2 days until they were mature and
differentiated.
Matured and differentiated podocytes were seeded
onto 6-well or Transwell plates. When 80–90% confluence was
reached, podocytes were supplied with serum-free RPMI 1640 medium
for another 6–8 h for synchronization. Thereafter, cells were
treated as follows: i) Normal glucose (NG, 5.6 mM glucose); ii) HG
(12.5 HG, 12.5 mM; 25 HG, 25 mM; and 50 HG, 50 mM glucose); and
iii) mannitol as an osmotic control [NG + M, 5.6 mM glucose and
44.4 mM mannitol (Dingguo Changsheng Biotechnology Co., Ltd.),
which has an osmotic pressure comparable with the 25 HG group].
Podocytes were also transfected with a siRNA, sequence:
5′-CCACTCAAGAACTGTCAAGTA-3′ (GeneChem Co., Ltd., Shanghai, China)
against GSK-3β based on the GSK-3β full-length mouse gene
(GenBank accession number: NM-019827.6) or a scrambled siRNA
(5′-UUCUCCGAACGUGUCACGUTT-3′; GeneChem Co., Ltd.) when treated NG
or HG (25 mM). Podocytes were transfected with 30 nM GSK-3β
siRNA for 36 h using Lipofectamine 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.) transfection reagent according to the
manufacturer's protocol (11).
Podocytes were grouped in the following treatments: i) NG; ii) NG +
GSK-3β scrambled siRNA; iii) NG + GSK-3β siRNA; iv)
HG (25 mM glucose); v) HG + GSK-3β scrambled siRNA; and vi)
HG + GSK-3β siRNA. Additionally, podocytes were treated with
water-soluble LiCl (Dingguo Changsheng Biotechnology Co., Ltd.) at
a final concentration of 10 mM under NG and HG conditions.
Podocytes were grouped as follows: i) NG (NG, 5.6 mM glucose); ii)
NG + LiCl (10 mM); iii) HG; and iv) HG + LiCl (10 mM). After 36 h
the podocytes were collected by centrifugation at 13,400 g for 5
min at room temperature in order to be used for various assays.
Immunoblotting
Immunoblotting was performed as previously described
(12). The primary antibodies used
were as follows: β-actin (cat. no. TA-09; 1:1,000; OriGene
Technologies, Inc., Beijing, China), nephrin(cat. no. ab58968;
1:1,000), podocin (cat. no. ab50993; 1:1,000), α-SMA (cat. no.
ab7817; 1:2,000), fibronectin (cat. no. ab2413; 1:2,000), GSK-3β
(cat. no. ab32391; 1:2,000), phosphorylated (p)-Tyr216-GSK-3β (cat.
no. ab75745; 1:2,000; Abcam, Cambridge, UK), p-Ser9-GSK-3β (cat.
no. 5558, 1:1,000; Cell Signaling Technology, Inc., Boston, USA).
Membranes were incubated with primary antibodies at 4°C overnight.
Subsequently, the membranes were washed phosphate-buffered saline
Tween-20 and the alkaline phosphatase-conjugated secondary antibody
(cat. no. IA-0082; 1:2,000; Dingguo Changsheng Biotechnology Co.,
Ltd.) was incubated at 37°C for 2 h. The blots were developed using
a 5-bromo-4-chloro-3-indolyl phosphate/nitro blue tetrazolium color
development kit (Boster Biological Technology, Ltd., Wuhan, China).
ImageJ version 2.1.4.7 software (National Institutes of Health,
Bethesda, MD, USA) was used for quantitative analysis of the
relative grayscale intensity of each protein expression band.
Indirect immunofluorescence
staining
Immunofluorescence staining was performed as
previously described (13). Mature
and differentiated podocytes seeded on coverslips were
serum-starved for 8 h, subsequently, graded concentrations of
glucose were added (12.5 HG, 12.5 mM; 25 HG, 25 mM; and 50 HG, 50
mM glucose). Following 24 h exposure to the different HG
concentrations, the cells were fixed in 4% paraformaldehyde, then
incubated with the primary antibodies for nephrin, podocin, α-SMA
and fibronectin. The cells were then exposed to the Alexa Fluor 488
secondary antibody (Invitrogen; Thermo Fisher Scientific, Inc.).
The coverslips were mounted with antifade mounting medium (Beyotime
Institute of Biotechnology, Shanghai, China) and then were observed
and photographed using an inverted fluorescence microscope (Olympus
Corporation, Tokyo, Japan). The immunofluorescence intensity was
measured with Image J software. The expression levels of nephrin,
podocin, α-SMA and fibronectin were calculated as the
immunofluorescence intensity normalized to that of nephrin under NG
conditions.
Detection of monolayer barrier
function in podocytes
Podocyte monolayer barrier function was measured
using the surrogate measure, podocyte permeability. A modification
of a previously described protocol (14) was adopted for the assessment of
podocyte permeability, where albumin influx was used as an
indicator (14). Differentiated
podocytes at a density of 4×105 cells/well were plated onto 12-well
Transwell plates (3 µm pore; Corning, Corning, NY, USA) and were
serum-starved overnight. Upon reaching 70–80% confluence, the cells
were exposed to different concentrations of glucose (NG; HG, 12.5
mM; HG, 25 mM and HG, 50 mM). The cells were then washed twice with
phosphate-buffered saline supplemented with magnesium chloride and
calcium chloride (both 1 mM). The upper compartment was refilled
with 0.25 ml RPMI 1640 medium and the lower compartment was
refilled with 0.5 ml RPMI 1640 supplemented with 40 mg/ml FBS.
Next, the cells were incubated at 37°C for 2 h. The total albumin
influx was determined by quantifying the concentration in the upper
compartment using a bicinchoninic acid protein assay kit (Dingguo
Changsheng Biotechnology Co., Ltd.).
Detection of GSK-3β activity
This assay was conducted using a GSK-3β activity
assay kit (Genmed Scientifics USA, Inc., Shanghai, China) according
to the manufacturer's protocol. The optical density of each
treatment group was detected using a Nanodrop 2000
spectrophotometer at 280 nm (Thermo Fisher Scientific, Inc.) and
GSK-3β activity was calculated in accordance with the formula
provided by the manufacturer of the kit.
Statistical analysis
Statistical analysis was performed using SPSS
software, version 17.0 (SPSS, Inc., Chicago, IL, USA). Data are
presented as the arithmetic mean ± standard error. Differences
between groups were evaluated using one-way analysis of variance
followed by a Student-Newman-Keuls post-hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Phenotypic conversion of podocytes
exposed to HG conditions
To verify the trans-differentiation of podocytes
into mesenchymal cells during HG conditions, podocytes were
cultured for 36 h with different concentrations of glucose. Western
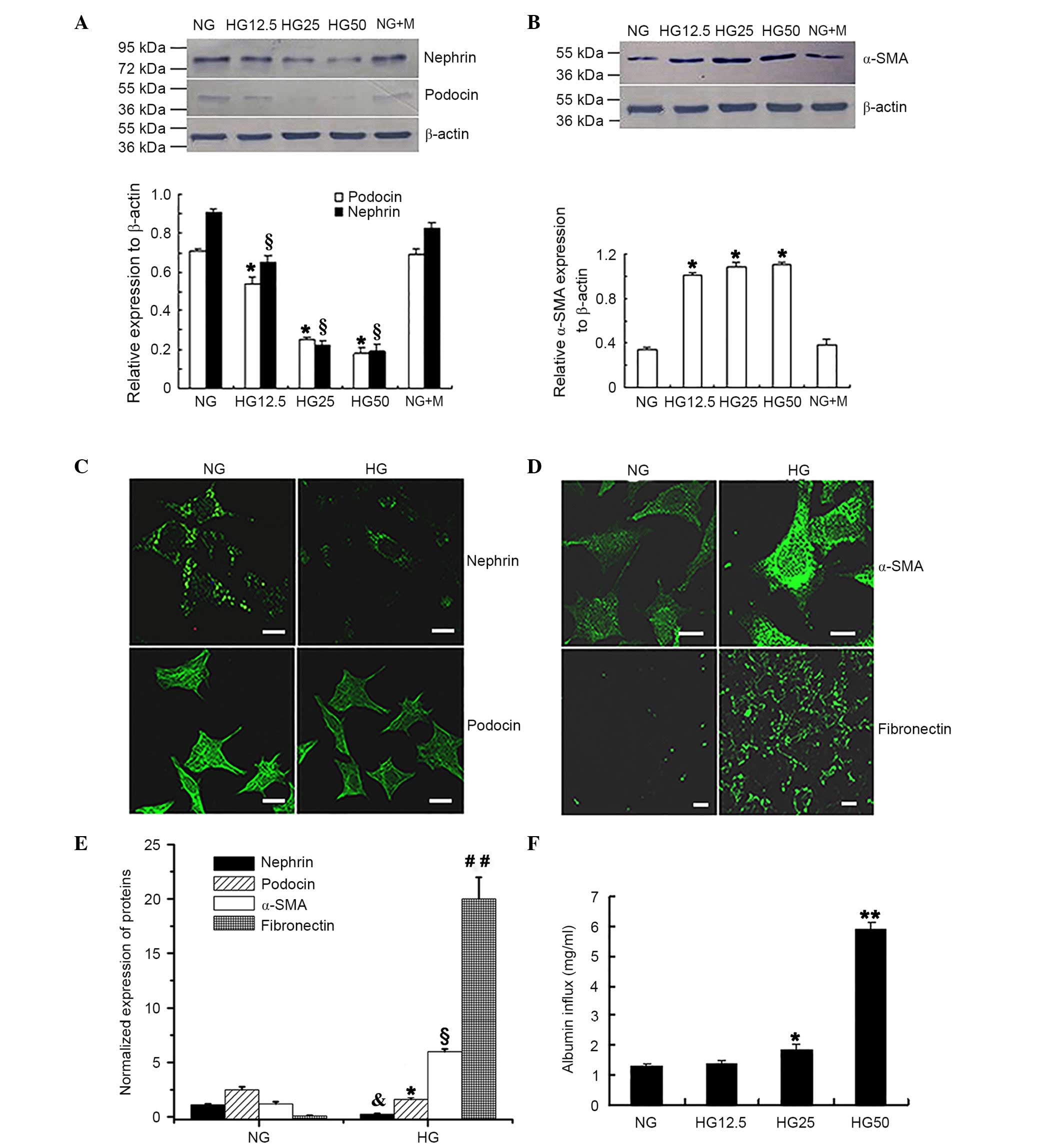
blot analysis (Fig. 1A and B)
determined that the expression levels of the epithelial cell
markers nephrin and podocin were significantly reduced when exposed
to increased HG concentrations when compared with the NG control
group (P<0.05; Fig. 1A). By
contrast, expression of the myofibroblast cell marker α-SMA was
significantly increased in cells treated with increased HG
concentrations compared with the NG control group (P<0.05;
Fig. 1B). No significant
difference was observed between the NG and the NG + M groups for
all of the epithelial cell markers investigated.
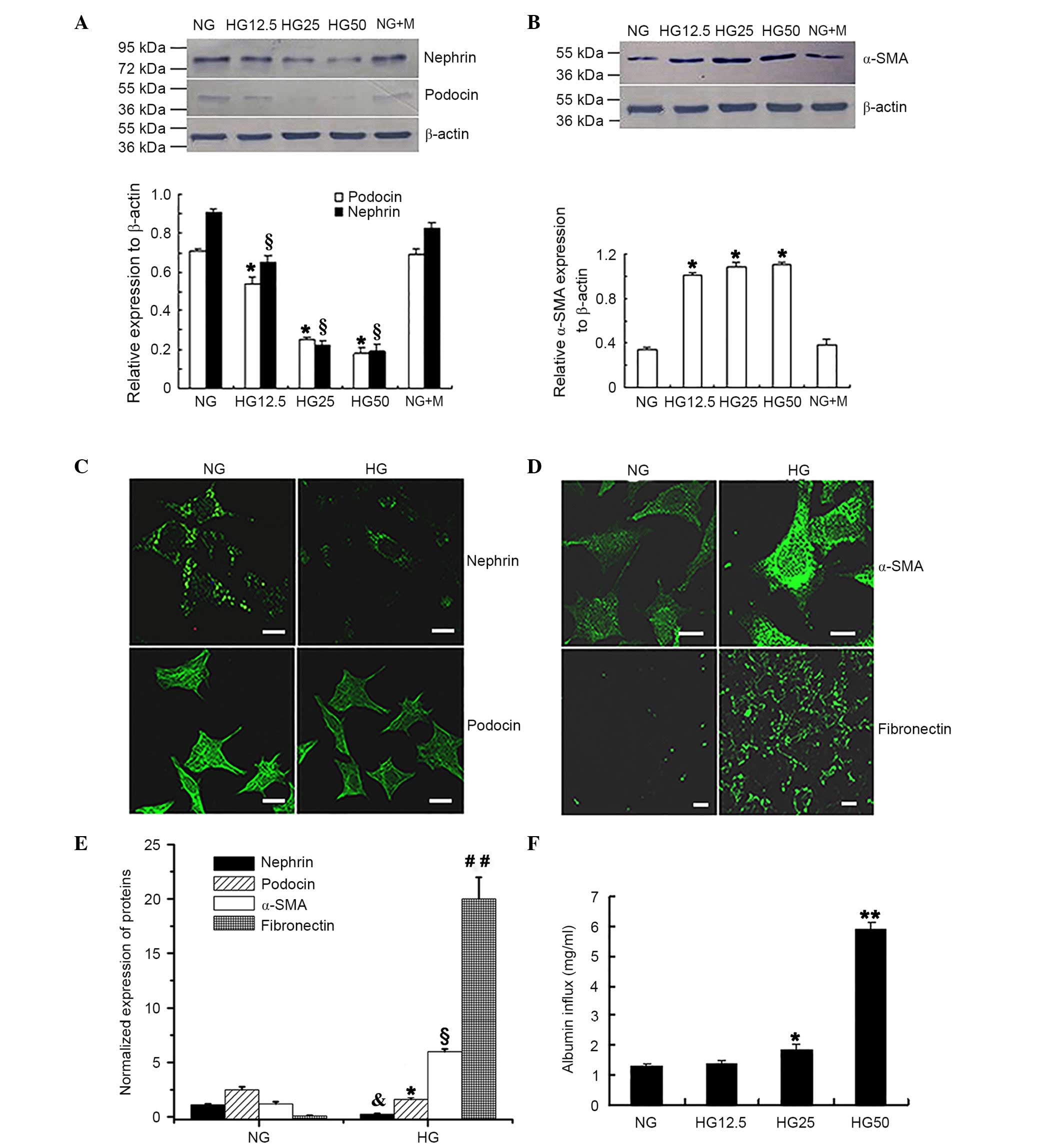 | Figure 1.HG-induced phenotypic conversion and
barrier dysfunction of podocytes. Western blot analysis determined
that the protein expression levels of (A) nephrin and podocin were
significantly reduced in the HG group.*P<0.05 vs. podocin
expression in NG group, §P<0.05 vs. nephrin
expression in NG group; n=4. (B) Protein expression of α-SMA was
increased with increased glucose concentrations. *P<0.05 vs. NG
group; n=4. Immunofluorescence staining presented reduced
expression levels of (C) nephrin and podocin in cells treated with
HG. (D) Increased expression of α-SMA and fibronectin was
identified in the HG group compared with the NG group. Fluorescence
indicated the protein expression of the relevant proteins. Scale
bar, 20 µm. (E) Protein expression levels of nephrin, podocin,
α-SMA and fibronectin from the immunofluorescence intensity
normalized to that of nephrin in the NG group. *P<0.05 vs.
podocin expression in the NG group, &P<0.05 vs.
nephrin expression in the NG group, §P<0.05 vs. α-SMA
expression in NG group, ##P<0.01 vs. fibronectin
expression in NG group; n=4. (F) Monolayer permeability of
differentiated and mature podocytes under HG conditions.
Quantitative analysis determined that HG increased albumin inflow
compared with NG treatment. *P<0.05 vs. NG group; **P<0.01
vs. NG group; n=4. HG, high glucose; NG, normal glucose; α-SMA,
α-smooth muscle actin; NG + M, NG + mannitol. |
Immunofluorescence analysis (Fig. 1C-E) of podocytes following exposure
to 25 mM D-glucose for 36 h revealed significantly reduced nephrin
and podocin expression (P<0.05; Fig. 1C and E); however, α-SMA and
fibronectin expression levels were significantly increased
(P<0.05; Fig. 1D and E)
compared with that observed in the NG control group.
Monolayer barrier dysfunction of
podocytes exposed to HG conditions
The Transwell chamber assay was conducted to
determine whether HG treatment resulted in barrier dysfunction in
podocytes. Fig. 1F indicated that
there was a significantly increased albumin inflow in the presence
of 25 mM D-glucose compared with that in the NG control group (5.6
mM D-glucose) group (P<0.05). In addition, increased albumin
inflow was observed in the 50 mM HG group compared with the 12.5 mM
HG group (P<0.01; Fig. 1F).
These observations suggested that monolayer barrier dysfunction
occurs in podocytes following HG treatment.
HG-induced GSK-3β expression and
activity in podocytes
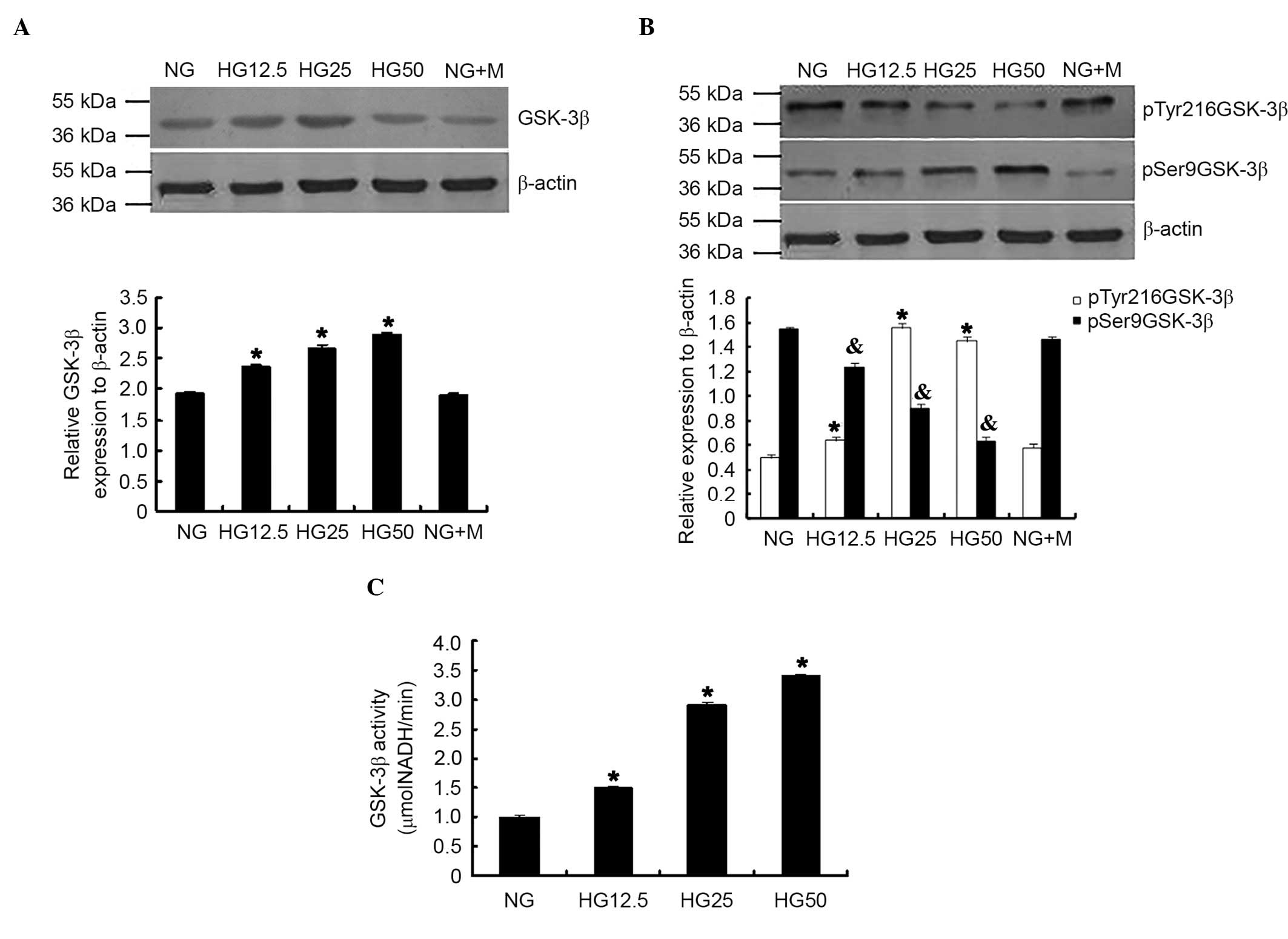
GSK-3β expression, phosphorylation levels and
activity were evaluated in podocytes. Increased HG concentrations
significantly induced total GSK-3β expression (P<0.05; Fig. 2A) and pTry216-GSK-3β; however,
reduced p-Ser9GSK-3β expression was observed with increased HG
concentrations (P<0.05; Fig.
2B). GSK-3β activity was significantly increased when compared
with the NG control group (P<0.05; Fig. 2C).
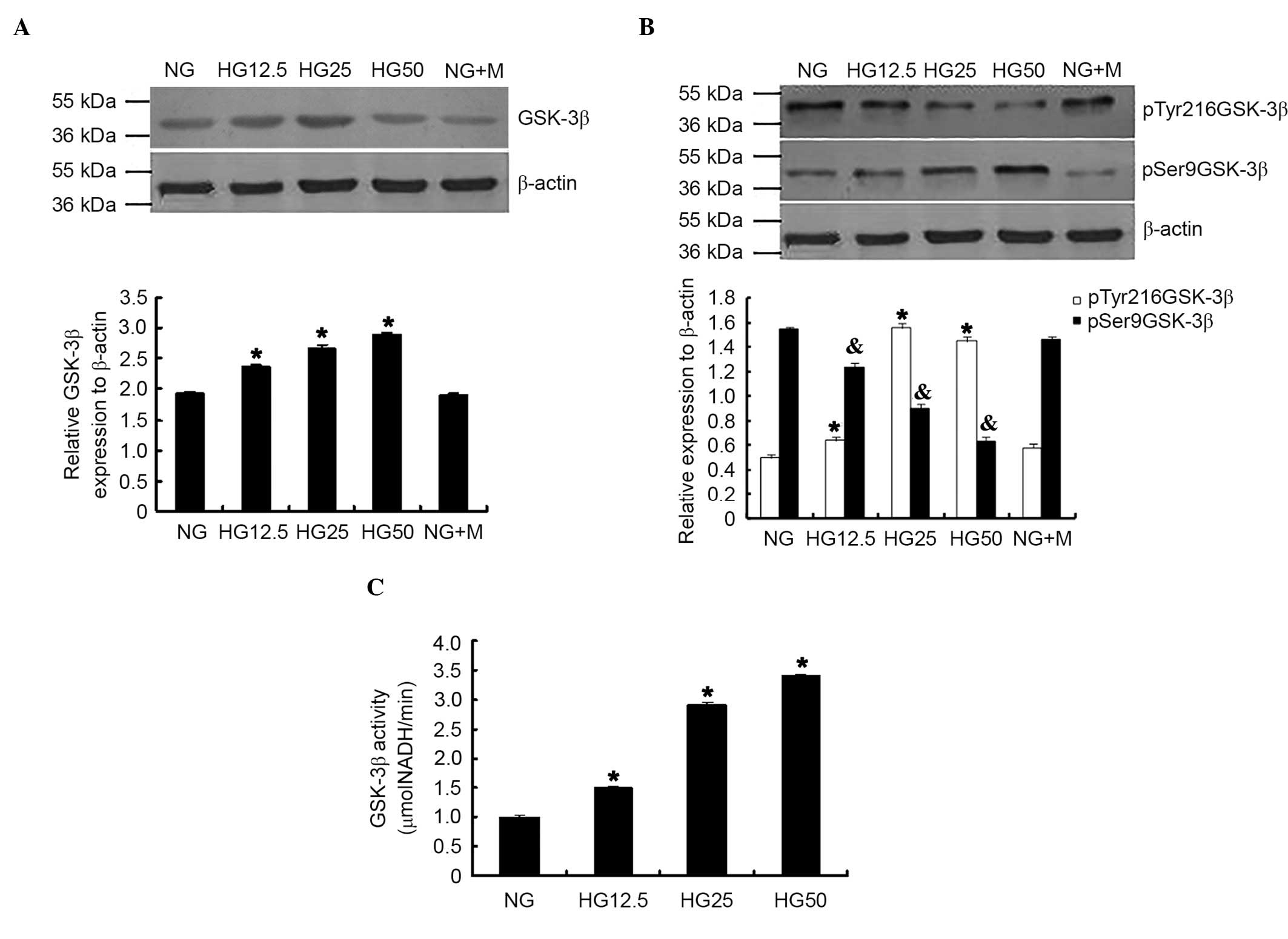 | Figure 2.HG conditions increased GSK-3β
expression, phosphorylation and activity in podocytes. (A) GSK-3β
expression, (B) phosphorylation and (C) activity were significantly
increased in the HG group compared with NG group. *P<0.05 vs. NG
group; n=3. p-Try216-GSK-3β expression was significantly increased;
however, p-Ser9-GSK-3β expression was reduced in the HG group.
*P<0.05 vs. p-Try216-GSK-3β expression in NG group.
&P<0.05 vs. p-Ser9-GSK-3β expression in NG group;
n=3. HG, high glucose; GSK-3β, glycogen synthase kinase-3β; NG,
normal glucose; p, phosphorylated; Tyr, tyrosine; Ser, serine; NG +
M, NG + mannitol; NADH, nicotinamide adenine dinucleotide. |
GSK-3β siRNA reversed podocyte EMT and
monolayer barrier dysfunction under HG conditions
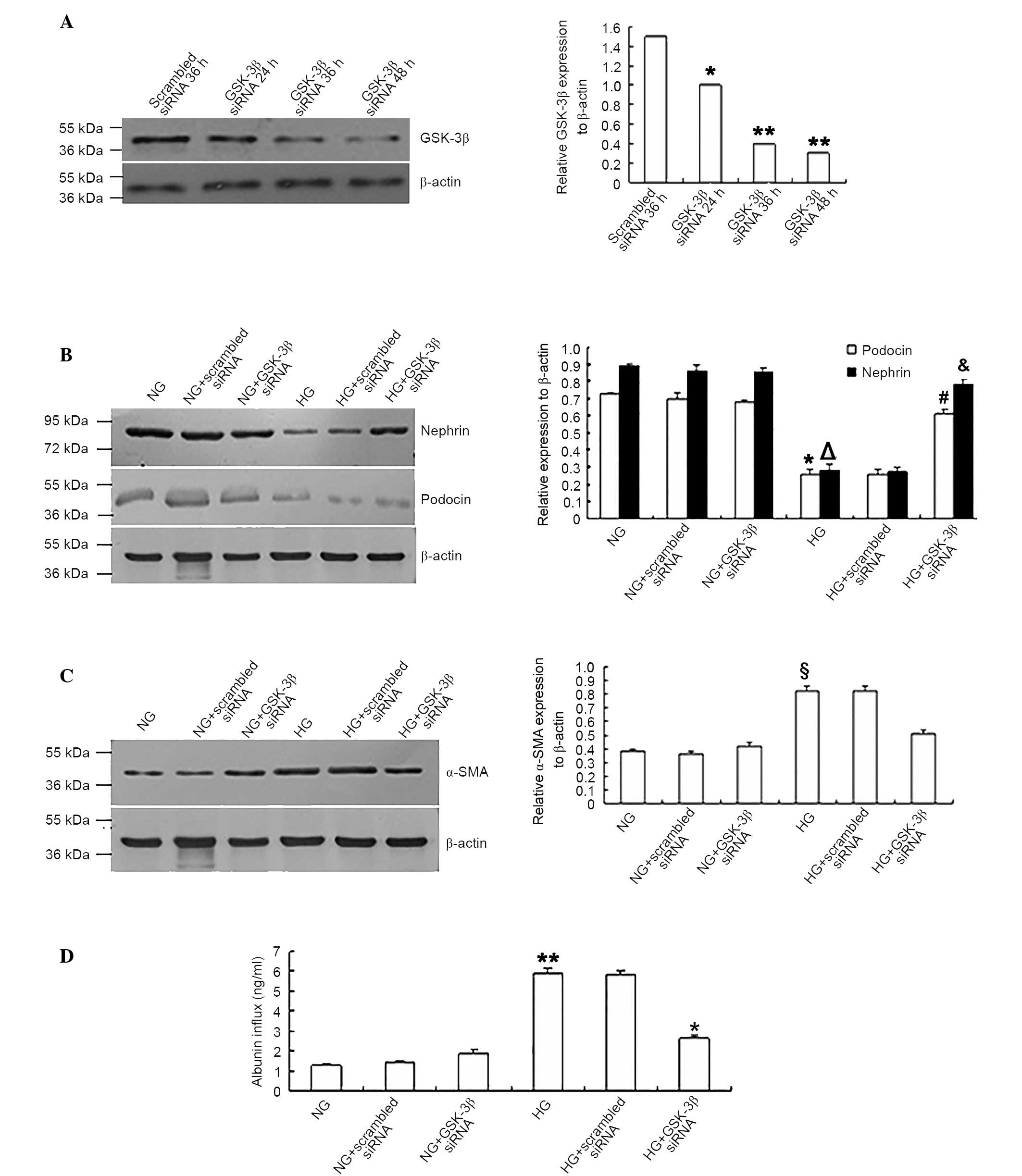
To confirm whether GSK-3β participated in the
trans-differentiation and barrier dysfunction of podocytes during
HG conditions, the cells were transfected with GSK-3β or
scrambled siRNA. Western blotting in Fig. 3A demonstrated that siRNA-mediated
inhibition of the expression of GSK-3β had occurred. When
GSK-3β siRNA-transfected podocytes were exposed to HG (25
mM), the expression levels of nephrin and podocin were
significantly increased compared with the scrambled siRNA control
group (P<0.05; Fig. 3B). The
expression levels of the mesenchymal protein α-SMA were
significantly reduced (P<0.05; Fig.
3C) compared with those transfected with scrambled siRNA. In
addition, the albumin inflow was significantly reduced in
GSK-3β siRNA-transfected podocytes compared with scrambled
siRNA-transfected group (P<0.05; Fig. 3D), indicating that the monolayer
barrier function of podocytes was improved.
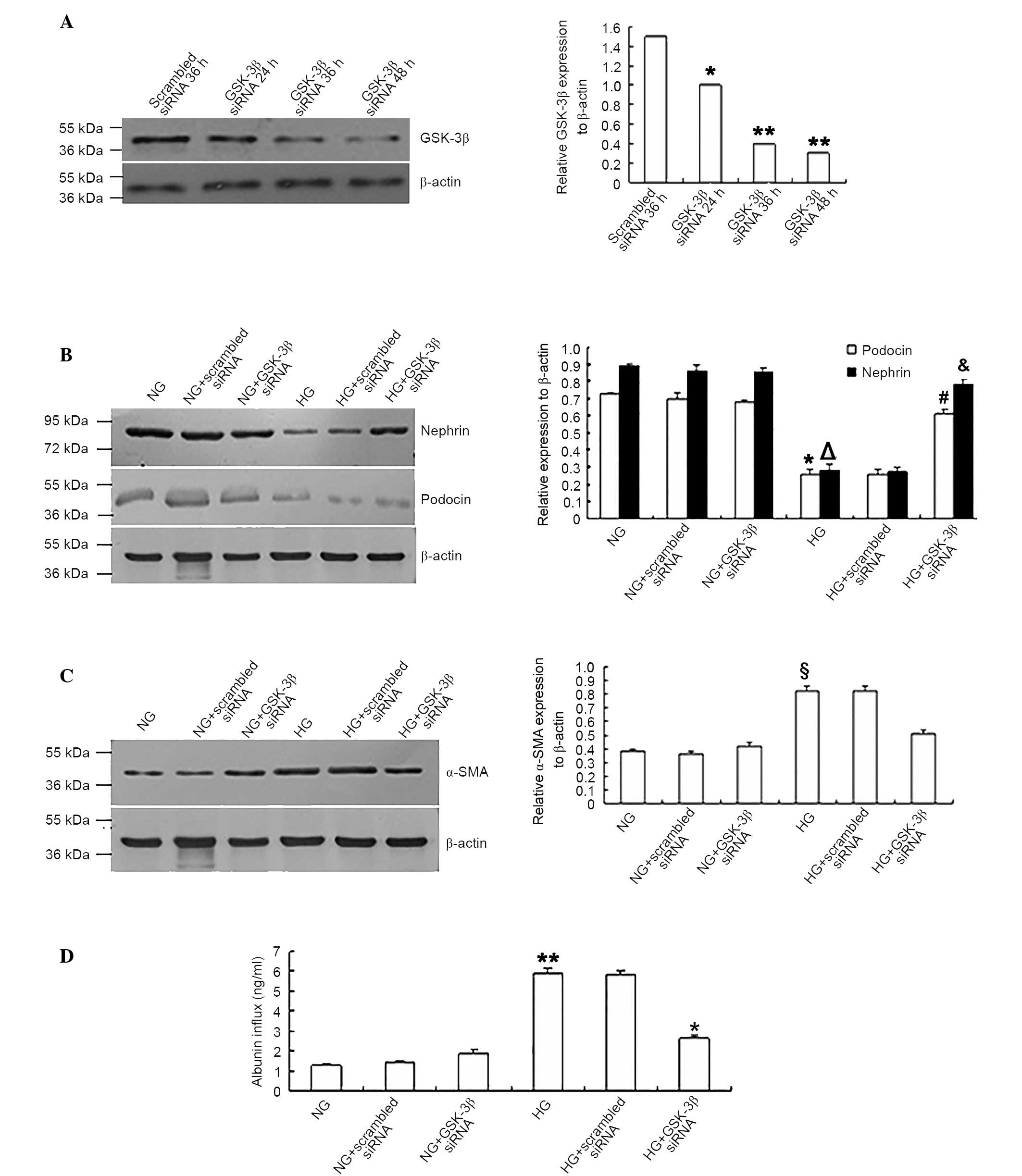 | Figure 3.GSK-3β siRNA reversed the
podocyte epithelial-mesenchymal transition and monolayer barrier
dysfunction under HG conditions. (A) GSK-3β siRNA suppressed
the expression of GSK-3β in podocytes. *P<0.05 vs. scrambled
siRNA 36 h group. **P<0.05 vs. scrambled siRNA 36 h group; n=4).
Podocytes transfected with GSK-3β siRNA expressed higher
levels of (B) nephrin and podocin (*P<0.05 vs. podocin
expression in NG group, §P<0.05 vs. nephrin
expression in NG group, #P<0.05 vs. podocin
expression in HG group, &P<0.05 vs. nephrin
expression in HG group), lower levels of (C) α-SMA
(§P<0.05 vs. α-SMA expression in NG group, *P<0.05
vs. α-SMA expression in HG group) and (D) reduced the albumin
inflow of podocytes under HG conditions compared with podocytes
transfected with scrambled siRNA and the NG group. **P<0.05 vs.
NG group, *P<0.05 vs. HG group; n=4. GSK-3β, glycogen synthase
kinase-3β; siRNA, small interfering RNA; HG, high glucose; NG,
normal glucose; α-SMA, α-smooth muscle actin. |
LiCl reversed podocyte EMT and
monolayer barrier dysfunction under HG conditions
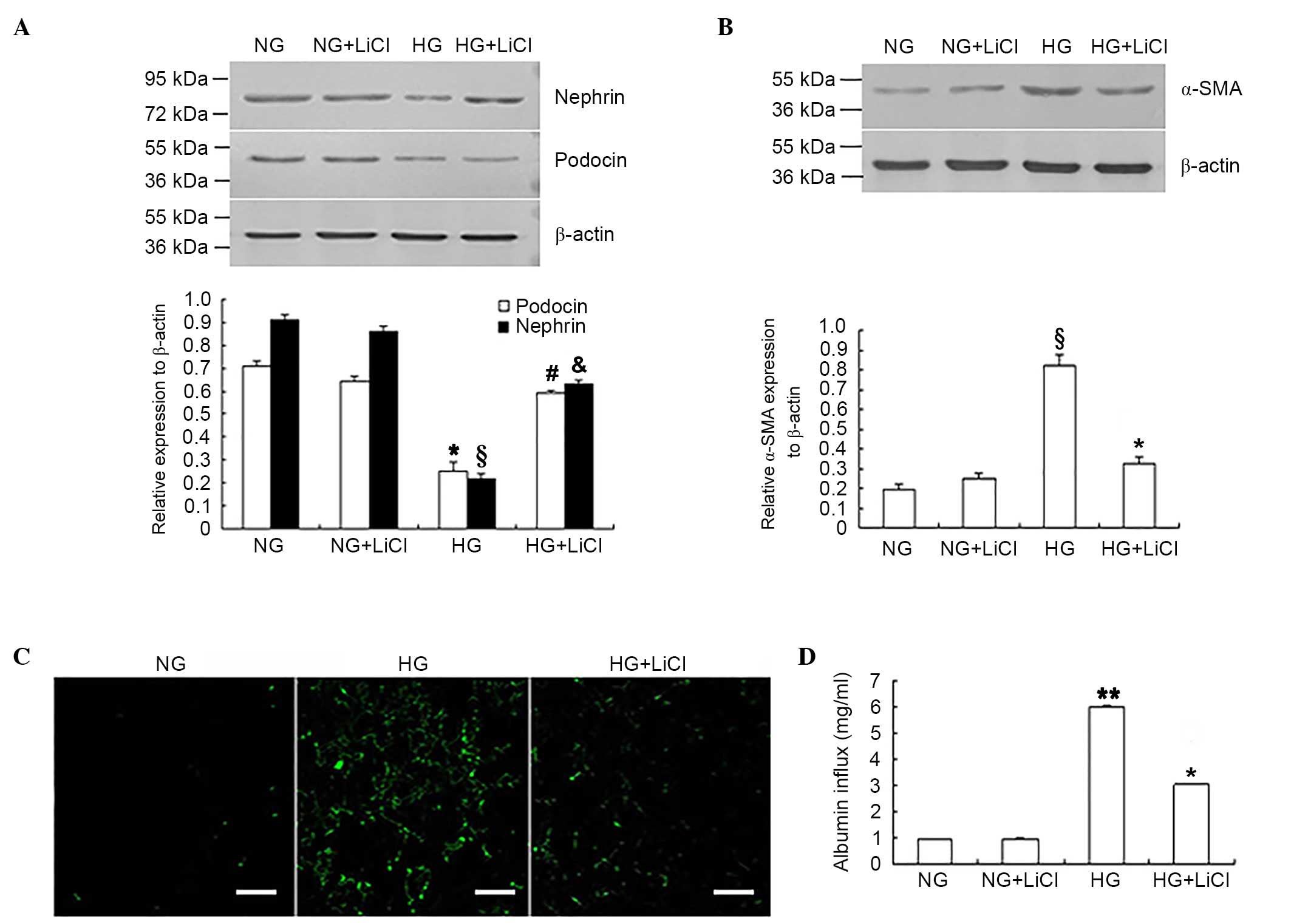
In addition to siRNA-mediated downregulation of
GSK-3β expression levels, the GSK-3β inhibitor, LiCl was used to
inhibit GSK-3β activity. Following GSK-3β inhibition, nephrin and
podocin expression levels were significantly increased in podocytes
under HG conditions when compared with the HG only group
(P<0.05; Fig. 4A), whereas
α-SMA and fibronectin expression levels were significantly reduced
when compared with the HG only group (P<0.05, Fig. 4B and C). LiCl was significantly
associated with the improvement in monolayer barrier function in
podocytes exposed to HG, which was reflected by the significant
reduction of the albumin inflow when compared with HG only group
(P<0.05; Fig. 4D).
Discussion
Podocyte damage is closely associated with the
development of albuminuria and is an important factor in the
occurrence and development of various kidney diseases (15). Previous studies have determined
that exfoliation and apoptosis of podocytes, and the fusion and
disappearance of podocyte processes contribute to the development
of DN (16–18). A previous study indicated that
podocyte exfoliation and apoptosis occurred following the
development of albuminuria (19).
Consequently, podocyte loss may be unlikely to initiate a process
during DN, which may lead to albuminuria (19). Therefore, earlier cellular events
may be involved. It has been proposed that stimulation of EMT in
podocytes is a reversible process that occurs prior to exfoliation
and apoptosis (9). Phenotypic
trans-differentiation of podocytes may lead to disordered cell
function, ultimately result in albuminuria.
Nephrin and podocin have been observed to interact
with other glomerular slit diaphragm components, including
CD2-associated protein and cytoskeleton-associated proteins (for
example, zonula occluden 1 and actin). These proteins are important
for maintaining podocyte integrity and preserving the normal
function of the glomerular slit diaphragm. A previous study has
reported that reduced expression of both nephrin and podocin is
closely associated with the occurrence of albuminuria (20). Fibronectin and α-SMA are phenotypic
markers of mesenchymal cells and increased expression of α-SMA in
non-smooth muscle cells has been established as an important basis
for cell activation and trans-differentiation (21). The increased expression levels of
these proteins act as potential markers of the mesenchymal
trans-differentiation process.
The results of the present study demonstrated that
HG conditions reduced nephrin and podocin expression, whereas α-SMA
and fibronectin expression was increased in cultured mouse
podocytes, indicating that HG induced EMT in podocytes. These
results were consistent with previous studies (22,23).
In addition, the current study demonstrated glucose
concentration-dependent impairment of the barrier function of
podocytes using Transwell experiments. These observations suggest
that high glucose-induced EMT led to the loss of functional
proteins, which in turn damaged the integrity of the slit diaphragm
and led to abnormal glomerular filtration. This process may
represent an important mechanism in the development of albuminuria.
However, these results require validation in vivo. Further
research is additionally required to investigate whether it is
possible to delay or minimize the effects of EMT in order to
suppress the progress of DN.
GSK-3β is a Ser/Thr adenosine
5′-monophosphate-activated protein kinase with highly conservative
sequence. GSK-3β may act as the primary regulatory enzyme of
numerous cellular signal transduction channels and has been
identified to influence cell growth and apoptosis (24). The influence of HG on GSK-3β
expression and activity in podocytes remains unclear. A previous
study reported that the activity of GSK-3β is increased in HG
conditions, resulting in the trans-differentiation of renal tubular
epithelial cells. Increased GSK-3β activity has also been reported
to be associated with HG-induced apoptosis of renal mesangial cells
(25). The results of the current
study indicated that HG induced GSK-3β activity, which was
associated with EMT and barrier dysfunction in podocytes. In
addition, HG-induced phosphorylation of GSK-3β at the Tyr216
activation site was observed in podocytes, which was consistent
with the study performed by Paeng et al (26). Therefore, this indicated the
importance of the expression, phosphorylation and activity of
GSK-3β in EMT and barrier dysfunction under HG conditions.
The importance of GSK-3β in DN remains to be fully
elucidated. Paeng et al (26) reported that enhanced GSK-3β
activity within podocytes under HG conditions was associated with
podocyte apoptosis, which has been suggested to be crucial for
albuminuria and progression of DN (26). Shang et al (27) reported that sulforaphane partially
ameliorated experimental DN by the inhibition of the GSK3β
signaling pathway (27). These
results implied that GSK-3β may be involved in DN. However,
Mariappan et al (28)
determined that the activation of GSK3β by sodium nitroprusside
(SNP) reduced the HG-induced laminin increase (in contrast to the
present study), an important characteristic of DN progression in
kidney-proximal tubular epithelial cells. In addition, diabetes led
to the inactivation of GSK3β by activation of the Src
proto-oncogene, pyruvate kinase 2, protein kinase B and
extracellular signal-related kinase. Furthermore, GSK3β activation
by SNP mitigated kidney injury induced by diabetes in vivo
(28), indicating that GSK3β may
suppress the progress of DN. To confirm the importance of GSK-3β in
HG-induced EMT and barrier dysfunction in podocytes, GSK-3β
siRNA was transfected in podocytes in order to downregulate GSK-3β
expression. LiCl was also used to inhibit GSK-3β activity under NG
and HG conditions. The results of the present study indicated that
GSK-3β expression and activity were essential for HG-induced EMT
and barrier dysfunction. As podocyte EMT and barrier dysfunction
are important for DN, the current results confirm the involvement
of GSK-3β in the pathogenesis and development of DN in
vitro.
A previous study on mouse podocytes reported that
treatment with a GSK-3β inhibitor and GSK-3β siRNA reduced
β-catenin and Snail expression levels and reversed HG-induced
upregulation of α-SMA expression levels; however, nephrin
expression levels were downregulated (11). The present study used further
markers of EMT, including the epithelial cell markers nephrin and
podocin, and the myofibroblast cell markers α-SMA and fibronectin
in order to confirm the occurrence of EMT in podocytes under HG
conditions. In addition to GSK-3β expression, the importance of
GSK-3β activity and phosphorylation in HG-induced EMT was
investigated in the present study. Furthermore, the effect of
GSK-3β expression and activity was observed on the barrier
dysfunction of podocytes exposed to HG conditions. Therefore, using
the recent study as the basis (11), the present study clarified the
importance of GSK-3β in DN progression by using in vitro
experiments.
In conclusion, the present study determined that
GSK-3β participated in HG-induced EMT and barrier dysfunction in
podocytes, which may suggest that GSK-3β is a potential therapeutic
target for novel DN treatment. Further experiments using an animal
of model of DN are required in order to characterize the effects of
GSK-3β expression and activity on podocyte EMT and function and to
fully determine the function of GSK-3β in the development of
albuminuria in patients with DN.
Acknowledgements
The present study was supported by the National
Basic Research Program of China 973 (grant no. 2012CB517606) and
the National Natural Science Foundation of China (grant nos.
81270807, 81400726 and 81070574).
References
|
1
|
Collins AJ, Foley RN, Chavers B,
Gilbertson D, Herzog C, Johansen K, Kasiske B, Kutner N, Liu J, St
Peter W, et al: United States renal data system 2011 annual data
report: Atlas of chronic kidney disease & end-stage renal
disease in the United States. Am J Kidney Dis. 59(1 Suppl 1). (A7):
e1–e420. 2012.
|
|
2
|
Wiggins RC: The spectrum of
podocytopathies: A unifying view of glomerular diseases. Kidney
Int. 71:1205–1214. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Juarez G Fernandez, Luño J, Barrio V, de
Vinuesa SG, Praga M, Goicoechea M, Cachofeiro V, Nieto J, Fernández
Vega F, Tato A, et al: Effect of dual blockade of the
renin-angiotensin system on the progression of type 2 diabetic
nephropathy: A randomized trial. Am J Kidney Dis. 61:211–218. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brenner BM, Cooper ME, de Zeeuw D, Keane
WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z and
Shahinfar S: RENAAL Study Investigators: Effects of losartan on
renal and cardiovascular outcomes in patients with type 2 diabetes
and nephropathy. N Engl J Med. 345:861–869. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Soda K, Balkin DM, Ferguson SM, Paradise
S, Milosevic I, Giovedi S, Volpicelli-Daley L, Tian X, Wu Y, Ma H,
et al: Role of dynamin, synaptojanin, and endophilin in podocyte
foot processes. J Clin Invest. 122:4401–4411. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li Y, Kang YS, Dai C, Kiss LP, Wen X and
Liu Y: Epithelial-to-mesenchymal transition is a potential pathway
leading to podocyte dysfunction and proteinuria. Am J Pathol.
172:299–308. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jope RS, Yuskaitis CJ and Beurel E:
Glycogen synthase kinase-3 (GSK3): Inflammation, diseases, and
therapeutics. Neurochem Res. 32:577–595. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Campa VM and Kypta RM: Issues associated
with the use of phosphospecific antibodies to localise active and
inactive pools of GSK-3 in cells. Biol Direct. 6:42011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu Y: New insights into
epithelial-mesenchymal transition in kidney fibrosis. J Am Soc
Nephrol. 21:212–222. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bachelder RE, Yoon SO, Franci C, de
Herreros AG and Mercurio AM: Glycogen synthase kinase-3 is an
endogenous inhibitor of Snail transcription: Implications for the
epithelial-mesenchymal transition. J Cell Biol. 168:29–33. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Guo J, Xia N, Yang L, Zhou S, Zhang Q,
Qiao Y and Liu Z: GSK-3β and vitamin D receptor are involved in
β-catenin and snail signaling in high glucose-induced
epithelial-mesenchymal transition of mouse podocytes. Cell Physiol
Biochem. 33:1087–1096. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sharma K, Deelman L, Madesh M, Kurz B,
Ciccone E, Siva S, Hu T, Zhu Y, Wang L, Henning R, et al:
Involvement of transforming growth factor-beta in regulation of
calcium transients in diabetic vascular smooth muscle cells. Am J
Physiol Renal Physiol. 285:F1258–F1270. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
McGowan TA, Madesh M, Zhu Y, Wang L, Russo
M, Deelman L, Henning R, Joseph S, Hajnoczky G and Sharma K:
TGF-beta-induced Ca(2+) influx involves the type III IP(3) receptor
and regulates actin cytoskeleton. Am J Physiol Renal Physiol.
282:F910–F920. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rico M, Mukherjee A, Konieczkowski M,
Bruggeman LA, Miller RT, Khan S, Schelling JR and Sedor JR:
WT1-interacting protein and ZO-1 translocate into podocyte nuclei
after puromycin aminonucleoside treatment. Am J Physiol Renal
Physiol. 289:F431–F441. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Leeuwis JW, Nguyen TQ, Dendooven A, Kok RJ
and Goldschmeding R: Targeting podocyte-associated diseases. Adv
Drug Del Rev. 62:1325–1336. 2010. View Article : Google Scholar
|
|
16
|
Dai C, Stolz DB, Bastacky SI, St-Arnaud R,
Wu C, Dedhar S and Liu Y: Essential role of integrin-linked kinase
in podocyte biology: Bridging the integrin and slit diaphragm
signaling. J Am Soc Nephrolo. 17:2164–2175. 2006. View Article : Google Scholar
|
|
17
|
El-Aouni C, Herbach N, Blattner SM, Henger
A, Rastaldi MP, Jarad G, Miner JH, Moeller MJ, St-Arnaud R, Dedhar
S, et al: Podocyte-specific deletion of integrin-linked kinase
results in severe glomerular basement membrane alterations and
progressive glomerulosclerosis. J Am Soc Nephrolo. 17:1334–1344.
2006. View Article : Google Scholar
|
|
18
|
Lee J and Kim MS: The role of GSK3 in
glucose homeostasis and the development of insulin resistance.
Diabetes Res Clin Pract. 77:(Suppl 1). S49–S57. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Marshall SM: The podocyte: A major player
in the development of diabetic nephropathy? Horm Metab Res.
37:(Suppl 1). S9–S16. 2005. View Article : Google Scholar
|
|
20
|
Billing H, Müller D, Ruf R, Lichtenberger
A, Hildebrandt F, August C, Querfeld U and Haffner D: NPHS2
mutation associated with recurrence of proteinuria after
transplantation. Pediatr Nephrol. 19:561–564. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hautmann MB, Adam PJ and Owens GK:
Similarities and differences in smooth muscle alpha-actin induction
by TGF-beta in smooth muscle versus non-smooth muscle cells.
Arterioscler Thromb Vasc Biol. 19:2049–2058. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lv Z, Hu M, Zhen J, Lin J, Wang Q and Wang
R: Rac1/PAK1 signaling promotes epithelial-mesenchymal transition
of podocytes in vitro via triggering β-catenin transcriptional
activity under high glucose conditions. Int J Biochem Cell Biol.
45:255–264. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chen T, Zheng LY, Xiao W, Gui D, Wang X
and Wang N: Emodin ameliorates high glucose induced-podocyte
epithelial-mesenchymal transition in-vitro and in-vivo. Cell
Physiol Biochem. 35:1425–1436. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shakoori A, Ougolkov A, Yu ZW, Zhang B,
Modarressi MH, Billadeau DD, Mai M, Takahashi Y and Minamoto T:
Deregulated GSK3beta activity in colorectal cancer: Its association
with tumor cell survival and proliferation. Biochem Biophysl Res
Commun. 334:1365–1373. 2005. View Article : Google Scholar
|
|
25
|
Lin CL, Wang JY, Huang YT, Kuo YH,
Surendran K and Wang FS: Wnt/beta-catenin signaling modulates
survival of high glucose-stressed mesangial cells. J Am Soc
Nephrol. 17:2812–2820. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Paeng J, Chang JH, Lee SH, Nam BY, Kang
HY, Kim S, Oh HJ, Park JT, Han SH, Yoo TH, et al: Enhanced glycogen
synthase kinase-3β activity mediates podocyte apoptosis under
diabetic conditions. Apoptosis. 19:1678–1690. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shang G, Tang X, Gao P, Guo F, Liu H, Zhao
Z, Chen Q, Jiang T, Zhang N and Li H: Sulforaphane attenuation of
experimental diabetic nephropathy involves GSK-3 beta/Fyn/Nrf2
signaling pathway. J Nutr Biochem. 26:596–606. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mariappan MM, Prasad S, D'Silva K, Cedillo
E, Sataranatarajan K, Barnes JL, Choudhury GG and Kasinath BS:
Activation of glycogen synthase kinase 3β ameliorates
diabetes-induced kidney injury. J Biol Chem. 289:35363–35375. 2014.
View Article : Google Scholar : PubMed/NCBI
|