Introduction
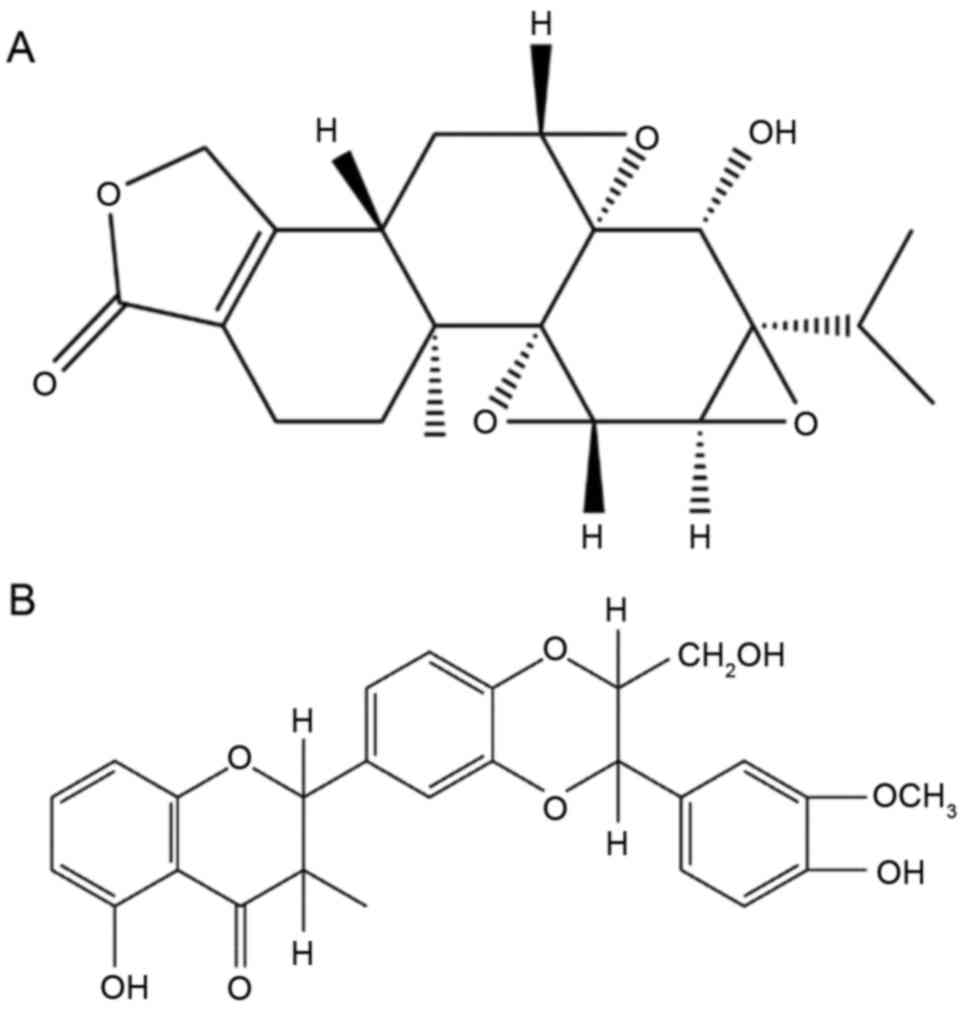
Triptolide (TP;
C20H24O6; Fig. 1A), a diterpene triepoxide, is
derived from the traditional Chinese medicinal herb Tripterygium
wilfordii Hook F (TWHF) (1),
and both are commonly prescribed to treat autoimmune and
inflammatory diseases, including rheumatoid arthritis, systemic
lupus erythematosus and nephritis in Chinese clinics. However, in
recent decades, TWHF, TP and their preparations have attracted
increased attention regarding their potential toxicity,
particularly liver and kidney injury, which have limited their
clinical application to a certain degree (2–4).
Reports have indicated that the adverse reactions observed were
primarily caused by TP, its major active component and toxic
ingredient. Currently, research efforts are focused on reducing
these adverse effects.
Attempts to identify the underlying mechanisms of TP
in disease treatment have led to promising results. A previous
study demonstrated that oral administration of TP in rats resulted
in acute hepatic injury and markedly elevated levels of alanine
transaminase (ALT) and aspartate aminotransferase (AST) in the
serum (5). Further studies have
revealed that TP-induced liver injury may be associated with the
excessive release of peroxides, which subsequently induces
oxidative stress and lipid peroxidation (6), the production of inflammatory
mediators leading to immunological injury, the suppression of cell
activities, the stimulation of apoptotic-associated proteins and
damage of the mitochondrial respiratory chain leading to apoptosis
(7–9).
Natural medicines from plants have been considered
as potentially effective and safe alternative treatments for liver
diseases, and are increasingly employed worldwide. Silybum
marianum (Asteraceae), a typical component in traditional
Chinese medicine, has been broadly utilized with a long history of
use as a remedy for various hepatic disorders, including hepatitis
and cirrhosis, and to prevent liver damage induced by chemicals and
environmental toxins (10,11).
Silymarin is an extract of Silybum marianum,
and is a lipophilic complex of two flavonoids (taxifolin and
quercetin) and three flavonolignane diastereomers: Silibinin, the
primary and active component
(C24H19O10; Fig. 1B), silydianin and silychristin
(12). Silymarin has been used
clinically either alone or as a major component of various
pharmaceutical preparations for centuries as a hepatoprotective
agent, and has exhibited protective effects against inflammation,
oxidation and apoptosis (11,13–15).
The anti-hepatotoxic mechanism of silymarin is associated with its
stabilizing effect on cytoplasmic membranes (16). Therefore, silymarin has been
investigated in numerous animal models and exerts marked
therapeutic effects on liver injury of different etiology (17), including alcoholic-induced liver
damage (18),
diethylnitrosamine-induced liver disease (19), hepatitis C virus and carbon
tetrachloride-induced oxidative disorders (20). Based on these studies, it may be
concluded that silymarin may scavenge reactive oxidative species
(ROS) and alleviate lipid peroxidation induced by various
lipophilic hepatotoxins. However, the potential protective effect
of silymarin against TP-induced hepatotoxicity remains to be
investigated.
Therefore, to the best of our knowledge, the present
study was the first to investigate the protective effect of
silymarin on TP-induced oxidative damage, inflammation and
apoptosis, and the potential underlying mechanisms. The results
indicated that silymarin pretreatment, particularly at high dose
(200 mg/kg), markedly reduced TP-induced hepatotoxicity.
Materials and methods
Materials
TP (purity >98% by high-performance liquid
chromatography analysis) was supplied by the National Institute for
the Control of Pharmaceutical and Biological Products (Beijing,
China). Silymarin was purchased from Sigma-Aldrich (Merck KGaA,
Darmstadt, Germany) and consisted primarily of silibinin (>30%),
isosilibinin, silicristin and silidianin. TP was dissolved in 0.05%
dimethyl sulfoxide saline. Silymarin was suspended in 0.5% sodium
carboxymethyl cellulose (CMC-Na) distilled water solution. Other
chemicals and reagents used were of analytical grade.
Animals
A total of 60 male Wistar rats (weight, 220±20 g;
6-8 weeks) were obtained from the Experimental Animal Center of
Guangzhou University of Chinese Medicine (Guangzhou, China). All
the experiments were performed in a specific-pathogen free
laboratory at a controlled temperature of 25±2°C and relative
humidity of 35–75% on a 12 h light/dark cycle. Animals had free
access to rat chow and tap water. All experimental protocols were
in compliance with the guidelines of the Committee for Animal Care
and Use of Guangzhou University of Chinese Medicine, and were
approved by the ethical committee of Guangzhou University of
Chinese Medicine.
Animal grouping
Rats were randomly divided (n=12/group) into five
experimental groups. Normal control (NC) and triptolide (TP) groups
received oral administration of normal saline (1 ml/100 g), whereas
silymarin-treated groups were orally administrated with silymarin
(50, 100 and 200 mg/kg) dissolved in 0.5% CMC-Na distilled water.
The doses of silymarin employed in the present study were based on
our prior trial and previous study (21). Following treatment with normal
saline or silymarin for 7 consecutive days, all groups, excluding
the NC group, were given TP (2 mg/kg) by intraperitoneal injection
to establish the liver injury animal model. At the end of the
experimental period (day 8), all rats were fasted for 12 h. On the
following day, the animals were anesthetized with an
intraperitoneal injection of 10% chloral hydrate. Blood samples
were collected from the abdominal aorta, and rats were subsequently
sacrificed by spinal dislocation and liver tissue was collected
from the left lobe.
Blood biochemical studies
Blood samples were placed at room temperature for 1
h. Following centrifugation at 1,000 × g for 10 min at room
temperature, the serum was separated for biochemical estimations.
The serum levels of ALT, AST, alkaline phosphatase (ALP), total
cholesterol (TC) and γ-glutamyl transferase (GGT) were measured
using a Hitachi-7180 type biochemical analyzer following the
standard methods.
Preparation of liver homogenate and
sections
The liver tissues were chopped into 1 cm3
sections and divided into two groups. One was prepared to make 1:9
(w/v) homogenates with cold saline or phosphate buffer saline (PBS)
using a tissue homogenizer (IKA T 18 Basic). The homogenate was
centrifuged at 1,000 × g for 10 min at 4°C to obtain the
supernatant samples for subsequent determinations. The other group
of liver tissues were fixed in 10% formalin at room temperature for
at least 24 h for further observation of tissue sections.
Measurement of antioxidant enzymatic
activities and lipid peroxidation
The supernatant of normal saline homogenates was
used to measure the activities of the important antioxidant enzymes
superoxide dismutase (SOD), glutathione peroxidase (GSH-Px),
glutathione S-transferase (GST) and catalase (CAT), as well as
glutathione (GSH) and malonaldehyde (MDA) levels in the liver,
according to the manufacturer's instructions [total SOD assay kit
(hydroxylamine method), GSH-PX assay kit (colorimetric method), GST
assay kit (colorimetric method), GSH assay kit (colorimetric
method), CAT assay kit (ultraviolet) and MDA assay kit (TBA
method); Nanjing Jiancheng Bioengineering Institute, Nanjing,
China]
Hepatic cytokine and cytochrome
assays
The levels of inflammatory cytokines tumor necrosis
factor (TNF)-α, interleukin (IL)-6, IL-10, IL-1β, and cytochrome
c (Cyt C) levels were measured in supernatants using
specific ELISA kits [E-30644 (IL-6), E-30418 (IL-1β), E-30633
(TNF-α), E-30649 (IL-10) and E-30273 (Cyt C); Beijing Chenglin
Biotechnology, Beijing, China] according to the manufacturer's
instructions.
Histopathological examination
After being fixed in 10% formalin for 24 h, the
liver tissue was dehydrated in graded ethanol (50–100%), cleared in
xylene and embedded in paraffin wax. The paraffin sections (5 µm
thickness) were examined for pathological changes in the liver
tissue using a light microscope (BK-DM320; Chongqing Optec
Instrument Co., Ltd., Chongqing, China) and photographed at ×200
magnification following hematoxylin and eosin (H&E) staining
for 5–10 min at room temperature.
Detection of apoptosis
A terminal deoxynucleotidyl-transferase-mediated
dUTP nick end labeling (TUNEL) apoptosis detection kit (Nanjing
Lufei Biotechnology Co., Ltd., Nanjing, China) was used to assess
the apoptosis rate of liver cells. Paraffin sections (5 µm) were
incubated with the TUNEL reaction mixture at 37°C for 60 min, then
incubated with converter-POD in a humidified chamber for 30 min at
37°C followed by incubation with DAB substrate (5 µl 20X DAB, 1 µl
30% H2O2 and 94 µ l PBS) for 10 min at 20°C.
The sections were washed and mounted in PBS. A total of 15 fields
(×200 magnification) for each section were randomly selected to
quantify the positive cells and define the apoptosis indexes using
ImageJ software (version 1.50; National Institutes of Health,
Bethesda, MD, USA).
Immunohistochemical staining and
quantitative analysis
Immunohistochemical analyses were performed to
determine the expression of Bcl-2-associated X (Bax) and Bcl-2 in
the liver. Paraffin sections (5 µm thick) of the liver tissue were
initially processed by dehydration. Following retrieval by citrate
buffer (pH=6) microwave antigen retrieval for 15 min, 3%
H2O2 was added to inactivate endogenous
enzymes for another 15 min. Then, 5% normal goat serum (ab7481;
Abcam, Cambridge, UK) diluted with PBS was used to block
non-specific binding for 10 min at room temperature. Subsequently,
sections were washed with 0.01 mol/l PBS following incubation of
sections with 50 µl rabbit monoclonal antibodies for Bcl-2 (1:100,
ab59348) and Bax (1:100; ab53154) (both from Abcam) at 4°C
overnight. The secondary antibody was goat anti-rabbit IgG H&L
(HRP) (1:1,000, ab6721; Abcam) for 30 min at 37°C. The slides were
counterstained with hematoxylin (Modified Mayer's, ab220365; Abcam)
for 2–3 min at room temperature. Finally, the sections were reacted
with a staining solution containing 0.03% 3,3′-diaminobenzidine
(Nanjing Lufei Biotechnology Co., Ltd.,) for 5–10 min at room
temperature. The sections were observed with an Olympus IX71
fluorescence microscope (Olympus Corporation, Tokyo, Japan) at ×200
magnification. A total of 15 fields in each section were randomly
selected to quantify positive cells by ImageJ software (version
1.50; National Institutes of Health).
Western blotting for cleaved caspase-3
(c-caspase-3), phosphorylated (p)-p38 and p-c-Jun N-terminal kinase
(JNK) protein expression
Western blot analysis was performed to examine the
expression of c-caspase-3, which stimulates cell apoptosis, and
TNF-α induced phosphorylation of p38 and JNK in the inflammatory
pathway. Liver tissue was homogenized with proteinase inhibitor on
ice to obtain total protein extract according to the protocol of
the T-PER Tissue Protein Extraction reagent (Thermo Fisher
Scientific, Inc., Waltham, MA, USA). Protein concentration was
determined following the protocol of a BCA protein assay kit
(G2026; Wuhan Goodbio Technology Co., Ltd., Wuhan, China). Extracts
containing equal amounts of protein (50 µg) were separated by 10%
SDS-PAGE and transferred to polyvinylidene fluoride membranes,
which were blocked at room temperature for 1 h in 0.5% TBST (50
mmol/l Tris-HCl, pH 7.6; 150 mmol/l NaCl; 0.1% Tween-20) containing
5% non-fat milk and subsequently incubated with primary rabbit
anti-rat polyclonal antibodies against c-caspase-3 (1:1,000, 9661;
Cell Signaling Technology, Inc., Danvers, MA, USA) and β-actin
(1:1,000, GB13001-1; Wuhan Goodbio Technology Co., Ltd.), and
rabbit anti-rat monoclonal antibodies against p-p38 (1:1,000, 4511)
and p-JNK (1:1,000, 4671) (both from Cell Signaling Technology,
Inc.) overnight at 4°C. β-actin was used as an internal control.
All primary antibodies were purchased from Cell Signaling
Technology, Inc. Subsequently, the membranes were washed with TBST
for 15 min and incubated with secondary antibodies (anti-rabbit
IgG, HRP-linked antibody, 1:3,000; Cell Signaling Technology, Inc.)
labeled with horseradish peroxidase for 30 min at room temperature,
followed by washing with TBST for 15 min. The membranes were then
developed using an electrochemiluminescence kit (G2014; Wuhan
Goodbio Technology Co., Ltd.) and the densities of the
immunoreactive bands were analyzed using ImageJ software (version
1.50; National Institutes of Health).
Statistical analysis
Data are presented as the mean ± standard deviation.
One-way analysis of variance followed by Fisher's least significant
difference tests was performed to statistically analyze the data.
SPSS software (version 16; SPSS, Inc., Chicago, IL, USA) was used
for statistical analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Silymarin reduces the serum levels of
biochemical parameters
The levels of ALT, AST, ALP, TC and GGT were
estimated in serum samples as sensitive biomarkers of liver
function. These enzymes (ALT, AST, ALP and GGT) were enzymes
derived from the injured liver tissue cells. As presented in
Table I, the levels of these serum
biochemical parameters in the TP group were significantly higher
compared with the NC group (P<0.01), which was indicative of
liver dysfunction. However, the levels of these indicators in the
three silymarin-pretreated groups markedly reduced to normal levels
in a dose-dependent manner, indicating that silymarin may
effectively ameliorate TP-induced liver injury.
 | Table I.Levels of ALT, AST, ALP, TC and GGT
in the serum of different treatment groups. |
Table I.
Levels of ALT, AST, ALP, TC and GGT
in the serum of different treatment groups.
| Group | ALT, U/l | AST, U/l | ALP, U/l | TC, mmol/l | GGT, U/l |
|---|
| NC |
31.1±4.3 |
65.4±10.0 |
128.7±13.9 |
1.5±0.1 |
1.0±0.0 |
| TP |
78.3±13.7a |
300.3±118.2a |
172.0±32.5a |
2.6±0.8a |
1.8±0.9a |
| SLT |
46.0±7.5c |
138.5±24.3c |
164.5±35.2 |
1.9±0.3c |
1.2±0.6 |
| SMT |
42.4±7.0c |
130.9±31.0c |
139.9±31.3b |
1.8±0.2c |
1.1±0.3b |
| SHT |
40.8±7.8c |
105.9±17.6c |
136.0±20.8b |
1.7±0.6c |
1.0±0.3b |
Silymarin alleviates alteration of
histological structure
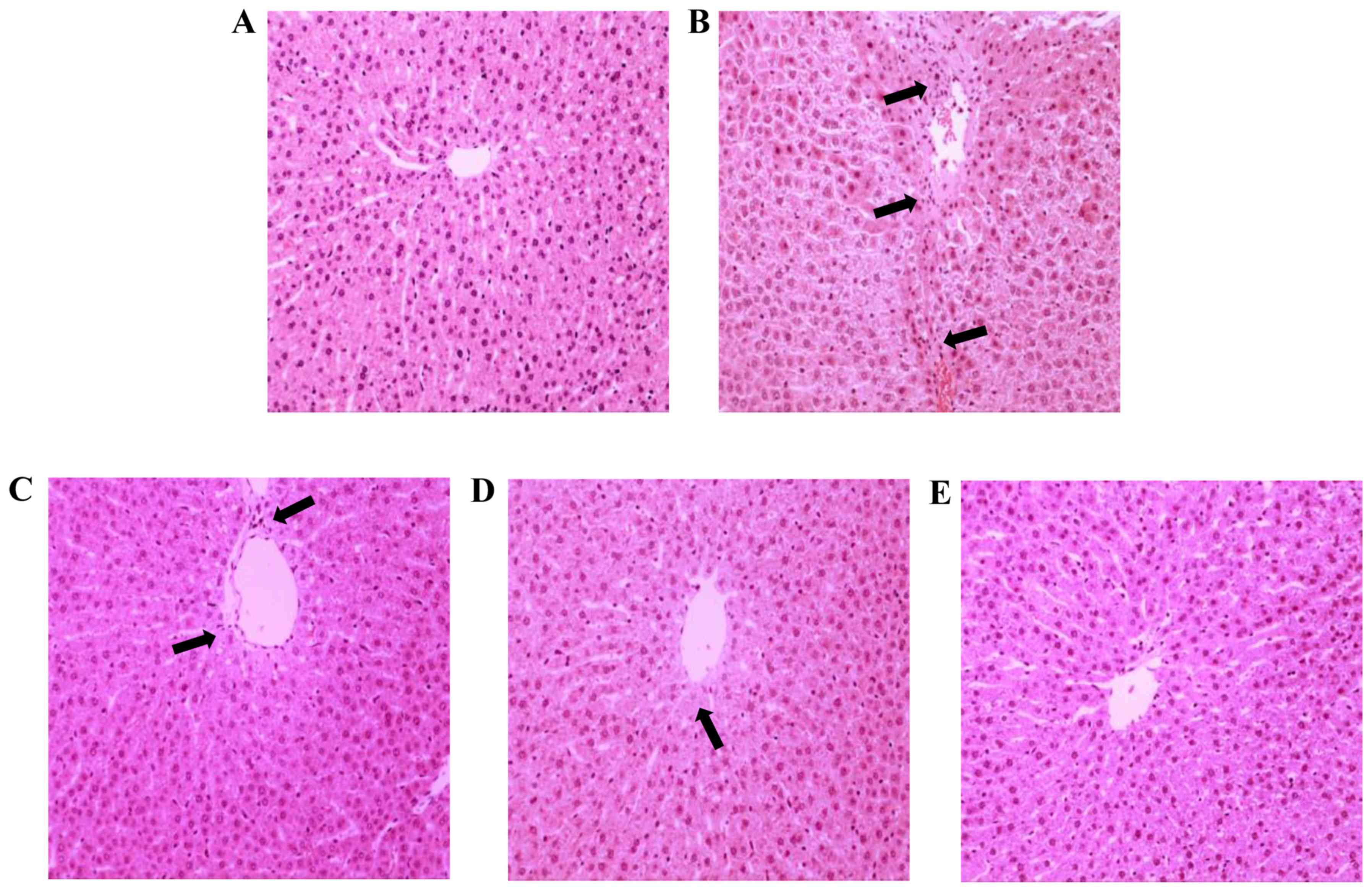
Hepatic histological changes directly depict the
degree of liver injury. To morphologically characterize the
potential pathological alternations in hepatocytes, routine H&E
staining was performed. As demonstrated in Fig. 2A, a clear and regular lobular
structure was observed, where hepatic cords remained legible and
radiated from the central vein in the NC group. Compared with the
NC group, hepatic parenchymal necrosis and inflammatory cell
infiltration was apparent, and disordered hepatic cords accompanied
by extensive vacuolation congestion was also observed in the TP
group (Fig. 2B), which was
consistent with the assay results for biochemical parameters in the
serum, indicating the successful establishment of the hepatic
injury model. Furthermore, hepatocytes were markedly swollen, with
condensed karyons and loosened cytoplasts. However, silymarin
pretreatment of three tested doses appeared to alleviate TP-induced
liver injury in a dose-dependent manner, as evidenced by reduced
inflammation infiltration, intact tissue structure, and reduced
necrotic and apoptotic mass (Fig.
2C-E), compared with the TP group. Cell apoptosis and
inflammatory infiltration was particularly limited when subjected
to silymarin pretreatment at the doses of 100 and 200 mg/kg.
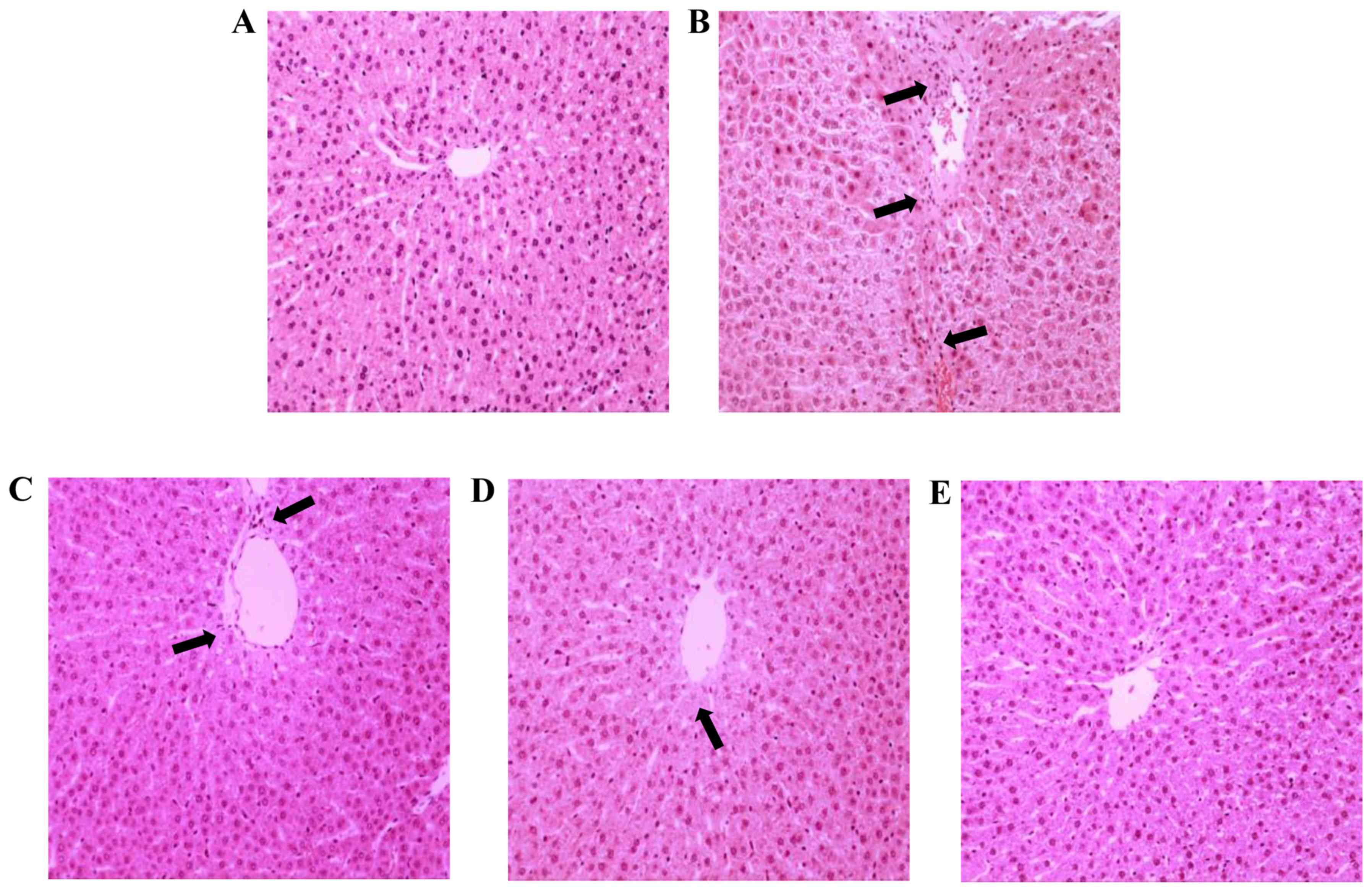 | Figure 2.Histological assessments were
performed by hematoxylin and eosin staining of liver tissues from
different treatment groups. (A) NC group sections exhibited normal
histological structure and the central vein was obvious. (B) TP
group sections appeared to exhibit fibrosis, focal necrosis and
congestion of the hepatoportal blood vessel, which was covered by
inflammatory cell infiltration (arrows). (C) SLT and (D) SMT groups
exhibited sporadic necrosis of hepatocytes, with improvements
compared with the TP group (arrows). (E) SHT group sections
exhibited normal morphology and a marked improvement in hepatocyte
structure, which was similar to that in the NC group, compared with
the TP group. Magnification, ×200. NC, normal control; TP,
triptolide; SLT, low-dose silymarin treatment; SMT, middle-dose
silymarin treatment; SHT, high-dose silymarin treatment. |
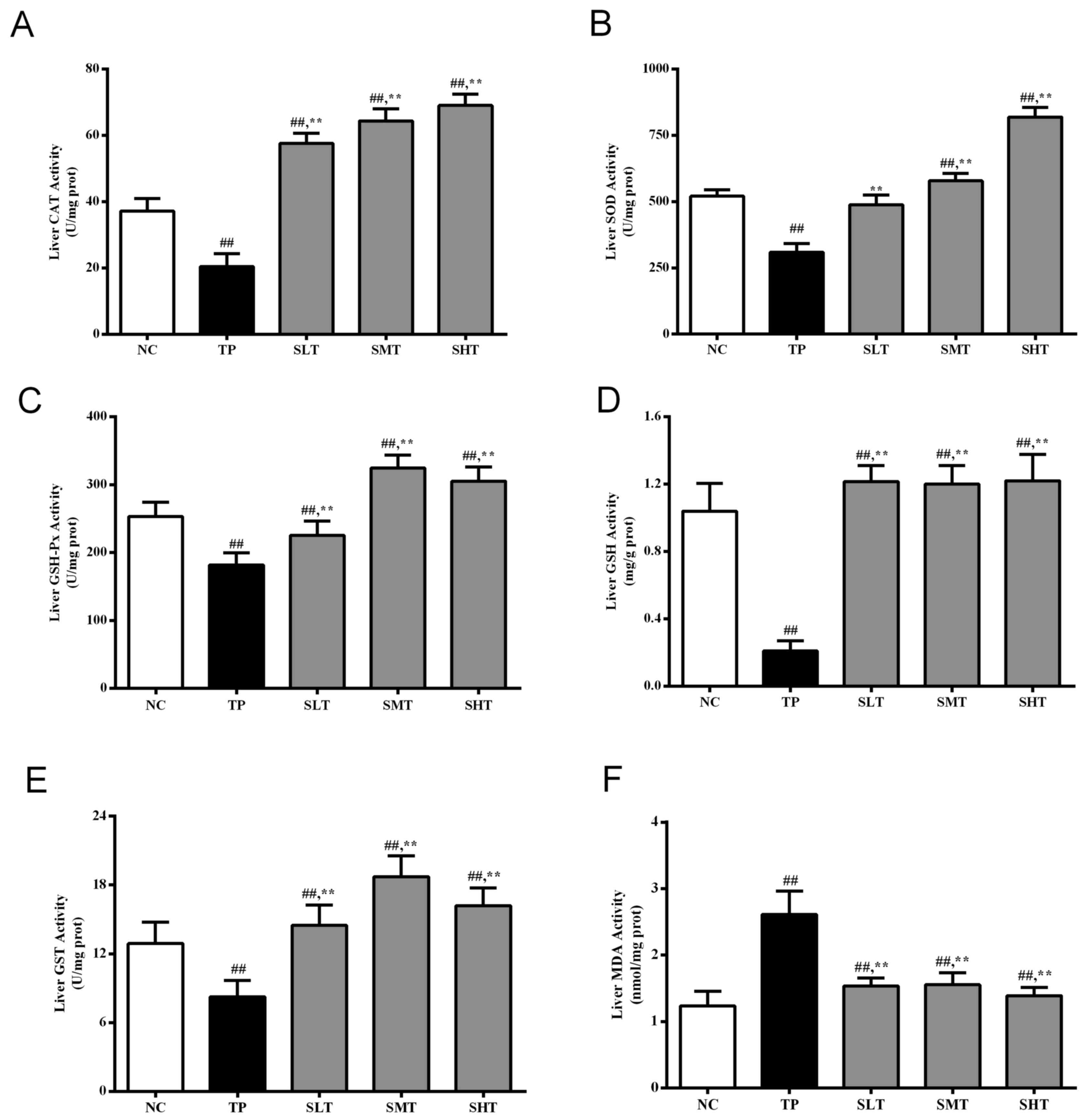
Silymarin upregulates antioxidant
enzymatic activities
As demonstrated in Fig.
3A-E, TP administration markedly reduced the activities of the
antioxidant enzymes SOD, GSH-Px, CAT and GST and GSH levels by
40.61, 28.18, 45.10, 35.97 and 79.81%, respectively, compared with
the NC group (P<0.05). However, pretreatment with silymarin,
particularly at middle and high doses, significantly upregulated
the activities compared with the TP group (P<0.05). Furthermore,
silymarin significantly elevated the CAT and GST activities to
levels that surpassed those in the NC group (Fig. 3A and E). Therefore, silymarin
exhibited excellent effects in mitigating TP-induced systemic
antioxidant enzyme exhaustion.
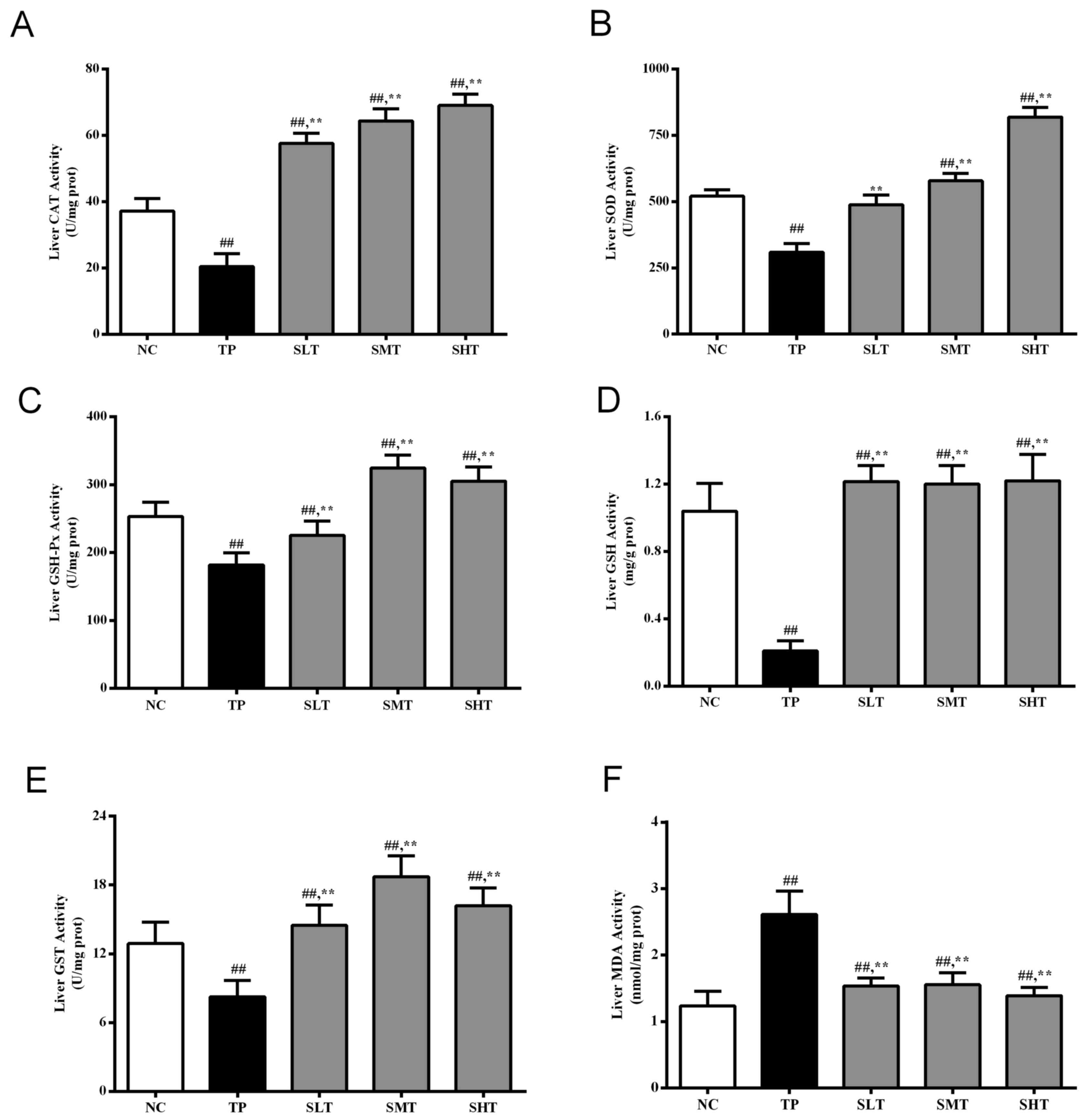 | Figure 3.Effect of silymarin on the activity
of antioxidant enzymes and MDA levels in the liver. The
activities/levels of (A) CAT, (B) SOD, (C) GSH-Px, (D) GSH, (E) GST
and (F) MDA in the liver of different treatment groups were
determined using respective kits. Data are presented as the mean ±
standard deviation, n=12. ##P<0.01 vs. NC group;
**P<0.01 vs. TP group. MDA, malonaldehyde; CAT, catalase; SOD,
superoxide dismutase; GSH-Px, glutathione peroxidase; GSH,
glutathione; GST, glutathione S-transferase; NC, normal control;
TP, triptolide; SLT, low-dose silymarin treatment; SMT, middle-dose
silymarin treatment; SHT, high-dose silymarin treatment. |
Silymarin suppresses TP-induced lipid
peroxidation
The hepatic MDA level was determined to evaluate the
degree of lipid peroxidation (Fig.
3F). MDA content increased significantly in the liver of the
rats in the TP group compared with the NC group (P<0.01).
However, silymarin significantly suppressed this excessive
accumulation of MDA compared with the TP group (P<0.01), and no
significant difference was observed between the NC and high-dose
silymarin group. Therefore, silymarin markedly suppressed
TP-induced lipid peroxidation, which was consistent with the
improvement in antioxidant enzymatic activities.
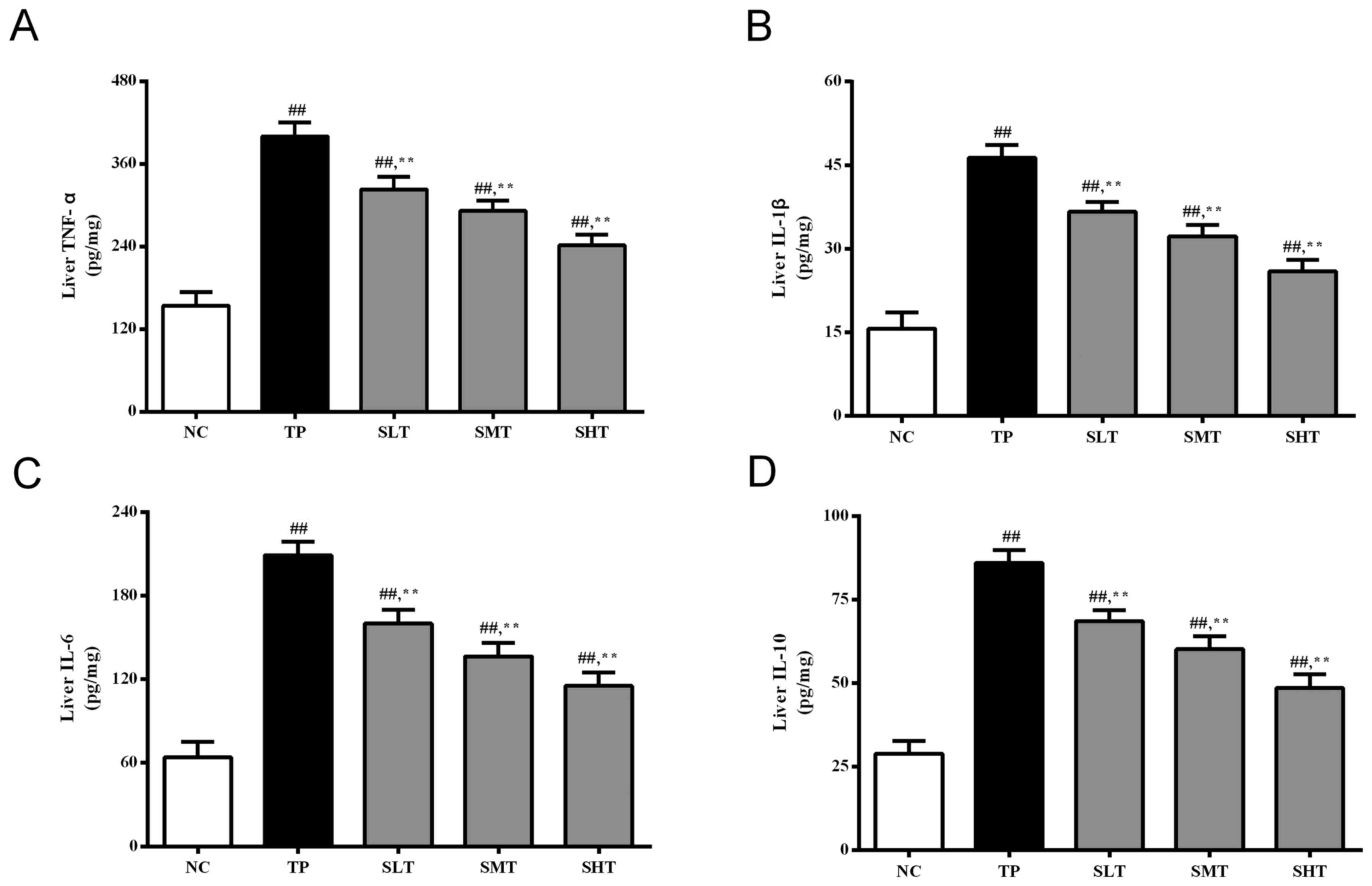
Silymarin decreases the production of
inflammatory cytokines
An excessive inflammatory response is associated
with oxidative stress (22). In
the present study, the levels of important inflammatory cytokines,
TNF-α, IL-1β, IL-6 and IL-10, in the liver were determined. The
levels of these inflammatory mediators were significantly higher in
the TP group compared with the NC group (Fig. 4), indicating that TP induced severe
inflammatory response in the liver. Promisingly, pretreatment with
silymarin significantly inhibited the production of these
proinflammatory factors in a dose-dependent manner compared with
the TP group (P<0.01). These results indicate that silymarin may
attenuate TP-induced liver injury by suppressing the inflammatory
response.
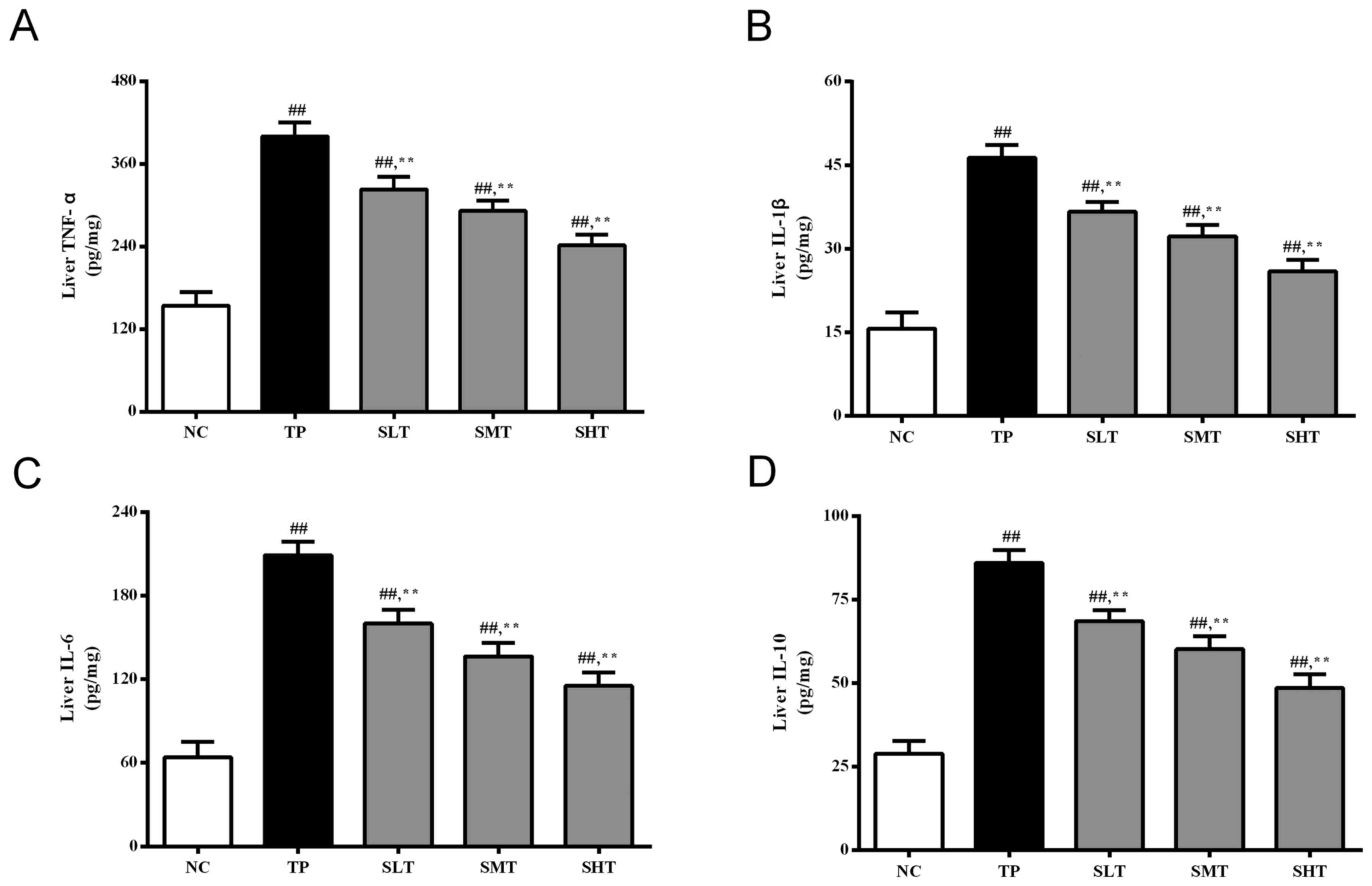 | Figure 4.Effect of silymarin on inflammatory
cytokines in the liver. ELISAs were performed to determine the
levels of (A) TNF-α, (B) IL-1β, (C) IL-6 and (D) IL-10 in the liver
of rats in different treatment groups. Data are presented as the
mean ± standard deviation, n=12. ##P<0.01 vs. NC
group; **P<0.01 vs. TP group. TNF, tumor necrosis factor; IL,
interleukin; NC, normal control; TP, triptolide; SLT, low-dose
silymarin treatment; SMT, middle-dose silymarin treatment; SHT,
high-dose silymarin treatment. |
Silymarin inhibits transduction of the
inflammatory pathway and reduces c-caspase-3 protein
expression
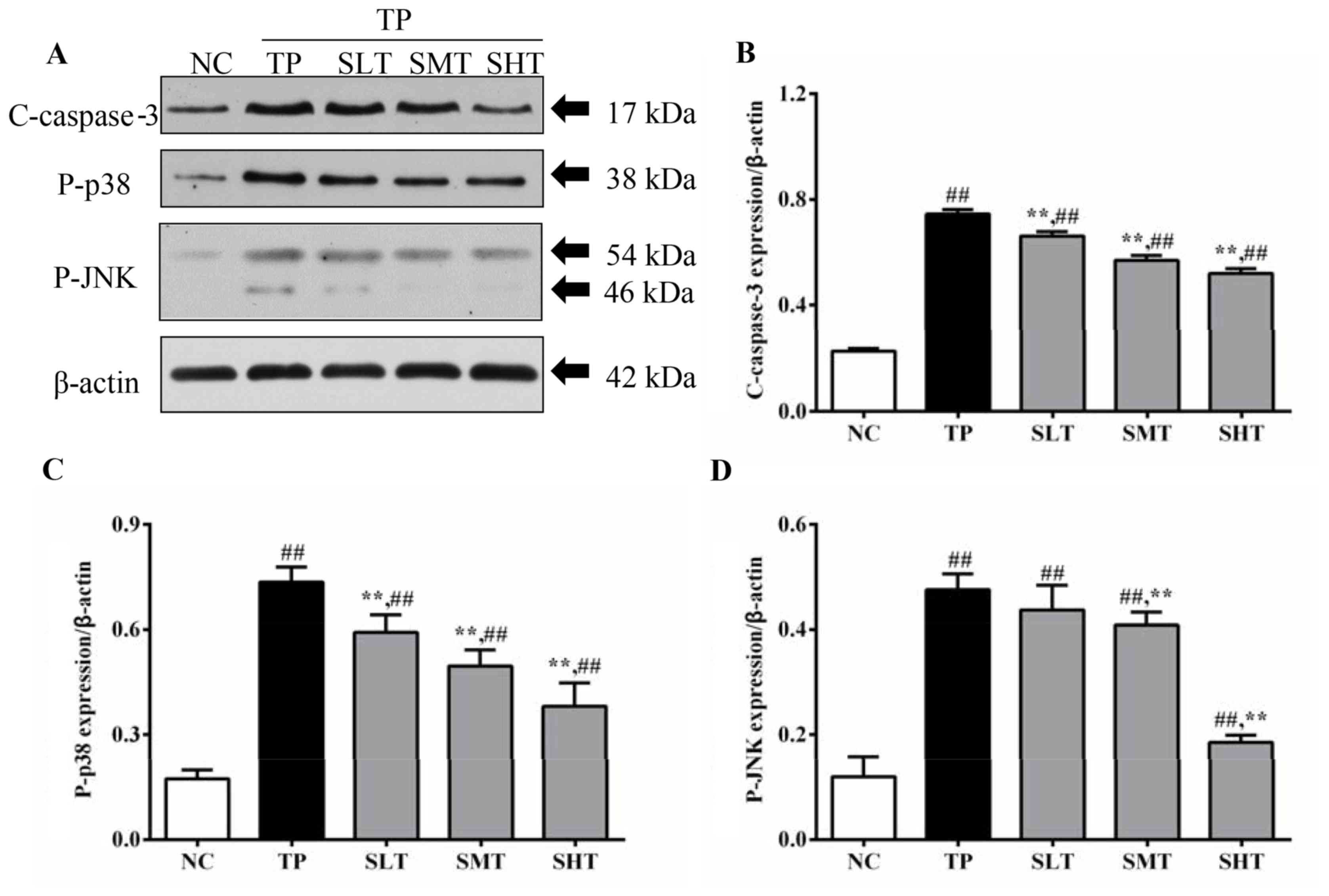
To illustrate the underlying mechanism of silymarin
inhibiting inflammatory responses, the protein expression of key
downstream proteins in the TNF-α pathway, and the
apoptosis-associated protein c-caspase-3, was measured (Fig. 5A). Expression levels of p-p38 in
the TP group were 3.5 times higher compared with the NC group
(P<0.01). However, the overexpression of p-p38 induced by TP was
reduced by 20.04, 33.11 and 48.44% in silymarin treated groups in a
dose-dependent manner (Fig. 5B). A
similar inhibitory effect of silymarin was also observed in the
expression of p-JNK. The level of p-JNK in TP group was three times
higher compared with the NC group (P<0.01). In silymarin
pretreated groups, the level of p-JNK decreased by 8.82, 14.93 and
61.46% in low, middle and high-dose groups, respectively, compared
with the TP group (Fig. 5C).
Therefore, the results indicated that silymarin, particularly at
100 and 200 mg/kg, significantly inhibited the phosphorylation of
inflammatory mediators that are induced by TNF-α. In addition, the
protein expression of c-caspase-3, a protein associated with
apoptosis, was also determined by western blot analysis. Following
TP injection, the level of c-caspase-3 in the TP group was 2.24
times higher compared with the NC group (P<0.01). In
silymarin-treated groups, the expression level of c-caspase-3 was
significantly decreased by 10.55, 22.93 and 29.73% in silymarin
low, middle and high-dose groups, respectively, compared with the
TP group (P<0.01; Fig. 5D).
These results indicate that silymarin may also exert antiapoptotic
effects in the liver of TP-treated rats.
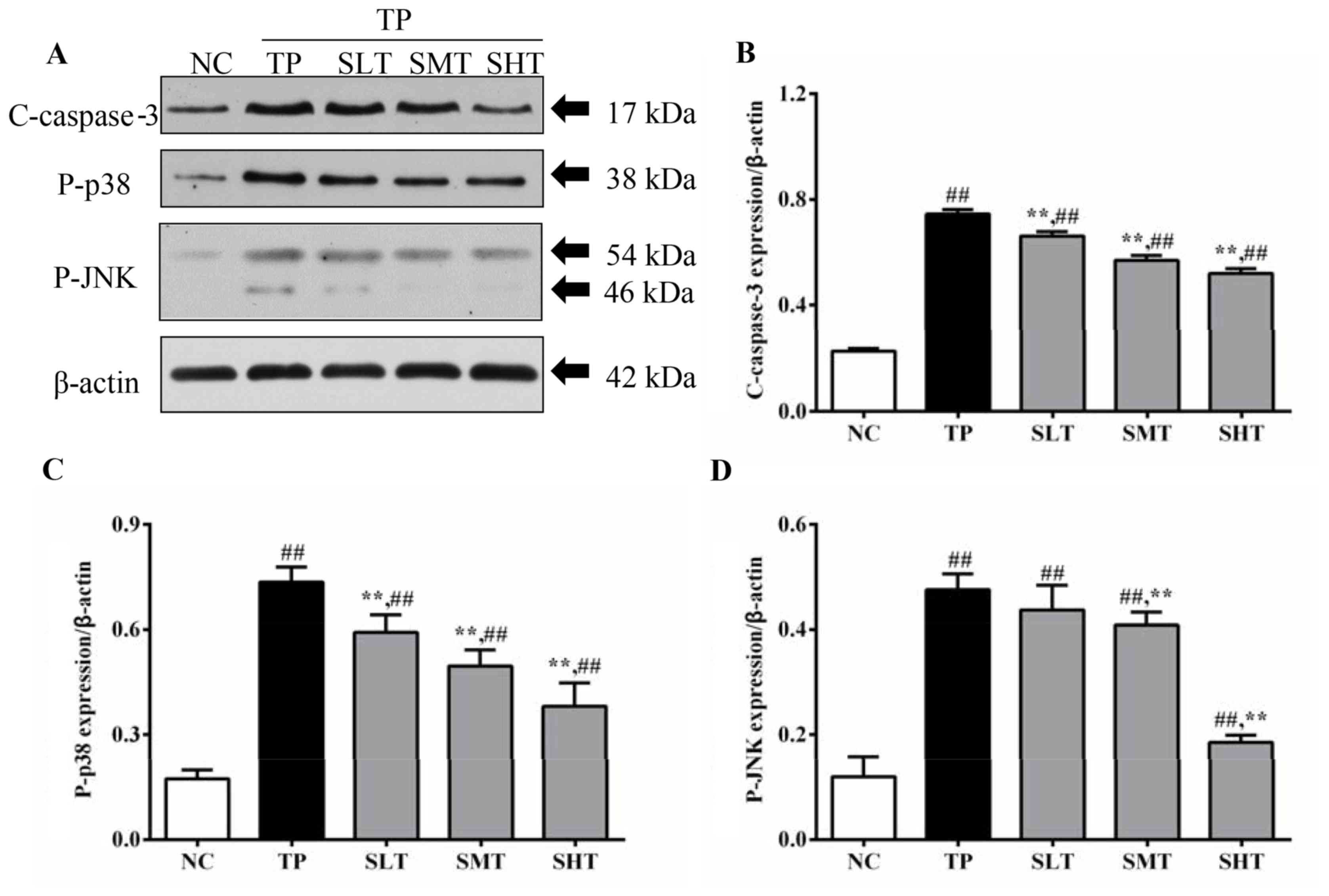 | Figure 5.Effects of silymarin on the protein
expression c-caspase-3, p-p38 and p-JNK. (A) Representative western
blot analysis of c-caspase-3, p-p38 and p-JNK expression.
Densitometric analysis was performed to quantify the expression
levels of (B) p-p38, (C) p-JNK and (D) c-caspase-3 in different
treatment groups. Data are presented as the mean ± standard
deviation, n=6. ##P<0.01 vs. NC group; **P<0.01
vs. TP group. c-caspase, cleaved-caspase; p, phosphorylated; JNK,
c-Jun N-terminal kinase; NC, normal control; TP, triptolide; SLT,
low-dose silymarin treatment; SMT, middle-dose silymarin treatment;
SHT, high-dose silymarin treatment. |
Silymarin inhibits hepatocyte
apoptosis
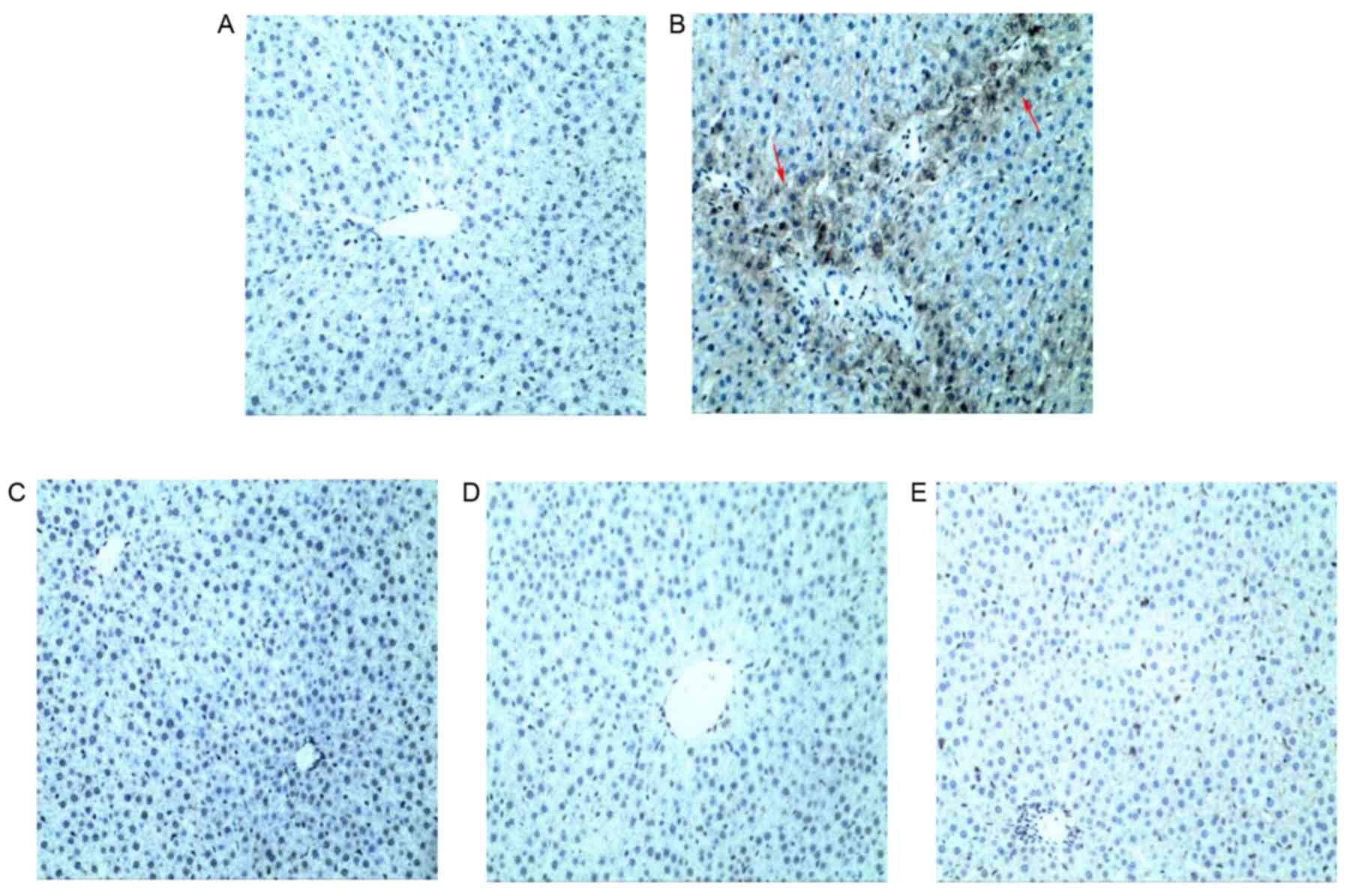
The apoptosis rates of different treatment groups
were detected using TUNEL staining and quantified by ImageJ
software, and representative photographs were taken under a light
microscope. As demonstrated in Fig.
6, TP administration resulted in numerous TUNEL-positive
hepatocytes and a significantly higher apoptotic index compared
with the NC group (Table II),
indicating the induction of severe hepatic apoptosis within 24 h of
treatment with TP. However, fewer TUNEL-positive hepatocytes and
significantly decreased apoptotic indexes (P<0.01) were observed
in livers pretreated with silymarin compared with the TP group,
indicating that silymarin pretreatment may protect the liver
against TP-induced hepatic injury. Notably, high-dose silymarin
pretreatment exhibited a superior effect in inhibiting the cell
apoptosis. These results indicated that silymarin may effectively
ameliorate the hepatocyte apoptosis induced by TP.
 | Table II.Positive rates for TUNEL analysis,
Bcl-2 and Bax immunohistochemistry, Bax/Bcl-2 expression ratio and
Cyt C content in the liver tissue of different treatment
groups. |
Table II.
Positive rates for TUNEL analysis,
Bcl-2 and Bax immunohistochemistry, Bax/Bcl-2 expression ratio and
Cyt C content in the liver tissue of different treatment
groups.
| Group | Cyt C (nmol/l) | TUNEL (%) | Bcl-2 (%) | Bax (%) | Bax/Bcl-2
ratio |
|---|
| NC |
105.8±9.2 |
8.5±0.3 |
28.5±1.1 |
7.2±0.7 |
0.27±0.1 |
| TP |
290.6±10.3a |
30.6±1.0a |
29.6±0.6 |
34.9±1.1a |
1.19±0.2a |
| SLT |
235.0±10.6b |
15.9±0.7b |
28.2±0.9 |
19.0±0.9b |
0.68±0.1b |
| SMT |
191.4±9.8b |
12.9±0.8b |
28.4±0.8 |
10.0±0.7b |
0.37±0.1b |
| SHT |
156.9±6.5b |
10.6±0.4b |
29.0±0.5 |
3.7±0.5b |
0.14±0.1b |
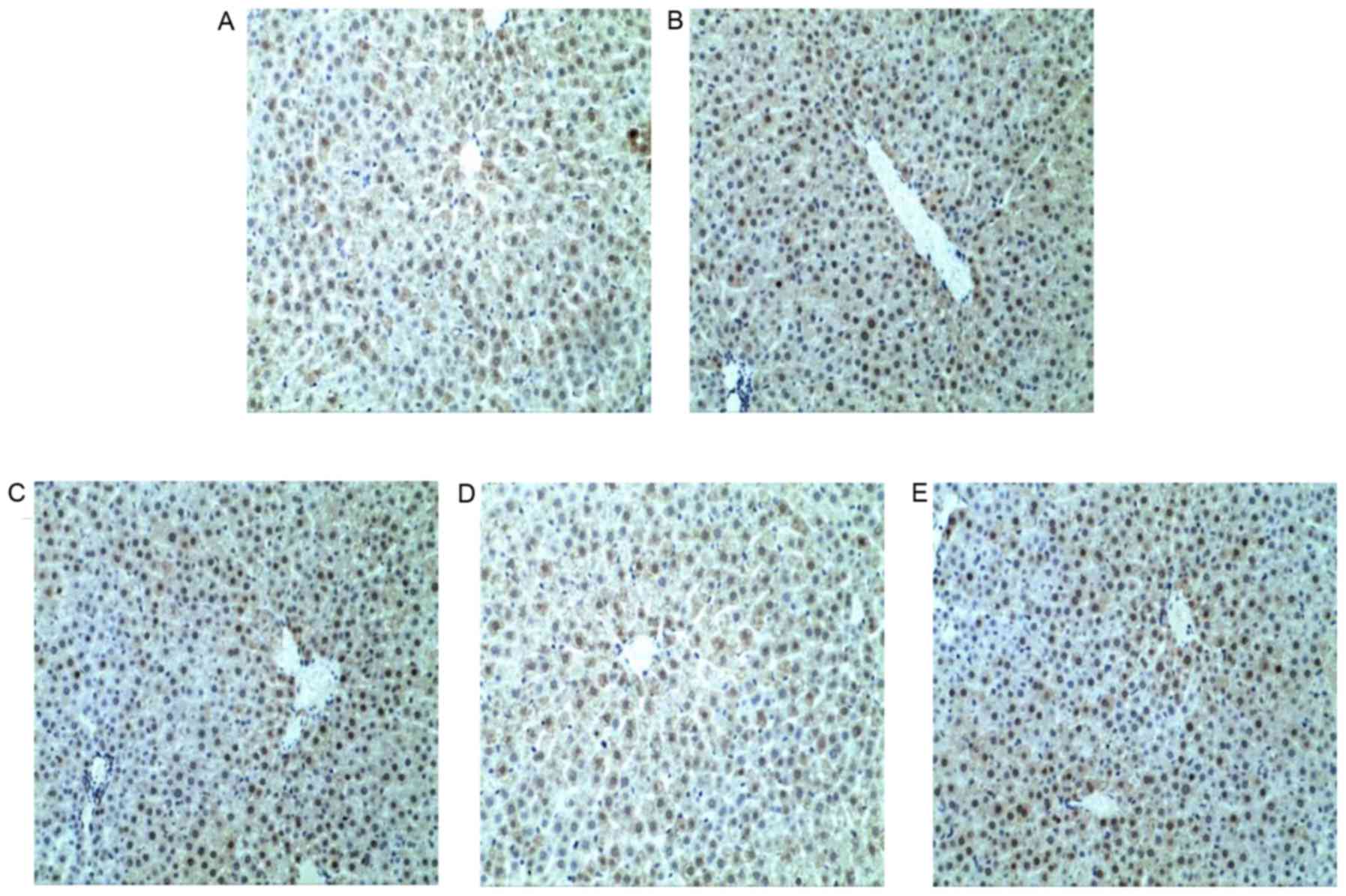
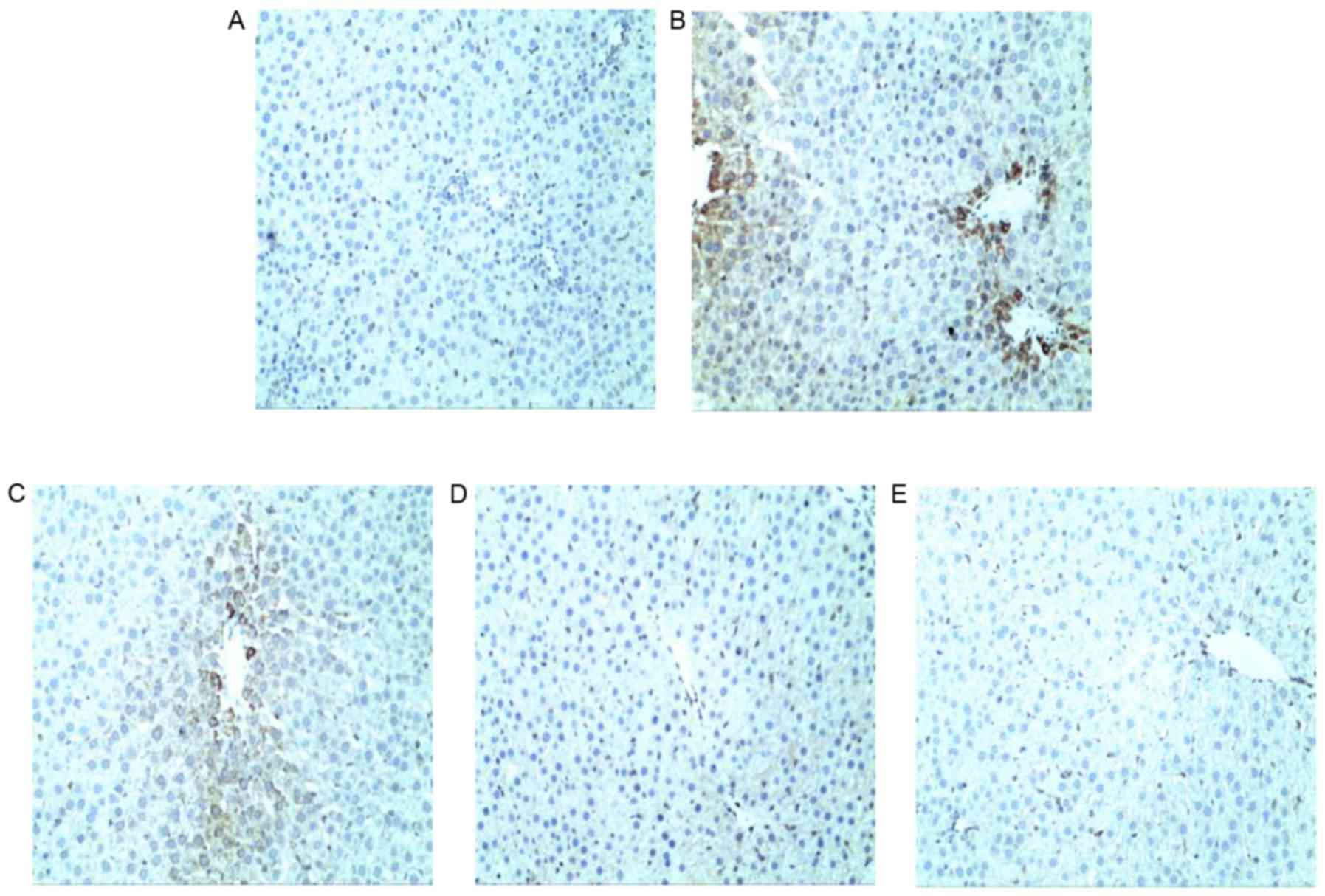
Effects of silymarin on the expression
of apoptosis-associated proteins
Representative photographs of different treatment
groups were taken under a light microscope. The positive rates were
calculated by ImageJ software based on 15 images of each group. No
significant alterations in the expression of the antiapoptotic
protein Bcl-2 were observed between NC, TP and silymarin treatment
groups (Fig. 7 and Table II). By contrast, the expression of
the proapoptotic protein Bax was significantly higher in the TP
group compared with the NC group (P<0.01; Fig. 8 and Table II). However, silymarin
significantly inhibited the expression of Bax and, therefore, the
ratio of Bax/Bcl-2 was also lowered, compared with the TP group in
a dose-dependent manner (P<0.01; Fig. 8 and Table II). As described above for western
blot results, the changes in the levels of c-caspase-3 exhibited a
similar pattern to Bax expression (Fig. 5). Furthermore, Cyt C levels in
supernatants were measured by ELISA, and levels were significantly
increased in the TP group compared with the NC group (P<0.01;
Table II). However, silymarin
pretreatment was observed to progressively reduce hepatic Cyt C
levels in a dose-dependent manner compared with the TP group
(P<0.01). These results are consistent with those for TUNEL
staining and c-caspase-3 protein expression, indicating that an
antiapoptotic effect may contribute to the protective action of
silymarin in the liver of TP-treated rats.
Discussion
The liver has a vital role in drug metabolism and is
a target organ that is affected by toxicants (23). TWHF, TP and their preparations have
been widely used for autoimmune and inflammatory diseases with
pronounced efficacy. Unfortunately, their application has been
increasingly restricted due to their potential adverse effects and
acute toxicity, particularly hepatic toxicity. To date, various
studies have been performed with the aim of identifying strategies
to reduce the side effects of these agents (24–26).
However, counteractive therapeutic approaches against TP-induced
hepatotoxicity are yet to be established. Therefore, the
development of effective strategies to counteract TP toxicity is
urgently required. Certain herbal drugs, including Glycyrrhiza
glabra L. (27), Curcuma
longa L. (28) and Salvia
miltiorrhiza Bunge (29), have
been demonstrated to improve the regeneration of liver cells, which
accelerates the healing process, and are therefore commonly
employed in the management of various liver disorders. It is
thought that Silybum marianum has been applied extensively
for more than 2,000 years as a natural hepatoprotective agent for
the treatment of hepatic diseases, including hepatitis and
cirrhosis, and to protect the liver from toxic substances (10,30).
At present, silymarin, the major active component of Silybum
marianum, is a major ingredient in a variety of pharmaceutical
preparations, Chinese and Western, that are used to treat liver
dysfunction (12). The present
study provides additional evidence to support our hypothesis that
silymarin pretreatment may prevent TP-induced hepatotoxicity, which
may occur by ameliorating oxidative stress, elevating antioxidant
enzymes activities, and inhibiting lipid peroxidation, the
inflammatory response and apoptosis.
Alterations in serum biochemical parameters and
histological structure are directly indicative of pathological
status in liver. Excessive levels of serum AST, ALT, ALP, TC and
GGT, which are released from damaged hepatocytes into bloodstream,
are associated with severe liver dysfunction in clinical practice
(31). In the present study, a
single administration of TP led to severe liver injury in rats in
the TP group, as evidenced by significant increases in serum AST,
ALT, ALP, TC and GGT compared with the NC group, which was
consistent with previous studies (32,33).
The results of the presents study also demonstrated that silymarin
pretreatment significantly reduced TP-induced increases in the
levels of these parameters, indicating improvements in hepatic
function. Increases in these serum biomarkers were further
validated by histopathological examination. TP caused obvious
damage to the hepatic architecture and led to serious pathological
abnormalities, including vacuole formation, inflammatory
infiltration and focal necrosis. However, pretreatment with
silymarin markedly reduced the presence of deteriorated hepatic
cells. Hepatoprotective effects of silymarin were evidenced by the
absence of cellular necrosis and inflammation in the liver section,
particularly in rats treated with middle and high-dose
silymarin.
Oxidative stress is a primary contributing factor in
several pathological conditions, such as TP-induced liver injury,
as it negatively affects cell membranes and function. Therefore,
application of bioactive substances possessing antioxidative
properties may be effective therapeutic agents for preventing and
treating hepatotoxicity (34). It
has been reported that silymarin functions as an antioxidant by
scavenging oxygen free radicals and decreasing lipid peroxidation
to accelerate hepatocyte regeneration with minimal adverse actions
(35–38). The results of the present study
were consistent with previous studies (39–41).
The activities of antioxidant enzymes, including SOD, CAT, GST and
GSH-Px, were decreased, while MDA production increased in the liver
of rats in the TP group. When endogenous antioxidant systems were
destroyed, an imbalance of oxidation and antioxidation occurred,
which directly or indirectly damaged the intracellular proteins
(42). Therefore, the mechanism of
TP-induced liver injury may be associated with excessive levels of
ROS and peroxides, which leads to induction of oxidative stress and
lipid peroxidation (6). In the
present study, pretreatment with silymarin, particularly high-dose
silymarin, reversed the reduction in antioxidant enzymes activities
to normal levels. These results indicate that silymarin may prevent
TP from binding with hepatic lipids and proteins and thus inhibit
lipid peroxidation and protect antioxidant enzymes. The capacity of
silymarin for trapping free radicals has also been demonstrated in
previous studies (37,43). Antioxidant action and anti-lipid
peroxidation properties may be contributing factors in the
protective effect of silymarin in TP-induced hepatocyte damage.
Inflammation is another important pathological
mechanism that may be involved in TP-induced hepatotoxicity. In a
previous report, TP activated hepatic Kupffer cell external
antibody CD68 to release substantial amounts of TNF-α (44), which causes normal cells to release
IL-6, IL-10 and IL-1β into the bloodstream, and is involved in the
pathogenesis of viral hepatitis, alcoholic or nonalcoholic fatty
liver, and ischemia-reperfusion injury (22,45,46).
TNF-α is one of the transcription factors of the mitogen-activated
protein kinase (MAPK) signaling pathway, which has been reported to
mediate inflammation and apoptosis (47). When triggered by inflammatory
cytokines such as TNF-α, MAPK cascades are initiated via p38 and
JNK pathways to regulate activator protein-1, which subsequently
leads to inflammatory responses and cell apoptosis (48). Phosphorylation of p38 and JNK may
also be induced by oxidative stress, which stimulates the
production of proinflammatory mediators and establishes a vicious
cycle that aggravates hepatic injuries (49). Previous reports have indicated that
silymarin, by acting on a variety of molecular targets, including
cytokines and enzymes (50),
restricts excessive inflammation caused by restraint stress
(22) and alcohol (51). The results of the present study are
consistent with these previous studies. Silymarin effectively
inhibited the protein expression levels of TNF-α, p-p38 and p-JNK,
which was increased significantly by TP injection, and subsequently
led to significant reductions in the production of inflammatory
cytokines (IL-6, IL-10 and IL-1β) and reduced inflammatory
infiltration in middle or high-dose silymarin treatment groups
compared with the TP group. These results indicate that a potential
anti-inflammatory effect of silymarin may also contribute to its
ability to attenuate TP-induced hepatotoxicity.
Rapid secretion of TNF-α may also lead to the
activation of mitochondria-controlled apoptosis, the cascade
reaction that begins with the release of Cyt C due to reduced
mitochondria membrane potential and destruction of the
mitochondrial membrane (52), and
results in the activation of caspase-3. ROS are thought to be
responsible for damaging the mitochondrial membrane and releasing
Cyt C (53). The release of Cyt C
is also regulated by the Bcl-2-family of proteins that are situated
on the mitochondrial membrane, of which Bcl-2 is the most typical
antiapoptotic protein and Bax is the most typical proapoptotic
protein (54). The ratio of
Bcl-2/Bax determines whether a cell survives or undergoes cell
death (54). When Bax expression
is elevated by apoptosis-inducing factors, the reduced ratio leads
to apoptosis. Additionally, JNK is also involved in mitochondrial
intrinsic apoptotic pathways. JNK inhibits the expression of Bcl-2
and stimulates the expression of Bax. These key proteins cooperate
to enhance the speed of apoptosis. Yang et al (55) previously demonstrated that
TP-induced cell apoptosis is closely associated with the imbalance
between Bcl-2 and Bax. Silymarin has been reported to maintain cell
membrane fluidity and promote liver cell repair, which is thought
to combat liver apoptosis (50).
As expected, in the present study, TP-induced increases in the
levels of Cyt C, Bax, JNK and c-caspase-3 were markedly prevented
by silymarin treatment. Although the level of Bcl-2 did not change
significantly between treatment groups, the alterations in the
ratio of Bcl-2/Bax indicated the antiapoptotic effects of silymarin
in a dose-dependent manner. These results were also verified by
TUNEL staining observations. Qualitative and quantitative results
of TUNEL staining demonstrated that the high-dose silymarin group
had fewer TUNEL-positive cells and a lower apoptosis index compared
with the TP group, which confirmed that inhibition of
mitochondrial-controlled apoptosis may be the one of the protective
mechanisms of silymarin against TP-induced hepatotoxicity.
Various studies have demonstrated that TP may be
metabolized to three or four monohydroxylated metabolites,
primarily by cytochrome P450 (CYP)3A4 and CYP3A2, respectively, in
humans or rat liver microsomes during the phase I metabolic pathway
(56–58). Therefore, hydroxylation and
desaturation controlled by CYP3A were hypothesized to have
important roles in TP detoxification (58). Further investigation of this
potential mechanism is required in future studies.
In conclusion, the present study demonstrated that
short-term oral administration of silymarin exerts pronounced
effects in TP-induced liver injury. It was demonstrated to reduce
lipid peroxidation and elevate antioxidant enzyme activity to
enhance hepatic antioxidative defense systems, reduce excessive
expression of proinflammatory cytokines, inhibit inflammatory
signaling and ameliorate cell apoptosis to strengthen liver
vitality. Silymarin exhibited satisfactory dose-dependent effects
in preventing TP-induced hepatotoxicity and improving hepatic
function. These results indicate that silymarin may be a potential
candidate for treating TP-induced hepatotoxicity.
Acknowledgements
The present study was supported by grants from the
Hong Kong, Macao and Taiwan Science and Technology Cooperation
Program of China (grant no. 2014DFH30010), the Science and
Technology Planning Project of Guangdong Province (grant nos.
2013B090800052, 2013B090600007 and 2013B090600026), Guangdong
International Cooperation Project (grant no. 2013508102016) and the
Science and Technology Major Project of Guangdong Province (grant
no. 2012A080205001).
References
|
1
|
Jia L, Feihai S, Cuiwen G, Wenwen W,
Xiaozhe S, Xinlu F, Min H, Jing J and Zhiying H: Activation of Nrf2
protects against triptolide-induced hepatotoxicity. PLoS One.
9:102014.
|
|
2
|
Chen BJ: Triptolide, a novel
immunosuppressive and anti-inflammatory agent purified from a
Chinese herb Tripterygium wilfordii Hook F. Leuk Lymphoma.
42:253–265. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shu B, Duan W, Yao J, Huang J, Jiang Z and
Zhang L: Caspase 3 is involved in the apoptosis induced by
triptolide in HK-2 cells. Toxicol In Vitro. 23:598–602. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Phillips PA, Dudeja V, McCarroll JA,
Borja-Cacho D, Dawra RK, Grizzle WE, Vickers SM and Saluja AK:
Triptolide induces pancreatic cancer cell death via inhibition of
heat shock protein 70. Cancer Res. 67:9407–9416. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mei ZN, Lia XK, Wu QR and Yang XL: The
research on the anti-inflammatory activity and hepatotoxicity of
triptolide-loaded solid lipid nanoparticle. Pharmacol Res.
51:345–351. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fu Q, Huang X, Shu B, Xue M, Zhang P, Wang
T, Liu L, Jiang Z and Zhang L: Inhibition of mitochondrial
respiratory chain is involved in triptolide-induced liver injury.
Fitoterapia. 82:1241–1248. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang J, Liu X..Bhalla K..Kim C.N..Ibrado
A.M..Cai J..Peng T.I..Jones D.P..Wang X.: Prevention of apoptosis
by Bcl-2: Release of Cytochrome c from mitochondria blocked.
Science. 275:1129–1132. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Newmeyer DD: Hot papers-apoptosis-the
release of cytochrome c from mitochondria: A primary site for Bcl-2
regulation of apoptosis by R.M. Kluck, E. Bossy-Wetzel, D.R. Green,
D.D. Newmeyer-Comments. Scientist. 13:16. 1999.
|
|
9
|
Shao LW, Huang LH, Yan S, Jin JD and Ren
SY: Cordycepin induces apoptosis in human liver cancer HepG2 cells
through extrinsic and intrinsic signaling pathways. Oncol Lett.
12:995–1000. 2016.PubMed/NCBI
|
|
10
|
Abenavoli L, Capasso R, Milic N and
Capasso F: Milk thistle in liver diseases: Past, present, future.
Phytother Res. 24:1423–1432. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pascual C, Gonz R, Armesto J and Muriel P:
Effect of silymarin and silybinin on oxygen radicals. Drug Devel
Res. 29:73–77. 1993. View Article : Google Scholar
|
|
12
|
Crocenzi FA and Roma MG: Silymarin as a
new hepatoprotective agent in experimental cholestasis: New
possibilities for an ancient medication. Curr Med Chem.
13:1055–1074. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arafa HMM: Uroprotective effects of
curcumin in cyclophosphamide-induced haemorrhagic cystitis
paradigm. Basic Clin Pharmacol Toxicol. 104:393–399. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Avci H, Tunca R, Epikmen E. T, Birincioğlu
SS, Sekkin SB Murat and Akşit H: Protective and antigenotoxic
effects of Silymarin and Curcumin in experimental cyclophosphamide
intoxication in rats. Kafkas Univ Vet Fak Derg. 22:693–701.
2016.
|
|
15
|
Schuppan D, Jia JD, Brinkhaus B and Hahn
EG: Herbal products for liver diseases: A therapeutic challenge for
the new millennium. Hepatology. 30:1099–1104. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hahn G, Lehmann HD, Kurten M, Uebel H and
Vogel G: On the pharmacology and toxicology of silymarin, an
antihepatotoxic active principle from Silybum marianum (L.)
Gaertn. Arzneimittelforschung. 18:698–704. 1968.PubMed/NCBI
|
|
17
|
Rajasekaran A and Periyasamy M: Synthesis
and evaluation of hepatoprotective activity of some new mannich
bases bearing benztriazole moiety. J Chil Chem Soc. 55:366–370.
2010. View Article : Google Scholar
|
|
18
|
Jia R, Cao LP, Du JL, Xu P, Jeney G and
Yin GJ: The protective effect of silymarin on the carbon
tetrachloride (CCl4)-induced liver injury in common carp
(Cyprinus carpio). In Vitro Cell Dev Biol-Anim. 49:155–161.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pappachan JM, Antonio FA, Edavalath M and
Mukherjee A: Non-alcoholic fatty liver disease: A diabetologist's
perspective. Endocrine. 45:344–353. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Voroneanu L, Nistor I, Dumea R, Apetrii M
and Covic A: Silymarin in type 2 diabetes mellitus: A systematic
review and meta-analysis of randomized controlled trials. J
Diabetes Res. 2016:51474682016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alcaraz-Contreras Y, Mendoza-Lozano RP,
Martínez-Alcaraz ER, Martínez-Alfaro M, Gallegos-Corona MA,
Ramírez-Morales MA and Vázquez-Guevara MA: Silymarin and
dimercaptosuccinic acid ameliorate lead-induced nephrotoxicity and
genotoxicity in rats. Hum Exp Toxicol. 35:398–403. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kim SH, Oh DS, Oh JY, Son TG, Yuk DY and
Jung YS: Silymarin prevents restraint stress-induced acute liver
injury by ameliorating oxidative stress and reducing inflammatory
response. Molecules. 21:4432016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Merrell MD and Cherrington NJ: Drug
metabolism alterations in nonalcoholic fatty liver disease. Drug
Metab Rev. 43:317–334. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li XX, Du FY, Liu HX, Ji JB and Xing J:
Investigation of the active components in Tripterygium
wilfordii leading to its acute hepatotoxicty and
nephrotoxicity. J Ethnopharmacol. 162:238–243. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li XJY, Jiang ZZ and Zhang LY: Triptolide:
Progress on research in pharmacodynamics and toxicology. J
Ethnopharmacol. 155:67–79. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yang GH, Wang L, Yu XT and Chen H:
Protective effect of 18 beta-glycyrrhetinic acid against
triptolide-induced hepatotoxicity in rats. Evid Based Complement
Alternat Med. 2017:34703202017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dastagir G and Rizvi MA: Glycyrrhiza
glabra L. (Liquorice). Pak J Pharm Sci. 29:1727–1733.
2016.PubMed/NCBI
|
|
28
|
Adaramoye OA, Odunewu AO and Farombi EO:
Hepatoprotective effect of Curcuma longa L. in
D-galactosamine induced liver injury in mice: Evidence of
antioxidant activity. Afr J Med Med Sci. Suppl 39:S27–S34.
2010.
|
|
29
|
Wan JM, Sit WH, Lee CL, Fu KH and Chan DK:
Protection of lethal toxicity of endotoxin by Salvia
miltiorrhiza BUNGE is via reduction in tumor necrosis factor
alpha release and liver injury. Int Immunopharmacol. 6:750–758.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wellington K and Jarvis B: Silymarin: A
review of its clinical properties in the management of hepatic
disorders. Biodrugs. 15:465–489. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Singh H, Sidhu S, Chopra K and Khan MU:
Hepatoprotective effect of trans-Chalcone on experimentally induced
hepatic injury in rats: Inhibition of hepatic inflammation and
fibrosis. Can J Physiol Pharmacol. 94:879–887. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ali MHH, Messiha BAS and Abdel-Latif HAT:
Protective effect of ursodeoxycholic acid, resveratrol, and
N-acetylcysteine on nonalcoholic fatty liver disease in rats. Pharm
Biol. 54:1198–1208. 2016.PubMed/NCBI
|
|
33
|
Xing H, Jia K, He J, Shi C, Fang M, Song
L, Zhang P, Zhao Y, Fu J and Li S: Establishment of the Tree Shrew
as an alcohol-induced fatty liver model for the study of alcoholic
liver diseases. PLoS One. 10:122015. View Article : Google Scholar
|
|
34
|
Cao LJ, Li HD, Yan M, Li ZH, Gong H, Jiang
P, Deng Y, Fang PF and Zhang BK: The protective effects of
isoliquiritigenin and glycyrrhetinic acid against
triptolide-induced oxidative stress in HepG2 cells involve Nrf2
activation. Evid Based Complement Alternat Med. 2016:89121842016.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Saller R, Meier R and Brignoli R: The use
of silymarin in the treatment of liver diseases. Drugs.
61:2035–2063. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Surai PF: Silymarin as a natural
antioxidant: An overview of the current evidence and perspectives.
Antioxidants (Basel). 4:204–247. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Feng B, Meng R, Huang B, Shen SM, Bi Y and
Zhu DL: Silymarin alleviates hepatic oxidative stress and protects
against metabolic disorders in high-fat diet-fed mice. Free Radic
Res. 50:314–327. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhang W, Hong RT and Tian TL: Silymarin's
protective effects and possible mechanisms on alcoholic fatty liver
for rats. Biomol Ther. 21:264–269. 2013. View Article : Google Scholar
|
|
39
|
Gu HP, Gu XZ, Xu QT and Kang WY:
Antioxidant activity in vitro and hepatoprotective effect of
Phlomis maximowiczii in vivo. Afr J Tradit Complement Altern
Med. 11:46–52. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Simeonova R, Vitcheva V, Kondeva-Burdina
M, Krasteva I, Manov V and Mitcheva M: Hepatoprotective and
antioxidant effects of saponarin, isolated from Gypsophila
trichotoma Wend. on paracetamol-induced liver damage in rats.
Biomed Res Int. 2013:7571262013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Yuan L, Gu XZ, Yin ZH and Kang WY:
Antioxidant activities in vitro and hepatoprotective effects of
Nelumbo nucifera leaves in vivo. Afr J Tradit Complement Altern
Med. 11:85–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Farrell GC: Drugs and steatohepatitis.
Semin Liver Dis. 22:185–194. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Desplaces A, Choppin J, Vogel G and Trost
W: The effects of silymarin on experimental phalloidine poisoning.
Arzneimittel-Forschung. 25:89–96. 1975.PubMed/NCBI
|
|
44
|
Woo K, Stewart SG, Kong GS,
Finch-Edmondson ML, Dwyer BJ, Yeung SY, Abraham LJ, Kampmann SS,
Diepeveen LA, Passman AM, et al: Identification of a thalidomide
derivative that selectively targets tumorigenic liver progenitor
cells and comparing its effects with lenalidomide and sorafenib.
Eur J Med Chem. 120:275–283. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Imanishi H, Scales WE and Campbell DA:
Tumor necrosis factor alpha alters the cytotoxic effect of hydrogen
peroxide in cultured hepatocytes. Biochem Biophys Res Commun.
230:120–124. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Auguet T, Vidal F, López-Dupla M, Broch M,
Gutiérrez C, Olona M, Oltra C, Aguilar C, González E, Quer JC, et
al: A study on the TNF-alpha system in Caucasian Spanish patients
with alcoholic liver disease. Drug Alcohol Depend. 92:91–99. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Kim EK and Choi EJ: Pathological roles of
MAPK signaling pathways in human diseases. Biochim Biophys Acta.
1802:396–405. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Herlaar E and Brown Z: p38 MAPK signalling
cascades in inflammatory disease. Mol Med Today. 5:439–447. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Jaeschke H: Reactive oxygen and mechanisms
of inflammatory liver injury: Present concepts. J Gastroenterol
Hepatol. 26:173–179. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jin YW, Zhao X, Zhang H, Li QS, Lu GD and
Zhao XG: Modulatory effect of silymarin on pulmonary vascular
dysfunction through HIF-1 alpha-iNOS following rat lung
ischemia-reperfusion injury. Exp Ther Med. 12:1135–1140. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zholobenko A and Modriansky M: Silymarin
and its constituents in cardiac preconditioning. Fitoterapia.
97:122–132. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Volbracht C, Leist M, Kolb SA and Nicotera
P: Apoptosis in caspase-inhibited neurons. Mol Med. 7:36–48.
2001.PubMed/NCBI
|
|
53
|
Wu D and Cederbaum AI: Oxidative stress
and alcoholic liver disease. Semin Liver Dis. 29:141–154. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Kuwana T and Newmeyer DD: Bcl-2-family
proteins and the role of mitochondria in apoptosis. Curr Opin Cell
Biol. 15:691–699. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yang F, Zhuo L, Ananda S, Sun TY, Li SX
and Liu L: Role of reactive oxygen species in triptolide-induced
apoptosis of renal tubular cells and renal injury in rats. J
Huazhong Univ Sci Technolog Med Sci. 31:335–341. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Tai T, Huang X, Su YW, Ji J, Su Y, Jiang Z
and Zhang L: Glycyrrhizin accelerates the metabolism of triptolide
through induction of CYP3A in rats. J Ethnopharmacol. 152:358–363.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Han FM, Peng ZH, Wang JJ and Chen Y: In
vivo effect of triptolide combined with glycyrrhetinic acid on rat
cytochrome P450 enzymes. Yao Xue Xue Bao. 48:1136–1141.
2013.PubMed/NCBI
|
|
58
|
Ye X, Li W, Yan Y, Mao C, Cai R, Xu H and
Yang X: Effects of cytochrome P4503A inducer dexamethasone on the
metabolism and toxicity of triptolide in rat. Toxicol Lett.
192:212–220. 2010. View Article : Google Scholar : PubMed/NCBI
|