Introduction
Gout is a common form of arthritis associated with
pain, fatigue and high fever (1).
According to epidemiological studies, the incidence of gout
increased from 1.42% in 1997 to 2.49% in 2012 in Britain (2), which is partly influenced by dietary
changes and age (3).
Hyperuricemia, defined as a level of serum uric acid (UA) >6.8
mg/dl, is caused by the overactivation of xanthine oxidase (XO)
following excessive purine intake (4,5).
High levels of UA contribute to the deposition of monosodium urate
(MSU) in joints and other tissues (6). The deposition of MSU in the joint
cavity activates inflammatory cytokines, inducing the accumulation
of macrophages and neutrophils, which leads to gouty arthritis
(7,8). Oxidative stress serves an important
role in the pathogenesis of gout (9) and is responsible for a series of
inflammatory events (10), such as
the production of interleukin (IL)-1β (11).
Based on the pathogenesis of gout, inhibiting
inflammation and lowering the serum UA level are considered to be
effective treatment strategies. Colchicine (COL), corticosteroids
and non-steroidal anti-inflammatory drugs are commonly used in the
treatment of gouty arthritis (12,13).
Allopurinol and febuxostat (FBX) are the main clinical agents for
treating hyperuricemia (14,15).
However, a number of adverse effects have been reported, including
liver damage, nephrotoxicity, bone marrow suppression and
hypersensitive bodily reactions (14–16).
It is therefore particularly important to find alternative
treatment agents for hyperuricemia and gouty arthritis.
Natural products have received increasing attention
in clinical applications owing to their diverse efficacies and low
adverse effects (17). Celery is
an annual or perennial umbelliferous plant widely distributed in
subtropical and tropical regions of Europe, Africa and Asia
(18). Celery has exhibited
antifungal, anti-inflammatory and anti-gastric ulcer effects in
rodents, and may lower blood pressure in patients with hypertension
(19–23). n-Butanol extracts from celery seeds
have been reported to improve lipid peroxidation through
antioxidation in diabetic rats (24). Methanol and petroleum extracts from
celery seeds reduced blood UA levels in rats (25). However, the antioxidant and
anti-inflammatory activities of celery seeds, especially their
aqueous extracts and volatile oil, have not been fully reported in
gout.
Rats with acute gouty arthritis, which was induced
by MSU to simulate acute gout in humans, have been used to
investigate the effects of various agents on joint swelling and
inflammation (26). Mice with
hyperuricemia, which was induced by yeast extract powder and
potassium oxonate (OXO) to simulate hyperuricemia in humans, have
been used to investigate compounds that lower UA level (27). Based on our previous study, the two
animal models can be used together to investigate the anti-gout
activity of various compounds (28). The aim of the present study was to
systematically analyze the main components of the aqueous extract
and volatile oil of celery seeds and to determine their anti-gout
effects in mice with hyperuricemia and rats with acute gouty
arthritis. The specific roles of the antioxidant and
anti-inflammatory activities of the aqueous extract and volatile
oil of celery seeds were also investigated.
Materials and methods
Preparation of celery seed aqueous and
oil extracts using supercritical carbon dioxide
To prepare celery seed aqueous extract (CSAE), 30 g
celery seed powder (Changchun Yonglong Food Co., Ltd.) was added to
300 ml distilled water and heated at 80°C for 2.5 h twice. The
supernatants from different samples were collected by
centrifugation at 7,100 × g, at 20°C for 10 min and pooled
together. CSAE powder was prepared using a R206 rotary evaporator
spray drier (Shanghai Senco Technology Co., Ltd.). The extraction
rate of CSAE was 10.0±0.5% (w/w).
To prepare celery seed oil extract (CSOL), 300 g
celery seed powder was placed in a HA221-50-06 supercritical carbon
dioxide extraction system (Nantong Wenao Import And Export Co.,
Ltd.) under the following conditions: 35°C and 25 MPa in the
extraction tank; 40°C and 8 MPa in the first separation; and 30°C
and 6 MPa in the second separation. The extraction period was 2 h,
and the oil was collected every 15 min. The extraction rate of CSOL
using supercritical carbon dioxide was 7.8±0.3% (w/w).
Composition analysis of CSAE and
CSOL
Main components analysis
The main components of CSAE powder, including total
sugar, mannitol, reducing sugar, protein, crude fat, total
flavonoids and total triterpenes were determined, as previously
described, by the phenol sulfuric acid method (29), high-performance liquid
chromatography (30),
3,5-dintrosalicylic acid reducing sugar assay (31), Kjeldahl method (32), Soxhlet extractor method (33), aluminum trichloride colorimetric
method (34) and vanillin-glacial
acetic acid-perchloric acid colorimetric method (35), respectively.
Fatty acid analysis
A 5% KOH-methanol solution was added to the CSAE
powder or CSOL, incubated in a 60°C water bath for 30 min and mixed
with 14% BF3-methanol solution at 60°C for 3 min. The
samples were mixed with hexane and the levels of fatty acids were
analyzed using a QP2010 gas chromatography-mass spectrometer
(Shimadzu Corporation). GC was performed using high-pressure-55%
phenyl methyl siloxane chromatographic column (30×0.32
mm2; diameter, 0.25 µm). The sample inlet temperature
was set at 270°C, and the column temperature at 100°C. The heating
rate was set at 10°C/min to 170°C, and at 3°C/min to 250°C. The
carrier gas used was helium, with a flow rate of 2.4 ml/min at 0.4
MPa. For mass spectrometry, electron positive ionization was used
as ion source, and the transition was m/z 380.0→20.0, the
temperature of ion source was 200°C, the interface temperature was
250°C, the solvent removal time was 1.5 min, and the detector
voltage was 1.14 kV.
Amino acid analysis
The CSAE powder and CSOL were hydrolyzed with 6
mol/l HCl at 110±1°C for 22 h. Following vacuum drying, the samples
were dissolved in 1 ml pH 2.2 buffer (19.6 g sodium citrate and
16.5 ml hydrochloric dissolved in 1 l of deionized water; pH 2.2).
The amino acid content was quantified by an L-8900 automatic amino
acid analyzer (Hitachi High-Technologies Corporation).
Mineral analysis
The CSAE powder was pretreated with hydrogen nitrate
110°C and 3 MPa for 30 min. The levels of mercury, lead, selenium,
arsenic, cadmium, zinc, iron, manganese, chromium, calcium, copper,
sodium and potassium were detected by inductively coupled plasma
optical emission spectrometry as previously described (36–38).
Flavonoid analysis
The flavonoid content of CSOL was analyzed using the
Agilent 1260 LC system with a diode array detector-fluorescence
detector and a C-18 column (150×4.6 mm; particle size, 5 µm)
(Agilent Technologies, Inc.) with the injection volume of 10 µl and
the flow rate of 1 ml/min by elution containing 98% methanol and 2%
ultrapure water at 20°C. The standards were obtained from Shanghai
Yuanye Bio-Technology Co. Ltd.
Animal experiments
The working concentrations of FBX and COL were
selected according to previous studies (39,40).
Celery seed treatment doses were selected following preliminary
experiments (data not shown).
Establishment of mouse hyperuricemia
model and drug treatment
A total of 120 male BALB/c mice (age, 8 weeks;
weight, 18–20 g) were provided by Liaoning Changsheng Biotechnology
Co., Ltd. All mice were housed in plastic cages at 23±1°C with 55%
relative humidity, a 12-h light/dark cycle (7:00-19:00) and
standard food and sterile mineral water ad libitum.
Mice were divided into two main groups: i) To
investigate CSAE (AE); and ii) to investigate CSOL (OL). Mice used
as control to examine CSAE were defined as ‘CTRL (AE)’ mice; mice
used as control to examine CSOL were defined as ‘CTRL (OL)’ mice. A
total of 60 mice were randomly divided into 5 groups (n=12
mice/group): i) Control [CTRL (AE)] mice group, which received 10
ml/kg saline by gavage; ii) hyperuricemia model mice [MC (AE)]
group, which received 10 ml/kg saline by gavage; iii) positive
control [FBX (AE)] group, which were MC mice that received 0.6
mg/ml FBX (Jiangsu Wanbang Biochemical Pharmaceutical Group Co.,
Ltd.) at 10 ml/kg by gavage; iv) low-dose CSAE-treated model
(CSAE-low) group, which received 75 mg/kg CSAE (equal to 0.75 g
celery seed) dissolved in 10 ml saline by gavage; and v) high-dose
CSAE-treated model (CSAE-high) group, which received 300 mg/kg
(equal to 3 g celery seed) dissolved in 10 ml saline by gavage.
CTRL (AE), MC (AE) and FBX (AE) were used as untreated control,
model control and positive control groups, respectively, in the
experiments analyzing the effects of CSAE in hyperuricemia model
mice.
The remaining 60 mice were randomly divided into 5
groups (n=12 mice/group): i) CTRL (OL) group, which received 5
ml/kg of olive oil by gavage; ii) MC (OL) group, which received 5
ml/kg of olive oil by gavage; iii) FBX (OL) group, which comprised
MC mice that received 6 mg/kg FBX dissolved in 5 ml olive oil by
gavage; iv) low-dose CSOL-treated (CSOL-low) model group, which
received 0.058 ml/kg CSOL (equal to 0.75 g celery seed) in 5 ml
olive oil by gavage; and v) high-dose CSOL-treated (CSOL-high)
model group, which received 0.233 ml/kg (equal to 3 g celery seed)
in 5 ml olive oil by gavage. CTRL (OL), MC (OL) and FBX (OL) were
used as untreated control, model control and positive control
groups, respectively, in the experiments analyzing the effects of
CSOL in hyperuricemia model mice.
With the exception of the CTRL mice, 12 h prior to
the oral administration of the aforementioned agents (saline, olive
oil, FBX, CSAE or CSOL), 20 g/kg yeast extract powder was
administered by gavage to the mice once a day for 8 days. On day 6,
7 and 8, 1 h prior to the oral administration of the aforementioned
agents, mice were intraperitoneally injected with 300 mg/kg OXO
(Sigma-Aldrich; Merck KGaA) to induce hyperuricemia (28); the CTRL mice were injected with
0.9% saline following the same schedule. During the 8 days, the
aforementioned agents (saline, olive oil, FBX, CSAE, CSOL or COL)
were administered every day. On day 8, after the last
administration of the agents, over 150 µl of blood were collected
from the caudal vein of all mice, and then the mice were
sacrificed. Liver samples were collected from all mice post mortem.
In summary, yeast extract powder was administered by gavage once a
day.
Establishment of rat acute gouty
arthritis model and drug treatment
A total of 120 male Wistar rats (age, 8 weeks;
weight, 180–220 g) were obtained from Liaoning Changsheng
Biotechnology Co., Ltd. All rats were housed in plastic cages at
23±1°C with 55% relative humidity, a 12-h light/dark cycle
(7:00-19:00) and ad libitum access to standard food and
mineral water.
A total of 60 rats were randomly divided into 5
groups (n=12 rats/group): i) CTRL (AE) group, which received 5
ml/kg saline by gavage for 8 days; ii) rat gouty arthritis MCr
(AE), which receive 5 ml/kg saline by gavage for 8 days; iii)
positive control [COL (AE)] model group, which received 0.4 mg/kg
COL (Yunnan Phytopharmaceutical Co., Ltd.) dissolved in 5 ml saline
by gavage for 8 days; iv) SAE-low group, which received 50 mg/kg
CSAE (equal to 0.5 g celery seed) dissolved in 5 ml saline by
gavage for 8 days; and v) CSAE-high group, which received 200 mg/kg
(equal to 2 g celery seed) dissolved in 5 ml saline by gavage for 8
days. CTRL (AE), MCr (AE) and COL (AE) were used as the untreated
control, model control and positive control groups, respectively,
in the experiments analyzing the effects of CSAE in gouty arthritis
model rats.
The remaining 60 rats were randomly divided into 5
groups (n=12 mice/group): i) CTRL (OL) group, which received 1
ml/kg olive oil by gavage for 8 days; ii) MCr (OL) group, which
received 1 ml/kg olive oil by gavage for 8 days; iii) COL (OL)
group, which was model rats that received 0.4 mg COL dissolved in 1
ml/kg olive oil by gavage for 8 days; iv) CSOL-low group, which
received 0.039 ml CSOL (0.5 g celery seed) dissolved in 0.961 ml/kg
olive oil by gavage for 8 days; and v) CSOL-high group, which
received 0.155 ml CSOL (2 g celery seed) dissolved in 0.845 ml/kg
olive oil by gavage for 8 days. CTRL (OL), MCr (OL) and FBX (OL)
were used as the untreated control, model control and positive
control groups, respectively, in the experiments analyzing the
effects of CSOL in gouty arthritis model rats.
MSU (Sigma-Aldrich; Merck KGaA) suspension was
prepared with sterile water in biological safety cabinets. The
endotoxins in the MSU samples were detected by a commercial kit
(Tachypleus Amebocyte Lysate for Endotoxin Detection Kit; cat. no.
RG025006; Xiamen Bioendo Technology Co., Ltd.) to exclude a
potential effect induced by Endotoxin. On day 6, the rats were
intra-articularly injected with 30 mg/ml MSU to the right ankle
(0.1 ml) at 4:00 PM (28), with
the exception of the CTRL rats, which were injected with 0.9%
saline at the same time.
Following the 8-day treatment, the right ankle
circumferences of all rats were measured using Vernier calipers at
24 and 48 h, and the swelling ratio (%) was calculated as follows:
Swelling ratio (%)=(Ct-C0)/C0,
where Ct is the circumference at time t, and
C0 is the circumference at 0 h. Prior to euthanasia,
blood samples were collected from the caudal vein of the rats.
Biochemical assay
In the hyperuricemia MC mouse model, the serum
levels of UA, and XO, and the liver levels of XO were determined
using an XO Activity Assay kit (cat. no. MAK078; Sigma-Aldrich;
Merck KGaA) and a UA Assay kit (cat. no. MAK077; Sigma-Aldrich;
Merck KGaA) according to the manufacturer's instructions. The serum
levels of reactive oxygen species (ROS; cat. no. 43124), superoxide
dismutase (SOD; cat. no. 43125) and glutathione peroxidase (GSH-Px;
cat. no. 43390) were determined using ELISA kits from Shanghai
Yuanye Bio-Technology Co., Ltd. according to the manufacturer's
instructions.
In the acute gout rat model, the serum levels of
IL-1β (cat. no. 43360), IL-6 (cat. no/41731), IL-10 (cat. no.
41736), monocyte chemoattractant protein 1 (MCP-1; cat. no. 41640)
and tumor necrosis factor α (TNF-α; cat. no. 41721) were determined
by ELISA kits from Shanghai Yuanye Bio-Technology Co. Ltd.
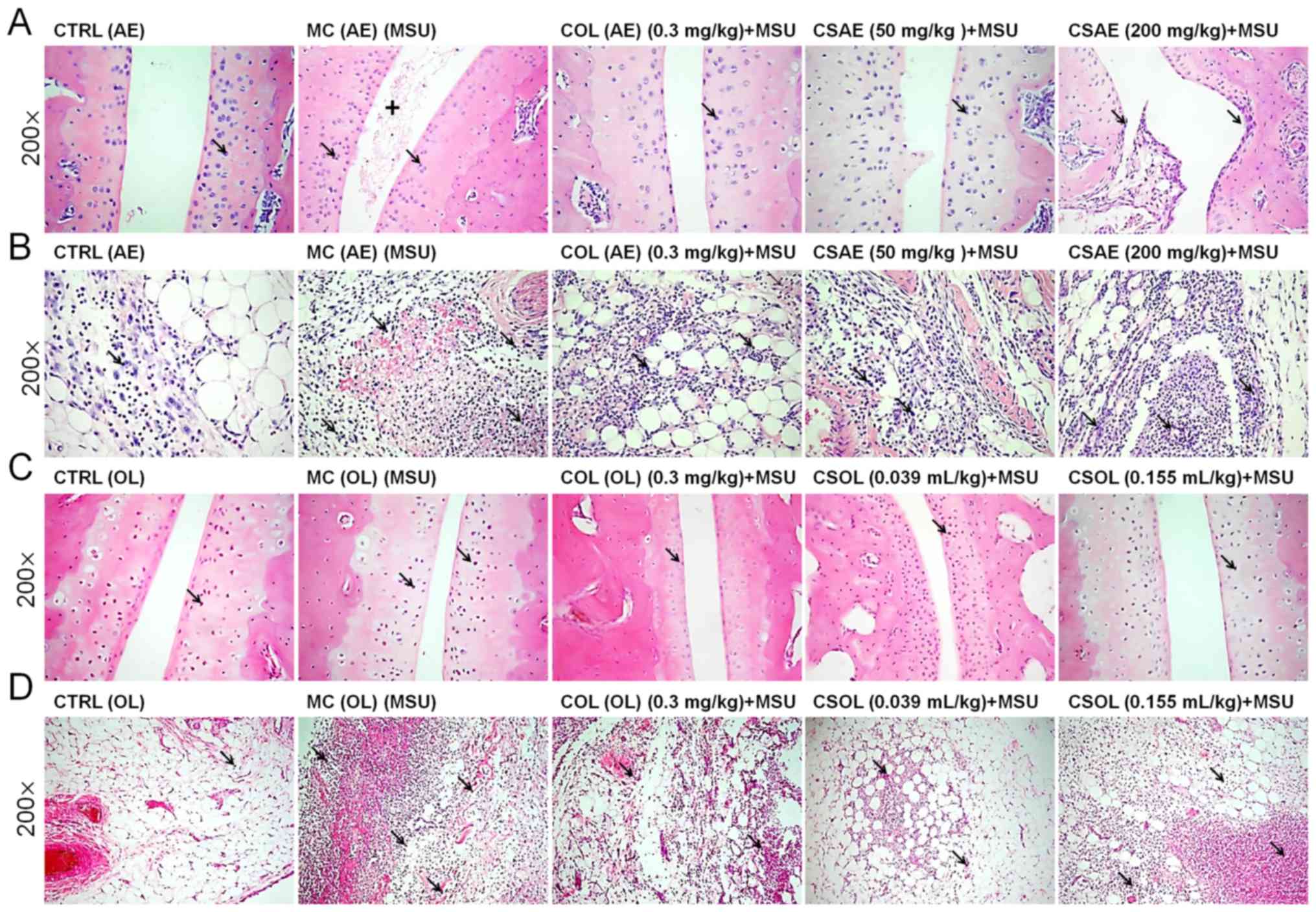
Pathological section of the ankle
joint
The right ankle of each rat was collected, fixed in
4% paraformaldehyde and decalcified with 10%
ethylenediaminetetraacetic acid. Following decalcification and
dehydration via increasing ethanol series, followed by incubation
in 50% of ethanol + 50% dimethylbenzene for 1 h at room
temperature, samples were incubated twice with dimethylbenzene for
20 min at room temperature, the samples were embedded in paraffin,
sliced into 5-µm sections and stained with hematoxylin and eosin
(H&E). The slides were stained with hematoxylin for 5 min at
room temperature and eosin for 3 min at room temperature and
observed under a light microscope (magnification, ×200), and three
fields of view were examined per section.
Statistical analysis
All data are expressed as mean ± SD. Statistical
analysis was performed by one-way analysis of variance followed by
Dunn's multiple comparison post-hoc test using SPSS software
(version 16.0; SPSS, Inc.). P<0.05 was considered to indicate a
statistically significant difference.
Results
Composition of CSAE and CSOL
The CSAE contained 90.3% total sugar, 2.73% reducing
sugar, 0.515% mannitol, 4.66% protein, 0.7% crude fat and 0.014%
total flavonoids (Table I). Among
the 35 types of the detected fatty acids, the contents of C16:0
(0.17%) and C18:2n6c (0.61%) were the highest (Table I). A total of 17 different amino
acids were detected in CSAE (Table
I). The overall mineral content was low, and the solution
contained, among other salts, 0.24% calcium and 0.0022% manganese
(Table I).
 | Table I.Composition of celery seed aqueous
extract. |
Table I.
Composition of celery seed aqueous
extract.
| Component | Compound | Content (%) |
|---|
| Main component | Total sugar | 90.3 |
|
| Total
triterpenes | 0.038 |
|
| Mannitol | 0.515 |
|
| Reducing sugar | 2.73 |
|
| Crude fat | 0.7 |
|
| Protein | 4.66 |
|
| Total
flavonoids | 0.014 |
| Fatty acid | Capric acid
(C10:0) |
2.36×10−4 |
|
| Undecanoic acid
(C11:0) |
0.01×10−4 |
|
| Lauric acid
(C12:0) |
3.16×10−4 |
|
| Tridecanoic acid
(C13:0) | ND |
|
| Myristic acid
(C14:0) |
16.48×10−4 |
|
| Myristoleic acid
(C14:1n5) |
0.41×10−4 |
|
| Pentadecanoic acid
(C15:0) |
3.04×10−4 |
|
| Pentadecenoic acid
(C15:1n5) |
0.11×10−4 |
|
| Hexadecanoic acid
(C16:0) |
1761.24×10−4 |
|
| Palmitoleic acid
(C16:1n7) |
17.08×10−4 |
|
| Heptadecanoic acid
(C17:0) |
6.36×10−4 |
|
| Heptadecenoic acid
(C17:1n7) |
3.43×10−4 |
|
| Stearic acid
(C18:0) |
289.50×10−4 |
|
| Oleic acid
(C18:1n9) | 1
85.10×10−4 |
|
| Elaidic acid
(C18:1n9t) | ND |
|
| Linoleic acid
(C18:2n6c) |
6087.74×10−4 |
|
| Trans-linoleic acid
(C18:2n6t) | ND |
|
| α-linolenic acid
(C18:3n3) |
568.85×10−4 |
|
| γ-Linolenic acid
(C18:3n6) |
103.81×10−4 |
|
| Arachidic acid
(C20:0) |
54.82×10−4 |
|
| Paullinic acid
(C20:1) |
61.99×10−4 |
|
| Eicosadienoic acid
(C20:2) | ND |
|
| Eicosatrienoic acid
(C20:3n3) | ND |
|
| Dihomo-γ-linolenic
acid (C20:3n6) |
98.90×10−4 |
|
| Arachidonic acid
(C20:4n6) |
115.07×10−4 |
|
| Eicosapentaenoic
acid (C20:5n3) |
120.20×10−4 |
|
| Heneicosanoic acid
(C21:0) |
71.64×10−4 |
|
| Docosanoic acid
(C22:0) |
88.04×10−4 |
|
| Erucic acid
(C22:1n9) |
107.84×10−4 |
|
|
cis-13,16-Docosadienoic acid methyl ester
(C22:2) |
119.11×10−4 |
|
| Docosahexaenoic
acid (C22:6n3) | ND |
|
| Tricosanoic acid
(C23:0) |
106.60×10−4 |
|
| Tetracosanoic acid
(C24:0) | ND |
|
| Nervonic acid
(C24:1n9) | ND |
|
| Octanoic acid
(C8:0) |
0.02×10−4 |
| Amino acid | Aspartic acid |
2.38×10−1 |
|
| L-Threonine |
1.68×10−1 |
|
| Serine |
0.22×10−1 |
|
| Glutamic acid |
2.55×10−1 |
|
| Glycine |
1.08×10−1 |
|
| Alanine |
1.32×10−1 |
|
| Cysteine |
3.52×10−1 |
|
| Valine |
0.77×10−1 |
|
| Methionine |
2.00×10−1 |
|
| Isoleucine |
1.17×10−1 |
|
| Leucine |
1.88×10−1 |
|
| Tyrosine |
0.69×10−1 |
|
| Phenylalanine |
15.35×10−1 |
|
| Lysine |
0.89×10−1 |
|
| Histidine |
4.77×10−1 |
|
| Arginine |
0.77×10−1 |
|
| Proline |
3.95×10−1 |
| Minerals | Mercury | ND |
|
| Lead |
0.18×10−4 |
|
| Selenium | ND |
|
| Arsenic |
0.19×10−4 |
|
| Cadmium | ND |
|
| Zinc |
29.94×10−4 |
|
| Iron |
36.16×10−4 |
|
| Manganese |
21.50×10−4 |
|
| Chromium |
1.92×10−4 |
|
| Calcium |
2,426×10−4 |
|
| Copper |
2.05×10−4 |
|
| Sodium |
1,258×10−4 |
|
| Potassium |
8,079×10−4 |
In the CSOL, among the 35 types of the detected
fatty acids, the contents of C18:2n6c (51.74%), C16:0 (9.8%),
C18:3n3 (3.2%), C18:0 (2.4%) and C18:1n9 (1.15%) were the highest.
Of the 17 amino acids identified in CSAE, only nine were detected
in CSOL. The total flavonoid content in CSOL was 0.03%, which
included seven distinct flavonoids, including naringenin, quercetin
and taxifolin (Table II).
 | Table II.Composition of celery seed oil
extract. |
Table II.
Composition of celery seed oil
extract.
| Component | Compound | Content (%) |
|---|
| Fatty acid | Capric acid
(C10:0) |
0.118×10−2 |
|
| Undecanoic acid
(C11:0) |
0.029×10−2 |
|
| Lauric acid
(C12:0) |
1.315×10−2 |
|
| Tridecanoic acid
(C13:0) |
0.059×10−2 |
|
| Myristic acid
(C14:0) |
9.120×10−2 |
|
| Myristoleic acid
(C14:1n5) |
0.013×10−2 |
|
| Pentadecanoic acid
(C15:0) |
1.033×10−2 |
|
| Pentadecenoic acid
(C15:1n5) |
0.049×10−2 |
|
| Hexadecanoic acid
(C16:0) |
983.766×10−2 |
|
| Palmitoleic acid
(C16:1n7) |
8.086×10−2 |
|
| Heptadecanoic acid
(C17:0) |
4.521×10−2 |
|
| Heptadecenoic acid
(C17:1n7) |
3.506×10−2 |
|
| Stearic acid
(C18:0) |
242.853×10−2 |
|
| Oleic acid
(C18:1n9) |
115.324×10−2 |
|
| Elaidic acid
(C18:1n9t) | ND |
|
| Linoleic acid
(C18:2n6c) |
5,174.071×10−2 |
|
| Trans-linoleic acid
(C18:2n6t) | ND |
|
| α-linolenic acid
(C18:3n3) |
320.313×10−2 |
|
| γ-Linolenic acid
(C18:3n6) |
0.436×10−2 |
|
| Arachidic acid
(C20:0) |
21.331×10−2 |
|
| Paullinic acid
(C20:1) |
6.764×10−2 |
|
| Eicosadienoic acid
(C20:2) |
1.579×10−2 |
|
| Eicosatrienoic acid
(C20:3n3) |
0.435×10−2 |
|
| Dihomo-γ-linolenic
acid (C20:3n6) |
0.114×10−2 |
|
| Arachidonic acid
(C20:4n6) |
1.543×10−2 |
|
| Eicosapentaenoic
acid (C20:5n3) |
0.035×10−2 |
|
| Heneicosanoic acid
(C21:0) |
1.082×10−2 |
|
| Docosanoic acid
(C22:0) |
21.793×10−2 |
|
| Erucic acid
(C22:1n9) |
0.257×10−2 |
|
|
cis-13,16-Docosadienoic acid methyl ester
(C22:2) |
0.211×10−2 |
|
| Docosahexaenoic
acid (C22:6n3) |
0.084×10−2 |
|
| Tricosanoic acid
(C23:0) |
2.165×10−2 |
|
| Tetracosanoic acid
(C24:0) |
9.214×10−2 |
|
| Nervonic acid
(C24:1n9) |
0.053×10−2 |
|
| Octanoic acid
(C8:0) |
0.251×10−2 |
| Amino acid | Aspartic acid | 0.007 |
|
| L-Threonine | ND |
|
| Serine | 0.003 |
|
| Glutamic acid | ND |
|
| Glycine | 0.001 |
|
| Alanine | ND |
|
| Cysteine | ND |
|
| Valine | ND |
|
| Methionine | 0.003 |
|
| Isoleucine | ND |
|
| Leucine | ND |
|
| Tyrosine | ND |
|
| Proline | 0.112 |
|
| Lysine | 0.003 |
|
| Arginine | 0.007 |
|
| Histidine | 0.004 |
|
| Phenylalanine | ND |
| Flavonoids |
Dihydromyricetin | ND |
|
| Myricetin | ND |
|
| Naringenin |
0.18×10−2 |
|
| Apigenin |
0.012×10−2 |
|
| Taxifolin |
0.52×10−2 |
|
| Eriodictyol |
0.032×10−2 |
|
| Luteolin |
0.024×10−2 |
|
| Aromadendrin |
0.095×10−2 |
|
| Quercetin |
2.3×10−2 |
|
| Kaempferol | ND |
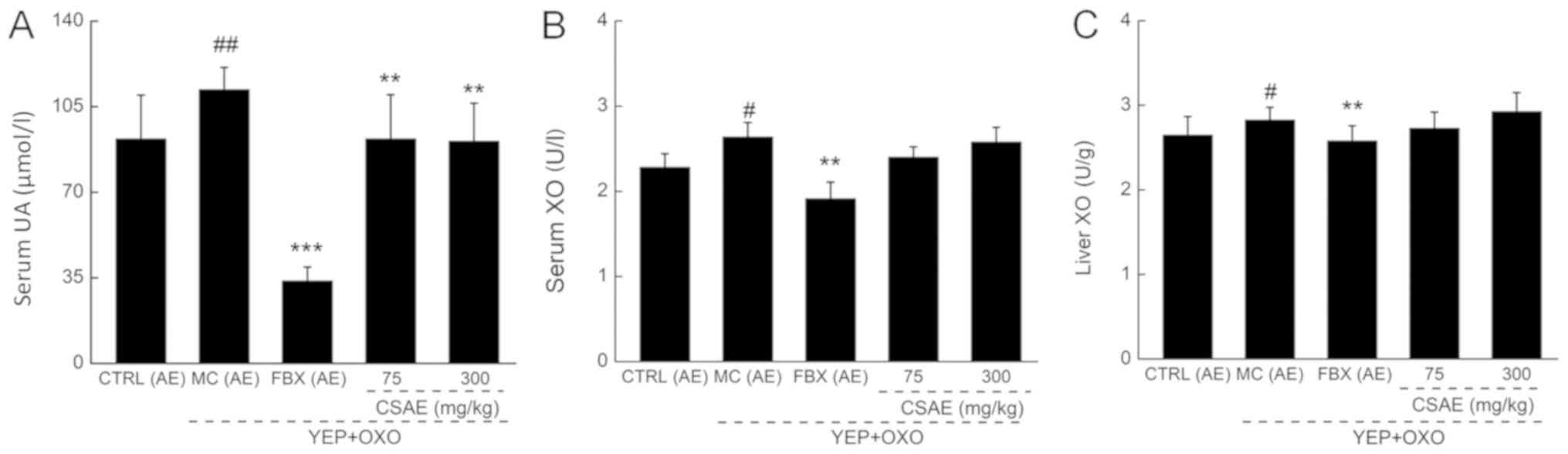
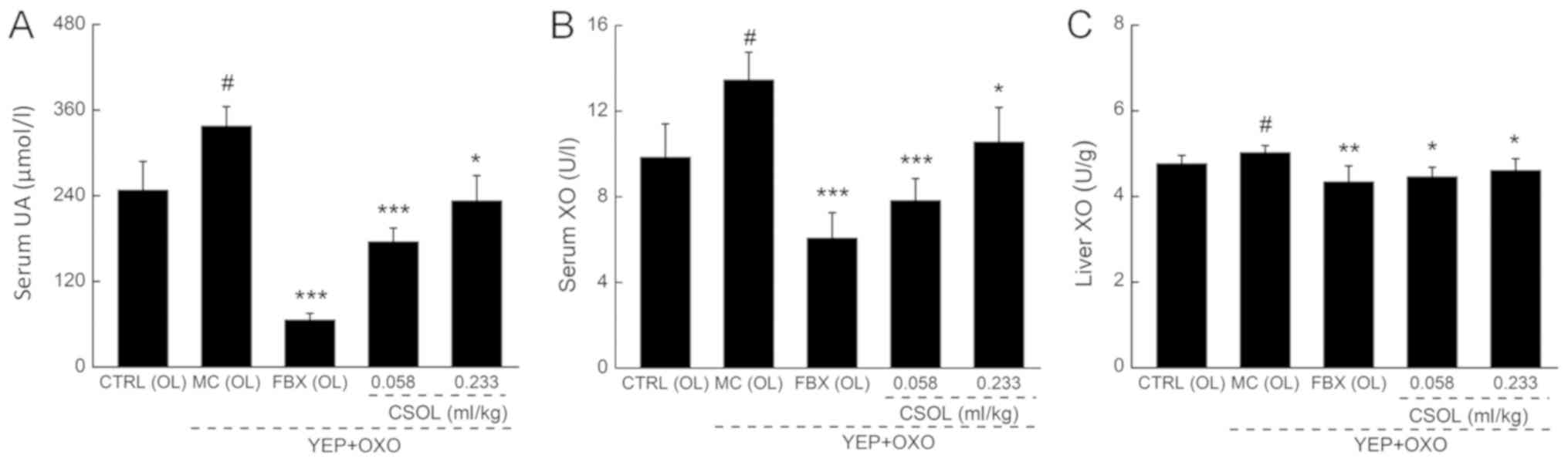
Effects of CSAE and CSOL in hyperuricemia
MC mice
Reductive effects of CSAE and CSOL on
the levels of UA and XO
The accumulation of UA in the body induces sodium
urate precipitation in the joint cavity, causing severe painful
arthritis (41). In the two
separate experiments, a significant increase in serum UA levels was
observed in mice with hyperuricemia compared with the respective
untreated CTRL mice (P<0.05; Figs.
1A and 2A). FBX treatments
resulted in a >60% reduction of the UA enhancement compared with
the respective MC group (P<0.001; Figs. 1A and 2A). Low- and high-dose CSAE and CSOL
administration strongly reduced serum UA levels in mice with
hyperuricemia compared with those in the respective MC group
(P<0.05; Figs. 1A and 2A).
XO is a regulator of purine metabolism, which
regulates the levels of the final product of purine metabolism, UA
(42). Significantly higher levels
of XO were observed in the serum (P<0.05, Figs. 1B and 2B) and liver (P<0.05, Figs. 1C and 2C) of MC mice compared with the CTRL
group. Low- and high-dose CSAE and CSOL slightly decreased the
pathologically elevated XO levels; CSOL-low treatment reduced the
XO activity by 41.9% in the serum (P<0.001; Fig. 2B) and by 11.3% in the liver
(P<0.05; Fig. 2C).
Regulatory effect of CSAE and CSOL on
oxidative stress
The production of UA is accompanied by a large
amount of ROS, and hyperuricemia is associated with the occurrence
of oxidative stress (43,44). Low SOD and GSH-Px levels and high
ROS levels were observed in hyperuricemia MC mice compared with the
CTRL group (P<0.05; Tables
III and IV). Low-dose CSAE
treatment resulted in 14.2 and 22.6% increase of GSH-Px (P<0.05)
and SOD (P<0.05) levels, respectively, and a 13.6% reduction of
ROS levels (P<0.01) in the serum compared with untreated MC
mice. Similar regulatory effects on the anti- and pro-oxidative
factors were observed in the CSOL-treated compared with untreated
MC mice (P<0.05; Tables III
and IV). However, FBX treatment
only enhanced the levels of SOD and reduced the levels of ROS in
the serum compared with untreated MC mice (P<0.05; Tables III and IV).
 | Table III.Effects of CSAE on the oxidative
stress-related factors in mice with hyperuricemia. |
Table III.
Effects of CSAE on the oxidative
stress-related factors in mice with hyperuricemia.
| Group | SOD (U/ml) | GSH-Px (U/ml) | ROS (U/ml) |
|---|
| CTRL (AE) | 41.2±3.6 | 61.3±7.3 | 59.5±6.5 |
| MC (AE) |
36.8±3.8a |
53.6±6.1a |
64.0±3.9a |
| FBX (AE) (6
mg/kg) |
43.0±4.6b | 57.2±5.9 |
54.5±59.0c |
| CSAE (75
mg/kg) |
45.1±4.7c |
61.2±4.2b |
55.3±6.1c |
| CSAE (300
mg/kg) |
47.8±3.5d | 50.2±1.9 |
57.6±4.2b |
 | Table IV.Effects of CSOL on the oxidative
stress-related factors in mice with hyperuricemia. |
Table IV.
Effects of CSOL on the oxidative
stress-related factors in mice with hyperuricemia.
| Group | SOD (U/ml) | GSH-Px (U/ml) | ROS (U/ml) |
|---|
| CTRL (OL) | 24.8±2.1 | 39.4±3.7 | 21.1±0.7 |
| MC (OL) |
21.4±2.1b |
35.2±2.0a |
22.6±1.3a |
| FBX (OL) (6
mg/kg) |
23.2±1.9c | 36.3±4.1 |
20.0±1.3d |
| CSOL (0.058
ml/kg) | 23.0±1.6 |
37.8±1.2c |
20.0±1.0d |
| CSOL (0.233
ml/kg) |
25.2±1.6d | 35.6±3.7 | 22.3±2.0 |
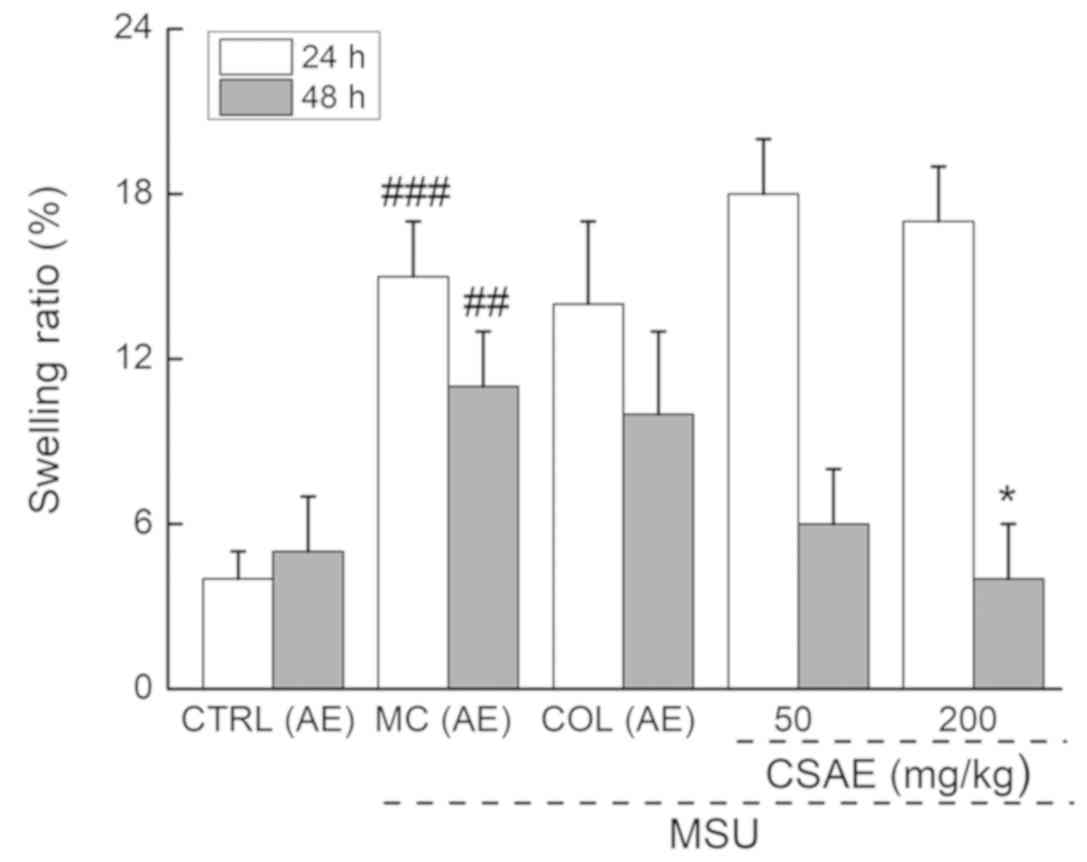
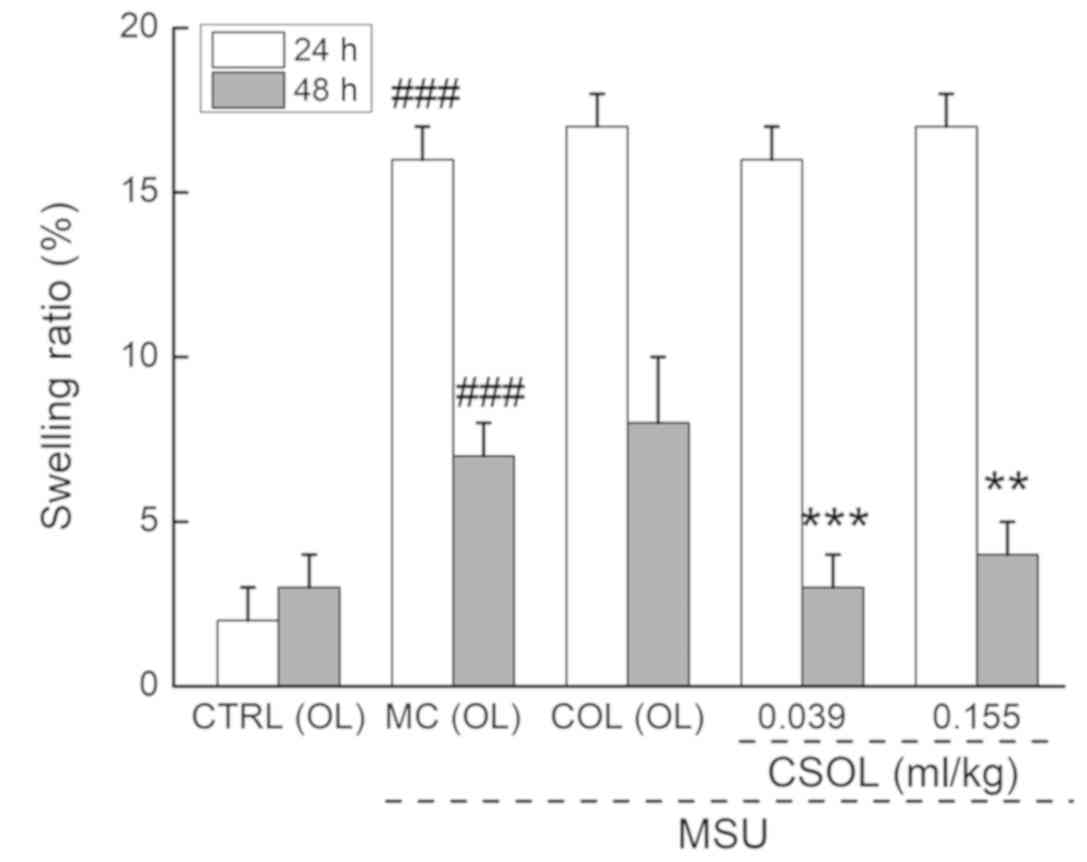
Effects of CSAE and CSOL on MSU-induced
acute gouty arthritis model rats
CSAE and CSOL regulate the swelling
and pathological changes of ankle joints
Compared with the CRL rats of the two experiments,
the swelling rates of the right ankle joint in the MCr rats with
MSU-induced gouty arthritis increased by >100% at 24 and 48 h
(P<0.001; Figs. 3 and 4). This effect was suppressed by
CSAE-high and low- and high-dose CSOL administration at 48 h
(P<0.05; Figs. 3 and 4). Compared with MCr rats with
MSU-induced gouty arthritis, COL treatment did not reduce the
swelling (P<0.05; Figs. 3 and
4).
In the MCr rats, there was a notable presence of
foreign substances, such as cell debris, in the ankle joint cavity,
a narrow joint space and enhanced numbers of inflammatory cells
around the joint cavity were observed compared with the untreated
CTRL rats of the two experiments (Fig.
5). These effects were detected in both ankle joints and joint
capsules. These pathological changes of the ankle joints of rats
with acute gouty arthritis appeared to be relieved by COL, CSAE-low
and CSOL-low treatments (Fig. 5).
However, CSAE-high and CSOL-high failed to relieve the inflammation
of the joints (Fig. 5), possibly
due to a negative feedback regulation.
Effects of CSAE and CSOL on
inflammatory factors
A previous study has demonstrated that the
pathogenesis of gout is associated with inflammation (45). Compared with the CTRL rats of the
two experiments, enhanced levels of the pro-inflammatory cytokines
IL-1β and IL-6 and reduced levels of the anti-inflammatory cytokine
IL-10 were observed in the respective hyperuricemia or gouty
arthritis MCr rats (P<0.05; Tables
V and VI). CSAE-high reduced
the levels of IL-1β by 22.4% (P<0.05), IL-6 by 20.4% (P<0.05)
and TNF-α by 17.2% (P<0.05), and enhanced the IL-10 levels by
8.8% (P<0.05) compared with untreated MCr rats; however, it did
not affect the levels of MCP-1 in the serum of rats with acute
gouty arthritis (Table V).
CSOL-low resulted in 14.2 and 19.4% reductions in the serum levels
of TNF-α (P<0.05) and IL-1β (P<0.05), respectively, and a
>14.3% increase in the serum levels of IL-10 (P<0.05)
compared with untreated acute gouty arthritis MCr rats (Table VI). CSOL did not affect the levels
of IL-6 or MCP-1 in rats with acute gouty arthritis (Table VI).
 | Table V.Effects of CSAE on inflammatory
factors in MSU-induced rats with acute gout. |
Table V.
Effects of CSAE on inflammatory
factors in MSU-induced rats with acute gout.
| Group | IL-1β (pg/ml) | IL-6 (pg/ml) | IL-10 (pg/ml) | MCP-1 (pg/ml) | TNF-α (pg/ml) |
|---|
| CTRL (AE) | 5.3±0.6 | 28.1±3.2 | 16.0±3.2 | 116.8±11.1 | 44.0±2.8 |
| MCr (AE) |
6.7±1.5a |
35.3±7.9a |
13.6±1.2a | 127.1±23.9 | 51.3±9.6 |
| COL (AE) (0.3
mg/kg) |
5.1±0.8b |
27.4±3.7b | 14.2±1.1 |
92.0±12.2c |
37.1±4.9c |
| CSAE (50
mg/kg) |
5.2±0.4b | 31.1±1.9 |
16.6±1.7c | 106.9±23.7 |
40.8±4.4b |
| CSAE (200
mg/kg) |
5.2±0.4b |
28.1±2.7b |
14.8±0.7b | 107.6±7.9 |
42.5±3.8b |
 | Table VI.Effects of CSOL on the inflammatory
factors in MSU-induced acute gouty rats. |
Table VI.
Effects of CSOL on the inflammatory
factors in MSU-induced acute gouty rats.
| Group | IL-1β (pg/ml) | IL-6 (pg/ml) | IL-10 (pg/ml) | MCP-1 (pg/ml) | TNF-α (pg/ml) |
|---|
| CTRL (OL) | 2.7±0.1 | 17.7±2.9 | 4.7±0.2 | 73.1±3.1 | 22.7±0.5 |
| MCr (OL) |
3.1±0.5a |
20.4±2.1a |
4.2±0.5a | 76.5±1.1 | 23.3±0.7 |
| COL (OL) (0.3
mg/kg) |
2.6±0.5b |
17.1±0.9b | 4.4±0.3 | 71.3±4.1 | 22.2±0.8 |
| CSOL (0.039
ml/kg) |
2.5±0.1b | 19.4±1.7 |
5.2±0.8b | 74.0±10.2 |
20.0±1.2b |
| CSOL (0.155
ml/kg) | 2.9±0.2 | 18.8±1.1 |
4.8±0.2b | 72.7±2.6 | 21.5±1.0 |
Discussion
The results of the present study suggested that CSAE
and CSOL exerted slightly suppressive effects on the serum UA
levels and XO activity in mice with hyperuricemia induced by OXO
and yeast extract, and reduced the ankle joint swelling rates in
rats with acute gouty arthritis induced by an intra-articular
injection of MSU.
The occurrence of hyperuricemia increases the
production of oxygen free radicals, promotes lipid peroxidation and
upregulates pro-inflammatory factor expression (6,46–48).
Celery juice and celery root can increase the antioxidant content
in rats (49). One of the major
functions of the flavonoids in plants is to scavenge free radicals
and exert anti-oxidant effects (50,51).
In the present study, CSAE and CSOL, which contain various types of
flavonoids, such as quercetin and taxifolin, inhibited XO activity,
promoted oxidative stress factors SOD and GSH-Px and reduced levels
of ROS in mice with hyperuricemia mice. As an effective antioxidant
enzyme, SOD catalyzes the rapid conversion of O2 and
•O2− to H2O2, following
which H2O2 can be converted to H2O
by GSH-Px catalysis inside cells (52). A negative correlation between the
levels of XO activity and SOD and GSH-Px has been reported in
patients with acute paraquat poisoning (53). Flaxseed oil has been demonstrated
to inhibit the gene expression levels of XO by increasing the
activity of SOD and GSH-Px in the brains of female rats treated
with g-irradiation and carbon tetrachloride (54). XO is a key enzyme in the catalytic
conversion of xanthine and hypoxanthine to UA (55,56),
which is responsible for the generation of ROS (43). As a feedback response, a large
amount of ROS is generated alongside the production of UA (43). Therefore, the suppressive effects
of CSEA and CSOL on UA in mice with hyperuricemia may be, at least
partially, associated with oxidative stress inhibition.
During the development of gouty arthritis, MSU
enters cells through endocytosis and induces inflammation (57). MSU stimulates synovial cells,
monocyte macrophages and neutrophils to produce IL-1β, which
promotes the release of a series of inflammatory cytokines, such as
IL-6, TNF-α and MCP-1 (41),
leading to the spread of inflammation (58). In clinical trials, high levels of
pro-inflammatory factors, especially IL-1β, have been detected in
patients with gout (59). IL-1β
has been investigated for its important roles in gout, and piperine
has been shown to exhibit anti-gouty arthritis effect by inhibiting
IL-1β (60). IL-1 inhibitors, such
as anakinra and canakinumab, which are drugs approved by the U.S.
Food and Drug Administration and the European Medicines Agency
(61), are reportedly effective
against gouty arthritis (62,63).
In addition, sustained oxidative stress can lead to chronic
inflammation (64). The
overproduction of ROS is a pathogenetic factor of acute gouty
arthritis (65,66). Excessive ROS production activates
the inflammasome, specifically NACHT, LRR and PYD
domains-containing protein 3, and promotes the production of IL-1β
in gouty arthritis (67). In the
present study, CSAE and CSOL reduced the pro-inflammatory factors
and enhanced the anti-inflammatory factor in the serum, and
mitigated the pathological changes of the ankle joints of rats with
MSU-induced acute gouty arthritis. The results of the present study
suggested that the anti-inflammatory properties of CSAE and CSOL,
as well as their modulatory effect on inflammatory cytokines,
especially IL-1β, may be central to their anti-gout effects,
possibly through the modulation of oxidative stress.
There were certain limitations to the present study.
Although the anti-gout effects of two celery seed extracts, CSAE
and CSOL, were demonstrated in two rodent models, the results did
not clearly determine which extract exhibited stronger effects. The
contents of CSAE and CSOL were systematically detected; however,
which component exhibited the anti-gouty arthritis and
anti-hyperuricemia properties remains to be determined. Based on
the current data, it is difficult to establish quality standards
for CSAE and CSOL. Additionally, although the anti-gout effects of
CSAE and CSOL were demonstrated to be related to antioxidation and
anti-inflammation, the detailed mechanisms require further
systematic investigation.
In conclusion, the present study demonstrated that
CSAE and CSOL exhibited the effect of suppressing serum UA levels
in mice with hyperuricemia and the swelling rates of ankle joints
in rats with gouty arthritis, which may be associated with the
modulation of XO activity and inflammation response by oxidative
stress regulation, providing experimental evidence to support the
further evaluation of CSAE and CSOL as agents for gout
treatment.
Acknowledgements
Not applicable.
Funding
The present study was supported by The National Key
Research and Development Program of China (grant no.
2018YFE0107800), The Special Projects of Cooperation between Jilin
University and Jilin Province in China (grant no. SXGJSF2017-1),
The ‘13th Five-year’ Science and Technology Project from the
Education Department in Jilin Province (grant no. JJKH20190108KJ)
and The Tianjin Municipal Science and Technology Commission (grant
no. 16JCQNJC09100).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DW and NH designed the experiments; SL, LL, HY, XJ
and WH performed the experiments; SL, LL and HY processed data; DW,
SL and LL wrote the paper; DW and NH revised the paper.
Ethics approval and consent to
participate
The experimental animal protocol was approved by the
Animal Ethics Committee of Jilin University (Changchun, China;
approval no. 20171124).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen LX and Schumacher HR: Gout: An
evidence-based review. J Clin Rheumatol. 14 (5 Suppl):S55–S62.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kuo CF, Grainge MJ, Mallen C, Zhang W and
Doherty M: Rising burden of gout in the UK but continuing
suboptimal management: A nationwide population study. Ann Rheum
Dis. 74:661–667. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Trifirò G, Morabito P, Cavagna L,
Ferrajolo C, Pecchioli S, Simonetti M, Bianchini E, Medea G,
Cricelli C, Caputi AP and Mazzaglia G: Epidemiology of gout and
hyperuricaemia in Italy during the years 2005–2009: A nationwide
population-based study. Ann Rheum Dis. 72:694–700. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu S, Perez-Ruiz F and Miner JN: Patients
with gout differ from healthy subjects in renal response to changes
in serum uric acid. Joint Bone Spine. 84:183–188. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lin Y, Liu PG, Liang WQ, Hu YJ, Xu P, Zhou
J, Pu JB and Zhang HJ: Luteolin-4′-O-glucoside and its aglycone,
two major flavones of Gnaphalium affine D. Don, resist
hyperuricemia and acute gouty arthritis activity in animal models.
Phytomedicine. 41:54–61. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Terkeltaub R: Update on gout: New
therapeutic strategies and options. Nat Rev Rheumatol. 6:30–38.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cronstein BN and Terkeltaub R: The
inflammatory process of gout and its treatment. Arthritis Res Ther.
8 (Suppl 1):S32006. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Martinon F, Petrilli V, Mayor A, Tardivel
A and Tschopp J: Gout-associated uric acid crystals activate the
NALP3 inflammasome. Nature. 440:237–241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Terkeltaub R: Update on gout: New
therapeutic strategies and options. Nat Rev Rheumatol. 6:30–38.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dalbeth N and Haskard DO: Mechanisms of
inflammation in gout. Rheumatology (Oxford, England). 44:1090–1096.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bai H, Yang B, Yu W, Xiao Y, Yu D and
Zhang Q: Cathepsin B links oxidative stress to the activation of
NLRP3 inflammasome. Exp Cell Res. 362:180–187. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Terkeltaub RA: Colchicine update: 2008.
Semin Arthritis Rheum. 38:411–419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fam AG: Strategies and controversies in
the treatment of gout and hyperuricaemia. Baillieres Clin
Rheumatol. 4:177–192. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Terkeltaub R, Bushinsky DA and Becker MA:
Recent developments in our understanding of the renal basis of
hyperuricemia and the development of novel antihyperuricemic
therapeutics. Arthritis Res Ther. 8 (Suppl):S42006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fam AG: Difficult gout and new approaches
for control of hyperuricemia in the allopurinol-allergic patient.
Curr Rheumatol Rep. 3:29–35. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fam AG: Treating acute gouty arthritis
with selective COX 2 inhibitors. BMJ. 325:980–981. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Salihu Shinkafi T, Bello L, Wara Hassan S
and Ali S: An ethnobotanical survey of antidiabetic plants used by
Hausa-Fulani tribes in Sokoto, Northwest Nigeria. J Ethnopharmacol.
172:91–99. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gauri M, Ali SJ and Khan MS: A Review of
Apium graveolens (Karafs) with special reference to Unani Medicine.
IAIM. 2:131–136. 2015.
|
|
19
|
Kooti W, Ghasemiboroon M, Asadi-Samani M,
Ahangarpoor A, Abadi MAN, Afrisham R and Dashti N: The effects of
hydro-alcoholic extract of celery on lipid profile of rats fed a
high fat diet. Adv Environmental Biol. 8:325–330. 2014.
|
|
20
|
Gharooni M and Sarkarati AR: Application
of Apium Graveolens in treatment of hypertension. Tehran Univ Med
J. 58:67–69. 2000.
|
|
21
|
Mencherini T, Cau A, Bianco G, Della
Loggia R, Aquino RP and Autore G: An extract of Apium graveolens
var. dulce leaves: Structure of the major constituent, apiin and
its anti-inflammatory properties. J Pharm Pharmacol. 59:891–897.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Momin RA and Nair MG: Mosquitocidal,
nematicidal, and antifungal compounds from Apium graveolens L.
seeds. J Agric Food Chem. 49:142–145. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Al-Howiriny T, Alsheikh A, Alqasoumi S,
Al-Yahya M, ElTahir K and Rafatullah S: Gastric antiulcer,
antisecretory and cytoprotective properties of celery (Apium
graveolens) in rats. Pharm Biol. 48:786–793. 2014. View Article : Google Scholar
|
|
24
|
Jabbar AA, Al-Sa'aidi and Alrodhan M:
Antioxidant activity of n-butanol extract of celery (Apium
graveolens) seed in streptozotocin-induced diabetic male rats. Res
Pharm Biotechnol. 4:24–29. 2012. View Article : Google Scholar
|
|
25
|
Al-Okbi D: Evaluation of anti-gout
activity of some plant food extracts. Pol J Food Nutr Sci.
58:389–395. 2008.
|
|
26
|
Zhou Q, Lin FF, Liu SM and Sui XF:
Influence of the total saponin fraction from Dioscorea nipponica
Makino on TLR2/4-IL1R receptor singnal pathway in rats of gouty
arthritis. J Ethnopharmacol. 206:274–282. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Amat N, Umar A, Hoxur P, Anaydulla M, Imam
G, Aziz R, Upur H, Kijjoa A and Moore N: Traditional Uighur
medicine Karapxa decoction, inhibits liver xanthine oxidase and
reduces serum uric acid concentrations in hyperuricemic mice and
scavenges free radicals in vitro. BMC Complement Altern Med.
15:1312015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li L, Teng M, Liu Y, Qu Y, Zhang Y, Lin F
and Wang D: Anti-gouty arthritis and antihyperuricemia effects of
sunflower (Helianthus annuus) head extract in gouty and
hyperuricemia animal models. Biomed Res Int.
2017:58520762017.PubMed/NCBI
|
|
29
|
Chow PS and Landhäusser SM: A method for
routine measurements of total sugar and starch content in woody
plant tissues. Tree Physiol. 24:1129–1136. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lee GO, Kosek P, Lima AA, Singh R, Yori
PP, Olortegui MP, Lamsam JL, Oliveira DB, Guerrant RL and Kosek M:
Lactulose: Mannitol diagnostic test by HPLC and LC-MSMS platforms:
Considerations for field studies of intestinal barrier function and
environmental enteropathy. J Pediatr Gastroenterol Nutr.
59:544–550. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
McKee LS: Measuring enzyme kinetics of
glycoside hydrolases using the 3,5-dinitrosalicylic acid assay.
Methods Mol Biol. 1588:27–36. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chromý V, Vinklárková B, Šprongl L and
Bittová M: The Kjeldahl method as a primary reference procedure for
total protein in certified reference materials used in clinical
chemistry. I. A review of Kjeldahl methods adopted by laboratory
medicine. Crit Rev Anal Chem. 45:106–111. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Smith CR and Tschinkel WR: Ant fat
extraction with a Soxhlet extractor. Cold Spring Harb Protoc.
2009:pdb.prot5243. 2009. View Article : Google Scholar
|
|
34
|
Zhang D, Zheng XY, Yan XW, Cao WG and Gang
W: Determination of Total Flavonoids and Rutin in Ephorbia
helioscopia L. from Chongqing. Med Plant. 2:30–32, 45.
2011.
|
|
35
|
Li JJ, Hu XQ, Zhang XF, Liu JJ and Cao LS:
Study on variation of main ingredients from spores and fruiting
bodies of Ganoderma lucidum. Zhongguo Zhong Yao Za Zhi.
39:4246–4251. 2014.(In Chinese). PubMed/NCBI
|
|
36
|
Silva EDS, da Silva EGP, Silva DDS, Novaes
CG, Amorim FAC, Dos Santos MJS and Bezerra MA: Evaluation of macro
and micronutrient elements content from soft drinks using principal
component analysis and Kohonen self-organizing maps. Food Chem.
273:9–14. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhang ZX, Lu Y, Li HP, Tu Y, Liu BY and
Yang ZG: Assessment of heavy metal contamination, distribution and
source identification in the sediments from the Zijiang River,
China. Sci Total Environ. 645:235–243. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Huang FF, Jiang SJ, Chen YL and Sahayam
AC: Chemical vapor generation sample introduction for the
determination of As, Cd, Sb, Hg, and Pb in nail polish by
inductively coupled plasma mass spectrometry. Spectroc Acta Part B
Atom Spectr. 140:84–88. 2018. View Article : Google Scholar
|
|
39
|
Sanchez-Lozada LG, Tapia E,
Bautista-Garcia P, Soto V, Avila-Casado C, Vega-Campos IP, Nakagawa
T, Zhao L, Franco M and Johnson RJ: Effects of febuxostat on
metabolic and renal alterations in rats with fructose-induced
metabolic syndrome. Am J Physiol Renal Physiol. 294:F710–F718.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Toker H, Yuce HB, Yildirim A, Tekin MB and
Gevrek F: The effect of colchicine on alveolar bone loss in
ligature-induced periodontitis. Braz Oral Res. 33:e0012019.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sabina EP and Rasool M: An in vivo and in
vitro potential of Indian ayurvedic herbal formulation Triphala on
experimental gouty arthritis in mice. Vascul Pharmacol. 48:14–20.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Merriman TR: An update on the genetic
architecture of hyperuricemia and gout. Arthritis Res Ther.
17:982015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Oguz N, Kirca M, Cetin A and Yesilkaya A:
Effect of uric acid on inflammatory COX-2 and ROS pathways in
vascular smooth muscle cells. J Recept Signal Transduct Res.
37:500–505. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tang L, Xu Y, Wei Y and He X: Uric acid
induces the expression of TNFa via the ROSMAPKNF-κB signaling
pathway in rat vascular smooth muscle cells. Mol Med Rep.
16:6928–6933. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dalbeth N, Merriman TR and Stamp LK: Gout.
Lancet. 388:2039–2052. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Singh M, Kalia AN, Sharma R and Balakumar
P: Hyperuricemia: Is it a risk factor for vascular endothelial
dysfunction and associated cardiovascular disorders? Current
Hypertension Rev. 5:1–6. 2009. View Article : Google Scholar
|
|
47
|
Billiet L, Doaty S, Katz JD and Velasquez
MT: Review of hyperuricemia as new marker for metabolic syndrome.
ISRN Rheumatol. 2014:8529542014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kanellis J, Watanabe S, Li JH, Kang DH, Li
P, Nakagawa T, Wamsley A, Sheikh-Hamad D, Lan HY, Feng L and
Johnson RJ: Uric acid stimulates monocyte chemoattractant protein-1
production in vascular smooth muscle cells via mitogen-activated
protein kinase and cyclooxygenase-2. Hypertension. 41:1287–1293.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kolarovic J, Popovic M, Zlinská J, Trivic
S and Vojnovic M: Antioxidant activities of celery and parsley
juices in rats treated with doxorubicin. Molecules. 15:6193–6204.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Nickavar B, Kamalinejad M and Izadpanah H:
In vitro free radical scavenging activity of five Salvia species.
Pak J Pharm Sci. 20:291–294. 2007.PubMed/NCBI
|
|
51
|
Yao Y, Sang W, Zhou M and Ren G: Phenolic
composition and antioxidant activities of 11 celery cultivars. J
Food Sci. 75:C9–C13. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Song Y, Driessens N, Costa M, De Deken X,
Detours V, Corvilain B, Maenhaut C, Miot F, Van Sande J, Many MC
and Dumont JE: Roles of hydrogen peroxide in thyroid physiology and
disease. J Clin Endocrinol Metab. 92:3764–3773. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zhang J, Lv G and Zhao Y: The significance
of serum xanthine oxidase and oxidation markers in acute paraquat
poisoning in humans. Clin Biochem. 44:221–225. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ismail AF, Salem AA and Eassawy MM:
Modulation of gamma-irradiation and carbon tetrachloride induced
oxidative stress in the brain of female rats by flaxseed oil. J
Photochem Photobiol B. 161:91–99. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ramallo IA, Zacchino SA and Furlan RL: A
rapid TLC autographic method for the detection of xanthine oxidase
inhibitors and superoxide scavengers. Phytochem Anal. 17:15–19.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Unno T, Sugimoto A and Kakuda T: Xanthine
oxidase inhibitors from the leaves of Lagerstroemia speciosa
(L.) Pers. J Ethnopharmacol. 93:391–395. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Rock KL, Kataoka H and Lai JJ: Uric acid
as a danger signal in gout and its comorbidities. Nat Rev
Rheumatol. 9:13–23. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Jeong JH, Hong S, Kwon OC, Ghang B, Hwang
I, Kim YG, Lee CK and Yoo B: CD14+ cells with the
phenotype of infiltrated monocytes consist of distinct populations
characterized by anti-inflammatory as well as pro-inflammatory
activity in gouty arthritis. Front Immunol. 8:12602017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Zeng M, Dang W, Chen B, Qing Y, Xie W,
Zhao M and Zhou J: IL-37 inhibits the production of
pro-inflammatory cytokines in MSU crystal-induced inflammatory
response. Clin Rheumatol. 35:2251–2258. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sabina EP, Nagar S and Rasool M: A role of
piperine on monosodium urate crystal-induced inflammation-an
experimental model of gouty arthritis. Inflammation. 34:184–192.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Dhimolea E: Canakinumab. Mabs. 2:3–13.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
So A, De Smedt T, Revaz S and Tschopp J: A
pilot study of IL-1 inhibition by anakinra in acute gout. Arthritis
Res Ther. 9:R282007. View
Article : Google Scholar : PubMed/NCBI
|
|
63
|
Schlesinger N, De Meulemeester M, Pikhlak
A, Yücel AE, Richard D, Murphy V, Arulmani U, Sallstig P and So A:
Canakinumab relieves symptoms of acute flares and improves
health-related quality of life (HRQoL) in difficult-to-treat gouty
arthritis patients by suppressing inflammation: Results of a
randomized, dose-ranging study. Arthritis Res Ther. 13:R532011.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Mittal M, Siddiqui MR, Tran K, Reddy SP
and Malik AB: Reactive oxygen species in inflammation and tissue
injury. Antioxid Redox Signal. 20:1126–1167. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Murunikkara V and Rasool M: Trikatu, a
herbal compound that suppresses monosodium urate crystal-induced
inflammation in rats, an experimental model for acute gouty
arthritis. Cell Biochem Funct. 32:106–114. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Sabina EP, Rasool M, Mathew L, Ezilrani P
and Indu H: 6-Shogaol inhibits monosodium urate crystal-induced
inflammation-an in vivo and in vitro study. Food Chem Toxicol.
48:229–235. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Li S, Wu H, Han D, Ma S, Fan W, Wang Y,
Zhang R, Fan M, Huang Y, Fu X and Cao F: A novel mechanism of
mesenchymal stromal cell-mediated protection against sepsis:
Restricting inflammasome activation in macrophages by increasing
mitophagy and decreasing mitochondrial ROS. Oxid Med Cell Longev.
2018:35376092018. View Article : Google Scholar : PubMed/NCBI
|