Introduction
Although considerable knowledge of cancer biology
has been acquired over the last few decades, cancer remains one of
the major causes of mortality worldwide. Surgical resection is the
most effective treatment; however, in the majority of cases, the
tumor cells have already advanced locally or metastasized to
distant organs by the time of diagnosis. Chemotherapy, a commonly
used treatment for cancers that may not be removed by surgery,
often results in severe side-effects due to the delivery of drugs
to normal cells (1). As a result of
these side-effects, the high doses of chemotherapy required to
completely eradicate cancer cells are not tolerated in humans. In
addition, the majority of cancer cells eventually acquire drug
resistance and result in mortality. Therefore, the development of
additional drugs or novel methods for the treatment of cancer is
urgently required.
Radiation therapy is a highly targeted and effective
way to treat certain types of cancer with limited metastasis
(2). This treatment uses high-energy
radiation, such as X-rays, γ-rays and charged particles.
High-energy radiation induces double strand breaks in DNA, which
promotes apoptosis of cancer cells (3). However, the radiation also results in
severe damage to normal cells. Therefore, irradiation must be
limited to the cancerous area to minimize the side-effects of this
treatment. In contrast to these high-energy radiations, less
energetic forms of radiation have not yet been fully evaluated for
their anti-cancer functions. Near-infrared radiation (NIR) is a
shorter wavelength of radiation in the infrared region of the
spectrum, ranging between 750 and 2,500 nm. It has previously been
reported that irradiation in the near-infrared region has multiple
effects on cells. NIR induces the proliferation of keratinocytes
(4), promotes cell attachment
(5), attenuates the infarct size
following myocardial infarction in rats and dogs (6,7) and
regenerates and induces the proliferation of skeletal muscle
(8). In addition, NIR has been
demonstrated to have an inhibitory effect on advanced neoplasia
(9). Broad-spectrum irradiation
ranging between 1,100 and 1,800 nm resulted in apoptosis in
multiple cancer cell types in vitro, independent of thermal
energy (10). These previous studies
have indicated that NIR may be useful for cancer treatment;
however, additional studies are required to further confirm the
effects of NIR on cancer cells. In the present study, a 915-nm
laser was used to investigate the effects of NIR on pancreatic
cancer cells.
Materials and methods
Near-infrared device and
irradiation
KP4 and MIA-PaCa2 cells (Japanese Collection of
Research Bioresources Cell Bank, Osaka, Japan) were cultured with
media in 96-well plates and incubated at 25°C prior to irradiation.
The cells were irradiated with a gallium arsenide-based laser
(Brother Industries, Nagoya, Japan) with a wavelength of 915 nm at
different powers and for varying durations, as indicated in
Fig. 1.
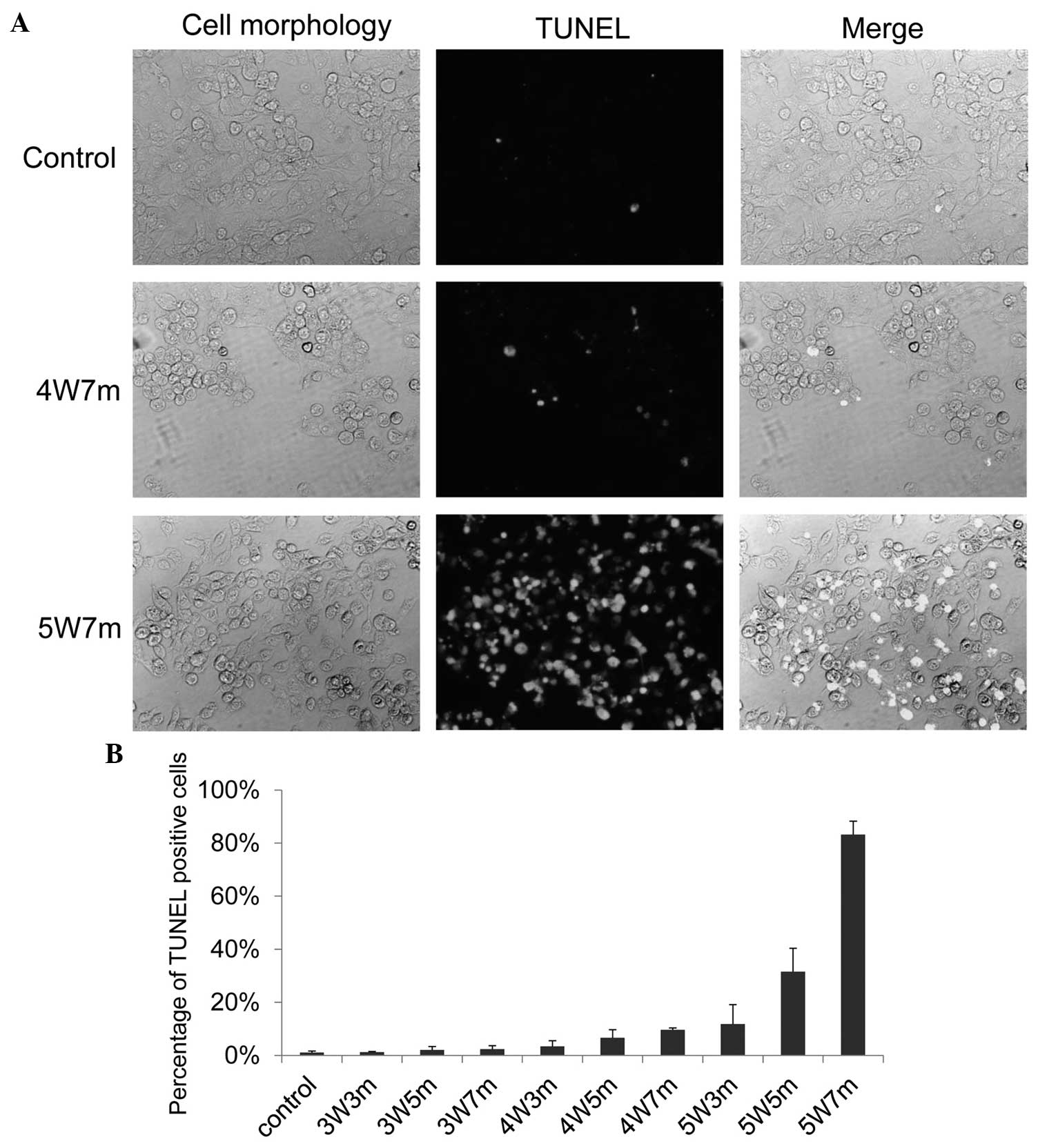
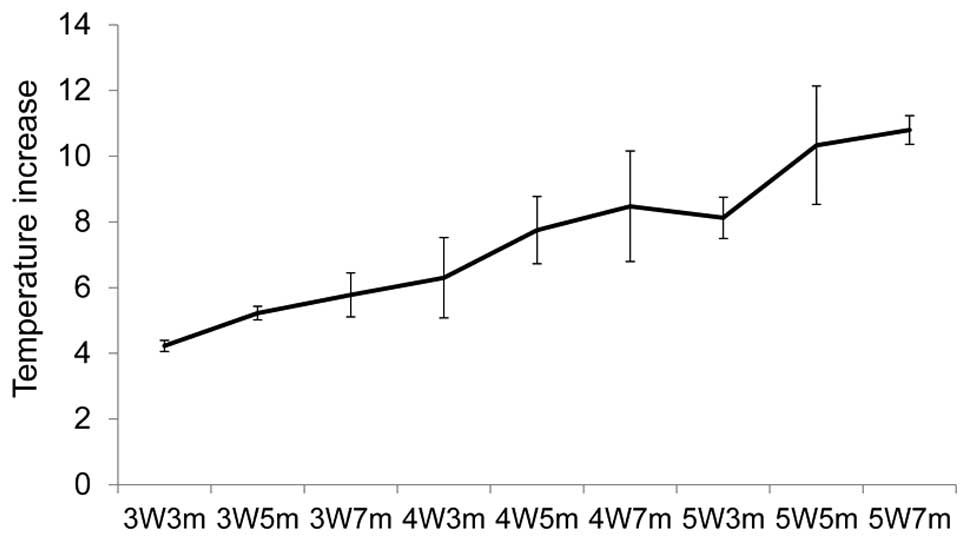
 | Figure 1.Near-infrared irradiation promotes
apoptosis of KP4 cells. (A) KP4 cells cultured in 96-well plates
were irradiated with a 915 nm laser at different powers and for
various durations; 24 h later, the cells were subjected to the
TUNEL assay to detect apoptotic cells. Representative pictures of
the TUNEL assay are presented. (B) TUNEL positive cells were
counted, and the graph indicates the percentage of TUNEL positive
cells. A total of 5 independent fields were selected for
evaluation, and 3 independent experiments were performed. 3W3m,
cells treated with a 3-Watt laser for 3 min; 3W5m, cells treated
with a 3-Watt laser for 5 min; 3W7m, cells treated with a 3-Watt
laser for 7 min; 4W3m, cells treated with a 4-Watt laser for 3 min;
4W5m, cells treated with a 4-Watt laser for 5 min; 4W7m, cells
treated with a 4-Watt laser for 7 min; 5W3m, cells treated with a
5-Watt laser for 3 min; 5W5m, cells treated with a 5-Watt laser for
5 min; 5W7m, cells treated with a 5-Watt laser for 7 min. P<0.05
between control and 4W7m or 5W7m. |
Cells
KP4 and MIA-PaCa2 cells were maintained in
Dulbecco's modified Eagle's medium (Wako Pure Chemical Industries,
Ltd., Osaka, Japan), and PK9 cells were maintained in RPMI (Wako
Pure Chemical Industries, Ltd.) supplemented with 10% FBS
(Equitech-Bio, Inc., Kerrville, TX, USA).
TUNEL assay
The cells were irradiated using the 915 nm laser,
and 24 h post-irradiation, the cells were fixed with 4%
paraformaldehyde (Wako Pure Chemical Industries, Ltd.) and
subjected to the TUNEL assay using the in situ Cell Death Detection
kit (Roche Diagnostics, Basel Switzerland) and fluorescein
according to the manufacturer's protocol. Cells in five randomly
selected fields were evaluated, and three independent experiments
were performed. Images were captured using a BX60 fluorescence
microscopy (Olympus, Tokyo, Japan) at 100X magnification.
Caspase-3 assay
The cells were irradiated using a 915 nm laser, and
2 h post-irradiation, the cells were fixed with 4% paraformaldehyde
and subjected to the caspase-3 assay using the NucView 488
Caspase-3 Assay kit for Live Cells (Biotium, Inc., Hayward, CA,
USA). Cells in five randomly selected fields were evaluated, and
three independent experiments were performed. Images were captured
using a BX60 fluorescence microscopy (Olympus, Tokyo, Japan) at
100X magnification.
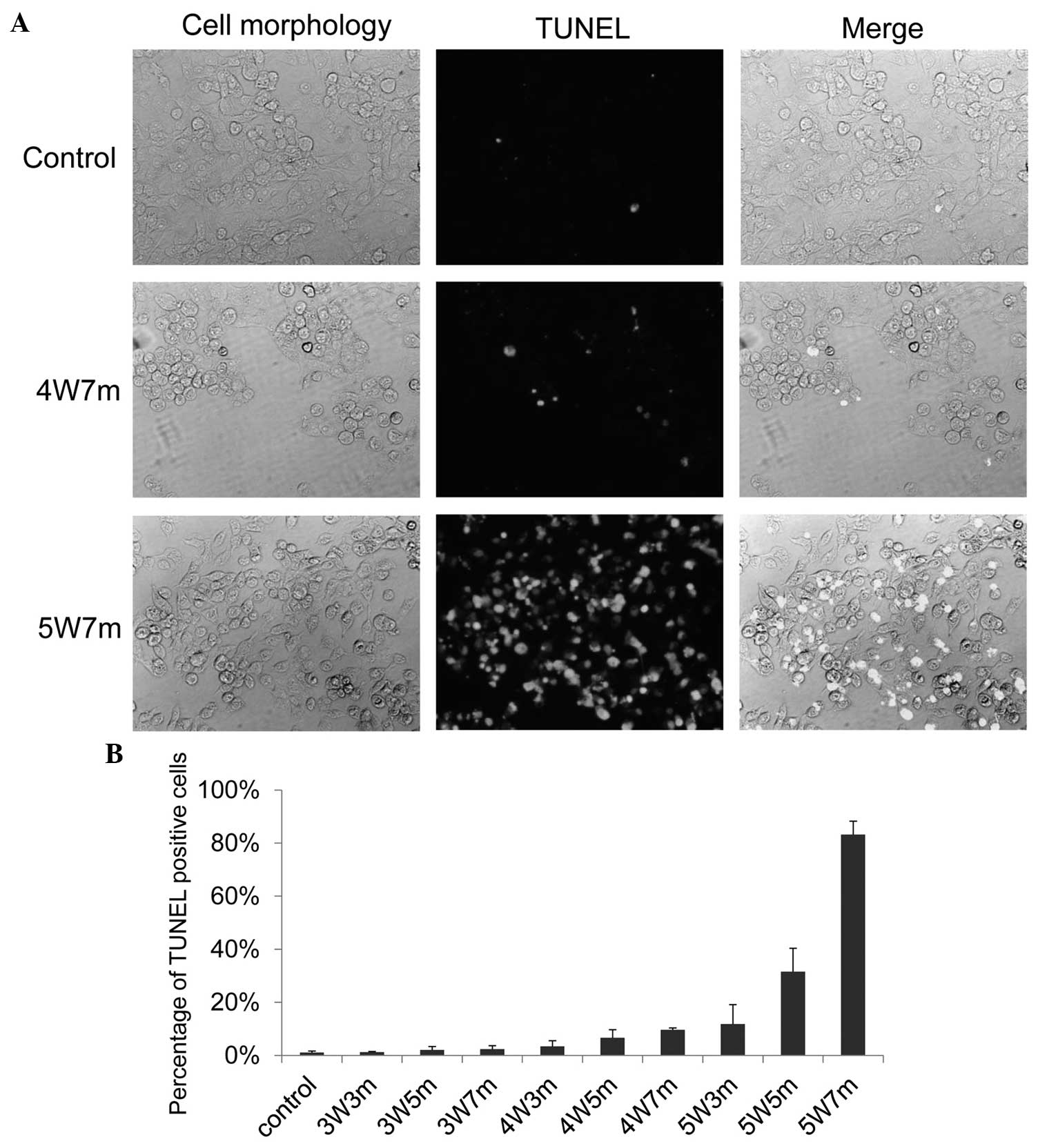
Temperature measurement
The temperature of the media during irradiation was
measured using a thermocouple (Brother Industries).
Statistical analysis
Data are expressed as the mean ± standard deviation.
Comparisons between the groups were performed using unpaired
Student's t-tests. P<0.05 was considered to indicate a
statistically significant difference.
Results
Apoptosis in KP4 pancreatic cancer
cells following NIR treatment
A 915-nm laser (Brother Industries) was used to
automatically irradiate cells in 96-well plates for different
durations and at varying powers. The KP4 pancreatic cancer cell
line was used to examine whether irradiation with a 915-nm laser
exerted an effect on cancer cells. The KP4 cells were irradiated
for different durations and at different powers, and then 24 h
later, the cells were subjected to the TUNEL assay to assess
apoptosis (Fig. 1A). A limited number
of apoptotic cells were observed following irradiation with a
3-Watt (W) laser; however, apoptotic cells were observed following
an increase in the power of the laser and the duration of
treatment. Almost 10% and 30% of the cells became apoptotic 24 h
following irradiation with a 4 W laser for 7 min and a 5 W for 5
min, respectively (Fig. 1B).
Apoptosis was induced in almost 90% of KP4 cells following
irradiation with a 5 W laser for 7 min (Fig. 1B).
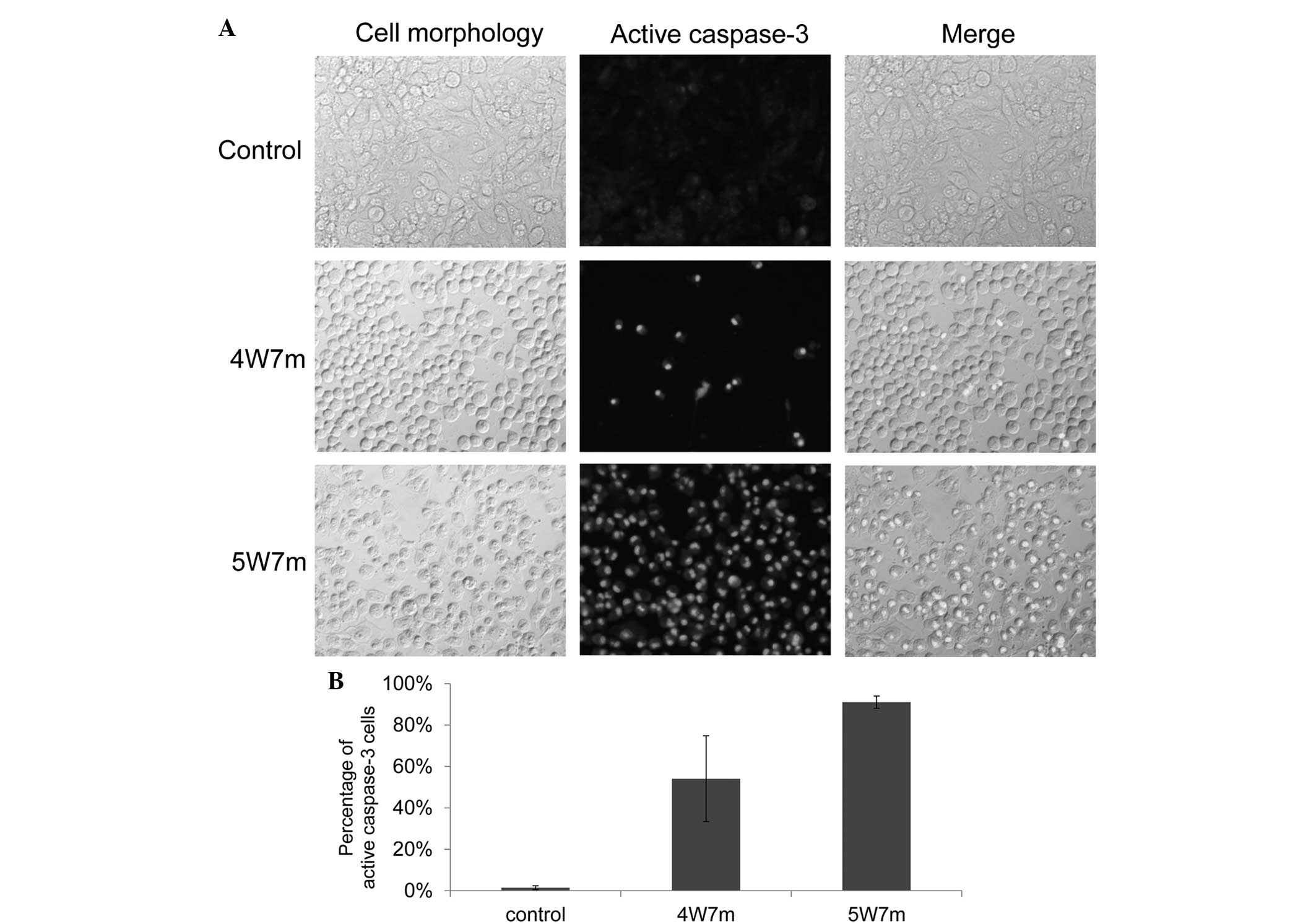
To further confirm these results, the activation of
caspase-3 following irradiation was examined. Caspase-3 is a member
of the cysteine-aspartic acid protease family and is activated in
the apoptotic cell by extrinsic (death ligand) and intrinsic
(mitochondrial) pathways. Activation of caspase-3 was examined 2 h
following irradiation (11). As
demonstrated in Fig. 2A, irradiation
induced activation of caspase-3 in a large proportion of the cells,
as ≤5% of the non-irradiated cells were positive for caspase-3
activation, compared with ≥50% of the cells irradiated with a 4 W
laser for 7 min. These results indicate that irradiation with a 915
nm laser promotes cellular apoptosis.
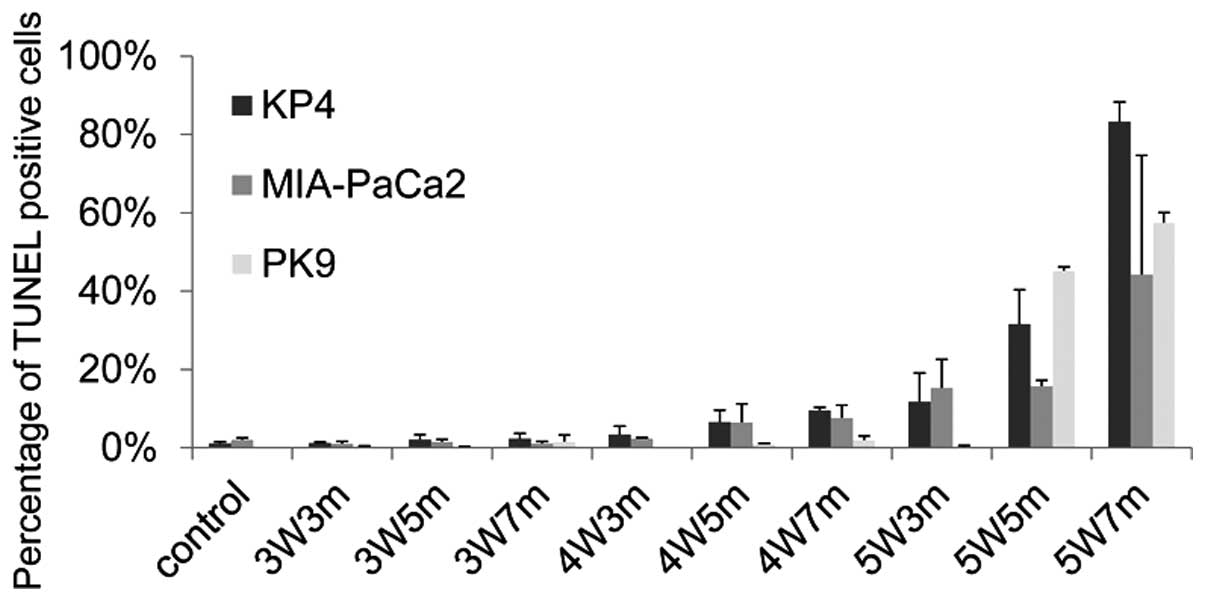
Apoptosis in MIA-PaCa2 and PK9
pancreatic cancer cells following NIR treatment
The effects of NIR treatment on additional
pancreatic cancer cell lines, consisting of the MIA-PaCa2 and PK9
cell lines, were also evaluated. Notably, these cells demonstrated
different sensitivity to irradiation (Fig. 3). Similarly to KP4 cells, apoptotic
MIA-PaCa2 cells started to appear following irradiation with a 4-W
laser, and ≥10% of MIA-PaCa2 cells became apoptotic following 3 min
of irradiation with a 5-W laser. Conversely, few apoptotic cells
were observed following irradiation of PK9 cells with a 5-W laser
for 3 min; however, there was a sudden increase in the number of
apoptotic cells when PK9 cells were irradiated for 5 min with a 5-W
laser. These results indicate that the threshold for apoptosis
induction using a 915-nm laser varies between different pancreatic
cancer cell lines.
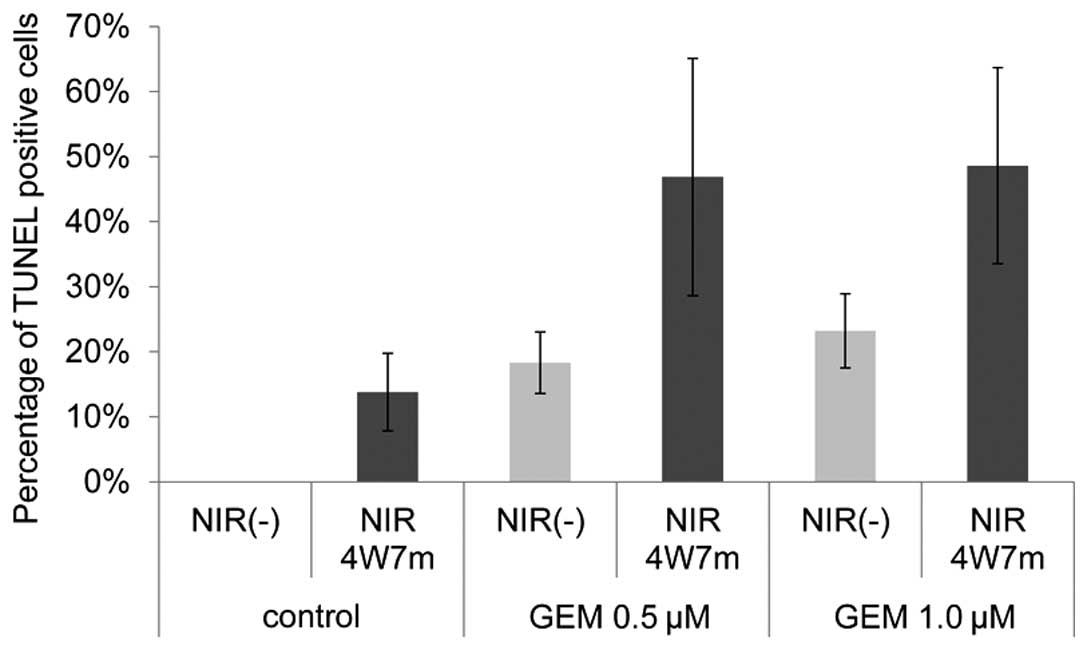
Evaluation of gemcitabine treatment in
combination with NIR on KP4 pancreatic cancer cells
The present study evaluated whether the combination
of an anticancer drug and NIR treatment exerted synergistic effects
on KP4 pancreatic cancer cells. Gemcitabine is widely used for the
treatment of pancreatic cancer. KP4 cells were treated with
gemcitabine for 48 h and were then treated or not treated with a
915-nm laser of 4 W for 7 min. The TUNEL assay was performed to
evaluate the percentage of apoptotic cells 24 h following
irradiation. As demonstrated in Fig.
4, the combination of gemcitabine and irradiation significantly
increased the percentage of apoptotic cells compared with either
treatment alone.
Exclusion of apoptosis induced by
thermal energy
To exclude the possibility that the observed
apoptosis was induced by thermal energy, the changes in temperature
during irradiation were measured. Temperature increases were
observed with each increase in power and duration (Fig. 5). An increase in temperature of ~11°C
was observed when the cells were irradiated with a 5-W laser for 7
min, which was the maximum power and duration used in the
experiments. The cells were incubated at 25°C prior to the
irradiation in all the experiments; therefore, it is unlikely that
apoptosis was induced by the increase in temperature.
Discussion
In the present study, an automatic machine was used
to irradiate pancreatic cancer cells with a 915-nm laser, and the
effects of irradiation on pancreatic cancer cells were examined. A
significant induction of apoptosis was observed with increasing
power and duration of the irradiation. The irradiation laser
induced temperature increases in the media; however, it appears
that apoptosis was induced by irradiation and not thermal energy.
Suppression of tumor cell proliferation requires an exposure for
≥60 min to high temperatures of ~42°C (11). In the present study, the cells were
incubated at 25°C prior to the irradiation. Therefore, a
temperature increase of ~10°C induced by the irradiation would not
be sufficient to induce apoptosis of the cells. In accordance with
the results of the present study, previous studies have
demonstrated that NIR resulted in reduced cell proliferation and
apoptosis in multiple cell lines, independent of the thermal energy
(10,12,13).
Low-energy non-ionizing radiation is known to affect
numerous cellular activities by modulating electrochemical systems
in cells, such as the modulation of mitochondrial signaling by NIR
(14,15). Cytochrome c oxidase is an enzyme that
mediates the transfer of electrons from cytochrome c to molecular
oxygen (16). The oxidase is a
receptor of NIR and activates mitochondrial signaling in mammalian
cells (17,18). Differentiation of neural progenitor
cells is also promoted by NIR. The radiation induces the production
of ATP, which subsequently activates P2Y receptors for neurite
outgrowth (19). Although the
molecular mechanisms by which low-energy radiation affects various
cellular activities are unclear, accumulating evidence indicates
that NIR may be used in multiple clinical treatments (6–10). A
number of previous studies have indicated the possible use of
low-energy radiation for cancer treatment (9,10). NIR
elicited selective cytotoxic effects on tumor tissues (20,21).
Although the exact molecular mechanisms of how NIR exerts cytotoxic
effects is not clear, a previous study indicated that double strand
breaks in DNA are associated with apoptosis induction (22). NIR has been demonstrated to activate
the DNA damage checkpoint pathway, resulting in cell cycle arrest
in G2/M phase or the induction of apoptosis (23). These previous studies have indicated
that NIR may be used for cancer treatment in combination with
ionizing radiation or chemotherapeutic agents.
In the present study, pancreatic cancer cells were
used to examine the effects of NIR. Pancreatic cancer is one of the
most aggressive types of human cancer and is the leading cause of
cancer-associated mortality (24,25).
Gemcitabine is currently the standard treatment for advanced or
resected pancreatic cancer (26).
However, since a large number of patients are resistant to
gemcitabine treatment, this drug provides only modest survival
benefits. In the present study, the combination of NIR and
gemcitabine was more effective than either single treatment alone.
Although it is not technically easy to directly irradiate
pancreatic cancer, the development of such devices may be useful
for the treatment of pancreatic cancer. Additional investigation
into the development of NIR therapy may contribute to an improved
prognosis for patients with cancer.
Acknowledgements
The authors would like to thank the members of the
Division of Cancer Biology for their helpful discussions and
technical assistance. This study was partially funded by a grant
from the Ministry of Education, Culture, Sports, Science and
Technology of Japan (grant nos. 2583114 and 23107010).
References
|
1
|
Chabner BA and Roberts TG Jr: Timeline:
Chemotherapy and the war on cancer. Nat Rev Cancer. 5:65–72. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Salama JK, Chmura SJ, Mehta N, Yenice KM,
Stadler WM, Vokes EE, Haraf DJ, Hellman S and Weichselbaum RR: An
initial report of a radiation dose-escalation trial in patients
with one to five sites of metastatic disease. Clin Cancer Res.
14:5255–5259. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Davis AJ and Chen DJ: DNA double strand
break repair via non-homologous end-joining. Transl Cancer Res.
2:130–143. 2013.PubMed/NCBI
|
|
4
|
Grossman N, Schneid N, Reuveni H, Halevy S
and Lubart R: 780 nm low power diode laser irradiation stimulates
proliferation of keratinocyte cultures: Involvement of reactive
oxygen species. Lasers Surg Med. 22:212–218. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Karu T and Pyatibrat L: Gene expression
under laser and light-emitting diodes radiation for modulation of
cell adhesion: Possible applications for biotechnology. IUBMB Life.
63:747–753. 2011.PubMed/NCBI
|
|
6
|
Oron U, Yaakobi T, Oron A, Mordechovitz D,
Shofti R, Hayam G, Dror U, Gepstein L, Wolf T, Haudenschild C and
Haim SB: Low-energy laser irradiation reduces formation of scar
tissue after myocardial infarction in rats and dogs. Circulation.
103:296–301. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Oron U, Yaakobi T, Oron A, Hayam G,
Gepstein L, Rubin O, Wolf T and Ben Haim S: Attenuation of infarct
size in rats and dogs after myocardial infarction by low-energy
laser irradiation. Lasers Surg Med. 28:204–211. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shefer G, Barash I, Oron U and Halevy O:
Low-energy laser irradiation enhances de novo protein synthesis via
its effects on translation-regulatory proteins in skeletal muscle
myoblasts. Biochim Biophys Acta. 1593:131–139. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Santana-Blank LA, Rodríguez-Santana E,
Vargas F, Reyes H, Fernández-Andrade P, Rukos S and
Santana-Rodríguez KE: Phase I trial of an infrared pulsed laser
device in patients with advanced neoplasias. Clin Cancer Res.
8:3082–3091. 2002.PubMed/NCBI
|
|
10
|
Tanaka Y, Matsuo K, Yuzuriha S, Yan H and
Nakayama J: Non-thermal cytocidal effect of infrared irradiation on
cultured cancer cells using specialized device. Cancer Sci.
101:1396–1402. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shalini S, Dorstyn L, Dawar S and Kumar S:
Old, new and emerging functions of caspases. Cell Death Differ.
22:526–539. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tanaka Y, Matsuo K and Yuzuriha S:
Near-infrared irradiation non-thermally affects subcutaneous
adipocytes and bones. Eplasty. 11:e122011.PubMed/NCBI
|
|
13
|
Tanaka Y, Matsuo K and Yuzuriha S:
Near-infrared irradiation nonthermally induces long-lasting
vasodilation by causing apoptosis of vascular smooth muscle cells.
Eplasty. 11:e222011.PubMed/NCBI
|
|
14
|
Schroeder P, Pohl C, Calles C, Marks C,
Wild S and Krutmann J: Cellular response to infrared radiation
involves retrograde mitochondrial signaling. Free Radic Biol Med.
43:128–135. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Karu TI: Mitochondrial signaling in
mammalian cells activated by red and near-IR radiation. Photochem
Photobiol. 84:1091–1099. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Karu TI: Multiple roles of cytochrome c
oxidase in mammalian cells under action of red and IR-A radiation.
IUBMB Life. 62:607–610. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karu T: Primary and secondary mechanisms
of action of visible to near-IR radiation on cells. J Photochem
Photobiol B. 49:1–17. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Karu TI, Pyatibrat LV, Kolyakov SF and
Afanasyeva NI: Absorption measurements of a cell monolayer relevant
to phototherapy: Reduction of cytochrome c oxidase under near IR
radiation. J Photochem Photobiol B. 81:98–106. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Anders JJ, Romanczyk TB, Ilev IK, Moges H,
Longo L, Wu X and Waynant RW: Light supports neurite outgrowth of
human neural progenitor cells in vitro: The role of P2Y receptors.
IEEE J- Sel Top Quantum Electron. 14:118–125. 2008. View Article : Google Scholar
|
|
20
|
Karu T, Pyatibrat L and Kalendo G:
Irradiation with He-Ne laser can influence the cytotoxic response
of HeLa cells to ionizing radiation. Int J Radiat Biol. 65:691–697.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dees C, Harkins J, Petersen MG, Fisher WG
and Wachter EA: Treatment of murine cutaneous melanoma with near
infrared light. Photochem Photobiol. 75:296–301. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tirlapur UK and König K: Femtosecond
near-infrared laser pulse induced strand breaks in mammalian cells.
Cell Mol Biol (Noisy-le-grand). 47:OL131–OL134. 2001.PubMed/NCBI
|
|
23
|
Tanaka Y, Tatewaki N, Nishida H, Eitsuka
T, Ikekawa N and Nakayama J: Non-thermal DNA damage of cancer cells
using near-infrared irradiation. Cancer Sci. 103:1467–1473. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hidalgo M: Pancreatic cancer. N Engl J
Med. 362:1605–1617. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Berlin J and Benson AB III: Chemotherapy:
Gemcitabine remains the standard of care for pancreatic cancer. Nat
Rev Clin Oncol. 7:135–137. 2010. View Article : Google Scholar : PubMed/NCBI
|