Introduction
At present, chemotherapy remains the optimal choice
for cancer therapy, and tumor multidrug resistance (MDR) is a major
factor that reduces the efficacy of chemotherapy (1). MDR is a phenotype that tumor cells
acquire, which confers resistance to certain chemotherapy drugs, as
well as concurrent cross-resistance to additional antitumor drugs
that have different structures or mechanisms of action (2,3). The
complexity of MDR has impeded the study of reversal agents
(3–5).
In recent years, the application of nanotechnology for drug carrier
design has resulted in the development of novel nanoparticle drug
delivery systems that aim to reverse MDR (6–8). Inorganic
nanodrug delivery systems, lipid-based systems and polymer nanodrug
delivery systems are the most common nanodrug delivery systems,
which exhibit non-toxic, biocompatible and highly stable properties
(8,9).
The application of nanoparticle drug delivery systems is increasing
due to their advantage of controlled and targeted drug release
(9,10). Studies have demonstrated that
entrapped small molecule drugs (10–200 nm in diameter) are more
conducive to drug uptake and efflux; these nanodrug particles
function via passive and active mechanisms, whereas in the systemic
blood circulation they exhibit sustained release that subsequently
enhances intracellular drug accumulation in tumor cells, yielding
an improved effect (1,11–14). In
the present review, the application of nanoparticle drug delivery
systems in reversing the MDR of tumors is reviewed, which may
provide an improved understanding of novel strategies for cancer
therapy.
MDR and applications of nanodrug
transmission systems
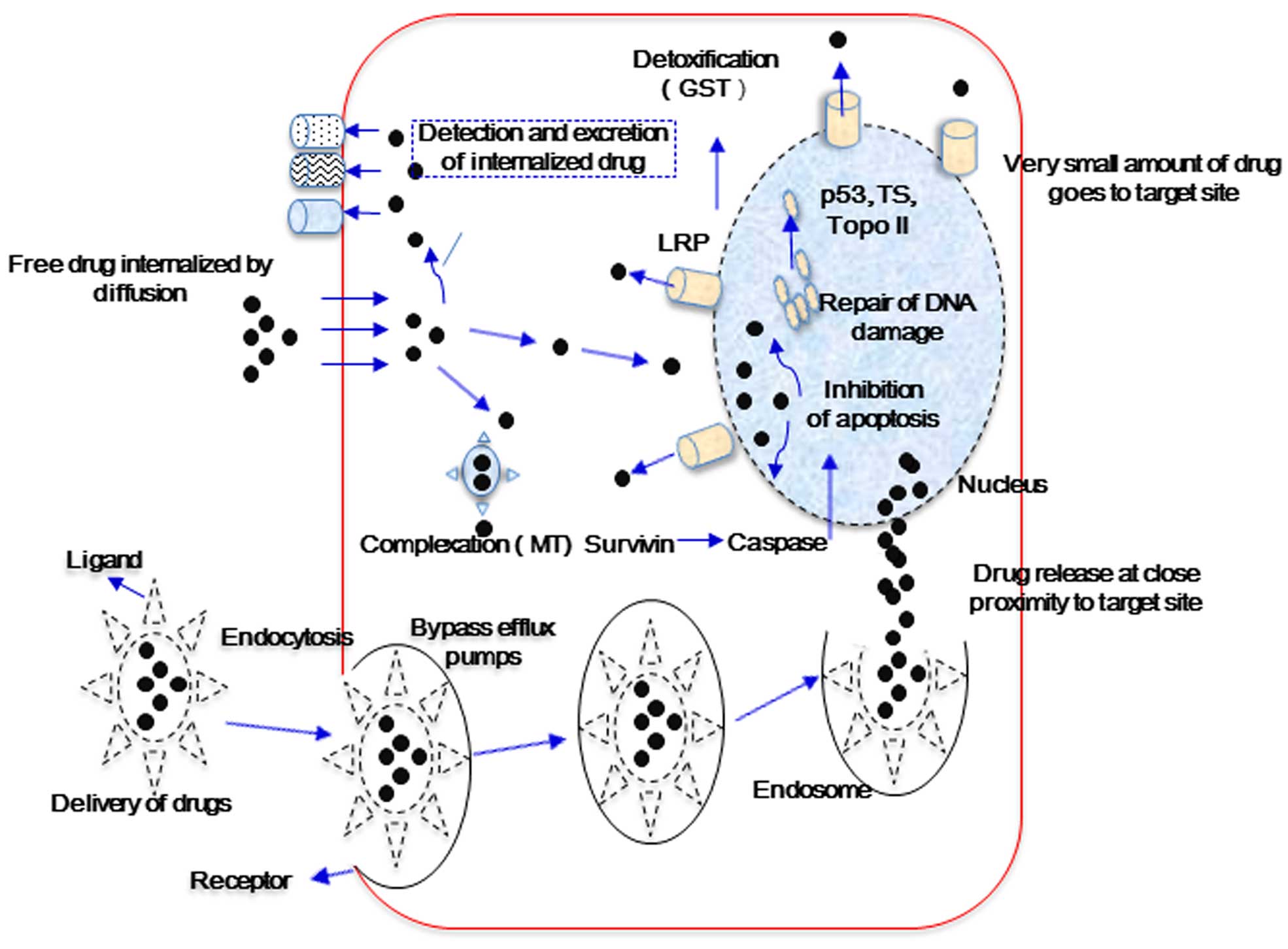
Cancer MDR may be caused by a number of complex
factors, including ATP-binding cassette (ABC) transporters,
multi-drug resistance protein [P-glycoprotein 1 (P-gp)],
MDR-associated proteins (MRPs), breast cancer resistance protein
(ABCG2), glutathione transferase, metallothionein, DNA
topoisomerase II and catalytic enzymes (2,3,5). These substances exhibit various
functions in the induction of tumor cell MDR (Fig. 1). Cellular MDR is divided into the
ATP-dependent efflux pumps and non-ATP-dependent efflux pumps
types. The ‘pumps’ type use the energy obtained from ATP hydrolysis
to efflux drugs via ATP-dependent transport proteins, such as P-gp,
MRPs and BCRPs, which decreases the intracellular drug
concentration and subsequently results in drug resistance. The ‘non
pumps’ type do not depend on the energy from ATP hydrolysis while
activating the anti-apoptotic proteins, such as Bcl-2, and efflux
drugs directly (2,7,9).
Nanoparticle drug transmission systems may alter drug uptake in
tumor cells (12). The system
delivers the chemotherapy drug directly to tumor cells, which
functions to reverse MDR (10).
Entrapment affects the pharmacokinetic properties of drugs; free
drugs cross the cell membrane passively and are easily identified
by the efflux pumps located on the cell membrane or captured by ABC
transporter proteins, whereas drug-loading nanoparticles may avoid
recognition by the ABC efflux pumps and endocytosis by ABC
transporters, leading to increased intracellular accumulation of
chemotherapeutic drugs (Fig. 1)
(10,12,14).
Liposomes
Liposomes are preparations that utilize a
phospholipid bilayer membrane vesicle to encapsulate drug
molecules. The hydrophilic and hydrophobic bilayer cores entrap
hydrophilic and lipophilic drugs, respectively. Liposomes have been
demonstrated to prolong the blood-circulation time of drugs, to
alter the pharmacokinetics and distribution of P-gp inhibitors
in vivo, and to increase the drug concentration in the tumor
cells, while reducing the impact on normal tissues, thus exerting
toxicity to enhance the effects of chemotherapy (15–21). A
study by Zhou et al (22),
which investigated MDR reversal using doxorubicin (DOX) liposomes
in vitro, demonstrated that DOX liposomes were mainly
detected in the nucleus of human breast cancer P-gp overexpression
cells (MCF-7/Adr) with an increased toxicity, and exhibited a
stronger cellular retention capacity in human carcinoma KBv200
cells. Kang et al (23) used
rhodamine (a P-gp substrate) to penetrate liposomes, and this
combination resulted in increased liposome retention in the
MCF-7/Adr cell line, which exhibits P-gp overexpression in
vitro. Further assessment demonstrated that the incorporation
of cholesterol and polyethyleneglycol-attached lipids was effective
in further increasing the rhodamine retention in MCF-7/Pgp cells.
More rigid liposomes are able to sequester rhodamine more
efficiently, thereby inhibiting direct interactions of rhodamine
with P-gp proteins. These studies indicated that by optimizing the
composition of liposomes, reduction of P-gp-mediated MDR may be
achieved.
Lipid nanoparticles
Lipid nanoparticles are a type of nanodrug delivery
system that are assembled using natural or synthetic lipids, such
as stearic acid, lecithin and triglycerides, as the matrix, to
entrap anticancer drugs (particle size, 50–1,000 nm) in a lipid
core (23,24). Lipid nanoparticles have various routes
of administration, exhibit good biological compatibility and
stability, and effectively control drug release to avoid
degradation and leakage. Solid lipid nanoparticles (SLNs) and
nanostructured lipid carriers (NLCs) are the most common types,
which have gained increasing attention as they represent promising
drug carriers (25,26). One study showed that NLCs exhibit
increased stability when compared with SLNs (24). Wong et al (27) showed that, compared with free
doxorubicin, DOX-loaded SLNs exhibit a high encapsulation
efficiency, a faster release rate in vitro, and an enhanced
uptake and retention capacity in human breast cancer cells
(MDA435/LCC6/MDR1), resulting in significantly enhanced
cytotoxicity. A novel polymer-lipid hybrid nanoparticle (PLN)
system has also been developed (28).
Prepared DOX-GG918-PLN and doxorubicin and mitomycin C co-loaded
PLN carriers exhibited a good antitumor effect in vitro and
in vivo, with significant reversal effects, which indicates
that the carriers present a novel technique for improving the
efficacy of local solid tumor chemotherapy (29–32).
Liposomes alone exhibit no specific targeting, however, via the
modification of nanodrug delivery systems using various ligands,
including folic acid or anti-transferrin monoclonal antibodies,
specific targeting may be obtained (33–35).
Ligands with selective and specific affinities may be incorporated
into the lipid bilayer of liposomes, which may then be identified
by specific cells, yielding targeted nanoparticles (36,37).
Polymeric micelles
Polymeric micelles, which are a type of drug carrier
with a hydrophobic core and hydrophilic polyethylene glycol (PEG)
shell, present an ideal choice for the effective delivery of
anticancer drugs (particle size, 10–100 nm) with poor solubility
(38,39). Compared with the free drug,
drug-loaded polymeric micelles, which demonstrate a higher
stability and biocompatibility in vitro and vivo, and
a significantly increased blood circulation time, are transferred
to the tumor site via active and passive targeting mechanisms.
Passive targeting occurs via the enhanced permeability and
retention effect, which causes drugs to be selectively accumulated
and released at the tumor site. By modifying the surface of polymer
micelles, drug accumulation by the tumor may be increased via the
active targeting pathway. Therefore, polymer micelles present an
ideal carrier molecule for active or passive targeted drug delivery
as they improve the therapeutic index while reducing toxic side
effects (40–44). The use of drug-conjugated polymer
micelles that exhibit simultaneous entrapment of two drugs and
maintain antitumor activity has been reported (38). Currently, several types of polymer
micelle transmission systems are being used to overcome MDR, and
certain studies have demonstrated that a number of block copolymers
may decrease the production of ATP in resistant cells, thus
reducing the activity of P-gp (45–47).
Saiyin et al (48) implemented
the simultaneous entrapment of a chemotherapeutic drug and
autophagy inhibitors, and engineered the sequential release of
these drugs. The prioritized release of the autophagy inhibitors
suppressed the phagocytosis of tumor cells, subsequently increasing
sensitivity to the chemotherapeutic drug, which resulted in a
synergistic effect. This combination provides a novel platform for
chemotherapy. Yu et al (49)
prepared docetaxel-loaded pH-responsive PEG-hyperbranched
polyacylhydrazone micelles, which exhibited increasing tumor
toxicity in vitro; however, when combined with glucose,
enhanced antitumor activity and lower systemic toxicity were
observed. Therefore, these results indicate that polymeric micelles
may be used for selective targeted drug delivery.
Combined treatment strategies based on
nanodrug delivery systems
Enhancing the efficiency of drug delivery to tumor
cells and preventing apoptosis by modulating intracellular signal
transduction mechanisms presents an effective method to overcome
MDR (50–52). The co-delivery of reversal agents and
chemotherapy drugs by nanodrug delivery systems may regulate the
expression of intracellular ABC transporter proteins and silence
MDR genes (52–54), thereby affecting the efflux or
apoptosis of tumor cells and reducing the toxicity of chemotherapy
(55–57). In a study by Abouzeid et al
(58), co-coated curcumin (a reversal
agent) and paclitaxel-loaded PEG-phosphatidylethanolamine/vitamin E
micelles were demonstrated to exhibit significantly increased
toxicity in human ovarian carcinoma resistant cells (SK-OV-3/TR)
in vitro and in vivo, with the synergistic antitumor
effects observed in vivo being superior to those observed
in vitro. Furthermore, Tang et al (59) reported that the co-delivery of DOX and
a P-gp inhibitor (verapamil) using a reduction-sensitive liposome
resulted in increased apoptosis induction and necrosis of MCF-7/Adr
tumor cells.
Mesoporous silica nanoparticles
Recently, gene technology and nanobiomaterial vector
delivery systems, such as silicon nanogene vectors as non-viral
gene vectors, have gained increasing attention as a promising
approach for tumor MDR reversal (60–63).
Silicon nanodrug systems exhibit good biocompatibility and a
non-cytotoxic surface that is easily modified. The main aims of the
formed mesoporous silica nanodrug delivery systems (MSNs) are to
control targeted-drug release and overcome MDR (64–66). With
regard to MDR reversal, MSNs are considered to alter the original
route of drug uptake, while avoiding identification, binding and
efflux by ABC proteins. In addition, the different MSN pore sizes
allow the effectively controlled release of intratumor drugs and
accumulation (67–70). MSNs present an alternative method for
the more efficient delivery of chemotherapy drugs and targeted gene
therapy. Meng et al (70)
revealed that coating P-gp-targeted siRNA with DOX using MSNs
significantly increased the chemotherapeutic drug concentration
within the cell nucleus of the squamous carcinoma resistant cell
line, KB-V1, and promoted cell apoptosis and death. Notably, Zhang
et al (71) also developed a
polymer-lipid supported-MSN. This system exhibited targeted and
controlled drug release in vitro and exhibited a significant
effect in the treatment of breast cancer, with a low toxicity in
vivo.
Conclusion
Cancer is a common disease that seriously affects
human health and reversal of MDR in cancer has long been a topic of
research. However, due to the complex and diverse resistance
mechanisms of cancer, the limitation of biological activity and
toxicity of MDR reversal agents, the existing reversal agents
cannot meet the requirements of treatment. Compared with
traditional anticancer drugs, nanodrug delivery systems show a
clear advantage in terms of reversing MDR during the process of
tumor therapy. Novel drug-loaded nanoparticle systems, such as the
co-entrapped reversal agents and chemotherapy drugs and the
co-loaded P-gp inhibitors and chemotherapy drugs, and the specific
modification of nanoparticles may alter the transmission method and
the targeting of drugs and antagonize the drug efflux by tumor
cells. Thus, the accumulation of drug within the tumor cells may be
improved. The good biocompatibility, high stability, drug release
and targeting of nanodrug delivery systems overcome the
shortcomings of the traditional drug delivery system, and show
great promise in cancer MDR reversal. However, with the enhanced
targeting, the tissue distribution of drugs has also changed and
led to new adverse reactions; therefore, additional in vivo
evaluation of safety and efficacy data are urgently required.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 81273707 and 81173215), the
Ministry of Education in the New Century Excellent Talents (grant
no. NECT-12-0677), the Natural Science Foundation of Guangdong
(grant nos. S2013010012880 and 2016A030311037), the Science and
Technology Program of Guangzhou (grant no. 2014J4500005), the
Science Program of the Department of Education of Guangdong (grant
nos. 2013KJCX0021 and 2015KGJHZ012) and the Science and Technology
Program of Guangdong (grant no. 2015A050502027).
Glossary
Abbreviations
Abbreviations:
|
MDR
|
multidrug resistance
|
|
SLNs
|
solid lipid nanoparticles
|
|
NLCs
|
nanostructured lipid carriers
|
|
PLN
|
polymer-lipid hybrid nanoparticle
|
|
MSNs
|
mesoporous silica nano drug delivery
systems
|
References
|
1
|
Gottesman MM, Fojo T and Bates SE:
Multidrug resistance in cancer: Role of ATP-dependent transporters.
Nat Rev Cancer. 2:48–58. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gottesman MM and Ling V: The molecular
basis of multidrug resistance in cancer: The early years of
P-glycoprotein research. FEBS Lett. 580:998–1009. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Choi CH: ABC transporters as multidrug
resistance mechanisms and the development of chemosensitizers for
their reversal. Cancer Cell Int. 5:302005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Noguchi K, Katayama K, Mitsuhashi J and
Sugimoto Y: Functions of the breast cancer resistance protein
(BCRP/ABCG2) in chemotherapy. Adv Drug Deliv Rev. 61:26–33. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sugimoto Y, Tsukahara S, Ishikawa E and
Mitsuhashi J: Breast cancer resistance protein: Molecular target
for anticancer drug resistance and
pharmacokinetics/pharmacodynamics. Cancer Sci. 96:457–465. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang F, Wang YC, Dou S, Xiong MH, Sun TM
and Wang J: Doxorubicin-tethered responsive gold nanoparticles
facilitate intracellular drug delivery for overcoming multidrug
resistance in cancer cells. ACS Nano. 5:3679–3692. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Diao YY, Han M, Chen DW and Gao JQ:
Progress in the study of micelle delivery system reversing
multidrug resistance. Yao Xue Xue Bao. 44:710–715. 2009.(In
Chinese). PubMed/NCBI
|
|
8
|
Kapse-Mistry S, Govender T, Srivastava R
and Yergeri M: Nanodrug delivery in reversing multidrug resistance
in cancer cells. Front Pharmacol. 5:1592014.PubMed/NCBI
|
|
9
|
Hu CM and Zhang L: Therapeutic
nanoparticles to combat cancer drug resistance. Curr Drug Metab.
10:836–841. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chidambaram M, Manavalan R and Kathiresan
K: Nanotherapeutics to overcome conventional cancer chemotherapy
limitations. J Pharm Pharm Sci. 14:67–77. 2011.PubMed/NCBI
|
|
11
|
Cho K, Wang X, Nie S, Chen ZG and Shin DM:
Therapeutic nanoparticles for drug delivery in cancer. Clin Cancer
Res. 14:1310–1316. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang J, Sui M and Fan W: Nanoparticles for
tumor targeted therapies and their pharmacokinetics. Curr Drug
Metab. 11:129–141. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Markman JL, Rekechenetskiy A, Holler E and
Ljubimova JY: Nanomedicine therapeutic approaches to overcome
cancer drug resistance. Adv Drug Deliv Rev. 65:1866–1879. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kirtane AR, Kalscheuer SM and Panyam J:
Exploiting nanotechnology to overcome tumor drug resistance:
Challenges and opportunities. Adv Drug Deliv Rev. 65:1731–1747.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lao J, Madani J, Puértolas T, Alvarez M,
Hernández A, Pazo-Cid R, Artal A and Antón Torres A: Liposomal
doxorubicin in the treatment of breast cancer patients: A review. J
Drug Deliv. 2013:4564092013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rivera E: Liposomal anthracyclines in
metastatic breast cancer: Clinical update. Oncologist. 8(Suppl 2):
3–9. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lorusso V, Manzione L and Silvestris N:
Role of liposomal anthracyclines in breast cancer. Ann Oncol.
18(Suppl 6): vi70–vi73. 2007.PubMed/NCBI
|
|
18
|
Arias JL, Clares B, Morales ME, Gallardo V
and Ruiz MA: Lipid-based drug delivery systems for cancer
treatment. Curr Drug Targets. 12:1151–1165. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Samad A, Sultana Y and Aqil M: Liposomal
drug delivery systems: An update review. Curr Drug Deliv.
4:297–305. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lian T and Ho RJ: Trends and developments
in liposome drug delivery systems. J Pharm Sci. 90:667–680. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Goyal P, Goyal K, Kumar Vijaya SG, Singh
A, Katare OP and Mishra DN: Liposomal drug delivery
systems-clinical applications. Acta Pharm. 55:1–25. 2005.PubMed/NCBI
|
|
22
|
Zhou WJ, Zhou W, Jia SW, et al: The
cytology evaluation of doxorubicin liposomes to overcome multidrug
resistance in vitro. Zhong Guo Yi Yuan Yao Xue Za Zhi.
32:1349–1352. 2012.(In Chinese).
|
|
23
|
Kang DI, Kang HK, Gwak HS, Han HK and Lim
SJ: Liposome composition is important for retention of liposomal
rhodamine in p-glycoprotein-overexpressing cancer cells. Drug
Deliv. 16:261–267. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shidhaye SS, Vaidya R, Sutar S, Patwardhan
A and Kadam VJ: Solid lipid nanoparticles and nanostructured lipid
carriers-innovative generations of solid lipid carriers. Curr Drug
Deliv. 5:324–331. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li XW, Sun LX, Lin XH and Zeng LQ: Solid
lipid nanoparticles as drug delivery system. Prog Chem. 19:87–92.
2007.
|
|
26
|
Xu DH, Gao JQ, Liang WQ, Yang JM and Yao
Q: Progress of solid lipid nanoparticles in overcoming multidrug
resistance. Zhong Guo Yao Xue Za Zhi. 45:401–403. 2010.
|
|
27
|
Wong HL, Bendayan R, Rauth AM and Wu XY:
Development of solid lipid nanoparticles containing ionically
complexed chemotherapeutic drugs and chemosensitizers. J Pharm Sci.
93:1993–2008. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wong HL, Rauth AM, Bendayan R, Manias JL,
Ramaswamy M, Liu Z, Erhan SZ and Wu XY: A new polymer-lipid hybrid
nanoparticle system increases cytotoxicity of doxorubicin against
multidrug-resistant human breast cancer cells. Pharm Res.
23:1574–1585. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wong HL, Rauth AM, Bendayan R and Wu XY:
In vivo evaluation of a new polymer-lipid hybrid nanoparticle (PLN)
formulation of doxorubicin in a murine solid tumor model. Eur J
Pharm Biopharm. 65:300–308. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wong HL, Bendayan R, Rauth AM and Wu XY:
Simultaneous delivery of doxorubicin and GG918 (Elacridar) by new
polymer-lipid hybrid nanoparticles (PLN) for enhanced treatment of
multidrug-resistant breast cancer. J Control Release. 116:275–284.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Shuhendler AJ, Prasad P, Zhang RX, Amini
MA, Sun M, Liu PP, Bristow RG, Rauth AM and Wu XY: Synergistic
nanoparticulate drug combination overcomes multidrug resistance,
increases efficacy, and reduces cardiotoxicity in a
nonimmunocompromised breast tumor model. Mol Pharm. 11:2659–2674.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Prasad P, Cheng J, Shuhendler A, Rauth AM
and Wu XY: A novel nanoparticle formulation overcomes multiple
types of membrane efflux pumps in human breast cancer cells. Drug
Deliv Transl Res. 2:95–105. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Miao J, Du YZ, Yuan H, Zhang XG and Hu FQ:
Drug resistance reversal activity of anticancer drug loaded solid
lipid nanoparticles in multi-drug resistant cancer cells. Colloids
Surf B Biointerfaces. 110:74–80. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bourseau-Guilmain E, Béjaud J, Griveau A,
Lautram N, Hindré F, Weyland M, Benoit JP and Garcion E:
Development and characterization of immuno-nanocarriers targeting
the cancer stem cell marker ac133. Int J Pharm. 423:93–101. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sahoo SK and Labhasetwar V: Enhanced
antiproliferative activity of transferrin-conjugated
paclitaxel-loaded nanoparticles is mediated via sustained
intracellular drug retention. Mol Pharm. 2:373–383. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhang MZH, Chen HG and Han J: Advances in
drug carrier to overcome mdr. Jie Fang Jun Yao Xue Xue Bao.
30:256–259. 2014.
|
|
37
|
Ye G, Ke AW and Li X: The mrk-16 modified
immune doxorubicin liposome in reversing multidrug resistance of
cancer cells. Journal of Modern Oncology. 15:754–757. 2007.
|
|
38
|
Zhang Y, Huang Y and Li S: Polymeric
micelles: Nanocarriers for cancer-targeted drug delivery. AAPS
PharmSciTech. 15:862–871. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tian Y and Mao S: Amphiphilic polymeric
micelles as the nanocarrier for peroral delivery of poorly soluble
anticancer drugs. Expert Opin Drug Deliv. 9:687–700. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Croy SR and Kwon GS: Polymeric micelles
for drug delivery. Curr Pharm Des. 12:4669–4684. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Adams ML, Lavasanifar A and Kwon GS:
Amphiphilic block copolymers for drug delivery. J Pharm Sci.
92:1343–1355. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Han SS, Li ZY, Zhu JY, Han K, Zeng ZY,
Hong W, Li WX, Jia HZ, Liu Y, Zhuo RX and Zhang XZ: Dual-pH
sensitive charge-reversal polypeptide micelles for tumor-triggered
targeting uptake and nuclear drug delivery. Small. 11:2543–2554.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Torchilin VP: Passive and active drug
targeting: Drug delivery to tumors as an example. Handb Exp
Pharmacol. 197:3–53. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kedar U, Phutane P, Shidhaye S and Kadam
V: Advances in polymeric micelles for drug delivery and tumor
targeting. Nanomedicine. 6:714–729. 2010.PubMed/NCBI
|
|
45
|
Prabhu RH, Patravale VB and Joshi MD:
Polymeric nanoparticles for targeted treatment in oncology: Current
insights. Int J Nanomedicine. 10:1001–1018. 2015.PubMed/NCBI
|
|
46
|
Mao SR, Tian Y and Wang LL: Advances in
drug nanocarriers: Polymer micelles. Shenyang Yao Ke Da Xue Xue
Bao. 27:979–986. 2010.
|
|
47
|
Zhang HJ, Zhang C and Ping QN: Research
and application of polymeric micelles as a pharmaceutically
acceptable carrier. Yao Xue Jin Zhan. 26:326–329. 2002.
|
|
48
|
Saiyin W, Wang D, Li L, Zhu L, Liu B,
Sheng L, Li Y, Zhu B, Mao L, Li G and Zhu X: Sequential release of
autophagy inhibitor and chemotherapeutic drug with polymeric
delivery system for oral squamous cell carcinoma therapy. Mol
Pharm. 11:1662–1675. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yu J, Deng H, Xie F, Chen W, Zhu B and Xu
Q: The potential of pH-responsive PEG-hyperbranched
polyacylhydrazone micelles for cancer therapy. Biomaterials.
35:3132–3144. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ganta S and Amiji M: Coadministration of
paclitaxel and curcumin in nanoemulsion formulations to overcome
multidrug resistance in tumor cells. Mol Pharm. 6:928–939. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Katsman A, Umezawa K and Bonavida B:
Chemosensitization and immunosensitization of resistant cancer
cells to apoptosis and inhibition of metastasis by the specific
NF-kappaB inhibitor DHMEQ. Curr Pharm Des. 15:792–808. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yadav S, Van Vlerken LE, Little SR and
Amiji MM: Evaluations of combination MDR-1 gene silencing and
paclitaxel administration in biodegradable polymeric nanoparticle
formulations to overcome multidrug resistance in cancer cells.
Cancer Chemother Pharmacol. 63:711–722. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Iyer AK, Singh A, Ganta S and Amiji MM:
Role of integrated cancer nanomedicine in overcoming drug
resistance. Adv Drug Deliv Rev. 65:1784–1802. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Li J, Wang Y, Zhu Y and Oupický D: Recent
advances in delivery of drug-nucleic acid combinations for cancer
treatment. J Control Release. 172:589–600. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hu ZX and Fu XD: The progress of
nanoparticles drug delivery system in mdr of tumor and its
reversal. Zhong Guo Yi Yuan Yao Xue Za Zhi. 31:1724–1727. 2011.
|
|
56
|
Chen JN, Shen Q and Li SS: Progress in the
study of drug delivery system based on nanoparticles to overcome
multi-drug resistance. Yao Xue Xue Bao. 44:333–337. 2009.(In
Chinese). PubMed/NCBI
|
|
57
|
Qin Y, Li M, Qiu Q, Pi JT and Chen HY: The
application of nanoparticles drug delivery system in multi-drug
resistance of tumor. Xian Dai Sheng Wu Yi Xue Jin Zhan.
14:55645599. –5600. 2014.
|
|
58
|
Abouzeid AH, Patel NR and Torchilin VP:
Polyethylene glycol-phosphatidylethanolamine (PEG-PE)/vitamin e
micelles for co-delivery of paclitaxel and curcumin to overcome
multi-drug resistance in ovarian cancer. Int J Pharm. 464:178–184.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tang J, Zhang L, Gao H, Liu Y, Zhang Q,
Ran R, Zhang Z and He Q: Co-delivery of doxorubicin and P-gp
inhibitor by a reduction-sensitive liposome to overcome multidrug
resistance, enhance anti-tumor efficiency and reduce toxicity. Drug
Deliv. 1–14. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wang X, Teng ZG, Huang XY and Lu GM:
Mesoporous silica nanoparticles for cancer theranostic drug
delivery. Yao Xue Xue Bao. 48:8–13. 2013.(In Chinese). PubMed/NCBI
|
|
61
|
Jiang XX, Yang H and Yang Y: Silicon
nanometer carrier with rna interference plasmid in reversing mdr in
human colon cancer. Practical Preventive Medicine. 20:1385–1389.
2013.
|
|
62
|
Hom C, Lu J, Liong M, Luo H, Li Z, Zink JI
and Tamanoi F: Mesoporous silica nanoparticles facilitate delivery
of siRNA to shutdown signaling pathways in mammalian cells. Small.
6:1185–1190. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Slowing II, Vivero-Escoto JL, Wu CW and
Lin VS: Mesoporous silica nanoparticles as controlled release drug
delivery and gene transfection carriers. Adv Drug Deliv Rev.
60:1278–1288. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zhao Y, Vivero-Escoto JL, Slowing II,
Trewyn BG and Lin VS: Capped mesoporous silica nanoparticles as
stimuli-responsive controlled release systems for intracellular
drug/gene delivery. Expert Opin Drug Deliv. 7:1013–1029. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Pan L, Liu J, He Q, Wang L and Shi J:
Overcoming multidrug resistance of cancer cells by direct
intranuclear drug delivery using TAT-conjugated mesoporous silica
nanoparticles. Biomaterials. 34:2719–2730. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
He Q and Shi J: MSN anti-cancer
nanomedicines: Chemotherapy enhancement, overcoming of drug
resistance and metastasis inhibition. Adv Mater. 26:391–411. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Vivero-Escoto JL, Slowing II, Trewyn BG
and Lin VS: Mesoporous silica nanoparticles for intracellular
controlled drug delivery. Small. 6:1952–1967. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Tang F, Li L and Chen D: Mesoporous silica
nanoparticles: Synthesis, biocompatibility and drug delivery. Adv
Mater. 24:1504–1534. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Gao Y, Chen Y, Ji X, He X, Yin Q, Zhang Z,
Shi J and Li Y: Controlled intracellular release of doxorubicin in
multidrug-resistant cancer cells by tuning the shell-pore sizes of
mesoporous silica nanoparticles. ACS Nano. 5:9788–9798. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Meng H, Liong M, Xia T, Li Z, Ji Z, Zink
JI and Nel AE: Engineered design of mesoporous silica nanoparticles
to deliver doxorubicin and P-glycoprotein siRNA to overcome drug
resistance in a cancer cell line. ACS Nano. 4:4539–4550. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Zhang X, Li F, Guo S, Chen X, Wang X, Li J
and Gan Y: Biofunctionalized polymer-lipid supported mesoporous
silica nanoparticles for release of chemotherapeutics in multidrug
resistant cancer cells. Biomaterials. 35:3650–3665. 2014.
View Article : Google Scholar : PubMed/NCBI
|