Introduction
Despite recent advances in detection and treatment,
colorectal cancer (CRC) remains the third most common type of
cancer and a major cause of cancer-related mortality worldwide
(1,2).
There have been a number of recent advances in CRC screening.
Probing a combination of sensitive and specific molecular markers
could be particularly promising for early diagnosis, prediction of
drug response and other clinical applications (3). Survivin is a member of the inhibitor of
apoptosis protein family. High survivin expression levels are
associated with poor outcomes in the majority of cancer types
(4–9).
There is also evidence of survivin expression in specific adult
tissues, including healthy oral epithelium, colonic epithelium,
placenta and healthy endometrium (4,10,11). A recent study reported that survivin
can also act as a subunit of the chromosomal passenger complex
(CPC), and direct the other subunits of CPC such as Aurora-B,
Borealin and the inner centromere protein to regulate chromosome
separation and cell division (4,12).
Mucins are high-molecular-weight, heavily
glycosylated proteins (13). At
present, >20 mucin types have been identified and classified
into two separate classes according to their structure and function
(14). The two structurally and
functionally distinct classes are: i) Secreted gel-forming mucins
(MUC2, MUC5AC, MUC5B and MUC6) and ii) transmembrane mucins (MUC1,
MUC3A, MUC3B, MUC4, MUC12 and MUC17). The MUC2 glycoprotein is a
secreted mucin that consists of two distinct regions with a high
degree of internal homology (15).
MUC2 is commonly expressed in the healthy colonic epithelium and
expression is decreased in non-mucinous colon adenocarcinomas
(16–18). MUC2 and MUC5AC are clustered at the
same chromosomal locus (11p15.5), and their expression and function
may be regulated by a common mechanism (19). The MUC5AC gene is primarily expressed
in the gastric and tracheobronchial mucosa; however, MUC5AC is not
expressed in the healthy colonic epithelium (20). Although the expression of MUC5AC
increases in differentiated CRC, the absence of MUC5AC expression
in tumors can be a prognostic factor for more aggressive colon
adenocarcinomas (21). Moreover, the
expression of MUC2 and MUC5 is regulated by an extracellular
signal-regulated kinase pathway in epithelial growth factor
(EGF)/RAS proto-oncogene, GTPase (Ras)/Raf proto-oncogene,
serine/threonine kinase (Raf)-positive cells (22). A study have indicated that EGF-mutant
cancer cell lines express high levels of survivin (23). At present, however, to the best of our
knowledge, no studies have investigated the link between survivin
expression and MUC2/MUC5 expression in CRC. In the present study,
the expression of survivin and its association with MUC2, MUC5 and
the clinicopathological features of CRC were examined.
Materials and methods
Patients and tissue samples
CRC and normal tissue samples were obtained from 6
patients who underwent surgery at the Affiliated Hospital of Guilin
Medical University (Guilin, China). A total of 20 normal colon
mucosa samples and 139 advanced carcinomas (76 men and 63 women)
were obtained from the Affiliated Hospital of Guilin Medical
University and the archive of Hiroshima University Hospital
(Hiroshima, Japan). All samples were obtained following approval by
the Ethics Committees of Guilin Medical University and Hiroshima
University. All patient records were complete, and each diagnosis
was obtained by attending clinicians. Histologically, 117 carcinoma
cases were classified as well/moderately differentiated and 22 as
poorly differentiated according to the criteria of the Japanese
Society for colorectal cancer (10,11).
Tissues from each patient were fixed in formalin, cut into parallel
4–5-mm sections and embedded in paraffin. Tissue sections 4-µm
thick were stained with hematoxylin and eosin for
immunohistochemical examination. Informed consent was obtained from
all subjects.
Immunohistochemistry
For immunohistochemical examination, tissue sections
(4 µm) were incubated with the following primary antibodies: MUC2
(catalog no. NCL-MUC2; mouse monoclonal antibody, dilution, 1:100;
Novocastra; Leica Microsystems GmbH, Wetzlar, Germany), MUC5
(catalog no. NCL-MUC5; mouse monoclonal antibody, dilution 1:100;
Novocastra; Leica Microsystems GmbH), survivin (cat no. NB500-201,
dilution, 1:1,000; Novus Biologicals, LLC, Littleton, CO, USA) and
Ki-67 (cat no. M7240, MIB-1, mouse monoclonal antibody, dilution,
1:100; Dako; Agilent Technologies, Inc., Santa Clara, CA, USA). All
were incubated at 4°C overnight following antigen retrieval by
microwave treatment in citrate buffer (pH 6.0; ZSGB-Bio, Beijing,
China) and detection by the avidin-biotin peroxidase complex system
using a labeled streptavidin-biotin kit (Dako; Agilent
Technologies, Inc.) according to manufacturers's protocol. For
MUC2, MUC5, survivin and Ki-67, immunoreactivity was graded
according to the percentage of positive tumor cells as follows:
Strong, >60% of tumor cells intensely stained; moderate, >20%
intensely stained; mild, 5–20% intensely stained; or negative,
<5% intensely stained. The expression levels of Survivin MUC2,
MUC5 and Ki-67 were also graded as high (>20% of positive cells)
or low (<20% of positive cells).
Western blot analysis
Colorectal tissues were lysed in
radioimmunoprecipitation lysis buffer (cat no. R0020; Beijing
Solarbio Science and Technology Co., Ltd., Beijing, China)
according to manufacturer's protocol. Protein concentrations were
detected by the Bradford method, using bovine serum albumin
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) as the standard.
Equal amounts of tissue extract (40 µg) underwent 10% SDS-PAGE
separation and were then transferred to a nitrocellulose membrane
(Bio-Rad Laboratories, Inc., Hercules, CA, USA) for antibody
blotting. The membrane was then blocked with 5% nonfat dried milk
(Santa Cruz Biotechnology, Inc., Dallas, TX, USA) at room
temperature for 1 h, and incubated with primary antibodies at 4°C
overnight and secondary antibodies (cat no. sc-2004, sc-2005,
dilution, 1:2,000; Santa Cruz Biotechnology, Inc.) for 1 h at room
temperature and then an enhanced chemiluminescence kit (cat no.
170-5061; Clarity™ Western ECL Substrate; Bio-Rad Laboratories,
Inc.) was used for visualization of specific protein antigens.
Then, images of the membrane were captured in a darkroom, and the
results were analyzed. The primary antibodies were anti-MUC2 (cat
no. NCL-MUC2; mouse monoclonal antibody; dilution 1:1,000;
Novocastra; Leica Microsystems GmbH), anti-MUC5 (cat no. NCL-MUC5;
mouse monoclonal antibody, dilution, 1:1,000; Novocastra; Leica
Microsystems GmbH), anti-survivin (cat no. NB500-201, dilution,
1:2,000; Novus Biologicals, LLC) and anti-β-actin (cat no. TA-09,
dilution, 1:5,000; ZSGB-Bio).
Statistical analysis
The SPSS software package v.17.0 (SPSS, Inc.,
Chicago, IL, USA) was used for analysis. A χ2 test was
used for comparison of data between groups. Survival analyses were
conducted using the Kaplan-Meier method and survival
characteristics were compared using log-rank tests. P<0.05 was
considered to indicate a statistically significant difference.
Results
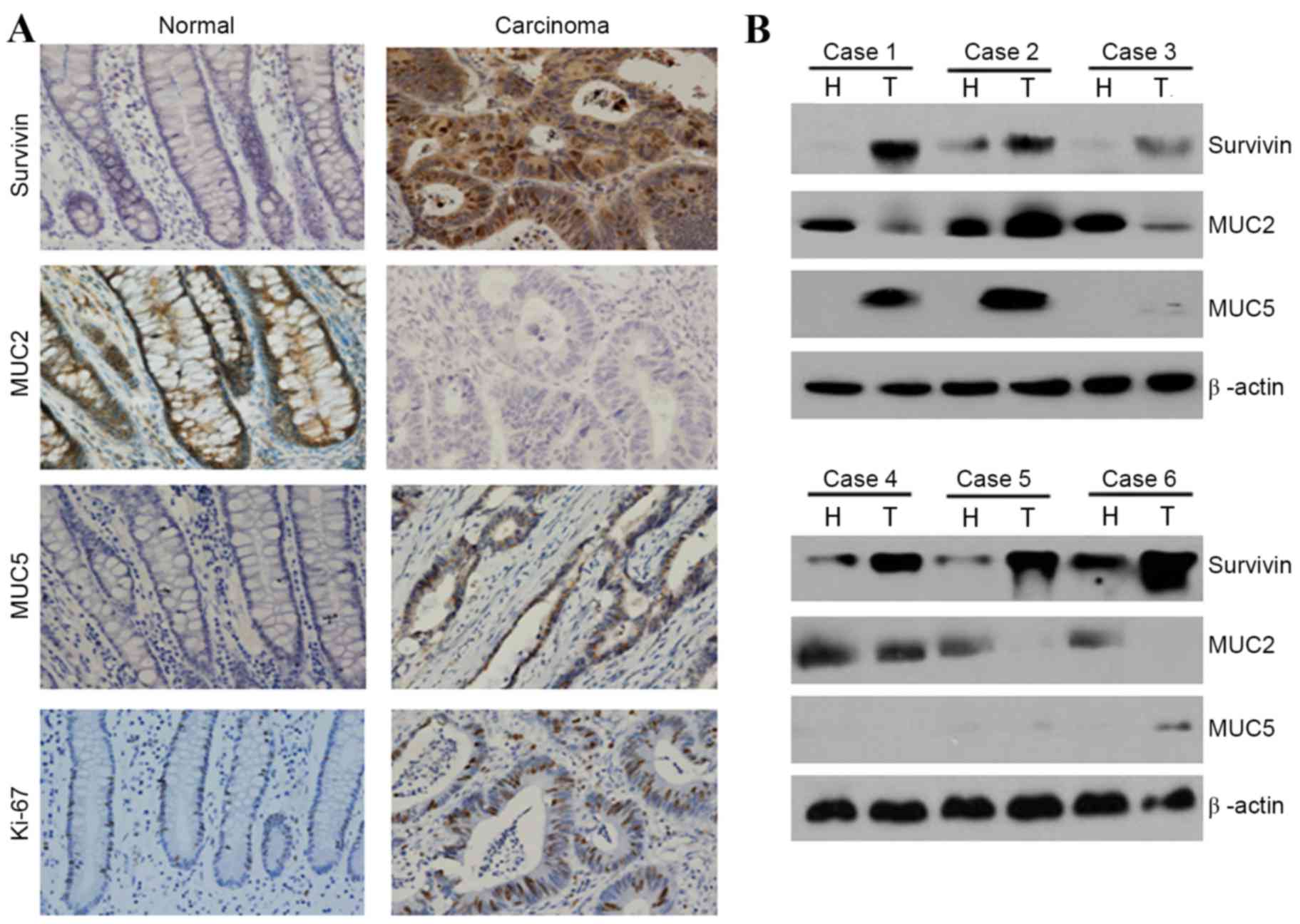
Expression of survivin, MUC2 and MUC5
in healthy and cancerous colon mucosa
Expression levels of survivin, MUC2 and MUC5 were
measured by immunohistochemical methods in 20 normal colon mucosa
samples and 139 carcinoma cases. High survivin expression rates
(nucleus, cytoplasmic staining) in healthy colon mucosa and CRC
cases were 0% (0/20) and 39.57% (55/139), respectively (Table I and Fig.
1A). Rates of high MUC2 expression (cytoplasmic staining) in
the healthy colon mucosa and in CRC tissue were 100% (20/20) and
48.20% (67/139), respectively (Table
I and Fig. 1A). Rates of high
MUC5 expression (cytoplasmic staining) in the healthy colon mucosa
and CRC tissue were 0% (0/20) and 28.06% (39/139), respectively
(Table I and Fig. 1A). In conclusion, the expression and
staining intensity of survivin and MUC5 were significantly
increased in CRC tissues (P<0.01), whereas those of MUC2 were
significantly decreased in CRC tissues (P<0.01).
 | Table I.Survivin, MUC2 and MUC5 expression in
normal colon mucosa and cancer. |
Table I.
Survivin, MUC2 and MUC5 expression in
normal colon mucosa and cancer.
|
|
| Survivin expression,
n |
| MUC2 expression,
n |
| MUC5 expression,
n |
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| Tissue type | Total | Low | High | P-value | Low | High | P-value | Low | High | P-value |
|---|
| Normal | 20 | 20 | 0 | <0.01a | 0 | 20 | <0.01a | 20 | 0 | <0.01a |
| Cancer | 139 | 84 | 55 |
| 72 | 67 |
| 100 | 39 |
|
Western blot analysis revealed that the expression
levels of survivin and MUC5 in healthy colon mucosa tissues were
lower than levels in CRC tissues (Fig.
1B). However, expression levels of MUC2 in the healthy colon
mucosa were higher than levels in CRC tissues (Fig. 1B). These findings support the
immunohistochemical data, as high expression of MUC2 was observed
in healthy colon mucosa, whereas high expression of survivin and
MUC5 was observed in CRC cells (Fig.
1B).
Survivin expression and correlation
with MUC2, MUC5, Ki-67 and clinicopathological features in CRC
The present study examined the correlation between
survivin, MUC2, MUC5 and Ki-67 in CRC cases. A total of 55/139
patients with CRC exhibited high survivin expression levels
(Table II). Moreover, of the 55
patients with high survivin expression, 28 exhibited high
expression of MUC5 and 41 exhibited high expression of Ki-67,
whereas 40 patients exhibited low expression of MUC2. This
demonstrated that survivin expression was directly associated with
MUC5 and Ki-67 expression, and inversely correlated with MUC2
expression in CRC (P<0.01).
 | Table II.Survivin expression and its
correlation with MUC2 and MUC5 expression in colorectal cancer. |
Table II.
Survivin expression and its
correlation with MUC2 and MUC5 expression in colorectal cancer.
|
| Survivin
expression |
|
|---|
|
|
|
|
|---|
| Clinicopathological
factor | Low (n=84) | High (n=55) | P-value |
|---|
| MUC2 expression,
n |
|
| <0.01 |
|
Low | 32 | 40 |
|
|
High | 52 | 15 |
|
| MUC5 expression,
n |
|
| <0.01 |
|
Low | 73 | 27 |
|
|
High | 11 | 28 |
|
| Ki-67 expression,
n |
|
| <0.01 |
|
Low | 57 | 14 |
|
|
High | 27 | 41 |
|
Patients with high survivin expression levels
demonstrated significantly increased incidences of lymph node
metastasis (P<0.01) and stage-D tumors (P<0.01) (8 Edition,
Japanese Classification of Colorectal Carcinoma) (10,11)
compared with cases exhibiting low survivin expression levels
(Table III). However, no evidence
of association between survivin expression level and tumor size,
gender or histological differentiation was found.
 | Table III.Survivin expression and its
correlation with clinicopathological findings in colorectal
cancer. |
Table III.
Survivin expression and its
correlation with clinicopathological findings in colorectal
cancer.
|
| Survivin
expression |
|
|---|
|
|
|
|
|---|
| Clinicopathological
factor | Low (n=84) | High (n=55) | P-value |
|---|
| Tumor size (mm),
n |
|
| 0.56 |
|
≥50 | 37 | 27 |
|
|
<50 | 47 | 28 |
|
| Histological
differentiation, n |
|
| <0.01 |
|
Poor | 10 | 12 |
|
|
Well/moderate | 74 | 43 |
|
| Lymph node
metastasis, n |
|
| <0.01 |
|
Negative | 60 | 16 |
|
|
Positive | 24 | 39 |
|
| Sex, n |
|
| 0.31 |
|
Male | 43 | 33 |
|
|
Female | 41 | 22 |
|
| Tumor stage, n |
|
| <0.01 |
|
B/C | 76 | 39 |
|
| D | 8 | 16 |
|
Patients with low MUC2 expression levels
demonstrated significantly lower cell differentiation (P<0.01)
and higher incidences of lymph node metastasis (P<0.05) and
stage-D tumors (P<0.01) when compared with cases displaying high
expression of MUC2 (Table IV). The
association between clinicopathological factors and MUC5 expression
in CRC was also examined. In comparison to MUC2, patients
expressing high levels of MUC5 tended to exhibit poor CRC cell
differentiation (P<0.05), higher rates of lymph node metastasis
(P<0.01) and higher tumor stage (P<0.01) (Table IV).
 | Table IV.MUC2 and MUC5 expression and its
correlation with clinicopathological findings in colorectal
cancer. |
Table IV.
MUC2 and MUC5 expression and its
correlation with clinicopathological findings in colorectal
cancer.
|
| MUC2
expression |
| MUC5
expression |
|
|---|
|
|
|
|
|
|
|---|
| Clinicopathological
factor | Low (n=72) | High (n=67) | P-value | Low (n=100) | High (n=39) | P-value |
|---|
| Tumor size (mm),
n |
|
| 0.099 |
|
| 0.99 |
|
≥50 | 38 | 26 |
| 46 | 18 |
|
|
<50 | 34 | 41 |
| 54 | 21 |
|
| Histological
differentiation, n |
|
| <0.01 |
|
| <0.05 |
|
Poor | 17 | 5 |
| 12 | 10 |
|
|
Well/moderate | 55 | 62 |
| 88 | 29 |
|
| Lymph node
metastasis, n |
|
| <0.05 |
|
| <0.01 |
|
Negative | 34 | 43 |
| 66 | 11 |
|
|
Positive | 38 | 24 |
| 34 | 28 |
|
| Sex, n |
|
|
|
|
| 0.21 |
|
Male | 38 | 38 |
| 58 | 18 |
|
|
Female | 34 | 29 |
| 42 | 21 |
|
| Tumor stage, n |
|
| <0.01 |
|
| <0.01 |
|
B/C | 54 | 61 |
| 90 | 25 |
|
| D | 18 | 6 |
| 10 | 14 |
|
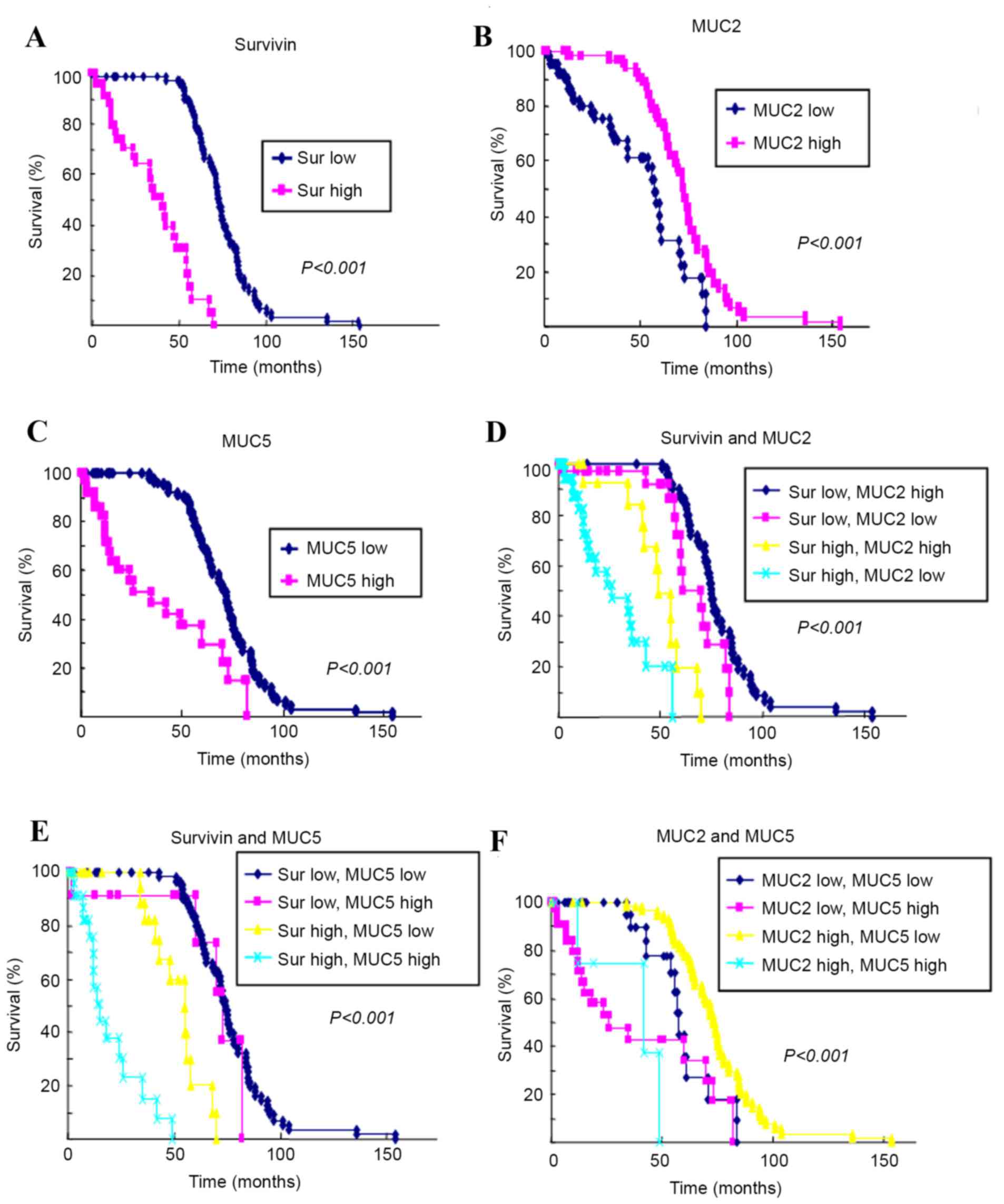
Survival analysis
The Kaplan-Meier method was used to assess the
survival rate of 139 patients who expressed survivin, MUC2 and MUC5
(Fig. 2). The 5-year survival rate of
those whose tumors expressed low levels of survivin and MUC5 was
higher than that of patients with high expression levels of
survivin and MUC5. By comparison, the 5-year survival rate of those
with tumors expressing high levels of MUC2 was higher than that of
patients whose tumors expressed low levels of MUC2.
Discussion
Survivin is a bifunctional protein that suppresses
apoptosis and regulates cell division, which is highly expressed in
various cancer types (12).
Additionally, >20 mucins are classified as either secreted
mucins or transmembrane mucins according to their structure and
function (13). MUC2 and MUC5 are
secreted mucins. However, to the best of our knowledge, there have
been no studies to date investigating the correlation of survivin
expression with MUC2 and MUC5 expression in CRC. The present study
focused on the expression levels of survivin, MUC2 and MUC5 in
healthy and CRC tissues using immunohistochemical analysis.
Additionally, the present study aimed to investigate the potential
of these biomarkers to aid in the early diagnosis of CRCs, as well
as other clinical applications.
In this study, survivin was revealed to be expressed
at high levels in CRC tissues, but at low levels in healthy colon
tissues (Fig. 1 and Table I). Moreover, patients with high
expression of survivin demonstrated significantly poorer cellular
differentiation, higher rates of lymph node metastasis and a higher
incidence of stage-D tumors than did cases with low expression of
survivin. Furthermore, overexpression of survivin has previously
been found to be associated with poor prognosis in CRC, HCC, and
head and neck cancer (4,10–12).
The present study also examined the expression
levels of MUC2 and MUC5 in healthy colon mucosa and in CRC
patients. MUC2 was found to be expressed at high levels in normal
colon tissue and at lower levels in CRC tissue (Fig. 1 and Table
I). Moreover, cases with low expression of MUC2 demonstrated
significantly poorer cell differentiation, higher rates of lymph
node metastasis and a higher incidence of stage-D tumors compared
with cases with high levels of expressed MUC2. Similarly, several
studies have shown that loss of MUC2 expression is correlated with
poor prognosis in CRC (24–26). Notably, however, another study found
that overexpression of MUC2 is associated with poorer overall
survival (27). In a further previous
study, decreased expression of MUC2 was found to be associated with
colon carcinogenesis, decreased apoptosis and increased migration
of intestinal epithelial cells (20).
A number of studies have shown that low expression
of MUC2 is associated with poorly differentiated adenocarcinoma of
the colon and rectum (28,29). By contrast, in the present study, MUC5
was expressed at high levels in CRC tissues but at low levels in
normal colon tissues (Fig. 1 and
Table I). Similarly, other studies
have shown that MUC5AC is not detected in the normal colon, but is
frequently found in adenomas and carcinomas (18,30–32). Other
prior studies reported that an increase in expression of MUC5AC was
observed in sporadic cancer with high microsatellite instability
(33) and that MUC5AC expression in
intrahepatic cholangiocarcinoma was found to be an independent
prognostic factor by multivariate survival analysis (34). The presence of MUC2 and/or MUC5AC in
colorectal mucinous adenocarcinoma has been shown to be associated
with proximal (right-sided) CRC location (32,33). There
was no statistically significant association between gender and
expression of MUC2 and/or MUC5 in the present study. Expression of
survivin was also compared with the expression of MUC2, MUC5 and
Ki-67 (Fig. 1; Table II). Survivin expression was found to
be directly correlated with MUC5 and Ki-67 expression, and
inversely correlated with MUC2 expression (Fig. 1 and Table
II). These findings led to the hypothesis that survivin and
MUC5 are expressed at high levels in CRC, whereas low MUC2
expression levels confer a poor prognosis in CRC.
In conclusion, the present study revealed that the
normal-to-carcinoma sequence was significantly associated with the
high expression and staining intensity of survivin and MUC5
(P<0.01), and the low expression of MUC2. Additionally, cases
with high expression of survivin and MUC5 and/or low expression of
MUC2 demonstrated significantly increased rates of lymph node
metastasis and incidences of advanced tumor stage. Therefore,
increased survivin and MUC5 or decreased MUC2 expression levels are
associated with the malignant potential of colon carcinoma. Further
investigations using appropriate techniques based on clinical data
are required to confirm the present findings.
Acknowledgements
This research was supported in part by grants from
The National Natural Science Foundation of China (no. 81460411),
Guangxi University of Science and Technology Research Projects (no.
ZD20140094), Guangxi Undergraduate Innovation Program
(201510601016) The Natural Science Foundation of Guangxi (grant no.
2015GXNSFAA139110).
References
|
1
|
Klimczak A, Kempińska-Mirosławska B, Mik
M, Dziki L and Dziki A: Incidence of colorectal cancer in Poland in
1999–2008. Arch Med Sci. 7:673–678. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferlay J, Steliarova-Foucher E,
Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, Forman D and
Bray F: Cancer incidence and mortality patterns in Europe:
Estimates for 40 countries in 2012. Eur J Cancer. 49:1374–1403.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Anderson JC and Shaw RD: Update on colon
cancer screening: Recent advances and observations in colorectal
cancer screening. Curr Gastroenterol Rep. 16:4032014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Qi G, Kudo Y, Ando T, Tsunematsu T,
Shimizu N, Siriwardena SB, Yoshida M, Keikhaee MR, Ogawa I and
Takata T: Nuclear Survivin expression is correlated with malignant
behaviors of head and neck cancer together with Aurora-B. Oral
Oncol. 46:263–270. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Qi G, Ogawa I, Kudo Y, Miyauchi M,
Siriwardena BS, Shimamoto F, Tatsuka M and Takata T: Aurora-B
expression and its correlation with cell proliferation and
metastasis in oral cancer. Virchows Arch. 450:297–302. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Qi G, Kudo Y, Tang B, Liu T, Jin S, Liu J,
Zuo X, Mi S, Shao W, Ma X, et al: PARP6 acts as a tumor suppressor
via downregulating Survivin expression in colorectal cancer.
Oncotarget. 7:18812–18824. 2016.PubMed/NCBI
|
|
7
|
Ikeguchi M, Ueta T, Yamane Y, Hirooka Y
and Kaibara N: Inducible nitric oxide synthase and survivin
messenger RNA expression in hepatocellular carcinoma. Clin Cancer
Res. 8:3131–3136. 2002.PubMed/NCBI
|
|
8
|
Wakana Y, Kasuya K, Katayanagi S, Tsuchida
A, Aoki T, Koyanagi Y, Ishii H and Ebihara Y: Effect of survivin on
cell proliferation and apoptosis in gastric cancer. Oncol Rep.
9:1213–1218. 2002.PubMed/NCBI
|
|
9
|
Sui L, Dong Y, Ohno M, Watanabe Y,
Sugimoto K and Tokuda M: Survivin expression and its correlation
with cell proliferation and prognosis in epithelial ovarian tumors.
Int J Oncol. 21:315–320. 2002.PubMed/NCBI
|
|
10
|
Qi G, Tuncel H, Aoki E, Tanaka S, Oka S,
Kaneko I, Okamoto M, Tatsuka M, Nakai S and Shimamoto F:
Intracellular localization of survivin determines biological
behavior in colorectal cancer. Oncol Rep. 22:557–562.
2009.PubMed/NCBI
|
|
11
|
Tuncel H, Shimamoto F, Qi H Kaneko
Guangying, Aoki E, Jikihara H, Nakai S, Takata T and Tatsuka M:
Nuclear Aurora B and cytoplasmic survivin expression is involved in
lymph node metastasis of colorectal cancer. Oncol Lett.
3:1109–1114. 2012.PubMed/NCBI
|
|
12
|
Tang B, Liang X, Tang F, Zhang J, Zeng S,
Jin S, Zhou L, Kudo Y and Qi G: Expression of USP22 and Survivin is
an indicator of malignant behavior in hepatocellular carcinoma. Int
J Oncol. 47:2208–2216. 2015.PubMed/NCBI
|
|
13
|
Andrianifahanana M, Moniaux N and Batra
SK: Regulation of mucin expression: Mechanistic aspects and
implications for cancer and inflammatory diseases. Biochim Biophys
Acta. 1765:189–222. 2006.PubMed/NCBI
|
|
14
|
Itoh Y, Kamata-Sakurai M, Denda-Nagai K,
Nagai S, Tsuiji M, Ishii-Schrade K, Okada K, Goto A, Fukayama M and
Irimura T: Identification and expression of human
epiglycanin/MUC21: A novel transmembrane mucin. Glycobiology.
18:74–83. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Toribara NW, Gum JJ, Culhane PJ, Lagace
RE, Hicks JW, Petersen GM and Kim YS: MUC-2 human small intestinal
mucin gene structure. Repeated arrays and polymorphism. J Clin
Invest. 88:1005–1013. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Manne U, Weiss HL and Grizzle WE: Racial
differences in the prognostic usefulness of MUC1 and MUC2 in
colorectal adenocarcinomas. Clin Cancer Res. 6:4017–4025.
2000.PubMed/NCBI
|
|
17
|
Gurevich LE, Kazantseva IA, Korsakova NA,
Tsar'Kov PV and Polishchuk LO: Expression of type 1 and type 2
mucins in colonic epithelial tumors. Arkh Patol. 69:12–16. 2007.(In
Russian). PubMed/NCBI
|
|
18
|
Ishizu H, Kumagai J, Eishi Y, Takizawa T
and Koike M: Mucin core protein expression by colorectal mucinous
carcinomas with or without mucus hyperplasia. J Gastroenterol.
39:125–132. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kanoh A, Takeuchi H, Kato K, Waki M, Usami
K and Irimura T: Interleukin-4 induces specific pp-GalNAc-T
expression and alterations in mucin O-glycosylation in colonic
epithelial cells. Biochim Biophys Acta. 1780:577–584. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bartman AE, Sanderson SJ, Ewing SL,
Niehans GA, Wiehr CL, Evans MK and Ho SB: Aberrant expression of
MUC5AC and MUC6 gastric mucin genes in colorectal polyps. Int J
Cancer. 80:210–218. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Imai Y, Yamagishi H, Fukuda K, Ono Y,
Inoue T and Ueda Y: Differential mucin phenotypes and their
significance in a variation of colorectal carcinoma. World J
Gastroenterol. 19:3957–3968. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Perrais M, Pigny P, Copin MC, Aubert JP
and Van Seuningen I: Induction of MUC2 and MUC5AC mucins by factors
of the epidermal growth factor (EGF) family is mediated by EGF
receptor/Ras/Raf/extracellular signal-regulated kinase cascade and
Sp1. J Biol Chem. 30:32258–32267. 2002. View Article : Google Scholar
|
|
23
|
Okamoto K, Okamoto I, Okamoto W, Tanaka K,
Takezawa K, Kuwata K, Yamaguchi H, Nishio K and Nakagawa K: Role of
Survivin in EGFR inhibitor-induced apoptosis in non-small cell lung
cancers positive for EGFR mutations. Cancer Res. 15:10402–10410.
2010. View Article : Google Scholar
|
|
24
|
Kang H, Min BS, Lee KY, Kim NK, Kim SN,
Choi J and Kim H: Loss of E-cadherin and MUC2 expressions
correlated with poor survival in patients with stages II and III
colorectal carcinoma. Ann Surg Oncol. 18:711–719. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lugli A, Zlobec I, Baker K, Minoo P,
Tornillo L, Terracciano L and Jass JR: Prognostic significance of
mucins in colorectal cancer with different DNA mismatch-repair
status. J Clin Pathol. 60:534–539. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Perçinel S, Savaş B, Ensari A, Kuzu I,
Kuzu MA, Bektaş M, Cetinkaya H and Kurşun N: Mucins in the
colorectal neoplastic spectrum with reference to conventional and
serrated adenomas. Turk J Gastroenterol. 18:230–238.
2007.PubMed/NCBI
|
|
27
|
Perez RO, Bresciani BH, Bresciani C,
Proscurshim I, Kiss D, Gama-Rodrigues J, Pereira DD, Rawet V,
Cecconnello I and Habr-Gama A: Mucinous colorectal adenocarcinoma:
Influence of mucin expression (Muc1, 2 and 5) on
clinico-pathological features and prognosis. Int J Colorectal Dis.
23:757–765. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Baas IO, Mulder JW, Offerhaus GJ,
Vogelstein B and Hamilton SR: An evaluation of six antibodies for
immunohistochemistry of mutant p53 gene product in archival
colorectal neoplasms. J Pathol. 172:5–12. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lanza G Jr, Maestri I, Dubini A, Gafa R,
Santini A, Ferretti S and Cavazzini L: p53 expression in colorectal
cancer: Relation to tumor type, DNA ploidy pattern and short-term
survival. Am J Clin Pathol. 105:604–612. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Biemer-Hüttmann AE, Walsh MD, McGuckin MA,
Ajioka Y, Watanabe H, Leggett BA and Jass JR: Immunohistochemical
staining patterns of MUC1, MUC2, MUC4, and MUC5AC mucins in
hyperplastic polyps, serrated adenomas, and traditional adenomas of
the colorectum. J Histochem Cytochem. 47:1039–1048. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Biemer-Huttmann AE, Walsh MD, McGuckin MA,
Simms LA, Young J, Leggett BA and Jass JR: Mucin core protein
expression in colorectal cancers with high levels of microsatellite
instability indicates a novel pathway of morphogenesis. Clin Cancer
Res. 6:1909–1916. 2000.PubMed/NCBI
|
|
32
|
Kocer B, Soran A, Erdogan S, Karabeyoglu
M, Yildirim O, Eroglu A, Bozkurt B and Cengiz O: Expression of
MUC5AC in colorectal carcinoma and relationship with prognosis.
Pathol Int. 52:470–477. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Losi L, Scarselli A, Benatti P, de Leon M
Ponz, Roncucci L, Pedroni M, Borghi F, Lamberti I, Rossi G, Marino
M, et al: Relationship between MUC5AC and altered expression of
MLH1 protein in mucinous and non-mucinous colorectal carcinomas.
Pathol Res Pract. 200:371–377. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Aishima S, Kuroda Y, Nishihara Y, Taguchi
K, Taketomi A, Maehara Y and Tsuneyoshi M: Gastric mucin phenotype
defies tumour progression and prognosis of intrahepatic
cholangiocarcinoma: Gastric foveolar type is associated with
aggressive tumour behaviour. Histopathology. 49:35–44. 2006.
View Article : Google Scholar : PubMed/NCBI
|