Introduction
Radiotherapy (RT) is one of the main therapies for
lung malignancies. As an organ that is sensitive to ionizing
radiation, the lung tends to be easily damaged by radiation beams
(1). Radiation-induced lung injury
(RILI) is a major dose-limiting complication that develops in 7–37%
of patients who undergo definitive RT for lung cancer (1–5). Although
the application of modern radiation techniques has allowed for more
accurate determination of target volume and a reduction of the dose
administered to the normal lung tissues, acute radiation
pneumonitis (RP) and late lung fibrosis have not been eradicated
(6–8).
Advanced non-invasive imaging techniques have provided a visual
understanding of the disease, which has improved the rates of
diagnosis and cure of RILI (9–11). In
addition, various factors predictive of RILI, particularly
dosimetric parameters, can contribute to the optimization of
treatment planning (12). Classical
countermeasures consisting of corticosteroids have demonstrated
only an ameliorating effect on RILI, but not prevention of disease
progression (1). Fortunately, with
advances in research into its pathogenic mechanisms, several
promising pharmacological interventions for RILI have been
developed (13–15). Nevertheless, these novel agents have
only been studied pre-clinically or in early clinical trials thus
far. Therefore, further research is still required.
Pathogenic mechanisms
RILI includes an acute inflammatory phase,
presenting as RP (1–3 months after RT), and a chronic fibrotic
phase, presenting as radiation fibrosis (6–24 months after RT)
(1). The pathological modifications
associated with RILI in these two phases comprise a dynamic
sequential process: Inflammation-induced depletion of alveolar
surface cells, infiltration of inflammatory cells into the
interstitial space, exudative response, and fibrotic changes
(16).
The alveolar epithelium in humans is composed of two
types of cells. Type I pneumocytes, which are squamous epithelial
cells covering >90% of the alveolar surface, are the first to be
damaged by radiation beams. Following irradiation, type I cells
undergo apoptosis, which promotes the proliferation of type II
pneumocytes and leads to repopulation of the alveolar epithelium.
Type II pneumocytes are cuboidal cells that are specialized in
synthesizing and secreting pulmonary surfactants; this substance
covers the alveolar surface and adjusts the surface tension. Thus,
hyperplasia of type II cells resulting from radiation, and the
associated surfactant overproduction, can be a non-specific
indicator of pulmonary damage and reconstruction (17,18).
Recent studies on animal models demonstrated that irradiated
alveolar epithelial cells play an important role in pulmonary
fibrosis (19,20).
Following RT, various cytokines are released.
Activated alveolar macrophages can produce chemotactic and
mitogenic cytokines, which act on immunocytes, fibroblasts and
endothelial cells. These cytokines lead to the local recruitment of
inflammatory leukocytes, including macrophages. Subsequently,
leukocytes adhere to the endothelial cells of microvasculature and
transmigrate to the interstitium; these cells further secret
cytokines to recruit and activate additional immunocytes to trigger
the inflammatory process (17). Tumor
necrosis factor-α (TNF-α) is a type of proinflammatory and
profibrotic cytokine that is synthesized by activated macrophages
(21). During the course of fibrosis,
TNF-α plays an important role in the secretion of proinflammatory
cytokines, such as interleukin (IL)-1 and IL-6, in the
proliferation of fibroblasts, and in the production of
extracellular matrix (ECM) proteins. Under the hypoxic conditions
in lung tissue following radiation, the macrophages will also
persistently produce reactive oxygen species (ROS), which promote
pulmonary injury and fibrosis (17).
Pulmonary fibrosis results from the accumulation of
fibroblasts, myofibroblasts, fibrin and ECM proteins in the
interstitium, followed by the pathological changes of scar
formation (22). However, the
molecular mechanism remains unclear, and numerous studies have been
conducted to investigate related factors (17,22–31).
Myofibroblasts are recognized as crucial factors in pulmonary
fibrosis. Commonly, myofibroblasts are considered to be generated
from resident fibroblasts, but recent evidence has indicated that
damaged epithelial cells may directly provide myofibroblasts by
means of epithelial-mesenchymal transition (EMT) (23). Nagarajan et al (24) revealed that a related pathway mediates
EMT in irradiated alveolar type II epithelial cells. In a study by
Phillips et al (25), it was
demonstrated that circulating fibrocytes are associated with the
pathogenesis of lung fibrosis.
Transforming growth factor-β (TGF-β) is a key
cytokine in the fibrotic process; it is derived mainly from
inflammatory cells, and also from pneumocytes and fibroblasts to
some degree (17). In epithelial
cells, upregulated TGF-β stimulates the expression of Smad
proteins, which induce the activation of other transcription
factors. TGF-β/Smad signaling plays an important role in promoting
pulmonary fibrosis in various ways, including ROS production,
activation of myofibroblasts and fibrocytes, and ECM synthesis
(31). In a study by Yano et
al (26), the Smad pathway was
shown to contribute to radiation-induced lung fibrosis via the
production of type I collagen, and not mitogen-activated protein
kinase (MAPK). TGF-β can act as a powerful stimulator of collagen
synthesis through modulating the transition from a human lung
fibroblast to a myofibroblast phenotype, which facilitates lung
fibrosis (27,28).
In addition to TGF-β, inflammatory cytokines derived
from T helper (Th) cells also contribute to lung fibrosis. Han
et al (29) noted that, in
mice, Th2 immune response-associated factors, including IL-13,
GATA-binding protein 3 and arginase 1, may be crucial in the
fibrotic process. ECM remodeling, which involves collagen-degrading
matrix metalloproteinases (MMPs) and tissue-inhibitors of MMPs,
also augments the fibrotic process (30). Yang et al (30) suggested that MMP-2 and MMP-9, which
degrade collagen IV in the basement membrane, were overexpressed in
mice post-radiation during the inflammatory response, and destroyed
the normal structure of the lung tissue.
Clinical manifestations
In the acute phase of RILI, typical clinical
symptoms including dyspnea, ranging from mild to serious, and dry
cough, which is observed in ~60% of patients with RP. Low-grade
temporal fever is uncommon, and occurs in ~10% of cases. Upon
physical examination in cases of suspected RILI, there may be no
apparent abnormalities. However, rare signs such as pleural
friction rub, moist rales, and consolidation may be heard
occasionally in some cases, in addition to the common presentations
(1). These manifestations may be
complicated by pre-existing lung disease, such as chronic
obstructive pulmonary disease (32).
The incidence of fatal RP is low; in a study by Palma et al
(33), it appeared in only 1.9% of
cases in all patients who accepted concurrent chemoradiation
therapy for non-small cell lung cancer (NSCLC).
Radiation fibrosis, which develops in the later
phase of RILI, is a scarring disease that can markedly reduce the
pulmonary function (32). It may be
developed without the patient having suffered the acute phase.
Different degrees of respiratory difficulty can occur in fibrotic
patients. Chronic pulmonary insufficiency commonly evolves in
patients with a large volume of irradiated lung tissue, and this
facilitates the development of pulmonary hypertension or even cor
pulmonale (pulmonary heart disease) (1). As a restrictive disease, pulmonary
function test outcomes in RP patients, including the first
expiratory volume in 1 sec (measuring gas movement) and the forced
vital capacity (indicating lung capacity), are reduced (16). Carbon monoxide diffusion capacity
(DLCO), an essential test that evaluates the gas diffusion
condition of RILI patients, decreases significantly when the local
radiation dose in normal lung tissue totals ≥13 Gy (34). DLCO loss tends to increase according
to radiation dose (~72% in patients who received 10–20 Gy, and ~90%
in patients who received >20 Gy) (34). However, the severity of lung injury is
usually defined by the presentation of clinical symptoms and the
corresponding treatment strategies, not pulmonary function indexes
(16,34).
Imaging findings
In cases of suspected RILI, non-invasive
radiological imaging, including chest radiography, computed
tomography (CT), single-photon emission CT (SPECT), magnetic
resonance imaging (MRI) and 18F-fluorodeoxyglucose positron
emission tomography (FDG-PET), may be applied to evaluate the
damaged region and potentially predict the corresponding clinical
features (6). Various radiological
abnormalities associated with RILI may be observed in the different
phases of lung pathological injury. An increased density on areas
of CT images is associated with inflammatory reactions during the
acute phase (7). Not all radiological
appearances of RILI are accompanied by clinical symptoms; 50–100%
of lung cancer patients who have undergone RT tend to present with
radiological signs of RILI, whereas only 5–35% develop clinical
symptoms (35–37). Thus, imaging examinations are
important for patients who have undergone thoracic irradiation. The
frequency of imaging examinations is determined on the basis of the
sensitivity of the specific radiographic assessment; it is reported
that CT is more sensitive and reveals RP-associated changes earlier
compared with chest radiography, as it provides 3D visualization of
the lung (6).
CT findings
For conventional thoracic RT, Libshitz and Shuman
(38) classified the lung
injury-associated CT findings into four types: i) Ground-glass
attenuation or homogeneous consolidation; ii) patch-like increased
density in the irradiated area that is not consistent with the
portal shape; iii) scattered consolidation that is consistent with
the portal shape but has a poorly-defined border; and iv) solid
consolidation that involves the entire region of irradiated lung
tissue. The former patterns correspond to the acute phase of
inflammatory exudation, while the latter patterns correspond to the
late phase of lung fibrosis.
With the improvement of radiation methods, certain
advanced techniques, including 3D conformal RT (3DCRT),
intensity-modulated RT (IMRT), and stereotactic body RT (SBRT),
which are able to deliver a maximized tumoricidal dose to tumors
while minimizing the irradiation of normal lung tissues, have been
developed.
3DCRT is a modern and sophisticated technique that
applies multiple radiation beams to form a conformal radiation
field properly fitted to target volumes. This method greatly
reduces the rate of RILI and has an improved curative effect
compared with conventional 2-dimensional radiotherapy. In patients
with NSCLC undergoing 3DCRT, CT images for lung areas with RILI can
develop into altered conventional fibrosis (increased density,
volume loss, and bronchiectasis in a shrunken extent compared with
conventional radiotherapy), scar-like patterns (an opacity change
in tumor tissues) or mass-like patterns (7).
In IMRT, intensity-modulated radiation is delivered
to irregularly shaped tumor volumes by means of the dynamic
multileaf collimators on the basis of 3DCRT. Given that tumor
location, size and disease entity determine the radiation portal
and beam angles, RILI may differ in shape and distribution
depending on tumor features (39).
SBRT is a novel RT technique in which multiple
radiation portals are applied from different directions, allowing
good treatment effects for medically inoperable early-stage NSCLC
patients. Radiation lesions in normal tissue are limited to the
periphery of the tumor and have a complex shape. In patients who
have undergone SBRT, the CT findings associated with RILI conform
more closely to the shape of the tumor, and there is no distinct
boundary dividing the irradiated and non-irradiated lung, in
contrast to conventional RT (8).
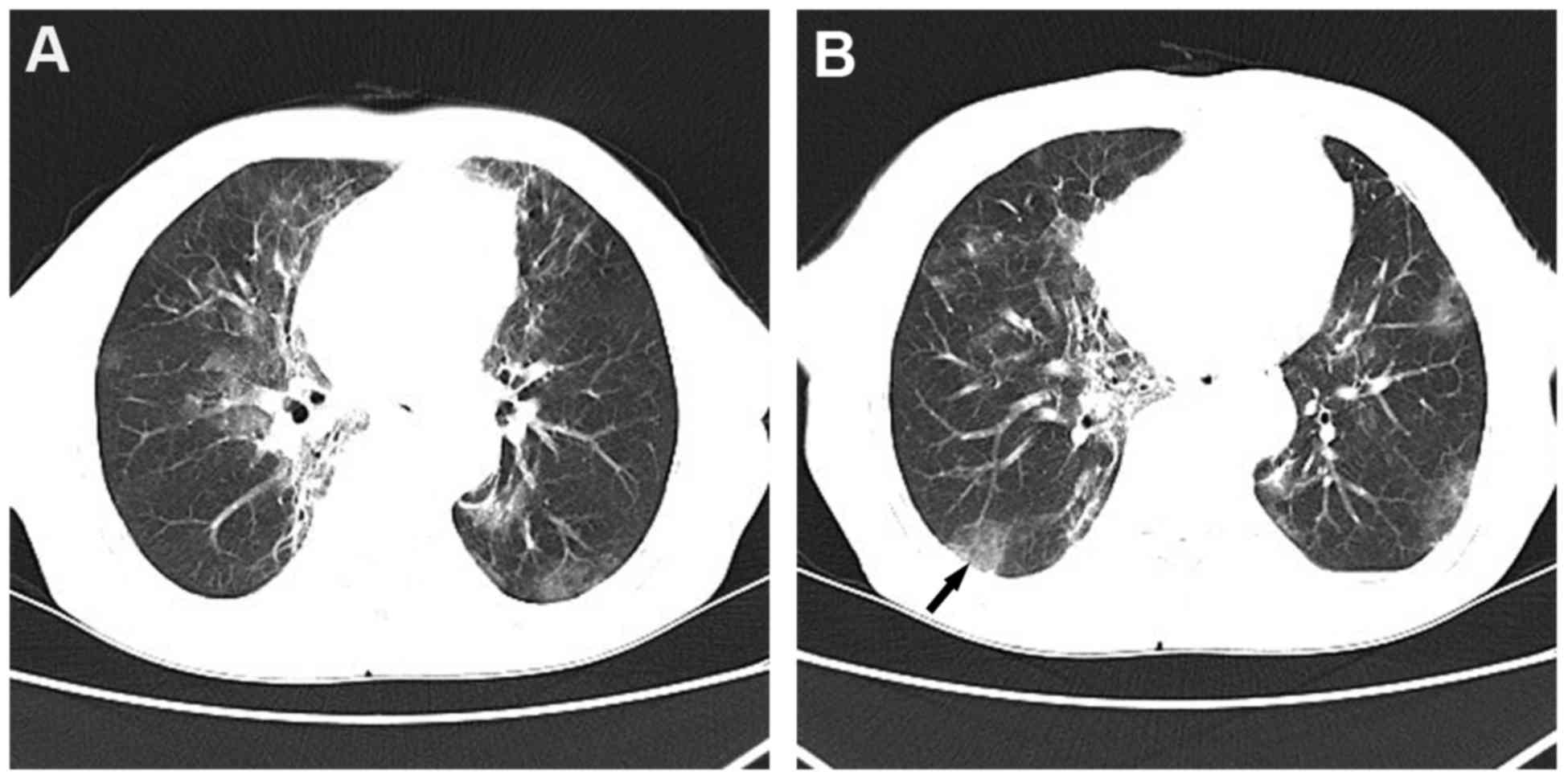
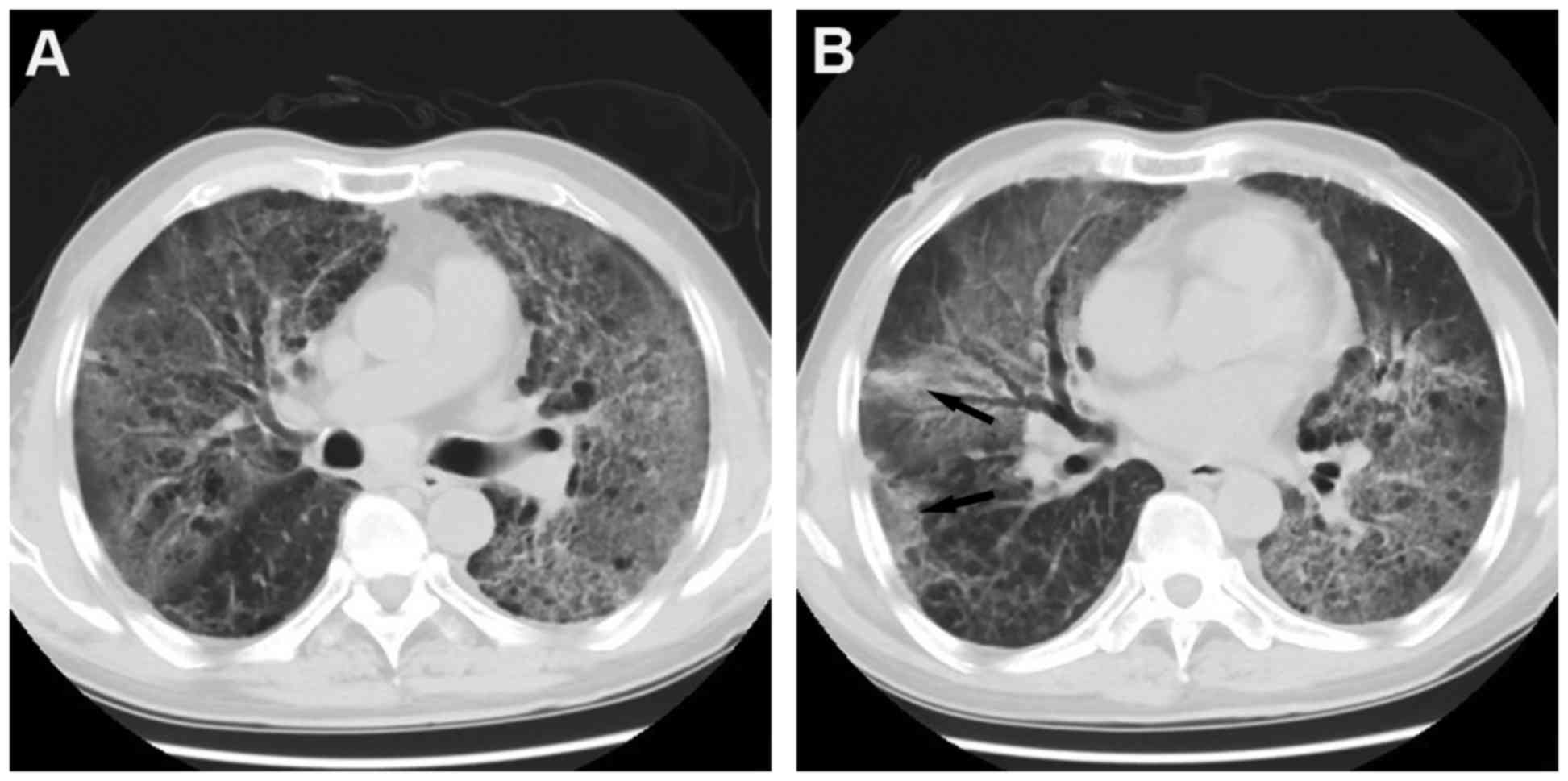
Figs. 1 and 2 show the typical CT imaging findings of
RP.
SPECT findings
CT scans depict density modifications of lung tissue
in RILI patients that are consistent with the 3D dose distribution
map. However, SPECT has been demonstrated to be a more sensitive
examination than CT imaging for assessing lung injury, by
evaluating regional lung perfusion and ventilation functions
(6,40). Physiologically, lungs tend to adjust
blood flow according to ventilation changes rather than adjust
ventilation according to blood flow changes. Therefore, perfusion
is a more sensitive factor than ventilation for predicting RILI
(6). Zhang et al (41) conducted a study of 20 patients with
locally advanced NSCLC who received radical- or non-radical-dose
IMRT, in order to quantitatively evaluate early abnormalities in
lung perfusion using SPECT imaging. SPECT was conducted prior to
and immediately subsequent to IMRT. The study calculated lung
perfusion index (LPI) with regard to blood flow through radioactive
count. The results revealed no statistically significant difference
between the LPIs pre- and post-IMRT (P=0.135). In the radical-dose
group, LPI difference was not statistically significant (P=0.993);
by contrast, the difference was significant in non-radical-dose
group (P=0.025). Thus, SPECT scanning is useful in evaluating early
alterations in perfusion in patients undergoing non-radical-dose
IMRT. Currently, SPECT scanning in assessing perfusion is primarily
judged by visual inspection by physicians; therefore, it is
inevitably biased and it is challenging to identify early subtle
changes in perfusion (9). Thus,
radioactive counts in qualifying SPECT images are required.
MRI findings
In previous studies, MRI findings have been
described for RILI lesions in animal models and human patients
(10,11). In a Japanese study conducted by Shioya
et al (10), MRI was used to
measure the extent of lung injury in rats that had undergone
hemithoracic radiation, indicating that MRI may be a sensitive
technique for detecting early RILI. Ireland et al (11) compared helium-3 MRI
(3He-MRI) acquired from patient with NSCLC pre- and
post-external-beam RT. In their study, all 5 patients with
pathologically confirmed NSCLC received CT and 3He-MRI
ventilation imaging. Post-irradiation, 3 patients developed
pneumonitis that was apparent on CT images. Concurrently, a
significant reduction of 3He-MRI ventilation was
observed in these 3 patients on post-irradiation imaging compared
with pre-irradiation imaging (P=0.02). This indicates that
3He-MRI is a potential method for describing RP by means
of expressing the reduction in ventilation.
PET findings
FDG-PET is a type of metabolic imaging technology
that can present regional functional information, and which has the
potential to evaluate RILI. In a study by Hart et al
(42), pulmonary metabolic radiation
response, a parameter generated from FDG-PET analysis, was found to
be associated with an increased probability of developing RILI
(P=0.033). McCurdy et al (9)
also demonstrated that the FDG-uptake dose-response was associated
with symptomatic RP in patients with lung cancer treated with
thoracic RT. Additionally, combined PET-CT and PET-MRI, which can
present anatomical and metabolic information, are promising
techniques (43). Studies indicated
that ventilation/perfusion index of PET-CT imaging was able to
predict the occurrence rate of RILI and PET-CT could be recommended
to differentiate RILI from cancer recurrence (44,45).
Predictive factors
Parameters from dose-volume histograms
(DVHs)
DVHs generated from 3DCRT planning have been
investigated in numerous studies, and have revealed the dosimetric
parameters that are able to predict RILI caused by external-beam
RT. Vdose, mean lung dose (MLD) and normal tissue
complication probability (NTCP), which are described below, are
three dosimetric parameters with high predictive value for RILI
that have been studied extensively (2). These parameters may assist clinicians
with optimizing radiation treatment planning.
Vdose and MLD
The definition for Vdose (e.g.,
V5, V10, V20, V30 or
V40) is described as the percentage of the whole
CT-measured volume of the irradiated lung that received equal to or
more than the threshold dose (5, 10, 20, 30 or 40 Gy,
respectively). MLD represents the mean dose applied over the whole
lung volume measured by CT imaging. Among the dosimetric factors,
V20 and MLD are the most frequently used parameters for
predicting RILI (33).
Hernando et al (3) conducted a study of 201 patients with
lung cancer, all of whom received RT utilizing 3D planning tools,
and investigated the correlation between DVH-based factors and RP
rates. In total, 39 (19%) of the 201 patients developed RP.
Univariate and multivariate analyses indicated that V30
and MLD were the only factors significantly associated with RP
rates. An increasing rate of RP was observed with increasing
V30 (RP rates: 6 and 24% in patients with V30
of ≤18 and >18%, respectively) and MLD values (RP rates: 10, 16,
27 and 44% in patients who received an MLD of <10, 11–20, 21–30
and >30 Gy, respectively). The authors concluded that dosimetric
factors were the best predictors of RP, superior to clinical
factors (age, gender, tumor location, chemotherapy application,
smoking, pre-RT forced expiratory volume in 1 sec and performance
status) for lung cancer patients treated with 3DCRT (3). Barriger et al (4) reviewed dosimetric data from 243 patients
with stage III NSCLC treated with concurrent cisplatin/etoposide
chemoradiotherapy to examine the rates and predictive factors for
RP. In that study, 17 (7%) of the patients developed grade ≥2 RP
according to the Common Terminology Criteria for Adverse Events
(CTCAE) version 3.0. The median MLD, V5, V20
and V30 values were 18 Gy, 52, 35 and 29%, respectively.
An increasing rate of RP was associated with increasing MLD (MLD
<18 Gy, 2.2% RP rate; MLD >18 Gy, 19% RP rate; P=0.015) and
V20 (V20 <35%, 4.8% RP rate;
V20 >35%, 17% RP rate; P=0.097). Thus, the results
revealed that an MLD >18 Gy was a predictive factor for RP, and
that V20 was possibly associated with RP. Furthermore, a
recent meta-analysis performed on 836 patients who received
concurrent chemoradiotherapy obtained a similar outcome; the
results suggested that 29.8% of patients developed symptomatic RP,
and that V20 was a significant factor in predicting
symptomatic RP (P=0.008) (33).
In previous studies, most of the Vdose
and MLD values used standardly refer to the bilateral lungs, which
means that each dosimetric parameter represents the average value
of the total lung parenchyma, rather than that of the unilateral
lung with the primary tumor (2–5).
Therefore, it is necessary to establish new parameters for use in
treatment planning to aid in concentrating the radiation beams on a
single lung. Ramella et al (5)
analyzed 97 patients with locally advanced NSCLC who received
complete 3DCRT with V20, V30 and MLD limits
of 31%, 18% and 20 Gy, respectively. The authors investigated novel
parameters V20ipsi and V30ipsi (percentages
of ipsilateral lung volume receiving >20 and >30 Gy,
respectively), which were indicated to be significant predictors of
RP. The cutoff points for V20ipsi and V30ipsi
were 52 and 39%, respectively: The risk of RP was 9% if
V20ipsi was ≤52% vs. 46% if V20ipsi was
>52%; and the risk of RP was 8% if V30ipsi was ≤39%
vs. 38% if V30ipsi was >39%. The differences in
V20ipsi and V30ipsi between the RP group and
the non-RP group were statistically significant (P=0.010 and
P=0.001, respectively). Furthermore, in their clinical practice, RP
incidence was reduced from 14.4 to 6.8% when adding the ipsilateral
constraints to standard lung dosimetric parameters. Thus, this may
be an accessible way to improve treatment planning.
Despite the numerous studies confirming the
predictive value of dosimetric factors, certain studies have
presented contrasting findings. Rodrigues et al (2) conducted a review of 12 studies to assess
the association between DVH parameters and RP rates. The study
showed a negative result, and the overall accuracy, sensitivity,
specificity and positive predictive value of DVH parameters were
found to be undesirable. Each DVH parameter in that study failed to
predict RP alone or in a model with additional variables. Another
meta-analysis also suggested that dose-volume metrics should be
explored further to evaluate the RP risk (12).
NTCP
NTCP is another parameter that can be calculated as
a function of the normal tissue DVH by different algorithms.
Various studies have demonstrated that NTCP is a strong predictor
of RILI (46). The Lyman model
(47) is the most widely applied NTCP
model, and is characterized by the binary (yes/no) toxicity
evaluation endpoint (48). Although
it is successful in estimating RP rates, there remains potential to
improve the standard Lyman model. Recent studies have attempted to
incorporate clinical risk factors in the model to better predict
RILI. Tucker et al (48)
introduced a generalized model accounting for censored
time-to-toxicity data and smoking status, and the results
demonstrated a higher predictive value of NTCP model compared with
the model developed on DVH alone. Adding single-nucleotide
polymorphisms to the standard Lyman model also enhanced its
predictive value for RP (43).
Serum markers
The pathogenesis of RP remains unclear; it is known
to be a complex inflammatory process that involves the cellular
interactions between lung parenchymal cells and circulating immune
cells, mediated through a series of cytokines (49). Thus, the plasma levels of distinct
cytokines may be of significance in identifying patients at risk of
developing RILI. However, these cytokines are derived from the
irradiated normal lung tissues as well as the tumor tissues,
including the tumor cells themselves, the immune cells of the tumor
microenvironment and the host stroma of NSCLC specimens,
influencing the circulating plasma cytokine concentrations
(50,51). This indicates that further
investigation is necessary to confirm the ability of cytokines in
predicting RILI. IL-6 and TGF-β are pro-inflammatory and
profibrogenic cytokines, which have been extensively investigated
in numerous studies, including human clinical reports and animal
trials. The fluctuating IL-6 and TGF-β plasma levels measured
before and during RT may be associated with the development of RILI
(49).
Rübe et al (49) analyzed the TGF-β1, TNF-α, IL-1β and
IL-6 circulating plasma levels in 52 patients with NSCLC (stage
I–III) to explore the prognostic values for the development of RP.
The Late Effects in Normal Tissue-Subjective Objective Management
Analysis (LENT-SOMA) system (Table I)
was used in the study, and the cytokine data was obtained before
RT, weekly during RT, every 3 months during follow-up, and at the
beginning of RP. In the study, 40% of patients developed RP, with
10 cases exhibiting RP of grade II or higher (grade II/III/IV,
3/6/1 patients). The study failed to confirm any correlation
between TGF-β1 or IL-6 plasma levels and the probability of RP
occurrence. However, it appeared to be possible to predict RILI
when cytokines were combined with dosimetric factors. In a study by
Stenmark et al (52), five
cytokines (IL-1β, IL-6, IL-8, TNF-α and TGF-β1), in 58 NSCLC
patients treated with definitive RT, were analyzed to ascertain
their value as predictive factors for RILI. All cytokines were
evaluated individually and in combination with physical dosimetric
parameters. The results indicated that a low level of pre-treatment
IL-8 was a significant predictor for RILI, while elevated TGF-β1
resulting from radiation was mildly correlated with the development
of RILI. The other three cytokines demonstrated no predictive
value. However, the combined model, utilizing IL-8, TGF-β1 and MLD,
yielded an advanced capacity for predicting RILI compared with any
variable alone (P<0.001). Therefore, the authors concluded that
a model based on inflammatory cytokines and dosimetric parameters
may estimate RILI accurately (52).
 | Table I.Summary of generally used grading
systems. |
Table I.
Summary of generally used grading
systems.
|
| Grade |
|---|
|
|
|
|---|
| Criteria | 1 | 2 | 3 | 4 | 5 |
|---|
| CTCAE 4.0 |
|
|
|
|
|
|
Pneumonitis | Asymptomatic;
observations only | Symptomatic;
requires medical intervention; limited ADL | Severe symptoms;
oxygen indicated; impair patient self-care ADL | Life-threatening
respiratory dysfunction; urgent intervention indicated | Mortality |
|
Pulmonary fibrosis | Mild hypoxemia;
pulmonary fibrosis <25% | Moderate hypoxemia;
pulmonary hypertension; pulmonary fibrosis 25–50% | Severe hypoxemia;
right-sided heart failure; pulmonary fibrosis 50–75% | Life-threatening
consequences; assisted ventilation indicated; pulmonary fibrosis
>75% | Mortality |
| RTOG:
Pneumonitis | Mild symptoms | Persistent symptoms
requiring symptomatic treatment | Severe symptoms,
possibly requiring intermittent O2 or steroids; evidence
of acute pneumonitis | Severe symptoms
requiring continuous O2 or assisted ventilation | – |
| RTOG/EORTC:
Fibrosis (LENT-SOMA) | Asymptomatic or
mild symptoms; slight imaging changes | Moderate symptoms;
patchy imaging changes | Severe symptoms;
increased density imaging changes | Severe symptoms
requiring continuous O2 or assisted ventilation | Mortality |
| SWOG
Pneumonitis | Imaging changes;
mild symptoms without steroids | Symptoms requiring
steroids or tap for effusion | Symptoms requiring
oxygen | Symptoms requiring
assisted ventilation | Mortality |
| Fibrosis | Asymptomatic;
imaging changes | – | Imaging changes
with symptoms (also code symptoms) | – | – |
A number of studies have indicated that surfactant
protein (SP) levels in the serum may be meaningful in predicting
RILI. Takahashi et al (53)
reported that SP-A and SP-D concentrations in RP patients were
higher than those of non-RP patients (P=0.0065 and P=0.0011,
respectively), which suggested an RP-diagnostic value of these two
variables. In an article analyzing the Radiation Therapy Oncology
Group (RTOG) 91–03 trial, an elevated serum level of SP at 20 Gy
and increased IL-6 serum density after 10 Gy radiation were
considered predictive factors of grade ≥2 acute lung toxicity
(54).
Clinical risk factors for the
development of RILI
Prediction of RILI is not only dependent on
dosimetric factors or plasma cytokine levels, but may also be
influenced by clinical risk factors. Patient characteristics,
including age, gender, comorbidity, tumor location, performance
status and smoking status, combined with treatment-related factors,
such as chemotherapy schedule and surgery, comprise the clinical
factors associated with RP. These factors have been widely
investigated in previous studies: Pre-treatment Karnofsky
performance status was associated with late lung toxicity (54), and chemotherapy (P<0.0001) and
advanced age (61–70 years) were notable predictive factors for RP
(55), whereas pre-RT surgery
demonstrated no effect on the development of RP (56). However, few reports of RILI to date
have systematically elucidated these risk factors.
In order to study the clinical factors
professionally, Vogelius et al (57) conducted a meta-analysis synthesizing
data from 31 independent studies with available odds ratio (OR)
data for RP, and provided a framework for this large amount of
information. The results indicated that advanced age (OR, 1.7;
P<0.0001), disease located in middle or lower lobe (OR, 1.9;
P=0.002) and the presence of comorbidities (OR, 2.3; P=0.007) were
significantly associated with RP. Sequential chemotherapy
scheduling was also associated with a higher risk of developing RP
(OR, 1.6; P=0.01) than concomitant chemotherapy scheduling. Smoking
status, which showed contrasting effects, was analyzed in two
parts: Ongoing smoking could prevent lung cancer patients from
developing RP (OR, 0.6; P=0.008); and a history of smoking
indicated a non-significant protective effect against RP (OR, 0.7;
P=0.06). No association of gender or surgery with RP development
was confirmed in the study. This research demonstrated a method of
synthesizing published clinical risk factor data across various
studies, facilitating its analysis with regard to RP. Depending on
the method, it may be beneficial to combine these factors with
dosimetric factors in a multivariate model in future research to
better understand the development of RP, and generate guidelines
for clinical research.
Grading systems
Several toxicity scoring systems evaluating the
clinical, functional and imaging changes of acute and late RILI
have been used in various studies. CTCAE version 4.0 (58) is currently the most recommended set of
guidelines by the National Cancer Institute. In addition, the RTOG
and European Organization for Research and Treatment of Cancer
(RTOG/EORTC) scoring system (designated as RTOG for brevity)
(59), as well as the Southwest
Oncology Group (SWOG) scoring system (60) are also generally applied (Table I). Other criteria from the Eastern
Cooperative Oncology Group (61) and
the World Health Organization (62)
are also in use (63). In generally
used systems, toxicity grades of 1, 4 and 5 similarly represent
mild symptoms, lethal conditions, and mortality, respectively.
However, the criteria vary for definitions of grades 2 and 3. RTOG
grade 2 is described as a persistent cough requiring narcotic
antitussive agents, while the grade 3 patients present with severe
cough requiring steroid treatment. By contrast, in SWOG grade 2,
steroid treatment is required. However, the CTCAE 4.0 system does
not involve the utility of steroid agents. For late lung toxicity,
RTOG criteria appear to be the easiest to follow among the scoring
systems, as they depicts lung fibrosis together with pneumonitis in
detail (64).
Treatments
In order to reduce the probability or mitigate the
severity of RILI, a variety of strategies have been investigated,
ranging from radiation techniques to pharmacological methods
(1). As standard, modern radiation
treatment planning techniques should be implemented to minimize the
dose to normal lung tissues. Age, sex, tumor location, smoking
status, pulmonary function, performance status and a number of
other patient characteristics should also be considered (1,16). Given
the high rate of infection in these patients, antibiotics are used
prophylactically (16). For
established RILI, multiple agents are used empirically, and
corticosteroids are a mainstay due to their anti-inflammatory
effects; the common dose is 60–100 mg/day for 2 weeks, followed by
an extended taper over 3–12 weeks (1). Although steroids are widely used in
patients with RILI, there appears to be no evidence confirming its
possible influence on long-standing fibrosis. Due to advances in
understanding the molecular pathology of RILI, several promising
prophylactic and therapeutic approaches for this disease have been
proposed.
Cytoprotective agents
Amifostine, an analog of cysteamine, is the first
broad-spectrum cytoprotectant to have been approved in various
countries for clinical use (65). It
is an organic thio-phosphate molecule. Following its
dephosphorylation by vascular endothelial cell alkaline
phosphatase, amifostine transforms into its biologically active
metabolite. The metabolite exerts its biological actions via two
approaches: Scavenging ROS generated following radiation, and
protecting nucleic acids from alkylating or platinum-based drugs
(65–67). Several clinical trials have reported
that amifostine could significantly reduce the incidence of RILI
without compromising the anti-tumor efficacy of radiation in lung
cancer patients (13,66,67).
Komaki et al (13) reported
that no severe RP was observed in patients with lung cancer in the
amifostine treatment group, compared with 16% of patients not
treated with amifostine (P=0.02). Furthermore, amifostine did not
exhibit any apparent effects on survival in these patients. The
authors thus concluded that amifostine had no tumor-protective
effect. Recently, Koukourakis et al (68) demonstrated that a moderate dose of
amifostine administered subcutaneously to irradiated postmastectomy
patients had a significant effect in preventing fibrosis in lung
and soft tissue.
Superoxide dismutases (SODs) are natural enzymes in
mammals that converting superoxide radicals into oxygen and
hydrogen peroxide (H2O2) prior to further
metabolism. In humans, three forms of SOD exist: Mn SOD, Cu/Zn SOD
and extracellular (EC) SOD (17). EC
SOD is the major extracellular antioxidant enzyme and is highly
produced in type II pneumocytes. Therefore, in the lungs, type II
pneumocytes may play a critical role in cytoprotection via EC SOD
(69). Numerous studies have
successfully demonstrated the effects of SOD administration on
radiation-induced fibrosis (RIF). Delanian et al (70) showed for the first time that
liposomal-form SOD (Lip-SOD) reversed RIF in a clinical trial. They
treated 42 distinct zones of RIF, involving the skin and underlying
tissues, with Lip-SOD in 34 patients. Regression was observed in
79% of the fibrotic zones, and treatment was well-tolerated. The
stability of the response at 3 and 5 years was 95 and 70%,
respectively. Lefaix et al (71) suggested that two agents, Mn SOD and
Cu/Zn SOD, exerted curative effects on RIF in animal models.
Epperly et al (72)
demonstrated that overexpression of Mn SOD in the lungs of
transgenic mice pre-radiation could decrease the occurrence of
irradiated lung alveolitis and fibrosis.
The anti-fibrotic properties of SODs may act via
mediating TGF-β1 repression and inducing the reversion of
myofibroblasts into normal fibroblasts (73). In previous studies, SOD-mimetic agents
were shown to alleviate RILI. For example, Gao et al
(74) administered EUK-207, a
SOD/catalase mimetic agent, to rats via subcutaneous injection,
starting at 7 days after total-body irradiation and stopping prior
to the development of pneumonitis. The results indicated that
EUK-207 may act as a mitigator of RP and fibrosis. EUK-207 was also
shown to diminish multiple vascular injuries in irradiated lungs
in vivo for the first time (74). Pan et al (75) suggested that pretreatment with the
recombinant protein SOD-TAT in mice demonstrated an advantage over
amifostine in reducing RIF and improving quality of life.
Suppressors of the renin-angiotensin
(RAS) system
Classically, in the RAS, biological effects are
initiated by the interplay between kidney mesangial cell-generated
renin (substrate) and liver-generated angiotensinogen (enzyme) in
circulation, followed by the production of angiotensin (Ang) I, an
inactive decapeptide. After being cleaved by angiotensin-converting
enzyme (ACE), Ang I transforms into the effective Ang II, which
binds to Ang II receptor type 1 (AT1) or type 2
(AT2) to exert its functions (including vasoconstrictor
activity to regulate blood pressure) (76). Furthermore, mounting evidence
indicates that Ang II is associated with the development of
fibrosis via TGF-β upregulation (77)
and ECM protein synthesis (78). Ang
II also contributes to the injury process as a powerful
proinflammatory substance (79).
Thus, ACE inhibitor (ACEI), which blocks Ang II synthesis, may play
a significant role in alleviating RILI. Ghosh et al
(14) indicated that the ACEI
captopril could increase survival and ameliorate RILI, including
increased breath rate, vascular reactive changes and
histopathological evidence, in irradiated mice. In a randomized
controlled trial, application of captopril in 55 patients
demonstrated a favorable efficacy in reducing pulmonary-related
mortality resulting from total-body irradiation (80). However, captopril is a special type of
ACEI, as the sulfhydryl group in its molecular structure was shown
to be capable of scavenging radicals (81), which suggested another mechanism by
which captopril could attenuate RILI. Wang et al (82) retrospectively analyzed 413 irradiated
NSCLC patients, of whom 65 were given ACEIs during RT (only 1
received captopril), and the results suggested lower symptomatic RP
rates in ACEI-treated patients compared with the non-ACEI-treated
group. This outcome indicated that ACEI agents other than captopril
could also reduce RILI. From another perspective, Molteni et
al (83) showed that Ang II
receptor inhibitors were helpful in palliating RILI. Additionally,
certain researchers suggested renin as a profibrotic mediator
independent from the angiotensin system, in the lung and other
organs, which may provide another approach to mitigating lung
fibrosis (84,85).
Statins
HMG-CoA-reductase inhibitors (statins) are
pleiotropic drugs mainly used as interventions for
hypercholesterolemia. Other than lowering blood lipid levels, they
have functions in reducing radiation-related proinflammatory and
profibrotic responses as well as apoptosis, in vitro and
in vivo (86,87). A pharmacological use of statins
involves inhibition of the radiation-induced activation of the
transcription factor nuclear factor κB, and of the resulting
overproduction of cytokines (including IL-6 and TNF-α) (88). Pre-treatment with lovastatin in
irradiated murine models achieved a reduction of endothelial
selectin and intercellular adhesion molecule 1, which are important
mediators in the inflammatory process (87). On the genetic level, simvastatin
reversed the radiation-induced dysregulation of gene expression
(such as p53, NRF2, and sphingolipid metabolic pathway genes) in
rat lungs (89). In addition, statins
showed an improved repair capacity for radiation-induced DNA
double-strand breaks (88).
Clinically, Wedlake et al (90) indicated that, among 308 patients who
received pelvic RT for cancer, statin (P=0.04) and statin + ACEI
(P=0.008) treatment regimens significantly relived
radiation-induced acute gastrointestinal symptoms and exhibited
long-term protective effects. Given the well-established clinical
use of statins for lipid-lowering purposes, it is desirable to
assess their application as radioprotectants in humans.
Growth factor-related protocols
TGF-β/Smad signaling is important in the
development of radiation-induced damage, and has been investigated
as a treatment target in numerous studies. Pentoxifylline (PTX), a
xanthine derivative, appears to mitigate fibrosis by blocking
Smad3/4-activated transcription (91). In a clinical trial by Ozturk et
al (15), 40 patients with
thoracic malignancies were randomly assigned to receive PTX (400
mg) or a placebo three times per day during the entire RT period.
The results showed a statistically significant protective effect of
PTX against acute and late lung radiotoxicity. In that study, the
initial curative mechanism of PTX was suggested to be platelet
reaggregation and TNF inhibition. Furthermore, Misirlioglu et
al (92) used a combined therapy
of PTX and α-tocopherol (vitamin E) for lung cancer patients during
and for 3 months after RT, which considerably ameliorated RILI.
SB203580 and WP631 are blockers of Smad signal transduction
pathway. They abrogate excessive proliferation, decrease the
expression of p21 and plasminogen activator inhibitor-1 following
radiation, and reduce TGF-β1 in human lung fibroblasts (93). SM16 (94) and LY2109761 (95) are two small-molecule TGF-β inhibitors
which have been confirmed to be valuable in alleviating RILI based
on different biological rationales.
Platelet-derived growth factor (PDGF) receptor
tyrosine kinase inhibitors (RTKIs) are reportedly beneficial in
mitigating RILI. Abdollahi et al (96) applied three different PDGF RTKIs
(SU9518, SU11657 or imatinib) to irradiated mice during the acute
RP phase; markedly reversal of lung fibrosis development was
observed based on the clinical, histological, and CT imaging
results. In a further study by the same authors, which assessed
whether imatinib administration following subsidence of acute
inflammation was effective in attenuating lung fibrosis in mice, a
positive result was obtained (97).
In these two studies, the therapeutic effect of PDGF RTKIs was
considered to be associated with the regulation of TGF-β.
Furthermore, Thomas et al (98) noted that imatinib relieved alveolitis
or fibrosis by means of preventing the mast cell influx into the
lungs following irradiation in mice.
Other treatment schemes
Yazici et al (99) revealed that the use of vitamin D
significantly reduced interstitial inflammation and collagen
deposition in irradiated rat lungs, and that the corresponding
alveolar structure and pneumocytes were protected. MSX-122, a novel
inhibitor of C-X-C chemokine receptor type 4, has demonstrated a
benefit in suppressing radiation-induced fibrotic processes in mice
(100). In addition to these
pharmacological therapies, certain other approaches, including
physiotherapy, hyperbaric oxygen therapy and impedance-controlled
microcurrent therapy may be promising in reducing radiation-related
late lung fibrosis (101).
Conclusions
RILI is a dynamic process characterized by RP and
lung fibrosis. Clinically, dyspnea, non-productive cough and
low-grade fever are the most typical symptoms of acute RP,
accompanied by a decline in pulmonary function. The exact
mechanisms of RILI remain unclear; hyperplasia of normal
pneumocytes, and the overexpression of proinflammatory and
profibrogenic cytokines are suspected causes. TGF-β has been widely
investigated for its multiple functions in the development of RILI,
on the molecular asnd genetic levels, in recent years. CT imaging
is a common method in evaluating RILI, while SPECT, MRI and PET are
more sensitive means that have been studied recently. Several
grading criteria, incorporating clinical manifestations, imaging
findings, and proper treatment measures, are employed in estimating
the severity of RILI. Aiming at the potential underlying
mechanisms, novel approaches for the prevention and treatment of
RILI are under research.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81672974 and
81602719).
References
|
1
|
Graves PR, Siddiqui F, Anscher MS and
Movsas B: Radiation pulmonary toxicity: From mechanisms to
management. Semin Radiat Oncol. 20:201–207. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rodrigues G, Lock M, D'Souza D, Yu E and
Van Dyk J: Prediction of radiation pneumonitis by dose-volume
histogram parameters in lung cancer-a systematic review. Radiother
Oncol. 71:127–138. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hernando ML, Marks LB, Bentel GC, Zhou SM,
Hollis D, Das SK, Fan M, Munley MT, Shafman TD, Anscher MS and Lind
PA: Radiation-induced pulmonary toxicity: A dose-volume histogram
analysis in 201 patients with lung cancer. Int J Radiat Oncol Biol
Phys. 51:650–659. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Barriger RB, Fakiris AJ, Hanna N, Yu M,
Mantravadi P and McGarry RC: Dose-volume analysis of radiation
pneumonitis in non-small-cell lung cancer patients treated with
concurrent cisplatinum and etoposide with or without consolidation
docetaxel. Int J Radiat Oncol Biol Phys. 78:1381–1386. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ramella S, Trodella L, Mineo TC, Pompeo E,
Stimato G, Gaudino D, Valentini V, Cellini F, Ciresa M, Fiore M, et
al: Adding ipsilateral V20 and V30 to conventional dosimetric
constraints predicts radiation pneumonitis in stage IIIA-B NSCLC
treated with combined-modality therapy. Int J Radiat Oncol Biol
Phys. 76:110–115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Robbins ME, Brunso-Bechtold JK, Peiffer
AM, Tsien CI, Bailey JE and Marks LB: Imaging radiation-induced
normal tissue injury. Radiat Res. 177:449–466. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Koenig TR, Munden RF, Erasmus JJ, Sabloff
BS, Gladish GW, Komaki R and Stevens CW: Radiation injury of the
lung after three-dimensional conformal radiation therapy. AJR Am J
Roentgenol. 178:1383–1388. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Linda A, Trovo M and Bradley JD: Radiation
injury of the lung after stereotactic body radiation therapy (SBRT)
for lung cancer: A timeline and pattern of CT changes. Eur J
Radiol. 79:147–154. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McCurdy MR, Castillo R, Martinez J, Al
Hallack MN, Lichter J, Zouain N and Guerrero T: [18F]-FDG uptake
dose-response correlates with radiation pneumonitis in lung cancer
patients. Radiothe Oncol. 104:52–57. 2012. View Article : Google Scholar
|
|
10
|
Shioya S, Tsuji C, Kurita D, Katoh H,
Tsuda M, Haida M, Kawana A and Ohta Y: Early damage to lung tissue
after irradiation detected by the magnetic resonance T2 relaxation
time. Radiat Res. 148:359–364. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ireland RH, Din OS, Swinscoe JA, Woodhouse
N, van Beek EJ, Wild JM and Hatton MQ: Detection of
radiation-induced lung injury in non-small cell lung cancer
patients using hyperpolarized helium-3 magnetic resonance imaging.
Radiother Oncol. 97:244–248. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang XJ, Sun JG, Sun J, Ming H, Wang XX,
Wu L and Chen ZT: Prediction of radiation pneumonitis in lung
cancer patients: A systematic review. J Cancer Res Clin Oncol.
138:2103–2116. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Komaki R, Lee JS, Milas L, Lee HK,
Fossella FV, Herbst RS, Allen PK, Liao Z, Stevens CW, Lu C, et al:
Effects of amifostine on acute toxicity from concurrent
chemotherapy and radiotherapy for inoperable non-small-cell lung
cancer: Report of a randomized comparative trial. Int J Radiat
Oncol Biol Phys. 58:1369–1377. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ghosh SN, Zhang R, Fish BL, Semenenko VA,
Li XA, Moulder JE, Jacobs ER and Medhora M: Renin-Angiotensin
system suppression mitigates experimental radiation pneumonitis.
Int J Radiat Oncol Biol Phys. 75:1528–1536. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ozturk B, Egehan I, Atavci S and Kitapci
M: Pentoxifylline in prevention of radiation-induced lung toxicity
in patients with breast and lung cancer: A double-blind randomized
trial. Int J Radiat Oncol Biol Phys. 58:213–219. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
López Rodríguez M and Cerezo Padellano L:
Toxicity associated to radiotherapy treatment in lung cancer
patients. Clin Transl Oncol. 9:506–512. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tsoutsou PG and Koukourakis MI: Radiation
pneumonitis and fibrosis: Mechanisms underlying its pathogenesis
and implications for future research. Int J Radiat Oncol Biol Phys.
66:1281–1293. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rubin P, Siemann DW, Shapiro DL,
Finkelstein JN and Penney DP: Surfactant release as an early
measure of radiation pneumonitis. Int J Radiat Oncol Biol Phys.
9:1669–1673. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Almeida C, Nagarajan D, Tian J, Leal SW,
Wheeler K, Munley M, Blackstock W and Zhao W: The role of alveolar
epithelium in radiation-induced lung injury. PLoS One.
8:e536282013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Citrin DE, Shankavaram U, Horton JA,
Shield W III, Zhao S, Asano H, White A, Sowers A, Thetford A and
Chung EJ: Role of type II pneumocyte senescence in
radiation-induced lung fibrosis. J Natl Cancer Inst. 105:1474–1484.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Piguet PF: Is ‘tumor necrosis factor’ the
major effector of pulmonary fibrosis? Eur Cytokine Netw. 1:257–258.
1990.PubMed/NCBI
|
|
22
|
Sime PJ: The antifibrogenic potential of
PPARgamma ligands in pulmonary fibrosis. J Investig Med.
56:534–538. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Grgic I, Duffield JS and Humphreys BD: The
origin of interstitial myofibroblasts in chronic kidney disease.
Pediatr Nephrol. 27:183–193. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nagarajan D, Melo T, Deng Z, Almeida C and
Zhao W: ERK/GSK3β/Snail signaling mediates radiation-induced
alveolar epithelial-to-mesenchymal transition. Free Radic Biol Med.
52:983–992. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Phillips RJ, Burdick MD, Hong K, Lutz MA,
Murray LA, Xue YY, Belperio JA, Keane MP and Strieter RM:
Circulating fibrocytes traffic to the lungs in response to CXCL12
and mediate fibrosis. J Clin Invest. 114:438–446. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yano H, Hamanaka R, Nakamura M, Sumiyoshi
H, Matsuo N and Yoshioka H: Smad, but not MAPK, pathway mediates
the expression of type I collagen in radiation induced fibrosis.
Biochem Biophys Res Commun. 418:457–463. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fine A and Goldstein RH: The effect of
transforming growth factor-beta on cell proliferation and collagen
formation by lung fibroblasts. J Biol Chem. 262:3897–3902.
1987.PubMed/NCBI
|
|
28
|
Hashimoto S, Gon Y, Takeshita I, Matsumoto
K, Maruoka S and Horie T: Transforming growth Factor-beta1 induces
phenotypic modulation of human lung fibroblasts to myofibroblast
through a c-Jun-NH2-terminal kinase-dependent pathway. Am J Respir
Crit Care Med. 163:152–157. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Han G, Zhang H, Xie CH and Zhou YF:
Th2-like immune response in radiation-induced lung fibrosis. Oncol
Rep. 26:383–388. 2011.PubMed/NCBI
|
|
30
|
Yang K, Palm J, König J, Seeland U,
Rosenkranz S, Feiden W, Rübe C and Rübe CE:
Matrix-metallo-proteinases and their tissue inhibitors in
radiation-induced lung injury. Int J Radiat Biol. 83:665–676. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ding NH, Li JJ and Sun LQ: Molecular
mechanisms and treatment of radiation-induced lung fibrosis. Curr
Drug Targets. 14:1347–1356. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Medhora M, Gao F, Jacobs ER and Moulder
JE: Radiation damage to the lung: Mitigation by
angiotensin-converting enzyme (ACE) inhibitors. Respirology.
17:66–71. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Palma DA, Senan S, Tsujino K, Barriger RB,
Rengan R, Moreno M, Bradley JD, Kim TH, Ramella S, Marks LB, et al:
Predicting radiation pneumonitis after chemoradiation therapy for
lung cancer: An international individual patient data
meta-analysis. Int J Radiat Oncol Biol Phys. 85:444–450. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Mehta V: Radiation pneumonitis and
pulmonary fibrosis in non-small-cell lung cancer: Pulmonary
function, prediction, and prevention. Int J Radiat Oncol Biol Phys.
63:5–24. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Marks LB, Fan M, Clough R, Munley M,
Bentel G, Coleman RE, Jaszczak R, Hollis D and Anscher M:
Radiation-induced pulmonary injury: Symptomatic versus subclinical
endpoints. Int J Radiat Biol. 76:469–475. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Goethals I, Dierckx R, De Meerleer G, De
Sutter J, De Winter O, De Neve W and Van de Wiele C: The role of
nuclear medicine in the prediction and detection of
radiation-associated normal pulmonary and cardiac damage. J Nucl
Med. 44:1531–1539. 2003.PubMed/NCBI
|
|
37
|
Graham MV, Purdy JA, Emami B, Harms W,
Bosch W, Lockett MA and Perez CA: Clinical dose-volume histogram
analysis for pneumonitis after 3D treatment for non-small cell lung
cancer (NSCLC). Int J Radiat Oncol Biol Phys. 45:323–329. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Libshitz HI and Shuman LS:
Radiation-induced pulmonary change: CT findings. J Comput Assist
Tomogr. 8:15–19. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Choi YW, Munden RF, Erasmus JJ, Park KJ,
Chung WK, Jeon SC and Park CK: Effects of radiation therapy on the
lung: Radiologic appearances and differential diagnosis.
Radiographics. 24:985–998. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Ghafoori P, Marks LB, Vujaskovic Z and
Kelsey CR: Radiation-induced lung injury: Assessment, management,
and prevention. Oncology (Williston Park). 22:37–47, 52-53.
2008.PubMed/NCBI
|
|
41
|
Zhang W, Wang J, Tang M, Pan J, Bai P, Lin
D, Qian F, Lin F, Yang X and Zhang S: Quantitative study of lung
perfusion SPECT scanning and pulmonary function testing for early
radiation-induced lung injury in patients with locally advanced
non-small cell lung cancer. Exp Ther Med. 3:631–635.
2012.PubMed/NCBI
|
|
42
|
Hart JP, McCurdy MR, Ezhil M, Wei W, Khan
M, Luo D, Munden RF, Johnson VE and Guerrero TM: Radiation
pneumonitis: Correlation of toxicity with pulmonary metabolic
radiation response. Int J Radiat Oncol Biol Phys. 71:967–971. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Tucker SL, Li M, Xu T, Gomez D, Yuan X, Yu
J, Liu Z, Yin M, Guan X, Wang LE, et al: Incorporating
single-nucleotide polymorphisms into the Lyman model to improve
prediction of radiation pneumonitis. Int J Radiat Oncol Biol Phys.
85:251–257. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Siva S, Hardcastle N, Kron T, Bressel M,
Callahan J, MacManus MP, Shaw M, Plumridge N, Hicks RJ, Steinfort
D, et al: Ventilation/perfusion positron emission tomography-based
assessment of radiation injury to lung. Int J Radiat Oncol Biol
Phys. 93:408–417. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Waissi W, Noël G and Giraud P: Follow-up
after lung stereotactic radiotherapy. Cancer Radiother. 19:566–572.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kim TH, Cho KH, Pyo HR, Lee JS, Zo JI, Lee
DH, Lee JM, Kim HY, Hwangbo B, Park SY, et al: Dose-volumetric
parameters for predicting severe radiation pneumonitis after
three-dimensional conformal radiation therapy for lung cancer.
Radiology. 235:208–215. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Lyman JT: Complication probability as
assessed from dose-volume histograms. Radiat Res Suppl. 8:S13–S19.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tucker SL, Liu HH, Liao Z, Wei X, Wang S,
Jin H, Komaki R, Martel MK and Mohan R: Analysis of radiation
pneumonitis risk using a generalized Lyman model. Int J Radiat
Oncol Biol Phys. 72:568–574. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Rübe CE, Palm J, Erren M, Fleckenstein J,
König J, Remberger K and Rübe C: Cytokine plasma levels: Reliable
predictors for radiation pneumonitis? PLoS One. 3:e28982008.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Tisdale MJ: Cachexia in cancer patients.
Nat Rev Cancer. 2:862–871. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kong F, Jirtle RL, Huang DH, Clough RW and
Anscher MS: Plasma transforming growth factor-beta1 level before
radiotherapy correlates with long term outcome of patients with
lung carcinoma. Cancer. 86:1712–1719. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Stenmark MH, Cai XW, Shedden K, Hayman JA,
Yuan S, Ritter T, Ten Haken RK, Lawrence TS and Kong FM: Combining
physical and biologic parameters to predict radiation-induced lung
toxicity in patients with non-small-cell lung cancer treated with
definitive radiation therapy. Int J Radiat Oncol Biol Phys.
84:e217–e222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Takahashi H, Imai Y, Fujishima T,
Shiratori M, Murakami S, Chiba H, Kon H, Kuroki Y and Abe S:
Diagnostic significance of surfactant proteins A and D in sera from
patients with radiation pneumonitis. Eur Respir J. 17:481–487.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Hartsell WF, Scott CB, Dundas GS,
Mohiuddin M, Meredith RF, Rubin P and Weigensberg IJ: Can serum
markers be used to predict acute and late toxicity in patients with
lung cancer? Analysis of RTOG 91–03. Am J Clin Oncol. 30:368–376.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Parashar B, Edwards A, Mehta R, Pasmantier
M, Wernicke AG, Sabbas A, Kerestez RS, Nori D and Chao KS:
Chemotherapy significantly increases the risk of radiation
pneumonitis in radiation therapy of advanced lung cancer. Am J Clin
Oncol. 34:160–164. 2011.PubMed/NCBI
|
|
56
|
Kocak Z, Yu X, Zhou SM, D'Amico TA, Hollis
D, Kahn D, Tisch A, Shafman TD and Marks LB: The impact of
pre-radiotherapy surgery on radiation-induced lung injury. Clin
Oncol (R Coll Radiol). 17:210–216. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Vogelius IR and Bentzen SM: A
literature-based meta-analysis of clinical risk factors for
development of radiation induced pneumonitis. Acta Oncol.
51:975–983. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
US Department of Health and Human
Services, . Common Terminology Criteria for Adverse Events (CTCAE).
Version 4.0. National Institutes of Health; 2009
|
|
59
|
Cox JD, Stetz J and Pajak TF: Toxicity
criteria of the radiation therapy oncology group (RTOG) and the
european organization for research and treatment of cancer (EORTC).
Int J Radiat Oncol Biol Phys. 31:1341–1346. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Green S and Weiss GR: Southwest oncology
group standard response criteria, endpoint definitions and toxicity
criteria. Invest New Drugs. 10:239–253. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Eastern Cooperative Oncology Group, . ECOG
Common Toxicity Criteria. http://ecog.dfci.harvard.edu/general/common_tox.html
|
|
62
|
S G: World Health Organization Handbook
for reporting results of cancer treatment. WHO Offset Publication;
1979
|
|
63
|
Tucker SL, Jin H, Wei X, Wang S, Martel
MK, Komaki R, Liu HH, Mohan R, Chen Y, Cox JD and Liao Z: Impact of
toxicity grade and scoring system on the relationship between mean
lung dose and risk of radiation pneumonitis in a large cohort of
patients with non-small cell lung cancer. Int J Radiat Oncol Biol
Phys. 77:691–698. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kong FM, Ten Haken R, Eisbruch A and
Lawrence TS: Non-small cell lung cancer therapy-related pulmonary
toxicity: An update on radiation pneumonitis and fibrosis. Semin
Oncol. 32 2 Suppl 3:S42–S54. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Capizzi RL and Oster W: Chemoprotective
and radioprotective effects of amifostine: An update of clinical
trials. Int J Hematol. 72:425–435. 2000.PubMed/NCBI
|
|
66
|
Antonadou D, Coliarakis N, Synodinou M,
Athanassiou H, Kouveli A, Verigos C, Georgakopoulos G, Panoussaki
K, Karageorgis P and Throuvalas N; Clinical Radiation Oncololgy
Hellenic Group, : Randomized phase III trial of radiation treatment
+/− amifostine in patients with advanced-stage lung cancer. Int J
Radiat Oncol Biol Phys. 51:915–922. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Antonadou D, Throuvalas N, Petridis A,
Bolanos N, Sagriotis A and Synodinou M: Effect of amifostine on
toxicities associated with radiochemotherapy in patients with
locally advanced non-small-cell lung cancer. Int J Radiat Oncol
Biol Phys. 57:402–408. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Koukourakis MI, Panteliadou M, Abatzoglou
IM, Sismanidou K, Sivridis E and Giatromanolaki A: Postmastectomy
hypofractionated and accelerated radiation therapy with (and
without) subcutaneous amifostine cytoprotection. Int J Radiat Oncol
Biol Phys. 85:e7–e13. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Folz RJ, Guan J, Seldin MF, Oury TD,
Enghild JJ and Crapo JD: Mouse extracellular superoxide dismutase:
Primary structure, tissue-specific gene expression, chromosomal
localization, and lung in situ hybridization. Am J Respir Cell Mol
Biol. 17:393–403. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Delanian S, Baillet F, Huart J, Lefaix JL,
Maulard C and Housset M: Successful treatment of radiation-induced
fibrosis using liposomal Cu/Zn superoxide dismutase: Clinical
trial. Radiother Oncol. 32:12–20. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Lefaix JL, Delanian S, Leplat JJ, Tricaud
Y, Martin M, Nimrod A, Baillet F and Daburon F: Successful
treatment of radiation-induced fibrosis using Cu/Zn-SOD and Mn-SOD:
An experimental study. Int J Radiat Oncol Biol Phys. 35:305–312.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Epperly MW, Bray JA, Krager S, Berry LM,
Gooding W, Engelhardt JF, Zwacka R, Travis EL and Greenberger JS:
Intratracheal injection of adenovirus containing the human MnSOD
transgene protects athymic nude mice from irradiation-induced
organizing alveolitis. Int J Radiat Oncol Biol Phys. 43:169–181.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Vozenin-Brotons MC, Sivan V, Gault N,
Renard C, Geffrotin C, Delanian S, Lefaix JL and Martin M:
Antifibrotic action of Cu/Zn SOD is mediated by TGF-beta1
repression and phenotypic reversion of myofibroblasts. Free Radic
Biol Med. 30:30–42. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Gao F, Fish BL, Szabo A, Doctrow SR, Kma
L, Molthen RC, Moulder JE, Jacobs ER and Medhora M: Short-Term
Treatment with a SOD/catalase mimetic, EUK-207, mitigates
pneumonitis and fibrosis after single-dose total-body or
whole-thoracic irradiation. Radiat Res. 178:468–480. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Pan J, Su Y, Hou X, He H, Liu S, Wu J and
Rao P: Protective effect of recombinant protein SOD-TAT on
radiation-induced lung injury in mice. Life Sci. 91:89–93. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Lavoie JL and Sigmund CD: Minireview:
Overview of the renin-angiotensin system-an endocrine and paracrine
system. Endocrinology. 144:2179–2183. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Border WA and Noble NA: Interactions of
transforming growth factor- and angiotensin II in renal fibrosis.
Hypertension. 31:181–188. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Gómez-Garre D, Ruiz-Ortega M, Ortego M,
Largo R, López-Armada MJ, Plaza JJ, González E and Egido J: Effects
and interactions of endothelin-1 and angiotensin II on matrix
protein expression and synthesis and mesangial cell growth.
Hypertension. 27:885–892. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Suzuki Y, Ruiz-Ortega M, Lorenzo O,
Ruperez M, Esteban V and Egido J: Inflammation and angiotensin II.
Int J Biochem Cell Biol. 35:881–900. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Cohen EP, Bedi M, Irving AA, Jacobs E,
Tomic R, Klein J, Lawton CA and Moulder JE: Mitigation of late
renal and pulmonary injury after hematopoietic stem cell
transplantation. Int J Radiat Oncol Biol Phys. 83:292–296. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Chopra M, Scott N, McMurray J, McLay J,
Bridges A, Smith WE and Belch JJ: Captopril: A free radical
scavenger. Br J Clin Pharmacol. 27:396–399. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Wang H, Liao Z, Zhuang Y, Xu T, Nguyen QN,
Levy LB, O'Reilly M, Gold KA and Gomez DR: Do
angiotensin-converting enzyme inhibitors reduce the risk of
symptomatic radiation pneumonitis in patients with non-small cell
lung cancer after definitive radiation therapy? Analysis of a
single-institution database. Int J Radiat Oncol Biol Phys.
87:1071–1077. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Molteni A, Wolfe LF, Ward WF, Ts'ao CH,
Molteni LB, Veno P, Fish BL, Taylor JM, Quintanilla N, Herndon B
and Moulder JE: Effect of an angiotensin II receptor blocker and
two angiotensin converting enzyme inhibitors on transforming growth
factor-beta (TGF-beta) and alpha-actomyosin (alpha SMA), important
mediators of radiation-induced pneumopathy and lung fibrosis. Curr
Pharm Des. 13:1307–1316. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Huang Y, Wongamorntham S, Kasting J,
McQuillan D, Owens RT, Yu L, Noble NA and Border W: Renin increases
mesangial cell transforming growth factor-beta1 and matrix proteins
through receptor-mediated, angiotensin II-independent mechanisms.
Kidney Int. 69:105–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Montes E, Ruiz V, Checa M, Maldonado V,
Melendez-Zajgla J, Montaño M, Ordoñez-Razo R, Cisneros J,
García-de-Alba C, Pardo A and Selman M: Renin is an
angiotensin-independent profibrotic mediator: Role in pulmonary
fibrosis. Eur Respir J. 39:141–148. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Ran XZ, Ran X, Zong ZW, Liu DQ, Xiang GM,
Su YP and Zheng HE: Protective effect of atorvastatin on
radiation-induced vascular endothelial cell injury in vitro. J
Radiat Res. 51:527–533. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Ostrau C, Hülsenbeck J, Herzog M, Schad A,
Torzewski M, Lackner KJ and Fritz G: Lovastatin attenuates ionizing
radiation-induced normal tissue damage in vivo. Radiother Oncol.
92:492–499. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Fritz G, Henninger C and Huelsenbeck J:
Potential use of HMG-CoA reductase inhibitors (statins) as
radioprotective agents. Br Med Bull. 97:17–26. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Mathew B, Huang Y, Jacobson JR, Berdyshev
E, Gerhold LM, Wang T, Moreno-Vinasco L, Lang G, Zhao Y, Chen CT,
et al: Simvastatin attenuates radiation-induced murine lung injury
and dysregulated lung gene expression. Am J Respir Cell Mol Biol.
44:415–422. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Wedlake LJ, Silia F, Benton B, Lalji A,
Thomas K, Dearnaley DP, Blake P, Tait D, Khoo VS and Andreyev HJ:
Evaluating the efficacy of statins and ACE-inhibitors in reducing
gastrointestinal toxicity in patients receiving radiotherapy for
pelvic malignancies. Eur J Cancer. 48:2117–2124. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Lin SL, Chen RH, Chen YM, Chiang WC, Lai
CF, Wu KD and Tsai TJ: Pentoxifylline attenuates tubulointerstitial
fibrosis by blocking Smad3/4-activated transcription and
profibrogenic effects of connective tissue growth factor. J Am Soc
Nephrol. 16:2702–2713. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Misirlioglu CH, Demirkasimoglu T,
Kucukplakci B, Sanri E and Altundag K: Pentoxifylline and
alpha-tocopherol in prevention of radiation-induced lung toxicity
in patients with lung cancer. Med Oncol. 24:308–311. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Li Y, Song SL, Peng RY, Wang DW, Jin MH,
Gao YB and Ma JJ: Effects of SB203580 and WP631 on Smad signal
transduction pathway in lung fibroblasts after irradiation. Ai
Zheng. 27:698–702. 2008.(In Chinese). PubMed/NCBI
|
|
94
|
Anscher MS, Thrasher B, Zgonjanin L,
Rabbani ZN, Corbley MJ, Fu K, Sun L, Lee WC, Ling LE and Vujaskovic
Z: Small molecular inhibitor of transforming growth factor-beta
protects against development of radiation-induced lung injury. Int
J Radiat Oncol Biol Phys. 71:829–837. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Flechsig P, Dadrich M, Bickelhaupt S,
Jenne J, Hauser K, Timke C, Peschke P, Hahn EW, Gröne HJ, Yingling
J, et al: LY2109761 attenuates radiation-induced pulmonary murine
fibrosis via reversal of TGF-β and BMP-associated proinflammatory
and proangiogenic signals. Clin Cancer Res. 18:3616–3627. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Abdollahi A, Li M, Ping G, Plathow C,
Domhan S, Kiessling F, Lee LB, McMahon G, Gröne HJ, Lipson KE and
Huber PE: Inhibition of platelet-derived growth factor signaling
attenuates pulmonary fibrosis. J Exp Med. 201:925–935. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Li M, Abdollahi A, Gröne HJ, Lipson KE,
Belka C and Huber PE: Late treatment with imatinib mesylate
ameliorates radiation-induced lung fibrosis in a mouse model.
Radiat Oncol. 4:662009. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Thomas DM, Fox J and Haston CK: Imatinib
therapy reduces radiation-induced pulmonary mast cell influx and
delays lung disease in the mouse. Int J Radiat Biol. 86:436–444.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Yazici G, Yildiz F, Iskit A, Erdemli E,
Surucu S, Firat P, Hayran M, Ozyigit G and Cengiz M: The effect of
vitamin D prophylaxis on radiation induced pulmonary damage. J
Radiat Res. 52:616–621. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Shu HK, Yoon Y, Hong S, Xu K, Gao H, Hao
C, Torres-Gonzalez E, Nayra C, Rojas M and Shim H: Inhibition of
the CXCL12/CXCR4-axis as preventive therapy for radiation-induced
pulmonary fibrosis. PLoS One. 8:e797682013. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
O'Sullivan B and Levin W: Late
radiation-related fibrosis: Pathogenesis, manifestations, and
current management. Semin Radiat Oncol. 13:274–289. 2003.
View Article : Google Scholar : PubMed/NCBI
|