Introduction
Hepatocellular carcinoma (HCC) ranks fifth for newly
diagnosed malignant tumors and is the third leading cause of
cancer-associated mortality worldwide in 2001 (1). In China, it is the second most common
type of malignant tumor, associated with 564,000 newly diagnosed
cases and 549,000 reported mortalities annually (2). The overall 5-year survival rate of HCC
is <5% (2). The portal vein is
prone to HCC invasion, leading to intrahepatic dissemination,
resulting in intrahepatic metastasis and a high disease recurrence
rate (3). The 5-year metastasis and
recurrence rate is reported to be 61.5% for early-diagnosed cases
subsequent to radical resection and 43.5% for subclinical HCCs,
significantly affecting the treatment outcome (3). Systemic or local chemotherapy following
surgery may improve the survival rate to an extent; however, the
clinical use of chemotherapeutic drugs is restricted by their low
specificity, leading to severe adverse effects, including toxicity
in the heart, lungs and kidneys.
Recent studies have indicated that the activation of
the Raf/mitogen-activated protein kinase kinase 1
(MEK)/mitogen-activated protein kinase 1 (ERK) pathway serves a
pivotal role in regulating HCC proliferation (4). Sorafenib is an inhibitor of
serine/threonine and tyrosine kinases. Sorafenib's antitumor
activity results from the downregulation of Ras oncogene activity,
which activates the Raf/MEK/ERK pathway to promote the
proliferation of tumor cells. Sorafenib, a novel multi-targeted
drug, has two antineoplastic mechanisms: i) The direct inhibition
of the Ras/Raf/MEK/ERK signaling pathway; ii) the indirect blockade
of tumor angiogenesis via the downstream inhibition of vascular
endothelial growth factor receptor (VEGFR)-2/platelet-derived
growth factor receptor (PDGFR)-β (5).
However, sorafenib produces certain adverse effects, including
diarrhea (8%), hypertension (2%), abdominal pain (2%) and hand-foot
skin reactions (HFSR) (6). For
example, Luo et al (7)
reported that the incidence of HFSR was 74.5% for sorafenib, with
the incidences of grade 1, 2 and 3 severity being 52.9, 21.6 and
21.6%, respectively. Chu et al (8) reported that the incidences of grade 1–3
and grade 3 HFRS were 38.8, and 8.9%, respectively. It is possible
that the inhibitory effects produced by sorafenib on the PDGFR and
Raf signaling pathways may disrupt the proliferation and repair of
normal cells and the blood supply to relevant tissues (9–11). The
inability of HCC patients to tolerate adverse effects often leads
to a reduction in the dose of sorafenib or the cessation of its
use, thereby diminishing its efficacy. Additionally, as sorafenib
is insoluble in water, only oral formulations are available at
present. As a result, it is important to improve the specificity of
binding between sorafenib and HCC cells in order to increase its
local accumulation in tumors, prolong its functional activity and
minimize its side effects on non-tumor hepatic cells and other
tissues.
To achieve these aims, the development of
sorafenib-incorporating nanoparticles using nanotechnology is
reported in the present study.
Materials and methods
Materials
Sorafenib was purchased from Bayer AG (Leverkusen,
Germany). Polyethylene glycol (PEG), polylactic acid,
dichloromethane, stannous octoate, rac-lactide, tetrahydrofuran and
methanol were provided by Xinhua Chemical Engineering Co., Ltd.
(Jiande, China). Cell Counting kit-8 (CCK-8) was obtained from
Sigma-Aldrich (Merck KGaA, Darmstadt, Germany).
A total of 33 ICR mice (male; 4 weeks old, 18–22 g)
and 36 Sprague-Dawley (SD) rats (male; 10 weeks old, 300–400 g)
were obtained from Shanghai Bikai Experimental Animal Center
[Shanghai, China; license no. SCXK (Hu) 2008-0016]. All animals
were quarantined for 1 week prior to the start of the experiment.
They were housed in an animal facility maintained with a 12 h
light/dark cycle, at a constant temperature of 23±1°C and humidity
of 44±5%, and had free access to water and food. The experimental
protocols were reviewed and approved by the Committee of Ethics on
Animal Experiments of the Shanghai Bikai Experimental Animal
Center, and all animal work procedures were approved by the
Institutional Animal Care and Use Committee of Shanghai University
of Traditional Chinese Medicine (Shanghai, China).
The H22 mouse HCC cell line was provided by the
Shanghai Institutes for Cell Biology, Chinese Academy of Sciences
(Shanghai, China). RPMI-1640 culture medium and 10% fetal bovine
serum was purchased from Sigma-Aldrich (Merck KGaA). The H22 mouse
HCC cell line was cultured in 5% CO2 at 37°C.
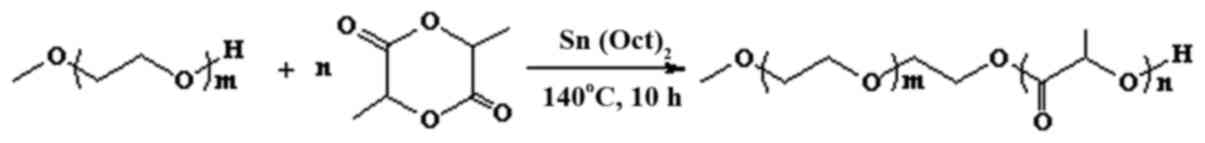
Synthesis of PEG monomethyl
ether-racemic polylactic acid (mPEG-PDLLA) block copolymer
Ring-opening polymerization was used to synthesize
mPEG-co-PDLLA block copolymers. Melted mPEG was placed in a Schlenk
tube (Shanghai Heqi Glassware Co., Ltd., Shanghai, China) and
vacuum-dehydrated. Refined DLLA and a stannous octoate catalyst
(Sigma-Aldrich; Merck KGaA) were added into the tube and vacuumized
three times. Nitrogen (Shanghai Jiaya Chemical Co., Ltd., Shanghai,
China) was introduced and the tube was vacuumized, sealed and
incubated in a 140°C oil bath for 10 h. At the end of the reaction,
the product was extracted using dichloromethane and cold ether
precipitation. mPEG-PDLLA block copolymers were obtained subsequent
to vacuum drying.
Preparation of sorafenib-incorporated
nanoparticles
Nanoprecipitation was used to prepare sorafenib
nanoparticles. Firstly, 250 mg of mPEG-PDLLA of block copolymer and
12.5 mg sorafenib were dissolved in a mixture of 12 ml
tetrahydrofuran and 6 ml methanol. The solution was agitated with
an automatic agitator until it became transparent. The solvent was
removed by vacuum rotary evaporation at 60°C and 50 ml distilled
water at 60°C was added. The water was rotary-evaporated at
atmospheric pressure for 10 min and the supernatant was collected
by centrifugation (2,504 × g at 4°C for 10 min) to obtain a
solution of sorafenib nanoparticles. Finally, the particle size and
ζ potential were measured using the Nano-ZS ZEN3600 apparatus
(Malvern Instruments China, Shanghai, China); the drug-loading
amount and drug-embedding ratio were measured with an ultraviolet
spectrophotometer. Sorafenib acetonitrile solution (0.01 mg/ml) was
prepared as the control solution. A total of 0.1 ml of sorafenib
nanoparticle concentrate was added to 5 ml acetonitrile, and the
concentrate was ultrasonicated for 5 min to fully extract the
sorafenib. Then, acetonitrile was added to make up the volume to 10
ml. Subsequent to being shaken and centrifuged at 8,452 × g at 4°C
for 20 min, the supernatant was collected to measure the UV
absorption at 263 nm wavelength, and the absorbance A2 was
recorded. The UV absorption of the control solution was measured at
a wavelength of 263 nm, and the absorbance (As) was recorded.
The release efficiency using in vitro
dialysis methods. The dialysis bags were placed in distilled water
for 24 h. A total of 8 ml sorafenib nanoparticle suspension was put
into the dialysis bags, the ends of the dialysis bags were clipped,
and the bags were placed into the release medium with magnetic
stirring (31 × g). Of the solution, 1.0 ml was sampled at 0, 0.5,
1, 2, 4, 8, 12,24, 36, 48, and 60 h, with 20 µl of this sample used
to measure the sorafenib content.
The inhibition effect of tumor growth
by sorafenib-incorporated nanoparticles
A total of four experimental groups were utilized in
the present study: Group I, RPMI-1640 culture medium alone (Merck
KGaA, Darmstadt, Germany); group II, blank-loaded nanoparticles
(6.9, 13.8 and 20.8 µmol/l); group III, sorafenib (6.9, 13.8 and
20.8 µmol/l); group IV, sorafenib nanoparticles (6.9, 13.8 and 20.8
µmol/l). RPMI-1640 culture medium was used as dilution solvent. H22
HCC cells (5×108/l) were seeded into plates and cultured
on the condition of 5% CO2 at 37°C, then the H22 HCC
cells were incubated with the RPMI-1640 culture medium plus
blank-loaded nanoparticles, sorafenib or sorafenib nanoparticles
groups in vitro at 37°C for 48 h. The optical density
(wavelength 280 nm) was measured by an ELISA reader following
incubation with CCK-8 (20 µl/well) for 2 h at 37°C. The growth
inhibition rate was calculated as follows: (OD control group - OD
observation group)/OD control group × 100%.
Pharmacokinetic studies of
sorafenib-incorporated nanoparticles in vivo
The SD rats were randomly divided into the sorafenib
group (S) and the sorafenib-incorporated nanoparticle group (SNP),
with three mice per group. The agents were injected via the tail
vein at a dose of 20 mg/kg. Blood samples (0.5 ml of each rat at
per time point) were collected into anticoagulant tubes from caudal
veins at 5, 15, 30, 45 and 60 min, and at 2, 4, 8, 12, 24, 36 and
48 h following the injection. Plasma was aspirated into cryo tubes
and stored at 4°C. A 3200Q-Trap tandem mass spectrometer (Applied
Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA) was
then used to detect the concentrations of sorafenib in blood plasma
at each time point. Pharmacokinetic parameters of the three drugs
[elimination constant, half-life (T1/2)], area under the
curve (AUC)0-48 h, AUCinf, volume of
distribution, serum clearance and concentration/time at max) were
calculated using Drug and Statistics Software version 1.2
(Mathematical Pharmacology Professional Committee of China,
Shanghai, China).
Establishment of a HCC orthotopic
transplantation model in mice
HCC cells in the logarithmic growth phase were
cultured in RPMI-1640 medium and prepared in a cellular suspension
(1×107/l) that was subcutaneously inoculated at a volume
of 0.5 ml into the hind limbs of 3 ICR mice in order to produce a
mass. After three weeks, when the size of the mass in each mouse
reached 1 cm in diameter as measured by vernier caliper, the mice
were sacrificed by exsanguination under deep isoflurane anesthesia
(2% isoflurane, in a sealed glass container) and the entire mass
was resected en bloc and cut into 2×1×1 mm sections.
Additionally, 30 ICR mice were anaesthetized with 60
mg/kg of 1% pentobarbital sodium intraperitoneally. Following the
disinfection of the supine abdominal skin, a 1-cm incision of the
upper abdomen was made to expose the left lateral lobe of the
liver. Tumor tissue from the first group of mice was implanted into
the liver parenchyma in the left lateral lobe and the abdominal
incision was closed using 2/0 silk. Following surgery, the mice
were allowed free access to water and a standard rodent diet.
Biodistribution and antitumor effects
of sorafenib-incorporated nanoparticles in mice
The size of the HCC mass in tumor-bearing mice was
determined by abdominal ultrasonography. When the tumor size
reached 1 cm in diameter, the tumor-bearing mice were assigned
randomly into three groups: Normal saline group; sorafenib group,
100 mg/kg/day by gastric perfusion; sorafenib-incorporating
nanoparticles group, 100 mg/kg/day via the tail vein. A total of 10
mice were allocated into each group. Following three weeks of
treatment, the mice were sacrificed by exsanguination under deep
isoflurane anesthesia, and the heart, lungs, muscles, spleen, tumor
and peritumor liver tissues were harvested to determine the drug
distribution and concentrations in vivo. The weight-volume
ratio was adjusted to 1:2 with distilled water. Following
homogenization, 100 µl homogenate was obtained and vortexed with 10
µl internal standard (loratadine, 100 ng/ml) and 400 µl
acetonitrile. Subsequent to centrifuging at 11,739 × g at 4°C for 3
min, the supernatant was transferred into sampling tubes to measure
the concentration of nanoparticles in tissues using a 3200Q-Trap
tandem mass spectrometer. The length and width of the HCC masses
were also measured. The tumor tissues were fixed in methanol for 24
h, dehydrated in ethanol and embedded in paraffin for pathological
examination.
The formula V = a × b2/2
was used to calculate the volume of HCC (V, volume;
a, length; b, width). The extent of necrosis was
stratified into 3 levels, according to the extent of necrosis:
Mild, ≤30%; moderate, >30-≤70%; severe, >70%. The tumor
inhibitory rate (%) = (1 -
Voberservation/Vcontrol) × 100%
was used to describe the antitumor effect of the drugs.
Statistical analysis
All data are expressed as the mean ± standard
deviation. Measurement data (sorafenib concentration in blood and
tissues) were compared using one-way analysis of variance. Other
data were compared using the χ2 test. Statistical
analyses were performed using SPSS software version 15.0 (SPSS,
Inc., Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Synthesis of mPEG-PDLLA block
copolymer
The mPEG-PDLLA block copolymer was synthetized by
ring-opening polymerization for use as a drug carrier. The
mPEG-PDLLA block copolymer demonstrated highly stable chemical and
physical properties. The m value range was 45–46 and n value range
15–16 (Fig. 1).
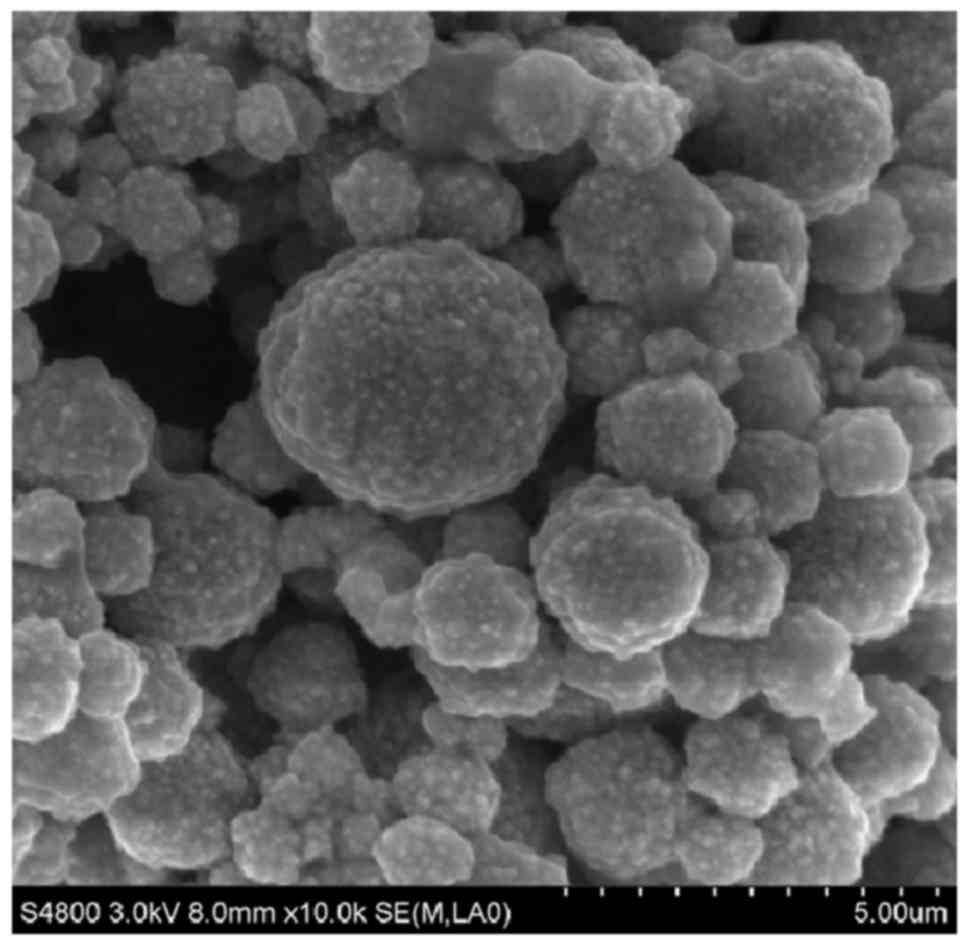
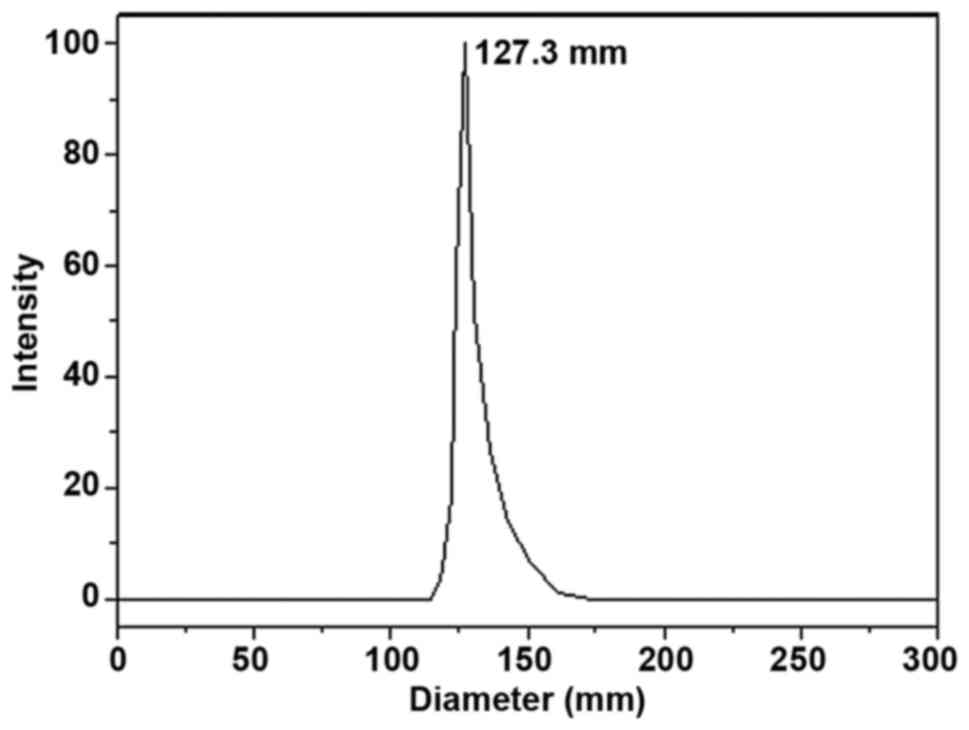
Physical and chemical properties
Sorafenib nanoparticles exhibited a spherical shape
and uniform size (Fig. 2) with a mean
particle size of 127.3±2.0 nm (Fig.
3) and a ξ potential of −3.35±0.42 mV. The drug loading value
was 6.5±0.2%; the encapsulation efficiency was 95±3.2%.
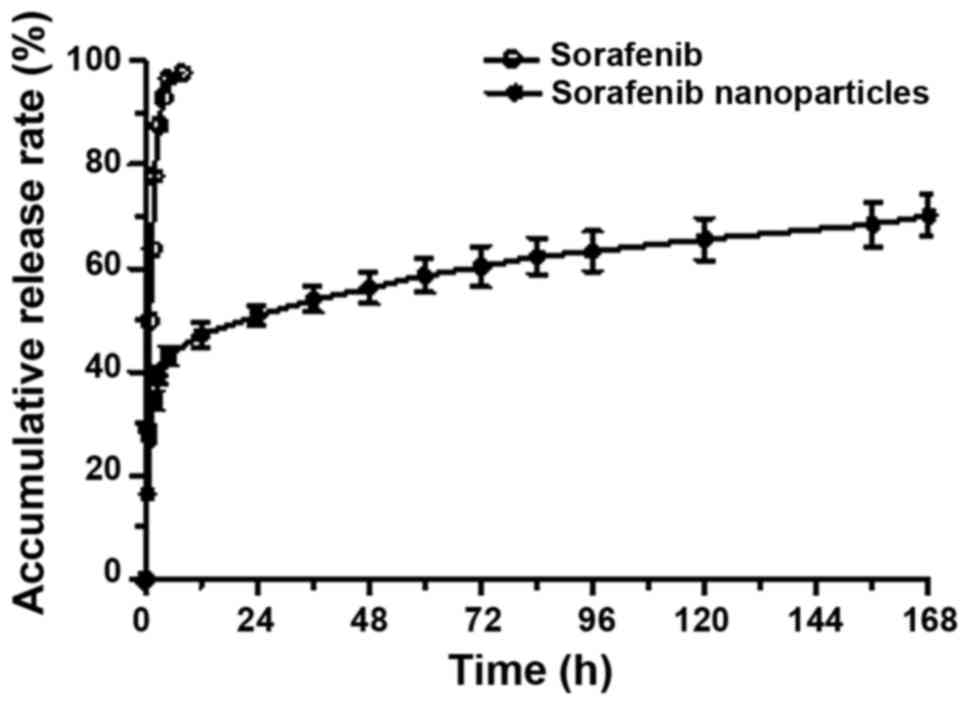
Release kinetics of
sorafenib-incorporated nanoparticles in vitro
Release of sorafenib was complete within 8 h, while
sorafenib-incorporating nanoparticles exhibited a relatively
improved delayed-release effect. The cumulative release rates were
50.91, 56.24, 60.26 and 63.28% at 24, 48, 72 and 96 h,
respectively, following the administration of the nanoparticles
(Fig. 4).
Growth inhibitory effects of
sorafenib-incorporated nanoparticles on HCC cells
There was no significant inhibition on the
proliferation of H22 HCC cells at 48 h in the RPMI-1640 culture
medium and mPEG-PDLLA block copolymer groups. No statistical
significance was identified between the RPMI-1640 culture medium
group and mPEG-PDLLA block copolymer groups. The growth inhibitory
effect on the H22 HCC cells in the sorafenib-incorporating
nanoparticle group was significantly enhanced compared with the
RPMI control group (P<0.05). An upward trend in the growth
inhibitory effect with the increase of drug concentration indicated
the dose-dependent properties of the nanoparticles (P<0.05,
between 6.9 and 20.8 µmol/l), whereas no significant difference
between sorafenib concentrations was observed. Additionally, the
growth inhibitory effect was significantly higher in the sorafenib
nanoparticle group than in the sorafenib group (F=74.988; P<0.05
in sorafenib nanoparticle group vs. sorafenib group; Table I).
 | Table I.In vitro growth inhibitory
effect of sorafenib nanoparticles on H22 HCC cells (mean values ±
standard deviation, n=3). |
Table I.
In vitro growth inhibitory
effect of sorafenib nanoparticles on H22 HCC cells (mean values ±
standard deviation, n=3).
|
| Sorafenib,
µmol/l |
|---|
|
|
|
|---|
| Treatment,%
inhibition | 6.9 | 13.8 | 20.8 |
|---|
| Sorafenib |
31±3.64 |
30.32±3.37 |
30.25±2.81 |
| Sorafenib
nanoparticles |
43.35±2.3a |
48.23±4.76a |
54.13±1.53a,b |
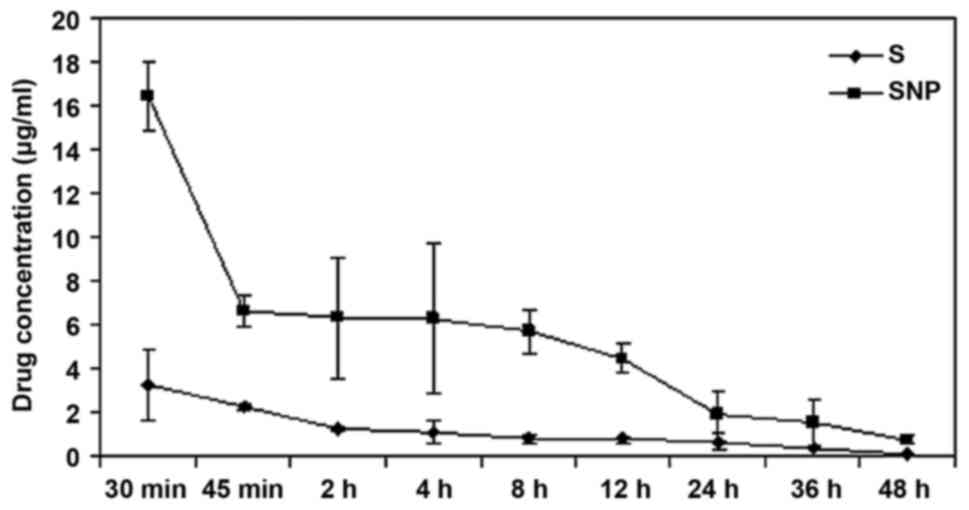
Pharmacokinetics of
sorafenib-incorporated nanoparticles
Sorafenib nanoparticles were metabolized rapidly at
an early stage, but released slowly thereafter, whereas sorafenib
underwent a rapid metabolic process throughout the time. The
T1/2 of sorafenib was 8.22±2.35 h, while the
T1/2 of sorafenib nanoparticles was 12.92±0.57 h. The
clearance rate of the nanoparticles was markedly lower than
sorafenib, thus the circulating time of the nanoparticles was
prolonged to a statistically significant extent (F=2.46;
P<0.05; Table II; Fig. 5).
 | Table II.Pharmacokinetic parameters of
sorafenib nanoparticles in vivo (mean ± standard deviation,
n=3). |
Table II.
Pharmacokinetic parameters of
sorafenib nanoparticles in vivo (mean ± standard deviation,
n=3).
| Parameter | Unit | Sorafenib | Sorafenib
nanoparticles |
|---|
| Elimination rate
constant | 1/h |
0.09±0.02 |
0.05±0.00 |
| Half-life | h |
8.22±2.35 |
12.92±0.57a |
| Time to peak | h |
0.08±0.00 |
0.08±0.00 |
| Concentration of
peak | µg/ml |
5.57±1.65 |
453.73±87.43a |
| Initial
concentration | µg/ml |
7.03±3.20 |
992.86±261.70a |
|
AUC0-t | h·µg/ml |
31.02±6.69 |
275.39±26.10a |
| AUC0-∞ | h·µg/ml |
31.64±6.47 |
289.96±29.33a |
| Volume of
distribution | ml/kg |
8,066.11±4,229.43 |
1,291.06±93.69a |
| Serum
clearance | ml/h/kg |
652.09±147.32 |
69.45±6.99a |
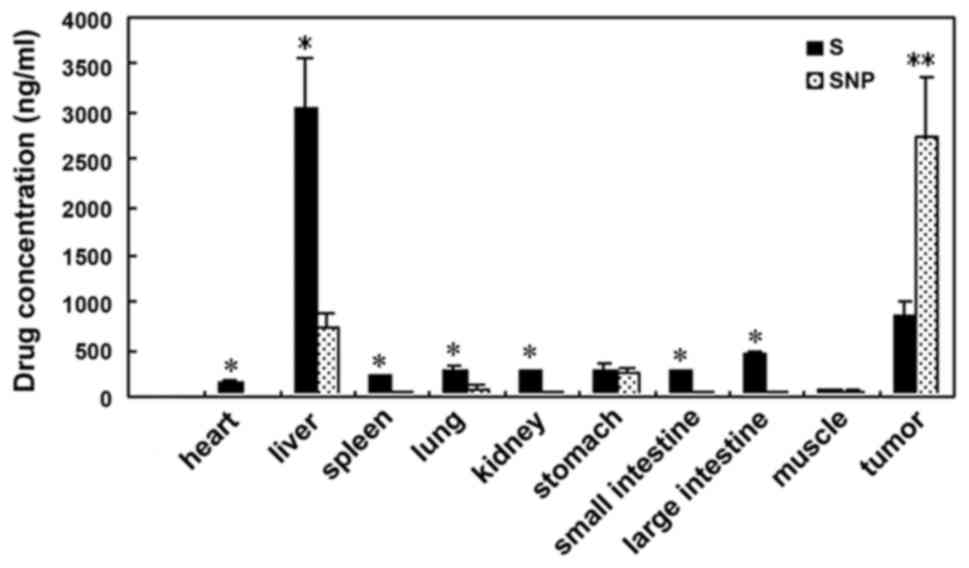
Biodistribution of
sorafenib-incorporated nanoparticles in mice
At three weeks following administration, the
sorafenib concentration in HCC tissue was 860.00±152.39 ng/mg in
the sorafenib group, and 2,751.33±629.6 ng/mg in the
sorafenib-incorporating nanoparticle group, demonstrating
statistical significance (P<0.05). However, in peritumor
tissues, the sorafenib concentration in the nanoparticle group
(728.77±156.39 ng/mg) was lower than in the sorafenib group
(3,030.00±537.03 ng/mg), with statistical significance
(F=69.47; P<0.05). In other tissues, including in the
heart, lungs, kidneys, small and large intestine and the spleen,
the concentration was also lower in the nanoparticle group
(P<0.05), whereas the concentration in the stomach and muscles
was not significantly different between the groups. The high
concentration in HCC, yet reduced concentration elsewhere indicates
the excellent targeting ability of sorafenib nanoparticles on tumor
tissues (Table III; Fig. 6).
 | Table III.The drug concentration of sorafenib
nanoparticles in various tissues (mean values ± standard deviation,
n=3). |
Table III.
The drug concentration of sorafenib
nanoparticles in various tissues (mean values ± standard deviation,
n=3).
|
| Concentration
following treatment, ng/mg |
|---|
|
|
|
|---|
| Tissue | Sorafenib | Sorafenib
nanoparticles |
|---|
| Brain |
19.40±2.16 |
7.96±3.85a |
| Heart |
153.67±25.72 |
17.90±1.56a |
| Lung |
292.67±37.00 |
92.20±32.77a |
| Kidney |
289.00±11.14 |
61.93±5.41a |
| Stomach |
293.67±59.77 |
241.23±71.39 |
| Small
intestine |
281.67±6.43 |
49.97±15.17a |
| Large
intestine |
457.67±37.07 |
37.80±13.85a |
| Muscle |
81.37±5.98 |
64.60±14.20 |
| Spleen |
214.33±17.21 |
45.47±12.70a |
| Liver |
3,030.00±537.03 |
728.77±156.39a |
| Tumor |
860.00±152.39 |
2,751.33±629.60a |
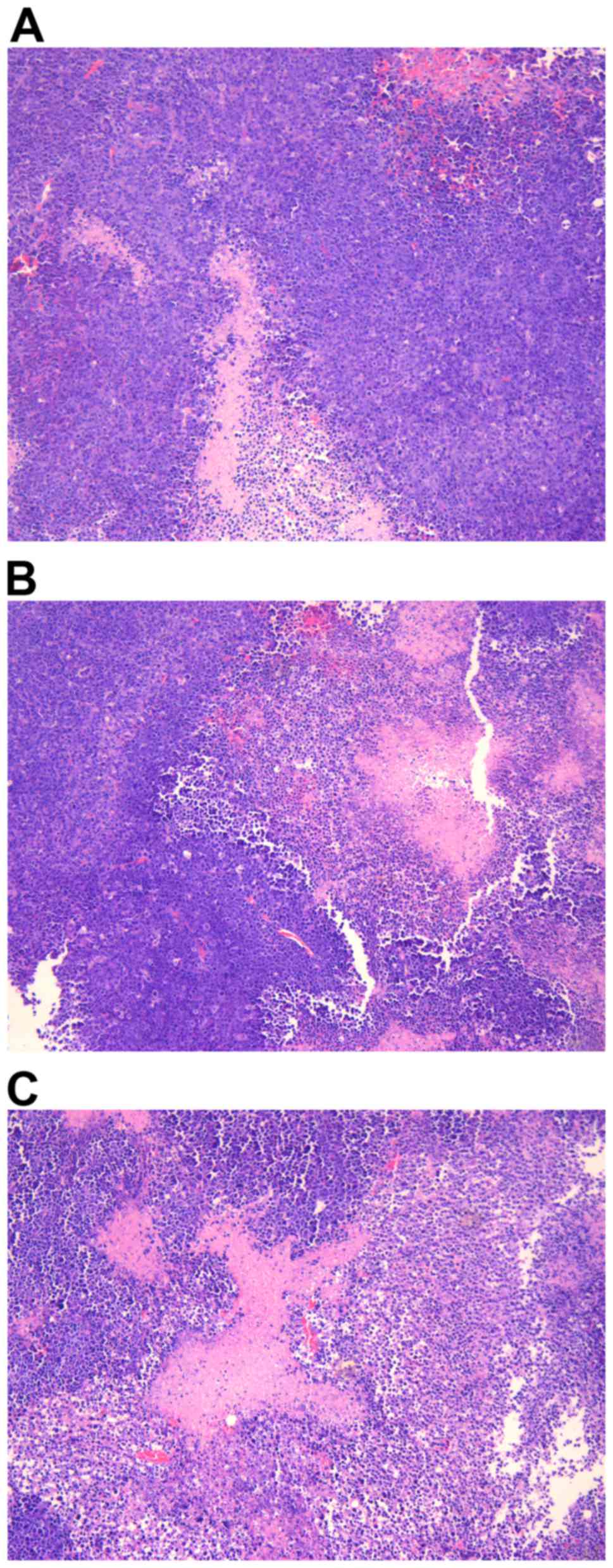
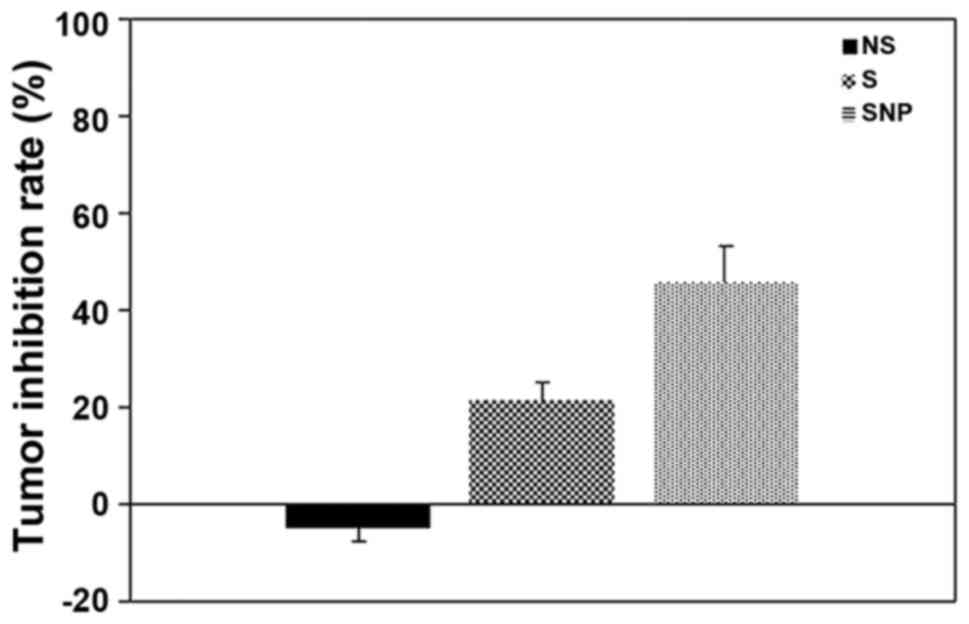
Tumor growth inhibition of sorafenib
nanoparticles in vivo
HCC tissues presented signs of necrosis to various
degrees three weeks following the administration of NS, sorafenib
or sorafenib-incorporated nanoparticles, with an extent of
29.17±9.70, 46.17±12.58 and 63.50±15.08%, respectively. Compared
with NS and sorafenib, the necrosis caused by
sorafenib-incorporated nanoparticles was more severe, to a
statistically significant extent (F=20.12; P<0.05;
Fig. 7); the HCC tumor inhibition
rates were −4.87±2.71, 21.58±3.29 and 45.78±7.46% respectively in
each group, indicating that the most potent antitumor effect was
associated with sorafenib-incorporating nanoparticles to a
statistically significant extent (F=8.752; P<0.05;
Fig. 8).
Discussion
Sorafenib is a novel multi-targeted antitumor agent
with two antitumor effects: Inhibiting tumor growth directly by
suppressing the Raf/MEK/ERK signaling pathway, and indirectly by
inhibiting angiogenesis via downregulating VEGFR and PDGFR. In
vitro research has demonstrated sorafenib may inhibit HCC cell
growth by influencing the cell cycle or inducing apoptosis
(12,13). Sun et al (12) observed that sorafenib attenuated the
autophagy of HepG2 HCC cells to inhibit proliferation and enhance
apoptosis. Liu et al (13)
reported that sorafenib inhibited the proliferation of PLC/PRF/5
and HepG2 HCC cells by inhibiting Raf kinase and blocking the
MEK/ERK signaling pathway, decreasing the level of cyclin D. In
addition, apoptosis was induced by sorafenib via the inhibition of
the Raf/MEK/ERK signaling pathway, decreasing the level of elF4E
phosphorylation and downregulating the expression of the
anti-apoptosis protein Mcl-1 (13).
In clinical trials, sorafenib has been demonstrated
to prolong the overall survival (OS) time and time to progression
of patients with advanced HCC. Using sorafenib to treat 110 HCC
patients, Wang et al (14)
observed a complete response (CR) in 12.7% of the patients, partial
response (PR) in 14.5% and stable disease (SD) in 36.4%, with a
total effective rate of 63.6%. The median OS and progression-free
survival (PFS) times were 10.5 and 5.0 months, respectively;
sorafenib significantly increased the long-term OS rate of patients
with progressive HCC (14). Abou-Alfa
et al (15) reported that in a
stage II clinical trial, of the 137 HCC patients receiving
sorafenib monotherapy, 3 achieved partial remission (2.2%), 8 were
progressing toward remission (5.8%), and 46 reached a level of
stabilization that was maintained over 16 weeks (33.6%). The median
time to progression (mTTP) was 4.2 months, and the median OS time
was 9.2 months. The mTTP of patients positive for phosphorylated
(p)-ERK was 178 days, while the mTTP for p-ERK-negative patients
was only 46 days, suggesting that the activation of the Ras signal
transduction pathway was important to the success of treatment
(15). Relatively few HCC patients
treated with sorafenib achieved PR or complete remission in the
Abou-Alfa et al (15) trial,
although it preliminarily indicated that sorafenib's effects are
molecularly targeted.
However, due to the inhibition of the Raf/MEK/ERK
pathway and direct inhibition of VEGFR-2,3 and PDGFR-β, sorafenib
may interfere with the function of normal cells, leading to adverse
effects. Two stage III clinical trials reported that sorafenib was
safe and prolonged the one-year OS and PFS rates of patients with
advanced HCC from 44 and 47, to 74 and 73%, respectively (16,17). Thus,
sorafenib is used as a standard agent for the systemic treatment of
advanced HCC. In addition, Hu et al (18) reported that in patients with HCC who
received a liver transplant, the disease-free survival (DFS) and OS
of patients treated with oral sorafenib were significantly improved
compared with the control group (DFS, 81.8 vs. 63.6%; OS, 90.9 vs.
72.7%; P<0.05). The acute rejection rate in the oral sorafenib
treatment group and the control group was 13.6 and 18.2%,
respectively, and the graft survival rate was 86.4 and 72.7%,
respectively, although these differences were not statistically
significant (18).
Developing nanoparticle carriers to transport a
large bolus of drug molecules into the cytosolic compartments of
cancer cells has become a highly active research area in
nanomedicine with the development of nanotechnology (19). The properties of nanoparticles that
are produced through nanotechnology include a larger specific
surface area and increasing numbers of surface atoms, surface
energy and surface tension as particle sizes decrease (20). All of these properties endow the
nanoparticles with improved absorbability and biological activity.
Thus, these particles exhibit many excellent properties for use as
drug carriers that alter the distribution patterns of drugs inside
the body. These properties enhance the absorption, utilization and
stability, improve the targeting effect, sustain the release of
drugs, prolong the action time, decrease the necessary dosage,
reduce or eliminate side effects and facilitate storage (19,20). In
our previous study, ring-opening block copolymers of PEG and PLA
were used as drug carriers, and the nanoprecipitation technique was
applied to prepare the sorafenib-precipitated nanoparticles
(21). Sorafenib nanoparticles were
successfully prepared, with a spherical shape and uniform size. The
drug loading and the encapsulation efficiency were
satisfactory.
In the present study, no significant difference was
observed in vitro between the various concentrations of
sorafenib in terms of the rate of H22 cell growth inhibition. By
contrast, the inhibition of the growth of H22 hepatic cells by
sorafenib-incorporated nanoparticles at the same concentration was
more effective, and the extent of inhibition increased in parallel
with the increase in sorafenib-incorporated nanoparticle
concentration, indicating that sorafenib-incorporated nanoparticles
were efficacious in inhibiting hepatic cancer cell proliferation
(Table I). In vivo drug
metabolism rates demonstrated that, while sorafenib had a rapid
metabolic profile, sorafenib nanoparticles were released and
metabolized more slowly and were in circulation for longer than
sorafenib (Table II; Fig. 5). The nanoparticle formulation
produced a high concentration of sorafenib in HCC tissues, but
relatively low concentrations in non-targeted organs (Fig. 6). The tumor necrosis was most severe
and the tumor inhibitory effects the most significant following the
administration of sorafenib nanoparticles (Figs. 7 and 8).
These data suggest that the tumor targeting and antitumor effects
of sorafenib nanoparticles were more significant than for sorafenib
alone.
In conclusion, sorafenib-incorporated nanoparticles
have the desired properties of sustained release and HCC
cell/hepatic tumor tissue specificity. The sorafenib-incorporated
nanoparticles may allow for a change in the route of administration
of sorafenib. The selective targeting of hepatic tumor tissues by
sorafenib-incorporated nanoparticles may provide a promising
strategy to reduce the adverse effects of sorafenib and may perhaps
facilitate an increase in the therapeutically tolerable doses of
sorafenib, when compared with standard sorafenib
administration.
Acknowledgements
This study was supported by the Major Project of
Science and Technology Commission of Shanghai Putuo district (grant
no. 2010-B-107). The authors are grateful to Professor Zhang Yan
(the Second Military Medicine University, Shanghai, China) for the
correction and translation of the manuscript.
References
|
1
|
Matsuda Y, Ichida T and Fukumoto M:
Hepatocellular carcinoma and liver transplantation: Clinical
perspective on molecular targeted strategies. Med Mol Morphol.
44:117–124. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tang ZY, Ye SL, Liu YK, Qin LX, Sun HC, Ye
QH, Wang L, Zhou J, Qiu SJ, Li Y, et al: A decade's studies on
metastasis of hepatocellular carcinoma. J Cancer Res Clin Oncol.
130:187–196. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lyons JF, Wilhelm S, Hibner B and Bollag
G: Discovery of a novel Raf kinase inhibitor. Endocr Relat Cancer.
8:219–225. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wilhelm SM, Carter C, Tang L, Wilkie D,
McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, et al:
BAY 43–9006 exhibits broad-spectrum oral antitumor activity and
targets the RAF/MEK/ERK pathway and receptor tyrosine kinases
involved in tumor progression and angiogenesis. Cancer Res.
64:7099–7109. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Clark JW, Eder JP, Ryan D, Lathia C and
Lenz HJ: Safety and pharmacokinetics of the dual action Raf kinase
and vascular endothelial growth factor receptor inhibitor,
BAY43-9006, in patients with advanced, refractory solid tumors.
Clin Cancer Res. 11:5472–5480. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Luo XN, Lu LG, Shao PJ, Hu BS, Li Y, Yu XY
and He X: Relationship between sorafenib-associated hand-food skin
reaction and efficacy in treatment of advanced hepatocellular
carcinoma. Zhonghua Yi Xue Za Zhi. 92:889–893. 2012.(In Chinese).
PubMed/NCBI
|
|
8
|
Chu D, Lacouture ME, Fillos T and Wu S:
Risk of hand-foot skin reaction with sorafenib: A systematic review
and meta-analysis. Acta Oncol. 47:176–186. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Stmmberg D, Awada A, Hirte H, Clark JW,
Seeber S, Piccart P, Hofstra E, Voliotis D, Christensen O,
Brueckner A and Schwartz B: Pooled safety analysis of BAY 43–9006
(sorafenib) monotherapy in patients with advanced solid tumours: Is
rash associated with treatment outcome? Eur J Cancer. 42:548–556.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Robert C, Sofia JC, Spatz A, Le Cesne A,
Malka D, Pautier P, Wechsler J, Lhomme C, Escudier B, Boige V, et
al: Cutaneous side effects of kinase inhibitors and blocking
antibodies. Lancet Oncol. 6:491–500. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang CH, Lin WC, Chuang CK, Chang YC, Pang
ST, Lin YC, Kuo TT, Hsieh JJ and Chang JW: Hand-foot skin reaction
in patients treated with sorafenib: A clinicopathological study of
cutaneous manifestations due to multitargeted kinase inhibitor
therapy. Br J Demmtol. 158:592–596. 2008. View Article : Google Scholar
|
|
12
|
Sun GT, Qiu WH, Shi MM and Chen Z:
Sorafenib inhibits human hepatoma cell line HepG2 autophagy. J Surg
Concepts Pract. 15:51–55. 2010.(In Chinese).
|
|
13
|
Liu L, Cao Y, Chen C, Zhang X, McNabola A,
Wilkie D, Wilhelm S, Lynch M and Carter C: Sorafenib blocks the
RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor
cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer
Res. 66:11851–11858. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang CP, Lu YY, Gao XD, Wang Z, Bai WL, Qu
JH, Zeng Z, Zhang M, Chang XJ, Yang YP and Jie FJ: Efficacy of
sorafenib for advanced hepatocellular carcinoma and prognostic
factors. Chin J Clin Oncol. 39:587–592. 2012.(In Chinese).
|
|
15
|
Abou-Alfa GK, Schwartz L, Ricci S, Amadori
D, Santoro A, Figer A, De Greve J, Douillard JY, Lathia C, Schwartz
B, et al: Phase II study of sorafenib in patients with advanced
hepatocellular carcinoma. J Clin Onco1. 24:4293–4300. 2006.
View Article : Google Scholar
|
|
16
|
Liovet J, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: A phase III randomized, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hu AB, He XS, Tai Q, Zhu XF, Ma Y, Wang
DP, Wang GD, Wu LW, Ju WQ and Huang JF: Efficacy and safety of
sorafenib in the prevention and treatment of hepatocellular
carcinoma recurrences after liver transplantation. Zhonghua Yi Xue
Za Zhi. 92:1264–1267. 2012.(In Chinese). PubMed/NCBI
|
|
19
|
Qin JM, Zhang YD, Wang HY, et al:
Nanotechnology usage in diagnosis and treatment of liver diseases.
Chin J Mod Med. 13:49–52. 2003.
|
|
20
|
Qin JM, Zhang YD, Wang HY and Wu MC:
Application and progress of nano-drugs in liver disease. Chin J
Hepatobiliary Surg. 10:646–648. 2004.(In Chinese).
|
|
21
|
Qin JM, Yin PH, Li Q, Sa ZQ, Sheng X, Yang
L, Huang T, Zhang M, Gao KP, Chen QH, et al: Anti-tumor effects of
brucine immuno-nanoparticles on hepatocellular carcinoma. Int J
Nanomedicine. 7:369–379. 2012. View Article : Google Scholar : PubMed/NCBI
|