Introduction
In 1882, Halsted pioneered the radical resection of
the breast. Breast surgery methods have changed since and
clinicians commonly perform breast-conserving surgery. However, the
optimal approach for radical resection remains controversial
(1). Along with social progress and
improvements in the quality of life, patients with cancer,
particularly patients with breast cancer have increasing
requirements for the function and cosmetic outcome following
surgery (2,3). A previous study identified that 61% of
patients reported that the opinions of their partners of the scars
were important to them (4). The way
an incision is closed and managed post-operatively affects cosmetic
outcome (5). Historically, in breast
cancer surgery, simultaneously ensuring treatment effect, shrinking
excision scope and attending to the cosmetic effect has been
important (6). To improve the
aesthetic results for female patients undergoing breast cancer
surgery, surgical techniques have been developed to render scars
less noticeable (7,8).
In China, the majority of patients with breast
cancer are treated with modified radical surgery using
discontinuous silk suture, which leaves a very noticeable scar
(9). A study on cosmetic surgery
identified that 50% of patients reported that the extent of the
visual scar greatly affected their self-assessment of the outcome
(10).
Previous studies have assessed how drugs can be used
to decrease scarring but the results demonstrated that there
remains no ‘gold standard’ for the prevention and treatment of
hypertrophic scars (11,12). The authors of the present study
evaluated the methods of closing wounds in modified radical surgery
in April 2014 and proposed using intradermal suture with Ti-Ni
memory alloy wire (13). After >2
years of practice and observation, the wounds of patients with
scarring markedly improved following intradermal suture with Ti-Ni
memory alloy wire.
The primary objective of the present study is to
assess the impact of using a Ti-Ni memory alloy wire intradermal
sutures on the cosmetic outcome of the wound scar within 25 weeks
following mastectomy.
Materials and methods
Study design
Prior to the start of the present study, the methods
of surgical suturing were altered and the postoperative effects
were observed. After >2 years of observing and evaluating
Vancouver Scar Scale (VSS) scores and the number of wound healing
day(s), the present study reviewed the retrospective data. The
present study is a retrospective observational cohort study with
parallel groups and compares conventional closure with closure
using intradermal sutures and Ti-Ni memory alloy wire in patients
undergoing mastectomy with or without axillary surgery.
Setting
The present study included diagnostic surgery and
post-operative adjuvant chemotherapy for patients with breast
cancer in the Department of Thoracic Surgery and Oncology of the
First Affiliated Hospital of Xi'an Jiaotong University (Shaanxi,
China), a process that took ~6 months. The patients were treated
with interrupted suture or intradermal suture.
Inclusion and exclusion criteria
The inclusion criteria were as follows: i) Female
patients with operable breast cancer (invasive carcinoma and/or
ductal carcinoma in situ); ii) age, ≥18 and ≤85 years; iii)
scheduled for mastectomy either alone or in association with
axillary clearance; iv) either sentinel lymph node biopsy or
standard level I/II axillary node dissection (14); v) written hospital-approved informed
consent by the patient; and vi) surgical wound classified class I
(Surgical Wound Classification) (15). Patients were excluded if any of the
following criteria were met: i) Undergoing surgery for modified
radical mastectomy with immediate breast reconstruction, cosmetic
breast operations, reduction, expansion, insertion of a prosthesis,
duct ectasia, infective breast disease or implant; ii) surgical
wounds identified as class II, III or IV using Centers for Disease
Control surgical site infection Surgical Wound Classification
(15); iii) inflammatory breast
cancer or skin ulceration; iv) presence of physical or psychiatric
conditions that could impair outcome assessment and intended
follow-up (5); v) personal or family
skin scar history; vi) received an experimental drug or used an
experimental medical device within 30 days prior to the planned
start of treatment; vii) employees of the assessor associated with
the proposed study or other studies under the direction of that
assessor; and viii) unlikely to comply with chemotherapy or
complete the 25-week follow-up visit.
Patients
The first patient received intradermal sutures using
Ti-Ni memory alloy wire in April 2014. In total, 98 female patients
aged between 24 and 74 years, categorized into the active (n=50)
and control (n=48) groups, were enrolled between April 2014 and
April 2016. A total of 10 patients suffered from diabetes in the
active group and 9 patients suffered from diabetes in the control
group. The patients of control group were treated with traditional
methods of wound closure. The present study reviewed all patient
data for those admitted to the Second Department of Thoracic
Surgery of the First Affiliated Hospital of Xi'an Jiaotong
University (Shaanxi, China) who met the inclusion criteria. The
present study focused on scarring. Baseline data were collected
following enrollment during the therapy period. The First
Affiliated Hospital of Xi'an Jiaotong University Ethics Committee
approved the present study. Written informed consent was obtained
from all patients.
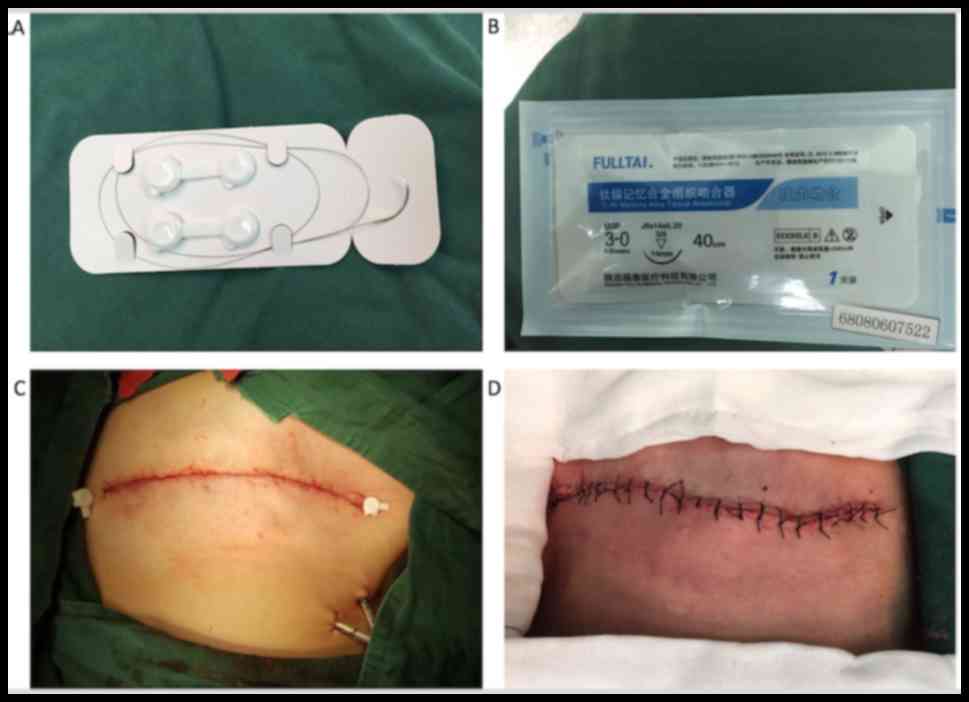
Study interventions
Experienced breast surgeons using a standardized
technique performed mastectomies (16). The skin incision included the tumor
biopsy site, any invaded or edematous skin and the nipple-areola
complex (17). The present study
addressed the type of wound closure in mastectomy. The patients
were divided into two groups, and the two groups were distinguished
by the use of two different types of wound closure. In the
intradermal suture group, intradermal suture using Ti-Ni memory
alloy wire was implemented. In the conventional closure group, the
incision was closed using the interrupted transcutaneous pattern
with Chinese silk (Fig. 1). These two
sutures were removed when the wounds were adequately healed (i.e.,
re-establishment of normal tissue integrity).
All patients were provided with a drainage tube and
suction bottle to prevent subcutaneous seroma following mastectomy.
All patients received chemotherapy and the same follow-up plan,
including chest-abdominal computed tomography and tumor markers,
was implemented every 3 months (18,19). The
scars were assessed 25 weeks following mastectomy. All scars were
assessed independently by three observers (one oncologist and two
breast cancer research associates) on the same day, using the VSS.
The VSS observes four physical characteristics of scars:
Vascularity, pigmentation, pliability and height (20,21). Each
variable contains ranked subscales that may be summed to obtain a
total score ranging from 0 to 13, with 0 representing normal skin
(Table I) (20,21).
 | Table I.Vancouver Scar Scale for assessment of
the physical characteristics of scars. |
Table I.
Vancouver Scar Scale for assessment of
the physical characteristics of scars.
| Characteristic | Score |
|---|
| Vascularity |
|
|
Normal | 0 |
| Pink | 1 |
| Red | 2 |
|
Purple | 3 |
| Pigmentation |
|
|
Normal | 0 |
|
Hypopigmentation | 1 |
|
Hyperpigmentation | 2 |
| Pliability |
|
|
Normal | 0 |
| Supple
(flexible with minimal resistance) | 1 |
| Yielding
(gives way to pressure) | 2 |
| Firm
(inflexible not easily moved; resistant to manual pressure) | 3 |
| Ropes
(rope-like tissue that blanches with extension of scar) | 4 |
|
Contracture (permanent
shortening of scar leading to deformity or distortion) | 5 |
| Height, mm |
|
| Normal
(flat) | 0 |
|
<2 | 1 |
| 2–5 | 2 |
|
>5 | 3 |
| Total score | 13 |
Statistical analysis
All statistical analyses were performed using
computer software SPSS (version 16.0; SPSS, Inc., Chicago, IL,
USA). In the present study, the differences between the baseline
characteristics of patients were compared using Fisher's exact test
for the different categories and independent sample t-test for
continuous variables. The endpoint means of the VSS scores were
analyzed using independent sample t-test. P<0.05 was considered
to indicate a statistically significant difference.
Results
Characteristics of enrolled
patients
All patients completed the present study. The
baseline characteristics of the patients were provided (Table II). The present study compared the
baseline characteristics of the two groups. The groups were similar
in terms of mean age (P>0.05), body mass index (P>0.05),
operating time (P>0.05), blood loss (P>0.05), length of
post-operative hospital stay (P>0.05), pathological stage (7th
edition; American Joint Committee on Cancer/Union for International
Cancer Control tumor-node-metastasis staging systems; P>0.05)
and medical history (P>0.05) (22).
 | Table II.Comparison of the baseline
characteristics of patients who underwent mastectomy (n=98). |
Table II.
Comparison of the baseline
characteristics of patients who underwent mastectomy (n=98).
| Characteristics | Active group
(n=50) | Control group
(n=48) | χ2 or
t-value | P-value |
|---|
| Mean ± SD age,
years | 47.38±11.64 | 46.58±11.79 | 0.337
(t-value) | 0.737 |
| BMI,
kg/m2 | 26.55±4.38 | 27.17±4.21 | 0.710
(t-value) | 0.479 |
| Diabetes, n
(%) | 0 | 1 (2.08) | | 0.490 |
| Pulmonary history
(COPD), n (%) | 1 (2.00) | 0 | | 1.000 |
| Cardiac history
(coronary disease), n (%) | 0 | 1 (2.08) | | 0.490 |
| Smoking history, n
(%) | 2 (4.00) | 2 (4.17) | | 0.676 |
| Working outside the
home, n (%) | 6
(12.00) | 4 (8.33) | | 0.741 |
| Pathological stage,
n (%) | | | 1.344
(χ2-value) | 0.969 |
| I | 1 (2.00) | 1 (2.08) |
|
|
|
IIA | 12 (24.00) | 12 (25.00) |
|
|
|
IIB | 15 (30.00) | 17 (35.42) |
|
|
|
IIIA | 9
(18.00) | 8
(16.67) |
|
|
|
IIIB | 11 (22.00) | 9
(18.75) |
|
|
|
IIIC | 1 (2.00) | 1 (2.08) |
|
|
| IV | 1 (2.00) | 0 |
|
|
| Mean ± SD operating
time, min | 100.98±11.31 | 103.54±11.01 | 1.135
(t-value) | 0.259 |
| Mean ± SD blood
loss, ml | 52.30±17.58 | 50.08±15.82 | 0.655
(t-value) | 0.514 |
| Mean ± SD
postoperative hospital stay, days | 4.36±0.83 | 4.45±0.97 | 0.542
(t-value) | 0.589 |
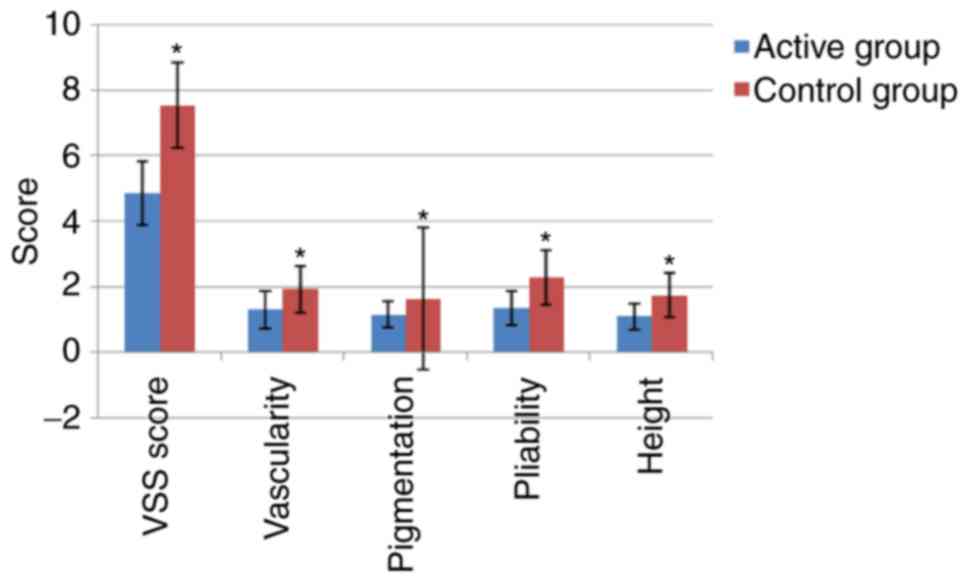
Cosmetic outcome
Results demonstrated that the mean VSS score of the
active group was decreased (indicating improved cosmetic outcome)
compared with that of the control group (P<0.001; Table III). The four features of the VSS
scores differed statistically (P<0.001). The cosmetic results of
suturing for four cases are also presented in Fig. 2. A comparison of cosmetic results
between the experimental and control groups is shown in Fig. 3, and statistical differences between
the active and control groups are shown.
 | Table III.Vancouver Scar Scale scores for the
active and the control group. |
Table III.
Vancouver Scar Scale scores for the
active and the control group.
|
Outcomea | Active group
(n=50) | Control group
(n=48) | t-value | P-value |
|---|
| Vancouver Scar
Scale score | 4.86±0.97 | 7.54±1.30 | 11.518 | <0.001 |
|
Vascularity | 1.30±0.58 | 1.92±0.71 | 4.718 | <0.001 |
|
Pigmentation | 1.14±0.40 | 1.63±2.16 | 5.336 | <0.001 |
|
Pliability | 1.34±0.52 | 2.27±0.84 | 6.543 | <0.001 |
|
Height | 1.08±0.40 | 1.73±0.68 | 5.771 | <0.001 |
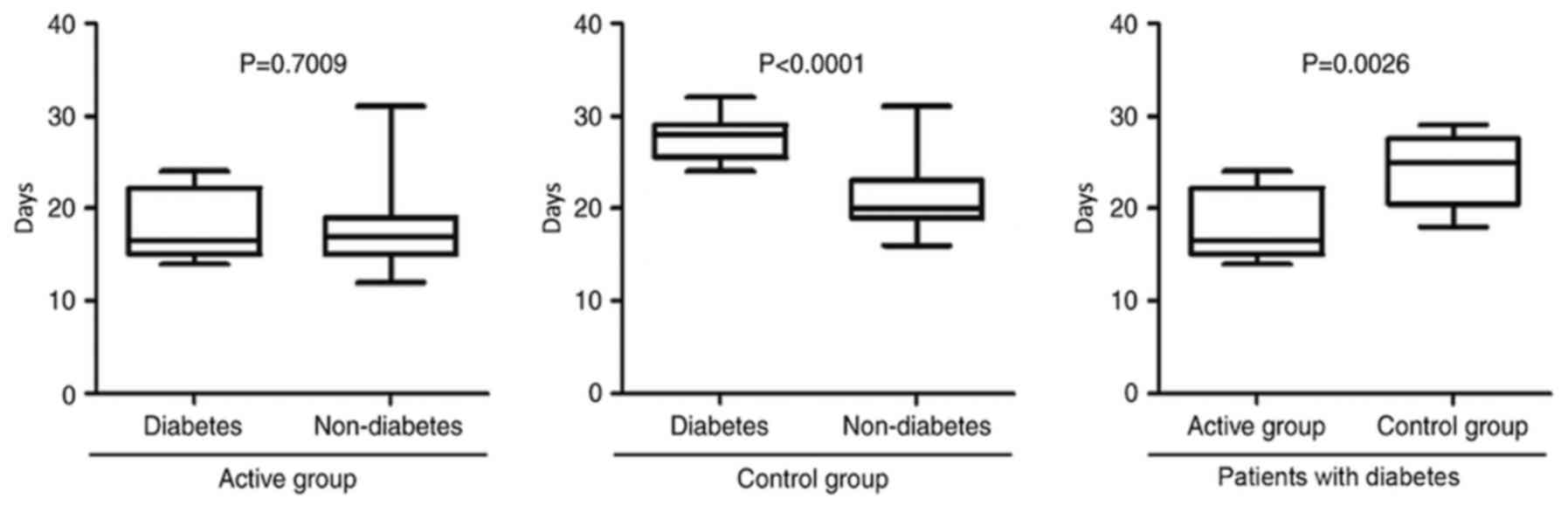
Unexpected benefits of using memory
alloy wire in patients with diabetes
Aside from improved recovery from the surgical
wound, the present study also observed accelerated wound healing in
both groups. The mean number of wound healing days required to take
out stitches was decreased for the active group compared with that
for the control group in patients with diabetes (P=0.0026; Fig. 4). Results indicated that using Ti-Ni
memory alloy wire was able to decrease the days of wound healing
required between patients with diabetes and their non-diabetic
counterparts (P=0.7009; Fig. 4).
Results of the present study suggested that using memory alloy
facilitated wound healing.
Discussion
In the present study, the scar of patients in the
active group was limited to a light spot in the majority of cases.
The results of the present study indicated that patients whose
incisions were closed using intradermal suture with Ti-Ni memory
alloy wire suture exhibited an improved cosmetic outcome compared
with those for whom incisions were closed using the interrupted
suturing technique. The cosmetic outcome was assessed using VSS.
VSS is a reliable, comprehensive approach for assessing linear
surgical scars (23). VSS assesses
four subjective variables (vascularity, pigmentation, pliability
and height) within a range of 0–13 for the total score (calculated
as the sum of all four subjective variables scores), where a lower
score (0–4) indicates improved healing (21).
In China, certain surgeons use discontinuous silk
suture to close the skin incision (9,24).
Therefore, suture track scars are present on each side of the
incision in numerous cases and one can observe a suture reaction,
inflammation, liquefaction, infection or incision dehiscence
requiring secondary suture (4). Scars
are usually caused by excessive repair of skin wounds due to
excessive proliferation, activation and migration of fibroblasts.
Increase in the biosynthesis of fibroblasts cause excessive
collagen deposition of extracellular matrix (25,26).
Collagen fibers also form here as a result of the body synthesizing
collagen at an increased rate compared with that at which it
catabolizes collagen over a longer period of time (27,28).
The present study indicated that continuous
intradermal suture was able to decrease scar formation compared
with the control group, although patients exhibited scar
hyperplasia. Despite this, intradermal suture may decrease the
discomfort the hyperplastic scar causes, including prominent
surface, thick texture, local pain, heat-induced itch. Intradermal
suture may also improve the function of sleep quality (29–31).
Typically, the time taken for wounds to heal in patients without
diabetes is decreased compared with patients with diabetes
(32–35). Consistent with these previous studies,
it was indicated in the present study that the time taken for
wounds to heal in patients with diabetes was increased compared
with that of the patients without diabetes in the control group.
However, the time taken for wounds to heal in patients with and
without diabetes was similar in the active group. Furthermore, it
was indicated that the time taken for wounds to heal in patients
with diabetes differed significantly between the active and control
groups, the healing time of active groups was shorter compared with
that of control groups. The present study suggested that continuous
intradermal suture of incision with Ti-Ni memory alloy wire may
promote skin incisions to heal and decrease scar hyperplasia, and
therefore this method may be recommended to other surgeons for
patients undergoing mastectomy with or without axillary
surgery.
The present study was a retrospective, observational
cohort study and had a number of limitations. The present study was
not double blind, which may have generated bias. The 2-year
follow-up period was short, and the prognosis of disease was not
assessed. VSS reflects the different physical characteristics
carried out by the observer, reflecting different physiological
aspects of wound healing and scar maturation. The present study
identified that VSS scores objectively reflected scar maturation.
However, the VSS does not include a self-assessment of the patient
outcome.
To conclude, the intradermal suture technique offers
an improved cosmetic outcome for patients undergoing mastectomy
with or without axillary surgery. The present study suggested that
intradermal suture using Ti-Ni memory alloy wire may represent an
effective means of inhibiting scars from forming following
mastectomy. For patients undergoing intradermal suture using Ti-Ni
memory alloy wire, the scar was less noticeable and wound healing
was improved compared with the control group, particularly in
patients with diabetes.
Acknowledgements
The present study was supported by the National
Science Foundation for Young Scientists of China (grant nos.
81402506 and 81602597).
References
|
1
|
Akram M and Siddiqui SA: Breast cancer
management: Past, present and evolving. Indian J Cancer.
49:277–282. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sehl M, Lu X, Silliman R and Ganz PA:
Decline in physical functioning in first 2 years after breast
cancer diagnosis predicts 10-year survival in older women. J Cancer
Surviv. 7:20–31. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Derks MG, de Glas NA, Bastiaannet E, de
Craen AJ, Portielje JE, van de Velde CJ, van Leeuwen FE and Liefers
GJ: Physical functioning in older patients with breast cancer: A
prospective cohort study in the TEAM trial. Oncologist. 7:946–953.
2016. View Article : Google Scholar
|
|
4
|
Joyce CW, Murphy S, Murphy S, Kelly JL and
Morrison CM: Scar wars: Preferences in breast surgery. Arch Plast
Surg. 42:596–600. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang ZT, Zhang HW, Fang XD, Wang LM, Li
XX, Li YF, Sun XW, Carver J, Simpkins D, Shen J and Weisberg M:
Cosmetic outcome and surgical site infection rates of antibacterial
absorbable (Polyglactin 910) suture compared to Chinese silk suture
in breast cancer surgery: A randomized pilot research. Chin Med J
(Engl). 124:719–724. 2011.PubMed/NCBI
|
|
6
|
Ünsal MG, Dural AC, Çelik MF, Akarsu C,
Başoğlu İ, Dilege ME, Kapan S and Alış H: The adaptation process of
a teaching and research hospital to changing trends in modern
breast surgery. Ulus Cerrahi Derg. 31:34–38. 2014.PubMed/NCBI
|
|
7
|
Peyser PM, Abel JA, Straker VF, Hall VL
and Rainsbury RM: Ultraconservative skin-sparing ‘keyhole’
mastectomy and immediate breast and areola reconstruction. Ann R
Coll Surg Engl. 82:227–235. 2000.PubMed/NCBI
|
|
8
|
Shrotria S: The periareolar incision -
gateway to the breast! Eur J Surg Oncol. 27:601–603. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang J, Zhang YF, Wang X, Wang J, Yang X,
Gao YQ and Fang Y: Treatment outcomes of occult breast carcinoma
and prognostic analyses. Chin Med J (Engl). 126:3026–3029.
2013.PubMed/NCBI
|
|
10
|
Hoeller U, Kuhlmey A, Bajrovic A, Grader
K, Berger J, Tribius S, Fehlauer F and Alberti W: Cosmesis from the
patient's and the doctor's view. Int J Radiat Oncol Biol Phys.
57:3452003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
O'Kane S: Wound remodeling and scarring. J
Wound Care. 11:296–299. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Truong PT, Lee JC, Soer B, Gaul CA and
Olivotto IA: Reliability and validity testing of the patient and
observer scar assessment scale in evaluating linear scars after
breast cancer surgery. Plast Reconstr Surg. 119:487–494. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Neelakantan L, Zglinski JK, Frotscher M
and Eggeler G: Design and fabrication of a bending rotation fatigue
test rig for in situ electrochemical analysis during fatigue
testing of NiTi shape memory alloy wires. Rev Sci Instrum.
84:0351022013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kinoshita T, Takasugi M, Iwamoto E,
Akashi-Tanaka S, Fukutomi T and Terui S: Sentinel lymph node biopsy
examination for breast cancer patients with clinically negative
axillary lymph nodes after neoadjuvant chemotherapy. Am J Surg.
191:225–229. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yamamoto T, Takahashi S, Ichihara K,
Hiyama Y, Uehara T, Hashimoto J, Hirobe M and Masumori N: How do we
understand the disagreement in the frequency of surgical site
infection between the CDC and Clavien-Dindo classifications? J
Infect Chemother. 21:130–133. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li YJ, Huang XE and Zhou XD: Local breast
cancer recurrence after mastectomy and breast-conserving surgery
for Paget's disease: A meta-analysis. Breast Care (Basel).
9:431–434. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ouldamer L, Bonastre J, Brunet-Houdard S,
Body G, Giraudeau B and Caille A: Dead space closure with quilting
suture versus conventional closure with drainage for the prevention
of seroma after mastectomy for breast cancer (QUISERMAS): Protocol
for a multicenter randomized controlled trial. BMJ Open.
6:e0099032016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
MacFater H, MacFater W, Hill A and Lill M:
Individualised follow-up booklets improve recall and satisfaction
for cancer patients. N Z Med J. 130:39–45. 2017.PubMed/NCBI
|
|
19
|
Allinson VM and Dent J: Supportive care
after breast cancer surgery. Nurs Times. 110:20–23. 2014.PubMed/NCBI
|
|
20
|
Pauline T, Truong F, Yong CM, Hayashi A,
Runkel JA, Phillips T and Olivotto IA: Standardized assessment of
breast cancer surgical scars integrating the vancouver scar scale,
short-form mcgill pain questionnaire and patients' perspectives.
Plast Reconstr Surg. 116:1291–1299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nedelec B, Shankowsky HA and Tredget EE:
Rating the resolving hypertrophic scar: Comparison of the vancouver
scar scale and scar volume. J Burn Care Rehabil. 21:205–212. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ursaru M, Jari I, Popescu R, Negru D, Naum
A and Scripcariu V: Multifactorial analysis of local and lymph node
recurrences after conservative or radical surgery for stage 0–II
breast cancer. Rev Med Chir Soc Med Nat Iasi. 118:1062–1067.
2014.PubMed/NCBI
|
|
23
|
Kaartinen IS, Välisuo PO, Bochko V,
Alander JT and Kuokkanen HO: How to assess scar hypertrophy - a
comparison of subjective scales and Spectrocutometry: A new
objective method. Wound Repair Regen. 19:316–323. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhao WX, Wang B, Yan SY and Zhang LY:
Strategy of points, lines and layers in needle assisted laparoscope
functional modified neck dissection through bilateral breast
approach. Zhonghua Wai Ke Za Zhi. 54:823–827. 2016.(In Chinese).
PubMed/NCBI
|
|
25
|
Liebl H and Kloth LC: Skin cell
proliferation stimulated by microneedles. J Am Coll Clin Wound
Spec. 4:2–6. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Guo J, Lin Q, Shao Y, Rong L and Zhang D:
miR-29b promotes skin wound healing and reduces excessive scar
formation by inhibition of the TGF-β1/Smad/CTGF signaling pathway.
Can J Physiol Pharmacol. 95:437–442. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li J, Chen L, Cao C, Yan H, Zhou B, Gao Y,
Li Q and Li J: The long non-coding RNA LncRNA8975-1 is upregulated
in hypertrophic scar fibroblasts and controls collagen expression.
Cell Physiol Biochem. 40:326–334. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li H, Yang L, Zhang Y and Gao Z:
Kaempferol inhibits fibroblast collagen synthesis, proliferation
and activation in hypertrophic scar via targeting TGF-β receptor
type I. Biomed Pharmacother. 83:967–974. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kotaluoto S, Pauniaho SL, Helminen M,
Kuokkanen H and Rantanen T: Wound healing after open appendectomies
in adult patients: A prospective, randomised trial comparing two
methods of wound closure. World J Surg. 36:2305–2310. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Koskela A, Kotaluoto S, Kaartinen I,
Pauniaho SL, Rantanen T and Kuokkanen H: Continuous absorbable
intradermal sutures yield better cosmetic results than
nonabsorbable interrupted sutures in open appendectomy wounds: A
prospective, randomized trial. World J Surg. 38:1044–1050. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Paolini S, Morace R, Lanzino G, Missori P,
Nano G, Cantore G and Esposito V: Absorbable intradermal closure of
elective craniotomy wounds. Neurosurgery. 62 Suppl 2:ONS490–ONS492.
2008.PubMed/NCBI
|
|
32
|
Sorg H, Tilkorn DJ, Hager S, Hauser J and
Mirastschijski U: Skin wound healing: An update on the current
knowledge and concepts. Eur Surg Res. 58:81–94. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nouvong A, Ambrus AM, Zhang ER, Hultman L
and Coller HA: Reactive oxygen species and bacterial biofilms in
diabetic wound healing. Physiol Genomics. 48:889–896. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Reed GW, Salehi N, Giglou PR, Kafa R,
Malik U, Maier M and Shishehbor MH: Time to wound healing and major
adverse limb events in patients with critical limb ischemia treated
with endovascular revascularization. Ann Vasc Surg. 36:190–198.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Khamaisi M, Katagiri S, Keenan H, Park K,
Maeda Y, Li Q, Qi W, Thomou T, Eschuk D, Tellechea A, et al: PKCδ
inhibition normalizes the wound-healing capacity of diabetic human
fibroblasts. J Clin Invest. 126:837–853. 2016. View Article : Google Scholar : PubMed/NCBI
|