Introduction
Adenoid cystic carcinoma (ACC) is a malignant
neoplasm that derives from glandular tissue. ACC is most commonly
located in the salivary glands, but it also occurs in other organs
that contain glands, including the trachea (1). The occurrence of ACC in the trachea is
extremely rare in Poland according to data from the Polish National
Cancer Registry; in 2014, the incidence of tracheal cancer was 11
cases among the female population and 18 cases among the male
population, of which few were ACC (2). ACC is characterized by slow growth and
local involvement; it exhibits a high tendency for recurrence.
Symptoms result from obstruction of the tracheal lumen (3). Dyspnea, which increases over months, is
the most common symptom (3). The
primary management of tracheal ACC is surgical resection of part of
the trachea and tumor with end-to-end anastomosis (3). Postoperative radiotherapy is recommended
for patients that undergo incomplete resection (3). Radical radiotherapy should be considered
as an option for patients with unresectable disease (3). The present study describes a case of
recurrent ACC of the trachea in a young woman treated with
irradiation.
Case report
A 23-year-old woman who had suffered from increasing
dyspnea for months was admitted to the Thoracic Surgery Department
of The Specialist District Hospital (Rzeszów, Poland) in December
2004 due to severe dyspnea accompanied by stridor. The patient
reported that she had not experienced fever or weight loss. She had
not suffered from a chronic disease, taken drugs, smoked cigarettes
or abused alcohol.
An irregular tumor mass of 15×21×26 mm within the
trachea at the level of tracheal bifurcation and slightly above and
forward/anterior was visualized by a thoracic computed tomography
(CT) scan. The tumor infiltrated the mediastinum anterior to the
tracheal carina, affecting the area between the opening of the
hemiazygos vein arch into the superior vena cava and aortic arch.
The tumor penetrated into the tracheal lumen just above the
bifurcation, medially narrowing the lumen to a ~9 cm sagittal
diameter. The patient did not present with pathologically enlarged
lymph nodes in the mediastinum or hila of the lungs. A
cauliflower-like tumor arising from the anterior wall and
infiltrating 2–3 cm upward inside the trachea, ~1 cm above its
bifurcation, was visualized with bronchofibroscopy.
To restore tracheal patency, during rigid
bronchoscopy the lesion was partially removed (R2 surgery). This
was followed by a right-sided thoracotomy, during which the segment
of the trachea with the tumor was resected and the paratracheal and
subcarinal lymph nodes were removed.
Histopathological examination revealed ACC of the
trachea. A neoplastic infiltration was present in the surgical
margin. Metastases infiltrating and extending through the capsule
were present in the lymph nodes.
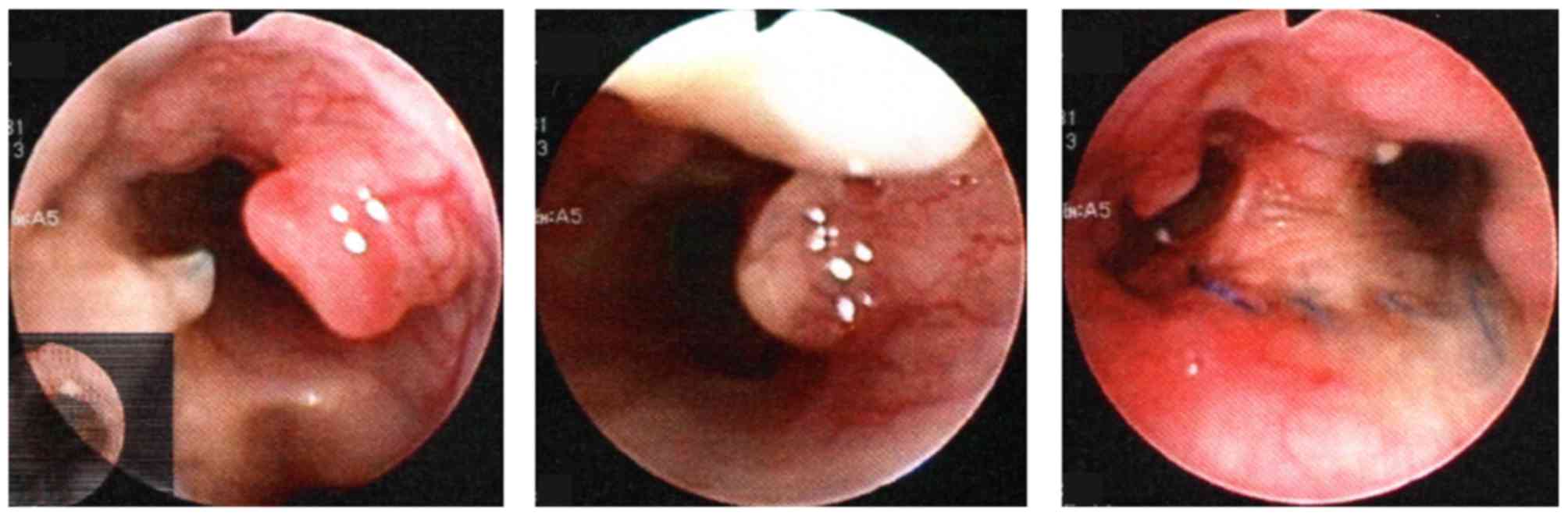
No adjuvant treatment was administered. The patient
remained under close observation and a follow-up bronchofibroscopy
was performed every 6 months. A polypous mucosal thickening,
slightly narrowing the lumen of the bronchus, was visualized at the
anastomosis site, particularly in the opening of the left primary
bronchus, after 8.5 years in July 2013. Specimens were collected by
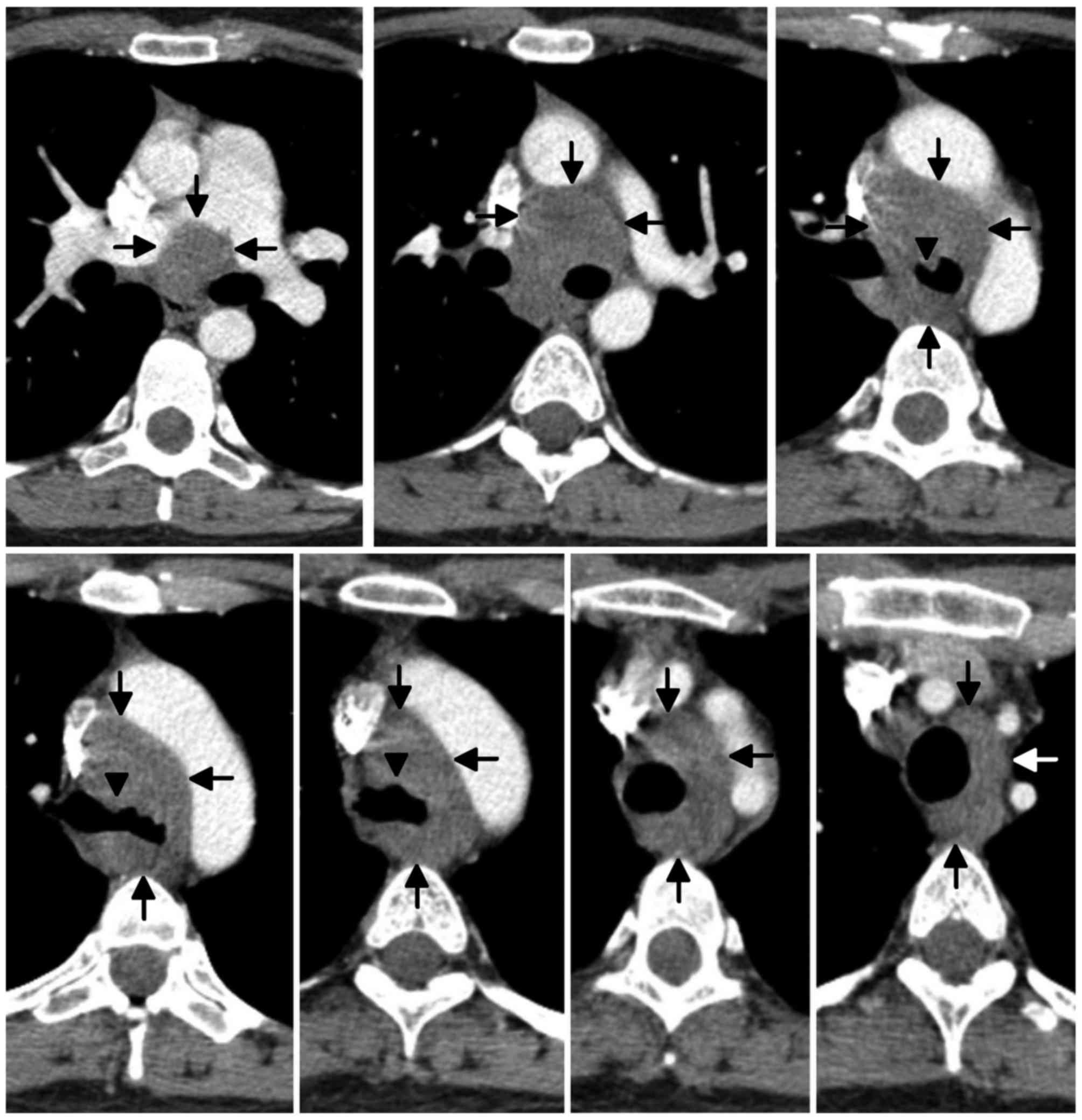
biopsy and a thoracic CT scan was performed. The CT scans revealed
small nodular lesions arising from the wall towards the lumen in
the region of the anastomosis, the lower part of the trachea, below
the anastomosis and in the left primary bronchus, below the
bifurcation. The lower segment of the trachea and short initial
segments of the main bronchi were surrounded by a neoplastic
infiltration between the division of the pulmonary artery and the
site of the aortic arch branches, which exhibited contrast
enhancement (Figs. 1 and 2). A recurrence was confirmed by
histopathological examination. The patient was then admitted to The
Maria Sklodowska Curie Memorial Cancer Centre and Institute of
Oncology (Warsaw, Poland).
Surgical resection was not performed due to the
extent of infiltration. Following assessment, the patient was
recommended radiotherapy. For the purposes of treatment planning,
CT and positron emission tomography (PET)-CT were performed. PET-CT
revealed the presence of small tumors in the lumen of the trachea
and the main bronchi, with an abnormal mass surrounding the trachea
and its bifurcation exhibiting a slightly increased fludeoxyglucose
metabolic rate, characteristic of ACC.
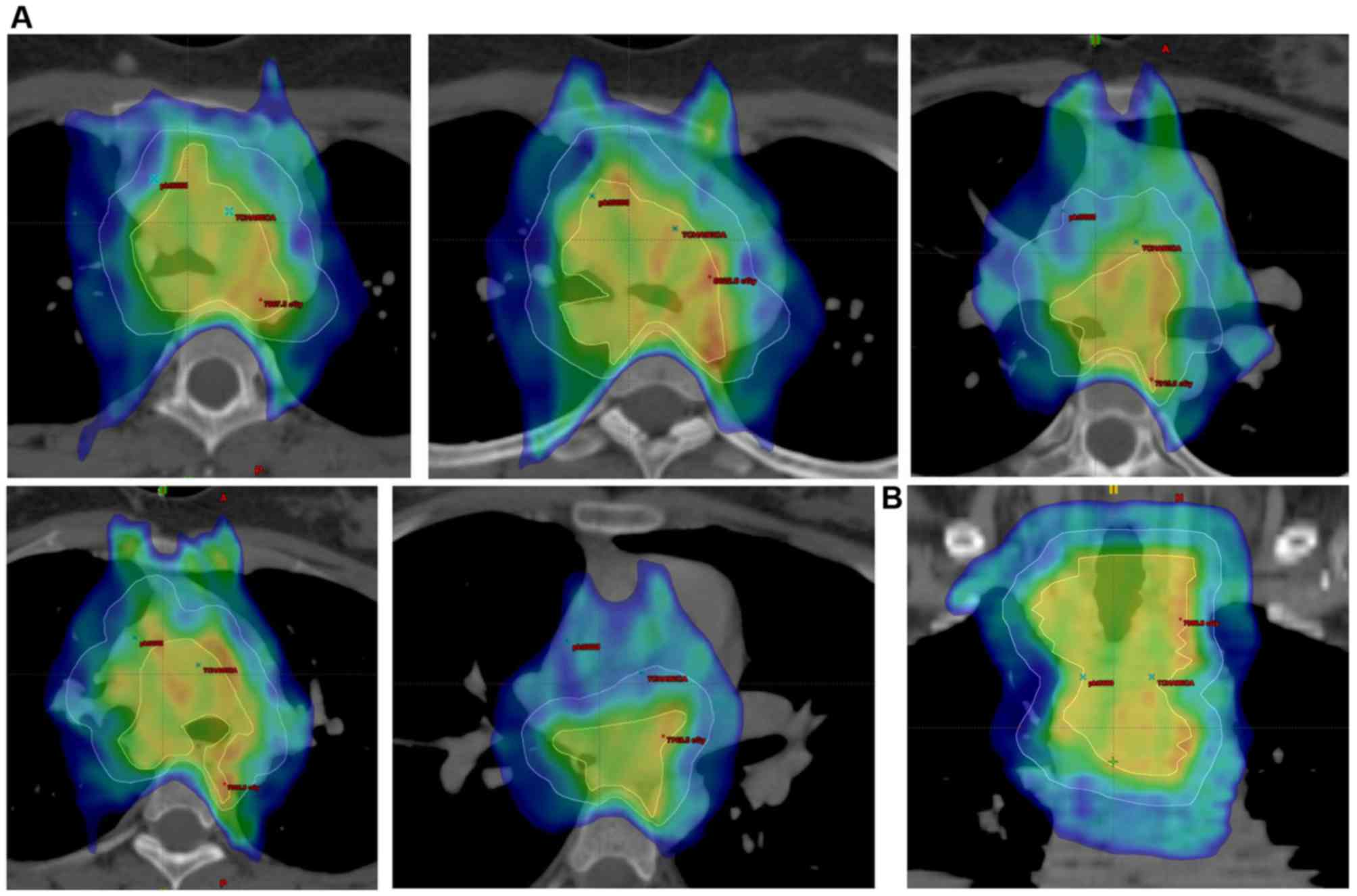
Hyperfractionated radiotherapy (2 fractions a day
with at least a 6-h interval, 10 fractions a week) for 6.5 weeks
was administered to the tumor, including the margin and
mediastinum. The gross tumor volume (GTV) with a 1-cm margin,
including the mediastinal structures, was defined as the clinical
target volume (CTV) area. The total dose of 7,590 cGy in fractions
of 115 cGy was administered to the GTV area and the total dose of
6,600 cGy in fractions of 100 cGy to the CTV area. The biologically
effective dose (for an α/β ratio=10) to the tumor was 84.63 Gy. The
radiotherapy planning was based on a 6 MV nine-field
intensity-modulated radiation therapy (IMRT) technique (Fig. 3). The biological doses administered to
critical organs were 1,326 cGy to the spinal cord and 1,685 cGy to
the heart.
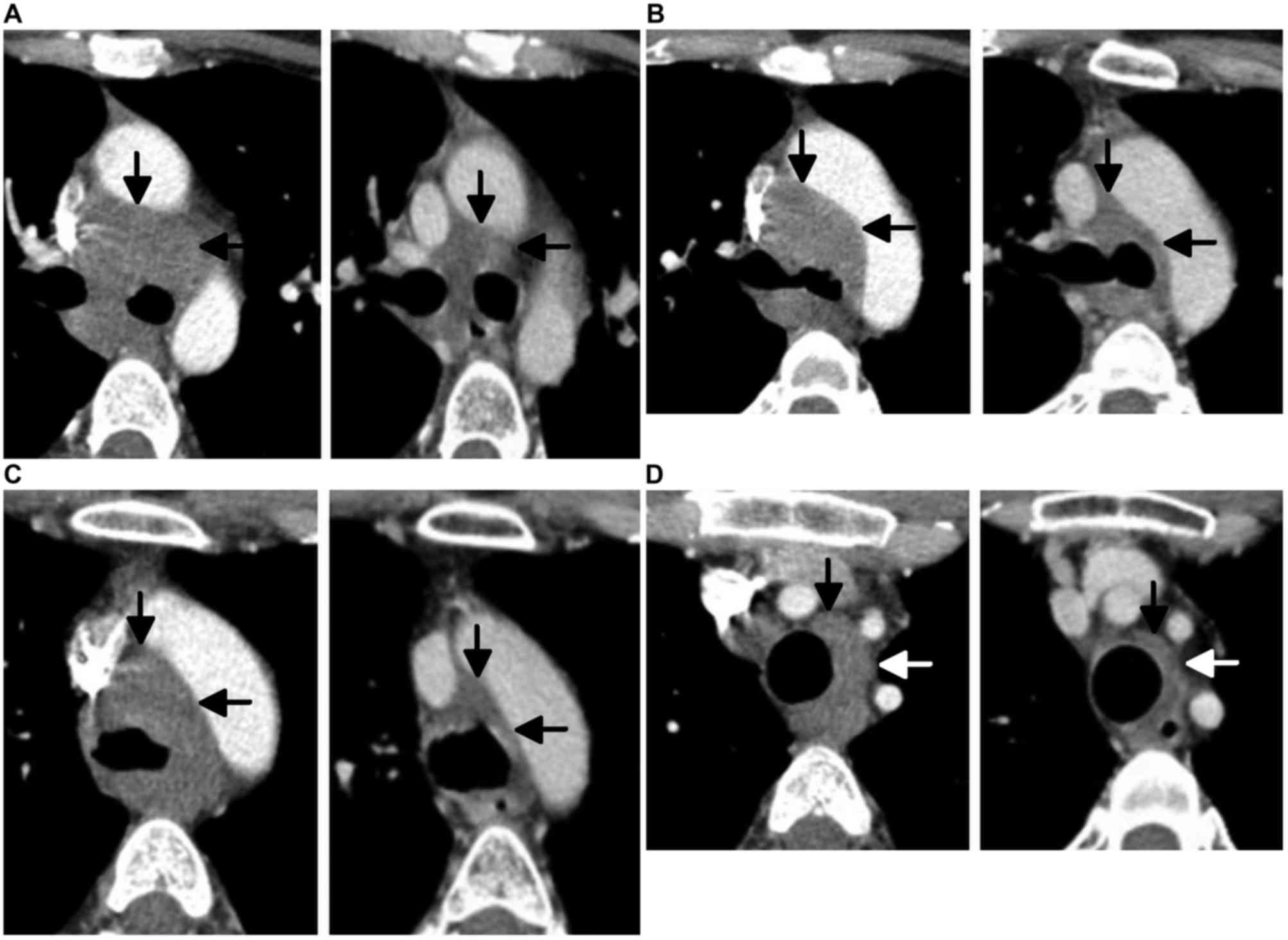
A CT scan following treatment exhibited a
considerable regression of the neoplastic infiltration (Fig. 4). A PET-CT scan revealed no features
of a metabolically active proliferative disease.
The patient remains under close follow-up. Imaging
examinations (CT and PET-CT) are systematically performed every 6
months. The last PET-CT (May 2017), revealed no features of
recurrence.
Discussion
ACC is a relatively rare malignant neoplasm that
derives from glandular tissue. After squamous cell carcinoma, ACC
is the second-most common trachea neoplasm, accounting for 30–40%
of cases, according to data from the literature (3). The estimated incidence is ~1 case per
million people, per year (3). ACC of
the trachea is most commonly located in the distal third of the
trachea in the region of its bifurcation. There is no evidence that
cigarette smoking increases the risk of ACC (3). The incidence of ACC is the same for
males and females, and usually occurs in the 4th or 5th decade of
life (4). However, the case reported
in the present study was diagnosed in a 23-year-old female
patient.
Macroscopically, ACC is a poorly delimited solid
tumor, usually in the form of polypous mucosal thickenings that
decrease the lumen of the trachea. At an advanced stage,
infiltration of the trachea wall and adjacent organs frequently
occurs, exhibiting a tendency for submucosal dissemination and
dissemination along nerves (1,5,6). Long cylindrical structures surrounded by
rectangular cells with hyperchromatic nuclei, characteristic of
ACC, are visible under a microscope (1). These tumors metastasize into mediastinal
lymph nodes and may metastasize to distant sites, most frequently
into the lungs (7).
Analysis performed by Gaissert et al
(8) demonstrated that the neoplasm
infiltrated the tissues surrounding the trachea in 60% of all
patients receiving surgery with ACC of the trachea, and adjacent
organs, primarily the esophagus, in a further 15%. Almost 60% were
non-radical surgeries. Metastases into the lymph nodes were present
in only 13% of patients undergoing surgical resection. This
indicates the tendency for neoplasms to infiltrate into and along
the tracheal mucosa, which predominates over metastasis into the
lymph nodes (8).
The predominant symptoms of tracheal neoplasms
result from the obturation of the tracheal lumen caused by the
tumor. Dyspnea, increasing over recent months and later accompanied
by stridor, is most often encountered. Other symptoms include
whistling sounds, from the lower part of the bronchial tree, cough,
chest pains and hemoptysis (4,9). The mean
time between the appearance of disease symptoms and the
establishment of a diagnosis is long: 18.3 months in patients with
neoplasms that can be resected and 23.7 months in patients with
inoperable neoplasms (8). Patients
are often treated for asthma for a substantial period of time prior
to the establishment of an appropriate diagnosis (7). In the present case, the female patient
presented with gradually increasing dyspnea and stridor, symptoms
indicating upper airway obstruction. The peak expiratory flow index
is reduced in patients with an obturation of the trachea, with a
flat flow-volume curve (3).
Bronchoscopy and thoracic CTs are typically used to
diagnose tracheal neoplasms. Abronchoscopic examination allows for
the macroscopic assessment of local neoplasm progression and allows
histological verification of the neoplasm. CT scans allow for the
visualization of infiltration extent and metastases into the lymph
nodes. On the basis of this examination, it is possible to create a
virtual bronchoscopy. Chest X-rays are ineffective in the
examination of tracheal neoplasms (1). Symptomatic management aims to restore
tracheal patency during a rigid bronchoscopy. Such a procedure was
performed in the present case.
Resection of the trachea and the tumor with
end-to-end anastomosis or artificial trachea implantation at the
defect site is the primary method of radical treatment. In cases
where it is not possible to complete surgical resection,
radiotherapy is administered to patients. ACC exhibits low
radiation sensitivity and therefore the highest possible dose
should be administered, taking the tolerance doses of adjacent
organs (including the trachea, esophagus, spinal cord, lungs and
heart) into account. A dose of 70 Gy in fractions of 2 Gy
administered once a day 5 days per week is indicated. Radiotherapy
should be planned on the basis of conformal techniques, preferably
with the use of IMRT (10). A
previous study has proposed the possibility of combining
teleradiotherapy with brachytherapy, boosting the radiotherapeutic
dose to macroscopic disease areas and therefore limiting
undesirable effects in adjacent critical tissues and organs
(10,11). Radiotherapy is shifting towards the
use of proton therapies (12). The
greater potential for sparing critical organs allows for an
increase in the maximal doses of radiation. There is published
study that presents the administration of doses of 80 Gy in
fractions of 2 Gy without alterations to the tolerated doses for
critical organs (12).
That the area at risk of microscopic disease has a
tendency for submucosal infiltration and infiltration around nerves
should be taken into account. Treating the upward and downward
margins from neoplastic infiltration is recommended (7,10).
The role of postoperative radiotherapy is not clear.
This procedure causes a decrease in local recurrence frequency;
however, an increase in survival time has not previously been
demonstrated. Metastasis into lymph nodes and a non-radical
surgical procedure are obligatory indications for the use of
postoperative radiotherapy (3,13). A dose
for the treatment of the microscopic disease should be at least 60
Gy in fractions of 2 Gy administered five times a week (3,11). A
higher dose should be given to residual disease areas and to
surgical sites following non-radical surgery (10). Postoperative radiotherapy planning
should be conducted on the basis of CTs performed prior to the
surgical procedure. Analysis performed by Chen et al
(13) indicates that there is an
improvement in disease-free and overall survival rates in patients
who received postoperative radiotherapy following a non-radical
procedure (13).
Chemotherapy is ineffective in the treatment of ACC
of the trachea: Attempts to use chemotherapy in combination with
radiotherapy or as palliative treatment have demonstrated no
benefit (13).
The largest retrospective analysis of cases of ACC
of the trachea was conducted at the Department of Thoracic Surgery
of Massachusetts General Hospital (Boston, MA, USA), including 135
patients from 1962–2002 (8). A total
of 75% of patients underwent surgical resection. It was decided
that surgery would not be performed in the remaining patients
following assessment, due to the local progression of the disease.
The authors emphasized that the increasing experience and novel
technical possibilities in procedures, primarily restorative
techniques, enabled surgery to be completed in patients with
increasingly advanced neoplastic processes. Postoperative
radiotherapy was performed for 70% of the patients that received
surgery. The mean survival time was 69 months for patients that
received surgery, and 41 months for patients that did not. The
5-year survival rate was 54% in patients that received surgery and
33% in patients that did not; the 10-year survival rates were 33
and 9%, respectively (8).
Another analysis of the SEER medical database
covered 94 cases of tracheal neoplasms from 1973 to 2004 (4). The data demonstrated that the 5-year
overall survival rate of patients with ACC of the trachea was
74.3%, whereas if this disease was diagnosed at a locoregionally
advanced stage, the survival rate increased to 90% (4).
Data from the literature indicate a significant
improvement of treatment outcomes following the use of surgical
resection with adjuvant radiotherapy (13). In the described case, non-radical
macroscopic surgery with subsequent close observation was not an
optimal procedure. According to the present study, irradiation of
late recurrences following prior R2 resection may enable a
locoregional control to be achieved; however, the patient prognosis
remains uncertain.
The aim of the present study was to indicate an
atypical case following the first treatment in the local hospital,
which contrasts with the regular practice in the Maria
Skłodowska-Curie Memorial Cancer Center and Institute of Oncology.
In this case the multidisciplinary team in an institution that
offers the complete range of oncological treatment would make the
therapeutic decisions.
References
|
1
|
Kwak SH, Lee KS, Chung MJ, Jeong YJ, Kim
GY and Kwon OJ: Adenoid cystic carcinoma of the airways: Helical CT
and histopathological correlation. AJR Am J Roentgenol.
183:277–281. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wojciechowska U, Olasek P, Czauderna K and
Didkowska J: Nowotwory złośliwe w polsce w 2014 roku. Cancer in
Poland in 2014Polish National Cancer Registry, Department of
Epidemiology and Cancer Prevention. Warszawa: pp. 48–50. 2016, (In
Poland).
|
|
3
|
Honings J, Gaissert HA, van der Heijden
HF, Verhagen AF, Kaanders JH and Marres HA: Clinical aspects and
treatment of primary tracheal malignancies. Acta Otolaryngol.
130:763–772. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Urdaneta AI, Yu JB and Wilson LD:
Population based cancer registry analysis of primary tracheal
carcinoma. Am J Clin Oncol. 34:32–37. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Choudhury BK, Barman G, Singh S and Ahmed
K: Adenoid cystic carcinoma of the upper trachea: A rare neoplasm.
J Clin Imaging Sci. 3:392013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vigg A, Mantri S and Vigg A and Vigg A:
Adenoid cystic carcinoma of trachea. Indian J Chest Dis Allied Sci.
46:287–289. 2004.PubMed/NCBI
|
|
7
|
El Marjany M, Arsalane A, Sifat H,
Andaloussi K, Oukabli M, Hadadi K, Kabiri el H and Mansouri H:
Primary adenoid cystic carcinoma of the trachea: A report of two
cases and literature review. Pan Afr Med J. 19:322014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gaissert HA, Grillo HC, Shadmehr MB,
Wright CD, Gokhale M, Wain JC and Mathisen DJ: Long-term survival
after resection of primary adenoid cystic and squamous cell
carcinoma of the trachea and carina. Ann Thorac Surg. 78:1889–1896.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang PY, Liu MS, Chen CH, Lin CM and Tsao
TC: Adenoid cystic carcinoma of the trachea: A report of seven
cases and literature review. Chang Gung Med J. 28:357–363.
2005.PubMed/NCBI
|
|
10
|
Choi NC: Radiation therapy in the
management of tracheal cancerSurgery of the trachea and bronchi.
Grillo HC: BC Decker; Hamilton, London: pp. 791–802. 2004
|
|
11
|
Haresh KP, Prabhakar R, Rath GK, Sharma
DN, Julka PK and Subramani V: Adenoid cystic carcinoma of the
trachea treated with PET-CT based intensity modulated radiotherapy.
J Thorac Oncol. 3:793–795. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Millar Bonner LP, Stripp D, Cooper JD,
Both S, James P and Rengan R: Definitive radiotherapy for
unresected adenoid cystic carcinoma of the trachea. Chest.
141:1323–1326. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen F, Huang M, Xu Y, Li T, Xie K, Zhang
L, Cheng D, Liu L, Che G, Hou M, et al: Primary tracheal adenoid
cystic carcinoma: Adjuvant treatment outcome. Int J Clin Oncol.
20:686–692. 2015. View Article : Google Scholar : PubMed/NCBI
|