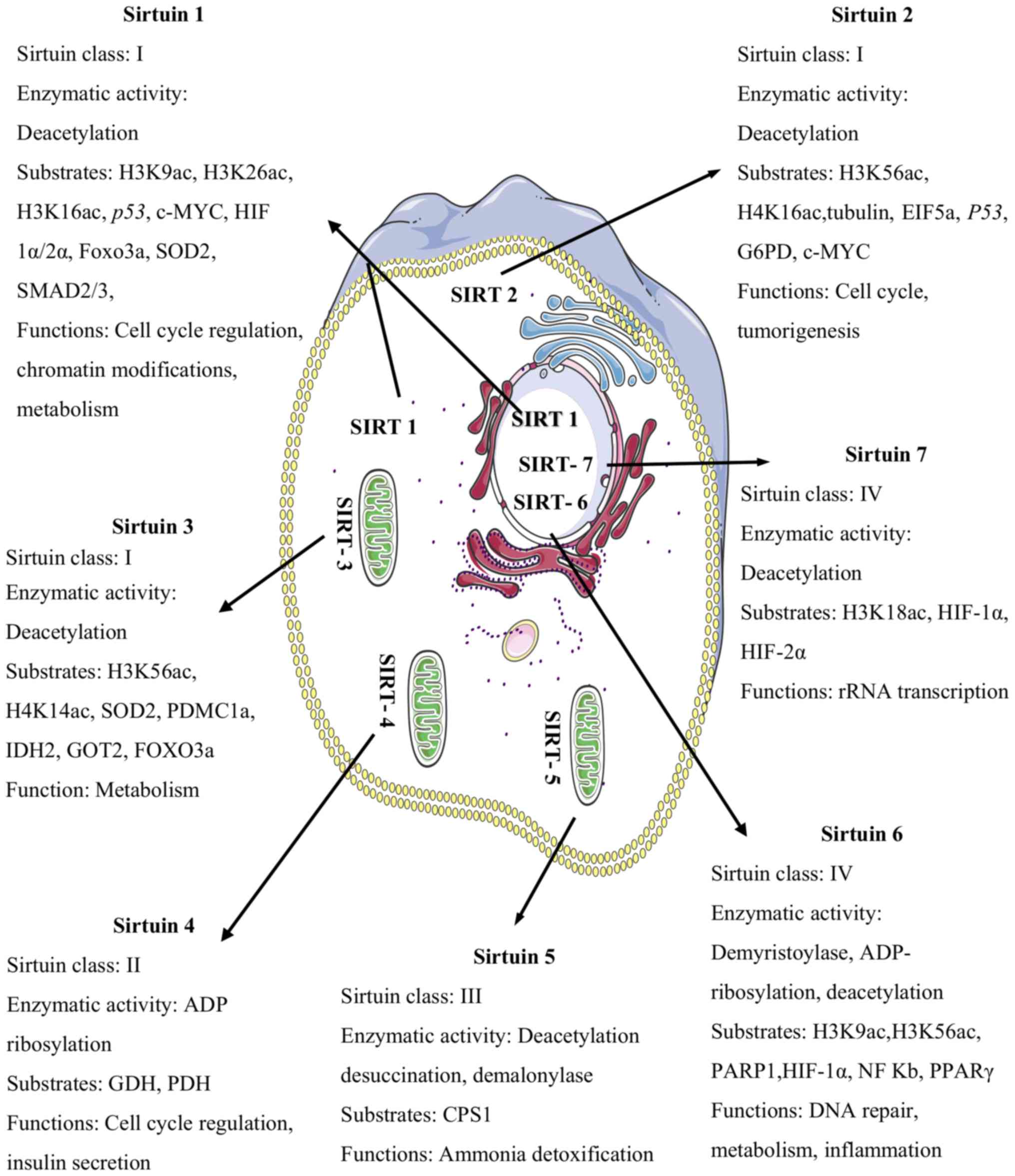
The sirtuin family proteins (SIRT) are class III
histone deacetylases (HDACs) comprised of seven members (SIRT1-7).
Sirtuin proteins are widely expressed in normal tissues and
reported to be involved in several biological processes (1–4) (Fig. 1). SIRT1 was the first family member to
be discovered and is still the most studied. Its biological role in
cancer has been studied extensively, yet there are conflicting
results regarding the association between the two as SIRT1 is known
to suppress or promote cancer depending on its cellular content or
type (2–4). The expression level of SIRT1 has been
shown to play an important role in the pathogenesis of oral cancer
(5–8),
the sixth most frequent cancer worldwide, with oral squamous cell
carcinoma (OSCC) being, by far, the commonest single entity,
accounting for about 90% of all malignancies in the oral cavity and
posing a major public health problem in many Asian countries
(9). The etiologies of oral cancer
include betel quid chewing, smoking, alcohol consumption, genetic
predisposition, and viruses, including human papillomavirus (HPV)
(9,10). The overall 5-year survival rates for
patients with OSCC (ranging from 34 to 62.9%) have not
significantly improved for decades in spite of advances in the
field of oncology. These findings underscore the importance of
encouraging new areas of research on factors that modify oral
cancer and therapeutic targets to treat it. The purpose of this
review is to summarize the findings of recent publications on SIRT1
with regard to oral cancer and to discuss its importance as a
possible therapeutic agent. To the best of our knowledge, this is
the first review evaluating the biological role of SIRT1 in the
modulation of oral cancer.
SIRT1 plays a key role in epigenetic regulation of
gene expression by changing the structure of chromatin. It has been
reported to deacetylate both histone and non-histone proteins.
Deacetylation of histones by SIRT1 has been shown to induce
chromatin condensation, whereas acetylation by histone
acetyltransferases (HATs) causes chromatin decondensation. This
balance is crucial for normal cellular functions, and any
disturbance of it will be related to cancer (24). SIRT1-mediated deacetylation of
non-histone proteins has been suggested to be more important in
cancer than histones (24,25). In tumour biology, SIRT1 seems to play
contradictory roles and deregulation of SIRT1 expression has
frequently been reported in many human malignancies (4,26–38) (Table
II).
As opposed to what occurs during cellular oxidative
stress, SIRT1 has been shown to induce mitochondrial translocation
of p53, leading to enhanced p53-independent
mitochondrial apoptosis (22). The
DNA repair mechanisms and genomic stability functions of SIRT1
imply a protective effect against cancer (reviewed in 2–4).
Therefore, the question arises as to whether SIRT1 acts primarily
as an oncogene or a tumour suppressor. It is, however, strongly
evident that SIRT1 is a critical regulator in the pathogenesis of
tumours. To clarify the contradictory roles of SIRT1 in
tumorigenesis, further studies are necessary.
The regulatory role of SIRT1 in oral cancer is
vigorously debated owing to the belief that it can have both
tumorigenic and non-tumorigenic roles (5–8) (Table III). Altered levels of SIRT1
expression have a significant impact on the pathophysiology of oral
cancer. Downregulation of SIRT1 expression is correlated with the
metastatic phenotype, whereas upregulation of this protein results
in opposite effects (5–8). It has been reported that stable
expression of SIRT1 aids in maintaining epithelial integrity by
inducing the expression of epithelial-cadherin (E-cadherin), and
this contributes to the prevention of both invasion and metastasis
in oral cancer (5–7). Conflicting data have also been reported
for prostate carcinoma. It has been reported that SIRT1 mediates
deacetylation of histone H3, causing transcriptional repression of
E-cadherin and leading to invasion and metastasis (41). However, SIRT1 has been demonstrated to
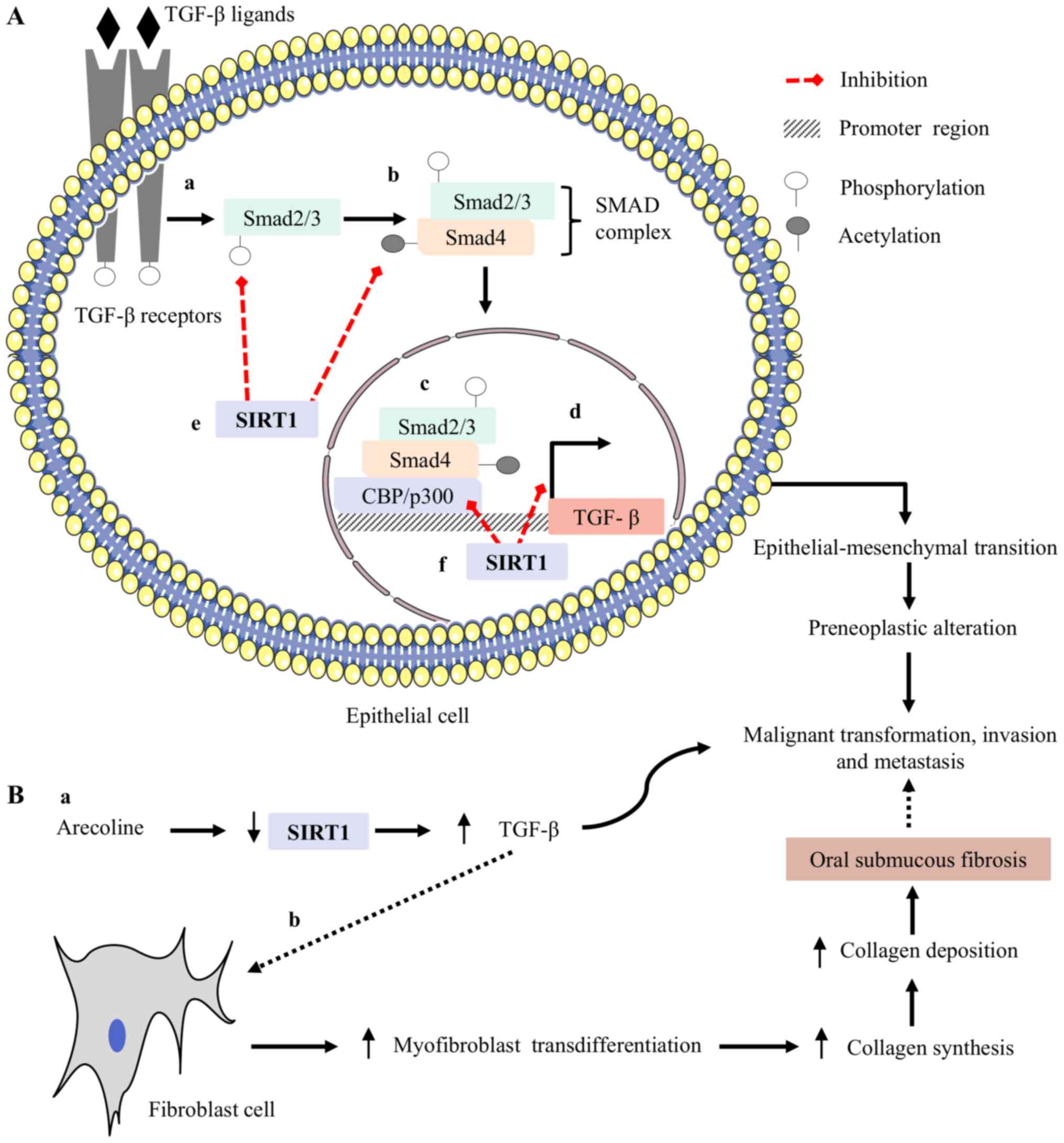
inhibit transforming growth factor-beta (TGF-β)-mediated malignant
transformation, invasion and metastasis in oral cancer (5). TGF-β is a growth factor and its
overexpression has been frequently reported to be involved in
precancerous oral lesions, leading to oral cancer (42,43).
Increased expression of TGF-β has been shown to enhance malignant
transformation, invasion and metastasis in oral epithelial cells by
inducing its downstream targets (5–6,43). Similarly, overexpressed TGF-β acts on
fibroblasts and has been reported to increase myofibroblastic
transdifferentiation (42,43). Myofibroblasts are the major source for
collagen synthesis in the extracellular matrix (ECM) of connective
tissues, and continuous increases in the deposition of collagen
lead to the pathogenesis of oral submucous fibrosis (OSF), a
precancerous condition (42,43) (Fig. 2).
The malignant transformation rate in patients with OSF ranges from
7–13% (10). SIRT1 has been shown to
induce transcriptional suppression of TGF-β-mediated downstream
targets in fibroblasts and to prevent malignant transformation
(44). Based on these observations,
SIRT1 may have the ability to prevent malignant transformation,
invasion, and metastasis.
Recently, our group evaluated a significant
association between arecoline and the expression of SIRT1 in oral
epithelial cells. Arecoline, the major alkaloid in betel quid, has
been reported to be involved in the pathogenesis of oral cancer by
facilitating the cellular transformation and transcriptional
repression of tumour suppressor genes (TSGs) (10,45,46). We
discovered that arecoline significantly induced DNA
hypermethylation, followed by downregulation of SIRT1 expression in
oral epithelial cells. The frequency of DNA hypermethylation was
found to be associated with precancerous oral lesions (data not
shown). Our data suggest that arecoline-mediated downregulation of
SIRT1 expression may be involved in the initial stage of
transformation of normal cells to oral cancer and the development
of precancerous oral lesions induced by betel quid chewing. Our
results fit well with the observation of an association of SIRT1
and TGF-β, wherein arecoline-mediated downregulation of SIRT1
expression in oral epithelial cells fails to prevent TGF-β-induced
malignant transformation in the oral mucosa of betel quid chewers.
Taken together, these results suggest that SIRT1 could serve as a
tumour suppressor in oral cancer. However, it remains unclear how
it directly affects this process.
Conversely, despite evidence of the
tumour-suppressing effects of SIRT1, some studies have demonstrated
the promoting effects of this protein (8). Upregulation of annexin A4 has been shown
to promote the progression and chemoresistance of numerous tumours
(47). Overexpression of SIRT1 has
been reported to induce cisplatin resistance in oral cancer by
elevating the level of annexin A4 (8), and chemical inhibitors of SIRT1
significantly abolish this action (8). Hypoxia within the tumour
microenvironment has a well-documented role to promote
tumorigenesis. Recent reports investigating the role of SIRT1 under
hypoxia have demonstrated that it promotes tumorigenesis via
incorporation with hypoxia-inducible factor-1 alpha (HIF-1α)
(48). Based on these findings, SIRT1
might have a significant tumour-inducing effect. Thus, further
studies are needed to clarify this issue and evaluate new
therapeutic approaches.
Activators and inhibitors of HDACs have been
developed in recent years and, to date, three histone deacetylase
inhibitors (HDACis) have received United States Food and Drug
Administration approval for therapeutic use (49–63)
(Table IV).
The use of HDACis in combination with conventional
chemotherapeutic agents has already been reported to be a promising
strategy against oral cancer (64–71)
(Table V). The class III HDAC SIRT1
is considered to be both a promoter and suppressor. Inhibitors of
SIRT1 have attracted interest and been found to induce apoptosis in
various cancer cell lines. Similarly, activators of SIRT1 have been
shown to possess the ability to prevent numerous cancers, including
leukaemia, skin cancer, prostate cancer and multiple myeloma
(25,34,62,63,72).
Therefore, the conflicting data reported in the literature support
the use of both activators and inhibitors of SIRT1 as strategies
for cancer therapy; hence, care needs to be taken regarding the
cytotoxicity and the dose of this protein when it is administered
as a therapeutic agent.
In spite of being involved in various physiological
and pathological processes, the effects of altered SIRT1 expression
in oral cancer are inconsistent. Reactive oxygen species (ROSs) are
the strongest risk factor associated with the pathogenesis of oral
cancer (10). Habits such as betel
quid chewing have been reported to induce generation of ROSs in the
oral epithelium and lead to genetic instability by damaging DNA and
other macromolecules (10,45). SIRT1 has been shown to increase the
synthesis of antioxidant enzymes such as glutathione and superoxide
dismutase 2 and prevent ROS-mediated genomic alterations (73). Consistent with this premise, it is
hypothesized that SIRT1 may play a significant role in inhibiting
the synthesis of ROSs and prevent DNA and macromolecule damage in
the oral mucosa of betel quid chewers. Further studies are thus
warranted to evaluate the regulatory mechanism of SIRT1 in ROS
generation in oral epithelial cells. Moreover, as demonstrated in
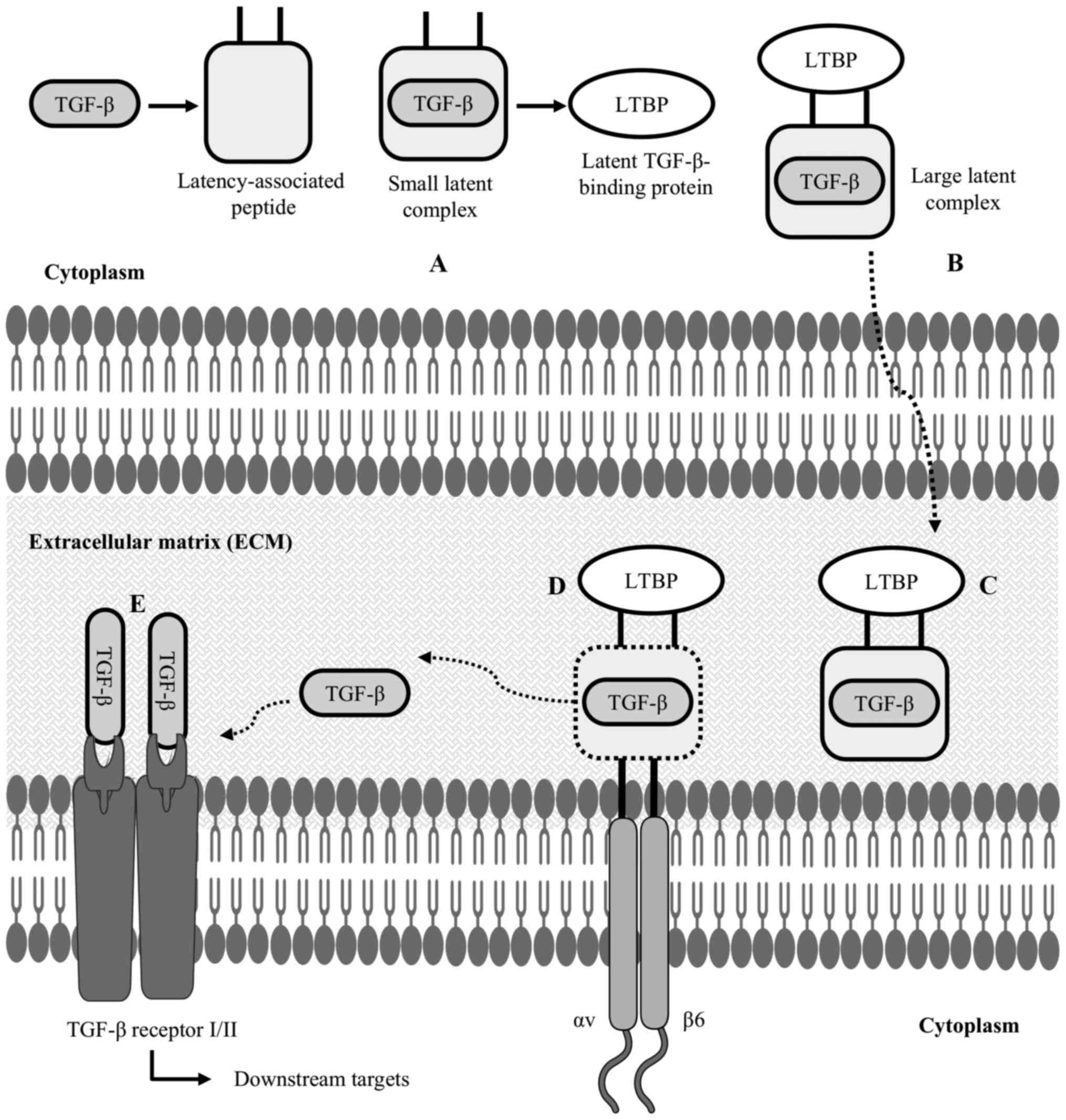
some of the studies cited above, SIRT1 may prevent TGF-β-mediated
invasion and metastasis in oral cancer (5,42,43). TGF-β is a growth factor and remains
hidden in its inactive state in the ECM (74). αvβ6 integrin has been shown
to facilitate the activation of the TGF-β downstream pathway by
allowing it to bind with its receptors (74) (Fig.
3).
Based on results of the studies referred to above
and our current data, it is hypothesized that SIRT1 may play a
significant tumour-suppressive role in oral cancer. Future studies
will undoubtedly pinpoint the molecular mechanisms via which SIRT1
influences oral carcinogenesis and identify efficacious SIRT1
activators for the prevention or treatment of precancerous oral
lesions that can lead to oral cancer.
Not applicable.
No funding was received.
The datasets generated and/or analyzed during the
present study are not publicly available due to the data containing
information that may compromise the consent of the participants but
are available from the corresponding author on reasonable
request.
SI and YA conducted the literature review and wrote
the manuscript. OU and IC contributed to the study design and the
writing of the manuscript, and made corrections. All authors have
read and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Carafa V, Rotili D, Forgione M, Cuomo F,
Serretiello E, Hailu GS, Jarho E, Lahtela-Kakkonen M, Mai A and
Altucci L: Sirtuin functions and modulation: From chemistry to the
clinic. Clin Epigenetics. 8:612016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Deng CX: SIRT1, is it a tumor promoter or
tumor suppressor? Int J Biol Sci. 5:147–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bosch-Presegué L and Vaquero A: The dual
role of sirtuins in cancer. Genes Cancer. 2:648–662. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang RH, Sengupta K, Li C, Kim HS, Cao L,
Xiao C, Kim S, Xu X, Zheng Y, Chilton B, et al: Impaired DNA damage
response, genome instability, and tumorigenesis in SIRT1 mutant
mice. Cancer Cell. 14:312–323. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen IC, Chiang WF, Huang HH, Chen PF,
Shen YY and Chiang HC: Role of SIRT1 in regulation of
epithelial-to-mesenchymal transition in oral squamous cell
carcinoma metastasis. Mol Cancer. 13:2542014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kang YY, Sun FL, Zhang Y and Wang Z: SIRT1
acts as a potential tumor suppressor in oral squamous cell
carcinoma. J Chin Med Assoc. 81:416–422. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Murofushi T, Tsuda H, Mikami Y, Yamaguchi
Y and Suzuki N: CAY10591, a SIRT1 activator, suppresses cell
growth, invasion, and migration in gingival epithelial carcinoma
cells. J Oral Sci. 59:415–423. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xiong P, Li YX, Tang YT and Chen HG:
Proteomic analyses of Sirt1-mediated cisplatin resistance in OSCC
cell line. Protein J. 30:499–508. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Warnakulasuriya S: Global epidemiology of
oral and oropharyngeal cancer. Oral Oncol. 45:309–316. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
IARC Working Group on the Evaluation of
Carcinogenic Risks to Humans: Betel-quid and areca-nut chewing and
some areca-nut-derived nitrosamines. IARC Monogr Eval Carcinog
Risks Hum. 85:1–334. 2004.PubMed/NCBI
|
|
11
|
Peters AH, O'Carroll D, Scherthan H,
Mechtler K, Sauer S, Schöfer C, Weipoltshammer K, Pagani M, Lachner
M, Kohlmaier A, et al: Loss of the Suv39h histone
methyltransferases impairs mammalian heterochromatin and genome
stability. Cell. 107:323–337. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vaquero A, Scher M, Lee D,
Erdjument-Bromage H, Tempst P and Reinberg D: Human SirT1 interacts
with histone H1 and promotes formation of facultative
heterochromatin. Mol Cell. 16:93–105. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vaquero A, Scher M, Erdjument-Bromage H,
Tempst P, Serrano L and Reinberg D: SIRT1 regulates the histone
methyl-transferase SUV39H1 during heterochromatin formation.
Nature. 450:440–444. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Palacios JA, Herranz D, De Bonis ML,
Velasco S, Serrano M and Blasco MA: SIRT1 contributes to telomere
maintenance and augments global homologous recombination. J Cell
Biol. 191:1299–1313. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yuan Z, Zhang X, Sengupta N, Lane WS and
Seto E: SIRT1 regulates the function of the Nijmegen breakage
syndrome protein. Mol Cell. 27:149–162. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jeong J, Juhn K, Lee H, Kim SH, Min BH,
Lee KM, Cho MH, Park GH and Lee KH: SIRT1 promotes DNA repair
activity and deacetylation of Ku70. Exp Mol Med. 39:8–13. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sawada M, Sun W, Hayes P, Leskov K,
Boothman DA and Matsuyama S: Ku70 suppresses the apoptotic
translocation of Bax to mitochondria. Nat Cell Biol. 5:320–329.
2003. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brunet A, Sweeney LB, Sturgill JF, Chua
KF, Greer PL, Lin Y, Tran H, Ross SE, Mostoslavsky R, Cohen HY, et
al: Stress-dependent regulation of FOXO transcription factors by
the SIRT1 deacetylase. Science. 303:2011–2015. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kobayashi Y, Furukawa-Hibi Y, Chen C,
Horio Y, Isobe K, Ikeda K and Motoyama N: SIRT1 is a critical
regulator of FOXO-mediated transcription in response to oxidative
stress. Int J Mol Med. 16:237–243. 2005.PubMed/NCBI
|
|
20
|
Motta MC, Divecha N, Lemieux M, Kamel C,
Chen D, Gu W, Bultsma Y, McBurney M and Guarente L: Mammalian SIRT1
represses forkhead transcription factors. Cell. 116:551–563. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chua KF, Mostoslavsky R, Lombard DB, Pang
WW, Saito S, Franco S, Kaushal D, Cheng HL, Fischer MR, Stokes N,
et al: Mammalian SIRT1 limits replicative life span in response to
chronic genotoxic stress. Cell Metab. 2:67–76. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yi J and Luo J: SIRT1 and p53, effect on
cancer, senescence and beyond. Biochim Biophys Acta.
1804:1684–1689. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Peng L, Yuan Z, Ling H, Fukasawa K,
Robertson K, Olashaw N, Koomen J, Chen J, Lane WS and Seto E: SIRT1
deacetylates the DNA methyltransferase 1 (DNMT1) protein and alters
its activities. Mol Cell Biol. 31:4720–4734. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Glozak MA, Sengupta N, Zhang X and Seto E:
Acetylation and deacetylation of non-histone proteins. Gene.
363:15–23. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Glozak MA and Seto E: Histone deacetylases
and cancer. Oncogene. 26:5420–5432. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Huffman DM, Grizzle WE, Bamman MM, Kim JS,
Eltoum IA, Elgavish A and Nagy TR: SIRT1 is significantly elevated
in mouse and human prostate cancer. Cancer Res. 67:6612–6618. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen HC, Jeng YM, Yuan RH, Hsu HC and Chen
YL: SIRT1 promotes tumorigenesis and resistance to chemotherapy in
hepatocellular carcinoma and its expression predicts poor
prognosis. Ann Surg Oncol. 19:2011–2019. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hao C, Zhu PX, Yang X, Han ZP, Jiang JH,
Zong C, Zhang XG, Liu WT, Zhao QD, Fan TT, et al: Overexpression of
SIRT1 promotes metastasis through an epithelial-mesenchymal
transition in hepatocellular carcinoma. BMC Cancer. 14:9782014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen X, Sun K, Jiao S, Cai N, Zhao X, Zou
H, Xie Y, Wang Z, Zhong M and Wei L: High levels of SIRT1
expression enhance tumorigenesis and associate with a poor
prognosis of colorectal carcinoma patients. Sci Rep. 4:74812014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhao G, Qin Q, Zhang J, Liu Y, Deng S, Liu
L, Wang B, Tian K and Wang C: Hypermethylation of HIC1 promoter and
aberrant expression of HIC1/SIRT1 might contribute to the
carcinogenesis of pancreatic cancer. Ann Surg Oncol. 20 Suppl
3:S301–S311. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Stunkel W, Peh BK, Tan YC, Nayagam VM,
Wang X, Salto-Tellez M, Ni B, Entzeroth M and Wood J: Function of
the SIRT1 protein deacetylase in cancer. Biotechnol J. 2:1360–1368.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ford J, Jiang M and Milner J:
Cancer-specific functions of SIRT1 enable human epithelial cancer
cell growth and survival. Cancer Res. 65:10457–10463. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
He Z, Yi J, Jin L, Pan B, Chen L and Song
H: Overexpression of Sirtuin-1 is associated with poor clinical
outcome in esophageal squamous cell carcinoma. Tumour Biol.
37:7139–7148. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hida Y, Kubo Y, Murao K and Arase S:
Strong expression of a longevity-related protein, SIRT1, in Bowen's
disease. Arch Dermatol Res. 299:103–106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bradbury CA, Khanim FL, Hayden R, Bunce
CM, White DA, Drayson MT, Craddock C and Turner BM: Histone
deacetylases in acute myeloid leukaemia show a distinctive pattern
of expression that changes selectively in response to deacetylase
inhibitors. Leukemia. 19:1751–1759. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jung W, Hong KD, Jung WY, Lee E, Shin BK,
Kim HK, Kim A and Kim BH: SIRT1 expression is associated with good
prognosis in colorectal cancer. Korean J Pathol. 47:332–339. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Jang SH, Min KW, Paik SS and Jang KS: Loss
of SIRT1 histone deacetylase expression associates with tumour
progression in colorectal adenocarcinoma. J Clin Pathol.
65:735–739. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Firestein R, Blander G, Michan S,
Oberdoerffer P, Ogino S, Campbell J, Bhimavarapu A, Luikenhuis S,
de Cabo R, Fuchs C, et al: The SIRT1 deacetylase suppresses
intestinal tumorigenesis and colon cancer growth. PLoS One.
3:e20202008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Voelter-Mahlknecht S and Mahlknecht U: The
sirtuins in the pathogenesis of cancer. Clin Epigenetics. 1:71–83.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Potente M, Ghaeni L, Baldessari D,
Mostoslavsky R, Rossig L, Dequiedt F, Haendeler J, Mione M, Dejana
E, Alt FW, et al: SIRT1 controls endothelial angiogenic functions
during vascular growth. Genes Dev. 21:2644–2658. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Byles V, Zhu L, Lovaas JD, Chmilewski LK,
Wang J, Faller DV and Dai Y: SIRT1 induces EMT by cooperating with
EMT transcription factors and enhances prostate cancer cell
migration and metastasis. Oncogene. 31:4619–4629. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Verrecchia F and Mauviel A: Transforming
growth factor-beta and fibrosis. World J Gastroenterol.
13:3056–3062. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ekanayaka RP and Tilakaratne WM: Oral
submucous fibrosis: Review on mechanisms of malignant
transformation. Oral Surg Oral Med Oral Pathol Oral Radiol.
122:192–199. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Chang YC, Lin CW, Yu CC, Wang BY, Huang
YH, Hsieh YC, Kuo YL and Chang WW: Resveratrol suppresses
myofibroblast activity of human buccal mucosal fibroblasts through
the epigenetic inhibition of ZEB1 expression. Oncotarget.
7:12137–12149. 2016.PubMed/NCBI
|
|
45
|
Uehara O, Takimoto K, Morikawa T, Harada
F, Takai R, Adhikari BR, Itatsu R, Nakamura T, Yoshida K, Matsuoka
H, et al: Upregulated expression of MMP-9 in gingival epithelial
cells induced by prolonged stimulation with arecoline. Oncol Lett.
14:1186–1192. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chiba I, Muthumala M, Yamazaki Y, Uz Zaman
A, Iizuka T, Amemiya A, Shibata T, Kashiwazaki H, Sugiura C and
Fukuda H: Characteristics of mutations in the p53 gene of oral
squamous-cell carcinomas associated with betel-quid chewing in Sri
Lanka. Int J Cancer. 77:839–842. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wei B, Guo C, Liu S and Sun MZ: Annexin A4
and cancer. Clin Chim Acta. 447:72–78. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Laemmle A, Lechleiter A, Roh V, Schwarz C,
Portmann S, Furer C, Keogh A, Tschan MP, Candinas D, Vorburger SA
and Stroka D: Inhibition of SIRT1 impairs the accumulation and
transcriptional activity of HIF-1α protein under hypoxic
conditions. PLoS One. 7:e334332012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ceccacci E and Minucci S: Inhibition of
histone deacetylases in cancer therapy: Lessons from leukaemia. Br
J Cancer. 114:605–611. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hu J, Jing H and Lin H: Sirtuin inhibitors
as anticancer agents. Future Med Chem. 6:945–966. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Jin Y, Cao Q, Chen C, Du X, Jin B and Pan
J: Tenovin-6-mediated inhibition of SIRT1/2 induces apoptosis in
acute lymphoblastic leukemia (ALL) cells and eliminates ALL
stem/progenitor cells. BMC Cancer. 15:2262015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Dai W, Zhou J, Jin B and Pan J: Class
III-specific HDAC inhibitor Tenovin-6 induces apoptosis, suppresses
migration and eliminates cancer stem cells in uveal melanoma. Sci
Rep. 6:226222016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Eckschlager T, Plch J, Stiborova M and
Hrabeta J: Histone deacetylase inhibitors as anticancer drugs. Int
J Mol Sci. 18(pii): E14142017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ota H, Tokunaga E, Chang K, Hikasa M,
Iijima K, Eto M, Kozaki K, Akishita M, Ouchi Y and Kaneki M: Sirt1
inhibitor, Sirtinol, induces senescence-like growth arrest with
attenuated Ras-MAPK signaling in human cancer cells. Oncogene.
25:176–185. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Bhalla S and Gordon LI: Functional
characterization of NAD dependent de-acetylases SIRT1 and SIRT2 in
B-cell chronic lymphocytic leukemia (CLL). Cancer Biol Ther.
17:300–309. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Süssmuth SD, Haider S, Landwehrmeyer GB,
Farmer R, Frost C, Tripepi G, Andersen CA, Di Bacco M, Lamanna C,
Diodato E, et al: An exploratory double-blind, randomized clinical
trial with selisistat, a SirT1 inhibitor, in patients with
Huntington's disease. Br J Clin Pharmacol. 79:465–476. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Heltweg B, Gatbonton T, Schuler AD,
Posakony J, Li H, Goehle S, Kollipara R, Depinho RA, Gu Y, Simon JA
and Bedalov A: Antitumor activity of a small-molecule inhibitor of
human silent information regulator 2 enzymes. Cancer Res.
66:4368–4377. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kalle AM, Mallika A, Badiger J, Alinakhi,
Talukdar P and Sachchidanand: Inhibition of SIRT1 by a small
molecule induces apoptosis in breast cancer cells. Biochem Biophys
Res Commun. 401:13–19. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Lai YH, Lin SY, Wu YS, Chen HW and Chen
JJW: AC-93253 iodide, a novel Src inhibitor, suppresses NSCLC
progression by modulating multiple Src-related signaling pathways.
J Hematol Oncol. 10:1722017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Rotili D, Tarantino D, Nebbioso A, Paolini
C, Huidobro C, Lara E, Mellini P, Lenoci A, Pezzi R, Botta G, et
al: Discovery of salermide-related sirtuin inhibitors: Binding mode
studies and antiproliferative effects in cancer cells including
cancer stem cells. J Med Chem. 55:10937–10947. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Lara E, Mai A, Calvanese V, Altucci L,
Lopez Nieva P, Martinez Chantar ML, Varela Rey M, Rotili D,
Nebbioso A, Ropero S, et al: Salermide, a Sirtuin inhibitor with a
strong cancer-specific proapoptotic effect. Oncogene. 28:781–791.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Jiang Z, Chen K, Cheng L, Yan B, Qian W,
Cao J, Li J, Wu E, Ma Q and Yang W: Resveratrol and cancer
treatment: Updates. Ann N Y Acad Sci. 1403:59–69. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Chauhan D, Bandi M, Singh AV, Ray A, Raje
N, Richardson P and Anderson KC: Preclinical evaluation of a novel
SIRT1 modulator SRT1720 in multiple myeloma cells. Br J Haematol.
155:588–598. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Tasoulas J, Giaginis C, Patsouris E,
Manolis E and Theocharis S: Histone deacetylase inhibitors in oral
squamous cell carcinoma treatment. Expert Opin Investig Drugs.
24:69–78. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Bruzzese F, Leone A, Rocco M, Carbone C,
Piro G, Caraglia M, Di Gennaro E and Budillon A: HDAC inhibitor
vorinostat enhances the antitumor effect of gefitinib in squamous
cell carcinoma of head and neck by modulating ErbB receptor
expression and reverting EMT. J Cell Physiol. 226:2378–2390. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Suzuki M, Endo M, Shinohara F, Echigo S
and Rikiishi H: Enhancement of cisplatin cytotoxicity by SAHA
involves endoplasmic reticulum stress-mediated apoptosis in oral
squamous cell carcinoma cells. Cancer Chemother Pharmacol.
64:1115–1122. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Eriksson I, Joosten M, Roberg K and
Ollinger K: The histone deacetylase inhibitor trichostatin A
reduces lysosomal pH and enhances cisplatin-induced apoptosis. Exp
Cell Res. 319:12–20. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sato T, Suzuki M, Sato Y, Echigo S and
Rikiishi H: Sequence-dependent interaction between cisplatin and
histone deacetylase inhibitors in human oral squamous cell
carcinoma cells. Int J Oncol. 28:1233–1241. 2006.PubMed/NCBI
|
|
69
|
Shoji M, Ninomiya I, Makino I, Kinoshita
J, Nakamura K, Oyama K, Nakagawara H, Fujita H, Tajima H, Takamura
H, et al: Valproic acid, a histone deacetylase inhibitor, enhances
radiosensitivity in esophageal squamous cell carcinoma. Int J
Oncol. 40:2140–2146. 2012.PubMed/NCBI
|
|
70
|
Gan CP, Hamid S, Hor SY, Zain RB, Ismail
SM, Wan Mustafa WM, Teo SH, Saunders N and Cheong SC: Valproic
acid: growth inhibition of head and neck cancer by induction of
terminal differentiation and senescence. Head Neck. 34:344–353.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Gong L, Wang WM, Ji Y, Wang Y and Li DW:
Effects of sodium butyrate on proliferation of human oral squamous
carcinoma cell line and expression of p27Kip1. Zhonghua Kou Qiang
Yi Xue Za Zhi. 45:619–622. 2010.PubMed/NCBI
|
|
72
|
Lin Z and Fang D: The roles of SIRT1 in
cancer. Genes Cancer. 4:97–104. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Salminen A, Kaarniranta K and Kauppinen A:
Crosstalk between oxidative stress and SIRT1: Impact on the ageing
process. Int J Mol Sci. 14:3834–3859. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Agarwal SK: Integrins and cadherins as
therapeutic targets in fibrosis. Front Pharmacol. 5:1312014.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Xue H, Atakilit A, Zhu W, Li X, Ramos DM
and Pytela R: Role of the avb6 integrin in human oral squamous cell
carcinoma growth in vivo and in vitro. Biochem Biophys Res Commun.
288:610–618. 2008. View Article : Google Scholar
|
|
76
|
Xu M, Yin L, Cai Y, Hu Q, Huang J, Ji Q,
Hu Y, Huang W, Liu F, Shi S and Deng X: Epigenetic regulation of
integrin β6 transcription induced by TGF-β1 in human oral squamous
cell carcinoma cells. J Cell Biochem. 119:4193–4204. 2018.
View Article : Google Scholar : PubMed/NCBI
|