Introduction
Breast cancer is the most common cancer in women and
the second leading cause of cancer mortality in women (1). Accurate diagnosis and staging are
essential for the selection of the most appropriate therapeutic
strategy and major determinants of patient prognosis and survival
(2).
A systematic work-up for operable invasive breast
carcinoma has usually been performed by physical examination,
bilateral mammogram and ultrasound with or without breast MRI. In
the case of operable stage IIIA (T3N1M0), additional imaging,
including bone scanning (BS), abdominal and pelvic CT (or
ultrasound or MRI), and chest imaging, may be used. The
significance of PET/CT in initial staging of breast carcinoma has
not yet been well-defined in routine clinical practice. Clinicians
usually refer patients for PET/CT scan when conventional imaging
studies are equivocal, suggestive or considered as ‘high risk’
according to patients’ histological and surgical manifestations.
Several studies show that PET/CT provides important information in
patients with stage II or III breast carcinoma with the detection
of unknown lymph node metastases outside axillary levels I and II
(infraclavicular, supraclavicular and internal mammary nodes) and
the detection of occult distant metastases (3–8).
However, this study included patients with stage II or III breast
cancer. In this retrospective study, we also included stage I
patients of invasive breast carcinoma (invasive ductal, invasive
lobular or mix type) with high histological grade (grade II–III)
and postoperative patients for whom clinical work-up had been
performed by conventional imaging modalities (CIM; mammogram,
ultrasound, chest X-ray, breast MRI, BS, abdominal and pelvic CT or
ultrasound or MRI) prior to surgery.
Materials and methods
In this retrospective study we included 141
consecutive newly diagnosed, histological high grade (grade II–III)
preoperative patients (mean age 47 years, range 28–78 years) and
195 postoperative high risk breast cancer patients (mean age 48
years, range 25–75 years) who were referred to PET/CT for initial
staging. Clinical stage had been determined by physical
examination, mammography, ultrasound of the breast and axilla, and
the breast MRI. The clinical stage III patients underwent a
conventional imaging work-up with BS, abdominal and pelvic CT (or
ultrasound or MRI), and chest imaging. T and N clinical scores were
evaluated according to the American Joint Committee on Cancer
(AJCC) classification (9).
No patients in this series had received chemotherapy
or radiotherapy prior to PET/CT examination. The patients fasted
for 6 h as the blood glucose level had to be less than 150 g/ml.
18F-FDG (5 MBq/kg) was intravenously injected into the
arm opposite to the tumor using a venous line to prevent
extravasation. Imaging was performed 60 min after the injection on
a PET/CT scanner (GE Discovery 690 PET/CT).
The PET/CT scans were interpreted by 2 nuclear
medicine specialists. If the interpretation differed, consensus was
reached with the aid of a third reader. The readers relied on
visual assessment of PET images (a well-defined focus, with uptake
clearly higher than surrounding background). The location of
hypermetabolic lymph nodes on the PET/CT image was noted according
to the AJCC seventh classification (9).
For distant metastases, form and intensity of
18F-FDG uptake and CT findings were considered
altogether. 18F-FDG uptake corresponding to degenerative
findings on the underlying CT scan (e.g. on facet articulation) and
uptake in a rib fracture in a patient with a history of trauma were
considered benign. However, high uptake on a classic area of
metastasis (e.g. body of a vertebra, pedicle, long bone) was
considered malignant even if the CT scan revealed subtle or no
change, in agreement with the well-known high sensitivity of
18F-FDG PET, compared with CT, for early bone marrow
involvement (10). For lung
evaluation, we considered any pulmonary nodules with high
18F-FDG uptake or the presence of multiple small round
nodules on the CT part as suggestive (even in the absence of an
increase in 18F-FDG uptake).
PET/CT findings considered to be suggestive of
malignancy were assessed using surgery, biopsy results or patient
follow-up. For bone foci, MRI was performed instead of biopsy. We
considered modification of stage resulting from findings of distant
metastasis or lymph node involvement outside classic areas of
axillary dissection, with an impact on treatment management.
Staging using PET/CT was compared with that of the conventional
modalities.
Results
Primary staging of preoperative
patients
Stage I. Nineteen patients had clinical stage
I (T1N0). All of the primary tumors had clear 18F-FDG
uptake [median maximum standardized uptake value (SUVmax), 5.7;
range, 1.2–13.7].
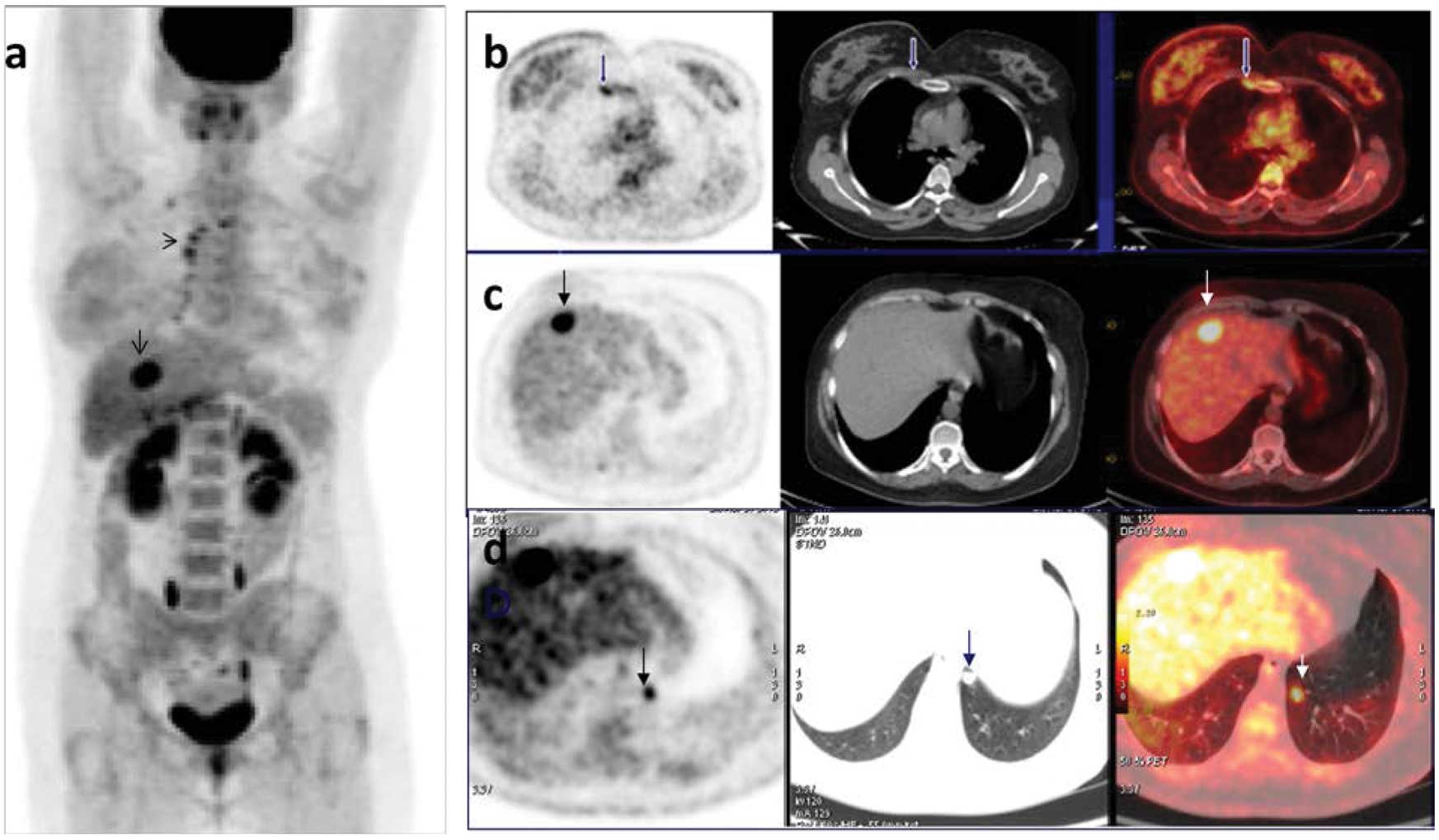
PET/CT increased the stage of 5 patients (26%).
Uptake in axillary lymph nodes in 2 patients, internal mammary
lymph nodes in 2 patients and bone metastases in one patient were
detected by PET/CT (Fig. 1).
Stage IIA. Fifty-one patients had clinical
stage IIA (12 T2N0M0 and 39 T1N1M0). All primary tumors had
18F-FDG uptake (T2N0M0 median SUVmax, 8.7; range,
2.8–15.8; T1N1M0 median SUVmax, 6.1; range, 1.8–21.7).
PET/CT increased the stage of 4 patients (33%) in
the T2N0 group. In 2 patients axillary level II lymph nodes which
were not detected by ultrasonographic (USG) imaging, in one patient
bone metastases which were not detected by BS (confirmed by
follow-up) and in one patient liver metastases were not detected by
contrast enhanced CT (CE-CT; confirmed by MRI), were
identified.
PET/CT increased the stage of 11 patients (28%) in
the T1N1 group. Exta-axillary lymph node metastases in 3 patients
(infraclavicular and supraclavicular lymph node metastases in 3
patients) and distant metastases in 8 patients (5 bone, 1 bone and
pleura, 1 bone and lung and 1 contralateral breast) were
detected.
Stage IIB. Forty-nine patients had clinical
stage IIB (2 T3N0 and 47 T2N1). All primary tumors had
18F-FDG avidity (in T3N0 group median SUVmax, 12.2;
range, 9.5–14.6; in T2N1 group median SUVmax, 9.4; range,
2.3–20.9).
PET/CT changed the stage in 23 patients (48%).
Infraclavicular (level III) uptake in 2 patients and internal
mammary uptake in 4 patients initially classified as T2N1 were
detected. These patients were reclassified as N3b (stage IIIC).
18F-FDG uptake which was suggestive of distant
metastasis was observed in 24 women: 11 with bone, 2 with liver
(confirmed by MRI), 1 with both bone and surrenal, 3 with bone and
liver metastases and 1 with pleural involvement.
Stage IIIA. Twelve patients had clinical
stage IIIA (11 T3N1 and 1 T2N2). All primary tumors exhibited
18F-FDG uptake (median SUVmax, 9.1; range,
3.2–28.5).
PET/CT changed the staging in 7 (58%) patients.
PET/CT revealed N3 lymph nodes (infra- or supraclavicular or
internal mammary) in 3 (25%) patients and uptake suggestive of
distant metastases in 4 (33%) patients. Sites of involvement in the
4 patients with distant lesions were bone (n=1), bone and liver
(n=2) and contralateral breast (n=1).
Stage IIIB. Two patients had clinical stage
IIIB (2 T4N1). The primary tumor showed 18F-FDG uptake
(median SUVmax, 8.4; range, 6.8–10).
PET/CT changed the staging in both patients (100%).
PET/CT detected internal mammary lymph nodes and distant metastases
in 2 patients (100%). There were bone metastases in one and both
bone and lung metastases in the other patient.
PET/CT detected multifocal lesions in 30 (21%)
patients, multicentric lesions in 21 (14%) patients and malign foci
in the contralateral breast (confirmed by biopsy) in 5 (3.5%)
patients.
In the detection of metastatic subcentimetric
pulmonary nodules with low 18F-FDG uptake, the CT
component of PET/CT increased sensitivity. By contrast, the PET
component of PET/CT revealed malign pleural invasion and effusion,
and adrenal and liver metastases which were equivocal in CT.
PET/CT detected liver metastasis in 13 patients, of
which only 5 had evidence by CE-CT.
PET/CT revealed true-positive bone metastases in 35
patients whereas BS revealed metastases in only 21 (61%). In all 14
patients with negative BS results, MRI and follow-up confirmed bone
involvement. Five of these 14 women had additional visceral
metastases.
PET/CT changed the staging, with impact on
therapeutic management in 15% (3/19) of stage I patients, 25%
(13/51) of stage IIA patients, 48% (24/49) of stage IIB patients,
58% (7/12) of stage IIIA patients and 100% (2/2) of patients with
stage IIIB due detection of extra-axillary and distant metastasis.
The planning for radiotherapy was modified according to PET/CT
results to encompass the internal mammary basin. Chemotherapy was
adapted to the metastatic diseases and certain bone lesions were
treated by radiation therapy (Tables
I and II).
 | Table IClinical stages of preoperative
patients. |
Table I
Clinical stages of preoperative
patients.
| Clinical stage/T, N,
M | No. of patients |
|---|
| Stage I | |
| T1N0 | 19 |
| Stage IIA | |
| T2N0 | 12 |
| T1N1 | 39 |
| Total | 51 |
| Stage IIB | |
| T3N0 | 2 |
| T2N1 | 47 |
| Total | 49 |
| Stage IIIA | |
| T3N1 | 11 |
| T2N2 | 1 |
| Total | 12 |
| Stage IIIB | |
| T4N1 | 2 |
| Stage IV | |
| Any T, any N,
M1 | 8 |
| Total | 141 |
 | Table IIImpact of 18F-FDG PET/CT
results in preoperative patients [number of patients (% per-patient
basis)]. |
Table II
Impact of 18F-FDG PET/CT
results in preoperative patients [number of patients (% per-patient
basis)].
| Variable | Stage I | Stage IIA | Stage IIB | Stage IIIA | Stage IIIB |
|---|
| No. of patients | 19 | 51 | 49 | 12 | 2 |
| Overall stage
modification with impact on therapeutic management | 3 (15%) | 13 (25%) | 23 (48%) | 7 (58%) | 2 (100%) |
| Detection of unknown
extra-axillary lymph node metastases | 2 (10%) | 3 (5.8%) | 6 (12.2%) | 4 (33.3%) | 2 (100%) |
| Internal
mammary | 2 | - | 4 | 1 | 2 |
|
Infraclavicular | - | 2 | 2 | 1 | - |
|
Supraclavicular | - | 1 | - | 1 | - |
| Mediastinal | - | - | - | 1 | - |
| Detection of
unsuspected distant metastases | 1 (5%) | 10 (19.6%) | 20 (40%) | 7 (58%) | 2 (100%) |
| Bone
metastases | 1 | 8 | 13 | 4 | 2 |
| Liver
metastases | - | 1 | 3 | 2 | - |
| Lung
metastases | - | 1 | 1 | 1 | 1 |
| Other sites
(surrenal, pleura) | - | 1 | 3 | - | - |
Postoperative patients
Of the examined 195 postoperative patients, PET/CT
detected residual tumor foci in the original breast which reflects
insufficient surgery in 18 patients (9%). Mastectomy should have
been performed on these patients instead of breast-conserving
surgery.
PET/CT detected ipsilateral axillary lymph nodes in
22 (11%) patients, extra-axillary regional lymph nodes in 21 (10%)
patients (10 internal mammary, 4 infraclavicular, 9
supraclavicular, 11 mediastinal, 4 jugular) and distant metastasis
in 24 (12%) patients (18 bone, 2 liver, 4 lung, 1 pleura and 2
adrenal). None of these metastatic sites had been detected by
conventional imaging modalities prior to surgery.
Additional PET/CT findings changed radiotherapy
planning in 22 (11%) patients and chemotherapy was adapted to the
metastatic diseases in 24 (12%) patients (Table III).
 | Table III18F-FDG PET/CT findings in
postoperative patients (% per-patient basis). |
Table III
18F-FDG PET/CT findings in
postoperative patients (% per-patient basis).
| Variable | No. of patients |
|---|
| Detection of residual
tumor | 18 (9.2%) |
| Detection of axillary
lymph nodes involvement which were not detected by CIM and SLNB
prior to surgery | 22 (11%) |
| Detection of unknown
extra-axillary node metastases | 21 (10%) |
| Internal
mammary | 10 |
|
Infraclavicular | 4 |
|
Supraclavicular | 9 |
| Mediastinal | 11 |
| Jugular | 4 |
| Detection of
unsuspected distant metastases | 24 (11%) |
| Bone | 18 |
| Liver | 2 |
| Lung | 4 |
| Pleura | 1 |
| Adrenal | 2 |
| Modification in
post-operative treatment plan | 46 (23%) |
| Radiotherapy
planning | 21 (10%) |
| Chemotherapy for
metastatic disease | 24 (11%) |
Five of eighteen postoperative patients whom PET/CT
showed bone metastases had negative preoperative BS and none
underwent BS following post surgical PET/CT scan since all patients
had additional nodal or visceral metastasis and the majority were
confirmed by MRI.
False-positive findings in articular regions which
belongs usually to inflammatory or degenerative changes in the
traumatic fracture sites were differentiated from malign
involvements by the CT component of PET/CT.
Discussion
There are several studies which show that PET/CT
provides important information on patients with stage II or III
breast carcinoma with the detection of unknown lymph node
metastases outside axillary levels I and II and detection of occult
distant metastases (3–8). Previous studies suggest that PET/CT
likely has no role in initial staging in patients with T1 (≤2 cm)
tumors since the sensitivity to detect the primary tumor and
axillary involvement is too low and the probability of finding
distant metastases is also low. These results are explained by the
various histopathology and size of the tumors. Lower sensitivity
has been reported in more differentiated and slow-growing tumors
and in noninvasive breast cancer, whereas improved performance has
been demonstrated for the detection of primary invasive breast
cancer with an overall sensitivity, specificity and accuracy of 90,
93 and 92%, respectively (11). In
our retrospective study all patients had grades II and III invasive
breast carcinoma. All 58 patients with T1 tumor (19 T1N0, 39 T1N1)
had good FDG uptake (median SUVmax, 5.9) and were detected by
PET/CT (sensitivity and specificity 100%). PET/CT also detected
internal mammary lymph node involvements in 2 patients and early
bone marrow metastases in 1 patient with stage I disease. These
findings prove that invasive breast cancer is a systemic disease
and even early breast cancer may give rise to metastases which were
not detected previously by routine clinical work-up.
In this study PET/CT was demonstrated to be more
sensitive in detecting multifocal lesions than the combination of
mammography and ultrasonography. PET/CT detected multifocal lesions
in 30 (21%) and multicentric lesions in 21 (14%) preoperative
patients. In the postoperative group, PET/CT detected residual
tumor foci in 18 (9%) patients. Ultrasonography and mammography
combination had not identified these lesions and patients underwent
breast-conserving surgery instead of mastectomy.
PET/CT identified axillary levels I and II lymph
node involvements in 109 (55%) preoperative patients. In 22 (11%)
postoperative patients PET/CT demonstrated increased metabolic
activity in the axillary lymph nodes which have typical morphology
for the metastases (round shape, loss of fatty hilus). This
postoperative group revealed that sentinel lymph node biopsy (SLNB)
may not detect macroscopic axillary metastatic lymph nodes in at
least 10% of high risk patients. This false-negative rate of SLNB
is too high in this high risk population with high prevalence of
axillary lymph node metastases (≥40%) and may be due to massive
invasion of a sentinel node that has lost its functional capacity
of phagocytosis and is detected by PET/CT. By identifying 50% or
more of cases of clinically occult lymph node disease in the
axilla, PET/CT reduces the risk linked to false-negative SLNB.
Since the positive predictive value is high in patients with
positive FDG PET/CT in the axilla (82%), axillary lymph node
dissection (ALND) may be performed directly without SLNB (12–14).
Detecting lymph node involvement in levels or basins
other than those addressed by routine ALND may have a major impact
on treatment strategies. Numerous studies suggest that FDG PET
outperforms conventional imaging in detecting involvement in
high-level axillary (level III) as well as in supraclavicular and
internal mammary lymph nodes (3,4,6,15,16)
PET/CT is particularly appealing compared to PET alone as it
provides the precise location of involved nodes (4,6,16).
In addition, false positives due to muscular and brown fat uptake
are avoided. In this study PET/CT revealed unsuspected
infraclavicular node involvement (N3a) in 11 (7.8%) preoperative
and in 4 (2%) postoperative patients, and supraclavicular node
involvement (N3c) in 8 (5.6%) preoperative and in 9 (4.6%)
postoperative patients. The differentiation of level III axillary
lymph nodes (infraclavicular lymph nodes) is important since
axillary clearance usually includes levels I and II nodes only.
Surgical studies have demonstrated that level III node involvement
(N3a) results in a poorer prognosis (17), for which a subsequently modified
surgical approach is useful (4).
The detection of extra-axillary involvement (supraclavicular and/or
internal mammary lymph nodes) is also extremely useful in
delineating the radiotherapy target zone or schedule surgery.
Patients with supraclavicular lymph nodes (N3c) may receive more
intensive treatment, combining induction chemotherapy, surgery,
postsurgical chemotherapy and irradiation, which improves the
disease-free survival and overall survival (18). In addition, visualization of an
internal mammary hot node by initial PET/CT may lead to a decision
on surgery and/or radiotherapy (4).
The findings of metastasis on the initial work-up
markedly changes treatment approaches. PET (19–21),
particularly PET/CT (4,10,16),
outperforms classic modalities to detect occult metastases. In this
retrospective study, on 195 postoperative high risk breast cancer
patients, PET/CT revealed distant metastases in 24 (12%) patients
whose metastatic involvement was not detected by conventional
imaging during the preoperative work-up.
Fuster et al (6) studied 60 consecutive patients with
breast cancer stage IIB or higher. PET/CT sensitivity and
specificity in detecting distant metastasis were 100 and 98%,
respectively, vs. 60 and 83% for conventional work-up
(contrast-enhanced chest CT, liver ultrasonography, 99 mTc-HDP BS).
It is well-known that PET outperforms BS for the detection of lytic
metastases and for early intra-medullary involvement, but has lower
sensitivity in cases of pure osteoblastic lesions (22). PET/CT is also highly sensitive in
detecting pleural, mediastinal, abdominal and pelvic metastases.
PET performs well to assess lung nodules larger than 1 cm, but its
sensitivity is low in smaller lesions, due to partial volume effect
and respiratory motion. Careful interpretation of the CT images may
depict small pulmonary nodules that do not present as hot spots on
PET.
In conclusion, this retrospective study clearly
showed that PET/CT appears to outperform conventional modalities in
the initial work-up of invasive breast cancer patients. PET/CT
allows diagnosis of infraclavicular, supraclavicular and internal
mammary node involvement and may detect occult distant metastases.
Additional PET/CT findings (findings of N3 disease or distant
disease) to conventional imaging modalities may cause substantial
change in the management of patients. In particular, PET/CT
findings in postoperative patients clearly showed that clinical
work-up by conventional imaging is insufficient for initial staging
of invasive breast carcinoma and PET/CT should be used as a
first-line test for high risk patients.
References
|
1
|
Jemal A, Siegel R, Ward E, Murray T, Xu J
and Thun MJ: Cancer statistics, 2007. CA Cancer J Clin. 57:43–66.
2007. View Article : Google Scholar
|
|
2
|
Esserman L: Integration of imaging in the
management of breast cancer. J Clin Oncol. 23:1601–1602. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Groheux D, Giaccchetti S, Espié M, et al:
The yield of 18F-FDG PET/CT in patients with clinical
stage IIA, IIB, or IIIA breast cancer: a prospective study. J Nucl
M. 52:1526–1534. 2011.
|
|
4
|
Groheux D, Moretti J, Baillet G, et al:
Effect of 18F-FDG PET/CT imaging in patients with
clinical stage II and III breast cancer. Int J Radiat Oncol Biol
Phys. 71:695–704. 2008.
|
|
5
|
Heusner TA, Kuemmel S, Umutlu L, et al:
Breast cancer staging in a single session: whole-body PET/CT
mammography. J Nucl Med. 49:1215–1222. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fuster D, Duch J, Paredes P, et al:
Preoperative staging of large primary breast cancer with
[18F] fluorodeoxyglucose positron emission
tomography/computed tomography compared with conventional imaging
procedures. J Clin Oncol. 26:4746–4751. 2008.
|
|
7
|
Aukema TS, Straver ME, Peeters MJ, et al:
Detection of extra-axillary lymph node involvement with FDG PET/CT
in patients with stage II–III breast cancer. Eur J Cancer.
46:3205–3210. 2010.PubMed/NCBI
|
|
8
|
Segaert I, Mottaghy F, Ceyssens S, et al:
Additional value of PET-CT in staging of clinical stage IIB and III
breast cancer. Breast J. 16:617–624. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC Cancer Staging Manual (7th edition).
Springer. New York: 2010.
|
|
10
|
Nakamoto Y, Cohade C, Tatsumi M, Hammoud D
and Wahl RL: CT appearance of bone metastases detected with FDG PET
as part of the same PET/CT examination. Radiology. 237:627–634.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Quon A and Gambhir SS: FDG-PET and beyond:
molecular breast cancer imaging. J Clin Oncol. 23:1664–1673. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heusner TA, Kuemmel S, Hahn S, et al:
Diagnostic value of full-dose FDG-PET/CT for axillary lymph node
staging in breast cancer patients. Eur J Nucl Med Mol Imaging.
36:1543–1550. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Groheux D, Hindié E, Rubello D, et al:
Should FDG PET/CT be used for initial staging of breast cancer? Eur
J Nucl Med Mol Imaging. 36:1539–1542. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee JH, Rosen EL and Mankoff DA: The role
of radiotracer imaging in the diagnosis and management of patients
with breast cancer: part 1 – overview, detection, and staging. J
Nucl Med. 50:569–581. 2009.
|
|
15
|
Yang WT, Le-Petross HT, Macapinlac H, et
al: Inflammatory breast cancer: PET/CT, MRI, mammography, and
sonography findings. Breast Cancer Res Treat. 109:417–426. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Carkaci S, Macapinlac HA, Cristofanilli M,
et al: Retrospective study of 18F FDG PET/CT in the
diagnosis of inflammatory breast cancer: preliminary data. J Nucl
Med. 50:231–238. 2009.
|
|
17
|
Kuru B, Camlibel M, Dinc S, Gulcelik MA
and Alagol H: Prognostic significance of axillary node and
infraclavicular lymph node status after mastectomy. Eur J Surg
Oncol. 29:839–844. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Brito RA, Valero V, Buzdar AU, et al:
Long-term results of combined-modality therapy for locally advanced
breast cancer with ipsilateral supraclavicular metastases: The
University of Texas M.D. Anderson Cancer Center experience. J Clin
Oncol. 19:628–633. 2001.
|
|
19
|
Cermik TF, Mavi A, Basu S and Alavi A:
Impact of FDG PET on the preoperative staging of newly diagnosed
breast cancer. Eur J Nucl Med Mol Imaging. 35:475–483. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Port ER, Yeung H, Gonen M, et al:
18F-2-fluoro-2-deoxy-D-glucose positron emission
tomography scanning affects surgical management in selected
patients with high-risk, operable breast carcinoma. Ann Surg Oncol.
13:677–684. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mahner S, Schirrmacher S, Brenner W, et
al: Comparison between positron emission tomography using
2-[fluorine-18] fluoro-2-deoxy-D-glucose, conventional imaging and
computed tomography for staging of breast cancer. Ann Oncol.
19:1249–1254. 2008.
|
|
22
|
Nakai T, Okuyama C, Kubota T, et al:
Pitfalls of FDG-PET for the diagnosis of osteoblastic bone
metastases in patients with breast cancer. Eur J Nucl Med Mol
Imaging. 32:1253–1258. 2005. View Article : Google Scholar : PubMed/NCBI
|