Introduction
Due to excellent spatial and temporal resolution,
ultrasound has become the first choice for the imaging examination
of thyroid nodules, with a detection rate as high as 70% (1,2). The
incidence of adult thyroid nodules is 20–75%, among which 5–6.5% of
nodules are diagnosed as malignant (3,4).
Thyroid disease is complex and varied and the differentiation
between benign and malignant nodules is clinically difficult. Fine
needle aspiration biopsy (FNAB) guided by ultrasound is the gold
standard for the diagnosis of thyroid cancer; however, the
dissatisfaction rate of tissue drawing is ∼10–20% (5). Therefore, an effective imaging
technique based on optimized systematical puncture biopsy to
accurately determine the position of the thyroid lesions is
required. This is likely to improve the detection rate of thyroid
cancer, reduce unnecessary repeated biopsies and reduce the
incidence of complications.
As identified in previous studies, the
contrast-enhanced ultrasound (CEUS) technique improves the
detection rate of lesions and diagnosis sensitivity (6–8).
Bartolotta et al(9)
performed CEUS on 18 patients with a solitary thyroid nodule and
confirmed its feasibility. The second generation CEUS contrast
agent SonoVue contains sulfur hexafluoride microbubbles, which
generate resonance under the action of an acoustic wave with low
mechanical index. The low acoustic energy emission and pulse
inversion harmonic imaging are combined to clearly exhibit the
microvascular perfusion in tumors (10). CEUS has been successfully applied
in the diagnosis and interventional therapy of focal liver lesions.
Ultrasound guidance effectively improves the safety of aspiration
biopsy. However, due to the difficulties in discriminating between
necrotic and non-necrotic areas in a tumor with conventional
ultrasound, the positive rate of biopsies is low, with increased
numbers of false negative results. In the current study, CEUS
combined with microflow imaging (MFI) was applied to guide the
puncture biopsy of the thyroid, and compared with conventional
ultrasound. The application value of CEUS is also discussed.
Subjects and methods
Subjects
A total of 48 patients with 51 suspected solid
thyroid nodules in Shaanxi Provincial Cancer Hospital Affiliated to
Medical School, Xi’an Jiaotong University from May 2011 to
September 2012 were enrolled in this study. There were 13 males
with 13 nodules and 35 females with 38 nodules. They were aged
17–64 years, with an average age of 47.2±5.7 years. The diameter of
the nodules was 0.6–4.3 cm (average, 1.6 cm). Patients
hypersusceptible to SonoVue or with coagulation dysfunction were
excluded. This study was approved by the ethics committee of
Shaanxi Provincial Cancer Hospital Affiliated to Medical School,
Xi’an Jiaotong University. Informed consent was obtained from all
patients.
Apparatus and methods
An iU22 ultrasound machine (L9-3 probe; Philips
Medical Systems, Ltd., Eindhoven, The Netherlands) was used to
detect the thyroid. The normal thyroid tissue around the nodule was
selected as the contrast cross-section and puncture cross-section.
The suspicious solid thyroid nodule was used as the inclusion
criterion, with no background of diffuse thyroid lesions. A
microbubble suspension prepared with 59 mg SonoVue dry powder
(Bracco Imaging S.p.A Inc., Milan, Italy) and 5 ml normal saline
was used as the contrast agent. An intravenous injection in the
elbow with 2.4 ml contrast agent with low mechanical index
(0.06–0.08) was administered and the process of contrast agent
infusion in the tumor was observed.
Patients lay in the supine position, with their neck
on a high pad. Following conventional disinfection, local
infiltration anesthesia with 2% lidocaine was conducted. A
BARD® automatic biopsy gun (Bard Biopsy Systems, Tempe,
AZ, USA) combined with an 18G biopsy needle was used for the
biopsy. The puncture point and needle insertion angle were
determined. The puncture direction and position were monitored by
ultrasound and the non-enhancement area with liquefaction necrosis
was avoided. When the biopsy needle reached the tumor margin and
the ejection distance and direction were determined, the tissues in
the tumor marginal area and high-enhancement area were directly
drawn, followed by pathological diagnosis by senior pathologists.
The whole process was conducted under strictly aseptic conditions.
Following biopsy, local gentle pressing was conducted for
hemostasis.
Statistical analysis
Statistical analysis was performed using SPSS 13.0
statistical software (SPSS Inc., Chicago, IL, USA). McNemar’s test
was used to compare the positive number of nodules and puncture
point positive rate between CEUS and conventional ultrasound. The
Chi-square test was performed to compare the positive and negative
puncture point predictive values between the two methods. P<0.05
was considered to indicate a statistically significant
difference.
Results
Number of PTC nodules detected by the two
methods
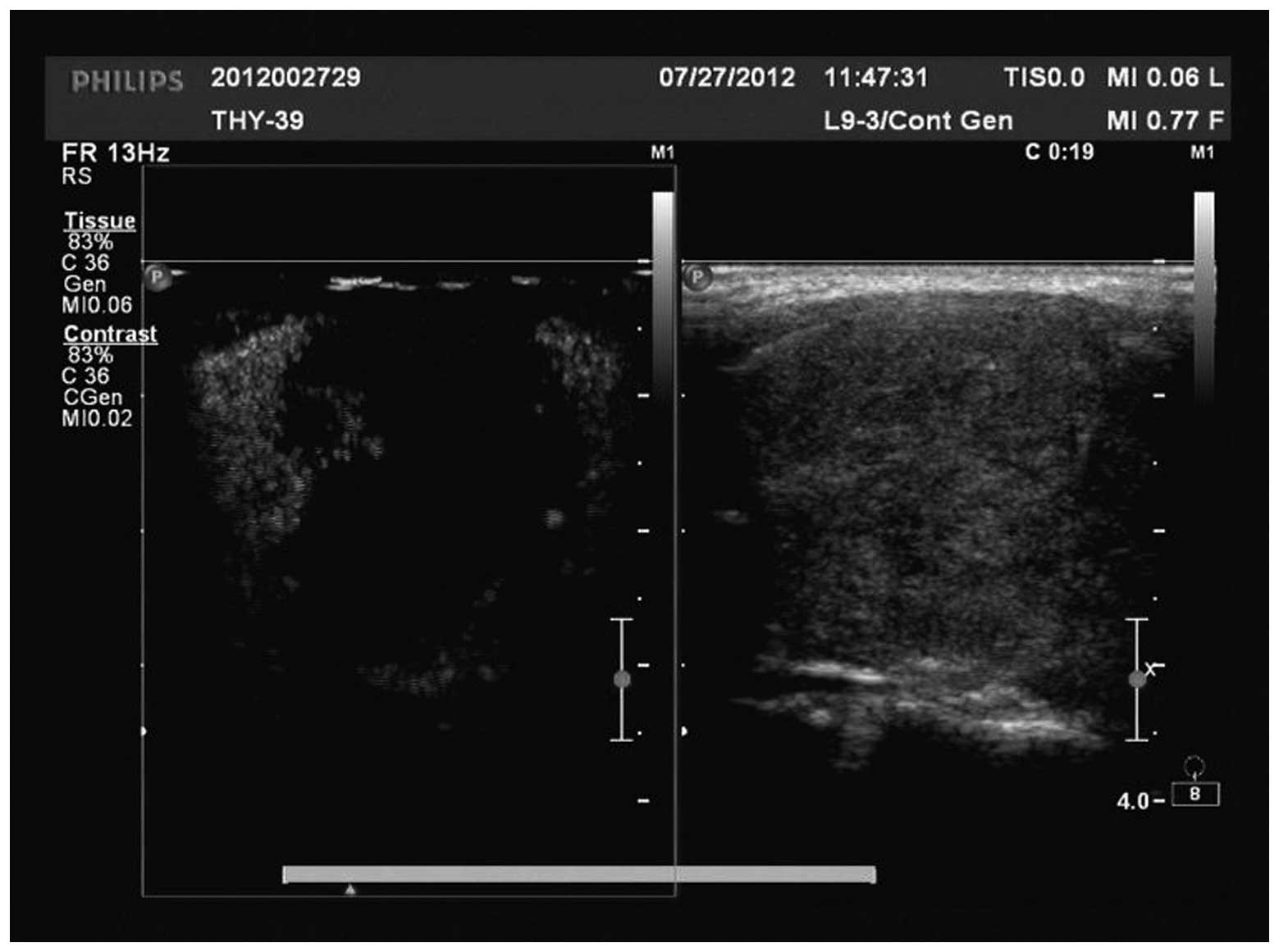
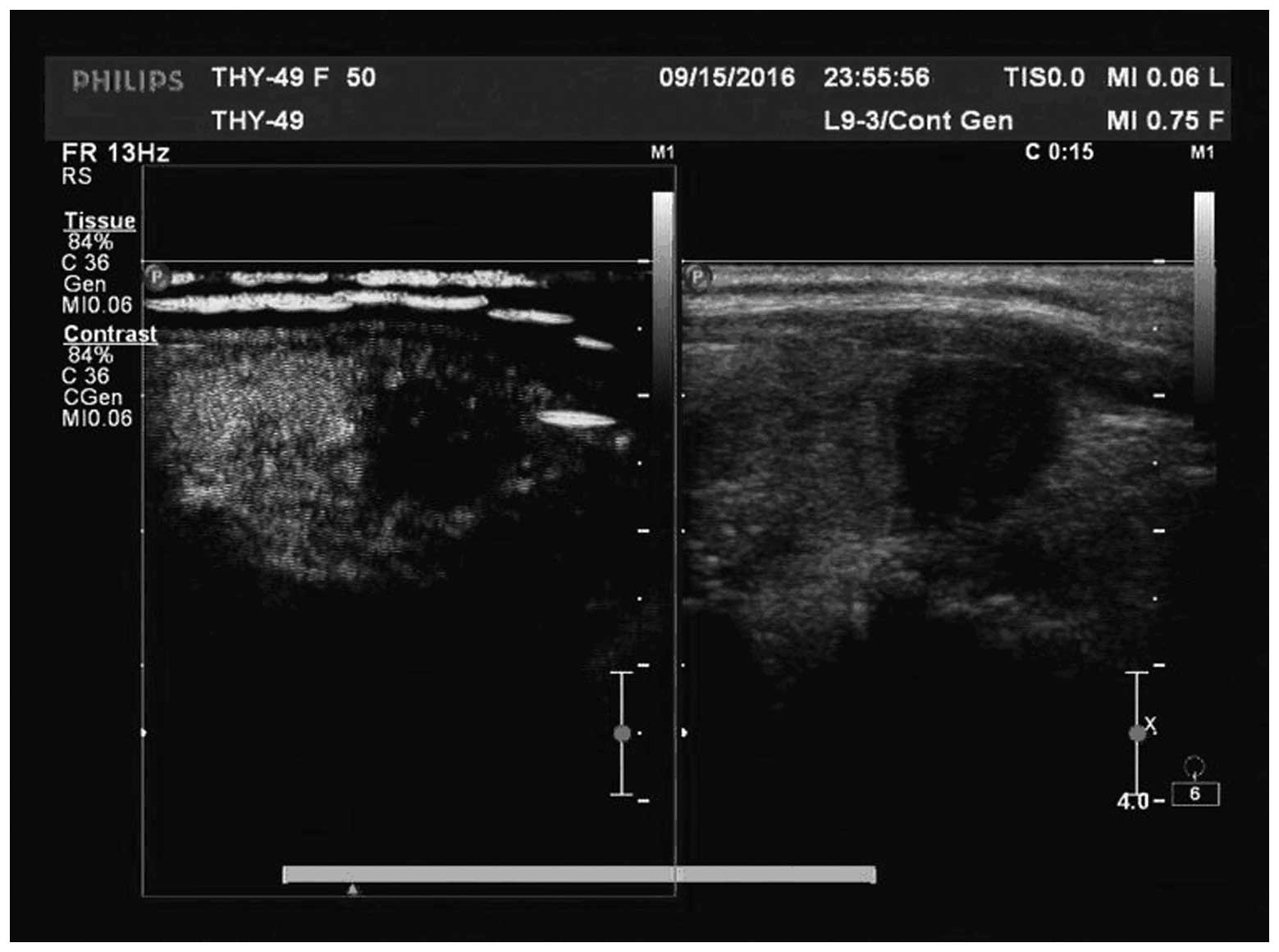
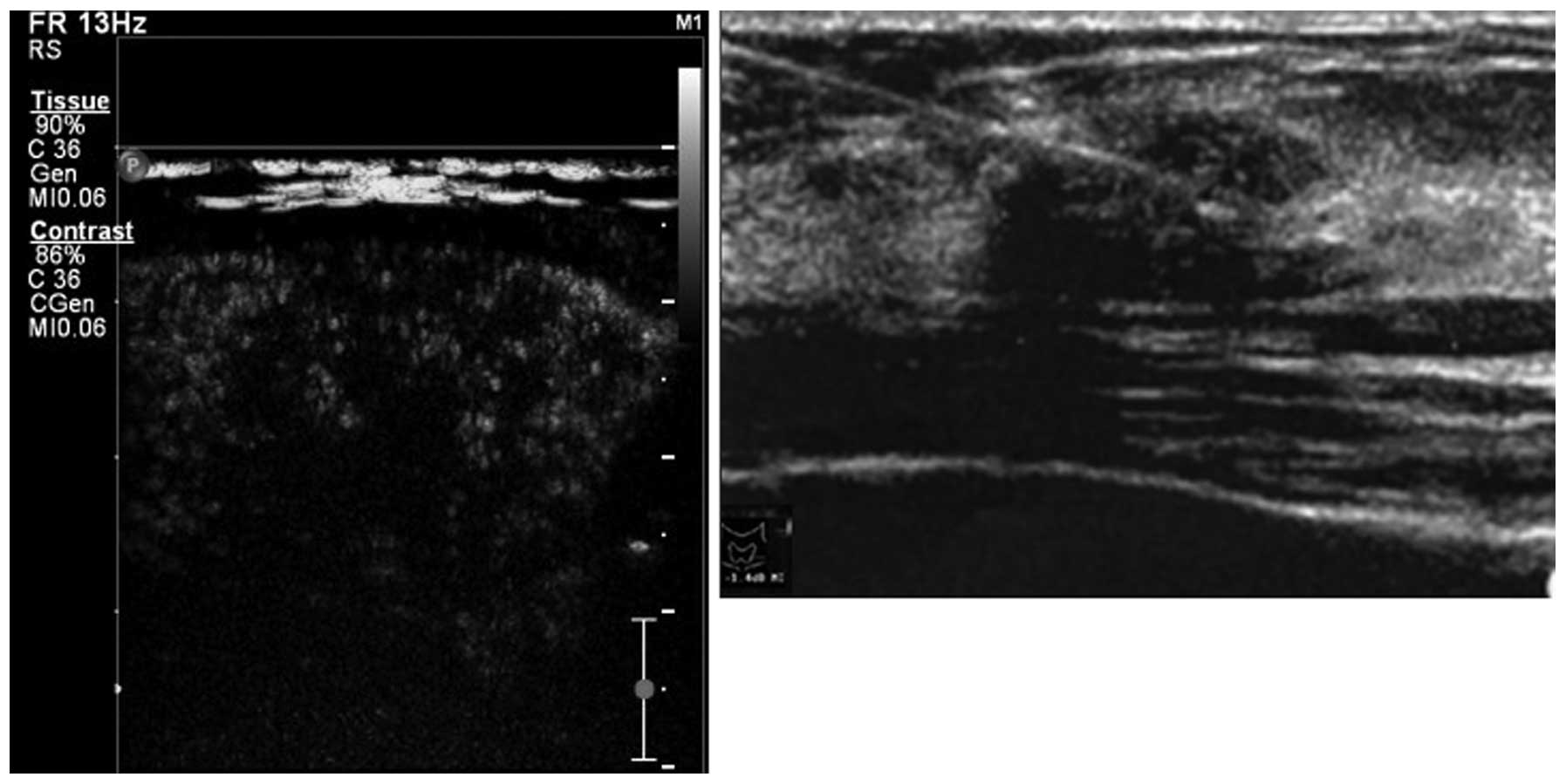
There were three types of manifestation, including
irregular weak concentric ring enhancement (Fig. 1), no or weak enhancement (Fig. 2) and uneven enhancement (Fig. 3) in the CEUS images of the 51
nodules in 48 patients. All nodules provided adequate specimens and
the satisfaction rate of tissue drawing was 100%. Of the 51
nodules, 44 (86.3%), five (9.8%) and two (3.9%) nodules were
pathologically diagnosed as PTC, nodular goiter and focal
Hashimoto’s disease, respectively. From the 44 nodules diagnosed as
PTC, 43 (97.7%) and 34 (77.3%) nodules were detected by CEUS and
conventional ultrasound, respectively, with a significant
difference between the two methods (P=0.022). Eleven (25%) nodules
were independently detected by CEUS and 31 (70.5%) nodules were
detected by CEUS and conventional ultrasound. Only one nodule was
not detected (2.3%).
Positive detection rates of puncture
points detected by the two methods
In 310 puncture points for 51 nodules, there were
240 (77.4%), 56 (18.1%) and 14 (4.5%) puncture points that were
pathologically diagnosed as PTC, nodular goiter and focal
Hashimoto’s disease, respectively. There were 127 and 212 puncture
points detected by conventional ultrasound and CEUS, with 2.49 and
4.16 puncture points per patient, respectively. The number of
detected puncture points and the specificity and accuracy of the
puncture points detected by CEUS and conventional ultrasound were
significantly different.
The pathological findings of the puncture points for
the two methods are shown Table I.
In the 240 puncture points pathologically diagnosed as PTC, 116
(48.3%) and 199 (82.9%) puncture points were detected by
conventional ultrasound and CEUS, respectively. In the 310 puncture
points, the 175 (56.5%) and 256 (82.6%) puncture points detected by
conventional ultrasound and CEUS, respectively, were consistent
with pathological findings. The sensitivity and accuracy of the
puncture point detection by CEUS were higher than those by
conventional ultrasound, respectively (P<0.001). The specificity
of puncture points detected by CEUS was lower than that by
conventional ultrasound (P=0.009). The negative predictive values
of puncture points detected by CEUS and conventional ultrasound
were 88.9% and 76.9%, respectively, with a significant difference
(P<0.001; Table II).
 | Table IPathological findings of puncture
points using the two methods. |
Table I
Pathological findings of puncture
points using the two methods.
| | Conventional
ultrasound
| CEUS
|
|---|
| Pathological
finding | Number of puncture
points | Positive | Negative | Positive | Negative |
|---|
| PTC positive | 240 | 116 | 124 | 199 | 41 |
| PTC negative | 70 | 11 | 59 | 13 | 57 |
| Total | 310 | 127 | 183 | 212 | 98 |
 | Table IIComparison of the positive rate of
puncture points between the two methods (%). |
Table II
Comparison of the positive rate of
puncture points between the two methods (%).
| Method | Sensitivity | Specificity | Accuracy | Positive predictive
value | Negative predictive
value |
|---|
| Conventional
ultrasound | 48.3 | 84.3 | 56.5 | 60.5 | 76.9 |
| CEUS | 82.9a | 81.4a | 82.6a | 67.5 | 88.9a |
Discussion
The incidence of PTC is increasing annually
(11), which may be related to new
detection means and increased awareness of PTC (12,13).
Although the prognosis of PTC is good, lymph node metastasis and a
high recurrence rate may also occur in the early stage (14–16).
Therefore, the early determination of nodule nature is clinically
significant. The conventional ultra-sound-guided biopsy shows
goiter, peripheral vessels and other important structures. However,
it is difficult to distinguish the necrotic and non-necrotic areas
in the tumor, which results in a low positive rate of tissue
drawing. Therefore, methods to improve the positive rate of
puncture for thyroid cancer and reduce the complications has become
a topic of concern for a number of scholars.
CEUS reflects the locus of contrast agent
microbubbles in the tissue vessel, describes the angioarchitecture
by a maximum intensity capture technique and clearly shows the
microvascular changes that color Doppler flow imaging (CDFI) is not
able to show. Therefore, the low-speed small blood vessels in
thyroid cancer are better reflected and detected. The neoplastic
vessels are usually distributed in a marginal area with active
tumor growth. In the central area of the tumor, tumor cells and
stroma hyperplasia cause an increase in intratumoral pressure,
leading to vascular compression, reduced perfusion, thrombus
formation, venous disorders and necrosis (17). In the current study, CEUS-guided
puncture biopsy in the high-enhancement area and peripheral area
with rich blood supply was performed on 51 nodules and the
satisfaction rate of tissue drawing was 100%. In the 44 patients
pathologically diagnosed with PTC, 43 cases were detected by CEUS,
indicating the clear advantages of CEUS compared with conventional
ultrasound. In the 11 nodules independently detected by CEUS, nine
nodules exhibited only a low echo by conventional ultrasound;
therefore, they were difficult to differentiate from other benign
nodules. The sensitivity and accuracy of the puncture points
obtained with CEUS are significantly higher than those obtained
with conventional ultrasound, which effectively improves the
positive rate and accuracy of puncture biopsy for thyroid cancer.
This indicates that CEUS is more helpful for selecting suspicious
lesions for thyroid puncture biopsy, compared with conventional
ultrasound. The results in this study are also consistent with
those of previous studies which have reported that CEUS improves
the sensitivity of puncture point biopsy (7,8).
The increased positive rate of puncture point biopsy
contributes to the detection of a greater number of thyroid cancer
patients using fewer puncture points, particularly for cystic-solid
mixed nodules and nodules with no clear substantial boundary,
regular shape or complete capsule, which conventional ultrasound
does not differentiate. CEUS-guided biopsy effectively prevents
tumor misdiagnosis and avoids unnecessary repeated sampling for the
nodule necrotic area without enhancement. Additionally, it prevents
excessive surgical treatment on benign nodules. In this study, 2.49
puncture points per patient were detected by conventional
ultrasound. The detection rate was 77.3% (34/44), with 10 missed
nodules. For CEUS, 4.16 puncture points per patient were detected.
The detection rate was 97.7% (43/44), with only one missed nodule.
CEUS detects the majority of malignant nodules, with the advantages
of optimum puncture positioning and relatively few puncture points;
therefore, it improves the efficiency of targeted puncture biopsy.
With the development of CEUS technology, the individualized biopsy
scheme with limited puncture points for thyroid tumor will be
achieved.
In CEUS-guided thyroid puncture biopsy, multi-time
and multi-angle tissue drawing sampling should be performed to
improve the sensitivity and accuracy (18,19)
and guarantee adequate specimens. Quinn et al(20) identified that the diagnosis rate of
biopsy using a coarse needle for thyroid disease is significantly
higher than that using a fine needle. However, the optimum puncture
position and number of puncture points should be determined
according to the lesion location and peripheral vital structures.
An increase in the number of puncture points is likely to cause
repeated sampling and the occurrence of complications. Therefore,
the most reliable diagnosis results should be obtained with the
fewest puncture points. However, CEUS also has certain limitations:
i) for nodules close to the thyroid edge (adjacent to the common
carotid artery or capsule), the procedure is highly difficult with
a risk of puncture. In these cases, particular attention should be
paid to the occurrence of complications. On the basis of local
infiltration anesthesia, 3–4 ml saline may be injected into the
thyroid and peripheral tissue to establish an isolation belt. This
effectively reduces the risk of puncture. ii) For nodules with a
diameter <0.5 cm, as the ejection distance of the puncture gun
is 1.5–2 cm, the puncture depth should be ∼0.7 cm away from the
nodule. The whole needle tract is revealed by ultrasound to enable
the nodule to be positioned at the extension line of the needle
tract. This is likely to improve the puncture accuracy for a tiny
nodule.
CEUS has a higher positive detection rate for
thyroid cancer than conventional ultrasound, with higher
sensitivity and puncture point accuracy. It has great clinical
application value in the guidance of thyroid puncture biopsy and is
the preferred method for detecting disease under non-surgical
conditions.
Acknowledgements
This study was supported by the
Science and Technology Research and Development Program of Shaanxi
Province (No. 2012K13-02-39).
References
|
1.
|
Solbiati L, Livraghi T, Ballarati E,
Ierace T and Crespi L: Tumors of the follicular epithelium.
Ultrasound of Superficial Structures. Solbiati L and Rizzatto G:
Churchill Livingstone; New York: pp. 63–71. 1995
|
|
2.
|
Hamazaki N, Kounoike Y, Suzaki Y, et al:
Usefulness of color Doppler sonography in the diagnosis of thyroid
nodules: comparison of velocity mode with power mode. Jpn J Med
Ultrason. 24:873–877. 1997.
|
|
3.
|
Tae HJ, Lim DJ, Baek KH, et al: Diagnostic
value of ultrasonography to distinguish between benign and
malignant lesions in the management of thyroid nodules. Thyroid.
17:461–466. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Frates MC, Benson CB, Charboneau JW, et
al: Management of thyroid nodules detected at US: Society of
Radiologists in Ultrasound consensus conference statement.
Radiology. 237:794–800. 2005. View Article : Google Scholar
|
|
5.
|
Cappelli C, Pirola I, Cumetti D, et al: Is
the anteroposterior and transverse diameter ratio of nonpalpable
thyroid nodules a sonographic criteria for recommending fine-needle
aspiration cytology? Clin Endocrinol (Oxf). 63:689–693. 2005.
View Article : Google Scholar
|
|
6.
|
Roy C, Buy X, Lang H, et al: Contrast
enhanced color Doppler endorectal sonography of prostate:
efficiency for detecting peripheral zone tumors and role for biopsy
procedure. J Urol. 170:69–72. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Halpern EJ, Rosenberg M and Gomella LG:
Prostate cancer: contrast-enhanced US for detection. Radiology.
219:219–225. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Halpern EJ, Verkh L, Forsberg F, Gomella
LG, Mattrey RF and Goldberg BB: Initial experience with
contrast-enhanced sonography of the prostate. AJR Am J Roentgenol.
174:1575–1580. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Bartolotta TV, Midiri M, Galia M, et al:
Qualitative and quantitative evaluation of solitary thyroid nodules
with contrast-enhanced ultrasound: initial results. Eur Radiol.
16:2234–2241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Kettenbach J, Helbich TH, Huber S, Zuna I
and Dock W: Computer-assisted quantitative assessment of power
Doppler US: effects of microbubble contrast agent in the
differentiation of breast tumors. Eur J Radiol. 53:238–244. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Davies L and Welch HG: Increasing
incidence of thyroid cancer in the United States, 1973–2002. JAMA.
295:2164–2167. 2006.
|
|
12.
|
Lin JD, Kuo SF, Chao TC and Hsueh C:
Incidental and nonincidental papillary thyroid microcarcinoma. Ann
Surg Oncol. 15:2287–2292. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Grodski S and Delbridge L: An update on
papillary microcarcinoma. Curr Opin Oncol. 21:1–4. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Besic N, Pilko G, Petric R, Hocevar M and
Zgajnar J: Papillary thyroid microcarcinoma: prognostic factors and
treatment. J Surg Oncol. 97:221–225. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Chung YS, Kim JY, Bae JS, et al: Lateral
lymph node metastasis in papillary thyroid carcinoma: results of
therapeutic lymph node dissection. Thyroid. 19:241–246. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Lim YC, Choi EC, Yoon YH, Kim EH and Koo
BS: Central lymph node metastases in unilateral papillary thyroid
microcarcinoma. Br J Surg. 96:253–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Galiè M, D’Onofrio M, Montani M, et al:
Tumor vessel compression hinders perfusion of ultrasonography
contrast agents. Neoplasia. 7:528–536. 2005.PubMed/NCBI
|
|
18.
|
Mehrotra P, Viswanathan H, Johnson SJ,
Wadehra V, Richardson DL and Lennard TW: Ultrasound guidance
improves the adequacy of our preoperative thyroid cytology but not
its accuracy. Cytopathology. 17:137–144. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Braga M, Cavalcanti TC, Collaco LM and
Graf H: Efficacy of ultrasound-guided fine-needle aspiration biopsy
in the diagnosis of complex thyroid nodules. J Clin Endocrinol
Metab. 86:4089–4091. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Quinn SF, Nelson HA and Demlow TA: Thyroid
biopsies: fine-needle aspiration biopsy versus spring-activated
core biopsy needle in 102 patients. J Vasc Interv Radiol.
5:619–623. 1994. View Article : Google Scholar : PubMed/NCBI
|