Introduction
Autoimmune hepatitis (AIH) is an unknown cause of
liver inflammation, and the diagnosis of AIH requires the presence
of characteristic clinical and laboratory features, and
histological abnormalities (1).
The incidence of AIH among white, Northern Europeans is 1.9 cases
per 100,000 people per year, and its point prevalence is 16.9 cases
per 100,000 people per year (2).
In the USA, AIH affects between 100,000 and 200,000 individuals
(3), and it accounts for 6% of
liver transplantations (4). The
frequency of AIH among patients with chronic liver disease in North
America is between 11 and 23% (5).
AIH should be considered in all individuals with acute and chronic
hepatitis with an undetermined cause (6). Clinical presentations of the disease
are variable, ranging from asymptomatic abnormal liver enzymes to
fulminant liver failure or advanced decompensated cirrhosis
(7). The frequency of cirrhosis at
presentation is >30% (8).
Concurrent immune disorders may mask the diagnosis of AIH. The
diagnostic criteria and scoring system for AIH were codified by an
international panel in 1993 (10)
and revised in 1999 (1).
In comparison with the age- and gender-matched
general population, with effective treatments available the
mortality of AIH is two-fold higher than that of the general
population (11,12). A long-term study reported that only
~40% of patients with AIH achieve complete remission (13). Traditionally, it was considered
that clinical and demographic factors were closely associated with
a poor outcome. Studies have reported that age distribution, serum
aspartate aminotransferase (AST), alanine aminotransferase (ALT)
and serum albumin levels were significant predictors of
liver-associated mortality or liver transplantation (14,15).
The majority of the current studies regarding the clinical
characteristics associated with a poor outcome have focused on
European and Japanese patients. Therefore, it is important to
identify the clinical manifestations found in Chinese patients with
AIH at various ages.
Patients and methods
Study population
Patients with AIH who were admitted to the Second
Xiangya Hospital (Changsha, China) between 2002 and 2013, and who
had complete clinical, laboratory and histological data, were
enrolled in this retrospective study. The diagnoses were based on
the 1999 revised criteria of the International Group of Autoimmune
Hepatitis (1). Liver biopsy
results were included if available, and two hepatopathologists
reviewed all liver tissue specimens. Those patients with
insufficient data for the diagnosis of AIH prior to treatment and
other liver diseases [viral hepatitis, Wilson’s disease,
non-alcoholic fatty liver disease (NFLD), primary biliary cirrhosis
(PBC) and primary sclerosing cholangitis (PSC)] were excluded from
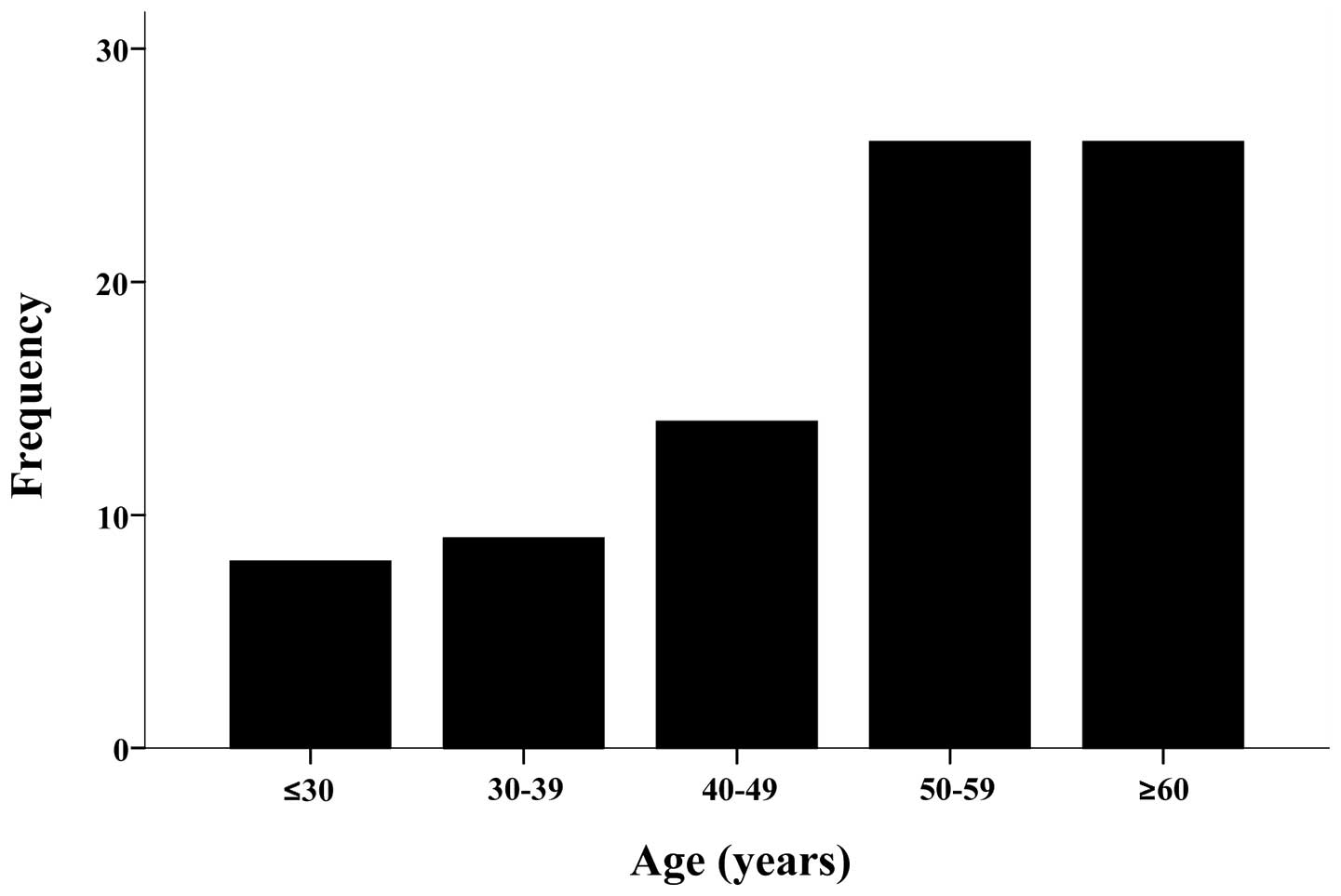
this study. Patients were categorized according to their age at
presentation into the following groups: ≤30 years, 31–39 years,
40–49 years, 50–59 years and ≥60 years. This study was approved by
The Ethics Committee of the Second Xiangya Hospital of Central
South University (Changsha, China). Informed consent was obtained
from all patients.
Clinical and laboratory assessments
Clinical examinations and conventional laboratory
tests were assessed prior to providing any specific therapy to the
patients. The presence of other concurrent autoimmune diseases was
also investigated. Liver function tests were performed, including
the measurements of the serum levels of alkaline phosphatase (ALP),
γ-glutamyl transpeptidase (γ-GT), AST, ALT, total bilirubin (TBIL)
and serum immunoglobulin G (IgG), by performing immunonephelometry
on all patients. Smooth muscle antibodies (SMA), antinuclear
antibodies (ANA), perinuclear antineutrophil cytoplasmic antibodies
(pANCA), antimitochondrial antibodies (AMA), antibodies to liver
kidney microsome type 1 (LKM1) and soluble liver
antigen/liver-pancreas antigen (SLA/LP) were evaluated using
indirect immunofluorescence. Each patient was seronegative for
AMA.
Statistical analysis
A descriptive analysis, including means, standard
deviation and frequencies, is presented. An independent sample
t-test was used to assess the correlation between continuous
variables and the χ2 test was used for the analysis of
categorical variables. P<0.05 was considered in indicate a
statistically significant difference. The SPSS statistical software
version 17.0 (SPSS, Inc., Chicago, IL, USA) was used for all
statistical analyses.
Results
Study population
A total of 83 Chinese patients fulfilled the 1999
revised criteria of the International Group of Autoimmune
Hepatitis; 41 patients (49.4%) were classified as ‘definite’ AIH
and 42 (50.6%) were classified as ‘probable’ AIH. At presentation,
the patients were graded according to their age. Patients aged ≤30
years (9.6%), 31–39 years (10.8%), 40–49 years (16.9%), 50–59 years
(31.3%) and ≥60 years (31.3%) with AIH were enrolled in the study.
In total, 26 patients (31.3%) were ≥60 years old. The mean age of
this group (the elderly population) was 65.62±4.92 years (range,
60–78 years) and the male to female ratio was 3:23. In total, 26
patients (31.3%) were aged between 50 and 59 years. The mean age
was 54.65±2.67 years and the male to female ratio was 2:24. A total
of eight patients (9.6%) constituted the young population, with the
mean age of 21.38±6.74 years (range, 10–30 years). The disease
frequency in each age range increased >40 years (Fig. 1), and the peak occurrences were in
the patients aged 50–59 years and in the elderly patients. Each
group was similar with regard to gender distribution.
Clinical presentation
The clinical manifestations of AIH are unspecific,
and other chronic liver diseases may have the same symptoms.
Anorexia, fatigue and jaundice were the most common symptoms
observed in >70% of the 83 patients. Furthermore, 15% presented
with a fever and ~10% of patients had pruritus. Overall, 76.9% of
patients presented with up to three symptoms, and 23.1% presented
with four symptoms. Liver cirrhosis was diagnosed in 10 (12%)
patients, among whom five patients (50%) were between the ages of
50 and 59 years and three patients (30%) were elderly. However, the
frequency of cirrhosis was not statistically different between the
elderly patients (≥60 years old) and the young patients (≤30 years
old) (P>0.05).
Laboratory data
The mean serum levels of liver function are
illustrated in Table I. Patients
aged ≤30 years (136.53±74.03 U/l, P=0.034) and aged 40–49 years
(147.43±52.71 U/l, P=0.021) presented with significantly lower
levels of of ALP than patients aged ≥60 years (238.78±163.29 U/l).
Patients aged ≤30 years (119.71±145.92 U/l) also presented with
significantly lower γ-GT levels compared with patients aged 50–59
years (257.69±175.56 U/l, P=0.037) and those aged ≥60 years
(253.27±193.96 U/l, P=0.043). Similarly, patients aged 31–39 years
(18.74±5.83 g/l) presented with significantly lower IgG levels than
those aged 50–59 years (25.41±6.05 g/l, P=0.049) and those aged ≥60
years (27.29±11.33 g/l, P=0.012). By contrast, patients aged ≤30
years (351.33±284.94 μmol/l) had significant higher TBIL levels
compared with those aged 31–39 years (116.46±106.09 μmol/l,
P=0.007), those aged 50–59 years (125.28±112.43 μmol/l, P=0.002)
and those aged ≥60 years (172.83±33.82 μmol/l, P=0.013).
 | Table IClinical features of 83 Chinese
patients with autoimmune hepatitis in each group. |
Table I
Clinical features of 83 Chinese
patients with autoimmune hepatitis in each group.
| Age category (years)
(n=83) |
|---|
|
|
|---|
| Features | ≤30 (n=8) | 31–39 (n=9) | 40–49 (n=14) | 50–59 (n=26) | ≥60 (n=26) |
|---|
| Female (n) | 5 | 6 | 13 | 24 | 23 |
| Age (years) | 21.3±6.7 | 37.4±1.9 | 45.9±2.8 | 54.6±2.6 | 65.6±4.9 |
| Cirrhosis (n) | 1 | 1 | 0 | 5 | 3 |
| ALT (U/l) | 151.8±133.7 | 312.2±338.4 | 288.5±233.5 | 384.2±397.7 | 287.9±288.4 |
| AST (U/l) | 193.6±147.9 | 422.9±596.9 | 353.0±314.1 | 385.7±367.1 | 310.6±213.1 |
| TBIL (μmol/l) | 351.3±284.9 | 116.5±106.1 | 203.5±224.9 | 125.3±112.4 | 172.2±172.8 |
| ALP (U/l) | 136.5±74.0 | 187.5±138.5 | 147.4±52.7 | 191.2±83.4 | 238.8±163.3 |
| γ-GT (U/l) | 119.7±145.9 | 161.5±95.1 | 135.8±81.7 | 257.7±175.6 | 253.3±194.0 |
| IgG (g/l) | 25.1±11.4 | 18.7±5.8 | 22.1±6.1 | 25.4±6.1 | 27.3±11.3 |
| ANA (≥1:40) | 5 | 3 | 7 | 17 | 19 |
In total, 51 of the 83 patients were positive for
ANA with a titer of ≥1:40. Among the elderly patients, 19 were
positive for ANA, while among the patients aged 50–59 years and ≤30
years, 17 and five patients were positive for ANA, respectively.
However, there were no differences in the positive proportions of
ANA among each group (Table
I).
Concurrent autoimmune diseases
Of the 26 elderly patients, 10 (59%) presented with
coexisting autoimmune diseases, including four patients with
Sjögren’s Syndrome, five patients with systemic lupus erythematosus
and one patient with ulcerative colitis. Similarly, 11 of the 26
patients aged 50–59 years presented with concurrent autoimmune
diseases (four patients with Sjögren’s Syndrome, two with
autoimmune thyroiditis and rheumatoid arthritis, and three with
systemic lupus erythematosus). Five of the eight younger patients
(aged ≤30 years) presented with concurrent autoimmune diseases (two
patients with autoimmune thyroiditis and systemic lupus
erythematosus, and one patient with rheumatoid arthritis). However,
the distribution of concurrent autoimmune diseases in each age
group was not statistically significant (P=0.398).
Discussion
In China, the etiology of chronic hepatitis is
mainly hepatitis virus infection. Since the recognition of
autoimmune liver diseases, these diseases have become one of the
major forms of non-viral chronic liver diseases in China. Studies
on the prevalence of Chinese patients with AIH are rare.
The present study investigated the differences
associated with age in the clinical and laboratory features of
Chinese patients with AIH diagnosed using the revised 1999 scoring
system (1). In this study, the age
of onset in Chinese patients showed that the peak occurrences of
AIH exist in the age groups of 50–59 years and ≥60 years, and there
are few young patients (9.6%) with AIH. The proportion of young
patients is smaller than in previous studies regarding Japanese
patients. The frequency of liver cirrhosis at first diagnosis of
AIH was <12%, lower than other studies where cirrhosis at
presentation was detected and reported in 27–42% of patients
(16,17).
The present study demonstrated that elderly patients
(≥60 years old) presented with higher serum ALP and γ-GT levels
compared with younger patients (≤30 years old). By contrast, the
young patients presented with higher TBIL levels compared with
elderly patients. This result indicated that patients aged ≤30
years may have more severe disease activity than elderly patients.
A previous study from Japan demonstrated that elderly patients
presented with more asymptomatic clinical features compared with
the young patients (17). The
results of the present study also suggested that elderly patients
may be misdiagnosed in the early stage due to the fact that they
may not exhibit any symptoms. This may be one of the reasons for
the prevalence of autoimmune diseases and the increased
presentation in elderly patients compared with younger patients in
China. However, the occurrence of cirrhosis in each group was
similar in the present study, and the rate was markedly lower
compared with groups of patients from North America (16) and Japan (17).
AIH is associated with a number of distinct
circulating autoantibodies. The most common autoantibodies are ANA
and SMA. It was revealed that 96% of adult patients with AIH from
North America had ANA and SMA (18). Anti-SLA/LP and pANCA may be useful
in identifying patients with AIH from those who lack typical
serological findings (19,20). Anti-SLA/LP are highly specific
markers of AIH and more commonly found in association with the
conventional autoantibodies; however, they also are occasionally
found in patients with AIH who are negative for ANA, SMA, and
anti-LKM1 (19). It has been
reported that anti-SLA are highly specific for the diagnosis of
autoimmune liver disease, and their detection may reveal patients
with a more severe degree of the disease and a worse predicted
outcome (21). pANCA are
non-specific, but are commonly present. They have been used to
reclassify patients with cryptogenic chronic hepatitis, such as
AIH; however, they have not been formally assimilated into the
diagnostic algorithm (20). In the
present study, we observed that ANA was the most common
autoantibody in Chinese patients with AIH. Among these Chinese
patients with AIH, 61.4% were ANA-positive. SLA/LP (14.5%) was
another common autoantibody. Serum levels of AST and IgG were found
to be higher in ANA-positive patients; however, there was no
statistically significant difference between patients who were
positive and negative for ANA, which was similar to a previous
Japanese study (22).
Concurrent immune disorders may mask the underlying
liver disease. Autoimmune thyroiditis, Graves’ disease, synovitis
and ulcerative colitis are the most common immune-mediated
disorders associated with AIH in adults from North America
(23). Notably, concurrent immune
diseases were more commonly observed in this group of Chinese
patients with AIH (42.2%) than in the group of patients from the
west (24). It has been reported
that associated autoimmune diseases were observed in 15–34% of
patients from the West (24). In
the present study it was observed that Sjögren’s Syndrome was the
most commonly associated autoimmune disorder. According to a
nationwide survey in Japan (22),
the prevalence of complicating Sjögren’s syndrome in patients with
AIH was ~10%. Czaja and Carpenter (16) reported that elderly patients
presented with concurrent thyroid and rheumatic diseases more often
than patients aged ≤30 years. Certain studies have suggested that
human leukocyte antigen DR4 occurred more frequently in elderly
patients. However, in the present study, autoimmune thyroiditis was
uncommon in elderly Chinese patients. The distribution of the human
leukocyte antigen is not fully recognized in China, and further
studies are required to analyze the human leukocyte antigen in
large number of patients with AIH.
A long-term study established that incomplete
normalization of ALT at 6 months, low serum albumin concentration
at diagnosis, and an age at presentation of <20 years or >60
years were significant independent predictors of a poor outcome
(15). However, histological
cirrhosis at diagnosis was not associated with a poor prognosis and
did not affect the response to initial immunosuppressive treatment.
In the present study, a considerable portion of patients with AIH
were aged >60 years, indicating a poor liver-associated outcome
under current management strategies. In addition, even when treated
with the usual management strategy, there is an increased risk that
extra-hepatic malignancy, such as skin (non-melanoma) and
hematological cancers, may be induced by immunosuppressive therapy.
Further studies should explore effective ways to improve the
survival of patients with AIH without increasing the risk of
extra-hepatic malignancy.
One of the limitations of the present study was the
relatively small number of patients; multicenter national data are
required. Moreover, the detection of HLA-DR3 and DR4 is rare in
China, and the results from the studies performed in other
countries have demonstrated that HLA status may affect clinical
manifestations, behavior and the outcome of treatment (16).
In conclusion, a substantial portion of patients
with AIH were >60 years old, indicating a poor liver-associated
outcome under current management strategies. Elderly patients
exhibited higher levels of ALP and γ-GT, and a lower TBIL level
than younger patients. Chinese patients with AIH had a lower
frequency of cirrhosis at presentation and a higher frequency of
concurrent autoimmune diseases compared with patients from Europe,
North America and Japan. However, the frequencies of cirrhosis,
concurrent autoimmune disease and autoantibodies were similar among
each group.
References
|
1
|
Alvarez F, Berg PA, Bianchi FB, et al:
International Autoimmune Hepatitis Group Report: review of criteria
for diagnosis of autoimmune hepatitis. J Hepatol. 31:929–938. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Seo S, Toutounjian R, Conrad A, et al:
Favorable outcomes of autoimmune hepatitis in a community clinic
setting. J Gastroenterol Hepatol. 23:1410–1414. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Czaja AJ: Autoimmune liver disease. Curr
Opin Gastroenterol. 19:232–242. 2003. View Article : Google Scholar
|
|
4
|
Wiesner RH, Demetris AJ, Belle SH, et al:
Acute allograft rejection: incidence, risk factors, and impact on
outcome. Hepatology. 28:638–645. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Feld JJ, Dinh H, Arenovich T, et al:
Autoimmune hepatitis: effect of symptoms and cirrhosis on natural
history and outcome. Hepatology. 42:53–62. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Czaja AJ: Diverse manifestations and
evolving treatments of autoimmune hepatitis. Minerva Gastroenterol
Dietol. 51:313–333. 2005.PubMed/NCBI
|
|
7
|
Floreani A, Niro G, Rosa Rizzotto E, et
al: Type I autoimmune hepatitis: clinical course and outcome in an
Italian multicentre study. Aliment Pharmacol Ther. 24:1051–1057.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Parker DR and Kingham JG: Type I
autoimmune hepatitis is primarily a disease of later life. QJM.
90:289–296. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ichai P, Duclos-Vallée JC, Guettier C, et
al: Usefulness of corticosteroids for the treatment of severe and
fulminant forms of autoimmune hepatitis. Liver Transpl.
13:996–1003. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Johnson PJ and McFarlane IG: Meeting
report: International Autoimmune Hepatitis Group. Hepatology.
18:998–1005. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ngu JH, Gearry RB, Frampton CM, et al:
Mortality and the risk of malignancy in autoimmune liver diseases:
a population-based study in Canterbury, New Zealand. Hepatology.
55:522–529. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hoeroldt B, McFarlane E, Dube A, et al:
Long-term outcomes of patients with autoimmune hepatitis managed at
a nontransplant center. Gastroenterology. 140:1980–1989. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Manns MP, Woynarowski M, Kreisel W, et al:
Budesonide induces remission more effectively than prednisone in a
controlled trial of patients with autoimmune hepatitis.
Gastroenterology. 139:1198–1206. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Al-Chalabi T, Underhill JA, Portmann BC,
et al: Effects of serum aspartate aminotransferase levels in
patients with autoimmune hepatitis influence disease course and
outcome. Clin Gastroenterol Hepatol. 6:1389–1395. 2008. View Article : Google Scholar
|
|
15
|
Ngu JH, Gearry RB, Frampton CM and Stedman
CA: Predictors of poor outcome in patients with autoimmune
hepatitis: A population-based study. Hepatology. 57:2399–2406.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Czaja AJ and Carpenter HA: Distinctive
clinical phenotype and treatment outcome of type 1 autoimmune
hepatitis in the elderly. Hepatology. 43:532–538. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miyake Y, Iwasaki Y, Takaki A, et al:
Clinical features of Japanese elderly patients with type 1
autoimmune hepatitis. Intern Med. 46:1945–1949. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Czaja AJ: Behavior and significance of
autoantibodies in type 1 autoimmune hepatitis. J Hepatol.
30:394–401. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Baeres M, Herkel J, Czaja AJ, et al:
Establishment of standardised SLA/LP immunoassays: specificity for
autoimmune hepatitis, worldwide occurrence, and clinical
characteristics. Gut. 51:259–264. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zauli D, Ghetti S, Grassi A, et al:
Anti-neutrophil cytoplasmic antibodies in type 1 and type 2
autoimmune hepatitis. Hepatology. 25:1105–1107. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Czaja AJ, Donaldson PT and Lohse AW:
Antibodies to soluble liver antigen/liver pancreas and HLA risk
factors for type 1 autoimmune hepatitis. Am J Gastroenterol.
97:413–419. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Toda G, Zeniya M, Watanabe F, et al:
Present status of autoimmune hepatitis in Japan - correlating the
characteristics with international criteria in an area with a high
rate of HCV infection. Japanese National Study Group of Autoimmune
Hepatitis. J Hepatol. 26:1207–1212. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Czaja AJ and Freese DK; American
Association for the Study of Liver Disease. Diagnosis and treatment
of autoimmune hepatitis. Hepatology. 36:479–497. 2002. View Article : Google Scholar
|
|
24
|
Krawitt EL: Autoimmune hepatitis. N Engl J
Med. 354:54–66. 2006. View Article : Google Scholar
|