Introduction
Among the studies on chronic lumbosacral pain
(1), lower lumbar instability
(2) has attracted much clinical
attention. Since Scheufler et al(3) reported that segmental instability is
caused by the degeneration of the fibrous ring-nucleus pulposus
complex in 1944, the diagnostic criteria for lower lumbar
instability has been more consistently defined (4) as the appearance of anomalies in the
lower lumbar spine (L3-S1) and corresponding
clinical symptoms and imaging changes in the motion segment under a
normal physiological workload. Lower lumbar instability is
clinically characterized by the following: lower back pain with hip
and lower limb referred pain; sudden pain in the waist due to
changes in position; stiff and blocked stair-stepping or excessive
activity in the spinous process when standing; intermittent
claudication; myasthenia in the lower limbs, and defecation and
urination obstructions in seriously affected patients. The
comparison of lumbar dynamic position radiographs in hyperextension
and hyper-flexion positions is an important factor in diagnostic
imaging. Lumbar X-ray radiographs in hyperextension and
hyperflexion positions suggest that the L3–5 segments
slide forward and back by >3 mm and the
L5-S1 segments slide by >4–5 mm. The angle
changes of the endplate are >10°, suggesting lower lumbar
instability (5). den Boer et
al(6) identified that lumbar
instability and lumbar segmental degeneration are characterized by
abnormal stress distribution of the nuclear-fiber ring, loose
column ligaments and repeated sprains, which explains the
pathogenesis of the usually merged lumbar intervertebral disc
herniation. The authors also highlighted the clinical significance
of lumbar mechanism dysfunction of the three columns on the
pathogenesis of lumbar degenerative instability and lower lumbar
instability in iatrogenic surgery and emphasized the necessity of
maintaining the stability of the three columns in treatment.
Another study (7) reported that
the surgical approach for conventional posterior lumbar
decompression and fusion is typically omniposterior resection.
Intra-operative vertebral laminae, spinous processes and other
important posterior column structures should receive wide excision.
However, the view of decompression in minimally invasive surgery
(8) is less clear than that in
open surgery and has a number of disadvantages, including
incomplete spinal decompression, potential vice injury risk, a
steep learning curve and the requirement for special equipment.
Extensive experience of open surgery is also required. All these
factors are unfavorable for the clinical application of minimally
invasive surgery. A total of 48 patients with lower lumbar
instability received posterior lumbar interbody fusion (PLIF) via
bilateral vertebral lamina fenestration using a threaded fusion
cage (TFC) from 2006 to 2009. The surgery retained the spinous
process and posterior longitudinal ligament. It is a practical
procedure with a good curative effect and indicates that surgical
methods for lower lumbar instability may simultaneously achieve the
important clinical aims of strong fusion, complete decompression
and stability maintenance of the three columns.
Materials and methods
General data
Among the 48 patients, 27 were males and 21 were
females, aged 47–72 years, with an average age of 62.3 years. These
patients had disease durations from 3 months to 15 years, with an
average of 2.6 years. All cases had varying degrees of chronic
lumbosacral pain which was aggravated after standing or walking for
a long time, and was not relieved following conservative clinical
treatment. The study included 25 cases of intermittent
claudication, 36 cases of unilateral lower limb pain and reduced
muscle strength, 8 cases of bilateral lower limb pain and reduced
muscle strength, 32 cases of restricted lower limb tendinous reflex
and 1 case of defecation and urination obstructions. This study was
conducted in accordance with the Declaration of Helsinki and with
approval from the Ethics Committee and the Institutional Review
Board (IRB) of the First Affiliated Hospital of Soochow University.
Written informed consent was obtained from all participants.
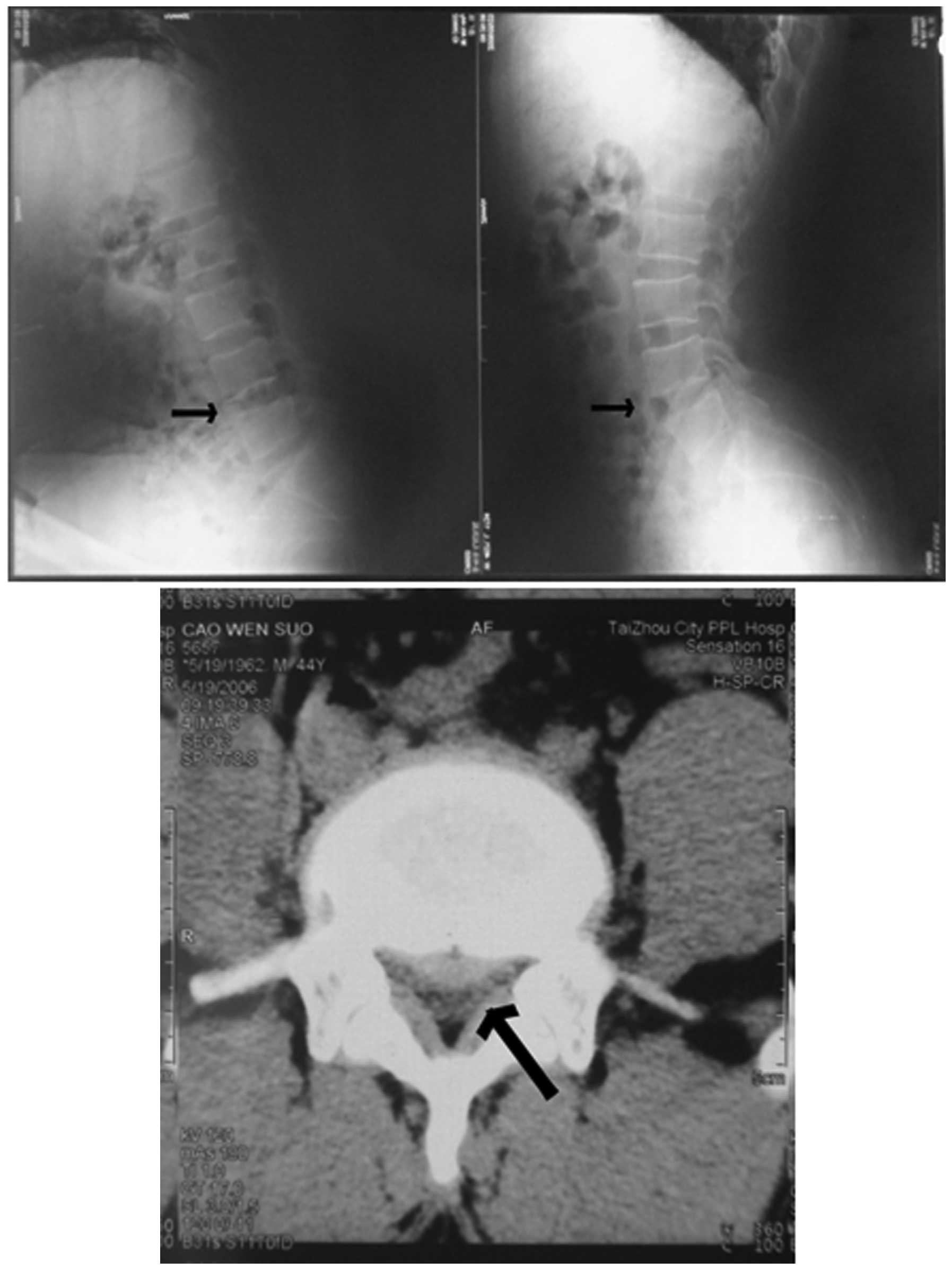
Imaging diagnosis
All patients received lumbar spine X-ray radiographs
(in the normotopia and lateral positions), computed tomography (CT)
and magnetic resonance imaging (MRI) examination. The results
indicated that the 48 cases of lumbar disc herniation combined with
intervertebral lesion were all suppressed by the dural sac and
nerve root. Of these, there were 35 cases of single-level lesions,
9 cases of double-level lesions and 4 cases of triple-level
lesions. The side with central-type disc herniation and
intervertebral lesion was in the right sternum in 46 patients and
19 patients had partial lateral central-type disc herniation.
Furthermore, 32 cases of lumbar degeneration, 27 cases of small
joint hyperplasia, 8 cases of longitudinal ligament ossification, 1
case of disconnected vertebral arch, 2 cases of spondylolisthesis I
and 1 case of spondylolisthesis II were observed. Comparison of
lumbar dynamic position radiographs of L3-S1
in the hyperextension and hyperflexion position demonstrates that
the inferior margin shift of the adjacent vertebra of the
intervertebral lesion was >4 mm and the angle change between the
adjacent inferior margin of the inferior vertebra and the superior
margin of the inferior vertebra was >10°. The intervertebral
lesion was consistent with the nerve compression (Fig. 1) and was diagnosed as lower lumbar
instability type I. The intervertebral lesion characterized by type
I, combined with lumbar spondylolisthesis I–II, was diagnosed as
type II. Among the cases in this study, 45 patients were diagnosed
as type I and 3 patients as type II.
Surgical method
Patients received lumbar anesthesia or general
anesthesia in the prone position and conventional sterile surgery,
with padded thorax and abdomen. The intervertebral lesion was
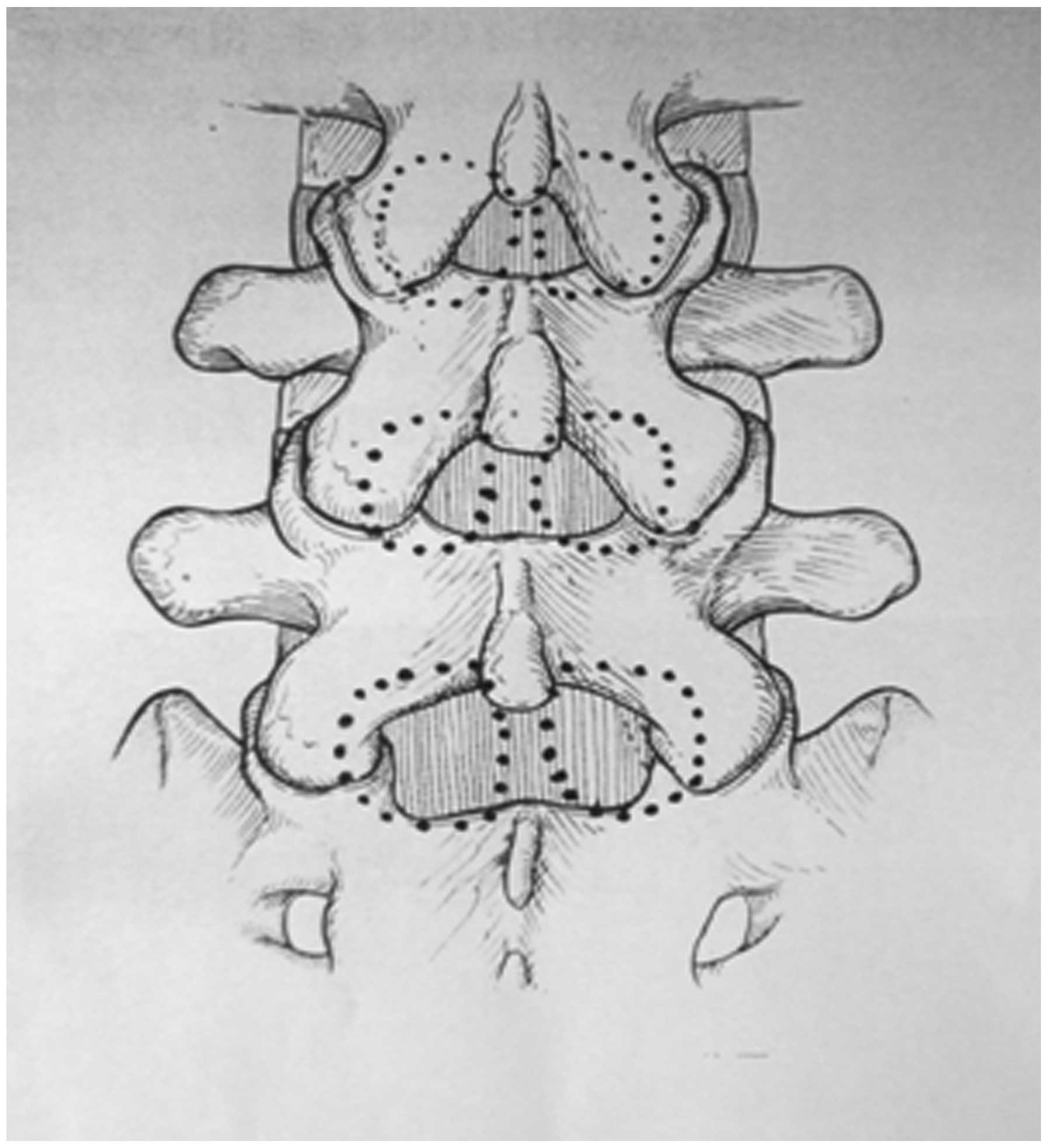
exposed in a median incision of the posterior lumbar. According to
the pre-operative CT and MRI, the herniated disk side was operated
on first. Following the removal of the 1/2 to 1/3 of the interior
small joint, adjacent lamina margin and its ligamentum flavum,
undercutting decompression was performed in the nerve root canal
and spinous basal parts. Ligamentum flavum in the lateral spinal
canal was carefully removed to form the bone window with a diameter
of 14–18 mm (Fig. 2). After the
tensions of the nerve root and dural sac were significantly
reduced, the intervertebral lesion was protected and led to the
middle. Following this, the fiber ring was cut and excision of the
nucleus pulposus was performed. The other side underwent the same
surgery. The spinal canal was flushed with ice-cold normal saline
(NS). Compression factors such as osteophytes of vertebrae
posterior margin, longitudinal ligament after ossification and
ligamentum flavum in small joint were detected and removed, to
avoid damage to epidural venous plexus. The TFC surgery protection
sleeve was placed on one side of the bone window. Under the
guidance of a C-arm X-ray machine, the superior and inferior
cartilage boards of the clearance were removed with a special
cutter. A TFC filled with crushed bones was implanted into a
suitable location, with a diameter of 10–14 mm and a length of
20–25 mm. The posterior margin was usually located at 3–5 mm before
the posterior margin of the vertebrae. The bones may be
reconditioned by the crushed bones in the margins of the small
joints, vertebral lamina and spinous processes cut off during
decompression. The other side underwent the same surgery. The TFC
in each side was attended to, to ensure that it avoided crossing
the center line of the clearance. Another ice-cold NS flushing and
spinal canal detection were carried out to remove the residual
cartilage fragments and nucleus pulposus. A poly(d,l-lactic acid)
absorbable anti-adhesive membrane was used to cover the bone window
and close the incision. One drainage tube was placed in each side
of the incision and removed after 48–72 h, depending on the lead
flow. The pedicle screw and connecting longitudinal stem of the
bilateral vertebra of the lesion clearance were placed first in
type II patients. The reduction of spondylolisthesis, as well as
appropriate lesion clearance and fixation, was followed by
decompression via vertebral lamina fenestration for TFC fusion.
Results
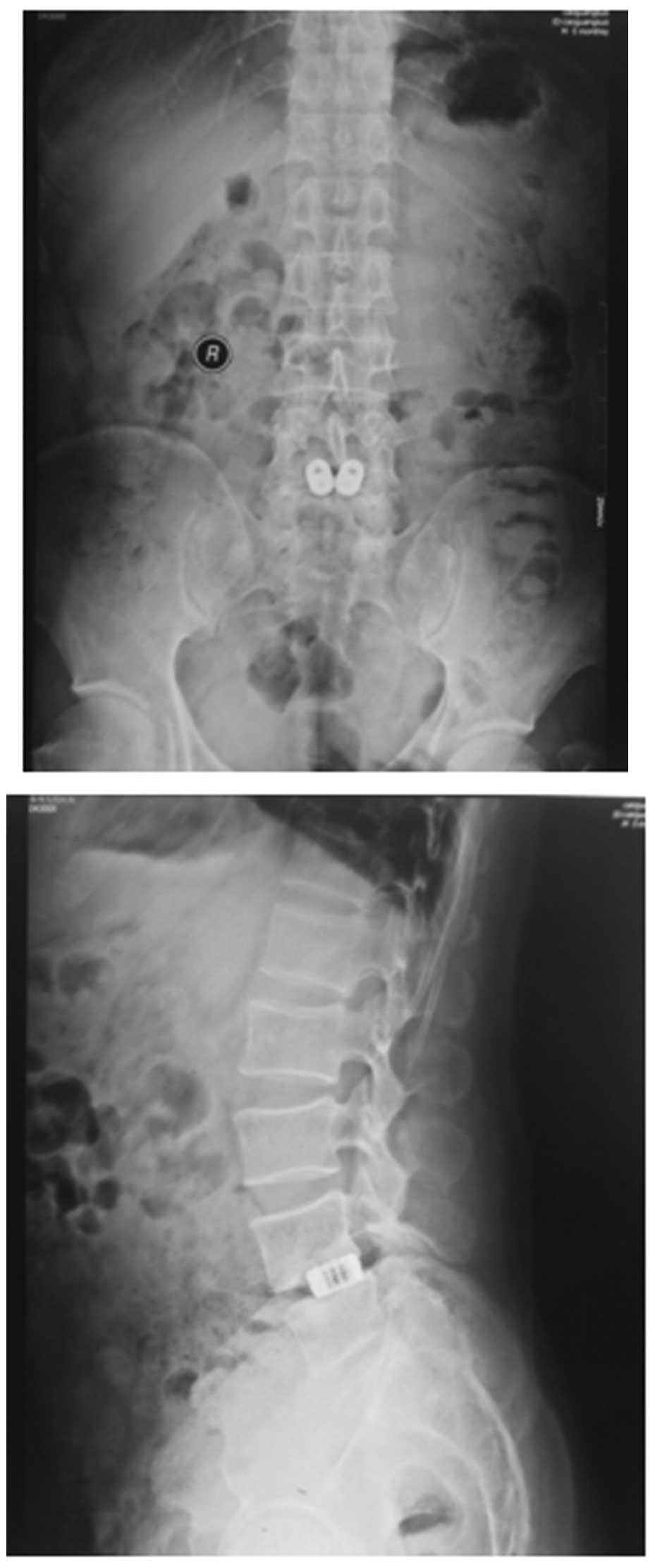
Bridwell method evaluation
All patients received follow-up for a period of 20
months to 3 years, with an average of 26.4 months. The method
created by Bridwell et al(9) was used to evaluate the lumbar fusion
conditions. The X-ray radiographs one year after surgery suggested
that the fusion rate between intervertebral grade I and II was
88.1%. At two years post-surgery, the fusion rate between
intervertebral grades I and II was 100% (Fig. 3),. Two cases of mildly reduced
intervertebral space height were observed; however, the reduction
was <10%.
Macnab curative effect
Functional recovery is the curative effects
evaluated by the improved Macnab criteria, as follows. Optimal
effects: disappearance of pain, no motor dysfunction, and a return
to work and activities; good effects: occasional pain,
disappearance of main symptoms, normal muscle strength, a negative
result in the straight legs raising test and femoral nerve stretch
test, light physical labor is tolerable; passable effects: symptoms
are improved but pain persists, and patients are capable of looking
after themselves in their daily life although unable to work; poor
effects: patients suffer nerve compression and require further
surgery. Using these criteria, in our study a total of 42 cases
(87.5%) were optimal, 5 cases (10.4%) were good and 1 case (2.0%)
was passable. All cases exhibited relieved lower limb pain and the
back pain relief rate was 97.9%. One patient demonstrated mild
cerebrospinal leakage in the incision 7 days after surgery; this
healed well after local processing and the stitches were removed
after 3 weeks. One type II case exhibited repeated left waist pain
from six months after surgery. The 14 month post-operative X-ray
radiographs suggested good interbody fusion; however, the pedicle
screw system was loosened and the back pain was relieved following
its removal.
Discussion
Lower lumbar instability is usually accompanied by
lumbar disc herniation, lumbar spondylolisthesis and segmental
lumbar spinal stenosis. With the exception of a few cases with mild
symptoms and short attacks who received conservative treatments for
short-term relief, all cases suffered repeated attacks and curing
the disease was difficult. These patients demonstrated clear
surgical indications and were suitable candidates for lumbar fusion
(10). This study aimed to achieve
lower lumbar fusion stability and spinal canal decompression,
eliminate nerve compression syndrome, restore the normal spinal
mechanism of balance, preserve the spinal physiological function
and delay the degenerative trend of the adjacent normal lumbar
segments. Particularly in those aged >35 years with lumbar disc
herniation, the abnormal activities of motion segments indicated by
lumbar dynamic position radiographs should be considered as
absolute indications of lumbar fusion during nucleus pulposus
enucleation. Otherwise post-operative lumbar spinal instability may
be aggravated. The three columns of the spine should be kept stable
for spinal decompression. Ray (11) reported 208 cases of PLIF using TFC
with a three year follow-up and identified a bone fusion rate of
96%. The author indicated that vertebral fusion using TFC is based
on full decompression of the lumbar spinal canal. This is
characterized by the inclusion of a large number of micropores and
locally implanted, autologous cancellous bone providing a large
fusion area, as well as equal and partial loading of the spinal
load, reducing axial shear. As a result, PLIF using TFC has become
a common surgical procedure in the treatment of lumbar instability,
due to the improved fusion effect compared with that of traditional
lumbar fusion (12).
In observational studies of PLIF using TFC and other
inter-body fusion cages in the treatment of lumbar instability
(13), several scholars identified
that the vertebral fusion rate and rate of clinical symptom
improvement are variable, with possible adverse complications,
including loose or slipped fusion cages, fusion failure and
aggravated lumbar and spinal instability. Several clinical
observations (14) suggested that
these adverse complications may be related to the different
approaches used in implanting fusion cages with spinal
decompression. A clinical study (15) demonstrated that patients with lower
lumbar spinal instability should preferentially receive fusion and
stability surgery. However, patients are often admitted with
long-term degeneration of stability and significant spinal
stenosis. Therefore, they should receive spinal canal decompression
surgery at the same time. The strong fusion and complete
decompression in the treatment of lumbar spinal instability and
surgical decompression, which maintains spinal stability, should be
used if possible (16),
particularly in the protection or persistence of the posterior
column. Furthermore, the ‘limited surgery approach’ should be
advocated to reduce the iatrogenic instability factors and provide
the best anatomical and biomechanical foundation for effective
vertebral interbody fusion. Martin et al(17) reported that, the spinal
decompression and implantation in PLIF were mainly used in
laminectomy or hemilaminectomy, with postoperative apparently
damaged stability of central and posterior column and exposed dural
sac. The external surface of the latter is vulnerable to adhesion
compression of the erector spinae and dural fiber scarring
following surgery (18).
Iatrogenic injury of the lumbar spinal stability mechanism, as well
as the damaged anterior fiber ring and posterior longitudinal
ligament, which increase the tendency of spinal pivoting and
slipping, should be regarded as important signs of post-operative
poor fusion and incompletely improved symptoms. Bilateral
decompression via vertebral lamina fenestration for TFC fusion was
combined with the principle of minimizing damage using minimally
invasive surgery (19) to further
retain the three column frame of the spine. This fulfils the
limited surgery approach, as well as thorough spinal decompression
and effective vertebral interbody fusion.
A related study (20) demonstrated that the clearance of
the L3–5 bilateral articular processes of an adult are
on average 33.5, 40.1 and 47.4 mm, respectively. With the addition
of a conventional resection of 1/3-1/2 inside the small joint for
intra-operative decompression, the diameter of the general bone
window is 14–18 mm and the area is 2.4–3.0 mm2. The full
spinal undercutting decompression (21) requires careful surgery. The proper
usage of TFC input protection devices is able to perfectly resolve
the contradiction between the ‘limited approach’ and the exposed
operative field to avoid nerve damage, iatrogenic instability and
other adverse complications. The treatment requires the following:
i) surgical personnel should coordinate with each other and
strictly abide by the surgical programs step by step. The surgeon
must have a good understanding of the lumbar spinal anatomical
structure and have considerable experience of lumbar spine surgery.
Intra-operatively, a good operative field should be exposed and in
each step the regional anatomy of the lumbar spine should be
considered (22). The adverse
complications of nerve injury may be avoided through accurate and
careful surgery, as well as coordination during surgery. Our study
had 1 case of post-operative mild cerebrospinal leakage, which was
related to spinal adhesion caused by serious compression and
repeated loosening, separation and complete removal of epidural
band cicatrix, without nervous dysfunction following post-operative
controversial treatment. ii) Accurate fenestration and full
decompression are the keys to successful surgery. During
fenestration, the position and direction of the vertebral
clearance, as well as the correlation between vertebral clearance
and the laminal clearance should be given attention. The window
formed was quasi-circular, with a larger transverse diameter,
beneficial for the placement of the nerve hook and TFC protection
devices. Part of the cortex in the basilar section of the spinous
process may be removed to allow fenestration. Following
fenestration, full undercutting decompression should be performed,
with equal attention given to the central spinal canal and nerve
root canal, particularly for the removal of pressure factors,
including ossified posterior longitudinal ligament, hyperplastic
osteophytes in the posterior vertebrae, medial margin of cohered
and hyperplastic articular process, narrow parapsidal furrow of the
superior articular process and a hyposulculus in the pedicle of the
vertebral arch, lateral recess and lateral ligament flavum
(21). While removing the osseous
oppression, the soft pressure factors of the nucleus pulposus, the
organized, calcified or hypertrophic fibers of the ligament fiavum
and the posterior longitudinal ligament should not be ignored.
During the decomposition of the adhesion, the integrity of the
dural sac should be maintained. The spinal canal should be checked
again after placing the TFC, removing iatrogenic pressure factors,
including fiber ring debris of the nucleus pulposus and crushed
bones from the resection of the lamina. iii) Correct understanding
of the placing of the TFC. Reduced resection of the vertebral
lamina preserves the structure of the posterior column, without the
increased difficulty in the full exposure of the spinal canal.
Following accurate fenestration, full undercutting decompression
and dealing with the basal part of the spinous process, the spinal
canal may be well-exposed. Following exploration of the spinal
canal and confirmation that the dural sac and nerve root have been
relieved from compression and fully loosened, the neural hook and
TFC protection devices may be properly placed. The C-arm X-ray
machine is used to monitor and distinguish the direction and depth
of the intervertebral disc space. According to pre-operative
assessment, a TFC with appropriate length and diameter is selected
to quickly and efficiently complete the vertebral fusion with its
self-drilling screw structure (23). iv) Adhesion around the spinal canal
should be actively prevented. Ice-cold NS is used intra-operatively
for flushing, which reduces hemorrhage and reactive edema, as well
as cicatrix in the spinal canal. While closing the spinal canal,
poly(d,l-lactic acid) is conventionally used to absorb the medical
film and close the bone window. This material accords with the
requirement to avoid epidural adhesion (24), without damaging or stimulating
tissues. This material has a microporous structure and good
adhesion and does not need to be sutured and fixed; therefore, it
is maintained in the body for ∼2 months and completely absorbed and
degraded within 6 months. The final degradation products are water
and carbon dioxide. Therefore, this material is used to close the
bone window as a membranous barrier and reduce the mechanical
stimulus of cicatrix outside the spinal canal and adhesion to the
dural sac.
In summary, the final purpose in the treatment of
lower lumbar spinal instability was lumbar spinal osseous fusion
and long-term stability. Clinical study has indicated that the PLIF
technology demonstrates a better accordance with the natural
biomechanical features of the lumbar spine (25). If bilateral decompression via
vertebral lamina fenestration is performed, the principle of
vertebral pressure support and the tension band principle of
posterior structures (26) is
effectively protected. This is ideal to achieve a steady vertebral
interbody fusion and effective spinal decompression, which is
significant for developing a lumbar spinal fusion procedure that is
effective, minimally invasive and normalizing at a reduced cost.
Further studies with numerous centers and related multiple factor
analysis, including ethnicity, physique, pathogenesis and spinal
canal forms, would aid the treatment of lower lumbar spinal
instability by combining the ‘limited surgical approach’ with
effective decompression and fusion.
References
|
1.
|
Du Bois M, Szpalski M and Donceel P:
Patients at risk for long-term sick leave because of low back pain.
Spine J. 9:350–359. 2009.PubMed/NCBI
|
|
2.
|
Müslüman AM, Yılmaz A, Cansever T, et al:
Posterior lumbar interbody fusion versus posterolateral fusion with
instrumentation in the treatment of low-grade isthmic
spondylolisthesis: midterm clinical outcomes. J Neurosurg Spine.
14:488–496. 2011.
|
|
3.
|
Scheufler KM, Dohmen H and Vougioukas VI:
Percutaneous transforaminal lumbar interbody fusion for the
treatment of degenerative lumbar instability. Neurosurgery. 60(4
Suppl 2): 203–212. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Ledet EH, Tymeson MP, Salerno S, Carl AL
and Cragg A: Biomechanical evaluation of a novel lumbosacral axial
fixation device. J Biomech Eng. 127:929–933. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Iguchi T, Kanemura A, Kasahara K, et al:
Lumbar instability and clinical symptoms: which is the more
critical factor for symptoms: sagittal translation or segment
angulation? J Spinal Disord Tech. 17:284–290. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
den Boer JJ, Oostendorp RA, Beems T,
Munneke M, Oerlemans M and Evers AW: A systematic review of
bio-psychosocial risk factors for an unfavourable outcome after
lumbar disc surgery. Eur Spine J. 15:527–536. 2006.PubMed/NCBI
|
|
7.
|
Hsieh MK, Chen LH, Niu CC, Fu TS, Lai PL
and Chen WJ: Postoperative anterior spondylediscitis after
posterior pedicle screw instrumentation. Spine. 11:24–29. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Villavicencio AT, Burneikiene S, Roeca CM,
Nelson EL and Mason A: Minimally invasive versus open
transforaminal lumbar interbody fusion. Surg Neurol Int. 1:122010.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Bridwell KH, Lenke LG, McEnery KW, Baldus
C and Blanke K: Anterior fresh frozen structural allografts in the
thoracic and lumbar spine. Do they work if combined with posterior
fusion and instrumentation in adult patients with kyphosis or
anterior column defects? Spine (Phila Pa 1976). 20:1410–1418. 1995.
View Article : Google Scholar
|
|
10.
|
Delawi D, Dhert WJ, Castelein RM, Verbout
AJ and Oner FC: The incidence of donor site pain after bone graft
harvesting from the posterior iliac crest may be overestimated: a
study on spine fracture patients. Spine (Phila Pa 1976).
32:1865–1868. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Ray CD: Threaded fusion cages for lumbar
interbody fusions. An economic comparison with 360 degrees fusions.
Spine (Phila Pa 1976). 22:681–685. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Zhao J, Zhang F, Chen X and Yao Y:
Posterior interbody fusion using a diagonal cage with unilateral
transpedicular screw fixation for lumbar stenosis. J Clin Neurosci.
18:324–328. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Rodgers WB, Gerber EJ and Patterson J:
Intraoperative and early postoperative complications in extreme
lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa
1976). 36:26–32. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Oppenheimer JH, DeCastro I and McDonnell
DE: Minimally invasive spine technology and minimally invasive
spine surgery: a historical review. Neurosurg Focus. 27:E92009.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Hu MW, Liu ZL, Zhou Y, Shu Y, Chen CL and
Yuan X: Posterior lumbar interbody fusion using spinous process and
laminae. J Bone Joint Surg Br. 94:373–377. 2012.PubMed/NCBI
|
|
16.
|
Shunwu F, Xing Z, Fengdong Z and Xiangqian
F: Minimally invasive transforaminal lumbar interbody fusion for
the treatment of degenerative lumbar diseases. Spine (Phila Pa
1976). 35:1615–1620. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Martin BI, Mirza SK, Comstock BA, Gray DT,
Kreuter W and Deyo RA: Are lumbar spine reoperation rates falling
with greater use of fusion surgery and new surgical technology?
Spine (Phila Pa 1976). 32:2119–2126. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Songer MN, Ghosh L and Spencer DL: Effects
of sodium hyaluronate on peridural fibrosis after lumbar laminotomy
and discectomy. Spine (Phila Pa 1976). 15:550–554. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Kim CW, Siemionow K, Anderson DG and
Phillips FM: The current state of minimally invasive spine surgery.
J Bone Joint Surg Am. 93:582–596. 2011.PubMed/NCBI
|
|
20.
|
Jindal G and Pukenas B: Normal spinal
anatomy on magnetic resonance imaging. Magn Reson Imaging Clin N
Am. 19:475–488. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Lakkol S, Bhatia C, Taranu R, Pollock R,
Hadgaonkar S and Krishna M: Efficacy of less invasive posterior
lumbar interbody fusion as revision surgery for patients with
recurrent symptoms after discectomy. J Bone Joint Surg Br.
93:1518–1523. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Brotis AG, Paterakis KN, Tsiamalou PM,
Fountas KN, Hahjigeorgiou GM and Karavelis A: Instrumented
posterior lumbar fusion outcomes for lumbar degenerative disorders
in a southern European, semirural population. J Spinal Disord Tech.
23:444–450. 2010. View Article : Google Scholar
|
|
23.
|
Vishteh AG, Crawford NR, Chamberlain RH,
et al: Biomechanical comparison of anterior versus posterior lumbar
threaded interbody fusion cages. Spine (Phila Pa 1976). 30:302–310.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Songer MN, Rauschning W, Carson EW and
Pandit SM: Analysis of peridural scar formation and its prevention
after lumbar laminotomy and discectomy in dogs. Spine (Phila Pa
1976). 20:571–580. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Kasis AG, Marshman LA, Krishna M and
Bhatia CK: Significantly improved outcomes with a less invasive
posterior lumbar interbody fusion incorporating total facetectomy.
Spine (Phila Pa 1976). 34:572–577. 2009. View Article : Google Scholar
|
|
26.
|
Mladenov KV, Vaeterlein C and Stuecker R:
Selective posterior thoracic fusion by means of direct vertebral
derotation in adolescent idiopathic scoliosis: effects on the
sagittal alignment. Eur Spine J. 20:1114–1117. 2011. View Article : Google Scholar
|