Introduction
Early gastric cancer (EGC) is defined as gastric
cancer that is confined to the mucosa or submucosa (T1 cancer),
irrespective of the presence of regional lymph node metastases
(1). In 1995, it was reported that
almost 10,000 cases of EGC are detected annually in Japan,
accounting for 40–50% of all gastric cancers (2).
Endoscopic submucosal dissection (ESD) is widely
recognized as a safe and effective treatment for EGC (3–6).
However, little information is available concerning the long-term
outcomes of ESD in large numbers of patients.
The gold standard study design for evaluation of the
efficacy of endoscopic treatment of EGC is a long-term,
large-scale, randomized controlled trial. The excellent prognosis
following surgical treatment of EGC, particularly in cases
indicated for endoscopic resection, makes randomized controlled
trials unethical. Therefore, the feasible evidence of the efficacy
of EMR/ESD comes from long-term clinical follow-up data.
In the present study, the clinical outcomes of a
large number of patients with EGC who underwent ESD were
investigated.
Patients and methods
Patients
A total of 1,332 EGCs in 1,209 consecutive patients
were treated by ESD at the affiliated hospitals of Nagasaki
University Hospital from January 2001 to December 2010. The
indications for ESD were determined by the presence or absence of
nodal metastasis (7–9) and according to the criteria for
endoscopic resection proposed in the Treatment Guidelines for
Gastric Cancer in Japan (10). The
indication criteria were defined as differentiated-type mucosal
cancer without ulceration, ≤20 mm in diameter. The
expanded-indication criteria were defined as follows:
Differentiated-type mucosal cancer without ulceration, irrespective
of tumor size; differentiated-type mucosal cancer with ulceration,
≤30 mm in diameter; differentiated-type minute (<500 μm from the
muscularis mucosae) submucosal invasive cancer, ≤30 mm in diameter;
and undifferentiated-type mucosal cancer without ulceration, ≤20 mm
in diameter with no lymphovascular involvement. The
out-of-indication criteria were defined as EGCs that did not meet
the indication criteria or the expanded-indication criteria.
Written informed consent was obtained from each patient.
ESD
The EGCs were first identified and demarcated using
white-light endoscopy and chromoendoscopy with indigo carmine
solution, after which marking around the lesions was performed by
cautery with a needle knife. Glycerol (10% glycerol and 5%
fructose; Chugai Pharmaceutical Co. Ltd., Tokyo, Japan) or
MucoUp® (Johnson and Johnson Co. Ltd., Tokyo, Japan)
were then injected into the submucosal layer to lift the mucosa. A
circumferential mucosal incision was made around the lesion using
an insulation-tipped (IT) Knife 2 (Olympus Medical Systems Corp.,
Tokyo, Japan) or a Flush Knife (Fujifilm Corp., Tokyo, Japan).
Submucosal dissection was performed using the IT Knife 2, a Hook
Knife (Olympus Medical Systems Corp.) or the Flush Knife to achieve
complete removal of the lesion. High-frequency generators (ICC 200
or VIO 300D; ERBE Elektromedizin GmbH, Tübingen, Germany) were used
during marking, incision of the gastric mucosa and exfoliation of
the gastric submucosa.
Early outcomes
Early outcomes (perforation, bleeding rate and
curability) were assessed for the 1,332 EGCs in the 1,209
consecutive patients. The patients included 882 men and 327 women,
with a mean age of 72 years (range, 33–95 years). Perforation was
diagnosed endoscopically or by the presence of free air on an
abdominal plain radiograph or computed tomography scan.
Procedure-associated bleeding was defined as bleeding that required
transfusion or surgical intervention, or bleeding that caused the
hemoglobin level to decrease by 2 g/dl (11).
En bloc resection refers to a resection in
one piece (11). The curability of
ESD was classified as either curative or non-curative (11,12).
Resections were deemed curative when a tumor was excised en
bloc and was within the indication or expanded-indication
criteria with tumor-free lateral and vertical margins and no
lymphovascular invasion. When histological evaluation was
challenging or identified that a lesion was outside the indication
or expanded-indication criteria and/or that it had a positive
margin or lymphovascular invasion, the curability was defined as
non-curative.
Long-term outcomes
Long-term outcomes were assessed for a total of 342
EGCs in 319 consecutive patients treated using ESD from January
2001 to December 2005. The follow-up was conducted >5 years
after the procedure. The patients included 224 men and 95 women,
with a mean age of 71 years (range, 33–92 years). Nineteen patients
had multiple EGCs with a total of 42 lesions. In the analysis of
long-term outcomes, 300 patients were enrolled due to the exclusion
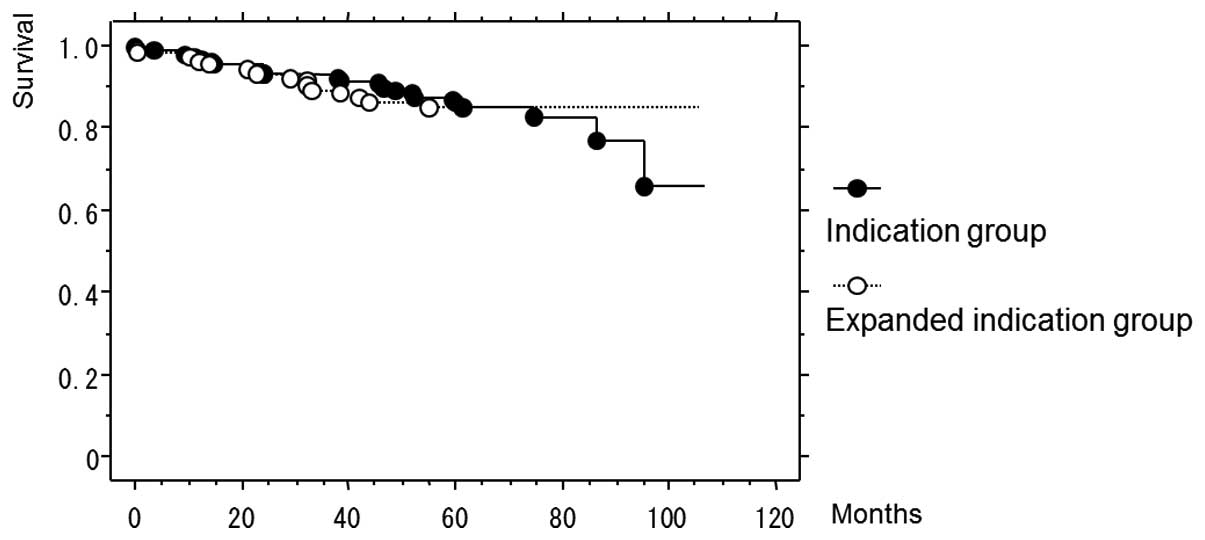
of the 19 patients with multiple EGCs. The overall survival rates
were compared between the indication and expanded-indication
groups, and between the patients who did or did not undergo
additional surgery in the out-of-indication group. The overall
survival rates among different age groups were also compared.
Statistical analysis
The statistical significance of the differences with
respect to each complication was determined using Fisher’s exact
test or the χ2 test. Data for the long-term outcomes
were calculated using the Kaplan-Meier method and analyzed by the
log-rank test. P<0.05 was considered to indicate a statistically
significant difference. This study was approved by the ethics
committee of Nagasaki University Hospital.
Results
Early outcomes
Table I categorizes
the resected lesions by histopathological examination. The
indication criteria included 617 (46.3%) lesions; 507 (38.1%)
lesions were included in the expanded-indication criteria and 208
(15.6%) lesions were included in the out-of-indication criteria.
Table II lists the early outcomes
of the patients. The curative resection rates for en bloc
resection were 96.6% (596/617) and 91.5% (464/507) in the
indication and expanded-indication groups, respectively. The total
perforation rate was 2.9% (39/1,332), and the rate for the
expanded-indication group was significantly higher than that for
the indication group [4.3% (22/507) versus 1.8% (11/617),
P<0.05; Table III]. Only one
case of late-onset perforation required surgery. Overall, the
ESD-associated bleeding rate was 2.0% (26/1,332) and it was
significantly higher for the out-of-indication group [4.8%
(10/208)] compared with the indication group [1.1% (7/617)]
(P<0.01) or the expanded-indication group [1.8% (9/507)]
(P<0.05; Table IV). The
complication rate was similar to those calculated in other studies
(13–15). Local recurrence was identified in
two patients and the lesions in these patients were excised with
piecemeal resection.
 | Table IAll EGC cases categorized by pathology
(n=1,332). |
Table I
All EGC cases categorized by pathology
(n=1,332).
| Criteria | Lesions [n (%)] |
|---|
| Indication
[differentiated M UL(−) ≤20 mm] | 617 (46.3%) |
| Expanded
indication | 507 (38.1%) |
| Differentiated M
UL(−) >20 mm | 293 |
| Differentiated M
UL(+) ≤30 mm | 146 |
| Differentiated SM1
≤30 mm | 62 |
| Undifferentiated M
UL(−) ≤20 mm | 6 |
| Out of
indication | 208 (15.6%) |
 | Table IIEarly outcomes. |
Table II
Early outcomes.
| Outcomes | Indication
(n=617) | Expanded indication
(n=507) | Out of indication
(n=208) |
|---|
| En bloc | 605/617 | 487/507 | 199/208 |
| 98.1% | 96.1% | 95.7% |
| Curative | 596/617 | 464/507 | - |
| 96.6% | 91.5% | |
| Piecemeal or
non-curative | 21/617 | 43/507 | 208/208 |
| 3.4% | 8.5% | 100% |
 | Table IIIPerforation rates. |
Table III
Perforation rates.
| Criteria | Perforation rate [%
(n/total)] |
|---|
| Indication | 1.8% (11/617) |
| Expanded
indication | 4.3% (22/507) |
| Out of
indication | 2.9% (6/208) |
| Total | 2.9% (39/1332) |
 | Table IVESD-associated later bleeding
rates. |
Table IV
ESD-associated later bleeding
rates.
| Criteria | Bleeding rate [%
(n/total)] |
|---|
| Indication | 1.1% (7/617) |
| Expanded
indication | 1.8% (9/507) |
| Out of
indication | 4.8% (10/208) |
| Total | 2.0% (26/1332) |
Long-term outcomes
Patients (n=319), consisting of 224 men and 95
women, with a mean age of 71 years (range, 33–92 years), were
followed up >5 years after ESD was performed. Of those, 19
patients (42 lesions) had multiple EGCs; thus, in the analysis of
long-term outcomes, the other 300 patients were enrolled. The
median follow-up term of observation was 66 months, ranging from 1
to 106 months. Table V presents
the categorization of the resected lesions that were enrolled in
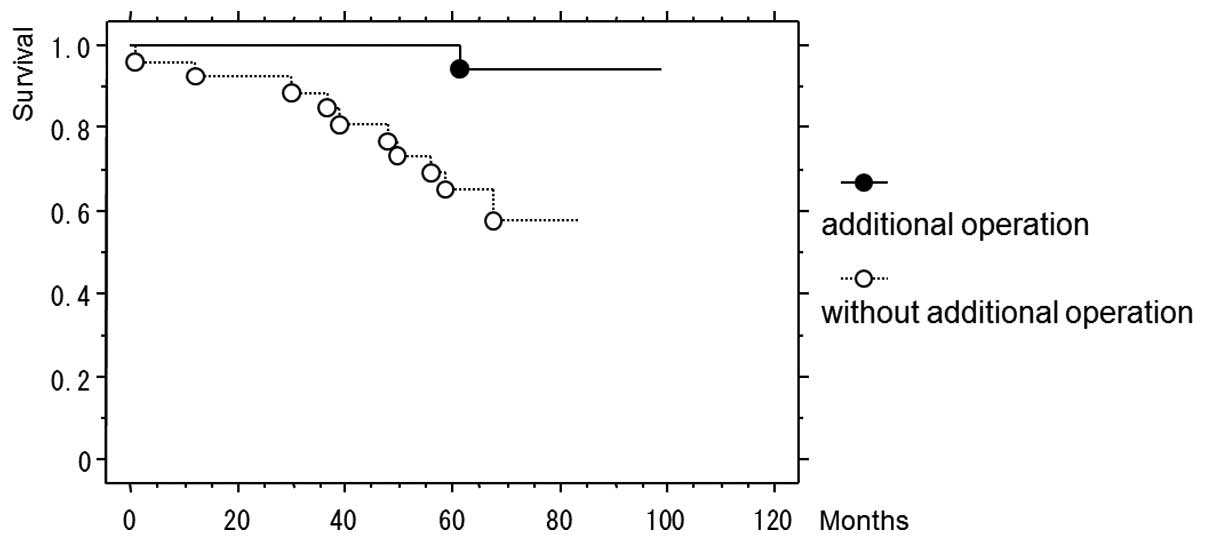
the long-term outcome analysis. Of the 49 patients in the
out-of-indication group, 23 underwent additional surgery and 26 did
not due to advanced age, concomitant diseases and/or rejection of
surgery by the patient. Of the 146 patients in the indication
group, 20 passed away; 18 mortalities were due to diseases other
than gastric cancer and two were due to unknown causes. Of the 105
patients in the expanded-indication group, 15 patients succumbed to
diseases other than gastric cancer. Of the 23 patients who
underwent additional surgery in the out-of-indication group, one
mortality occurred, which was not due to gastric cancer. Among the
26 patients who did not undergo additional surgery in the
out-of-indication group, 10 mortalities occurred, including one due
to gastric cancer. The five-year survival rate was not
significantly different between the indication and
expanded-indication groups (Fig.
1). However, in the out-of-indication group, the five-year
survival rate of the patients who did not undergo additional
surgery (65.0%) was significantly lower than that of the patients
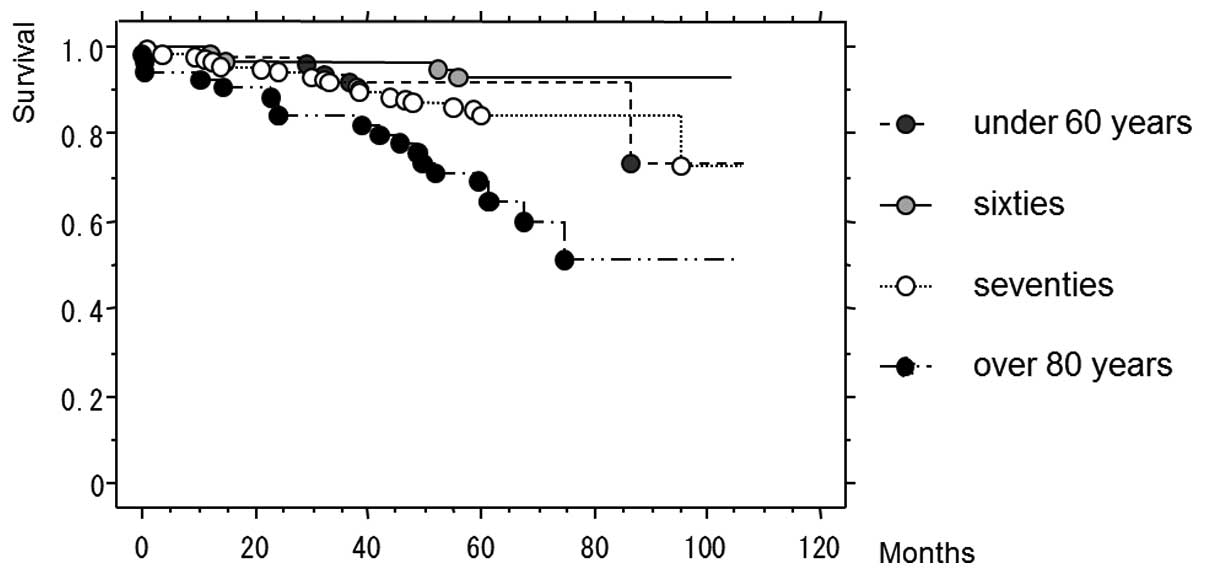
who did undergo additional surgery (100%) (P=0.0062; Fig. 2). In the analysis by age, the
five-year survival rate of the patients >80 years old (67.1%)
was significantly lower than those of the younger age groups
(<60 years old, 91.6%; sixties, 93.0%; seventies, 84.5%)
(P<0.0001; Fig. 3).
 | Table VCases followed up >5 years after
ESD, with the exception of those with multiple lesions (n=300). |
Table V
Cases followed up >5 years after
ESD, with the exception of those with multiple lesions (n=300).
| Criteria | Patients (n) |
|---|
| Indication
(differentiated M UL(−) ≤20 mm) | 146 |
| Expanded
indication | 105 |
| Differentiated M
UL(−) >20 mm | 72 |
| Differentiated M
UL(+) ≤30 mm | 21 |
| Differentiated SM1
≤30 mm | 10 |
| Undifferentiated M
≤20 mm | 2 |
| Out of
indication: | 49 |
| Additional surgery
(+) | 23 |
| Additional surgery
(−) | 26 |
Discussion
Gotoda et al (7) suggested that early gastric cancer
with no risk of lymph node metastasis is definable by using a large
database, so the indications for endoscopic treatment have been
expanded in Japan. En bloc resection of ESD provides a much
higher curative resection rate than piecemeal resection via
endoscopic mucosal resection (EMR) (11). In addition, ESD permits precise
histopathological examination for the assessment of curability to
guide further management and to stratify the risk of a patient
developing metastases. Successful outcomes are therefore enabled
following ESD (6,16). In the present study, two cases of
EGC local recurrence were excised via piecemeal resection of ESD.
It is important to be able to excise via en bloc resection.
ESD is an excellent procedure as it decreases the incidence of
local recurrence following en bloc resection more
effectively than EMR (17). The
development of ESD has allowed the indications for endoscopic
treatment to be extended. In the present study, although the
perforation rate was higher for the expanded-indication group than
for the indication group, most of the perforations were controlled
endoscopically.
Although endoscopic treatment is an accepted therapy
for EGC in Japan (3–6), there have been few studies concerning
the long-term outcomes (18,19).
The present study has demonstrated that the survival rate of
patients meeting the expanded-indication criteria has been similar
to that of patients meeting the indication criteria. Therefore, the
current expanded indications may be appropriate. In the present
study, mortalities due to gastric cancer were not observed in the
patients in the indication and the expanded-indication groups.
However, 13.9% (35/251) of the patients in these two groups
succumbed to diseases other than gastric cancer. In particular, the
survival rate of the patients >80 years old was poor; most of
the patients >80 years of age succumbed to non-cancerous
diseases such as pulmonary disease, heart disease and cerebral
infarction. As may be expected, the life expectancies of the older
patients were shorter than the life expectancies of the younger
patients. This result may be a natural outcome; however, there are
a number of studies that suggest ESD is effective even in elderly
patients (13,18,19).
The natural history of EGC has been poorly delineated. Therefore,
the degree to which EGC improves the prognosis of elderly patients,
regardless of the presence or absence of a therapeutic
intervention, has not been fully clarified. In the present study, a
number of the elderly patients had concomitant diseases, but the
mortalities of a number of the others were unpredictable. Although
it is difficult to decide whether elderly patients with EGC should
undergo ESD, this issue merits careful thought. When the lesions
are judged as out-of-indication according to histopathological
analysis, additional surgery with lymph node dissection is
recommended. In the present study, in the out-of-indication group,
the five-year survival rate of the patients who did not undergo
additional surgery was significantly lower than that of the
patients who underwent additional surgery. The reasons for not
having additional surgery included advanced age and comorbid
disease, and such patients may not require ESD. However, as a
number of elderly patients may live for a long time, it is
difficult to decide whether ESD should be performed. This is an
issue for future study.
In conclusion, the results of the present study
demonstrated that the early and long-term outcomes of ESD for
patients meeting the expanded-indication criteria are similar to
those of patients meeting the indication criteria. When deciding
whether to perform ESD in elderly patients, it is necessary to
consider the presence of underlying comorbid diseases.
References
|
1
|
Sano T, Kobori O and Muto T: Lymph node
metastasis from early gastric cancer: endoscopic resection of
tumour. Br J Surg. 79:241–244. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shimizu S, Tada M and Kawai K: Early
gastric cancer: its surveillance and natural course. Endoscopy.
27:27–31. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ono H, Kondo H, Gotoda T, et al:
Endoscopic mucosal resection for treatment of early gastric cancer.
Gut. 48:225–229. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Abe N, Yamaguchi Y, Takeuchi H, et al: Key
factors for successful en bloc endoscopic submucosal dissection of
early stage gastric cancer using an insulation-tipped diathermic
knife. Hepatogastroenterology. 53:639–642. 2006.
|
|
5
|
Oda I, Saito D, Tada M, et al: A
multicenter retrospective study of endoscopic resection for early
gastric cancer. Gastric Cancer. 9:262–270. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gotoda T: Endoscopic resection of early
gastric cancer. Gastric Cancer. 10:1–11. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gotoda T, Yanagisawa A, Sasako M, et al:
Incidence of lymph node metastasis from early gastric cancer:
estimation with a large number of cases at two large centers.
Gastric Cancer. 3:219–225. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gotoda T, Iwasaki M, Kusano C, Seewald S
and Oda I: Endoscopic resection of early gastric cancer treated by
guideline and expanded National Cancer Centre criteria. Br J Surg.
97:868–871. 2010. View
Article : Google Scholar
|
|
9
|
Hirasawa T, Fujisaki J, Fukunaga T, et al:
Lymph node metastasis from undifferentiated-type mucosal gastric
cancer satisfying the expanded criteria for endoscopic resection
based on routine histological examination. Gastric Cancer.
13:267–270. 2010. View Article : Google Scholar
|
|
10
|
Japanese Gastric Cancer Association.
Treatment Guidelines for Gastric Cancer in Japan. 3rd edition.
Kanehara; Tokyo: 2010, (In Japanese).
|
|
11
|
Oda I, Gotoda T, Hamanaka H, et al:
Endoscopic submucosal dissection for early gastric cancer:
Technical feasibility, operation time and complications from a
large consecutive series. Dig Endosc. 17:54–58. 2005. View Article : Google Scholar
|
|
12
|
Yokoi C, Gotoda T, Hamanaka H and Oda I:
Endoscopic submucosal dissection allows curative resection of
locally recurrent early gastric cancer after prior endoscopic
mucosal resection. Gastrointest Endosc. 64:212–218. 2006.
View Article : Google Scholar
|
|
13
|
Toyokawa T, Fujita I, Morikawa T, et al:
Clinical outcomes of ESD for early gastric neoplasms in elderly
patients. Eur J Clin Invest. 41:474–478. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jeon SW, Jung MK, Kim SK, et al: Clinical
outcomes for perforations during endoscopic submucosal dissection
in patients with gastric lesions. Surg Endosc. 24:911–916. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kakushima N, Fujishiro M, Kodashima S, et
al: Technical feasibility of endoscopic submucosal dissection for
gastric neoplasms in the elderly Japanese population. J
Gastroenterol Hepatol. 22:311–314. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Soetikno R, Kaltenbach T, Yeh R and Gotoda
T: Endoscopic mucosal resection for early cancers of the upper
gastrointestinal tract. J Clin Oncol. 23:4490–4498. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takenaka R, Kawahara Y, Okada H, et al:
Risk factors associated with local recurrence of early gastric
cancers after endoscopic submucosal dissection. Gastrointest
Endosc. 68:887–894. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kusano C, Iwasaki M, Kaltenbach T, Conlin
A, Oda I and Gotoda T: Should elderly patients undergo additional
surgery after non-curative endoscopic resection for early gastric
cancer? Long-term comparative outcomes. Am J Gastroenterol.
106:1064–1069. 2011. View Article : Google Scholar
|
|
19
|
Abe N, Gotoda T, Hirasawa T, et al:
Multicenter study of the long-term outcomes of endoscopic
submucosal dissection for early gastric cancer in patients 80 years
of age or older. Gastric Cancer. 15:70–75. 2012.PubMed/NCBI
|