Introduction
Type 2 diabetes mellitus (T2DM) is a major risk
factor for cardiovascular disease and is associated with
significant cardiovascular morbidity and mortality (1). Patients with T2DM have an increased
risk of acute coronary events (1).
Acute coronary events are often caused by the rupture of unstable
coronary atherosclerotic plaques and coronary stenosis (2,3).
Therefore, assessment of atherosclerotic plaque morphology and
pathological features has become an important part of the clinical
investigation of coronary artery disease (4). Multi-detector computed tomography
angiography (MDCTA) has been increasingly used in the evaluation of
coronary arteries (5). In an acute
setting, MDCTA is associated with 95% sensitivity and 90%
specificity in diagnosing non-ST-elevation myocardial infarction
and unstable angina pectoris (6).
The ability to detect not only coronary stenosis, but also
non-obstructive coronary atherosclerotic plaques using a
non-invasive method indicates that MDCTA imaging is a potentially
valuable tool for risk stratification. In previous studies, MDCTA
has been used to predict cardiac events and prognosis in patients
with suspected coronary artery disease (7–14).
However, there is limited information on the predictive value of
MDCTA on acute coronary events in patients with T2DM.
Therefore, the purpose of the present study was to
investigate the MDCTA characteristics of coronary plaques in
patients with T2DM. The sensitivity and specificity of MDCTA in
predicting acute coronary events in these patients was also
evaluated.
Subjects and methods
Study population
The study was approved by the Institutional Ethics
Committee of Liaocheng People’s Hospital (Liaocheng, China) and
written informed consent was provided by all the participants.
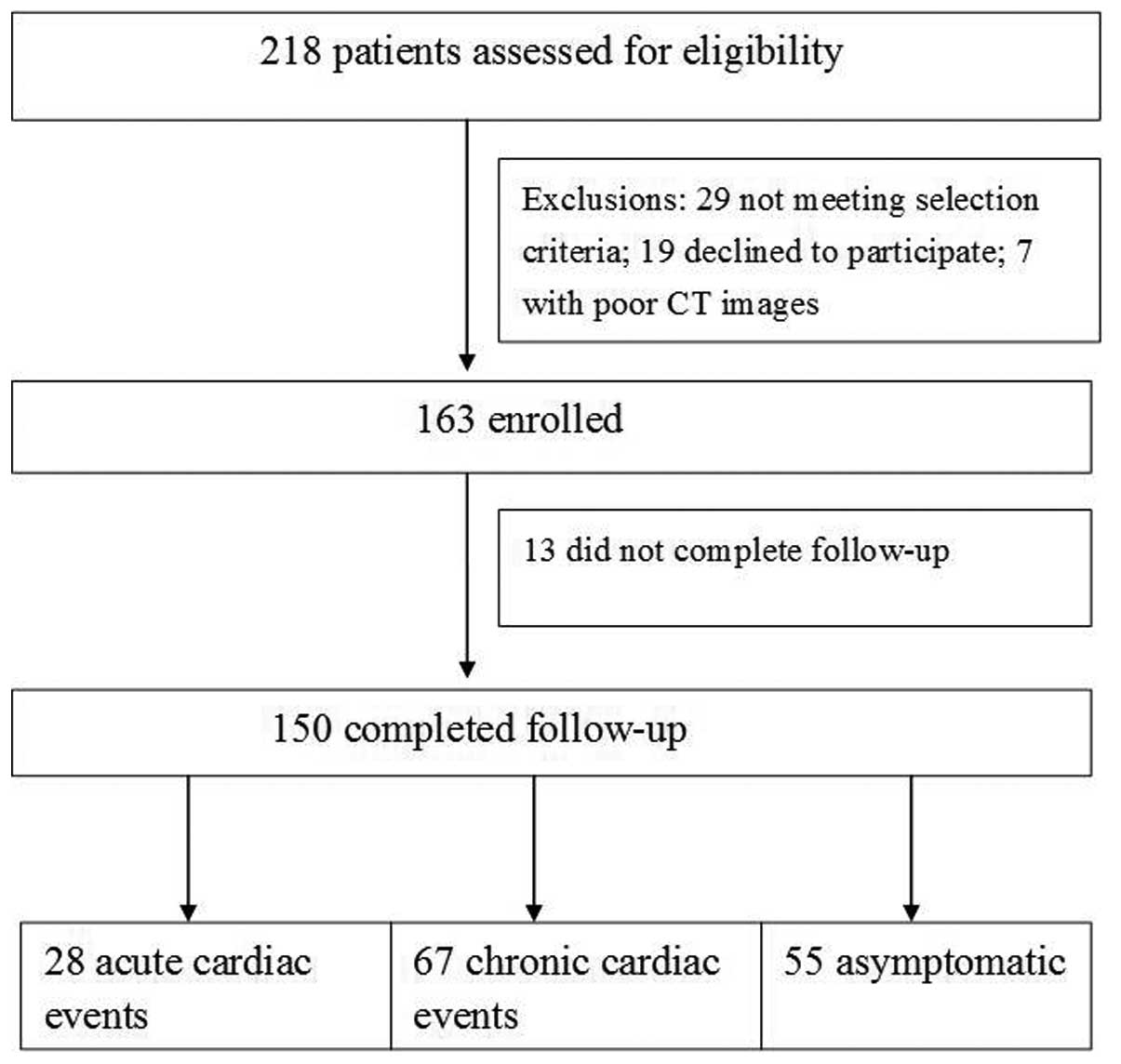
Between February 2007 and November 2009, 218 consecutive patients
with T2DM were referred to our department at Liaocheng People’s
Hospital (Liaocheng, China) for coronary MDCTA due to nonspecific
chest pain, exertional dyspnea or ST-T depression or flattening
observed on an electrocardiogram (ECG). These patients were
screened for the present study. Patients who had undergone previous
coronary balloon angioplasty, stenting or coronary artery bypass
grafting were excluded. Additional exclusion criteria were as
follows: i) Heart rate >90 beats/min, atrial fibrillation or
other arrhythmias; ii) renal dysfunction (serum creatinine ≥120
mmol/l); iii) other chronic illnesses, including severe respiratory
insufficiency and hyperthyroidism; and iv) patients who were unable
to provide written consent. In total, 150 patients were recruited
and 58 patients were excluded in the study. The reasons for
exclusion are listed in Fig.
1.
MDCTA protocol
The first 95 patients were scanned by a Philips
Brilliance 64-detector CT (Philips Medical Systems, Eindhoven,
Netherlands). Prior to the scans, β-blockers were administered to
patients whose heart rate was ≥70 beats/min, and 0.3 mg
nitroglycerin was sublingually administered to all patients 15 min
prior to the scans. Retrospective ECG-gated helical MDCTA was
performed with a 64-detector CT. The scan parameters were 64×0.625
mm collimation, 120 kV tube voltage, 400–600 mAs tube current, 0.42
sec rotation time and 0.2 pitch. Data acquisition was completed
within 4.1–5.9 sec with a radiation dose of 13.9–16.8 mSv (median,
15.1 mSv). In the remaining 55 patients, a prospective ECG-gated
scan was performed with a 128-detector CT and the heart rate was
restricted to within 60–70 beats/min. The scan parameters were 120
kV tube voltage, 200 mAs tube current, 128×0.625 mm collimation,
0.18–0.27 sec rotation time and 0.2 pitch. Scanning was completed
within 3.9–6.8 sec with a radiation dose between 3.16 and 4.14 mSv
(median, 3.6 mSv).
A 50–60 ml (dependent on body mass index) bolus of
iodinated contrast agent (iopamidol; 370 mg iodine/ml; Bracco Sine
Pharmaceutical Corp. Ltd, Pudong, China) was injected into the
antecubital vein at a flow rate of 4–5 ml/sec. The scanning range
was between the tracheal bifurcation and 10 mm below the inferior
cardiac apex. Best quality images were selected for evaluation and
other phases or ECG editing was performed if required. All initial
data sets were transferred to a post-processing workstation
(Brilliance-workshop; Philips Medical Systems) for image analysis.
Alternative image reconstruction methods for evaluation of coronary
arteries and plaques included maximum intensity projection,
multi-planar reconstruction, curvature plane reconstruction and
volume rendering.
Stenosis and plaque analysis
Two cardiovascular radiologists analyzed the images
independently. The radiologists were blinded to the medical
histories, clinical diagnoses and results of other investigations
for all the patients. In cases of disagreement, the features of
plaque and stenosis evaluations were re-evaluated for a consensus
judgment.
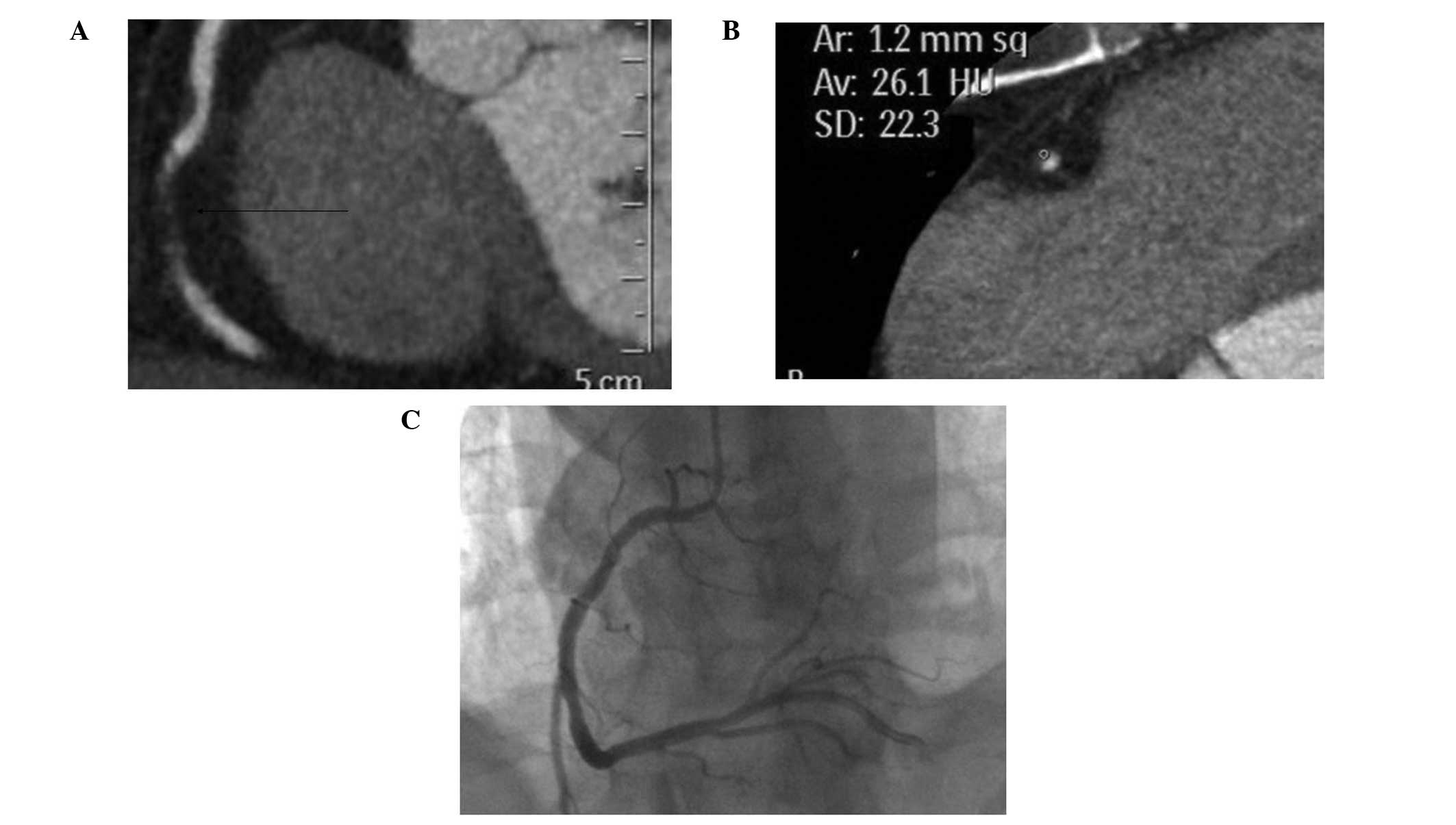
Subsequently, the type of plaque was determined to
be non-calcified, calcified or mixed (15). Non-calcified plaques had a lower
density compared with the contrast-enhanced lumen, while calcified
plaques had a higher density. Mixed plaques exhibited soft and
calcified elements within a single plaque. Measurements were
performed in axial and multiplanar reconstruction images and four
points were selected randomly. Regions of interest of >1.0
mm2 (at least 3 contiguous pixels; area, 1.03
mm2) and the smallest CT value was defined as the size
of the plaques (Figs. 2 and
3). The coronary artery plaques
were classified into four types as previously described (16,17):
Type I concentric lesions, type II eccentric lesions with a wide
base but smooth margin, type III eccentric lesions with a narrow
base and rough surface and type IV long segments of irregular
lesions.
The number of affected coronary vessels, segments
and plaques, as well as the types of plaques and grading of
stenosis caused by the plaques were evaluated. Coronary arteries
were divided into a 15 segment model of the American Heart
Association (18). The involved
vessels were classified as single, double or triple vessels. The
degree of stenosis was defined as the percentage of stenosis and
adjacent normal vessel lumen (normal or mild, <50% stenosis;
moderate, 50–75% stenosis; severe, ≥75% stenosis) (19).
Follow-up
Follow-ups were conducted by structured telephone
interviews with the patients or relatives that understood the
patients’ condition. The follow-up questionnaires included the
general health of the patients, use of medications, cardiovascular
events, including hospital admissions, coronary artery angiography
or stenting, or coronary artery bypass grafting. The interviews
were conducted every 6 months for at least 24 months.
Acute coronary events were defined as acute coronary
syndrome (ST- or non-ST elevation myocardial infarction or unstable
angina) or sudden cardiac mortality (study group). Patients with
stable angina or with angiographically identified coronary artery
stenosis requiring elective coronary stenting or bypass grafting 6
months following MDCTA, were considered as having chronic coronary
events (control group) (14).
Statistic analysis
Data are expressed as the mean ± SD.
χ2-test was used to compare the categorical data between
the study and control groups. P<0.05 was considered to indicate
a statistically significant difference. All statistical analyses
were performed using the SPSS statistical package (version 11.5 for
Windows; SPSS, Inc., Chicago, IL, USA).
Results
General observations
A total of 163 patients were recruited to the study,
but only 150 patients completed the follow-up (mean follow-up time,
30±5.6 months; range, 24–57 months; Fig. 1). The baseline characteristics of
these patients are summarized in Table
I.
 | Table IBaseline characteristics. |
Table I
Baseline characteristics.
| Characteristics | Study group
(n=28) | Control group
(n=67) | P-value |
|---|
| Age, years | 64.7±14.6 | 63.6±15.3 | NS |
| Gender, male, n
(%) | 16 (57.1) | 29 (43.3) | NS |
| BMI,
kg/m2 | 25.8±3.54 | 25.3±1.49 | NS |
| Other cardiovascular
risk factors, n (%) |
| Hypertension | 17 (60.7) | 42 (62.7) | NS |
|
Hypercholesterolemia | 13 (46.4) | 32 (47.8) | NS |
| Smoking | 15 (53.6) | 34 (50.7) | NS |
| Family history of
CHD | 9 (32.1) | 21 (31.3) | NS |
| Clinical
presentation, n (%) |
| Abnormal ECG | 24 (85.7) | 46 (68.7) | NS |
| Atypical angina | 8 (28.6) | 46 (68.7) | NS |
| Nonspecific chest
pain | 17 (60.7) | 38 (56.7) | NS |
| Dyspnea | 18 (64.3) | 45 (67.2) | NS |
| Diabetes treatment, n
(%) |
| Oral agents | 2 (7.1) | 12 (17.9) | NS |
| Oral agents plus
insulin | 26 (92.8) | 55 (82.8) | NS |
During the follow-up period, acute coronary events
occurred in 28 patients (18.7%), including acute myocardial
infarction in eight individuals (5.3%), unstable angina in 19
patients (12.7%) and sudden mortality in one patient (0.7%). Within
the first six months of the follow-up period, 15 patients
exhibiting acute coronary events underwent coronary stenting and
eight received coronary bypass grafting. Chronic coronary events
occurred in 67 patients (44.7%), including stable angina pectoris
in 58 individuals, elective coronary stenting in seven patients and
elective coronary bypass grafting in two patients. The remaining 55
patients (36.7%) were asymptomatic and free of coronary events
during the follow-up period.
Coronary artery plaques on MDCTA
images
A total of 420 segments were analyzed in the study
group and 1,005 segments were analyzed in the control group
(Table II). Triple-vessel
diseases were identified in 67.8% of the study group and 68.6% of
the control group (P=0.380). A moderate to severe degree of
coronary stenosis was identified in 89.8% of the study group and
88% of the control group (P=0.380).
 | Table IIComparison of coronary lesions and
degree of coronary stenosis between groups. |
Table II
Comparison of coronary lesions and
degree of coronary stenosis between groups.
| Coronary lesions | Study group
(n=28) | Control group
(n=67) | P-value |
|---|
| Vessels involved, n
(%) |
| Single | 4 (14.4) | 8 (12) | NS |
| Double | 5 (17.8) | 13 (19.4) | NS |
| Triple | 19 (67.8) | 46 (68.6) | NS |
| Stenosis grade, n
(%) |
| <50% | 43 (10.2) | 121 (12.0) | NS |
| 50–75% | 263 (62.6) | 641 (63.8) | NS |
| ≥75% | 114 (27.2) | 243 (24.2) | NS |
The numbers and characteristics of the coronary
plaques in the study and control groups are shown in Table III. In the study group, there
were 236 non-calcified, 315 mixed and 87 calcified plaques. By
contrast, in the control group, the numbers of non-calcified, mixed
and calcified plaques were 148, 596 and 843, respectively. The
proportion of calcified plaques in the study group was
significantly lower compared with the control group (13.6 vs.
53.2%; P<0.01). In addition, the proportion of non-calcified
plaques in the study group was significantly higher compared with
the control group (37 vs. 9.3%; P<0.001).
 | Table IIIComparison of plaque numbers and
characteristics between the acute and chronic groups. |
Table III
Comparison of plaque numbers and
characteristics between the acute and chronic groups.
| Plaque
characteristics | Study group (plaques,
638) | Control group
(plaques, 1,586) | P-value |
|---|
| Non-calcified, n
(%) | 236 (37) | 148 (9.3) | <0.001 |
| Mixed, n (%) | 315 (49.4) | 595 (37.5) | <0.001 |
| Calcified, n
(%) | 87 (13.6) | 843 (53.2) | <0.001 |
Plaque morphology and acute coronary
events
The numbers of various plaque types observed
following MDCTA are listed in Table
IV. In the study group, there was no statistically significant
difference in plaque type between the patients with moderate or
severe coronary stenosis (P=0.349). However, in the control group,
there were statistically significant differences in plaque type
among the patients with various grades of stenosis
(P<0.001).
 | Table IVComparison of plaque morphology
between the study and control groups. |
Table IV
Comparison of plaque morphology
between the study and control groups.
| Plaque
morphology | Study group
(plaques, 638) | Control group
(plaques, 1,586) | P-value |
|---|
| Type I, n (%) | 38 (6) | 89 (5.6) | 0.825 |
| Type II, n (%) | 65 (10.2) | 637 (42.2) | <0.001 |
| Type III, n
(%) | 486 (76.2) | 276 (17.4) | <0.001 |
| Type IV, n (%) | 49 (7.6) | 584 (36.8) | <0.001 |
As shown in Table
IV, there was no statistically significant difference in the
proportion of type I plaques between the study and control groups
(P>0.05). However, the proportion of type III plaques in the
study group was higher compared with the control group, whereas the
proportion of type II and IV plaques was lower (P<0.01).
Using type III plaques to predict acute coronary
events, the sensitivity and specificity levels were 63.8 and 76.2%,
respectively. However, using type II and IV plaques to predict
chronic coronary events, the sensitivity and specificity levels
were 91.5 and 79%, respectively.
Discussion
The main observations of the present study were as
follows. Firstly, the proportion of non-calcified and type III
plaques in patients with acute coronary events was higher compared
with patients with stable angina. Secondly, the proportion of
calcified plaques in patients with stable angina was higher
compared with patients with acute coronary events. Finally, the
sensitivity and specificity levels of type III plaques in
predicting acute coronary events were 63.8 and 76.2%, respectively,
whereas the sensitivity and specificity levels of type II and IV
plaques in predicting chronic coronary events were 91.5 and 79%,
respectively. These observations indicate that non-invasive MDCTA
may be used to evaluate the vulnerability of coronary plaques in
patients with T2DM and as a tool to predict acute coronary
events.
Previous studies have found that numerous coronary
lesions in patients with coronary heart disease are non-obstructive
and vessels with mild to moderate stenosis are responsible for
cardiac events (20,21). The vulnerability of intracoronary
lesions is a key factor for acute cardiac events in these patients
with mild to moderate stenosis (20,21).
Acute coronary syndrome is often caused by rupture of coronary
artery atherosclerosis plaques, rather than lumen stenosis
(22). Therefore, early detection
of vulnerable or unsteady plaques is important in guiding
prevention and treatment of acute cardiac events. Non-calcified
plaques are unsteady and have been commonly observed in patients
with acute coronary syndrome (23,24).
Consistent with previous studies, the results of the present study
demonstrate that there is little difference in stenosis severity
between patients with acute and chronic coronary events. By
contrast, the types of coronary plaques detected by MDCTA appear to
be associated with coronary events. The current study also
identified that patients with acute coronary syndrome exhibited an
increased number of non-calcified plaques and fewer calcified
plaques compared with patients with stable angina. These results
indicate that in patients with T2DM, analysis of stenosis severity
using MDCTA alone may be insufficient. Evaluation of plaque
morphology and vulnerability using MDCTA offers additional
information on the future risk of acute coronary events.
The reliability of MDCTA in assessing coronary
plaque stability has been increasingly studied in recent years. A
previous study by Motoyama et al (25) demonstrated that MDCTA can be used
to accurately assess plaque composition by measuring the CT value
of the plaque on thin-CT images. Falk et al (26) identified that eccentric lesions
were an index of unsteady plaques. The lipid core of the plaque is
present in the inner lining of the coronary lumen and is prone to
rupture under the impact of blood flow. Ruptured plaques adsorb
platelets, resulting in new clot formation, obstruction of coronary
flow and acute coronary syndrome or sudden mortality (27). In the present study, the coronary
plaques were divided into four types as previously described
(16,17). Type III plaques, those with an
eccentric center and rough surface, appear to be associated with
acute coronary events. The predictive sensitivity and specificity
levels of type III plaques for acute coronary events were 63.8 and
76.2%, respectively. By contrast, eccentric lesions with a wide
base but smooth margin (type II plaques) and long segments of
irregular lesions (type IV plaques) are relatively stable plaques
and demonstrated 91.5% sensitivity and 79% specificity in
predicting chronic coronary events.
A potential limitation of the present study
regarding the first 95 patients is that at the beginning of the
study, retrospective ECG-gated helical MDCTA was performed using a
64-detector CT. In the remaining 55 patients, prospective ECG-gated
scans were performed using a 128-detector CT. The imaging quality
of the 128-detector MDCTA is generally superior to the 64-detector
MDCTA and the dose of radiation is also lower (5,27).
In total, 7 patients were excluded from the study due to poor
imaging quality and these patients were scanned with the
64-detector MDCTA.
In conclusion, MDCTA is a non-invasive tool that can
be used to measure the severity of coronary stenosis and assess the
morphology of coronary plaques. In patients with T2DM, eccentric
plaques with rough surfaces have a moderate sensitivity and
specificity in predicting acute coronary events. Eccentric plaques
with smooth surfaces and long segments of irregular coronary
lesions are more likely to be associated with chronic coronary
events. These observations indicate that morphology analysis using
MDCTA may improve coronary risk stratification in patients with
T2DM.
References
|
1
|
Macisaac RJ and Jerums G: Intensive
glucose control and cardiovascular outcomes in type 2 diabetes.
Heart Lung Circ. 20:647–654. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hendel RC, Patel MR, Kramer CM, Poon M,
Hendel RC, Carr JC, et al: ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR
2006 appropriateness criteria for cardiac computed tomography and
cardiac magnetic resonance imaging: a report of the American
College of Cardiology Foundation Quality Strategic Directions
Committee Appropriateness Criteria Working Group, American College
of Radiology, Society of Cardiovascular Computed Tomography,
Society for Cardiovascular Magnetic Resonance, American Society of
Nuclear Cardiology, North American Society for Cardiac Imaging,
Society for Cardiovascular Angiography and Interventions, and
Society of Interventional Radiology. J Am Coll Cardiol.
48:1475–1497. 2006.
|
|
3
|
Schroeder S, Achenbach S, Bengel F,
Burgstahler C, Cademartiri F, Feyter P, et al: Cardiac computed
tomography: indications, applications, limitations, and training
requirements: report of a Writing Group deployed by the Working
Group Nuclear Cardiology and Cardiac CT of the European Society of
Cardiology and the European Council of Nuclear Cardiology. Eur
Heart J. 29:531–556. 2008.
|
|
4
|
Murray SW, Stables RH and Palmer ND:
Virtual histology imaging in acute coronary syndromes: useful or
just a research tool? J Invasive Cardiol. 22:84–91. 2010.PubMed/NCBI
|
|
5
|
Duarte R, Fernandez G, Castellon D and
Costa JC: Prospective coronary CT angiography 128-MDCT versus
retrospective 64-MDCT: Improved image quality and reduced radiation
dose. Heart Lung Circ. 20:119–125. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vanhoenacker PK, Decramer I, Bladt O,
Sarno G, Bevernage C and Wijns W: Detection of non-ST-elevation
myocardial infarction and unstable angina in the acute setting:
meta-analysis of diagnostic performance of multi-detector computed
tomographic angiography. BMC Cardiovas Disord. 7:392007. View Article : Google Scholar
|
|
7
|
Pundziute G, Schuijf JD, Jukema JW,
Boersma E, de Roos A, van der Wall EE and Bax JJ: Prognostic value
of multislice computed tomography coronary angiography in patients
with known or suspected coronary artery disease. J Am Coll Cardiol.
49:62–70. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Min JK, Shaw LJ, Devereux RB, Okin PM,
Weinsaft JW, Russo DJ, et al: Prognostic value of multidetector
coronary computed tomographic angiography for prediction of
all-cause mortality. J Am Coll Cardiol. 50:1161–1170. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gaemperli O, Valenta I, Schepis T, Husmann
L, Scheffel H, Desbiolles L, et al: Coronary 64-slice CT
angiography predicts outcome in patients with known or suspected
coronary artery disease. Eur Radiol. 18:1162–1173. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Van Werkhoven JM, Cademartiri F, Seitun S,
Maffei E, Palumbo A, Martini C, et al: Diabetes: prognostic value
of CT coronary angiography - comparison with a nondiabetic
population. Radiology. 256:83–92. 2010.PubMed/NCBI
|
|
11
|
Carrigan TP, Nair D, Schoenhagen P, Curtin
RJ, Popovic ZB, Halliburton S, et al: Prognostic utility of
64-slice computed tomography in patients with suspected but no
documented coronary artery disease. Eur Heart J. 30:362–371. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hadamitzky M, Freissmuth B, Meyer T, Hein
F, Kastrati A, Martinoff S, Schömig A and Hausleiter J: Prognostic
value of coronary computed tomographic angiography for prediction
of cardiac events in patients with suspected coronary artery
disease. JACC Cardiovasc Imaging. 2:404–411. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chow BJ, Wells GA, Chen L, Yam Y,
Galiwango P, Abraham A, et al: Prognostic value of 64-slice cardiac
computed tomography severity of coronary artery disease, coronary
atherosclerosis, and left ventricular ejection fraction. J Am Coll
Cardiol. 55:1017–1028. 2010. View Article : Google Scholar
|
|
14
|
Wackers FJ, Young LH, Inzucchi SE, Chyun
DA, Davey JA, Barrett EJ, et al; Detection of Ischemia in
Asymptomatic Diabetics Investigators. Detection of silent
myocardial ischemia in asymptomatic diabetic subjects: the DIAD
study. Diabetes Care. 27:1954–1961. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ibebuogu UN, Nasir K, Gopal A, et al:
Comparison of atherosclerotic plaque burden and composition between
diabetic and non diabetic patients by non invasive CT angiography.
Int J Cardiovasc Imaging. 25:717–723. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Casscells W, Naghavi M and Willerson JT:
Vulnerable atherosclerotic plaque: a multifocal disease.
Circulation. 107:2072–2075. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fayad ZA and Fuster V: Clinical imaging of
the high-risk or vulnerable atherosclerotic plaque. Circ Res.
89:305–316. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Austen WG, Edwards JE, Frye RL, Gensini
GG, Gott VL, Griffith LS, et al: A reporting system on patients
evaluated for coronary artery disease. Report of the Ad Hoc
Committee for Grading of Coronary Artery Disease, Council on
Cardiovascular Surgery, American Heart Association. Circulation.
51(Suppl 4): S5–S40. 1975. View Article : Google Scholar
|
|
19
|
Hausleiter J, Meyer T, Hadamitzky M,
Kastrati A, Martinoff S and Schömig A: Prevalence of noncalcified
coronary plaques by 64-slice computed tomography in patients with
an intermediate risk for significant coronary artery disease. J Am
Coll Cardiol. 48:312–318. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Giroud D, Li JM, Urban P, Meier B and
Rutishauer W: Relation of the site of acute myocardial infarction
to the most severe coronary arterial stenosis at prior angiography.
Am J Cardiol. 69:729–732. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alderman EL, Corley SD, Fisher LD,
Chaitman BR, Faxon DP, Foster ED, et al: Five-year angiographic
follow-up of factors associated with progression of coronary artery
disease in the Coronary Artery Surgery Study (CASS). CASS
Participating Investigators and Staff. J Am Coll Cardiol.
22:1141–1154. 1993.PubMed/NCBI
|
|
22
|
Raggi P, Shaw LJ, Berman DS and Callister
TQ: Prognostic value of coronary artery calcium screening in
subjects with and without diabetes. J Am Coll Cardiol.
43:1663–1669. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Schuijf JD, Beck T, Burgstahler C, Jukema
JW, Dirksen MS, de Roos A, van der Wall EE, Schroeder S, Wijns W
and Bax JJ: Differences in plaque composition and distribution in
stable coronary artery disease versus acute coronary syndromes;
non-invasive evaluation with multi-slice computed tomography. Acute
Card Care. 9:48–53. 2007. View Article : Google Scholar
|
|
24
|
Hamirani YS, Nasir K, Gopal A, Ahmadi N,
Pal R, Flores F, Blumenthal RS and Budoff MJ: Atherosclerotic
plaque composition among patients with stenotic coronary artery
disease on noninvasive CT angiography. Coron Artery Dis.
21:222–227. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Motoyama S, Kondo T, Anno H, Sugiura A,
Ito Y, Mori K, et al: Atherosclerotic plaque characterization by
0.5-mm-slice multislice computed tomographic imaging. Circ J.
71:363–366. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Falk E, Shah PK and Fuster V: Coronary
plaque disruption. Circulation. 92:657–671. 1995. View Article : Google Scholar
|
|
27
|
Freeman A, Learner R, Eggleton S, Lambros
J and Friedman D: Marked reduction of effective radiation dose in
patients undergoing CT coronary angiography using prospective ECG
gating. Heart Lung Circ. 20:512–516. 2011. View Article : Google Scholar : PubMed/NCBI
|