Introduction
Hypereosinophilic syndrome (HES) is a rare disorder
that was first classified by Hardy and Anderson in 1968 (1). The syndrome refers to a group of
leukoproliferative disorders that are characterized by the presence
of marked peripheral blood eosinophilia and organ damage caused by
the infiltration of eosinophils (2). HES used to be asympatic unless end
organ injury due to massive eosinophilic invasivion happens.
Virtually all organs can be involved, however, involvement of the
urinary bladder is relatively rare. In the present study, a case of
eosinophilic cystitis in a patient with HES was reported. To the
best of our knowledge, there have only been a few definite cases
previously reported in literature (3). Detailed clinicopathological data and
follow-up information has been provided for the current case.
Case report
A 56-year-old male with one month history of gross
hematuria and urinary urgency was admitted to our hospital on
December 2012. The patient had no significant past medical history
and the physical examination was unremarkable. Initial
ultrasonography revealed marked thickening of the bladder wall,
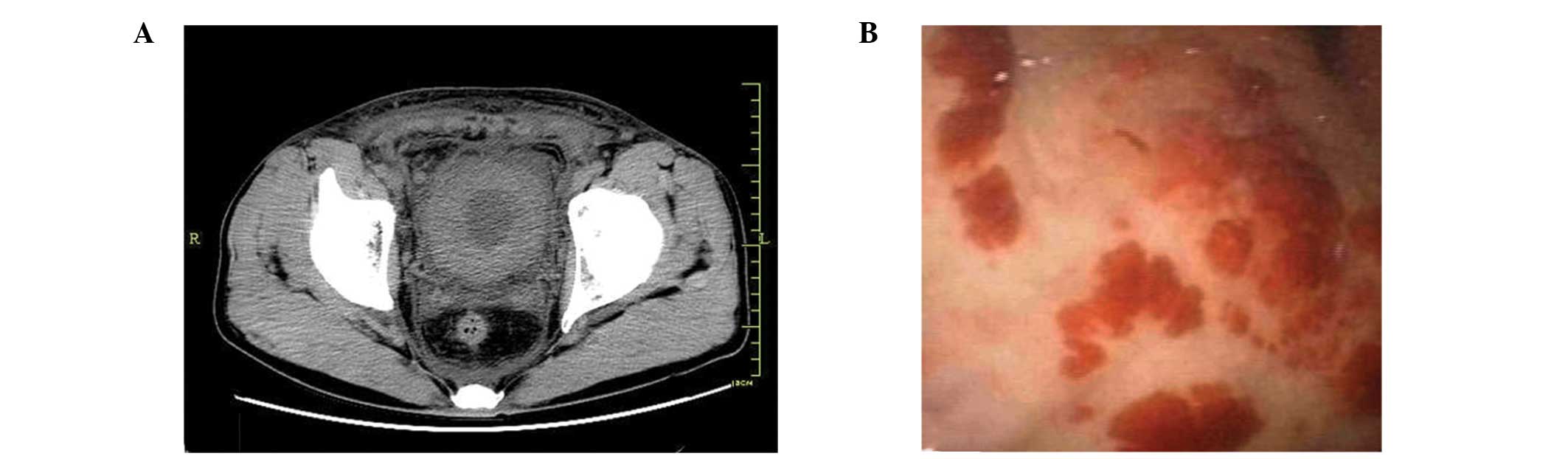
which was further confirmed by computed tomography scans (Fig. 1). Laboratory examinations revealed
a white blood cell count of 16.8×103
cells/mm3 (reference range, 4.0–10.0×103
cells/mm3) and significant eosinophilia of 36%
(reference range, 0.5–5.0%). Stool analysis for ova and parasites
was negative. Cystoscopic examination was conducted and the
observations revealed an erythematous velvety appearance of the
bladder mucosa (Fig. 1). A biopsy
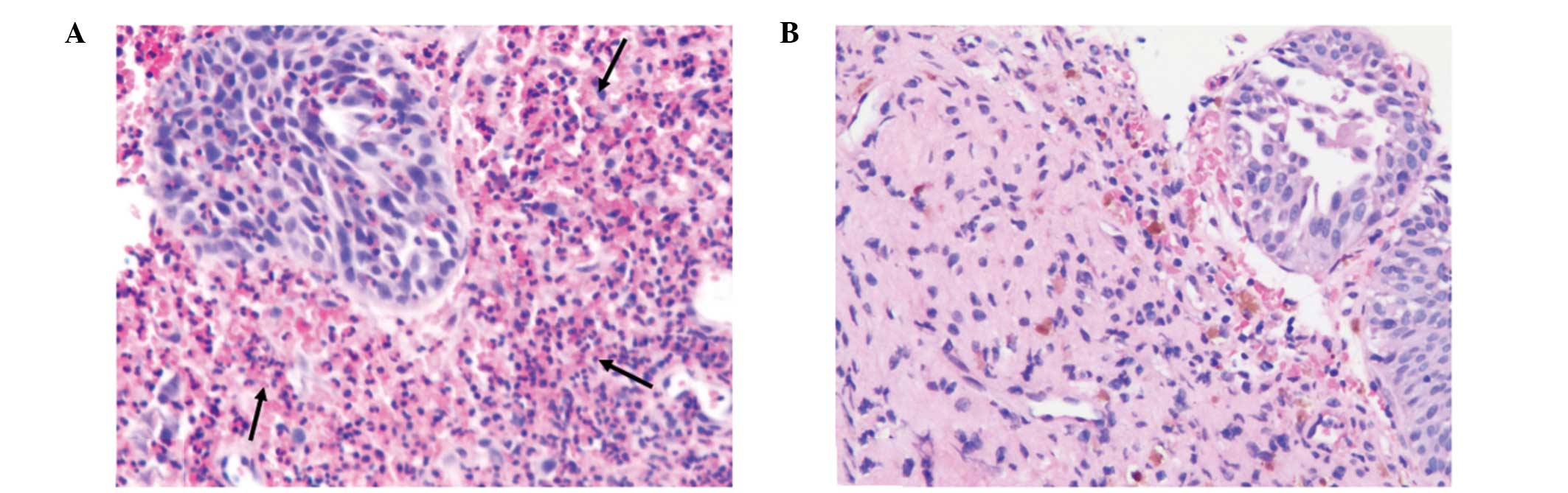
was performed and the bladder mucosa showed diffuse infiltration of
eosinophils, which indicated eosinophilic cystitis (Fig. 2). Bone marrow aspiration revealed
marked eosinophilia, but no primitive cell predominance, which
eliminated a diagnosis of leukemia. Therefore, hypereosinophilic
syndrome (HES) complicated with eosinophilic cystitis was diagnosed
and oral prednisone with a slow tapering regimen was administered
to the patient for 6 weeks.
During the follow-up period of six months, the
laboratory examinations revealed a fluctuant eosinophil count. At
the most recent examination, the level of eosinophilia was shown to
be 11%, which indicated a partial hematological remission. The
subsequent cystoscopy and random bladder mucosa biopsies showed
complete remission of cystitis histologically (Fig. 2).
Discussion
HES is an uncommon condition characterized by
eosinophilia and multiple organ damage. The disease has a
significant male dominance and is usually diagnosed between the
ages of 20 and 50 years (4).
Currently, the pathophysiology of HES is not well described. The
dysregulated overproduction of eosinophils may be due to a number
of reasons, including the overproduction or dysfunction of
eosinophilopoietic cytokines, such as interleukin-5, and clonal
eosinophilic proliferation subsequent to primary abnormalities in
the hematopoietic stem cells. There are three diagnostic criteria
for HES. Firstly, persistent eosinophilia of >1.5×109
cells/l. Secondly, the exclusion of secondary causes of
eosinophilia, including allergic reactions or parasitic infection,
and finally organ damage (5). In
addition, according to World Health Organization’s classification
of myeloid neoplasm and acute leukemia, the diagnosis of HES
requires the exclusion of other acute or chronic myeloid neoplasms
(6). The conversion of HES to
acute leukemia is infrequent.
Eosinophilic cystitis associated with HES is a rare
clinical entity. To the best of our knowledge, only five cases have
been reported in the literature (3,7–10).
The most common symptoms caused by eosinophilic cystitis include
dysuria, gross hematuria and suprapubic pain during micturition
(11). However, the mechanisms
underlying how and why these overproduced eosinophils infiltrate
the bladder and cause the specific symptoms remain unclear. It has
been hypothesized that eosinophilic tissue damage is associated
with the release of major basic protein, eosinophil peroxidase,
eosinophil cationic protein and eosinophil-derived neurotoxin
(8). In imaging examinations, the
bladder wall exhibits diffuse or localized thickening. The
characteristic observation with cystoscopy is erythematous edema,
which may be easily mistaken as an invasive tumor or glandular
cystitis. Thus, tissue biopsy is essential to establish a definite
diagnosis and eliminate possible concomitant bladder
malignancies.
Due to the limited number of HES cases, there is no
standard guideline therapy for the management of HES and there is
no known cure for eosinophilic cystitis. Thus, individualized
treatment and close follow-up examinations are essential. The aim
of therapy should be to reduce the excessive production of
eosinophils in order to prevent organ damage (10). As indicated by the majority of
reported cases, prednisone is recommended as the primary drug.
Symptomatic patients should be treated with prednisone therapy (1
mg/kg per day) until clinical improvement occurs, followed by a
slow tapering regimen of prednisone. The majority of patients
experience complete or partial remission following corticosteroid
treatment. For symptomatic patients with intracrable disease which
is non-responsive to steroids, chemotherapeutic agents, including
hydroxyurea, vincristine, 6-mercaptoputine, busulfan and
chlorambucil, should be administered. In the present case, partial
hematological remission was achieved following prednisone therapy.
However, the bladder infiltration was resolved completely.
Therefore, we hypothesize that prednisone is an effective agent in
reducing organ eosinophilic infiltration and preventing organ
damage.
In conclusion, the present study has described a
case of HES with eosinophilic cystitis as the initial
manifestation. Although this is an uncommon inflammation condition,
eosinophilic cystitis should be considered when encountering an HES
patient with urinary symptoms.
References
|
1
|
Hardy WR and Anderson RE: The
hypereosinophilic syndromes. Ann Intern Med. 68:1220–1229. 1968.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chusid MJ, Dale DC, West BC and Wolff SM:
The hypereosinophilic syndrome: analysis of fourteen cases with
review of the literature. Medicine (Baltimore). 54:1–27. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kojima K, Maeda J, Mikami S, et al:
Eosinophilic cystitis presented as a manifestation of
hypereosinophilic syndrome: a case report and review of the
literature. Nephron Extra. 3:30–35. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fauci AS, Harley JB, Roberts WC, Ferrans
VJ, Gralnick HR and Bjornson BH: NIH conference. The idiopathic
hypereosinophilic syndrome Clinical, pathophysiologic, and
therapeutic considerations. Ann Intern Med. 97:78–92. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Klion AD, Bochner BS, Gleich GJ, et al:
Approaches to the treatment of hypereosinophilic syndromes: a
workshop summary report. J Allergy Clin Immunol. 117:1292–1302.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vardiman JW, Thiele J, Arber DA, et al:
The 2008 revision of the World Health Organization (WHO)
classification of myeloid neoplasms and acute leukemia: rationale
and important changes. Blood. 114:937–951. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dinary B, Shaheen K, Eisa N, Alraies MC,
Alraiyes AH and Ravakhah K: Hypereosinophilic syndrome induced
cystitis mimicking bladder tumor. N Am J Med Sci. 5:331–333. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Amin MA, Hamid MA and Saba S:
Hypereosinophilic syndrome presenting with eosinophilic colitis,
enteritis and cystitis. Chin J Dig Dis. 6:206–208. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hosoki K, Nagao M, Iguchi K, et al: An
8-year-old boy with hypereosinophilic syndrome. Int Arch Allergy
Immunol. 155(Suppl 1): 117–122. 2011.PubMed/NCBI
|
|
10
|
Nofal R: Eosinophilic cystitis as symptom
of an idiopathic hypereosinophilic syndrome. Aktuelle Urol.
38:148–151. 2007.(In German).
|
|
11
|
Popescu OE, Landas SK and Haas GP: The
spectrum of eosinophilic cystitis in males: case series and
literature review. Arch Pathol Lab Med. 133:289–294.
2009.PubMed/NCBI
|