Introduction
Severe acute pancreatitis (SAP) is a serious
surgical disease with a high mortality rate (1). The incidence of SAP has increased
markedly in recent years. A number of clinical and experimental
studies have been conducted to investigate the pathogenesis of SAP;
however, the exact mechanism underlying the pathogenesis of SAP
remains unclear (2,3). In addition, the effect of
conventional treatments is not satisfactory and there is no
specific therapy for SAP (4).
Previous studies have shown that a pathological change in
pancreatic microcirculation plays an important role in acute
pancreatitis, with a local disorder in pancreatic microcirculation,
microvascular thrombosis and blood flow blockage able to cause SAP
(5,6). Following the occurrence of SAP,
leukocytes are activated and accumulate immediately in the
pancreatic tissue. Subsequently, inflammatory mediators are
released, leading to an increase in pancreatic microvascular spasm
and permeability. Thus, pancreatic tissue ischemia-reperfusion
damage appears, and through the ‘waterfall cascade’, local acute
pancreatitis lesions rapidly develop into systemic inflammatory
response syndrome (7). The
intestinal tract is the largest reservoir of bacteria, and the
intestinal mucosa functions as the barrier for the body to prevent
bacteria and endotoxin invasion (8). While the gastrointestinal system is
functioning normally, bacteria and endotoxin pass out from the
bowels, without bacterial translocation and endotoxin absorption.
However, once SAP occurs, the immune barrier is impaired, leading
to bacteria and endotoxin invasion into the blood system (9). This further promotes the systemic
inflammatory response by activating inflammatory cells and
releasing cytokines and inflammatory mediators. A systemic
inflammatory response can cause extensive damage to various organs
of the body. Previous studies have indicated that pancreatic
ischemia may be a key causative factor for hemorrhage and necrosis
(10,11). In addition to the necrosis of
pancreatic tissues, the microcirculation disorder characterized by
ischemia is associated with the development of pancreatic
hemorrhage and necrosis (12).
Traditional Chinese medicine has been used for the
treatment of acute pancreatitis in China for a number of years.
Certain traditional Chinese medicines, with their essential roles
in epithelial cell integrity and immune function, have been shown
to be important for the maintenance of gut barrier function
(13). Lai Fu Cheng Qi decoction
is one of the most widely used basic formulas. The decoction is
considered to exert certain protective effects on the
gastrointestinal tract and systemic organs, with functions
including the regulation of gastrointestinal peristalsis,
increasing the electroactivity of the intestinal smooth muscle and
motilin release (14). Despite
wide application, the beneficial effects of this Chinese
prescription are controversial and the exact mechanisms underlying
the protective function remain unknown. Thus, the aim of the
present study was to investigate the protective effect of Lai Fu
Cheng Qi decoction on myocardial injury induced by SAP in rats and
the possible underlying mechanism.
Materials and methods
Reagents and instruments
Lai Fu Cheng Qi decoction was provided by the
General Hospital Affiliated to Tianjin Medical University (Tianjin,
China). The prescription consisted of 20 g Rheum palmatum
L., 15 g Mirabilite, 15 g Magnolia officinalis Rehd et
Wils., 10 g Fructus Aurantii, 15 g Semen Raphani, 10 g Radix
Aucklandiae and 10 g Achyranthes bidentata. Sodium
taurocholate was purchased from Beijing Bioxin Biological
Technology Co., Ltd. (Beijing, China). An ATPase detection kit was
purchased from Nanjing Jiancheng Biological Engineering Institute
(#A070-1; Nanjing, China) and a bicinchoninic acid (BCA) protein
assay kit was provided by Beijing Gainingjinnuo Biotechnology Co.,
Ltd. (Beijing, China). A Tissue Mitochondria Isolation Kit was
purchased from the Beyotime Institute of Biotechnology (#C3606;
Haimen, China) and a TUNEL in situ cell apoptosis detection
kit was purchased from Beijing Dingguochangsheng Biotechnology Co.,
Ltd. (#TUNEL-A1; Beijing, China). Serum biochemical indexes were
detected using a Vitros 250 automatic biochemical analyzer (Johnson
& Johnson, Rochester, NY, USA). A Cell Lab Quanta SC (CLQSC)
Flow Cytometer was obtained from Beckman Coulter (Miami, FL, USA)
and an Olympus CK40 inverted microscope was purchased from Olympus
Corporation (Tokyo, Japan).
Animals and grouping
In total, 30 male Sprague-Dawley rats with a body
mass of 200–250 g were provided by Beijing Weitong Lihua
Experimental Animal Technology Co., Ltd. (Beijing, China). The
animals were housed in standard conditions with free access to food
and water. All animal experiments were conducted according to the
ethical guidelines of Tianjin Medical University, and all efforts
were made to minimize animal suffering. The study was approved by
the ethics committee of Tianjin Medical University.
The animals were randomly divided into three groups,
which included the sham (n=10), SAP (n=10) and the Lai Fu Cheng Qi
decoction treatment group (n=10).
Model preparation and administration
SAP was induced in the SAP and decoction treatment
groups by a retrograde pancreatic duct injection of 5% sodium
taurocholate (1 ml/kg body weight). Briefly, an incision was made
in the abdomen at ~1 cm under the xiphoid midline following
anesthetization using 10% chloral hydrate (3 ml/kg; China
Pharmaceutical Group Shanghai Reagent Company, Shanghai, China).
Once the biliopancreatic duct and the duodenal papilla opening was
located, a syringe needle was placed (from the intestinal wall
contralaterally to the duodenal nipple) into the biliopancreatic
duct through the duodenal papillary opening on the cholo-pancreatic
duct. After clipping the cholangitic porta hepatis with a small
artery clamp, 5% sodium taurocholate was slowly infused (0.1
ml/min) retrogradely into the pancreatic duct. At 5 min after the
injection, the syringe and arterial clamp were removed, the
incision was sutured, and the abdomen was closed. In the sham
group, an incision was made in the abdomen and the pancreatic
tissue was marginally rotated several times prior to closing the
abdomen. The abdomen was closed without a sodium taurocholate
injection.
At 8 and 16 h after model preparation, the rats in
the decoction treatment group received an intragastric
administration of Lai Fu Cheng Qi decoction (2.5 ml/kg body
weight). As controls, the rats in the sham and SAP groups received
an equal volume of saline by intragastric administration.
Specimen collection
General conditions of the rats following modeling
were observed. At 24 h after modeling, three rats in the SAP group
and one rat in the decoction treatment group had died. The
remaining rats in all three groups were euthanized by
intraperitoneal injection of 10% chloral hydrate at 24 h after
modeling. The abdomen was opened by surgery, and the pancreas and
heart were removed. In addition, blood from the abdominal aorta was
collected. The aforementioned procedures were all performed under
sterile conditions. The heart tissue was dissected into four
sections on ice, and these four sections were used for the
detection of Na+-K+-ATPase activity,
mitochondrial membrane potential, myocardial cell apoptosis and
pathological examination.
Detection of serum creatine kinase
isoenzyme (CK-MB) and lactate dehydrogenase (LDH) levels
Arterial blood was naturally coagulated at room
temperature for 1 h. The blood was subsequently centrifuged at
1006.2 × g for 10 min at 4°C to collect the serum. The CK-MB and
LDH concentrations in the serum were detected using the Vitros 250
automatic biochemical analyzer.
Detection of
Na+-K+-ATPase activity in the myocardial
cells
One section of the heart tissue was ground into a
homogenate, and the Na+-K+-ATPase activity
was detected using a spectrophotometric method, as previously
described (15,16). The experiment was conducted
according to the instructions provided in the ATPase detection kit.
Briefly, protein levels in the heart homogenate were determined
using the BCA protein assay kit. The optical density (OD) of the
color developed was measured at a wavelength of 562 nm in a
spectrophotometer (Beijing Puxi General Instrument Co., Ltd.,
Beijing, China). The Na+-K+-ATPase activity
was expressed as U/mgprot and was calculated based on the following
formula: Na+-K+-ATPase activity = [(OD of
test tube − OD of control tube)/(OD of standard tube − OD of
control tube)] × concentration of standard tube (0.02 μmol/ml) × 6
× 7.8/protein level of the homogenate (mgprot/ml).
Detection of the mitochondrial membrane
potential in the myocardial cells
Using one section of the heart tissue, mitochondria
were isolated using the myocardial mitochondria isolation kit and
were used to detect the mitochondrial membrane potential. Briefly,
the isolated mitochondria were resuspended in 0.5 ml
phosphate-buffered saline (Wuhan Boster Biotechnology, Ltd., Wuhan,
China), and 10 μl rhodamine 123 working solution (Sigma-Aldrich,
St. Louis, MO, USA) was added and incubated with the mitochondria
at 37°C in 5% CO2 for 15 min. Following incubation, the
mitochondrial membrane potential was analyzed on a flow cytometer
with an excitation wavelength of 488 nm and an emission wavelength
of 633 nm.
Detection of myocardial cell apoptosis
with a TUNEL assay
A TUNEL assay was performed according to the
instructions of the apoptosis detection kit. The nuclei of the
apoptotic cells exhibited brown/yellow staining, while those of
non-apoptotic cells and the negative control were stained blue. The
number of apoptotic cells was counted in each group and the
apoptotic index (apoptotic cell number/total cell number × 100%)
was calculated.
Hematoxylin and eosin (HE) staining
Pancreatic tissues and one section of the heart
tissue were fixed in 4% paraformaldehyde and embedded in paraffin
(Beijing Dingguochangsheng Biotechnology Co., Ltd.). The tissues
were sliced into sections and stained with HE (Beijing CellChip
Biotechnology Co. Ltd., Beijing, China). Briefly, the tissue
sections were dewaxed in xylene (Tianjin East Tengen Fine Chemical
Reagent Co., Tianjin, China) and rehydrated in graded alcohols.
After washing with running water and distilled water, the sections
were stained with hematoxylin for 3–5 min. Following a second wash
with running water, the sections were differentiated with 1% HCl in
70% alcohol. Subsequently, the sections were stained with eosin for
1–4 min after washing with running water. Following dehydration and
differentiation in alcohol, the sections were mounted on cover
slips and observed under light microscopy.
Pathological scoring system
The morphology of the pancreas and heart was
evaluated by professional pathologists and the severity of the
pathological changes was scored according to previous studies
(17,18). According to the pathological
changes in edema, infiltration of inflammatory cells, hemorrhage
and necrosis in the pancreatic tissues, the following pathological
scores were proposed: 0, no pathological changes; 1, mild
pathological changes; 2, moderate pathological changes; 3, severe
pathological changes; and 4, very severe pathological changes.
According to the pathological changes with regard to infiltration
of inflammatory cells and myocardial necrosis in the heart tissues,
the following pathological scores were proposed: 0, no pathological
changes; 1, mild pathological changes; 2, moderate pathological
changes; 3, severe pathological changes; 4, very severe
pathological changes; and 5, extremely severe pathological changes.
The pathological scores of the pancreas (maximum, 16) and heart
(maximum, 20) were the total pathological scores, inlcuding the
scores for edema, infiltration of inflammatory cells, hemorrhage
and necrosis.
Statistical analysis
Data are expressed as the mean ± standard deviation
and SPSS statistical software, version 13.0 (SPSS, Inc., Chicago,
IL, USA) was used for statistical analysis. The mortality rates
were analyzed using Fisher’s exact probability for a 2×2
contingency table. Comparisons between groups were analyzed using
one-way analysis of variance. P<0.05 was considered to indicate
a statistically significant difference.
Results
General conditions of the rats following
modeling
Following the induction of SAP in the rats, the
general conditions of the rats were observed. In the sham group,
the general conditions of the rats prior to and following surgery
were good and did not change significantly. However, the general
conditions of the rats in the SAP group were relatively poor. Rats
in the SAP group exhibited symptoms of piloerection, laziness,
depression, lags in responses and shortness of breath. Three rats
had died at 24 h after modeling; thus, the mortality rate was 30%
in the SAP group. Following treatment with Lai Fu Cheng Qi
decoction, the general conditions of the rats in the decoction
treatment group were improved. For example, the symptoms of
depression and the lags in responses gradually disappeared. Only
one rat had died at 24 h after modeling; thus, the mortality rate
was 10% in the decoction treatment group. However, there was no
statistically significant difference in the morbidity rate between
the SAP and decoction treatment groups (data not shown), indicating
that the general conditions of the SAP rats were improved by
treatment with Lai Fu Cheng Qi decoction.
Lai Fu Cheng Qi decoction treatment
decreases the serum levels of CK-MB and LDH in SAP rats
To determine the effect of Lai Fu Cheng Qi decoction
on the serum levels of CK-MB and LDH, the concentrations of CK-MB
and LDH in the serum were measured using an automatic biochemical
analyzer (Table I). Compared with
the sham group, the serum levels of CK-MB and LDH in the SAP and
decoction treatment groups increased significantly (P<0.01).
However, the levels of CK-MB and LDH in the decoction treatment
group were significantly lower compared with those in the SAP group
(P<0.01). These results indicated that SAP increased the levels
of CK-MB and LDH in the serum; however, this increase was inhibited
by administration of Lai Fu Cheng Qi decoction.
 | Table IEffect of Lai Fu Cheng Qi decoction on
the serum CK-MB and LDH levels. |
Table I
Effect of Lai Fu Cheng Qi decoction on
the serum CK-MB and LDH levels.
| Group | Cases (n) | CK-MB (μ/ml) | LDH (μ/l) |
|---|
| Sham group | 10 | 639.33±37.72 | 593.17±45.43 |
| SAP group | 7 |
2133.29±111.60a |
1873.71±141.86a |
| Decoction treatment
group | 9 |
1332.78±120.39a,b | 953.11±74.23a,b |
Lai Fu Cheng Qi decoction treatment
increases the Na+-K+-ATPase activity of
myocardial cells in SAP rats
To evaluate the effect of Lai Fu Cheng Qi decoction
on Na+-K+-ATPase activity, the
Na+-K+-ATPase activity of the myocardial
cells was detected using a spectrophotometric method. As shown in
Table II, the
Na+-K+-ATPase activity of the myocardial
cells in the SAP group was significantly lower compared with that
of the sham group (P<0.01). In addition, the
Na+-K+-ATPase activity in the decoction
treatment group was significantly lower compared with that in the
sham group (P<0.01). However, the decoction treatment group had
a significantly higher level of Na+-K+-ATPase
activity when compared with the SAP group (P<0.01). These
results indicated that SAP reduced the
Na+-K+-ATPase activity of myocardial cells,
while Lai Fu Cheng Qi decoction was able to reverse the effect of
SAP by increasing the Na+-K+-ATPase
activity.
 | Table IIEffect of Lai Fu Cheng Qi decoction on
Na+-K+-ATPase activity. |
Table II
Effect of Lai Fu Cheng Qi decoction on
Na+-K+-ATPase activity.
| Group | Cases (n) |
Na+-K+-ATPase
activity (U/mgprot) |
|---|
| Sham group | 10 | 10.65±0.96 |
| SAP group | 7 | 4.62±0.51a |
| Decoction treatment
group | 9 | 8.06±0.73a,b |
Lai Fu Cheng Qi decoction treatment
increases the myocardial mitochondrial membrane potential
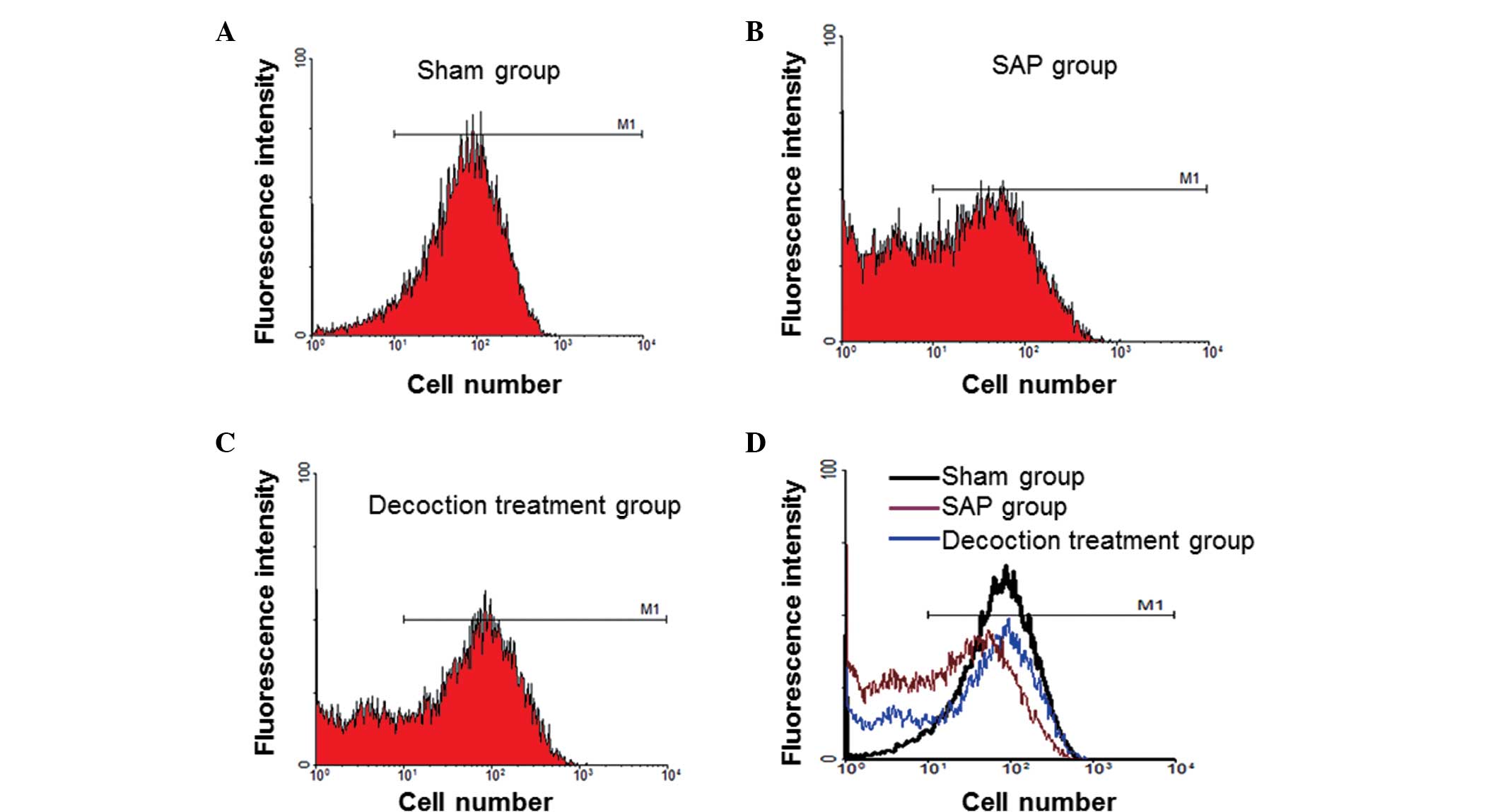
To analyze the effect of Lai Fu Cheng Qi decoction
on the mitochondrial membrane potential, mitochondria of the
myocardial cells were isolated and the mitochondrial membrane
potential was measured by flow cytometric analysis. Representative
flow cytometry results are shown in Fig. 1. Cells that did not exhibit a
decrease in mitochondrial membrane potential were counted and the
percentage was calculated (Table
III). In the SAP group, the ratio of cells without a decrease
in mitochondrial membrane potential was significantly lower
compared with the sham group (P<0.01). Following treatment with
Lai Fu Cheng Qi decoction, the ratio of cells without a decrease in
mitochondrial membrane potential was significantly higher when
compared with the SAP group (P<0.05). Compared with the rats in
the sham group, the rats in the decoction treatment group exhibited
a significantly lower ratio of cells without a decrease in
mitochondrial membrane potential. These results indicated that the
mitochondrial membrane potential of myocardial cells decreased
following SAP induction, while Lai Fu Cheng Qi decoction was able
to reverse the effect of SAP by increasing the mitochondrial
membrane potential.
 | Table IIIEffect of Lai Fu Cheng Qi decoction
on the mitochondrial membrane potential. |
Table III
Effect of Lai Fu Cheng Qi decoction
on the mitochondrial membrane potential.
| Group | Cases (n) | Cells without a
decrease in mitochondrial membrane potential (%) |
|---|
| Sham group | 10 | 95.13±1.94 |
| SAP group | 7 | 45.59±2.97a |
| Decoction treatment
group | 9 | 66.61±3.99a,b |
Lai Fu Cheng Qi decoction treatment
decreases the rate of apoptosis of myocardial cells in SAP
rats
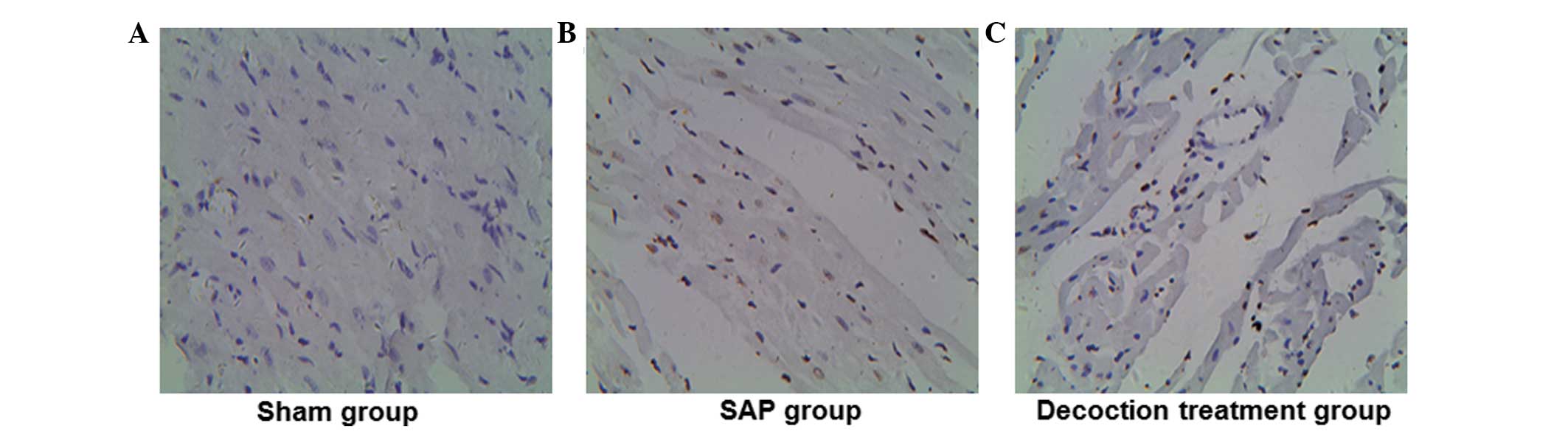
To investigate the effect of Lai Fu Cheng Qi
decoction on the rate of myocardial apoptosis in rats with SAP, a
TUNEL assay was performed. Representative TUNEL assay results are
shown in Fig. 2. The nuclei of the
apoptotic cells were stained brown/yellow, while those of
non-apoptotic cells and the negative control were stained blue. In
the sham group (Fig. 2A), the
majority of the nuclei in the myocardial cells were stained blue
and only a few myocardial cells exhibited brown/yellow staining in
the nuclei. However, in the SAP group, a large number of myocardial
cells exhibited brown/yellow staining in the nuclei (Fig. 2B). In addition, the number of cells
with brown/yellow staining in the decoction treatment group was
higher compared with that in the sham group, whereas the number was
lower when compared with the SAP group (Fig. 2C). The number of apoptotic cells
was counted in each group and the apoptotic index (apoptotic cell
number/total cell number × 100%) was calculated. As shown in
Table IV, the apoptosis index in
the SAP group was significantly higher when compared with the sham
group (P<0.01). Although the apoptosis index of the decoction
treatment group was significantly higher compared with that of the
sham group (P<0.01), when compared with the SAP group, the
apoptosis index of the decoction treatment group decreased
significantly (P<0.01). These results indicated that Lai Fu
Cheng Qi decoction treatment alleviated the rate of apoptosis
induced by SAP in myocardial cells.
 | Table IVEffect of Lai Fu Cheng Qi decoction
on the apoptosis of myocardial cells. |
Table IV
Effect of Lai Fu Cheng Qi decoction
on the apoptosis of myocardial cells.
| Group | Cases (n) | Apoptosis index
(%) |
|---|
| Sham group | 10 | 1.76±0.54 |
| SAP group | 7 | 31.62±4.68a |
| Decoction treatment
group | 9 | 24.06±3.75a,b |
Lai Fu Cheng Qi decoction treatment
alleviates the pathological features of the pancreas and heart in
SAP rats
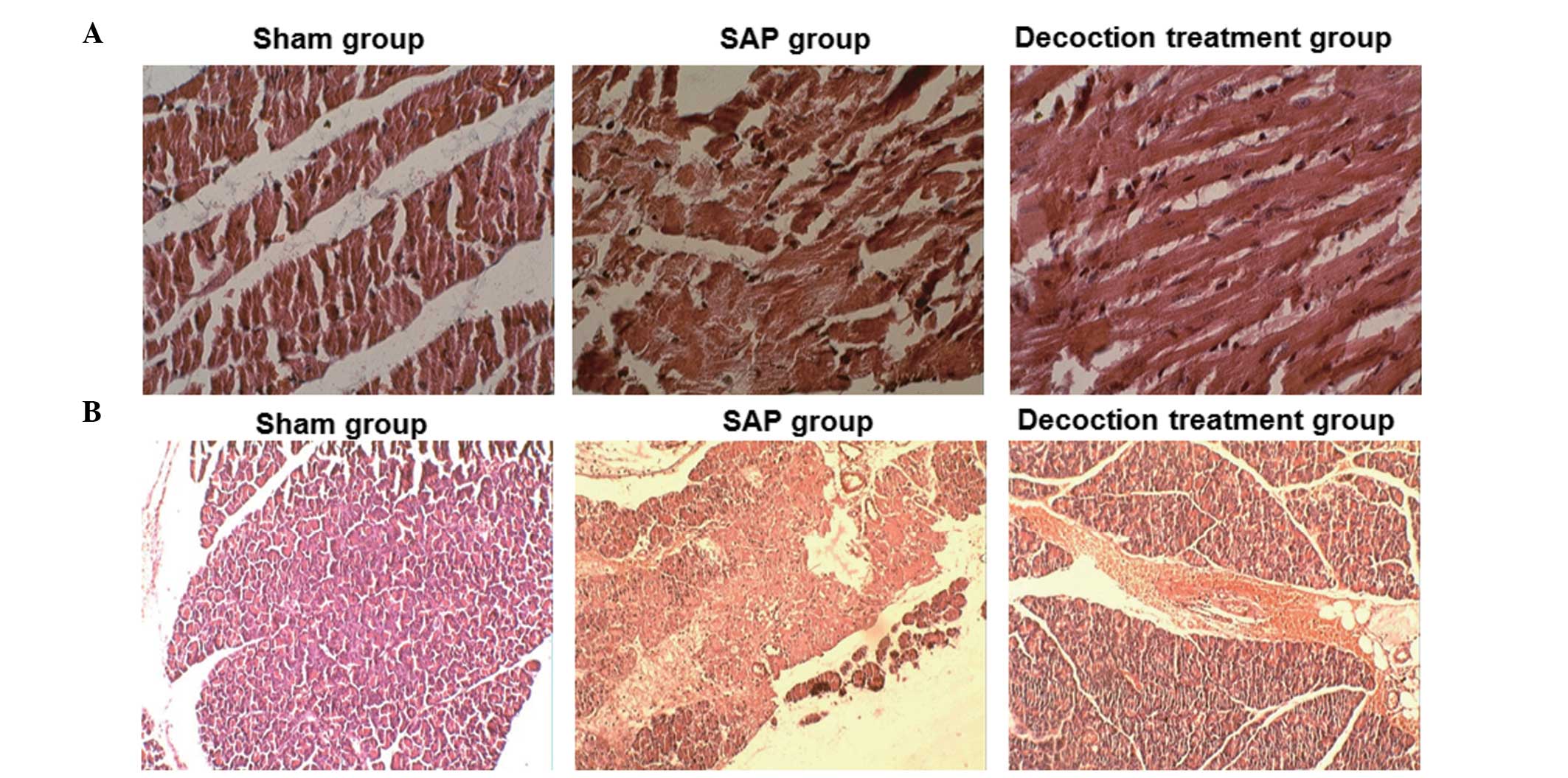
To detect the effects of Lai Fu Cheng Qi decoction
on the pathological changes to the pancreas and heart, HE staining
was performed. Representative HE staining results are shown in
Fig. 3. The morphology of the
pancreas and heart was evaluated by professional pathologists. The
sham group exhibited a normal morphology of the pancreas (Fig. 3A), and no marked pathological
changes were observed. By contrast, the SAP group revealed
morphological changes of interstitial edema, interstitial
hemorrhage, hemorrhage, necrosis and fat necrosis. The necrotic
area was infiltrated with inflammatory cells, which consisted
primarily of neutrophils, and the lobular structure was destructed.
Following treatment with Lai Fu Cheng Qi decoction, the
pathological features of the pancreas in the decoction treatment
group were found to improve. Similarly, as shown in Fig. 3B, the sham group exhibited a normal
morphology of the myocardial tissue and no significant pathological
changes were observed. However, in the SAP group, the myocardial
fibers were significantly degenerated and swelled. The majority of
the myocardial fiber structures had disappeared and a number of the
myocardial membranes were broken. The myocardial fibers were
arranged disorderly and the blood vessels exhibited congestion. The
aforementioned pathological changes were consistent with the
pathological features of myocardial injury induced by SAP.
Following treatment with Lai Fu Cheng Qi decoction, the
pathological features of the heart in the decoction treatment group
were improved. However, edema and mild degeneration of the
myocardial fibers was observed in the decoction treatment group,
and a number of myocardial fibers had lost cross striations.
In addition, the severity of the pathological
changes was scored. The pathological scores of the pancreas and
heart are shown in Table V. When
compared with the sham group, the pathological scores of the
pancreas and heart in the SAP and decoction treatment groups were
significantly higher (P<0.01). However, following treatment with
Lai Fu Cheng Qi decoction, the pathological scores of the pancreas
and the heart in the decoction treatment group were significantly
lower compared with those in the SAP group (P<0.01).
 | Table VEffect of Lai Fu Cheng Qi decoction
on the pathological scores of the pancreas and heart. |
Table V
Effect of Lai Fu Cheng Qi decoction
on the pathological scores of the pancreas and heart.
| Group | Cases (n) | Pathological scores
of the pancreas | Pathological scores
of the heart |
|---|
| Sham group | 10 | 1.67±0.82 | 0 |
| SAP group | 7 | 12.14±1.35a | 2.86±0.69a |
| Decoction treatment
group | 9 | 6.33±1.41a,b | 1.67±0.50a,b |
Collectively, these results indicated that SAP
induced injury in the pancreas and the heart; however, these
injuries were alleviated following treatment with Lai Fu Cheng Qi
decoction.
Discussion
Traditional Chinese medicine has been used for the
treatment of SAP for a number of years (19). In recent years, the effect of a
decoction and the component drugs have been studied systematically,
with significant progress achieved. The effect of decoction on SAP
is considered to be achieved by promoting gastrointestinal
peristalsis, protecting the intestinal barrier function, inhibiting
the functions of cytokines and other inflammatory mediators,
improving pancreatic microcirculation, protecting pancreatic cells
and subcellular organelles and inhibiting the function of
pancreatic enzymes (20,21). Lai Fu Cheng Qi decoction exerts
specific effects in addition to the aforementioned effects. Lai Fu
Cheng Qi decoction can increase the blood flow to the heart,
enhance the removal of oxygen free radicals, reduce endotoxin
release, inhibit cytokines induced by endotoxin and contribute to
inflammation attenuation (22).
These effects can further restore gastrointestinal peristalsis,
eliminate intestinal toxicant accumulation and reduce endotoxin
absorption (7). Additionally, Lai
Fu Cheng Qi decoction is known to be effective for the treatment of
SAP (23). According to clinical
observations, following the application of this decoction, the
abdominal symptoms in patients with SAP are relieved through the
excretion of stool and the reduction in endotoxin absorption.
Furthermore, the possibility of acquiring multiple organ
dysfunction syndrome is reduced. In the present study, the levels
of serum CK-MB and LDH, the mitochondrial membrane potential,
Na+-K+-ATPase activity, myocardial cell
apoptosis and the pathological changes to the pancreas and the
heart were examined, in order to further investigate the protective
mechanism of Lai Fu Cheng Qi decoction on SAP-induced myocardial
injury.
Following the establishment of SAP, the general
conditions of the rats were observed. In total, three rats from the
SAP group and one rat from the decoction treatment group had died
at 24 h after modeling. However, there were no statistically
significant differences in the morbidity rate between the SAP and
decoction treatment groups, which may be partly due to the small
sample size included in the study. In addition, the treatment time
of decoction in the current study design was only 24 h, which was
relatively limited. Therefore, further studies with a larger sample
size and a longer treatment time period are required.
Levels of CK-MB and LDH in the serum can be used as
markers of myocardial injury (24,25).
In the present study, changes in the serum levels of CK-MB and LDH
were also detected. The results demonstrated that the serum levels
of CK-MB and LDH in the SAP rats treated with Lai Fu Cheng Qi
decoction were significantly decreased. This result indicated that
the upregulation of serum CK-MB and LDH levels in SAP rats with
myocardial injury was inhibited by Lai Fu Cheng Qi decoction
treatment. Therefore, the results provide preliminary experimental
evidence that Lai Fu Cheng Qi decoction exerts myocardial
protective effects in rats with SAP.
A decrease in the mitochondrial membrane potential
is a sign of early apoptotic events (26). Rhodamine 123 is an indicator of
mitochondrial transmembrane potential. Through the fluorescence
signal intensity, the changes in mitochondrial membrane potential
and cell apoptosis at an early stage can be detected. In the
present study, the percentage of myocardial cells that did not
undergo a decrease in the mitochondrial membrane potential in the
decoction treatment group was significantly higher compared with
that of the SAP group. These results indicated that Lai Fu Cheng Qi
decoction was able to inhibit the decrease in mitochondrial
membrane potential induced by SAP, subsequently inhibiting the
apoptosis of myocardial cells.
Na+-K+-ATPase is an antiporter
enzyme located in the plasma membrane of all animal cells. The
Na+-K+-ATPase aids the maintenance of a
resting potential and regulates the cellular volume (27). The enzyme also functions as a
signal transducer/integrator to regulate the mitogen-activated
protein kinase signaling pathway, reactive oxygen species and
intracellular calcium. In the present study, the myocardial cell
Na+-K+-ATPase activity in the Lai Fu Cheng Qi
decoction treatment group was higher when compared with the SAP
group that did not receive treatment. Therefore, Lai Fu Cheng Qi
decoction may improve the activity of the
Na+-K+-ATPase, prevent intracellular calcium
overload, sustain the matrix volume stability and inhibit ischemia
and hypoxia; thus, exerting myocardial protective effects. The
myocardial protective effects of Lai Fu Cheng Qi decoction were
further verified by a TUNEL assay. The results revealed that the
apoptosis index of the decoction treatment group decreased
significantly when compared with the SAP group.
The pathological changes observed in the pancreatic
and myocardial tissues of the rats in the SAP group were consistent
with the injuries induced by SAP. Following treatment with Lai Fu
Cheng Qi decoction, the pathological features of the pancreas and
the heart were alleviated. However, the features of edema and
neutrophil infiltration remained in the decoction treatment group.
The severity of the pathological changes was graded. Consistently,
the pathological scores of the pancreas and heart in the decoction
treatment group were significantly lower compared with those in the
SAP group, indicating that Lai Fu Cheng Qi decoction was able to
improve the pathological changes induced by SAP.
In conclusion, the present study demonstrated that
Lai Fu Cheng Qi decoction is able to effectively decrease the serum
levels of CK-MB and LDH, increase
Na+-K+-ATPase activity, inhibit a decrease in
mitochondrial membrane potential and inhibit the apoptosis of
myocardial cells, subsequently reducing the myocardial injuries
induced by SAP. The present study is a pilot study that included a
limited number of rat models. Future studies with a larger sample
size and prospective trials are required to further investigate the
mechanisms underlying the protective effects of Lai Fu Cheng Qi
decoction on SAP-induced myocardial injury.
Acknowledgements
The authors thank Professor Yuechuan Li (Department
of Thoracic Medicine, Tianjin Chest Hospital) and Professor Meilin
Xu (Department of Pathology, Tianjin Chest Hospital) for their
assistance in the writing of the manuscript, the collection of the
literature data and specimens, and statistical analysis.
References
|
1
|
Harper SJ and Cheslyn-Curtis S: Acute
pancreatitis. Ann Clin Biochem. 48:23–37. 2011. View Article : Google Scholar
|
|
2
|
Chen Y, Zak Y, Hernandez-Boussard T, Park
W and Visser BC: The epidemiology of idiopathic acute pancreatitis,
analysis of the nationwide inpatient sample from 1998 to 2007.
Pancreas. 42:1–5. 2013. View Article : Google Scholar
|
|
3
|
Suzuki M, Sai JK and Shimizu T: Acute
pancreatitis in children and adolescents. World J Gastrointest
Pathophysiol. 5:416–426. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zerem E: Treatment of severe acute
pancreatitis and its complications. World J Gastroenterol.
20:13879–13892. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Foitzik T, Eibl G, Hotz HG, Faulhaber J,
Kirchengast M and Buhr HJ: Endothelin receptor blockade in severe
acute pancreatitis leads to systemic enhancement of
microcirculation, stabilization of capillary permeability and
improved survival rates. Surgery. 128:399–407. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Menger MD, Plusczyk T and Vollmar B:
Microcirculatory derangements in acute pancreatitis. J
Hepatobiliary Pancreat Surg. 8:187–194. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Klar E, Messmer K, Warshaw AL and Herfarth
C: Pancreatic ischaemia in experimental acute pancreatitis:
mechanism, significance and therapy. Br J Surg. 77:1205–1210. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Abreu-Martin MT and Targan SR: Regulation
of immune responses of the intestinal mucosa. Crit Rev Immunol.
16:277–309. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rychter JW, van Minnen LP, Verheem A, et
al: Pretreatment but not treatment with probiotics abolishes mouse
intestinal barrier dysfunction in acute pancreatitis. Surgery.
145:157–167. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi C, Zhao X, Lagergren A, Sigvardsson M,
et al: Immune status and inflammatory response differ locally and
systemically in severe acute pancreatitis. Scand J Gastroenterol.
41:472–480. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cuthbertson CM and Christophi C:
Disturbances of the microcirculation in acute pancreatitis. Br J
Surg. 93:518–530. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lehocky P and Sarr MG: Early enteral
feeding in severe acute pancreatitis: can it prevent secondary
pancreatic (super) infection? Dig Surg. 17:571–577. 2000.
View Article : Google Scholar
|
|
13
|
Chen H, Li F, Jia JG, Diao YP, Li ZX and
Sun JB: Effects of traditional Chinese medicine on intestinal
mucosal permeability in early phase of severe acute pancreatitis.
Chin Med J (Engl). 123:1537–1542. 2010.
|
|
14
|
Yu JN, Kou L and Wang J: Therapeutic
effect of Lai Fu Cheng Qi Decoction on severe acute pancreatitis
associated lung injury patients. Guo Ji Hu Xi Za Zhi. 11:859–862.
2012.(In Chinese).
|
|
15
|
Sarkar PK: A quick assay for
Na+-K+-ATPase specific activity. Z
Naturforsch C. 57:562–564. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vague P, Dufayet D, Coste T, Moriscot C,
Jannot MF and Raccah D: Association of diabetic neuropathy with
Na/K ATPase gene polymorphism. Diabetologia. 40:506–511. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xu YC, Li ZS, Tu ZX, Shi XG, Wang LZ, Gong
YF, Man XH and Jin J: Role of MCP-1/JE in pathogenesis of severe
acute pancreatitis. Yi Xian Bing Xue. 4:94–97. 2004.(In
Chinese).
|
|
18
|
Yu M, Yang YZ, Shen XD, Shu XH and Pan WM:
Evaluation of the cardiac function by high frequency
echocardiography in viral myocarditis mice. Zhonghua Chao Sheng
Ying Xiang Xue Za Zhi. 10:54–56. 2001.(In Chinese).
|
|
19
|
Lv B: Application of Chinese medicine in
the treatment of severe acute pancreatitis. Zhonghua Xiao Hua Za
Zhi. 33:743–745. 2013.(In Chinese).
|
|
20
|
Xia Q, Jiang JM, Gong X, Chen GY, Li L and
Huang ZW: Experimental study of Tong Xia purgative method in
ameliorating lung injury in acute necrotizing pancreatitis. World J
Gastroenterol. 6:115–118. 2000.
|
|
21
|
Jia P, Zhang Z, Zhou Z and Jiang J: Impact
of WPY on pancreatic microcirculation of acute pancreatitis in
mice. Hua Xi Yi Ke Da Xue Xue Bao. 32:92–95. 2001.(In Chinese).
|
|
22
|
Di H and You SY: Effect of Lai-Fu-Qi-Cheng
treatment on acute pancreatitis associated with intestinal
paralysis in 30 cases. Zhongguo Zhong Xi Yi Jie He Wai Ke Za Zhi.
15:128–129. 2009.(In Chinese).
|
|
23
|
Di H and You SY: Effect of Lai-Fu-Qi-Cheng
treatment on acute pancreatitis associated with intestinal
paralysis in 30 cases. Zhongguo Zhong Xi Yi Jie He Wai Ke Za Zhi.
15:128–129. 2009.(In Chinese).
|
|
24
|
Dahlin LG, Kågedal B, Nylander E, et al:
Early identification of permanent myocardial damage after coronary
surgery is aided by repeated measurements of CK-MB. Scand
Cardiovasc J. 36:35–40. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dai JZ and Fan H: Protective effects of
Danhong injection against heart injury in rats with severe acute
pancreatitis. Shi Jie Hua Ren Xiao Hua Za Zhi. 10:969–975. 2009.(In
Chinese).
|
|
26
|
Fraser JA and Huang CL: A quantitative
analysis of cell volume and resting potential determination and
regulation in excitable cells. J Physiol. 559:459–478. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Huigsloot M, Tijdens IB, Mulder GJ and van
de Water B: Differential regulation of doxorubicin-induced
mitochondrial dysfunction and apoptosis by Bcl-2 in mammary
adenocarcinoma (MTLn3) cells. J Biol Chem. 277:35869–35879. 2002.
View Article : Google Scholar : PubMed/NCBI
|