Introduction
During the course of studies investigating the
effects of natural products on the infectivity of viruses (1–6), the
survival of viruses outside of the infected cells has been found to
be strongly affected by environmental factors, indicating a role of
the environment in virus transmission. Transmission of influenza
virus is known to occur directly and indirectly (7,8).
Direct transmission occurs through inhalation of virus-containing
droplets, which are exhaled by an infected individual. Although
droplet-borne infection is considered to be the major route for
influenza virus transmission (9),
the role of transmission via the contact route has also been
emphasized (7,8). This indirect transmission occurs
primarily through hand contact with a virus-contaminated surface
around the infected individual. Viruses exhaled from the infected
person can be easily deposited on various surfaces that
subsequently come into contact with the uninfected individuals.
One potential source may be clothing, onto which the
droplets containing influenza virus can be deposited. However,
viruses are normally inactive outside of the infected cells or
bodies. Thus, the viruses may be inactive following deposit on the
clothing. By contrast, the viruses may be protected by the clothes
from environmentally inactivating conditions. In the latter case,
the binding of the virus to the clothes must be reversible in order
for transmission to occur. As a result, the efficiency of virus
transmission may be strongly affected by the survival of influenza
virus on the clothes and by the reversibility of the virus binding
to the clothes.
A small number of studies have investigated the role
of contaminated clothing in the transmission of viruses,
quantitatively or semi-quantitatively. Laevens et al
(10) examined the experimental
spread of swine fever virus by contaminated clothing and footwear
in pig housing. In addition, Lai et al (11) reported the inactivation and
survival of severe acute respiratory syndrome virus on hospital
gowns. Sakaguchi et al (12) demonstrated the long-term (>8 h)
survival (transmissibility) of influenza virus on clothing used in
a healthcare setting. However, in this study, the hospital gowns
were contaminated with 0.5 ml virus preparation; thus, the volume
was too large to examine the role of the deposit of
virus-containing droplets in an actual environment.
To examine the role of indirect transmission by the
virus-contaminated clothes in epidemics of influenza A virus, the
present study quantitatively examined the viability and
transmissibility of the virus from the contaminated surfaces of
various types of clothing.
Materials and methods
Clothing
In total, nine types of clothing were used as test
samples. The properties of these clothes are provided in Table I. The clothes had been worn for the
daily activities of college students (Wakayama Medical University
School of Health and Nursing Science, Wakayama, Japan); thus, had
the potential to be contaminated by influenza A virus during the
epidemic season. The clothing had been subjected to routine wearing
and washing for several months or years. The thickness of the cloth
was determined using a micrometer screw gauge and the samples were
cut into ~1.5-cm2 sections. Subsequently, the samples
were sterilized using an autoclave, and air-dried for several
days.
 | Table IProperties of the clothes and the
inactivation of influenza virus. |
Table I
Properties of the clothes and the
inactivation of influenza virus.
| Clothing | Materials | Color | Thickness (mm) | Relative remaining
virus infectivity at 20 min after deposita |
|---|
| Jersey | Polyester 100% | Navy blue | 0.16 | <0.001 |
| One-piece | Polyester 100% | Black | 0.39 | <0.001 |
| Jeans | Cotton 98%
Polyurethane 2% | Blue | 1.22 | <0.001 |
| Hemp pants | Cannabis
55%
Cotton 45% | Khaki | 0.52 | <0.001 |
| Black sweater | Acrylic fiber
100% | Black | 2.78 | 0.002 |
| Parka | Polyester 100 % | Gray | 1.02 | 0.004 |
| Cardigan | Cotton 100% | Pink | 1.43 | 0.014 |
| T-shirt | Cotton 100% | White | 0.78 | 0.17 |
| White sweater | Pilus 100% | White | 1.49 | 0.85 |
Cells and viruses
An MDCK cell line (obtained from Dr Nakajima, Nagoya
City University School of Medicine, Nagoya, Japan) was grown in
Eagle’s minimum essential medium (MEM; Nissui Pharmaceutical Co.,
Ltd., Tokyo, Japan) containing 5% fetal bovine serum. Influenza
virus A/PR/8/34 (H1N1) (obtained from Dr Nakajima) was used
throughout the experiments. The viruses were propagated in MDCK
cells cultured in MEM supplemented with 0.1% bovine serum albumin
(BSA) and acetylated trypsin (4 μg/ml). The viruses were stored at
−80°C until required for further use. The amount of infectious
virus was measured using a plaque assay on the MDCK cells, as
described previously (13).
Experimental contamination of the
clothing by influenza virus
A 10-μl aliquot of the stock virus preparation
(106–107 plaque-forming units/ml) was placed
on the surface of 15 (for triplicate samples) to 16 (for
quadruplicate samples) pieces of the test cloths in a glass Petri
dish, with a one minute interval. The contaminated cloths were left
in the dish without cover in a safety cabinet (Sanyo MHE-131AJ;
Panasonic Healthcare, Tokyo, Japan) under air blowing. The average
temperature and humidity in the cabinet was 27°C and 30%,
respectively. At the indicated time points after virus deposition,
one piece of the contaminated cloth was transferred into a glass
test tube, immediately followed by the addition of 1,000 μl
ice-cold Dulbecco’s phosphate-buffered saline (PBS) without
Ca2+ and Mg2+, but containing 0.1% BSA.
Vigorous mixing using a Vortex mixer was performed several times
for a few seconds to completely elute the inoculated virus into the
PBS from the cloths. All the test cloths were examined in
triplicate or quadruplicate. The virus samples were maintained in
an ice-water bath until the completion of sampling from all the
test cloths for comparison. At the end of sampling, aliquots of
these virus samples were serially diluted with ice-cold PBS
containing 0.1% BSA, and the amount of infectious virus in the
samples was measured. For a negative control without exposure to
the test cloths, a 10-μl aliquot of the stock virus preparation was
placed directly on the inner surface of the glass test tube with a
loose aluminum cap. The sample was kept in the safety cabinet for
the indicated period, followed by the addition of PBS containing
0.1% BSA at the indicated time.
Assessment of water evaporation from the
contaminated cloths
A 10-μl aliquot of a virus-free medium was
inoculated on the surface of the test cloths in a glass Petri dish.
The weight of the test cloths had previously been measured. The
samples were exposed to air without cover in a similar manner to
the aforementioned virus experiments, with the exception that the
virus was absent. The weight of the inoculated cloths was
determined in triplicate at 0, 10, 15 and 20 min after the
inoculation. The relative water content was calculated by dividing
the weight at each time point by the weight at time 0.
Results and Discussion
The potential risk of indirect transmission through
the contact of hands with virus-contaminated surfaces has been
increasingly emphasized as a cause of the pandemic spread of
influenza A virus, in addition to the classical direct transmission
by droplets from the infected individuals (7,8). To
quantitatively evaluate this potential risk of indirect
transmission among college students, the present study analyzed the
ability of influenza A virus to retain its infectivity and
transmissibility on clothing worn by students in daily life. In
total, nine types of clothing (Table
I) that had been used for several months or years as ordinary
clothes, with regular washing, were collected from students.
Humans can produce respiratory droplets by several
means, including breathing, talking, coughing and sneezing. Since
there are natural variations in the number and size of such
droplets generated from the same individual during these
activities, it is difficult to determine the size and number of
droplets. The size of the droplets exhaled by infected individuals
vary widely (μm-mm). Although the droplets with a smaller size are
likely to be dominant (9), in the
present study, a 10-μl volume (~2.7 mm in diameter if spherical)
was arbitrarily selected to quantitatively contaminate the clothing
with the virus. Namely, a 10-μl sample of virus preparation was
deposited on the test cloths and the contaminated cloths were
maintained in air for 20 min to mimic the actual situation that may
occur between the time of clothing contamination and the time of
exposure to the hands of the second individual. After leaving for
20 min in air, the cloths were transferred to glass test tubes, the
contaminated virus was extracted with PBS containing 0.1% BSA by
vigorous mixing with a Vortex mixer, and the amount of infectious
virus recovered in the extract was measured. Notably, the measured
values reflect only the infectious virus recovered in the extracts,
not those irreversibly absorbed on the cloths. Such irreversibly
bound viruses, even if infectious, are not transmissible to
others.
As shown in the last column of Table I, the amount of infectious virus
recovered markedly differed among the clothing samples. For the
jersey, one-piece, jeans and hemp pants, the recovered virus
infectivity was below the level of detection, indicating that
during the 20-min period, these cloths inactivated or irreversibly
bound the influenza virus. These cloths were followed by the black
sweater, parka and cardigan, in this order, with the cardigan the
least effective in inactivation or irreversible virus absorption.
There appeared to be essentially no or marginal loss of the virus
infectivity for the T-shirt and white sweater. These results
indicated that the ability of influenza A virus to retain
transmissibility in contaminated clothing strongly depended on the
nature of the clothes.
Four clothing samples (jersey, cardigan, T-shirt and
white sweater), that exhibited marked differences in the recovered
virus infectivity at 20 min (Table
I), were compared for the kinetics of the loss of infectivity.
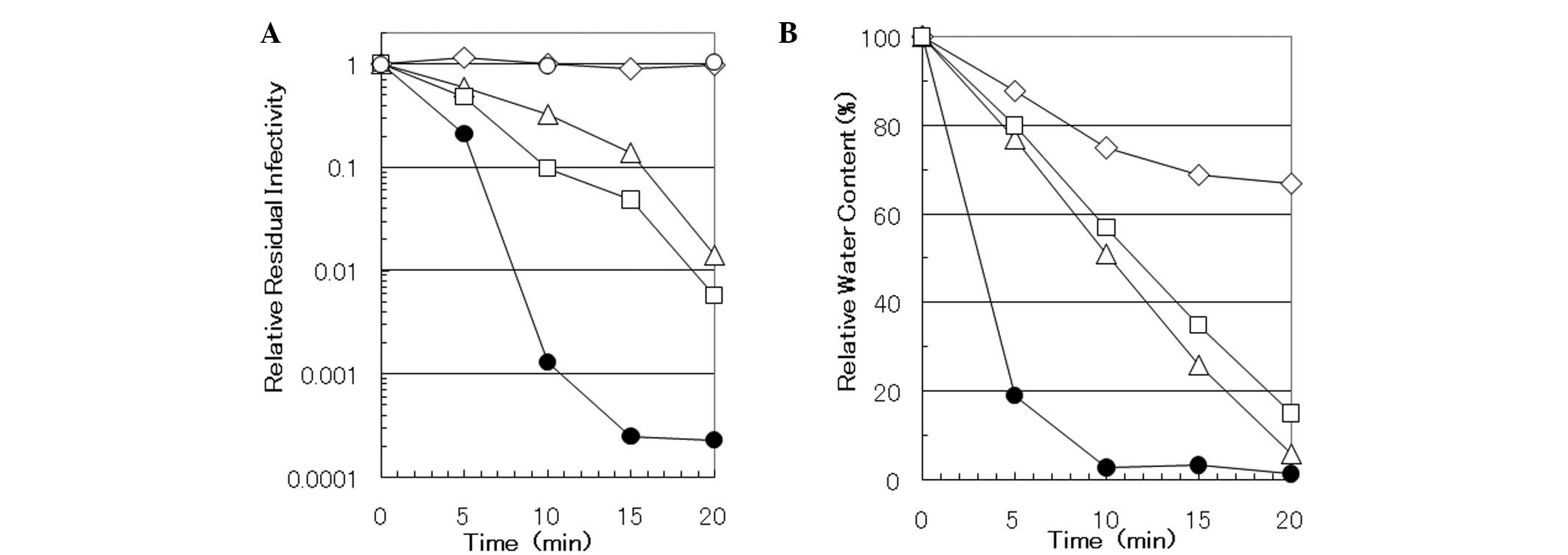
Fig. 1A shows the time course, in
which a trend is clear. For the white sweater, there was
essentially no loss of virus over the 20-min incubation period
(diamond), which was similar to the control (open circles), in
which the virus preparation was inoculated on the inner surface of
the glass test tube. For the cardigan (triangle) and T-shirt
(square), a gradual loss was observed, while virus infectivity was
rapidly lost for the jersey (closed circle). These results
correlate with the relative remaining virus infectivity at 20 min,
with the exception of the T-shirt. Variation for the T-shirt may
have been caused by differences among the clothing samples with
regard to the time necessary for the evaporation of water from the
deposit, since we observed that different samples from the same
items of clothing often showed variability in virus recovery, and
this variability was often very noticeable among independent
experiments. Although little experimental fluctuations were
observed for the PBS control and the white sweater, both the
cardigan and T-shirt, which were intermediate in virus recovery
(Fig. 1A), exhibited strong
variation among the experiments, suggesting that recovery from
these samples may be easily influenced by variations in the
experiments. The presence or absence of these variations in virus
recovery may be associated with the observation that the mode of
absorption of virus-containing liquid into test cloths is quite
variable among samples from different types of material, as well as
numerous samples from the same item of clothing. For example, the
absorbance of virus-containing solution was stable in all of the
samples from the white sweater, whereas in some samples from the
cardigan and T-shirt the solution was immediately absorbed, yet in
others it remained unabsorbed for a longer period of time. These
observations support the importance of water in the deposit for the
maintenance of the infectivity and transmissibility of influenza
virus on contaminated clothes.
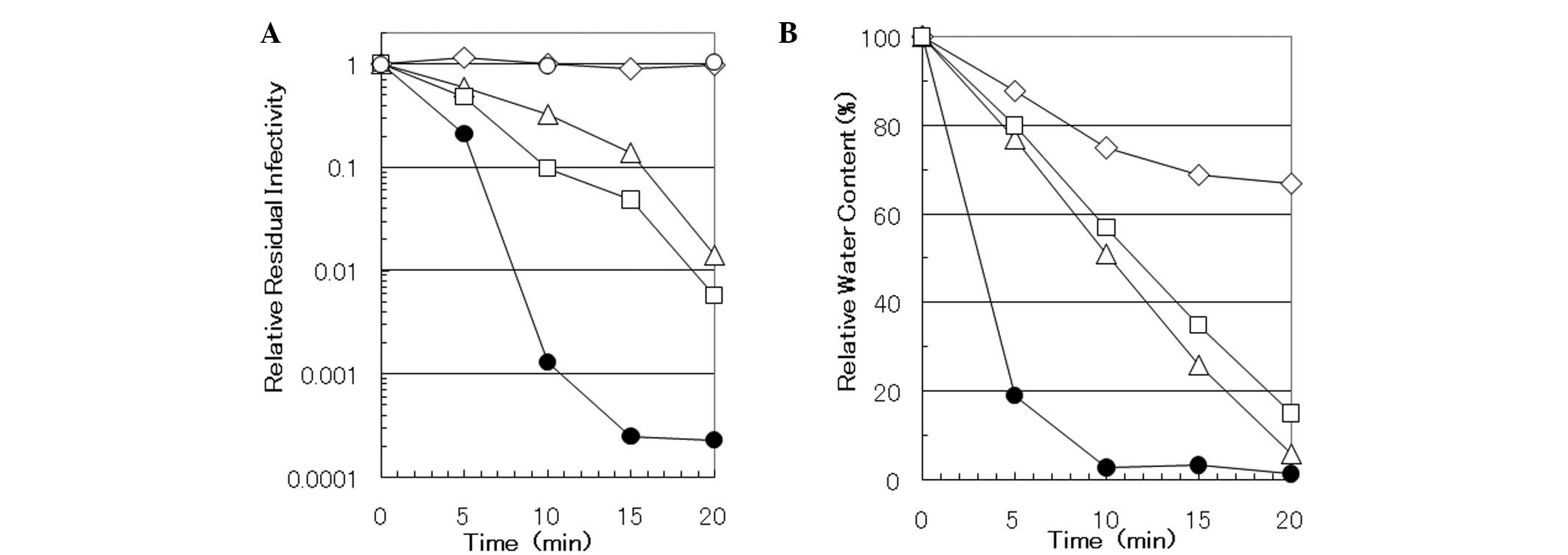 | Figure 1Time course of (A) virus-inactivation
and (B) water-evaporation of the clothing. (A) A virus preparation
was inoculated on the various cloths, which were subsequently
transferred to a test tube and incubated for 0, 5, 10, 15 and 20
min after the inoculation. Following extraction and determination
of virus infectivity, the relative residual infectivity was
calculated by dividing the infectivity at each time point by that
at time 0. (B) A virus-free medium was inoculated onto the test
cloths and the weight of the inoculated cloths was measured prior
to inoculation and at 0, 10, 15 and 20 min after inoculation. The
relative water content was calculated by dividing the water content
at each time point by that at time 0. ○, test tube; △, cardigan; □,
T-shirt; ●, jersey; ⋄, white sweater. |
Previously, a non-physiological pH was shown to
cause the inactivation of certain enveloped viruses (14); thus, pH alteration may be involved
in the observed decrease in the virus infectivity recovered in the
extracts. The pH of the sample cloths was measured by soaking in 20
volumes (volume/weight) of distilled water at room temperature for
3 or 48 h, with occasional mixing using a Vortex mixer. However,
the solution in all the cloth samples showed a neutral pH
regardless of the incubation time. Since the virus preparation was
developed using PBS containing 0.1% BSA, which exerts a strong
buffering function, the pH of the deposited solution on these
cloths at the site of inoculation should be even closer to a
neutral pH. These results indicated that the pH of the cloths
played no role in the different recoveries observed for the virus
infectivity from the test cloths.
In addition, the observed differences were not found
to correlate with the thickness of the material or with the types
of materials of the sample cloth (Table I). However, a dependence may exist
on the material color. Darker colored material appeared to cause a
greater loss in virus infectivity (black sweater and black
one-piece vs. white sweater; Table
I), indicating that the wavelength of light that is absorbed by
the cloths may be associated with the loss of virus
infectivity.
An aqueous environment is generally preferable for
virus survival; as described above, water loss from the
contaminated clothing may be associated with the observed virus
recovery and inactivation. In a safety cabinet, rapid airflow
maintains the sterility and bioprotective efficacy of the cabinet.
This airflow caused the evaporation of water from the sample cloths
over time. Time courses of evaporation from the jersey, cardigan,
T-shirt and white sweater were evaluated (Fig. 1B) by examining the relative amount
of residual water as a function of time. These four cloths
represent four water loss patterns of the nine cloths examined. The
jersey rapidly lost water, reaching >95% loss within 10 min
after leaving the contaminated cloths in the safety cabinet (closed
circle). Similar results were obtained for the one-piece; the
amount of residual water at 10 min after deposit was 3.3% of the
input, as compared with 2.8% of the input for the jersey. These two
cloths exhibited a virus recovery that was below the detection
level at 20 min after the deposit of virus suspension on the cloths
(Table I). By contrast, the white
sweater lost little water over time, with ~70% of the water
remaining after 20 min (diamond); this sample conferred the highest
virus recovery among the test cloths (Table I and Fig. 1A). The other two sample cloths
exhibited intermediate water evaporation between the jersey and
white sweater, with the water content of the cardigan (triangle)
and T-shirt (square) exhibiting water loss of ~20% for every 5-min
interval. Essentially similar results were obtained for the parker
and black sweater. These cloths showed intermediate virus
recoveries in Table I. Therefore,
the results demonstrated a correlation between water loss and virus
recovery; namely, the cloth samples that lost water faster yielded
the lower virus recovery (fewer transmissible infectious viruses).
In addition, the rate of water loss appeared to be associated with
the water-repelling nature (hydrophobic) of the cloths; the cloths
that were more hydrophilic lost water faster (data not shown).
Transmission of influenza virus is known to occur
both directly and indirectly. The present study examined the
recovery of influenza virus from experimentally virus-contaminated
clothing, in order to understand the role of contaminated clothes
in the transmission of influenza A virus during an epidemic period.
Although the amount of infectious virus recovered from the
contaminated clothes was markedly different between the clothing
samples, the difference in recovery correlated with the residual
amount of water in the deposited virus preparation on the test
cloths. Considering that water from natural droplets would quickly
evaporate once the droplet had fallen onto the clothes, indirect
transmission of influenza through virus-contaminated clothing may
occur, if only under limited circumstances. To understand the role
of indirect transmission, further work is required; such as the
study of the survival of viruses on contaminated hands and
environmental surfaces, such as doorknobs and household
furniture.
Acknowledgements
The study was supported in part by a Grant-in-Aid
for Challenging Exploratory Research (no. 23660017) and for
Scientific Research (C) (no. 25463335) from the Japan Society for
the Promotion of Science. The authors thank Dr Tsutomu Arakawa
(Alliance Protein Laboratories, Inc., Camerillo, CA, USA) for his
helpful discussion.
References
|
1
|
Uozaki M, Yamasaki H, Katsuyama Y, Higuchi
M, Higuti T and Koyama AH: Antiviral effect of octyl gallate
against DNA and RNA viruses. Antiviral Res. 73:85–91. 2007.
View Article : Google Scholar
|
|
2
|
Yamasaki H, Tsujimoto K, Koyama AH, Ejima
D and Arakawa T: Arginine facilitates inactivation of enveloped
viruses. J Pharm Sci. 97:3067–3073. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Arakawa T, Yamasaki H, Ikeda K, Ejima D,
Naito T and Koyama AH: Antiviral and virucidal activities of
natural products. Curr Med Chem. 16:2485–2497. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Uozaki M, Ikeda K, Tujimoto K, et al:
Antiviral effects of dehydroascorbic acid. Exp Ther Med. 1:983–986.
2010.PubMed/NCBI
|
|
5
|
Ikeda K, Yamasaki H, Suzuki Y, Koyama AH
and Arakawa T: Novel strategy with acidic arginine solution for the
treatment of influenza A virus infection. Exp Ther Med. 1:251–256.
2010.PubMed/NCBI
|
|
6
|
Ikeda K, Yamasaki H, Minami S, et al:
Arginine inactivates human herpesvirus 2 and inhibits genital
herpesvirus infection. Int J Mol Med. 30:1307–1312. 2012.PubMed/NCBI
|
|
7
|
American Medical Association. General
infection and infestations; influenza. American Medical Association
Family Medical Guide. Clayman CB: 3rd edition. Random House, Inc;
New York, NY: pp. 597–598. 1994
|
|
8
|
Brankston G, Gitterman L, Hirji Z, Lemieux
C and Gardam M: Transmission of influenza a in human beings. Lancet
Infect Dis. 7:257–265. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wright PF, Newman G and Kawaoka Y:
Orthomyxoviruses. Fields Virology. Knipe DM, Howley PM, Griffin DE,
et al: 5th edition. Lippincott Williams and Wilkins; Philadelphia,
PA: pp. 1691–1740. 2007
|
|
10
|
Laevens H, Koenen F, Deluyker H and de
Kruif A: Experimental infection of slaughter pigs with classical
swine fever virus: transmission of the virus, course of the disease
and antibody response. Vet Rec. 145:243–248. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lai MY, Cheng PK and Lim WW: Survival of
severe acute respiratory syndrome coronavirus. Clin Infect Dis.
41:e67–e71. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sakaguchi H, Wada K, Kajioka J, et al:
Maintenance of influenza virus infectivity on the surfaces of
personal protective equipment and clothing used in healthcare
settings. Environ Health Prev Med. 15:344–349. 2010. View Article : Google Scholar :
|
|
13
|
Kurokawa M, Koyama AH, Yasuoka S and
Adachi A: Influenza virus overcomes apoptosis by rapid
multiplication. Int J Mol Med. 3:527–530. 1999.PubMed/NCBI
|
|
14
|
Nishide M, Tsujimoto K, Uozaki M, Ikeda K,
Yamasaki H, Koyama AH and Arakawa T: Effect of electrolytes on
virus inactivation by acidic solutions. Int J Mol Med. 27:803–809.
2011.PubMed/NCBI
|